- 1Department of Medicine and Surgery, University of Parma, Parma, Italy
- 2Faculty of Health and Life Sciences Exeter University, Exeter, United Kingdom
- 3Department of Nursing, University of Suffolk, Ipswich, United Kingdom
This discursive paper focuses on undergraduate medical education’s role in tackling gender bias in clinical practice, specifically preventing and managing from a non-biomedical perspective chronic pain in women. A preliminary web search of medical schools’ curricula was performed to identify programs content related to gender bias in pain management. The web search included 10 universities’ websites selected from the top 10 rankings QS Universities Rankings 2022 for medical schools. Additionally, a questionnaire was sent to all deans of the selected academic institutions to explore the curriculum content further. The web search, and the lack of response from the deans, highlighted that relevant curriculum components on gender bias and chronic pain needed to be implemented. Therefore, this paper introduces an innovative curriculum development approach designed by the multi-professional research team to be implemented in medical school programs. This novel educational strategy could also cross-contaminate other healthcare practitioners’ university programs and, thus, stimulate an interprofessional debate into fostering inclusiveness and equal opportunities in health.
1. Introduction
Medical education has been concerned with providing predominantly undergraduate students with the knowledge of the biophysical determinant of illnesses of the human body (1). With this discursive paper, an interprofessional team of academics and researchers from anthropology, nursing, education, medical science, and public health aimed to design a curriculum development intervention for medical education on psychosocial aspects of health, specifically chronic pain and gender.
Western medicine is transitioning from a clinical and biological model to a new one developed around the more exhaustive definition of health as per the WHO definition that says “...a state of complete well-being, mental and not the mere absence of the state of disease or infirmity.”
The so-called patient-centered medicine aims (2, 3) at placing the person at the center of care and at defining disease not only as a mere organic/physiological dysfunction of the organism (disease) but as a complex phenomenon experienced, both individually (illness) and socially (sickness) (4, 5). Nevertheless, Western medicine remains firmly rooted in biological determinism and the need to rely on data and evidence to offer answers using the most advanced technology. This biological determinism not only shapes medical and operational practices in healthcare settings but also strongly characterizes curricula and university programs attended by healthcare students and professionals. The limits of an exclusively “technical” approach with scant attention to the person emerge clearly when biomedicine is confronted with chronic pain, especially when the patient is female. Chronic pain is an enigma for evidence-based medicine because it is invisible. It cannot be traced objectively and visually in the organism, it cannot be examined by the “medical gaze” (6), and thus it escapes from empirical supervision. However, on the other hand, pain is also an experience (7): it is not a mere physiological sensation but, instead, is the result of an elaboration process of this sensation, where emotional, cognitive, individual, social, cultural, and environmental factors play a central role. In this sense, pain takes shape in the peculiarity of individual biographies, also manifesting itself as a “total” (8), having a multidimensional impact and affecting several aspects of life (psychic, social, relational, etc.). Therefore, pain management should be based on a holistic and personalized care approach. This approach contributes to defining pain as a multidimensional experience shaped by several elements. Among these elements are sex and gender differences that influence health and disease, particularly the processes of pain chronicization (9–12).
Chronic pain primarily affects the female population (13–16). However, most studies investigating pain mechanisms are mainly conducted on the male population (17–20), while physiological mechanisms underlying women’s pain and gender/sex differences are yet to be explored in-depth. The same is true for pharmacology (21, 22): most drugs are tested on the 70-kilo ideal male type, and the recommended dosages refer to this standard, even if women and men have different abilities to metabolize the active ingredients (23).
In literature, and especially in gender medicine studies, it has been repeatedly highlighted how doctors’ scant consideration and preparation for women’s health and female patients’ pain may be responsible for gender bias1 in care settings (23–27). Gender stereotypes influence biomedical ways of analyzing, interpreting, and treating female pain. For instance, several studies have shown that female pain is often underestimated since health professionals tend to frame it as a phenomenon amplified by behavioral and attitudinal traits that are considered to be “typically” females–such as amplified emotionality, psychological vulnerability and dramatization–which would lead them to less tolerate pain and manifest it exaggeratedly (24, 28–30). This leads professionals to be more inclined to interpret the symptoms reported by the male population as organic and those reported by the female population as psychosomatic, underestimating them (31, 32). The invisibility of pain and the difficulty in identifying a specific pathology that causes chronic pain also lead to the stigmatization of women suffering from complex chronic pain syndromes, as is well shown in the literature (29, 30, 33–35). Many women with chronic pain report that they were not believed and that their pain was not treated (29, 33).
