
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Med. , 05 June 2023
Sec. Pulmonary Medicine
Volume 10 - 2023 | https://doi.org/10.3389/fmed.2023.1180746
This article is part of the Research Topic Future Research Questions for Improving COPD Diagnosis and Care View all 13 articles
 Anna Lena Jung1,2*
Anna Lena Jung1,2* Maria Han1,3
Maria Han1,3 Kathrin Griss1,4
Kathrin Griss1,4 Wilhelm Bertrams1
Wilhelm Bertrams1 Christoph Nell5
Christoph Nell5 Timm Greulich5
Timm Greulich5 Andreas Klemmer5
Andreas Klemmer5 Hendrik Pott5
Hendrik Pott5 Dominik Heider6,7
Dominik Heider6,7 Claus F. Vogelmeier5
Claus F. Vogelmeier5 Stefan Hippenstiel4
Stefan Hippenstiel4 Norbert Suttorp4
Norbert Suttorp4 Bernd Schmeck1,2,5,7,8
Bernd Schmeck1,2,5,7,8Introduction: Community-acquired pneumonia (CAP) and acute exacerbations of chronic obstructive pulmonary disease (AECOPD) result in high morbidity, mortality, and socio-economic burden. The usage of easily accessible biomarkers informing on disease entity, severity, prognosis, and pathophysiological endotypes is limited in clinical practice. Here, we have analyzed selected plasma markers for their value in differential diagnosis and severity grading in a clinical cohort.
Methods: A pilot cohort of hospitalized patients suffering from CAP (n = 27), AECOPD (n = 10), and healthy subjects (n = 22) were characterized clinically. Clinical scores (PSI, CURB, CRB65, GOLD I-IV, and GOLD ABCD) were obtained, and interleukin-6 (IL-6), interleukin-8 (IL-8), interleukin-2-receptor (IL-2R), lipopolysaccharide-binding protein (LBP), resistin, thrombospondin-1 (TSP-1), lactotransferrin (LTF), neutrophil gelatinase-associated lipocalin (NGAL), neutrophil-elastase-2 (ELA2), hepatocyte growth factor (HGF), soluble Fas (sFas), as well as TNF-related apoptosis-inducing ligand (TRAIL) were measured in plasma.
Results: In CAP patients and healthy volunteers, we found significantly different levels of ELA2, HGF, IL-2R, IL-6, IL-8, LBP, resistin, LTF, and TRAIL. The panel of LBP, sFas, and TRAIL could discriminate between uncomplicated and severe CAP. AECOPD patients showed significantly different levels of LTF and TRAIL compared to healthy subjects. Ensemble feature selection revealed that CAP and AECOPD can be discriminated by IL-6, resistin, together with IL-2R. These factors even allow the differentiation between COPD patients suffering from an exacerbation or pneumonia.
Discussion: Taken together, we identified immune mediators in patient plasma that provide information on differential diagnosis and disease severity and can therefore serve as biomarkers. Further studies are required for validation in bigger cohorts.
Community-acquired pneumonia (CAP) constitutes a crucial cause of morbidity and mortality worldwide, predominantly affecting young children and the elderly (1). Representing the most frequent cause of death due to infection in Europe, CAP accounts for 1 million hospitalizations per year, resulting in 230,000 deaths and socio-economical costs of 10.1 billion € (2–4). Due to the abrupt onset of severe illness, the difficulty in identifying the liable pathogen and the challenge of distinguishing CAP from other acute airway infections, there is an urgent need for easily accessible but specific biomarkers allowing rapid and reliable diagnosis and risk stratification. To date, the diagnosis of CAP mostly relies on chest radiographs and analyses of blood and sputum parameters, as well as auscultation of the lungs and measurement of blood pressure, breathing rate, and recent mental confusion (5). For risk stratification, calculation of clinical scores like CRB65, which are based on defined parameters, roughly allows classification into uncomplicated, moderate, or severe CAP. However, specific biomarkers are still missing (6).
Chronic obstructive pulmonary disease (COPD) represents another highly relevant respiratory disease, being the fourth leading cause of death worldwide with an increasing tendency (7, 8). In Europe, COPD affects about 2–10% of the population and accounts for 3% of all deaths (9). Acute exacerbations of COPD (AECOPD), predominantly caused by viral or bacterial infections, contribute considerably to the burden of the disease. In the United States, AECOPD accounted for 726,000 hospitalizations in 2000, resulting in 119,000 deaths (10) and incurring costs of 30 billion $ (8). Diagnosis of AECOPD mostly relies on increasing cough, sputum, and dyspnoea (11), supported by chest radiographs, blood, and microbiological sputum analyses. Depending on symptoms, AECOPD can be subdivided into type I patients suffering from increasing dyspnoea and optionally sputum, and type II patients with purulent sputum (12). The exacerbation history seems to be the most dependable predictor for future exacerbations (13). As in pneumonia, the availability of reliable biomarkers clearly defining either the entity, stage, or severity of the disease or predicting its progression are of utmost importance.
Biomarkers are classically defined as objectively quantifiable molecules specifically indicating a biological state, which can be physiological or pathogenic, or a response to an expose or (therapeutic) intervention (14). Compared to symptom-based clinical findings, biomarkers have the advantage of allowing a better standardization of measurement and a less investigator-dependent interpretation (15). Due to the variety of molecules, the established handling, and the simplicity of collection, blood is a preferred medium for biomarker analyses (16). At present, the level of C-reactive protein (CRP), the blood sedimentation rate, as well as the leucocyte count, constitute clinical parameters classically indicating inflammation. However, whether this inflammation is of infectious etiology cannot be ascertained (15). Procalcitonin (PCT) represents a current biomarker allowing a more specific discrimination between inflammation of bacterial or non-bacterial origin (17). A potential predictor for mortality in COPD patients is the combination of midrange proadrenomedullin (MR-proADM) and ADO (age, dyspnoea, airflow obstruction), BOD (body mass index, airflow obstruction, dyspnoea) or BODE (body mass index, airflow obstruction, dyspnoea, exercise capability) indices (18, 19). Moreover, MR-proADM could be associated with severe AECOPD but not with CAP (20).
Here, we analyzed selected plasma markers that have been shown to indicate their value as biomarkers for the diagnosis and assessment of the severity of CAP and AECOPD.
