- 1Department of Ophthalmology, Keio University School of Medicine, Tokyo, Japan
- 2Otake Eye Clinic, Kanagawa, Japan
Purpose: The aim of this study was to explore the association between myopia and dry eye (DE)-related ocular parameters.
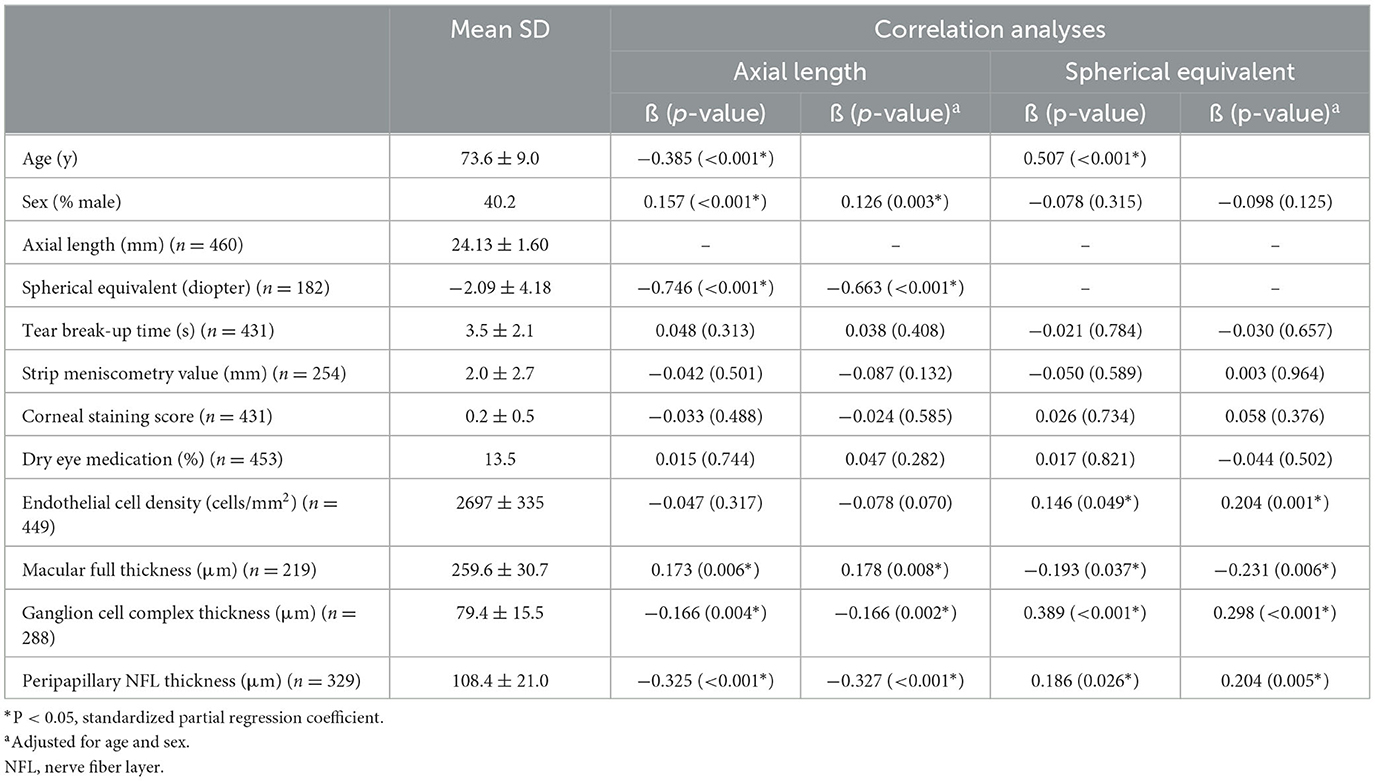
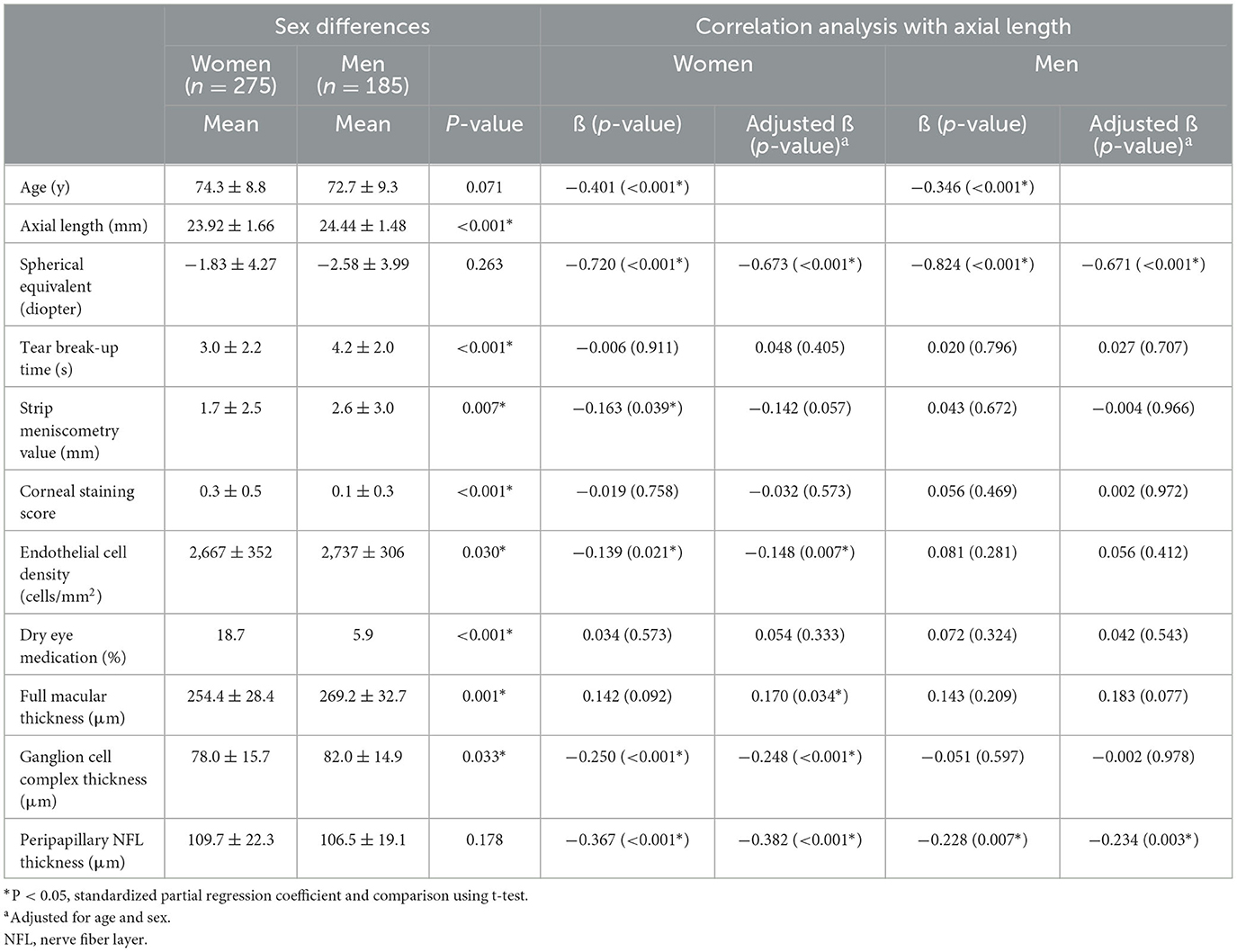
Methods: We recruited a total of 460 patients (mean age, 73.6 years; 40.2% men) and performed DE-related, axial length (AL) and retinal examinations. Statistical analysis revealed a significant sex difference in AL, strip meniscometry value, corneal staining score, corneal endothelial cell density, ganglion cell complex (GCC) thickness, and full macular thickness. AL was strongly age- and sex-dependent, so subsequent analyses were stratified by sex.
Results: Among DE-related parameters, strip meniscometry value (ß = −0.167, p = 0.033) and corneal endothelial cell density (ß = −0.139, p = 0.023) were correlated with AL in women but not in men. Regarding retinal parameters, GCC thickness and full macular thickness were correlated with AL in women but not in men.
Conclusion: The current results suggest a relationship between tear production and AL in elderly women and support the hypothesis that there may be a common upstream factor including the parasympathetic nervous system in the association between tear production and AL or DE and myopia.
Introduction
Growing evidence suggests that dry eye (DE) may be associated with myopia (1–7). We previously reported a possible relationship between DE and myopia on the basis of integrating a DE-related questionnaire, axial length (AL), and myopic error (1). Further research revealed a relationship