The gender biases within a clinician-person relationship can result in a lack of equity and access to care. Literature (24, 36) is rich in examples of such biases. Compared to men, women receive less intensive and effective pain care (37–42). Women are less likely to be prescribed analgesics and opiates (37, 43) and more likely to receive antidepressant prescriptions than men (38). Furthermore, when male and female patients express the same type of pain, female patients are more likely to be referred to psychotherapy, while men receive pharmacological medications (29, 42, 44, 45). Psychologizing women’s chronic pain not only leads to an underestimation of a massive health problem but also has a negative impact on their illness experience; many women, in fact, state that they feel abandoned by health professionals, family members or partners, friends, and colleagues (29, 46).
Physicians’ gender stereotypes are responsible for inequalities in medicine and clinical practice. Research must examine how these stereotypes generate care disparities and influence patient–professional interactions. Therefore, to reduce gender bias, the awareness of values and attitudes toward gender must increase within the medical society. A possible approach is including gender theory and discussions in medical school curricula. However, a growing body of literature shows how gender medicine, specifically women’s health, is almost neglected in the medical schools’ curricula (47, 48). In addition, 70% of postgraduate physicians in training indicated that gender medicine concepts are never or sporadically discussed in their training program (49).
Because sex and gender are health determinants, incorporating these contents into medical curricula could promote a more comprehensive patient-centered approach. Research should focus on understanding how basic pain mechanisms may differ in the two sexes and the diverse ways in which gender differences currently influence diagnostic and treatment decisions. In addition, optimal pain management requires that clinicians understand and examine their gender stereotypes and be prepared to evaluate whether these stereotypes result in less-than-optimal pain management for specific individuals. This paper aims to analyze whether courses centered on gender medicine and, in particular, on female pain are provided in medical schools’ curricula. The paper aims to design a medical school’s curriculum innovation intervention for tackling gender-based health inequalities and fostering a biopsychosocial model for preventing and treating pain.
2. Method
The project implied several explorative steps allowing the research team to reflect on and design a suitable new course aiming at tackling gender bias in pain management in medical students.
The first step consisted of browsing the available web content of 10 worldwide top universities and medical schools (50) programs. Specifically, the web search sought any humanistic or social sciences lectures, training, or awareness courses within the programs selected. This first step was necessary as it is highly probable that interventions or training proposals aimed at raising pain/gender awareness are included in program modules with a humanistic and relational focus. In fact, training medical students to orient their clinical lenses to observe pain as a complex and gendered phenomenon is directly linked with implementing their communication, psycho, and social skills (51, 52). We directed our attention to the manifest content of medical school websites as a retrospective process to help us answer our initial question. Therefore, we explored 10 of the most important worldwide medical schools’ curricula and the available content to uncover to what extent medical curricula may contribute to tackling gender-based health inequalities and promote a non-biomedical approach to managing pain in women.
The second step of the project aimed at collecting more information on the university’s websites mentioned above on the humanistic contents of their programs. A questionnaire was emailed to the Deans for students’ teaching and learning experience and heads of departments of each of the 10 involved medical schools. The research team designed the three open-ended questions to investigate education leaders’ awareness or possibility of foreseeing training on the project topic (Appendix 1). Three separate reminders were sent to elicit a response and maximize participation.
The last step consisted of the course design phase, considering the previous steps’ findings. Therefore, the research team designed an innovative educational program in medical education that combines authors’ different points of view and respective disciplines background.
The study took place under local regulations, and no ethical approval was sought from the university ethics committee. Therefore, no personal and sensitive data were expected to be collected according to the developed questionnaire. Moreover, the invited Deans/heads of the Department have yet to respond to the questionnaire; thus, only literature review data are presented in this article.
