- 1Department of Anesthesiology and Intensive Care, Astana Medical University, Astana, Kazakhstan
- 2The National Scientific Center of Traumatology and Orthopedics Named After Academician Batpenov N.D., Astana, Kazakhstan
Introduction: Coronavirus infection is a dangerous airborne disease that can lead to serious lung damage. Data on the effectiveness of low-frequency chest vibrations in the treatment of lung diseases are available; however, not so many of them exist. Vibroacoustic pulmonary therapy is a component of physiotherapy that improves lung perfusion and drainage without requiring active patient participation. This study aimed to increase statistical efficiency through maximizing the relevant information obtained from the clinical data. Calculating the sample size to determine the power of subsequent studies was also necessary.
Research methods: A pilot randomized parallel trial involving 60 patients was conducted. The patients were divided into two equal groups, where they received sessions of vibroacoustic pulmonary therapy using the “VibroLung” device in two modes “acute respiratory distress syndrome (ARDS)” and “Pneumonia,” with identical treatment. The patients were > 18 years old with detected COVID-19 by PCR and grade 2 and 3 lung lesions detected by computer tomography (CT). Blood sampling was performed in the morning at the same time before and after the hardware massage to determine PaO2, PaCO2, and P/F.
Results: As a result of the test, the following data were obtained: on the first day in the group using the “ARDS” mode, PaO2 indicators averaged 65, CI 95% [58.6–73.2] and on average 77.5, CI 95% [69.8–85.2], “before” and “after,” respectively, which indicates improved oxygenation after the procedure. However, in the second group with the “Pneumonia” mode after its use, PaCO2 was higher after the session, on average 48.7, CI 95% [40.8–56.6], whereas before that, the following indicators had, on average 43.6, CI 95% [37.2–50].
Conclusion: Thus, the data obtained yielded ambiguous results, which are the basis for further study in future randomized controlled trials. As the treatment of coronavirus infection has no etiological treatment, even small shifts in the therapy of this category of patients can be significant.
Clinical trial registration: ClinicalTrials.gov, identifier NCT05143372.
Introduction
COVID-19 is a highly contagious infectious disease that has had a significant impact worldwide since 2019. COVID-19 continues to affect the human body without requiring any special treatment (1, 2). In addition to the general symptoms of intoxication, the disease course varies from mild-to-severe damage to the lungs and other body systems. The treatment of patients with coronavirus pneumonia requires an adequate comprehensive approach, including physiotherapy (3, 4). The symptoms of this pathology include cough, shortness of breath, and sputum discharge (5). Vibroacoustic lung therapy can be a rational component of physiotherapy in the treatment of respiratory diseases, which, instead of manual massage, saves the time and effort of medical personnel who already have a heavy load (6). This improves perfusion and drainage functions, ultimately improving respiratory activity. Vibroacoustic therapy is of interest in many areas of medicine, there are many questions about the effective parameters of the technique (frequency, amplitude, etc.). The range of applications of vibroacoustic therapy (VAT) is wide, including the treatment of pain, fibromyalgia, neurological pathologies. A preliminary review of the treatment of pain with the use of VAT has shown a positive effect, but more reliable studies and results in this area are needed (7).
A review of 7 studies of patients with cerebral palsy showed a positive effect on motor function when using VAT (8).
In addition, there are studies in favor of low-frequency vibration (0.5–120 Hz) in patients with acute stroke with thrombolysis, dissolution of blood clots, which is important for patients with coronavirus infection (9–11).
The “VibroLung” device was used as a component of physiotherapy during the pilot trial in patients with respiratory diseases and is actively used in hospitals in the Commonwealth of Independent States (CIS) countries (6).
The purpose of this pilot test was to determine the acceptability of vibroacoustic massage.
Information on the topic was unavailable when searching the MEDLINE and Cochrane databases. In the past, when treating a patient with a coronavirus infection and concomitant background, an integrated approach using a vibroacoustic device has shown effectiveness and interest in continuing trials (12).
Materials and methods
The study is a simple, blind, randomized parallel trial. Data were collected from the intensive care unit of the City Infectious Diseases Hospital of Astana, Republic of Kazakhstan, from December 2021 to July 2022.
Inclusion criteria:
• Age > 18 years,
• Confirmed COVID-19 using PCR test,
• The degree of lung damage according to computed tomography: CT-2 (25–50% of lung parenchyma is affected); CT-3 (50–75% of lung parenchyma is affected).
