- 1School of Information and Management, Guangxi Medical University, Nanning, China
- 2Department of Gynaecology, Longhua District People's Hospital, Shenzhen, China
- 3Medical Records Library, Longhua District People's Hospital, Shenzhen, China
- 4School of Life Sciences, Central South University, Changsha, China
Objective: Hepatitis B virus (HBV) infection is a major health threat worldwide, especially in developing countries. We aimed to investigate the impact of hepatitis B carrier on pregnancy complications in pregnant women, in China.
Methods: This retrospective cohort study was conducted by using data from the EHR system of Longhua District People’s Hospital in Shenzhen, China, from January 2018 to June 2022. Binary logistic regression was used to evaluate the relationship between HBsAg carrier status and pregnancy complications and pregnancy outcomes.
Results: The study included 2095 HBsAg carriers (exposed group) and 23,019 normal pregnant women (unexposed group). Pregnant women in the exposed group were older than the pregnant women in the unexposed group (29 (27,32) vs. 29 (26,32), p < 0.001). In addition, the incidence of some adverse pregnancy complications in the exposure group was lower than that in the unexposed group, including hypothyroidism of pregnancy (adjusted odds ratio [aOR], 0.779; 95% confidence interval [CI], 0.617–0.984; p = 0.036), hyperthyroidism of pregnancy (aOR, 0.388; 95% CI, 0.159–0.984; p = 0.038), pregnancy induced hypertension (aOR, 0.699; 95% CI, 0.551–0.887; p = 0.003), antepartum hemorrhage (aOR, 0.294; 95% CI, 0.093–0.929; p = 0.037). However, compared with the unexposed group, the exposed group had a higher risk of lower birth weight (aOR, 1.12; 95% CI, 1.02–1.23; p = 0.018) and intrahepatic cholestasis of pregnancy (aOR, 2.888, 95% CI, 2.207–3.780; p < 0.001).
Conclusion: The prevalence rate of HBsAg carriers in pregnant women in Longhua District of Shenzhen was 8.34%. Compared with normal pregnant women, HBsAg carriers have a higher risk of ICP, a lower risk of gestational hypothyroidism and PIH, and a lower birth weight of their infants.
Introduction
Hepatitis B virus (HBV) infection is a major health threat worldwide. In 2019, about 296 million people worldwide were infected with HBV, and 1.5 million new infections occur each year. The geographic distribution of HBV infection is highly heterogeneous, with HBV prevalence levels above 7% (African Region) and less than 2% (Region of the Americas) (1). The largest burden of HBV infection is in China (2), where nearly 23,355,000 cases of HBV infection occurred in 2019 (about 29.0% of global HBV infections) (3), and the maternal infection rate was as high as 5.58% (4). In areas with high prevalence of HBV infection, although successfully introduced large-scale hepatitis b vaccination, vertical transmission is the main mode of infection, due to the high maternal viral load or HBV/DNA levels, maternal micro blood transfusion or mother blood leakage etc., (5), each year about 4 million to 5 million children around the world by their mothers infected with HBV (6). If maternal HBV infection affects pregnancy, it may also affect the survival of offspring. Therefore, the key question is, does maternal HBV infection affect pregnancy?
In this field, there are few reports on the association between HBsAg carriers and pregnancy complications and the relationship between them is unclear. Chen et al. reported that HBsAg-positive pregnant women have an increasing risk of intrahepatic cholestasis of pregnancy (ICP), low birth weight, fallopian cysts, cesarean scar pregnancy, thrombocytopenia, and fetal distress (7). Wan et al. found that maternal HBsAg carrying was associated with increasing risk of pregnancy-induced hypertension, fetal distress, cesarean delivery and macrosomia (8). However, Sun et al. found that the incidence of labor induction and small-for-gestational age (SGA) infants in HBV carriers was lower than that in the normal group, and there were no significant differences in pregnancy complications, delivery or perinatal outcomes (9). Huang et al. found that maternal chronic HBV infection will occur without increasing the risk of pregnancy-induced hypertension (10).
Obviously, the current research on the relationship between hepatitis B carriers and pregnancy complications and outcomes is insufficient. Therefore, this study aims to explore the influence of HBsAg carrier status during pregnancy on pregnancy complications and outcomes in the population of Longhua District, Shenzhen, China (Its population is 2.535 million, more than most cities in China). This is a retrospective cohort study to analyze the relationship between pregnancy complications and outcomes in 23,019 normal pregnant women and 2095 pregnant women were the HBsAg carrier.