3. Results
The research team selected medical schools among the top 10 universities per several continents (Europe, Asia, America, and Canada) according to the Top 10 ranking QS Universities Rankings 2022 (Appendix 2). The team selected three universities per continent, plus one for the United Kingdom. Each university website was searched for downloadable programs and curriculum content. Therefore, the search aimed to detect humanities, social science, anthropology, psychology, sociology, and similar fields elements incorporated in the selected curricula. In addition, any element or suggestion about person-centered care, medical humanities, model of care, communication, and interprofessional approaches was also considered. Universities with these characteristics and access were included. Finally, the accessible university programs and curriculum were analyzed.
The general perception of the programs analyzed was limited space for humanistic content. The number of hours dedicated to these lectures is generally minimal compared to the number of hours devoted to formative sciences and clinical skills. However, this final material selection brought the team’s attention to several crucial aspects. Although supported and preannounced to have a humanistic approach to health, some universities only possess some teaching with this content in the actual program. For example, one university describes its approach to medicine as holistic, but this concept needs to be explained or expanded within the program.
However, the same medical school proposed a course in psychological medicine in the third year. An interesting aspect is represented by an Asian approach for first-year students with a module called a journey to understand myself, society, human beings and human life. Nevertheless, the contents of this very promising module are not accessible, but they give an idea of a more person-centered model. A North American university teaches the “narrative medicine” approach within foundational seminars across all the programs.
Interesting to notice that some academic contexts put the study of communication, medical humanities, or psychology in the first 2 years. At the same time, others dedicate seminars on the same topics in the second part of their pathway when they are more senior. The Canadian model (CANmeds) adopted by two selected universities (Europe and Toronto) is worth mentioning. CANmeds consists of an integrated model of care developed by and for physicians. According to this model, the students approach medicine from the first year in an integrated way, combining clinical skills with aspects of medicine more concerned with relationships and community health.
The response to the second step of our inquiry into medical education was very scarce. The educational leaders have yet to respond to emails containing the brief questionnaire. Therefore, the research team decided to expand the search for references further in postgraduate education courses or training in the medical and health profession. From this last purposive review, the team found specific courses for the medical profession (sometimes open to interprofessionality) that are more focused on gender medicine and pain management. This last fact highlights that, at this moment, the education on topics so sensitive and deep into the human experience of illness is relegated to the ones who are probably already interested in it or looking for further specialization. Among the different courses, Harvard University, with a master’s in public health, designed a course in Gender, Women and Health. In comparison, the University of Aberdeen has a course on Women’s Health in a Global Setting, open to all health professions.
4. Discussion
The findings from this last search inspired the research team to enrich their course proposal, investing in a longitudinal pathway throughout the medical degree.
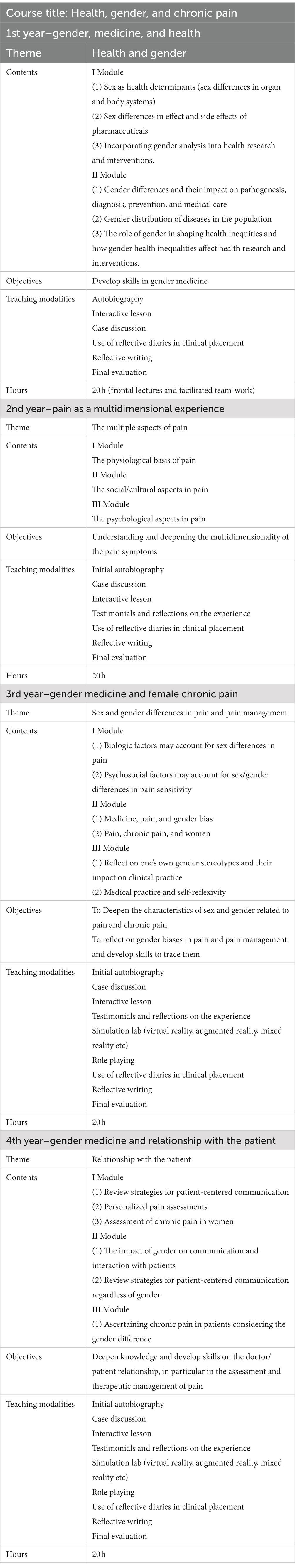
Therefore, this group proposes a foundational course that should become integral to the medical training curriculum. The course should last 4 years, starting from the first year of studies, with consequential modules that deepen, each time, different topics. The authors propose a four-year course considering the average length of medical education programs. In addition, the proposed workshops embedded in each year of study will ensure proportionate integration to student’s clinical practical experience; therefore, this approach will support the student’s progression in a reflective and lifelong learning perspective (53).