Patients with CAP or AECOPD were recruited within 24 h after hospitalization along with healthy controls. Inclusion criteria for patients with CAP included pulmonary infiltrates on chest radiograph and clinical presentation. The inclusion criteria for patients with AECOPD were patients with a previously confirmed diagnosis of COPD and an acute worsening without pulmonary infiltrates on chest radiograph. Patients receiving specific immunosuppressive therapy were excluded from the study, as were pregnant patients and those with human immunodeficiency virus. The BioInflame study was approved by the ethics committee of the Charité – Universitätsmedizin Berlin (no. EA2/030/09) and the University Medical Center Marburg (no. 55/17). All donors were ≥ 18 years of age and provided written informed consent for the use of their blood samples for scientific purposes. Blood plasma was isolated by centrifugation (3,000× g; 10 min at room temperature) of one collected Vacutainer ethylenediaminetetraacetic acid tube. After centrifugation, the plasma phase was transferred and stored at −80°C.
Biomarker measurements were performed in duplicate on stored frozen plasma samples from the day of study enrollment. Plasma levels of IL-6, LBP, and IL-2R were measured using the IMMULITE immunoassay system (Siemens Medical Solutions Diagnostics, Germany). Additionally, plasma levels of ELA2, HGF, IL-6, IL-8, LTF, NGAL, resistin, sFas, TSP-1, and TRAIL were measured with the MILLIPLEX® MAP Human Circulating Cancer Biomarker Magnetic Bead Panel 1 and the MILLIPLEX® MAP Human Sepsis Magnetic Bead Panel 3 (Merck Millipore, Germany) on a Luminex MAGPIX® following the manufacturer’s instructions (Luminex Multiplexing Instrument, Merck Millipore). Biomarker levels below the lowest standard were extrapolated corresponding to the equation of the standard curve.
Statistical analyses were performed using GraphPad Prism version 9.5 (GraphPad software, Inc., CA, United States). Data were analyzed with non-parametric tests. For comparison of two groups, Mann–Whitney U Test was used. If all three groups were compared, Kruskal-Wallis Test followed by a post hoc test (Mann–Whitney U) was used. Receiver Operating Characteristic (ROC) curves were generated to identify biomarkers that clearly distinguish between two groups. To identify a group of parameters that clearly distinguishes between two groups, ensemble feature selection (EFS) was performed.
Importance analysis of the plasma biomarkers and their ranking was performed using EFS at the web-interface1 (21, 22).
Patients and the public were not involved in this study’s design, recruitment and conduct.
We included 27 patients hospitalized with CAP on a regular ward, ten patients with an acute exacerbation of COPD, and 22 healthy controls (Table 1). Samples were taken from all the patients within the first 24 h after hospital admission. The healthy control group was significantly younger than the CAP group, but CAP and AECOPD did not differ significantly. It also contained more female subjects, whereas in the CAP group, men were predominant, and the AECOPD group was balanced in terms of gender. In CAP patients, intermediate severity scores were most frequent, but mild or severe cases were also present (Table 2). All patients underwent routine microbiological testing, but did not show bacterial growth in blood culture and no specific causative pathogen in sputum culture. The majority of CAP patients (n = 17) were prescribed beta-lactam antibiotics, either alone or in combination with a beta-lactamase inhibitor or macrolide. Additionally, five patients received cephalosporine antibiotics, and four patients were prescribed fluoroquinolone antibiotics. In the AECOPD group, most patients experienced at least one exacerbation per year. They showed higher levels of airflow obstruction and breathlessness (Table 3). For AECOPD patients, systemic corticosteroids (oral or intravenous) were administered as the first-line treatment upon hospital admission, followed by antibiotics (amoxicillin/clavulanic acid). Four out of the ten AECOPD patients were already under systemic corticosteroid treatment prior to hospital admission. As COPD patients are more likely to develop pneumonia and suffer from more severe pneumonia (23), the CAP group was subdivided into patients with underlying COPD (n = 8) and without COPD (n = 19) (Table 4). All of the patients included here were effectively treated with appropriate medical care, including antibiotics and supportive measures, and were able to overcome the infection and recover; none of them died.
We performed multiplex analysis of molecules associated with sepsis and tumor diseases to test their significance in plasma samples as biomarkers for the diagnosis of CAP and AECOPD. The individual statistical analysis showed that eight of the twelve analyzed potential biomarkers were differentially expressed in CAP compared to healthy controls. Plasma levels of ELA2, HGF, IL-2R, IL-6, IL-8, LBP, and resistin as well as leukocyte, monocyte, and neutrophil counts were significantly elevated (Figure 1; Supplementary Figure S1). NGAL showed the same trend (p = 0.002). In contrast, levels of LTF and TRAIL were significantly reduced. No significant differences were found for sFas and TSP-1. In AECOPD patients, leukocyte, monocyte, and neutrophil counts were significantly higher compared to healthy controls (Figure 1; Supplementary Figure S1). Levels of LTF and TRAIL were significantly lower. sFas was reduced as well (p = 0.038). Comparing CAP with AECOPD, patients with CAP revealed significantly higher levels of ELA-2, IL-6, resistin, NGAL and CRP. To test whether some biomarkers might be expressed simultaneously, we performed Pearson’s correlation analysis among all significantly expressed proteins and found the best positive correlations between resistin with NGAL and IL-6 with IL-8 (Supplementary Figure S2).