Exclusion criteria:
• Age < 18 years,
• Acute stroke,
• Acute coronary syndrome,
• Traumatic chest injury,
• Infectious processes in the chest area.
Consent to participate in this project was obtained from the participants or their guardians before the intervention. The trial included 60 patients (Supplementary material) diagnosed with pneumonia caused by coronavirus infection, confirmed using computed tomography and PCR tests for the presence of the virus. All the described patients were on a mechanically ventilator. They were divided into two equal groups. In one group, patients underwent vibroacoustic pulmonary therapy using the “VibroLung” device in a mode called “acute respiratory distress syndrome (ARDS)” (main group n = 30), in the other—in the “Pneumonia” mode (comparison group n = 30). In the “ARDS” mode, the physical emphasis is evenly distributed on slow and fast modulations with a frequency of 20 to 300 Hz, which provides both endobronchial resonance and parenchymal effects, but, as is typical for nosology and hyperhydration of the lungs in ARDS, such effects are most effective. In the “Pneumonia” mode, the effect of fast and slow modulations is applied evenly over all frequencies, aimed at draining a multi-caliber tracheobronchial tree–within 120–300 Hz (13).
Both groups had an identical algorithm of action: sessions were conducted six times a day for 5 min for 3 days in combination with treatment in accordance with the protocol for the treatment of patients with coronavirus infection of the Ministry of Health of the Republic of Kazakhstan (14). The effectiveness of the effect increases with an increase in the multiplicity, but not with an increase in the duration of the procedure (session). Effective duration of the procedure: 3–5 min (15).
The emitters of the device were applied to the most affected areas of the patient’s lungs, corresponding to the CT or radiography data, and one or the other mode of the device was turned on. Because the device has long cords for emitters and is portable, the patient’s position does not matter and does not require active participation, which is important for patients undergoing artificial lung ventilation. Immediately before the procedure, arterial blood was collected once in the morning to determine PaO2, PaCO2, and P/F blood, as well as 10 min after the session.
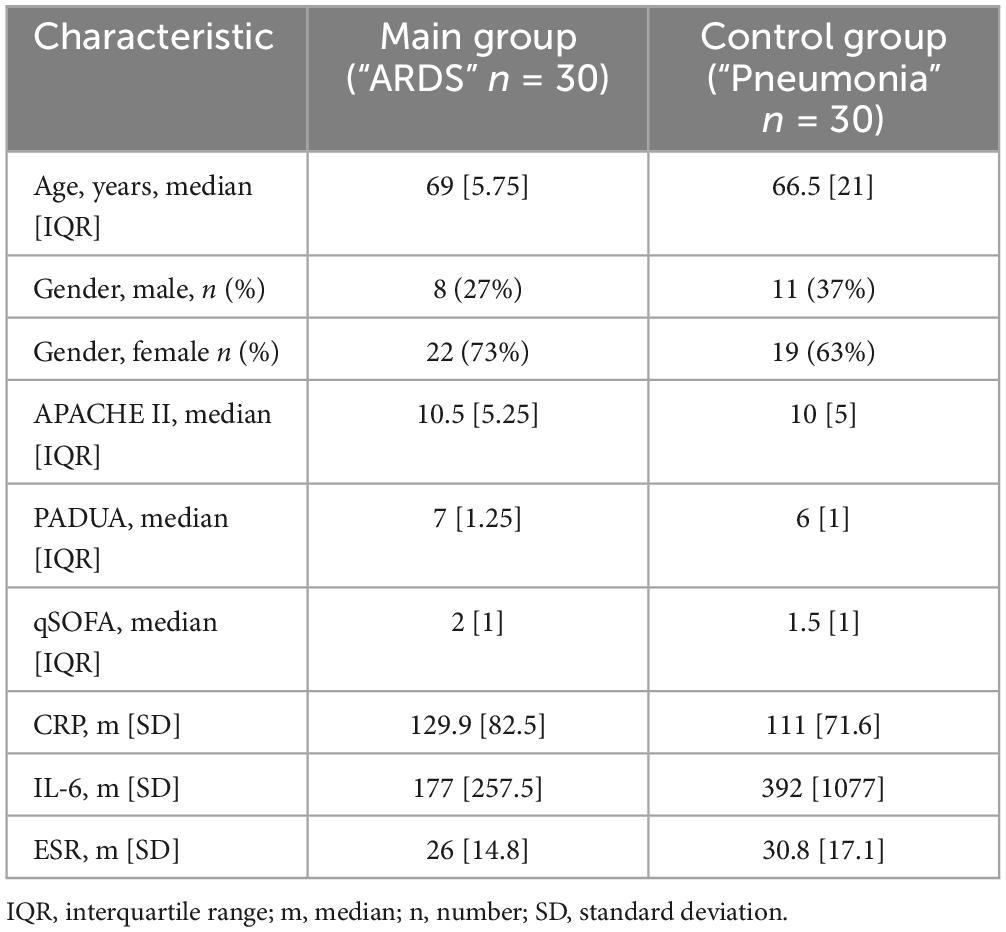
The initial patient data will be shown below (Table 1).