The course will consist of a mix of teaching and learning strategies. In addition, the course will provide for each year an analysis of specific initial needs (teachers will also use that to reorient the program) and an assessment of learning, educational impact, and satisfaction at the end of each module. The program is detailed in the table here below.
5. Conclusion
Undergraduate medical students have traditionally been exposed to biophysical-focused curricula with little attention to patients’ needs and expectations. A similar trend has been taking place in clinical research. In addition to a specific focus on biological feedback to new medications and treatments, men represent the predominant population studied.
The predominant role of men in biomedical science has been negatively impacting the delivery of high-quality and personalized medical care to women. Gender bias is equally in place regarding pain assessment and management in the women population. This may drastically impact women’s health and well-being, especially regarding chronic pain and daily living habits. Our purposive literature review and the subsequent exploration of medical schools’ curricula have confirmed this concerning trend. Unfortunately, we could not ascertain relevant practices in this primary educational and medical area as none of the HE institutions we contacted responded to our questionnaire. Furthermore, only 10 universities from the most prestigious academic institutions in the world, as per the Top 10 ranking QS Universities Rankings 2022, were scrutinized. Despite this may constitute a limitation, the research team adopted this strategy due to time constraints and the assumption that world-renowned academic institutions would have posed much more emphasis on gender bias in medical practice and women’s chronic pain management from a non-biomedical perspective.
The proposed educational intervention aims to stimulate a debate within the scientific community and allow the incorporation of a novel approach to limiting the effects of gender bias on future medical practitioners. This innovative approach spreads throughout the undergraduate medical curriculum, ensuring continuity and sustaining an adequate and harmonious development of clinical skills and increased awareness in medical students to manage chronic pain in the female population appropriately. Furthermore, it is worth stressing that gender bias in medical science does not impact negatively only on women’s health as medical science must be as much as possible inclusive, fair, and open to the full spectrum of gender identities.
We recommend this approach in any medical school and curriculum cross-contamination in all other allied health professions university programs in a lifelong interprofessional perspective.
Future studies will include testing the curriculum mentioned above development strategy and exploring its actual and perceived outcomes on the student population.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
Author contributions
CM, EDL, CD’A, and AB contributed to the conception and design of the study. CD’A and CM focused on the introduction section. EDL and AB worked on the methodology. All authors focused on the discussion and the curriculum development intervention and contributed to the manuscript revision, and approval of the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2023.1189126/full#supplementary-material
Footnotes
1. ^By gender bias, we mean the bias generated by stereotypes, i.e., distortions, which occur when gender differences have not been adequately considered. The stereotype (from the Greek “stereos” and “typos,” i.e., “rigid image”) is equivalent to the representation shared by a social group regarding another social group to which characteristics are attributed that derive from approximate generalizations.
References
1. Kelly, M, Ellaway, R, Scherpbier, A, King, N, and Dornan, T. Body pedagogics: embodied learning for the health professions. Med Educ. (2019) 53:967–77. doi: 10.1111/medu.13916
2. Bardes, CL. Defining patient-centered medicine. N Engl J Med. (2012) 366:9. doi: 10.1056/NEJMp1200070
3. Sacristán, JA. Patient-centered medicine and patient-oriented research: improving health outcomes for individual patients. BMC Med Inform Decis Mak. (2013) 13:1. doi: 10.1186/1472-6947-13-6
4. Eisenberg, L. Disease and illness. Distinction between professional and popular ideas of sickness, culture. Med Psychiatry. (1977) 1:9–23. doi: 10.1007/BF00114808
5. Kleinman, A, Eisenberg, L, and Good, B. Culture, illness and care. Clinical lessons from anthropologic and cross-cultural research. Ann Intern Med. (1978) 88:251–8. doi: 10.7326/0003-4819-88-2-251
6. Foucault, M. Nascita della clinica. Il ruolo della medicina nella costituzione delle scienze umane. Torino: Einaudi (1969). 254 p.