between tear break-up time (BUT) and choroidal thickness (2), a known parameter of myopia progression (8). Furthermore, a relationship between myopia and DE in younger subjects was suggested in a study examining tear evaporation rate (3) and tear ferning patterns (4), and another study with 682 teenagers demonstrated that BUT was correlated with myopic error (5).
AL elongates in myopia, which may lead to exposure keratitis such as in thyroid eye disease (9, 10). However, the association between AL elongation and the worsening of DE symptoms in healthy subjects is not fully determined. As AL increases after adolescence in high myopia, this relationship may be also observed in the elderly (11, 12). Our previous observational study examined the longitudinal change in the AL of eyes implanted with either a violet light-filtering or non-filtering intra-ocular lens (11). We found greater AL elongation with a violet light-filtering lens possibly due to the suppressive effect of violet light on AL elongation described previously (13). In contrast, an epidemiological study found that refractive status shifted to hyperopic with age (14), and it is generally believed AL stops increasing after the age of 20 years (15). The observed refractive difference between adolescents and older populations might partly be explained by the fact that children spend less time outdoors and more time near work (16). In fact, a survey in Hungary revealed a 3-fold increase in the prevalence of myopia in a young population compared to the elderly (16). Longitudinal data on AL in the general population is not available, and changes in AL in adulthood have not been determined.