All data were entered into the MC Excel database as patients were registered by the researcher. At the end of the set period, the data were statistically processed.
The sample size was not calculated owing to the uneven admission of patients with coronavirus infection at different times from 2021 to 2022 because of the variability of the peak incidence.
Participants were randomly assigned to either the treatment or comparison group at a 1:1 ratio using a random number generator on the site www.randomizer.org. The researcher handed the medical workers a preprepared opaque envelope with randomly assigned numbers. Owing to the need to select a mode on the device display screen, all medical personnel knew regarding the selected mode when it was hidden from the patient.
Medical workers trained in the procedure and use of the device conducted a session of vibroacoustic therapy, as well as performed blood sampling.
Data were analyzed using the Statistical Package for Social Sciences (SPSS) version 20.
The Kolmogorov–Smirnov criterion was used to determine the normality of data. Student’s t-tests were used only for normally distributed data. In cases with an abnormal distribution, intragroup analysis was performed using the Wilcoxon test in each group before and after VALT.
Ethical approval
The study was approved by the Ethics Committee of the Research Institute of Orthopedics and Traumatology in Astana on 19.11.21 and registered on ClinicalTrials.gov., ID: NCT05143372.
Results
Regarding the initial data of patients in both groups, age and sex did not show large differences, as did scores on the APACHE II, qSOFA, and PADUA scales. Based on laboratory data, patients showed a difference in the mean values (SD) of CRP, IL-6, and ECR (Table 1).
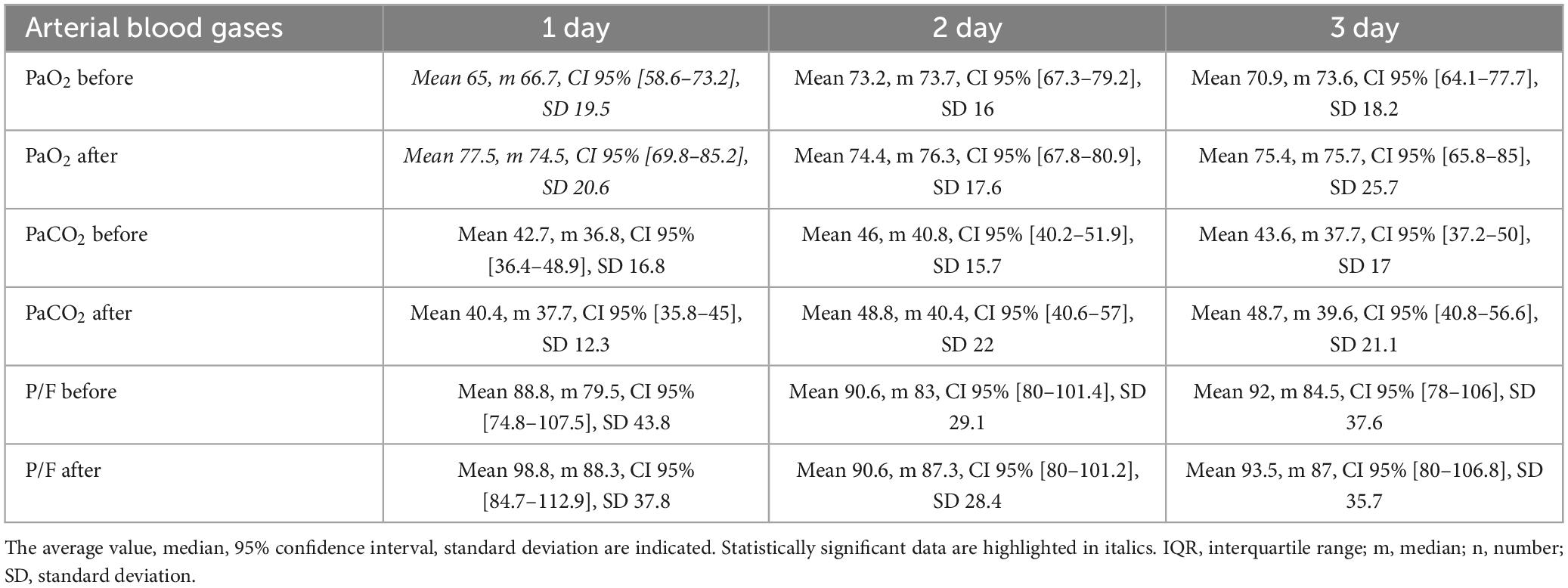
When analyzing the results, the following information was obtained: in the group using the “ARDS” mode, on the first day, the average value of PaO2 increased by 12.5 mmHg. After the procedure, the median increased by 7.8 mmHg, 95% confidence interval: it became [69.8–85.2], and the standard deviation after that was 20.6 mmHg (Table 2).