7. Raja, SN, Carr, DB, Cohen, M, Finnerup, NB, Flor, H, Gibson, S, et al. The revised International Association for the Study of Pain definition of pain: concepts, challenges, and compromises. Pain. (2020) 161:1976–82. doi: 10.1097/j.pain.0000000000001939
8. Saunders, C. The evolution of palliative care. Patient Educ Couns. (2000) 41:7–13. doi: 10.1016/s0738-3991(00)00110-5
9. Keogh, E. Sex and gender differences in pain: past, present, and future. Pain. (2022) 163:S108–16. doi: 10.1097/j.pain.0000000000002738
10. Bartley, E, and Fillingim, RB. Sex differences in pain: a brief review of clinical and experimental findings. Br J Anaesth. (2013) 111:52–8. doi: 10.1093/bja/aet127
11. Fillingim, RB. Sex, gender, and pain: a review of recent clinical and experimental findings. J Pain. (2009) 10:447–85. doi: 10.1016/j.jpain.2008.12.001
12. Pieretti, S, Giannuario, A, Di Giovannandrea, R, Marzoli, A, Piccaro, G, Minosi, P, et al. Gender differences in pain and its relief. Ann Ist Super Sanità. (2016) 52:184–9. doi: 10.4415/ANN_16_02_09
13. Casale, R, Atzeni, F, Bazzichi, L, Beretta, G, Costantini, E, Sacerdote, P, et al. Pain in women: a perspective review on a relevant clinical issue that deserves prioritization. Pain Ther. (2021) 10:287–314. doi: 10.1007/s40122-021-00244-1
14. Zimmer, Z, Fraser, K, Grol-Prokopczyk, H, and Zajacova, A. A global study of pain prevalence across 52 countries: examining the role of country-level contextual factors. Pain. (2022) 163:1740–50. doi: 10.1097/j.pain.0000000000002557
15. Mills, SEE, Nicolson, KP, and Smith, BH. Chronic pain: a review of its epidemiology and associated factors in population-based studies. Br J Anaesth. (2019) 123:e273–83. doi: 10.1016/j.bja.2019.03.023
16. Umeda, M, and Okifuji, A. Exploring the sex differences in conditioned pain modulation and its biobehavioral determinants in healthy adults. Musculoskelet Sci Pract. (2023) 63:102710. doi: 10.1016/j.msksp.2022.102710
17. Mogil, JS, and Chanda, ML. The case for the inclusion of female subjects in basic science studies of pain. Pain. (2005) 117:1–5. doi: 10.1016/j.pain.2005.06.020
18. Franconi, F, Campesi, I, Colombo, D, and Antonini, P. Sex-gender variable: methodological recommendations for increasing scientific value of clinical studies. Cells. (2019) 8:5. doi: 10.3390/cells8050476
19. Osborne, NR, and Davis, KD. Sex and gender differences in pain. Int Rev Neurobiol. (2022):164. doi: 10.1016/bs.irn.2022.06.013
20. Garattini, S, and Banzi, R. Una medicina che penalizza le donne. Le prove di una scomoda verità e alcune proposte di soluzione. Cinisello Balsamo: Diffusione San Paolo (2022). 266 p.
21. Gobbi, M, Piccirillo, R, and Pasina, L. Differenze di genere negli effetti e nelle interazioni tra farmaci: basi farmacocinetiche e farmacodinamiche In: S Garattini and R Banzi, editors. Una medicina che penalizza le donne. Le prove di una scomoda verità e alcune prospettive di soluzione Cinisello Balsamo: Edizioni San Paolo (2022). 101–37.
22. Banzi, R, and Gerardi, C. L’attenzione al genere nella ricerca e nello sviluppo dei farmaci In: S Garattini and R Banzi, editors. Una medicina che penalizza le donne. Le prove di una scomoda verità e alcune prospettive di soluzione, Cinisello Balsamo: Edizioni San Paolo (2022). 139–62.