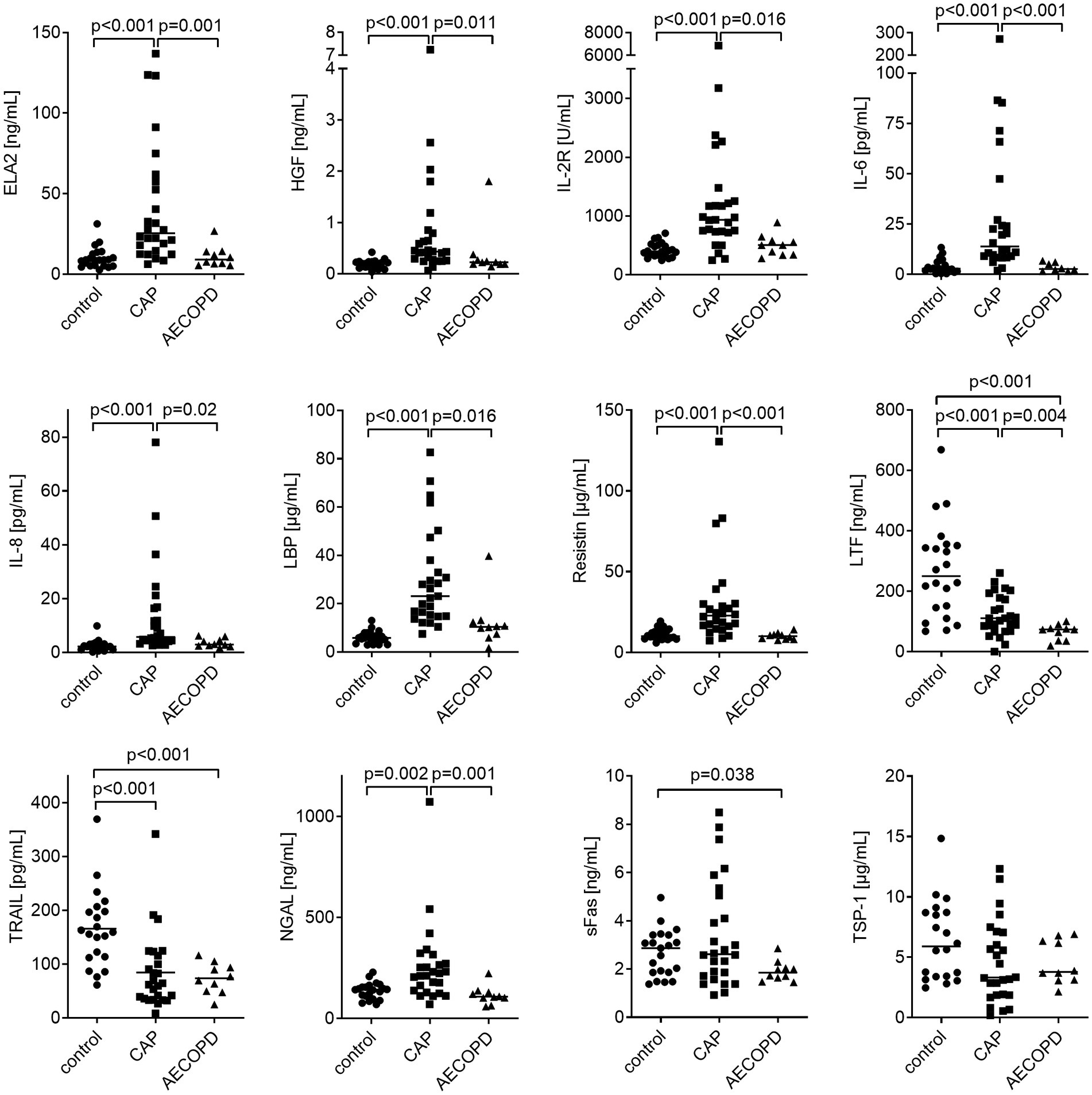
Figure 1. Biomarker expression in plasma samples from CAP and AECOPD patients compared to healthy controls. Data are presented as scatter plots with the median shown as a line. Statistics: Kruskal-Wallis test was performed and p ≤ 0.001 was considered significant.
To augment the diagnostic significance of the analyzed parameters and statistically link each parameter to the prediction of CAP or AECOPD, respectively, we calculated the area under the curve (AUC) of the receiver operating characteristics (ROC) curve for all significantly regulated biomarkers from Figure 1. In CAP patients compared to healthy controls, the AUC values of LBP, IL-8, IL-6, HGF, IL-2R, ELA2, resistin, TRAIL, and LTF had significant p-values, but only the top two (LBP and IL-8) are presented in Figure 2. As the diagnostic potential of a composite of potential biomarkers might be higher than single parameters, feature selection was performed. To this end, EFS was chosen, as it combines eight feature selection methods and thereby improves the prediction performance (21). This multivariate analysis returns the importance of each significantly regulated marker, which are normalized quantifications of the predictive capabilities of the given variables (Figure 2C). The selected features are LBP, IL-6, and IL-2R, which we define as a marker panel for CAP diagnosis.
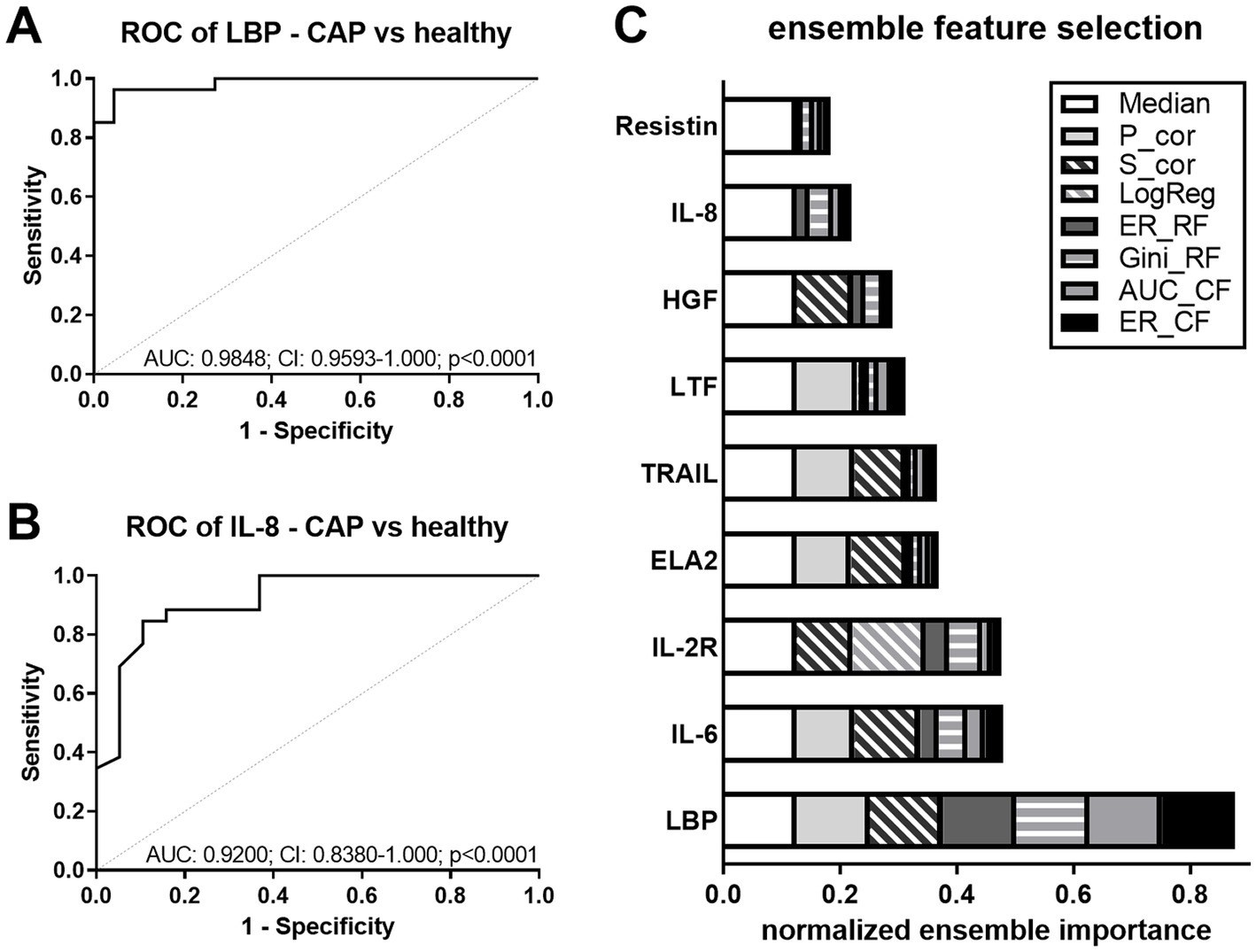
Figure 2. Discrimination between CAP and healthy controls. (A,B) ROC curves for the discrimination between healthy controls and CAP using LBP (A) and IL-8 (B). Dashed line (grey) shows line of identity. AUC, area under the curve; CI, confidence interval, and p-values are depicted in the graphs. (C) Ensemble feature selection for healthy controls and CAP using all significantly regulated biomarkers. The cumulative barplot shows individual features for all feature selection methods. P_cor, Pearson product moment correlation; S_cor, Spearman’s rank correlation; LogReg, logistic regression; ER_RF, error-rate-based variable importance measure embedded in randomForest; Gini_RF, Gini-index-based variable importance measure embedded in randomForest; AUC_CF, area under the curve embedded in cforest; ER_CF, error-rate-based variable importance measure embedded in cforest.