Materials and methods
Subject
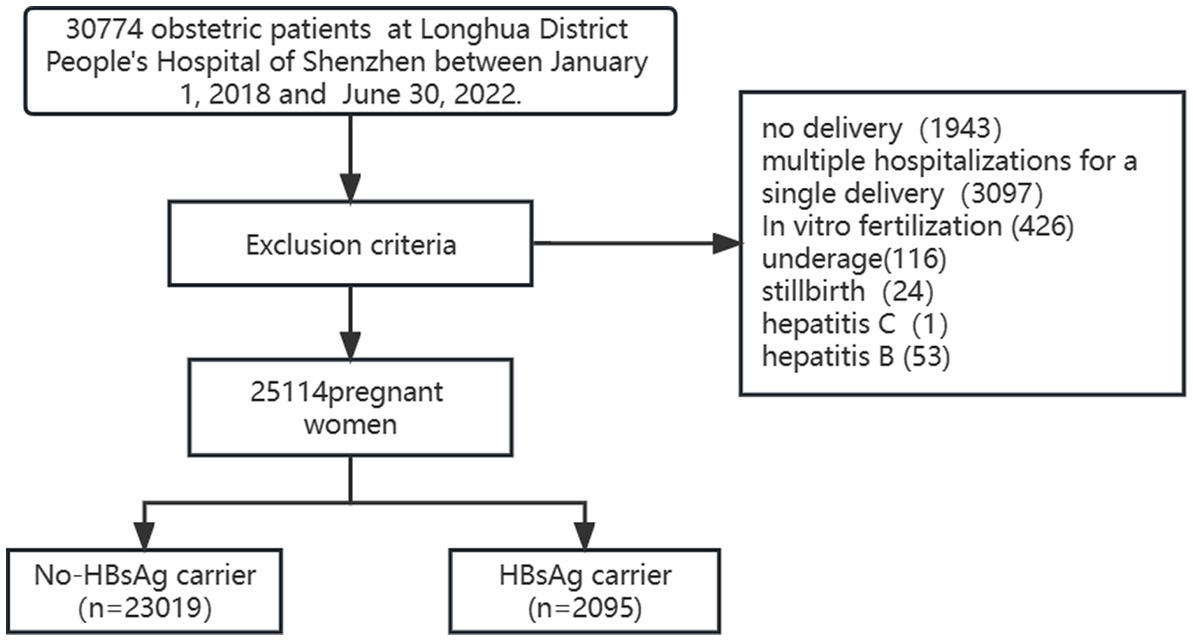
This was a retrospective study based on data from the Electronic Medical Record (EMR) information system for the period January 2018 to June 2022 in Longhua District People’s Hospital of Shenzhen, a tertiary referral hospital located in China Special Economic Zone. Only anonymized data from the EMR information system were used in this study. No patients were included as study participants. After filtering by exclusion criteria, 23,019 normal pregnant women (unexposed group) and 2095 HBsAg carrier pregnant women (exposed group) were included in this study (Figure 1). HBsAg carriers were identified by obstetricians based on the criteria of serological.
Inclusion and exclusion criteria
All pregnant women in Shenzhen were tested for the hepatitis B triad at the first prenatal visit (11–13 weeks of gestation), and HBV-DNA was tested for HBHBS-positive patients. Patients were excluded as follows: (1) patient was a single pregnancy but hospitalized multiple times (2) patient was hospitalized for purposes other than delivery (3) stillbirth (4) underage (5) in vitro fertilization (Ivf) (6) chronic viral hepatitis B infection (7) chronic viral hepatitis C infection (8) incomplete data. This study was authorized by our hospital ethics committee. (Longhua District People’s Hospital Ethical Review (Research) [2023] No. (001)).
Outcome measurements
Complications of pregnancy include pregnancy induced hypertension (PIH), gestational diabetes mellitus (GDM), intrahepatic cholestasis of pregnancy (ICP), anemia of pregnancy, hypothyroidism of pregnancy, hyperthyroidism of pregnancy, and digestive diseases of pregnancy. Pregnancy outcomes include premature rupture of fetal membranes, meconium-staining amniotic fluid, premature delivery, Neonatal weight, postpartum hemorrhage, and cesarean section.