DE is a prevalent geriatric ocular surface disease. It has recently been defined as a multifactorial disease characterized by a persistently unstable and/or deficient tear film causing discomfort and/or visual impairment, accompanied by variable degrees of ocular surface epitheliopathy, inflammation, and neurosensory abnormalities (17). Decreased lacrimal secretion leads to aqueous tear deficiency and is a typical clinical manifestation of DE in addition to excessive tear evaporation and shortened BUT. BUT is a complex indicator because it is influenced by tear secretion, cornea, and eyelid (meibomian gland). The measurement of tear secretion reflects the aqueous tear component and can be conveniently done by tear strip meniscometry (18, 19). It is a simple test for measuring lower tear meniscus volume and could be a relevant parameter in assessing the relationship between DE and myopia.
The aim of this study was to explore the association between myopia and DE-related ocular parameters based on tear strip meniscometry, BUT, and retinal thickness measured with optical coherence tomography (OCT) and AL. We selected an older population to complement results from previous studies of children and younger subjects (1–7).
Methods
Recruitment of patients and Institutional Review Board approval
We consecutively recruited outpatients for preoperative evaluation and postoperative follow-up at Otake Eye Clinic and Tsukuba Central Hospital in Japan from January 2019 to August 2022. The Institutional Review Board and Ethics Committee of the Tsukuba Central Hospital (approved on 12 December 2014, permission number 141201) and Kanagawa Medical Association (approved on 12 November 2018, permission number krec2059006) approved the study, and it was carried out in accordance with the Declaration of Helsinki. The need for informed consent was waived by the Institutional Review Board of the Tsukuba Central Hospital and the Institutional Review Board of the Kanagawa Medical Association since it was conducted in an opt-out fashion.
The Institutional Review Board and Ethics Committee of Keio University School of Medicine approved this study (approval date 28 June 2021; approval number 20210080) to permit authorship for authors (KN, HT, EY, and MA) who were appointed at the Keio University School of Medicine.
Inclusion and exclusion criteria
Outpatients aged 40 years or older with a measurement of AL and best-corrected visual acuity better than 20/30 in both eyes were consecutively enrolled during the study period. Patients with glaucoma, optic neuropathy, and retinal degeneration were excluded. Macular diseases including age-related macular degeneration, epiretinal membrane, and macular edema were also excluded from analysis since they are significantly associated with macular thickness (20). Contact lens wearers were excluded as contact lenses may contribute to DE (21, 22). None of the patients had undergone any non-medical interventions on the ocular surface, such as punctal plug insertion or punctal occlusion, or any surgical interventions within 6 months prior to being included.
Ophthalmological examinations
Board-certified ophthalmologists tested subjects with tear strip meniscometry and vital corneal staining. Detailed procedures have been described previously (18). Strip meniscometry is a new non-invasive lacrimal function test to measure lower tear meniscus volume in 5 s using SMTube strips (Echo Electricity Co., Ltd., Fukushima, Japan) (18, 19). The tip of the SMTube strip is gently immersed into the lower tear meniscus, and the resting tear is absorbed into the column part of the SMTube strip with the tear propagation path stained by blue dye. Although the Schirmer test is a gold standard for evaluating tear production (23, 24), we used tear strip meniscometry to measure tear meniscus volume. We chose this method for being a 5 s non-invasive procedure and for producing results with a statistically significant linear correlation not only with subjective symptoms but also with the Schirmer test value, tear meniscus height measurement by anterior optical coherence tomography, BUT, and corneal staining score (18, 19). It is minimally invasive and the relatively quick examination can minimize reflex tearing. AL was measured using the IOLMaster 700 (Carl Zeiss Meditec AG, Jena, Germany). The corneal endothelial cell density was measured with NONCON ROBO II (Konan Medical, Nishinomiya, Japan).
OCT measurement
Spectral domain OCT data were obtained using the RS 3000R (Nidek Co. Ltd., Aichi, Japan), and all OCT imaging was performed using the raster-scan protocol (25). A macular ganglion cell complex (GCC) [retinal nerve fiber layer (RNFL) + ganglion cell layer (GCL) + inner plexiform layer (IPL)] diameter of 9 mm and full retinal thickness in the central macular area diameter of 1 mm were analyzed. Using software supplied by the manufacturer, the thickness of (i) NFL, (ii) GCL + IPL, (iii) internal limiting membrane (INL) + outer plexiform layer (OPL), (iv) ONL + inner segment layer (IS), and (v) outer segment layer (OS) + retinal pigment epithelium (RPE) were exported as a pixel image (512 × 128 pixels), and the mean thickness values of the whole analysis area (9.0 × 9.0 mm, corrected for axial length) excluding the optic disk and peripapillary atrophy were calculated.