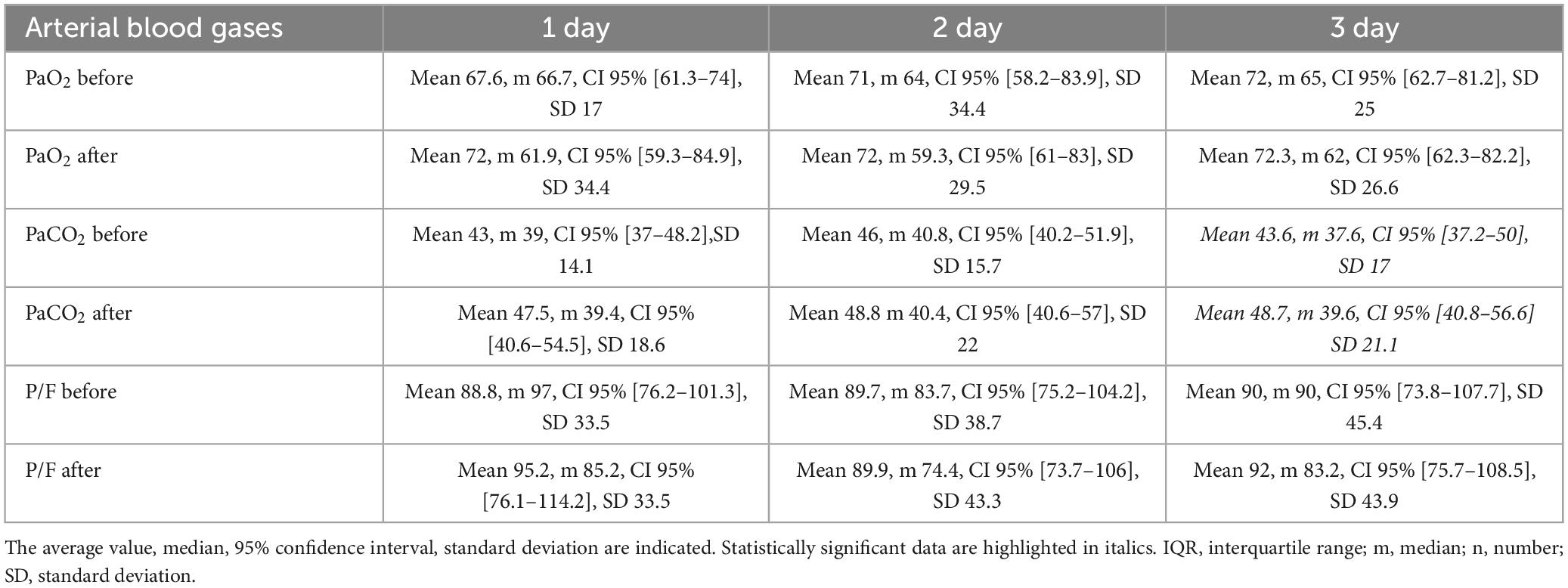
As for the group using the “Pneumonia” mode, the results on the change in the PaCO2 level on the third day were shown and were “Before” average 43.6, m 37.6, CI 95% [37.2–50], SD 17 and “After” mean 48.7, m 39.6, CI 95% [40.8–56.6] SD 21.1. Vibroacoustic pulmonological apparatus was used in this mode (Table 3).