As it is critical in clinical routine to determine which patient has a higher risk to develop a more severe form of pneumonia, we aimed to find plasma markers for this discrimination. We subdivided the CAP patients according to the pneumonia severity index (PSI) risk class (uncomplicated (u) CAP: 1–3; severe (s) CAP: 4–5) and tested whether our collected parameters support this stratification. Smaller group sizes after separation (uCAP: 10; sCAP: 17) precluded robust statistical differentiation between the two groups, but TRAIL emerged as the most appropriate parameter allowing discrimination of uCAP and sCAP with a value of p < 0.05 (Supplementary Figure S3A). In ROC analysis, TRAIL had an AUC of 0.7406 (Supplementary Figure S3B). To combine the power of all measured plasma parameters, EFS was performed. The selected features were LBP, sFas, TRAIL, IL-6, and IL-8, of which LBP ranked highest (0.8) according to its normalized ensemble importance (Supplementary Figure S3C).
To elucidate the diagnostic value of the differentially expressed markers in AECOPD plasma compared to healthy controls, ROC analysis was performed for the significantly regulated biomarkers from Figure 1. AUC values of LTF and TRAIL were > 0.89 with significant p-values (Supplementary Figure S4).
As CAP and AECOPD often exhibit similar symptoms and can be difficult to distinguish, we performed ROC analyses comparing AECOPD and CAP patients based on all significantly regulated plasma proteins from Figure 1. AUC values of IL-6, resistin, NGAL, and ELA2 showed significant p-values, but only the top two (IL-6 and resistin) are presented in Figures 3A,B. Multi-parametric analysis was performed to discriminate CAP from AECOPD. The selected features were IL-6, NGAL, and resistin, of which IL-6 ranked highest (0.78) according to its normalized ensemble importance (Figure 3C).
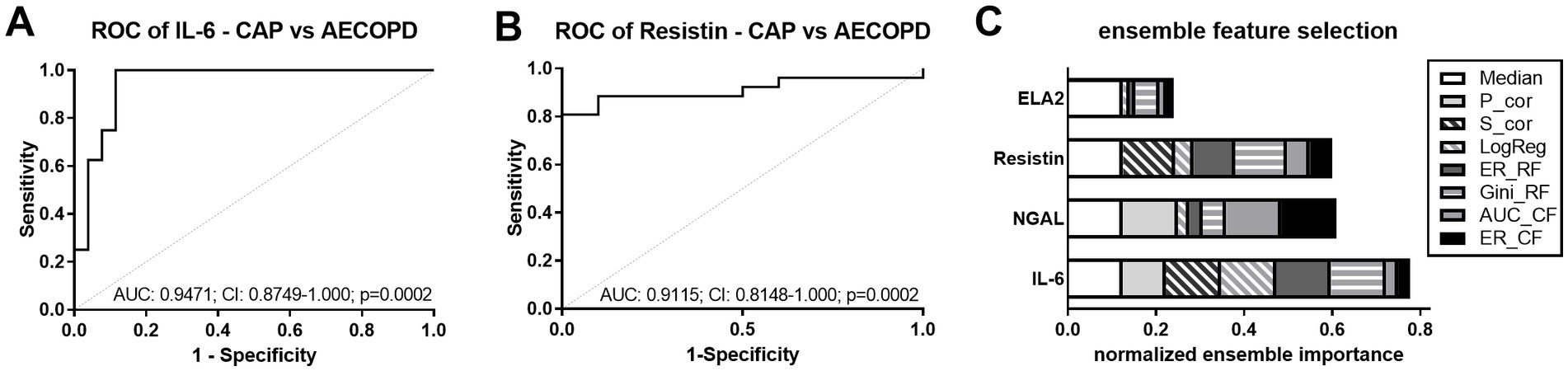
Figure 3. Discrimination between CAP and AECOPD. (A,B) ROC curves for the discrimination between CAP and AECOPD by IL-6 (A) and resistin (B). Dashed line (grey) shows line of identity. AUC, area under the curve; CI, confidence interval and p-values are depicted in the graphs. (C) EFS for CAP and AECOPD for all significantly regulated biomarkers. The cumulative barplot shows individual features for all feature selection methods. P_cor, Pearson product moment correlation; S_cor, Spearman’s rank correlation; LogReg, logistic regression; ER_RF, error-rate-based variable importance measure embedded in randomForest; Gini_RF, Gini-index-based variable importance measure embedded in randomForest; AUC_CF, area under the curve embedded in cforest; ER_CF, error-rate-based variable importance measure embedded in cforest.