Statistical analysis
Data are given as the mean ± SD, where appropriate. Macular measurements of patients with macular disease (age-related macular degeneration and epiretinal membrane) were excluded from the analysis. Data from the left eye were analyzed. To identify which ophthalmic parameters were correlated with AL and phakic refraction, regression analysis was conducted with AL and refraction as dependent variables, while demographic (age and sex) and ophthalmic parameters (myopia-related parameters and DE-related parameters) were used as independent variables. Sex differences were identified, and all subsequent analyses were conducted after stratification by sex. The regression line and probability ellipse were computed for axial length and variables by the least-squares method. The correlation was analyzed using Pearson's correlation coefficient. All analyses were performed using StatFlexR (Atech, Osaka, Japan) with a P-value of < 0.05 considered to be statistically significant.
Results
A total of 460 outpatients (40.2% men, mean age of 73.6 ± 9.0 years, range 46–96 years) were enrolled. Of these, 43.1% were pseudophakic, and 5.7% took DE medication. There was no difference between phakic and pseudophakic cases in relation to BUT (p = 0.846, 3.5 ± 2.1 mm in phakic and 3.5 ± 2.2 in pseudophakic), corneal staining score (p = 0.476, 0.2 ± 0.4 and 0.2 ± 0.4), and meniscometry value (p = 0.067, 2.4 ± 2.4 mm and 1.7 ± 2.7). Regression analysis revealed that+ both AL and phakic spherical equivalent were correlated with corneal endothelial density and retinal thickness but not with DE-related parameters (Table 1).
We identified significant sex differences in BUT, strip meniscometry value, corneal staining score, corneal endothelial cell density, AL, GCC thickness, and full macular thickness (Table 2). AL was strongly age- and sex-dependent (Table 1 and Figure 1), which is why we stratified by sex in subsequent analyses (Table 2). Strip meniscometry value (ß = −0.163, p = 0.039; Figure 2) and corneal endothelial cell density (ß = −0.139, p = 0.021; Figure 3) were correlated with AL in women but not in men. Regarding retinal parameters, GCC thickness (ß = −0.250, p < 0.001; Figure 4) and full macular thickness (ß = −0.170, p = 0.034, adjusted for age) were correlated with AL in women but not in men. The correlation of peripapillary NFL thickness and AL was observed in both sexes (Figure 5).
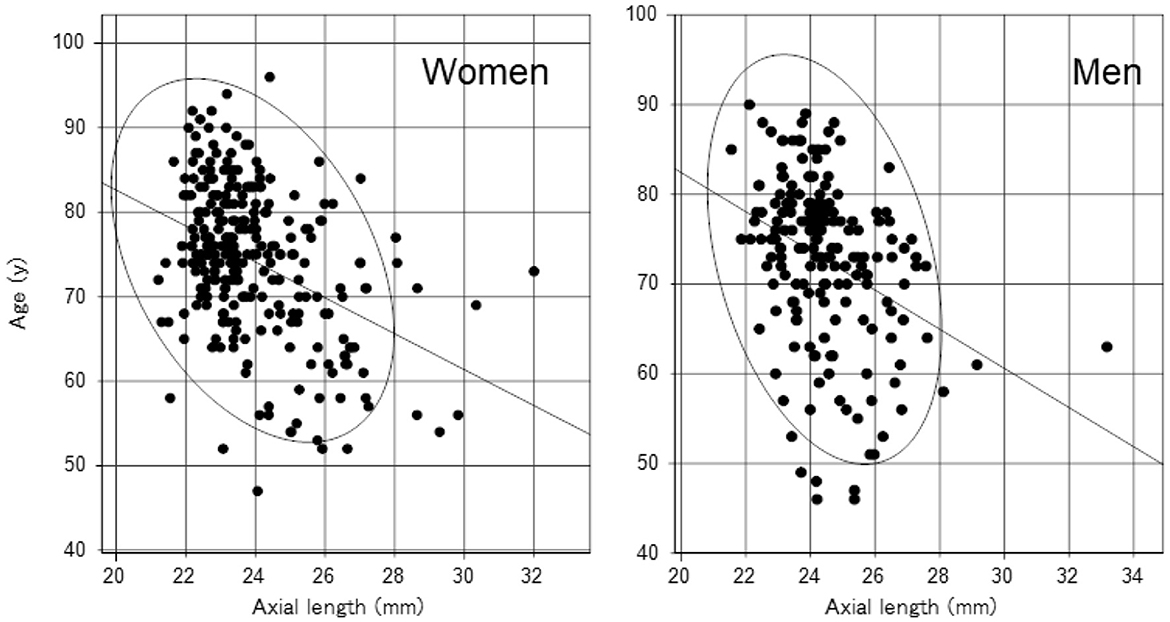
Figure 1. Scatter plots and regression lines of an age-related decrease in axial length with a probability ellipse (confidence interval 95%). Age correlated with axial length in women (ß = −0.401, p < 0.001) and men (ß = −0.346, p < 0.001). The regression line and probability ellipse were computed for axial length and variables by the least-squares method in Figures 1–5. Correlation was analyzed using the Pearson's correlation coefficient in Table 2.