Statistical analysis
The statistical package SPSS Statistics 24.0 (IBM-SPSS, Chicago, United States) was used for data analysis. Quantitative data was expressed as mean ± standard deviation (SD) or quartile and qualitative data as percentage (%). For univariate analysis, the t-test was used when the quantitative data obeyed normal distribution, and the Mann–Whitney u test was used when the data did not obey normal distribution; Pearson X2 test or Fisher test were used for qualitative data. Binary Logistic regression analysis was used to detect the relationship between HBsAg carrier and pregnancy outcomes and complications. p < 0.05 was considered statistically significant. Results were expressed in terms of odds ratios (OR) and adjusted odds ratios (aOR), with their respective 95% confidence intervals (95%CI). Variables in step 1 were neonatal weight, hypothyroidism of pregnancy, hyperthyroidism of pregnancy, PIH, ICP, antepartum hemorrhage, ethnicity, maternal age. In step 2, adjusted for maternal age and ethnicity, variables.
Results
Basic demographic data
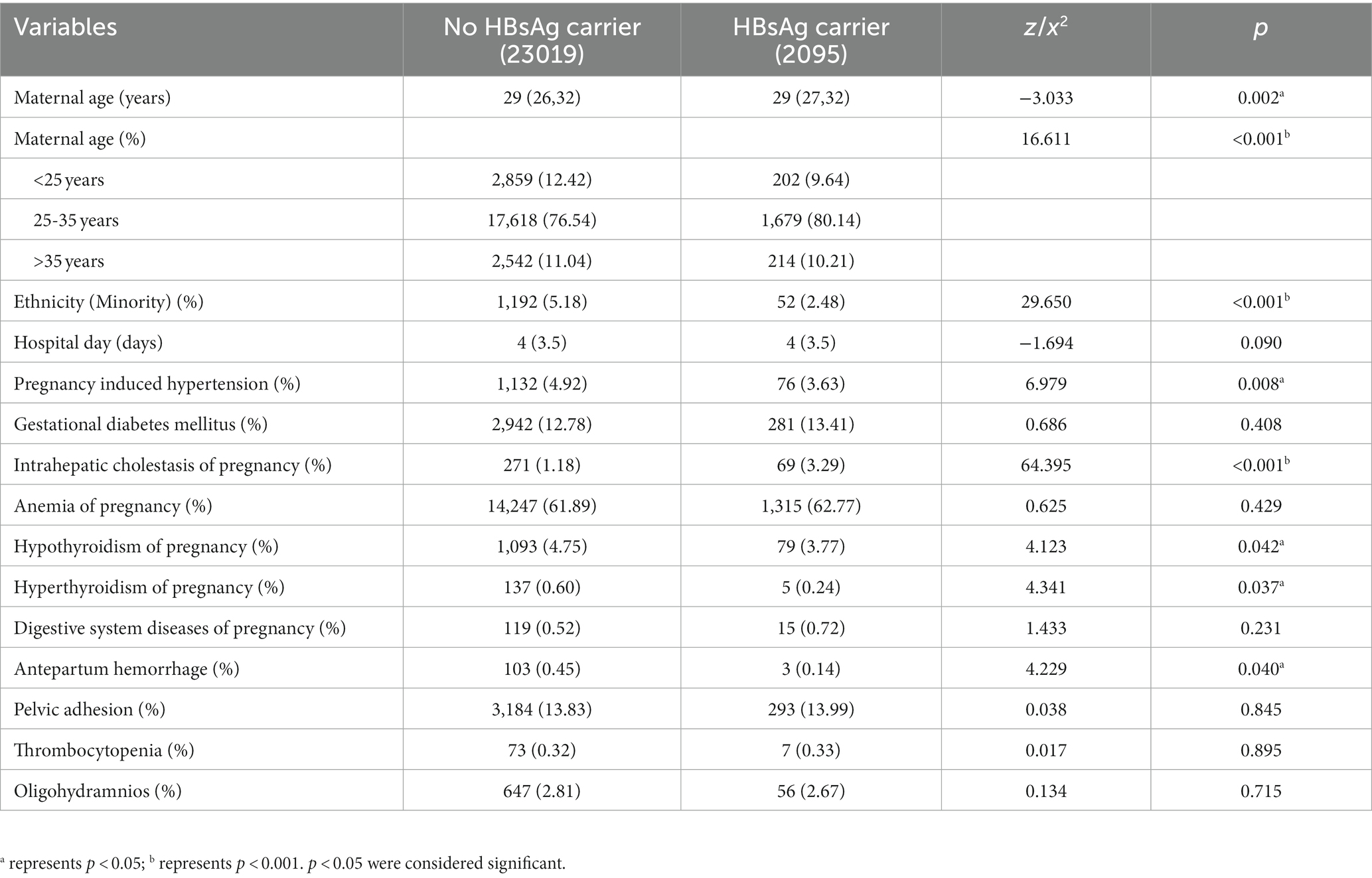
Among the 25,114 pregnant women in the database, 2095 (8.34%) HBsAg carriers were identified. Less than the Guangdong HBV prevalence (9.84%) in the study of Jue Liu et al (4). The average age of the HBsAg carrier group was 29 (27, 32) years, which was higher than that of the unexposed group 29 (26, 32) years (Z = −3.033, p = 0.002). The ethnic minority proportion in the HBsAg carrier group was 2.48% (52), significantly less than 5.18% (1192) in the unexposed group (X2 = 29.650, p < 0.001). The mean length of hospital stay between the HBsAg carrier group and the unexposed groups was not statistically significant (Z = −1.694, p = 0.090). As shown in Table 1.