The selected features to discriminate CAP and AECOPD from the EFS analysis (Figure 3C) were again tested for their reliability when CAP patients with and without pre-existing COPD were compared to AECOPD patients. IL-6 and resistin were still significantly different when the CAP patient had a pre-existing COPD (Figures 4A–C). The ROC analyses for IL-6, NGAL, and resistin, between AECOPD and CAP+COPD revealed AUCs >0.79 with significant p-values (Figures 4D–F).
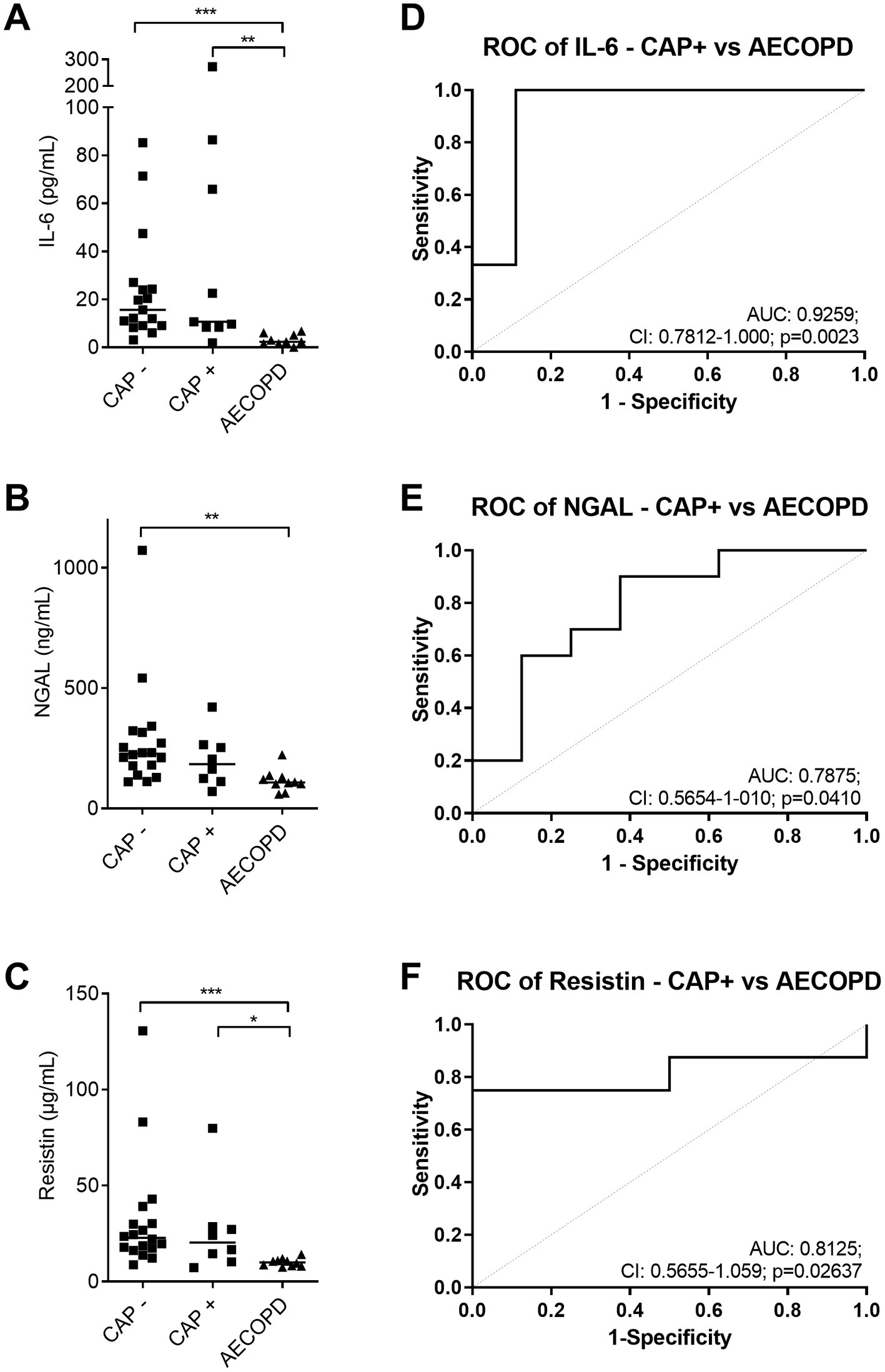
Figure 4. Discrimination between AECOPD and CAP with pre-existing COPD. (A–C) Amount of IL-6 (A), NGAL (B), and resistin (C) in plasma samples from CAP (−/+ COPD) and AECOPD patients. Data are presented as scatter plots and the line shows the median. (D–F) ROC curves for the discrimination between CAP+COPD and AECOPD by IL-6 (D), NGAL (E), and resistin (F). Dashed line (grey) shows line of identity. AUC, area under the curve; CI, confidence interval (CI), and p-value are depicted in the graph. Statistics: Kruskal-Wallis test was performed and p < 0.05 was considered significant (*p < 0.05, **p < 0.01, ***p < 0.001).
In this study, we investigated a set of plasma proteins as potential biomarkers for CAP or AECOPD, respectively.
In CAP patients, we found that the plasma levels of ELA2, HGF, IL-2R, IL-6, IL-8, LBP, and resistin were elevated, while LTF and TRAIL were reduced. Among these, LBP, IL-6, and IL-2R are features for CAP diagnosis, and the combination of LBP, sFas, TRAIL, IL-6, and IL-8 allowed discrimination between uncomplicated and severe forms of pneumonia.