23. Pilutti, S, Costa, G, Errico, AD., and Monaco, RD. Prospettive di genere e salute. Dalle disuguaglianze alle differenze (Policy brief). (2016). Available at: https://iris.unito.it/retrieve/handle/2318/1612090/263356/Policy%20brief%20-%20Genere%20e%20Salute.pdf
24. Lloyd, EP, Paganini, GA, and Brinke, L. Gender stereotypes explain disparities in pain care and inform equitable policies. Policy Insights Behav Brain Sci. (2020) 7:198–204. doi: 10.1177/2372732220942894
25. Hamberg, K, Risberg, G, Johansson, EE, and Westman, G. Gender bias in physicians’ management of neck pain: a study of the answers in a Swedish national examination. J Womens Health Gend Based Med. (2002) 11:653–66. doi: 10.1089/152460902760360595
26. Clerc Liaudat, C, Vaucher, P, de Francesco, T, Jaunin-Stalder, N, Herzig, L, Verdon, F, et al. Sex/gender bias in the management of chest pain in ambulatory care. Womens Health. (2018) 14:174550651880564. doi: 10.1177/1745506518805641
27. Leresche, L. Defining gender disparities in pain management. Clin Orthop Relat Res. (2011) 469:1871–7. doi: 10.1007/s11999-010-1759-9
28. Colameco, S, Becker, LA, and Simpson, M. Sex bias in the assessment of patient complaints. J Fam Pract. (1983) 6:1117–21.
29. Samulowitz, A, Gremyr, I, Eriksson, E, and Hensing, G. “Brave men” and “emotional women”: a theory-guided literature review on gender bias in health care and gendered norms towards patients with chronic pain. Pain Res Manage. (2018) 2018:1–14. doi: 10.1155/2018/6358624
30. Moretti, C. Il dolore illegittimo. Un’etnografia della sindrome fibromialgica. Pisa: ETS (2019). 375 p.
31. Riuz, MT, and Verbrugge, LM. A two way view of gender bias in medicine. J Epidemiol Community Health. (1997) 51:106–9. doi: 10.1136/jech.51.2.106
32. Bernstein, B, and Kane, R. Physicians’ attitudes toward female patients. Med Care. (1981) 19:600–8. doi: 10.1097/00005650-198106000-00004
33. Barker, KK. The fibromyalgia story. Medical Authority & Women’s worlds of pain. Philadelphia: Temple University Press (2005). 252 p.
34. Jackson, JE. Stigma, liminality, and chronic pain: mind–body borderlands. Am Ethnol. (2005) 32:332–53. doi: 10.1525/ae.2005.32.3.332
35. Perugino, F, De Angelis, V, Pompili, M, and Martelletti, P. Stigma and chronic pain. Pain Ther. (2022) 11:1085–94. doi: 10.1007/s40122-022-00418-5
36. Majedi, H, Dehghani, SS, Soleyman-Jahi, S, Tafakhori, A, Emami, SA, Mireskandari, M, et al. Assessment of factors predicting inadequate pain Management in Chronic Pain Patients. Anesth Pain Med. (2019) 2019:e97229. doi: 10.5812/aapm.97229
37. Chen, E, Shofer, FS, Dean, AJ, Hollander, JE, Baxt, WG, Robey, JL, et al. Gender disparity in analgesic treatment of emergency department patients with acute abdominal pain. Acad Emerg Med. (2008) 15:414–8. doi: 10.1111/j.1553-2712.2008.00100.x
38. Lord, B, Cui, J, and Kelly, AM. The impact of patient sex on paramedic pain management in the prehospital setting. Am J Emerg Med. (2009) 27:525–9. doi: 10.1016/j.ajem.2008.04.003
39. Hoffmann, DE, and Tarzian, AJ. The girl who cried pain: a bias against women in the treatment of pain. J Law Med Ethics. (2001) 29:13–27. doi: 10.1111/j.1748-720x.2001.tb00037.x
40. Elderkin-Thompson, V, and Waitzkin, H. Differences in clinical communication by gender. J Gen Intern Med. (1999) 14:112–21. doi: 10.1046/j.1525-1497.1999.00296.x