Discussion
The purpose of this study was to determine the acceptability of vibroacoustic pulmonary massage. Taking into account the results obtained, it is necessary to note a certain positive effect of vibroacoustic lung therapy in the treatment of pneumonia in both modes of operation of the device. It should also be noted that in the “ARDS” mode, an improvement in the oxygen content in arterial blood was observed on the first day, whereas in the “Pneumonia” mode, a decrease in carbon dioxide was observed on the third day of receiving VALT sessions. These results are encouraging, but for greater reliability of the results, further study of the field of physiotherapy methods using a larger sample in a randomized controlled trial is necessary. It depends on the power, frequency or other mechanisms of action of the shaft, which have yet to be studied in more depth.
Coronavirus infection differs from other diseases with an extremely high mortality rate worldwide, including in our region, which limits the long-term results of this study.
Another disadvantage is the need to conduct the study in a single clinic. Thus, establishing a causal relationship between the observed changes is difficult.
For a more specific and accurate generalization of the results of the effects of vibroacoustic lung therapy, continuing the study with long-term follow-up is necessary, as the use of vaccines against the virus has reduced the severity of the disease and reduced the mortality of patients (16). Therefore, a multicenter study with a larger sample size is required. COVID-19 has caused enormous harm to the health of the population worldwide, and today, although not in such quantities, cases of the disease remain being registered. Therefore, owing to the lack of etiological treatment, a rational integrated approach is advisable for this category of patients (17, 18). A number of studies have focused on the positive impact and safety of using low-frequency vibrations and vibrations separately on respiratory function and on the body as a whole; however, no combination of them in one device that we attempted to study, including vibration in coronavirus disease exists (19, 20).
Vibroacoustic waves in the form of triangular-shaped modulations with a relatively “slow” period (1.1–10 s) are used for exposure in order to improve ventilation-perfusion ratios, recruitment and drainage of large-caliber bronchi. Vibroacoustic waves of “faster” modulation (0.2–1.0 s) are used to further improve the drainage function of small-caliber bronchi and sawtooth-shaped alveolar sacs with decreasing and increasing frequency. Due to the acoustic properties of the chest, the rapidly decreasing frequency of vibroacoustic waves causes an effect resembling a light tapping on the chest, the rapidly increasing frequency of vibroacoustic waves resembles the effect of soft pressure on the chest, which contributes to the discharge of sputum. According to clinical observations, the frequency range from 20 to 60 Hz most effectively affects the chest. At the same time, the frequency range of vibroacoustic waves of 37–42 Hz for most patients is the most effective in terms of creating maximum pressure fluctuations in the lumen of the large airways (21). To enhance the effect in this frequency segment, a temporary emphasis is placed in all programs. Exposure at higher frequencies is less prolonged and has less time emphasis, because when exposed at higher frequencies, the penetrating power of the sound wave is less. Thus, for effective exposure, the best effect is achieved when exposed to a relatively wide frequency range, regardless of the nature of the pathology. Low-frequency pressure fluctuations of 20–60 Hz (22) in the lumen of the respiratory tract contribute to both a better intake of air into the lungs and drainage function. Low-frequency sound waves probably have an effect on the parietal parenchyma, and the rapidly changing frequency of the signal contributes to a better drainage effect of the small bronchi. The more intense the inflammatory process, the more edematous the pulmonary parenchyma is, respectively, it is more accessible to the penetration of higher frequency sound waves (above 100 Hz). For the most optimal effect in various lung pathologies, executive programs can be more divided into 3 groups, depending on the percentage of elements of fast (with a period of 0.2–1 s) and deep slow (1.1–10 s) frequency modulation, which mainly determines the drainage effect. In pathology, where the drainage effect is not a priority (restrictive pathology), the content of such elements is less. In executive programs that pursue the main goal of improving drainage, the content of such elements is greater. The above information is according to the manufacturer’s manual.