LBP is known to be involved in the acute-phase response against gram-negative bacteria by binding the lipid A moiety of soluble LPS and presenting it to CD14 on cellular membranes. It is mainly produced in the liver and its plasma concentration increases exponentially during acute inflammatory response (24), but it is also found in alveolar fluid (25). It was found that the serum level of LBP was significantly higher in patients with sCAP compared to uCAP and correlated with disease severity, which we also observed. Moreover, LBP has a higher predictive power than CRB-65 (26). Tejera et al. found higher serum levels of LBP in hospitalized CAP patients (27). Likewise, the pro-inflammatory cytokine IL-6 has been found to be increased in CAP patients in other studies. The serum levels of IL-6 were significantly higher in high-risk compared to low-risk CAP patients, and its level correlated with disease severity and decreased on day 3 and 5 after hospitalization (28). Bacci et al. and Andrijevic et al. made similar observations, as IL-6 levels correlated with PSI and CURB score and high IL-6 serum levels were associated with higher lethality of hospitalized patients and decreased from the day of admission to day seven of treatment (29, 30). In our study, IL-6 showed a trend of gradual upregulation with pneumonia severity, it was a selected feature for discrimination between uCAP and sCAP and correlated with the plasma levels of IL-8, which has been described to be significantly higher in sCAP patients compared to milder CAP (30). Soluble IL-2R is a marker for T-cell activation (31). sFas, Fas ligand, and their ratio were associated with a high sepsis-related organ failure assessment (SOFA) score in patients with bacteremia (32). We found it to be decreased in CAP compared to healthy controls but higher in sCAP compared to uCAP. TRAIL is a type II transmembrane protein and belongs to the TNF/TNFR superfamily, which is involved in infection control and the regulation of both innate and adaptive immune responses (33). TRAIL level in airway epithelial cells of COPD patients is elevated (34). The serum concentration of TRAIL has been demonstrated to negatively correlate with pulmonary function (35).
In AECOPD patients, LTF, and TRAIL were significantly reduced in plasma samples, and both had AUC values indicating discriminative potential to differentiate between AECOPD and healthy controls. LTF is an iron-binding protein and provides protection against pathogens and their metabolites. Moreover, it has bactericidal properties that lead to the release of LPS from the outer membrane of gram-negative bacteria (36). It has the capability to enhance phagocytosis of pathogens and cell adherence and controls the release of pro-inflammatory cytokines (37, 38). LTF has been described to be down-regulated in asthmatic patients (39) as observed in our CAP and AECOPD patients.
Since the incidence of pneumonia in COPD patients is almost twice as high as in the general population (40), COPD patients can suffer from both AEs and CAP, which require different clinical treatments and must be differentiated accordingly. This differential diagnosis is traditionally based on radiological findings. It is important to have biological markers to improve the differential diagnosis, reduce unnecessary use of antibiotics, and lower mortality and expenditures for care. Comparing CAP and AECOPD patients, CAP patients had significantly higher levels of IL-6 and CRP. Huerta et al. also observed higher IL-6 levels in CAP patients compared to AECOPD as well (41). EFS revealed that IL-6, NGAL, and resistin are suitable markers for discrimination between AECOPD and CAP, and the discrimination was still possible with these selected features even when the CAP patient additionally suffers from COPD. Resistin, which correlated with NGAL, is an important pro-inflammatory cytokine produced by monocytes and epithelial cells (42). The levels of resistin were higher in sCAP patients compared to uCAP patients, which is in line with the observation that sepsis patients also have elevated levels of resistin (43, 44). Several studies indicate that resistin and NGAL are increased in sepsis patients and serve as markers for disease severity (45–47). Plasma NGAL concentrations increased with severity and could predict mortality (48), which we did not test. NGAL and IL-6 were significantly higher in patients with lower respiratory tract infections compared to healthy controls, but Liu et al. did not observe differences between CAP and AECOPD in their study (49).
The proposed biomarkers for CAP diagnosis and differential diagnosis between CAP and AECOPD should be validated in larger cohorts in the future. As we had significantly younger healthy controls compared to CAP patients, we wanted to exclude the possibility that the increase in their plasma expression was solely due to the difference in age between the two groups. Therefore, we tested for correlation between age and the suggested markers, but did not observe any correlation (all R2 < 0.05; Supplementary Figure S5).
We identified a plasma biomarker panel that shows potential for CAP and AECOPD diagnosis and stratification even in CAP cases with COPD as an underlying disease. Future studies with larger cohorts and a multicentric design are needed for further evaluation.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
BioInflame study was approved by the ethics committee of the Charité–Universitätsmedizin Berlin (no. EA2/030/09) and the University Medical Center Marburg (no. 55/17). The patients/participants provided their written informed consent to participate in this study.
AJ analyzed the data and wrote the manuscript in consultation with WB and BS. KG performed the experiments. CN and DH performed statistical analyses. MH, TG, AK, HP, CV, SH, and NS collected the patient’s material. BS supervised the manuscript. All authors contributed to the article and approved the submitted version.