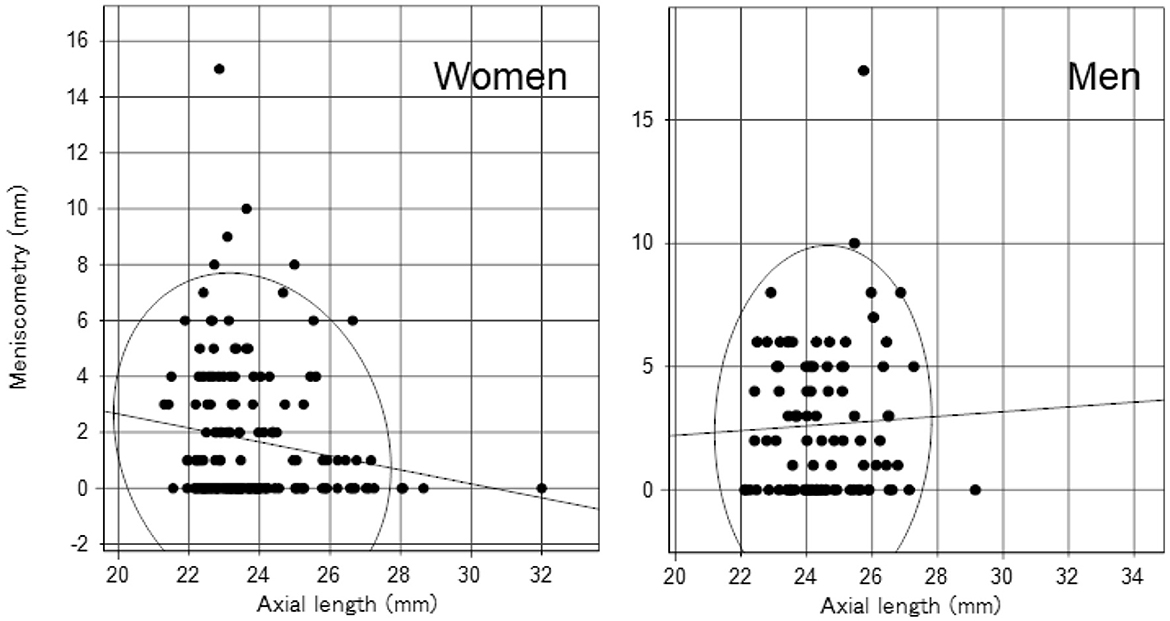
Figure 2. Scatter plots and regression lines of axial length and tear strip meniscometry value with a probability ellipse (confidence interval 95%). Axial length correlated with tear strip meniscometry in women (ß = −0.163, p = 0.039) but not in men (ß = 0.043, p = 0.672).

Figure 3. Scatter plots and regression lines of axial length and corneal endothelial cell density with a probability ellipse (confidence interval 95%). Axial length correlated with corneal endothelial cell density in women (ß = −0.139, p = 0.021) but not in men (ß = 0.081, p = 0.281).

Figure 4. Scatter plots and regression lines of axial length and GCC (ganglion cell complex) thickness with a probability ellipse (confidence interval 95%). Axial length correlated with GCC thickness in women (ß = −0.250, p < 0.001) but not in men (ß = −0.051, p = 0.597).

Figure 5. Scatter plots and regression lines of axial length and peripapillary nerve fiber layer (NFL) thickness with a probability ellipse (confidence interval 95%). Axial length correlated with NFL thickness in women (ß = −0.367, p < 0.001) and men (ß = −0.228, p = 0.007).
Discussion
Findings in the present study agree with prior studies (2–4) where lacrimal and corneal examination results indicate a substantial relationship between myopia and DE. The current results obtained in elderly patients could support the relationship between myopia and DE since tear production measurement is strongly linked to the proposed hypothesis that the parasympathetic nervous system might be involved in the relationship between these two ocular conditions (2). The ocular surface in older patients is much more complicated and disturbed compared with younger subjects, possibly by previous cataract surgery, conjunctivochalasis, and meibomian gland dysfunction although there was no difference between phakic and pseudophakic cases in relation to BUT, corneal staining score, and meniscometry value. Therefore, it would be acceptable if the results contradicted previous results (2) showing a clear association between BUT and AL. Nevertheless, the present results are noteworthy suggesting a significant correlation between tear production and AL in elderly women.
The lacrimal gland is innervated from the parasympathetic nervous system (26–28). The parasympathetic nervous system is also closely associated with choroidal thickness, which is involved in modulating ocular elongation and control of the refractive error (29–31). Tear meniscus volume as a proxy of lacrimal gland activity can be measured by tear strip meniscometry without reflex lacrimation and is a sensitive indicator of ocular surface dryness correlated with BUT and the Schirmer test (18). Taken together, the current results agree with the hypothesis (2) that there may be a common upstream factor including the parasympathetic nervous system in the association between tear production and AL or DE and myopia. Evidence from basic and clinical research has not been able to fully elucidate the association between dry eye and myopia. Although some clinical studies have shown a relationship between dry eye and myopia, the causal relationship is still unknown. It is speculated that the parasympathetic system is involved; however, more nuanced hypotheses should be proposed in further studies on the subject.
In our study, AL decreased with age, which is consistent with prior studies including a large Japanese study (32–34). Cataracts develop earlier in high myopes and could introduce a bias in the current study that included many cataract patients. However, our results were clear and comparable with prior large studies.