41. Verbrugge, LM. Sex differences in complains and diagnosis. J Behav Med. (1980) 3:327–55. doi: 10.1007/BF00845289
42. McNeill, JA, Sherwood, GD, and Starck, PL. The hidden error of mismanaged pain: a systems approach. J Pain Symptom Manag. (2004) 28:47–58. doi: 10.1016/j.jpainsymman.2003.11.005
43. Donovan, K, Taliaferro, LA, Brock, CW, and Bazargan, S. Sex differences in the adequacy of pain management among patients referred to a multidisciplinary Cancer pain clinic. J Pain Symptom Manag. (2008) 36:167–72. doi: 10.1016/j.jpainsymman.2007.09.013
44. Bernardes, S, Costa, M, and Carvalho, H. Engendering pain management practices: the role of physician sex on chronic low-back pain assessment and treatment prescriptions. J Pain. (2013) 14:931–40. doi: 10.1016/j.jpain.2013.03.004
45. Zhang, L. Gender biases in estimation of others’ pain. J Pain. (2021) 22:1048–59. doi: 10.1016/j.jpain.2021.03.001
46. McManimen, S, McClellan, D, Stoothoff, J, Gleason, K, and Jason, LA. Dismissing chronic illness: a qualitative analysis of negative health care experiences. Health Care Women Int. (2019) 40:241–58. doi: 10.1080/07399332.2018.1521811
47. Khamisy-Farah, R, and Bragazzi, NL. How to integrate sex and gender medicine into medical and allied health profession undergraduate, graduate, and post-graduate education: insights from a rapid systematic literature review and a thematic meta-synthesis. J Pers Med. (2022) 12:4. doi: 10.3390/jpm12040612
48. Miller, VM, Rice, M, Schiebinger, L, Jenkins, MR, Werbinski, J, Núñez, A, et al. Embedding concepts of sex and gender health differences into medical curricula. J Women's Health. (2013) 22:194–202. doi: 10.1089/jwh.2012.4193
49. Jenkins, MR, Herrmann, A, Tashjian, A, Ramineni, T, Ramakrishnan, R, Raef, D, et al. Sex and gender in medical education: a national student survey. Biol Sex Differ. (2016) 7:45. doi: 10.1186/s13293-016-0094-6. eCollection 2016
50. QS World University Rankings. Top Global Universities. Available at: (2023). https://www.topuniversities.com/university-rankings/world-university-rankings/2022 (Accessed March 17 2023).
51. Wald, HS, McFarland, J, and Markovina, I. Medical humanities in medical education and practice. Med Teach. (2019) 41:492–6. doi: 10.1080/0142159X.2018.1497151
52. Adams, ZM, Mekbib, K, Encandela, J, and Reisman, A. Variation in medical humanities program mission statements in United States and Canadian medical schools. Med Teach. (2022) 45:615–22. doi: 10.1080/0142159X.2022.2151886
Keywords: chronic pain, women, gender bias, education, gender medicine
Citation: Moretti C, De Luca E, D’Apice C, Artioli G, Sarli L and Bonacaro A (2023) Gender and sex bias in prevention and clinical treatment of women’s chronic pain: hypotheses of a curriculum development. Front. Med. 10:1189126. doi: 10.3389/fmed.2023.1189126
Edited by:
Maral Tajerian, Queens College (CUNY), United StatesReviewed by:
Catarina Tomé Pires, Autonomous University of Lisbon, PortugalCopyright © 2023 Moretti, De Luca, D’Apice, Artioli, Sarli and Bonacaro. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chiara Moretti, Y2hpYXJhLm1vcmV0dGlAdW5pcHIuaXQ=; Enrico De Luca, RS5EZS1MdWNhQGV4ZXRlci5hYy51aw==
 Chiara Moretti
Chiara Moretti Enrico De Luca
Enrico De Luca Clelia D’Apice
Clelia D’Apice Giovanna Artioli1
Giovanna Artioli1 Leopoldo Sarli
Leopoldo Sarli Antonio Bonacaro
Antonio Bonacaro