This work has been funded in part by the Bundesministerium für Bildung und Forschung (Federal Ministry of Education and Research: PermedCOPD – FKZ 01EK2203A; ERACoSysMed2 – SysMed-COPD – FKZ 031L0140; e:Med CAPSYS – FKZ 01ZX1604E), the Deutsche Forschungsgemeinschaft (SFB/TR-84 TP C01), and the von-Behring-Röntgen-Stiftung (66-LV07) to BS, the Deutsche Forschungsgemeinschaft (SFB/TR-84 TP A04/B06) to SH, as well as the Hessisches Ministerium für Wissenschaft und Kunst (LOEWE Diffusible Signals LOEWE-Schwerpunkt Diffusible Signals) to DH, AJ, and BS. Open Access funding provided by the Open Access Publishing Fund of Philipps-Universität Marburg with support of the Deutsche Forschungsgemeinschaft (DFG, German Research Foundation).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2023.1180746/full#supplementary-material
1. Prina, E, Ranzani, OT, and Torres, A. Community-acquired pneumonia. Lancet. (2015) 386:1097–108. doi: 10.1016/S0140-6736(15)60733-4
2. Gibson, GJ, Loddenkemper, R, Lundbäck, B, and Sibille, Y. Respiratory health and disease in Europe: the new European lung white book. Eur Respir J. (2013) 42:559–63. doi: 10.1183/09031936.00105513
3. Nair, H, Brooks, WA, Katz, M, Roca, A, Berkley, JA, Madhi, SA, et al. Global burden of respiratory infections due to seasonal influenza in young children: a systematic review and meta-analysis. Lancet. (2011) 378:1917–30. doi: 10.1016/S0140-6736(11)61051-9
4. Loddenkemper, R, Gibson, GJ, and Sibille, Y. The burden of lung disease in Europe: why a European white book on lung disease? Eur Respir J. (2003) 22:869. doi: 10.1183/09031936.03.0107803
5. van der Poll, T, and Opal, SM. Pathogenesis, treatment, and prevention of pneumococcal pneumonia. Lancet. (2009) 374:1543–56. doi: 10.1016/S0140-6736(09)61114-4
6. Renaud, B, and Santin, A. Severe community acquired pneumonia: what should we predict? Crit Care. (2009) 13:421. doi: 10.1186/cc8111
7. Murray, CJ, and Lopez, AD. Mortality by cause for eight regions of the world: global burden of disease study. Lancet. (1997) 349:1269–76. doi: 10.1016/S0140-6736(96)07493-4
8. Mirza, S, Clay, RD, Koslow, MA, and Scanlon, PD. COPD guidelines: a review of the 2018 GOLD report. Mayo Clin Proc. (2018) 93:1488–502. doi: 10.1016/j.mayocp.2018.05.026
9. WHO. (2011). World health statistics 2011. Available at: https://www.who.int/whosis/whostat/2011/en/
10. Mannino, DM. COPD: epidemiology, prevalence, morbidity and mortality, and disease heterogeneity. Chest. (2002) 121:121S–6S. doi: 10.1378/chest.121.5_suppl.121s
11. Rodriguez-Roisin, R. Toward a consensus definition for COPD exacerbations. Chest. (2000) 117:398S–401S. doi: 10.1378/chest.117.5_suppl_2.398s
12. Stockley, RA. New approaches to the management of COPD. Chest. (2000) 117:58S–62S. doi: 10.1378/chest.117.2_suppl.58s
13. Donaldson, GC, and Wedzicha, JA. COPD exacerbations. 1: epidemiology. Thorax. (2006) 61:164–8. doi: 10.1136/thx.2005.041806
14. Rifai, N, Gillette, MA, and Carr, SA. Protein biomarker discovery and validation: the long and uncertain path to clinical utility. Nat Biotechnol. (2006) 24:971–83. doi: 10.1038/nbt235
15. Schuetz, P, Christ-Crain, M, and Müller, B. Biomarkers to improve diagnostic and prognostic accuracy in systemic infections. Curr Opin Crit Care. (2007) 13:578–85. doi: 10.1097/MCC.0b013e3282c9ac2a
16. Anderson, NL, and Anderson, NG. The human plasma proteome: history, character, and diagnostic prospects. Mol Cell Proteomics. (2002) 1:845–67. doi: 10.1074/mcp.r200007-mcp200
17. Simon, L, Gauvin, F, Amre, DK, Saint-Louis, P, and Lacroix, J. Serum procalcitonin and C-reactive protein levels as markers of bacterial infection: a systematic review and meta-analysis. Clin Infect Dis. (2004) 39:206–17. doi: 10.1086/421997
18. Brusse-Keizer, M, Zuur-Telgen, M, van der Palen, J, VanderValk, P, Kerstjens, H, Boersma, W, et al. Adrenomedullin optimises mortality prediction in COPD patients. Respir Med. (2015) 109:734–42. doi: 10.1016/j.rmed.2015.02.013
19. Stolz, D, Kostikas, K, Blasi, F, Boersma, W, Milenkovic, B, Lacoma, A, et al. Adrenomedullin refines mortality prediction by the BODE index in COPD: the “BODE-A” index. Eur Respir J. (2014) 43:397–408. doi: 10.1183/09031936.0058713
20. Citgez, E, Zuur-Telgen, M, van der Palen, J, van der Valk, P, Stolz, D, and Brusse-Keizer, M. Stable-state midrange proadrenomedullin is associated with severe exacerbations in COPD. Chest. (2018) 154:51–7. doi: 10.1016/j.chest.2018.02.006
21. Neumann, U, Genze, N, and Heider, D. EFS: an ensemble feature selection tool implemented as R-package and web-application. Bio Data Min. (2017) 10:21. doi: 10.1186/s13040-017-0142-8.eCollection2017
22. Neumann, U, Riemenschneider, M, Sowa, JP, Baars, T, Kälsch, J, Canbay, A, et al. Compensation of feature selection biases accompanied with improved predictive performance for binary classification by using a novel ensemble feature selection approach. BioData Min. (2016) 9:36. doi: 10.1186/s13040-016-0114-4
23. Molinos, L, Clemente, MG, Miranda, B, Alvarez, C, del Busto, B, Cocina, BR, et al. Community-acquired pneumonia in patients with and without chronic obstructive pulmonary disease. J Infect. (2009) 58:417–24. doi: 10.1016/j.jinf.2009.03.003
24. Muta, T, and Takeshige, K. Essential roles of CD14 and lipopolysaccharide-binding protein for activation of toll-like receptor (TLR)2 as well as TLR4 reconstitution of TLR2- and TLR4-activation by distinguishable ligands in LPS preparations. Eur J Biochem. (2001) 268:4580–9. doi: 10.1046/j.432-327.2001.02385.x
25. Martin, TR, Mathison, JC, Tobias, PS, Letúrcq, DJ, Moriarty, AM, Maunder, RJ, et al. Lipopolysaccharide binding protein enhances the responsiveness of alveolar macrophages to bacterial lipopolysaccharide. Implications for cytokine production in normal and injured lungs. J Clin Invest. (1992) 90:2209–19. doi: 10.1172/JCI116106
26. Zobel, K, Martus, P, Pletz, MW, Ewig, S, Prediger, M, Welte, T, et al. Interleukin 6, lipopolysaccharide-binding protein and interleukin 10 in the prediction of risk and etiologic patterns in patients with community-acquired pneumonia: results from the German competence network CAPNETZ. BMC Pulm Med. (2012) 12:6. doi: 10.1186/1471-2466-12-6
27. Tejera, A, Santolaria, F, Diez, ML, Alemán-Valls, MR, González-Reimers, E, Martínez-Riera, A, et al. Prognosis of community acquired pneumonia (CAP): value of triggering receptor expressed on myeloid cells-1 (TREM-1) and other mediators of the inflammatory response. Cytokine. (2007) 38:117–23. doi: 10.1016/j.cyto.2007.05.002