Corneal endothelial cell density was low and correlated with AL in women, which was consistent with previous research (35, 36) describing lower endothelial cell density and higher hexagonality and coefficient of variation in women. The authors speculated that the abnormalities of endothelial parameters in female participants might be associated with a different susceptibilities of the endothelial cells, which may explain the relationship between high myopia and abnormal endothelial morphology in female participants in their study. Another group (37, 38) observed an accelerated reduction of endothelial cell density and corneal nerve damage in DE compared with non-DE and suggested that chronic inflammation involving the deep cornea and/or aqueous humor may play a role. As DE is more prevalent in women, this hypothesis could be applicable to our results.
Hanyuda et al. indicated that the correlation of posterior vitreous detachment and AL with female sex may be due to hormonal factors (39). They suggested it may be partly attributed to vitreous liquefaction followed by perimenopausal hormonal changes. In our study, peripapillary NFL thickness was correlated with AL in both sexes, in line with previous research. Nevertheless, macular full thickness and GCC thickness were correlated with AL in women only, suggesting AL may more strongly contribute to retinal thickness in women than men. A possible explanation of these unexpected results is that the peripapillary NFL may be affected by AL rather than sex differences although the detailed reason is unclear. It has been repeatedly documented that the retina is thinner in women than men and thinner in myopia than emmetropia (40, 41); however, sex differences in the association of AL and retinal thickness have not been fully determined. Overall, the current study confirms sex differences in AL, corneal endothelial cell density, and retinal thickness. A further study with a large number of non-surgical cases would be warranted to confirm these findings.
This study reveals a relationship between myopia and DE in elderly subjects that had previously been suggested in young subjects. Consequently, the current results could support the hypothesis that tear production and AL or DE and myopia may share a common upstream factor including the parasympathetic nervous system. This research subject is new and requires further study of the different factors involved and optimal methodology to provide conclusive evidence.
The current study has several limitations. We included patients with pseudophakic eyes who might have retained ocular surface modifications even after a long postoperative period (42). Additionally, aging eyes undergo a variety of changes, including decreased tear secretion and poor lacrimal drainage, which could affect DE-related examination results. DE is a systemic disease which correlates with age and hormone levels. This study does not discern the influence of hormone levels and other confounding factors on DE. Further investigations would be warranted to assess hormone levels and other DE-related systemic parameters for determining the association of DE and myopia. Nevertheless, tear strip meniscometry is a sensitive indicator for the severity of aqueous tear deficiency type DE. In spite of these limitations, our results in elderly subjects confirm a relationship between myopia and DE that has previously been established in young subjects.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Tsukuba Central Hospital and Kanagawa Medical Association. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author contributions
MA designed the study, collected data, analyzed data, and wrote manuscript. All authors reviewed and approved final version of the manuscript.
Acknowledgments
We appreciate Dr. Toshihide Kurihara for valuable scientific contribution. We thank Yo Tanida CO, Akiko Murakami CO, and Mico Arai CO for technical assistance.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Yotsukura E, Torii H, Inokuchi M, Tokumura M, Uchino M, Nakamura K, et al. Current prevalence of myopia and association of myopia with environmental factors among schoolchildren in Japan. JAMA Ophthalmol. (2019) 137:1233–9. doi: 10.1001/jamaophthalmol.2019.3103
2. Hazra D, Yotsukura E, Torii H, Mori K, Maruyama T, Ogawa M, et al. Relation between dry eye and myopia based on tear film breakup time, higher order aberration, choroidal thickness, and axial length. Sci Rep. (2022) 12:10891. doi: 10.1038/s41598-022-15023-x
3. Fagehi R, El-Hiti GA, Alsubaie MH, Abusharha A, Alanazi MA, Masmali AM, et al. Measurements of tear evaporation rate in subjects with refractive errors using a portable evaporimeter. Healthcare. (2022) 10:405. doi: 10.3390/healthcare10020405
4. Alanazi MA, El-Hiti GA, Al-Madani A, Fagehi R. Analysis of tear ferning patterns in young female subjects with refractive errors. J Ophthalmol. (2021) 2021:9524143. doi: 10.1155/2021/9524143
5. Ibrahim-Hirayama OM, Ayaki M, Yotsukura E, Torii H, Negishi K. Dry Eye Disease and High Myopia in Teenagers; a Reciprocal Relationship. ARVO annual meeting abstract number 1442, Denver, CO, USA (2022).