Univariate analysis of influencing factors
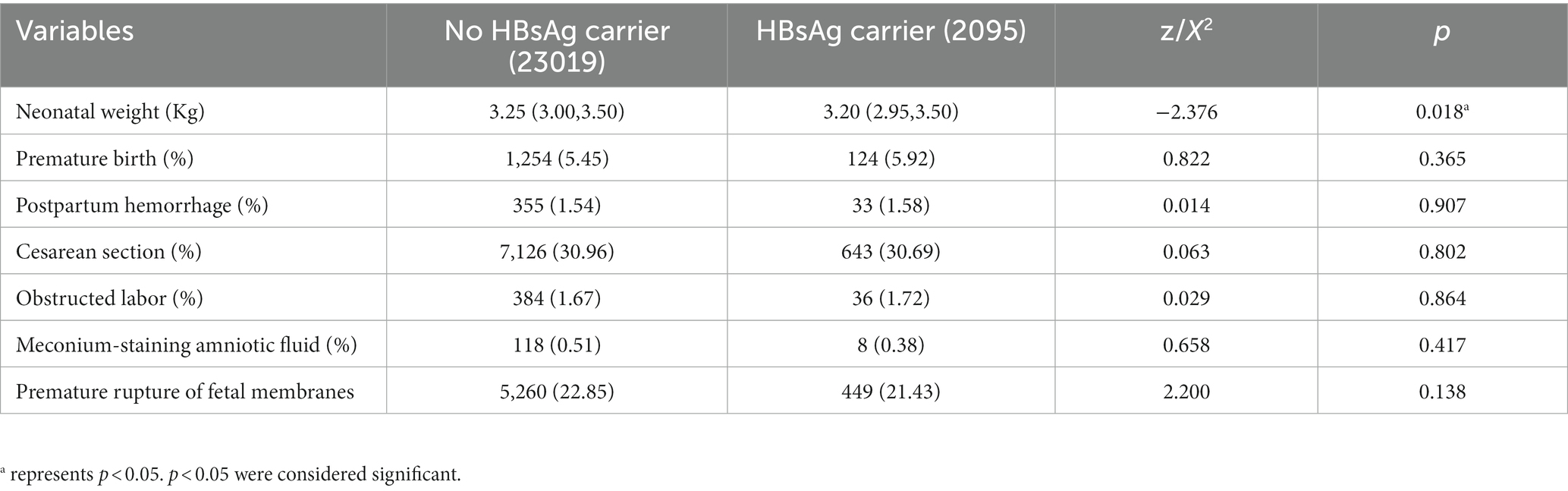
Among the pregnancy complications, PIH, hypothyroidism of pregnancy, hyperthyroidism of pregnancy, antepartum hemorrhage and ICP showed statistically significant differences between HBsAg carrier group and non-exposed group (all p < 0.05). In pregnancy outcomes, only the difference in neonatal birth weight was statistically significant between the two groups (p = 0.018). The incidence of gestational diabetes mellitus, anemia of pregnancy, pelvic adhesion, thrombocytopenia, oligohydramnios, premature birth, postpartum hemorrhage, cesarean section, obstructed labor, meconium-staining amniotic fluid and premature rupture of fetal membranes did not differ significantly between the HBsAg carrier group and non-exposed groups (all p > 0.05). As shown in Tables 1, 2.