28. Antunes, G, Evans, SA, Lordan, JL, and Frew, AJ. Systemic cytokine levels in community-acquired pneumonia and their association with disease severity. Eur Respir J. (2002) 20:990–5. doi: 10.1183/09031936.02.0295102
29. Bacci, MR, Leme, RC, Zing, NP, Murad, N, Adami, F, Hinnig, PF, et al. IL-6 and TNF-α serum levels are associated with early death in community-acquired pneumonia patients. Braz J Med Biol Res. (2015) 48:427–32. doi: 10.1590/1414-431x20144402
30. Andrijevic, I, Matijasevic, J, Andrijevic, L, Kovacevic, T, and Zaric, B. Interleukin-6 and procalcitonin as biomarkers in mortality prediction of hospitalized patients with community acquired pneumonia. Ann Thorac Med. (2014) 9:162–7. doi: 10.4103/1817-737.134072
31. Rubin, LA, and Nelson, DL. The soluble interleukin-2 receptor: biology, function, and clinical application. Ann Intern Med. (1990) 113:619–27. doi: 10.7326/0003-4819-113-8-619
32. Huttunen, R, Syrjänen, J, Vuento, R, Laine, J, Hurme, M, and Aittoniemi, J. Apoptosis markers soluble Fas (sFas), Fas ligand (FasL) and sFas/FasL ratio in patients with bacteremia: a prospective cohort study. J Infect. (2012) 64:276–81. doi: 10.1016/j.jinf.2011.12.006
33. Gyurkovska, V, and Ivanovska, N. Distinct roles of TNF-related apoptosis-inducing ligand (TRAIL) in viral and bacterial infections: from pathogenesis to pathogen clearance. Inflamm Res. (2016) 65:427–37. doi: 10.1007/s00011-016-0934-1
34. Haw, TJ, Starkey, MR, Nair, PM, Pavlidis, S, Liu, G, Nguyen, DH, et al. A pathogenic role for tumor necrosis factor-related apoptosis-inducing ligand in chronic obstructive pulmonary disease. Mucosal Immunol. (2016) 9:859–72. doi: 10.1038/mi.2015.111
35. Wu, Y, Shen, Y, Zhang, J, Wan, C, Wang, T, Xu, D, et al. Increased serum TRAIL and DR5 levels correlated with lung function and inflammation in stable COPD patients. Int J Chron Obstruct Pulmon Dis. (2015) 10:2405–12. doi: 10.2147/COPD.S92260. eCollection 2015
36. Farnaud, S, and Evans, RW. Lactoferrin--a multifunctional protein with antimicrobial properties. Mol Immunol. (2003) 40:395–405. doi: 10.1016/s0161-5890(03)00152-4
37. Adamik, B, Zimecki, M, Właszczyk, A, and Kübler, A. Immunological status of septic and trauma patients. I. High tumor necrosis factor alpha serum levels in septic and trauma patients are not responsible for increased mortality: a prognostic value of serum interleukin 6. Arch Immunol Ther Exp. (1997) 45:169–75.
38. Adamik, B, Zimecki, M, Właszczyk, A, and Kübler, A. Immunological status of septic and trauma patients. II. Proliferative response and production of interleukin 6 and tumor necrosis factor alpha by peripheral blood mononuclear cells from septic survivor, nonsurvivor and trauma patients: a correlation with the survival rate. Arch Immunol Ther Exp. (1997) 45:277–84.
39. Nie, X, Wei, J, Hao, Y, Tao, J, Li, Y, Liu, M, et al. Consistent biomarkers and related pathogenesis underlying asthma revealed by systems biology approach. Int J Mol Sci. (2019) 20:4037. doi: 10.3390/ijms20164037
40. Müllerova, H, Chigbo, C, Hagan, GW, Woodhead, MA, Miravitlles, M, Davis, KJ, et al. The natural history of community-acquired pneumonia in COPD patients: a population database analysis. Respir Med. (2012) 106:1124–33. doi: 10.1016/j.rmed.2012.04.008
41. Huerta, A, Crisafulli, E, Menéndez, R, Martínez, R, Soler, N, Guerrero, M, et al. Pneumonic and nonpneumonic exacerbations of COPD: inflammatory response and clinical characteristics. Chest. (2013) 144:1134–42. doi: 10.1378/chest.13-0488
42. Pang, SS, and Le, YY. Role of resistin in inflammation and inflammation-related diseases. Cell Mol Immunol. (2006) 3:29–34.
43. Yousef, AA, Amr, YM, and Suliman, GA. The diagnostic value of serum leptin monitoring and its correlation with tumor necrosis factor-alpha in critically ill patients: a prospective observational study. Crit Care. (2010) 14:R33. doi: 10.1186/cc8911
44. Robinson, K, Prins, J, and Venkatesh, B. Clinical review: adiponectin biology and its role in inflammation and critical illness. Crit Care. (2011) 15:221. doi: 10.1186/cc10021
45. Sundén-Cullberg, J, Nyström, T, Lee, ML, Mullins, GE, Tokics, L, Andersson, J, et al. Pronounced elevation of resistin correlates with severity of disease in severe sepsis and septic shock. Crit Care Med. (2007) 35:1536–42. doi: 10.1097/01.CCM.0000266536.14736.03
46. Koch, A, Gressner, OA, Sanson, E, Tacke, F, and Trautwein, C. Serum resistin levels in critically ill patients are associated with inflammation, organ dysfunction and metabolism and may predict survival of non-septic patients. Crit Care. (2009) 13:R95. doi: 10.1186/cc7925
47. Macdonald, SP, Stone, SF, Neil, CL, van Eeden, PE, Fatovich, DM, Arendts, G, et al. Sustained elevation of resistin, NGAL and IL-8 are associated with severe sepsis/septic shock in the emergency department. PLoS One. (2014) 9:e110678. doi: 10.1371/journal.pone.0110678
48. Kim, JW, Hong, DY, Lee, KR, Kim, SY, Baek, KJ, and Park, SO. Usefulness of plasma neutrophil gelatinase-associated lipocalin concentration for predicting the severity and mortality of patients with community-acquired pneumonia. Clin Chim Acta. (2016) 462:140–5. doi: 10.1016/j.cca.2016.09.011
Keywords: pneumonia, COPD, acute exacerbation, severity, biomarker, inflammation
Citation: Jung AL, Han M, Griss K, Bertrams W, Nell C, Greulich T, Klemmer A, Pott H, Heider D, Vogelmeier CF, Hippenstiel S, Suttorp N and Schmeck B (2023) Novel protein biomarkers for pneumonia and acute exacerbations in COPD: a pilot study. Front. Med. 10:1180746. doi: 10.3389/fmed.2023.1180746
Received: 06 March 2023; Accepted: 19 May 2023;
Published: 05 June 2023.
Edited by:
Azmy Faisal, Manchester Metropolitan University, United KingdomReviewed by:
Eleni Papakonstantinou, Aristotle University of Thessaloniki, GreeceCopyright © 2023 Jung, Han, Griss, Bertrams, Nell, Greulich, Klemmer, Pott, Heider, Vogelmeier, Hippenstiel, Suttorp and Schmeck. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Anna Lena Jung, YW5uYS5qdW5nQHVuaS1tYXJidXJnLmRl
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.