6. Ilhan N, Ilhan O, Ayhan Tuzcu E, Daglioglu MC, Coskun M, Parlakfikirer N, et al. Is there a relationship between pathologic myopia and dry eye syndrome? Cornea. (2014) 33:169–71. doi: 10.1097/ICO.0000000000000033
7. Fahmy RM, Aldarwesh A. Correlation between dry eye and refractive error in Saudi young adults using noninvasive Keratograph 4. Indian J Ophthalmol. (2018) 66:653–6. doi: 10.4103/ijo.IJO_1103_17
8. Lee SS, Alonso-Caneiro D, Lingham G, Chen FK, Sanfilippo PG, Yazar S, et al. Choroidal thickening during young adulthood and baseline choroidal thickness predicts refractive error change. Invest Ophthalmol Vis Sci. (2022) 63:34. doi: 10.1167/iovs.63.5.34
9. Rana HS, Akella SS, Clabeaux CE, Skurski ZP, Aakalu VK. Ocular surface disease in thyroid eye disease: a narrative review. Ocul Surf. (2022) 24:67–73. doi: 10.1016/j.jtos.2022.02.001
10. Abusharaha A, Alturki AA, Alanazi SA, Fagehi R, Al-Johani N, El-Hiti GA, et al. Assessment of tear-evaporation rate in thyroid-gland patients. Clin Ophthalmol. (2019) 13:131–5. doi: 10.2147/OPTH.S188614
11. Torii H, Ohnuma K, Kurihara T, Tsubota K, Negishi K. Violet light transmission is related to myopia progression in adult high myopia. Sci Rep. (2017) 7:14523. doi: 10.1038/s41598-017-09388-7
12. Saka N, Moriyama M, Shimada N, Nagaoka N, Fukuda K, Hayashi K, et al. Changes of axial length measured by IOL master during 2 years in eyes of adults with pathologic myopia. Graefes Arch Clin Exp Ophthalmol. (2013) 251:495–9. doi: 10.1007/s00417-012-2066-9
13. Torii H, Kurihara T, Seko Y, Negishi K, Ohnuma K, Inaba T, et al. Violet light exposure can be a preventive strategy against myopia progression. EBioMedicine. (2017) 15:210–9. doi: 10.1016/j.ebiom.2016.12.007
15. Gordon RA, Donzis PB. Refractive development of the human eye. Arch Ophthalmol. (1985) 103:785–9. doi: 10.1001/archopht.1985.01050060045020
16. Németh J, Daiki T, Dankovics G, Barna I, Limburg H, Nagy ZZ. Prevalence of refractive errors in Hungary reveals three-fold increase in myopia. Int J Ophthalmol. (2022) 15:1174–9. doi: 10.18240/ijo.2022.07.19
17. Tsubota K, Pflugfelder SC, Liu Z, Baudouin C, Kim HM, Messmer EM, et al. Defining dry eye from a clinical perspective. Int J Mol Sci. (2020) 21:9271. doi: 10.3390/ijms21239271
18. Negishi K, Ayaki M, Uchino M, Takei K, Tsubota K. Strip meniscometry correlates with ocular surface tests and symptoms. Transl Vis Sci Technol. (2020) 9:31. doi: 10.1167/tvst.9.12.31
19. Miyasaka K, Ayaki M, Negishi K. Tear strip meniscometry and its clinical application: analysis of more than 2000 cases. Transl Vis Sci Technol. (2022) 11:3. doi: 10.1167/tvst.11.5.3
20. Chiang TT, Keenan TD, Agrón E, Liao J, Klein B, Chew EY, et al. Macular thickness in intermediate age-related macular degeneration is influenced by disease severity and subretinal drusenoid deposit presence. Invest Ophthalmol Vis Sci. (2020) 61:59. doi: 10.1167/iovs.61.6.59
21. Lafosse E, Wolffsohn JS, Talens-Estarelles C, García-Lázaro S. Presbyopia and the aging eye: existing refractive approaches and their potential impact on dry eye signs and symptoms. Cont Lens Anterior Eye. (2020) 43:103–14. doi: 10.1016/j.clae.2019.08.005
22. Richdale K, Sinnott LT, Skadahl E, Nichols JJ. Frequency of and factors associated with contact lens dissatisfaction and discontinuation. Cornea. (2007) 26:168–74. doi: 10.1097/01.ico.0000248382.32143.86
23. Chidi-Egboka NC, Briggs NE, Jalbert I, Golebiowski B. The ocular surface in children: a review of current knowledge and meta-analysis of tear film stability and tear secretion in children. Ocul Surf. (2019) 17:28–39. doi: 10.1016/j.jtos.2018.09.006
24. Su TY, Ho WT, Lu CY, Chang SW, Chiang HK. Correlations among ocular surface temperature difference value, the tear meniscus height, Schirmer's test and fluorescein tear film break up time. Br J Ophthalmol. (2015) 99:482–7. doi: 10.1136/bjophthalmol-2014-305183
25. Ayaki M, Kuze M, Kondo M, Tsubota K, Negishi K. Association between retinal nerve fiber layer thickness and eye fatigue. Biomed Res Int. (2019) 2019:3014567. doi: 10.1155/2019/3014567
26. Sano K, Kawashima M, Ikeura K, Arita R, Tsubota K. Abdominal breathing increases tear secretion in healthy women. Ocul Surf. (2015) 13:82–7. doi: 10.1016/j.jtos.2014.08.002