It is worth noting the undesirable effect observed by a medical professional that when using the “ARDS” mode, vibration has greater power and possibly less comfort than when using the “Pneumonia” mode. The device “Vibrolung” was developed by a domestic manufacturer to improve the course and outcomes of respiratory diseases of various etiologies. According to the developer’s instructions, the principle of the shaft effect is based on the generation of an audio signal from a bifocal position by two emitters in the range of 20–300 Hz. The “floating effect” of the sound wave causes a resonant effect, which has a safe and highly effective effect on any kind of lesion of both the lung parenchyma itself and bronchial tree, alveoli, and vessels. The “floating” frequency of the signal allows you to achieve better results with less intensity and exposure time. The resulting vibroacoustic wave causes fluctuations, first of all, of the inhomogeneous parenchyma of the lung and intrapulmonary compartment (edema, mucus, infiltration, hypostatic transudate), which improves drainage, ventilation, and aeration and reduces penetration and spread. With mechanical breathing (ventilator), regular vibroacoustic action reduces the zone of lung collapse and atelectasis due to external pressure, which increases the positive end expiratory pressure (PEEP) without an additional increase in ventilation parameters.
The “ARDS” and “Pneumonia” modes in accordance with the manufacturer’s instructions, differ in indications for use. In this regard, distinctive properties of these schemes when used in patients with coronavirus infection, which has not been done before, have been of interest.
Researchers from CIS countries actively use this component of physiotherapy and publish data on successful results in patients with respiratory pathologies; however, no data on COVID-19 exist (7). Other researchers have reflected on the safety of using oscillator devices in human patients with COVID-19 on artificial lung ventilation (23).
According to the instructions for the device, low-frequency waves and vibrations propagating together cause vibrations of the structural units of the pulmonary parenchyma, thereby improving the perfusion and drainage function of the lungs. The formation of secretions in patients with coronavirus infection occurs in one-third of the cases (24).
As the device is relatively new and not sufficiently widespread, the data do not depend on the effectiveness of its use. Evidence for the positive effect of early physiotherapy on outcomes in patients with respiratory diseases is sufficient, but not in those with coronavirus infection (24–26). Vibration provides rapid evacuation of bronchial secretions, accelerates the gravitational redistribution of intra-pulmonary fluid, and improves ventilation–perfusion ratios (4).
Today, in the period after coronavirus infection, its impact on the respiratory system, rehabilitation, and in this case, vibroacoustic pulmonary therapy is of great importance. New lung physiotherapy devices and infections raise an immeasurable number of questions that require to be addressed.
Conclusion
Thus, the use of vibroacoustic massage in the complex therapy of respiratory diseases may restore bronchial conduction disorders, improve lung ventilation and gas exchange, and improve blood circulation (27–30). Consequently, this can have an impact on faster clinical recovery, reducing the duration of inpatient treatment. Therefore, further multicenter randomized controlled trials are required to confirm the effectiveness of vibroacoustic therapy in this new group of critically ill patients. Moreover, to prove its effectiveness in further studies, introducing this component of physiotherapy for coronavirus infection complicated by respiratory insufficiency into clinical practice for future research in the field of rehabilitation of respiratory disorders after COVID-19 is advisable.
Author’s note
The authors have read the CONSORT 2010 statement: extension to randomized pilot and feasibility trials, and the manuscript was prepared and revised according to the CONSORT 2010 statement: extension to randomized pilot and feasibility trials.
Data availability statement
The original contributions presented in this study are included in this article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The study was approved by the Ethics Committee the National Scientific Center of Traumatology and Orthopedics Named After Batpenov in Astana on 19.11.2021. Written informed consent from patients (guardians) was received.
Authors contributions
AK: conceptualization. AB: review and editing of manuscript. Both authors issued final approval for the version to be submitted.
Acknowledgments
We thank to members of the intensive care unit for the opportunity to conduct research.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2023.1225384/full#supplementary-material
References
1. Cates J, Lucero-Obusan S, Dal RM, Schirmer P, Garg S, Oda G, et al. Risk of nosocomial complications related to COVID-19 and influenza – Veterans Health Administration, United States, October 1, 2018-May 31, 2020. MMWR Morb Mortal Wkly Rep. (2020) 69:15281534. doi: 10.15585/mmwr.mm6942e3
2. World Health Organization.WHO Coronavirus (COVID-19) Dashboard. Geneva: World Health Organization (2021).
3. Warwick WJ, Hansen LG. The long-term effect of high-frequency chest compression therapy on pulmonary complications of cystic fibrosis. Pediatrician Pulmonol. (1991) 11:265–71. doi: 10.1002/ppul.1950110314
4. McNarry MA, Berg RMG, Shelley J, Hudson J, Saynor ZL, Duckers J, et al. Inspiratory muscle training enhances recovery post-COVID-19: a randomized controlled trial. Eur Respir J. (2022) 60:2103101. doi: 10.1183/13993003.03101-2021
5. Smondack P, Gravier F, Prieur G, Repel A, Muir J, Cuvelier A. Physiotherapy and COVID-19. From intensive care unit to home care-An overview of international guidelines. Rev Mal Respir. (2020) 37:811–22. doi: 10.1016/j.rmr.2020.09.001
6. Sabirov DM, Rosstal AL, Makhsudov DR. Vibroacoustic therapy in severe acute respiratory distress syndrome of mixed genesis (clinical observation). Bull Emerg Med. (2021) 2021:14.
7. Kantor J, Campbell EA, Kantorová L, Mareèková J, Regec V, Karasová K, et al. Exploring vibroacoustic therapy in adults experiencing pain: a scoping review. BMJ Open. (2022) 12:e046591. doi: 10.1136/bmjopen-2020-046591
8. Kantor J, Kantorová L, Mareèková J, Peng D, Vilímek Z. Potential of vibroacoustic therapy in persons with cerebral palsy: an advanced narrative review. Int J Environ Res Public Health. (2019) 16:3940. doi: 10.3390/ijerph16203940
9. Hoffmann A, Gill H. External vibration with a frequency of 50 Hz contributes to the dissolution of blood clots in the laboratory. I am. J Biomed Sci. (2012) 4:274–84. doi: 10.5099/aj120400274.
10. Hoffmann A, Gill H. Diastolic synchronized vibro-percussion with a frequency of 50 Hz, conducted through a meat barrier the size of the chest wall, enhances the dissolution of the clot and the effectiveness of remotely administered streptokinase in a model of acute coronary thrombosis in vitro. Tromb J. (2012) 10:23. doi: 10.1186/1477-9560-10-23
11. Dhanesha N, Schnell T, Rahmatalla S, Deshow J, Tedens D, Parker BM, et al. Low-frequency vibrations improve thrombolytic therapy and improve stroke outcomes. To Iron. (2020) 51:1855–61. doi: 10.1161/STROKEAHA.120.029405
12. Bekniyazova A, Kadralinova A, Konkayeva M, Yeltayeva A, Konkayev A. Clinical case: Complex treatment using vibroacoustic therapy in a patient with coinfection and COVID-19. Front Med. (2022) 9:893306. doi: 10.3389/fmed.2022.893306
13. Shchikota AM, Morozova SA, Turova EA, Pogonchenkova IV, Rassulova MA. Capacity of vibroacoustic therapy for correction of respiratory manifestations of post COVID-19 syndrome. Vopr Kurortol Fizioter Lech Fiz Kult. (2022) 99:5–12. doi: 10.17116/kurort2022990615
14. Pya YV, Mukatova IY, Kapyshev TS, Konkayev AK, Bekniyazova AZ. Protocol No. 169 of the Ministry of Health of the Republic of Kazakhstan dated September16, 2022. Vibroacoustic pulmonary therapy. Astana: Ministry of Health of the Republic of Kazakhstan (2022).