27. Ding C, Walcott B, Keyser KT. Sympathetic neural control of the mouse lacrimal gland. Invest Ophthalmol Vis Sci. (2003) 44:1513–20. doi: 10.1167/iovs.02-0406
28. Jin K, Imada T, Hisamura R, Ito M, Toriumi H, Tanaka KF, et al. Identification of lacrimal gland postganglionic innervation and its regulation of tear secretion. Am J Pathol. (2020) 190:1068–79. doi: 10.1016/j.ajpath.2020.01.007
29. Hieda O, Hiraoka T, Fujikado T, Ishiko S, Hasebe S, Torii H, et al. Study group. efficacy and safety of 0.01% atropine for prevention of childhood myopia in a 2-year randomized placebo-controlled study. Jpn J Ophthalmol. (2021) 65:315–25. doi: 10.1007/s10384-021-00822-y
30. Nickla DL, Wallman J. The multifunctional choroid. Prog Retin Eye Res. (2010) 29:144–68. doi: 10.1016/j.preteyeres.2009.12.002
31. Flores-Moreno I, Lugo F, Duker JS, Ruiz-Moreno JM. The relationship between axial length and choroidal thickness in eyes with high myopia. Am J Ophthalmol. (2013) 155:314–9.e1. doi: 10.1016/j.ajo.2012.07.015
32. Fuse N, Sakurai M, Motoike IN, Kojima K, Takai-Igarashi T, Nakaya N, et al. Genome-wide association study of axial length in population-based cohorts in japan. Ophthalmol Sci. (2022) 2:100113 doi: 10.1016/j.xops.2022.100113
33. Fledelius HC, Goldschmidt E. Oculometry findings in high myopia at adult age: considerations based on oculometric follow-up data over 28 years in a cohort-based Danish high myopia series. Acta Ophthalmol. (2010) 88:472–8. doi: 10.1111/j.1755-3768.2008.01472.x
34. Fotedar R, Wang JJ, Burlutsky G, Morgan IG, Rose K, Wong TY, et al. Distribution of axial length and ocular biometry measured using partial coherence laser interferometry (IOL Master) in an older white population. Ophthalmology. (2010) 117:417–23.23. doi: 10.1016/j.ophtha.2009.07.028
35. Aketa N, Uchino M, Kawashima M, Uchino Y, Yuki K, Ozawa Y, et al. Myopia, corneal endothelial cell density and morphology in a Japanese population-based cross-sectional study: the JPHC-NEXT Eye Study. Sci Rep. (2021) 11:6366. doi: 10.1038/s41598-021-85617-4
36. Sopapornamorn N, Lekskul M, Panichkul S. Corneal endothelial cell density and morphology in Phramongkutklao Hospital. Clin Ophthalmol. (2008) 2:147–51. doi: 10.2147/OPTH.S2242
37. Kheirkhah A, Saboo US, Abud TB, Dohlman TH, Arnoldner MA, Hamrah P, et al. Reduced corneal endothelial cell density in patients with dry eye disease. Am J Ophthalmol. (2015) 159:1022–6.e2. doi: 10.1016/j.ajo.2015.03.011
38. Kheirkhah A, Satitpitakul V, Hamrah P, Dana R. Patients with dry eye disease and low subbasal nerve density are at high risk for accelerated corneal endothelial cell loss. Cornea. (2017) 36:196–201. doi: 10.1097/ICO.0000000000001057
39. Hanyuda A, Torii H, Hayashi K, Uchida A, Mori K, Yotsukura E, et al. Relationship of choroidal thickness and axial length with posterior vitreous detachment in patients with high myopia. Sci Rep. (2022) 12:4093. doi: 10.1038/s41598-022-08101-7
40. Cheng D, Ruan K, Wu M, Qiao Y, Gao W, Lian H, et al. Characteristics of the optic nerve head in myopic eyes using swept-source optical coherence tomography. Invest Ophthalmol Vis Sci. (2022) 63:20. doi: 10.1167/iovs.63.6.20
41. Salehi MA, Nowroozi A, Gouravani M, Mohammadi S, Arevalo JF. Associations of refractive errors and retinal changes measured by optical coherence tomography: a systematic review and meta-analysis. Surv Ophthalmol. (2022) 67:591–607. doi: 10.1016/j.survophthal.2021.07.007
Keywords: axial length, dry eye, myopia, tears, ganglion cell complex, corneal endothelium, sex differences
Citation: Ayaki M, Torii H, Yotsukura E and Negishi K (2023) Sex differences in the relationship between axial length and dry eye in elderly patients. Front. Med. 10:1170696. doi: 10.3389/fmed.2023.1170696
Received: 21 February 2023; Accepted: 28 April 2023;
Published: 02 June 2023.
Edited by:
Shida Chen, Sun Yat-sen University, ChinaReviewed by:
Ju Zhang, Shandong Eye Institute & Hospital, ChinaYan Zhang, Tianjin Medical University Eye Hospital, China
Copyright © 2023 Ayaki, Torii, Yotsukura and Negishi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Masahiko Ayaki, bWF5YWtpQG9saXZlLm9jbi5uZS5qcA==
 Masahiko Ayaki
Masahiko Ayaki Hidemasa Torii1
Hidemasa Torii1 Kazuno Negishi
Kazuno Negishi