15. Eremenko AA, Zyulyaeva TP, Kalinina AA, Rozina NA. Evaluation of effectiveness of vibroacoustic lung massage in self-breathing patients after cardiosurgical operations. Clin Exp Surg. (2020) 8:126–34. doi: 10.33029/2308-1198-2020-8-4-126-134
16. Thompson M, Burgess J, Naleway A, Tyner H, Yoon S, Meece J, et al. Prevention and Attenuation of Covid-19 with the BNT162b2 and mRNA-1273 Vaccines. N Engl J Med. (2021) 385:320–9. doi: 10.1056/NEJMoa2107058
17. Dong E, Du H, Gardner L. Interactive web dashboard for real-time COVID-19 tracking. Lancet Infect Dis. (2020) 20:533–4. doi: 10.1016/S1473-309930120-1
18. Zampogna E, Paneroni M, Belli S, Aliani M, Gandolfo A, Visca D, et al. Pulmonary rehabilitation in patients recovering from COVID-19. Respiration. (2021) 100:416–22. doi: 10.1159/000514387
19. Phillips J, Hing W, Pope R, Canov A, Harley N, Lee AL. Active cycle of breathing technique versus oscillating PEP therapy versus walking with huffing during an acute exacerbation of bronchiectasis: a randomised, controlled trial protocol. BMC Pulm Med. (2023) 23:36. doi: 10.1186/s12890-023-02324-8
20. Chuang ML, Chou YL, Lee CY, Huang SF. Instantaneous response to high frequency vibrations of the chest wall in patients with acute pulmonary respiratory failure receiving artificial ventilation: a randomized controlled trial. Medication. (2017) 96:e5912. doi: 10.1097/MD.0000000000005912
21. Schieppati D, Germon R, Galli F, Rigamonti MG, Stucchi M, Boffito DC. The influence of frequency and amplitude on the viscoelasticity of mucus of a new mechanical-acoustic frequency. Respir Med. (2019) 153:52–9. doi: 10.1016/j.rmed.2019.04.011
22. aetna No: 0067. Chest Physiotherapy and Airway Clearance Devices. (2023). Available online at: https://www.aetna.com/cpb/medical/data/1_99/0067.html
23. Corrêa TD, Matos GFJ, Bravim BA, Cordioli RL, Garrido ADPG, Assuncao MSC. Recommendations for intensive care of critically ill patients with suspected or confirmed COVID-19 infection. Einstein. (2020) 18:eAE5793. doi: 10.31744/einstein_journal/2020AE5793
24. Javaherian M, Shadmehr A, Keshtkar A, Beigmohammadi MT, Dabbaghipour N, Syed A, et al. Safety and efficacy of 256 lung physiotherapy in hospitalized patients with severe pneumonia COVID-19 (PPTCOVID study): A prospective, randomized, single-blind, controlled trial. PLoS One. (2023) 18:e0268428. doi: 10.1371/journal.pone.0268428
25. Hu YL, Ding T. Clinical characteristics of COVID-19 patients in Xiaogan, China: comparison between recent imported cases and earlier local cases. Am J Transl. (2021) 13:11999–11205.
26. Lazzeri M, Lanza A, Bellini R. Respiratory physiotherapy in patients with COVID-19 infection in the acute period: Position paper of the Italian Association of Respiratory Physiotherapists (ARIR) Monaldi Arch. Thoracic dis. (2020) 90:1285.
27. Çelik M, Yayık A, Kerget B, Kerget F, Doymuş O, Aksakal A. High-frequency oscillations of the chest wall in patients with COVID-19: experimental feasibility study of mine. Eurasianjmed. (2022) 54:150–6. doi: 10.5152/eurasianjmed.2022.21048
28. Pancera S, Buraschi R, Bianchi LNC, Porta R, Negrini S, Arienti C. Effectiveness of continuous chest wall vibration with concurrent aerobic training on dyspnea and functional exercise capacity in patients with chronic obstructive pulmonary disease: a randomized controlled trial. Arch Phys Med Rehabil. (2021) 102:1457–64. doi: 10.1016/j.apmr.2021.03.006
29. Braz Júnior DS, Dornelas de Andrade A, Teixeira AS, Cavalcanti CA, Morais AB, Marinho PE. Whole-body vibration improves functional capacity and quality of life in patients with severe chronic obstructive pulmonary disease (COPD): a pilot study. Int J Chron Obstruct Pulmon Dis. (2015) 10:125–32. doi: 10.2147/COPD.S73751
Keywords: COVID-19, vibroacoustic therapy, respiratory insufficiency, physiotherapy, pilot randomized trial
Citation: Konkayev A and Bekniyazova A (2023) Vibroacoustic therapy in the treatment of patients with COVID-19 complicated by respiratory failure: a pilot randomized controlled trial. Front. Med. 10:1225384. doi: 10.3389/fmed.2023.1225384
Received: 19 May 2023; Accepted: 20 November 2023;
Published: 14 December 2023.
Edited by:
Ata Murat Kaynar, University of Pittsburgh, United StatesReviewed by:
Raffaele Campisi, Azienda Ospedaliero Universitaria Policlinico G. Rodolico-San Marco, ItalyJiří Kantor, Palacký University, Olomouc, Czechia
Copyright © 2023 Konkayev and Bekniyazova. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Aidos Konkayev, S29ua2FldjE5QGdtYWlsLmNvbQ==
 Aidos Konkayev
Aidos Konkayev Assema Bekniyazova
Assema Bekniyazova