Analysis of influencing factors
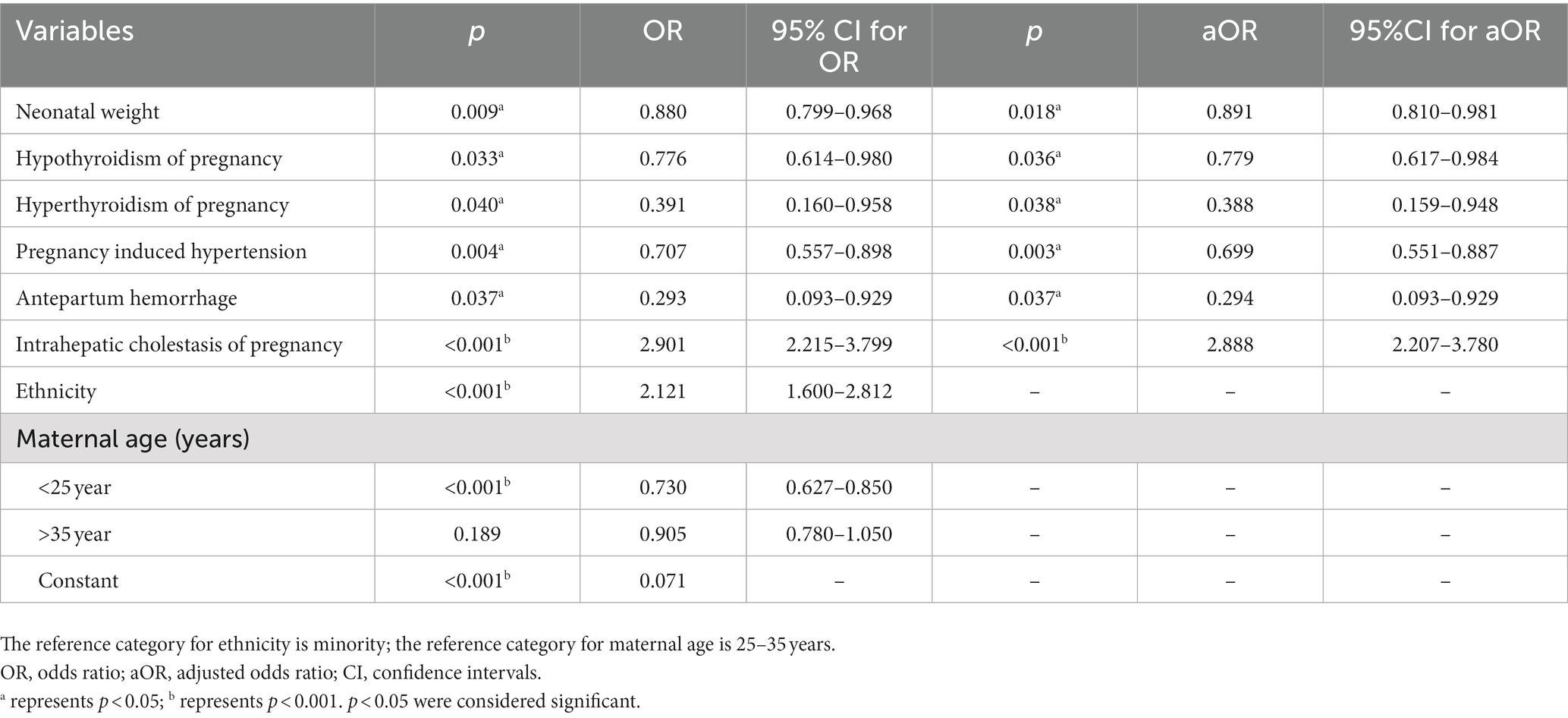
The results of the multivariate analysis were slightly altered when adjusted for maternal age and ethnicity. Compared with the unexposed group, the exposed group had a higher risk of lower birth weight (aOR, 1.12; 95% CI, 1.02–1.23; p = 0.018) and intrahepatic cholestasis of pregnancy (aOR, 2.888, 95% CI, 2.207–3.780; p < 0.001) The HBsAg carrier group had lower rates of some adverse pregnancy complications, including hypothyroidism of pregnancy (aOR, 0.779; 95% CI, 0.617–0.984; p = 0.036), hyperthyroidism of pregnancy (aOR, 0.388; 95% CI, 0.159–0.984; p = 0.038), PIH (aOR, 0.699; 95% CI,0.551–0.887; p = 0.003), antepartum hemorrhage (aOR, 0.294; 95% CI, 0.093–0.929; p = 0.037). As shown in Table 3.
Discussion
The percentage of HBsAg carriers among pregnant women in this study was 8.34%, higher than the average infection rate in China (5.44%), but slightly lower than the average infection rate of Guangdong Province (9.84%) (4). One of the reasons may be that this study did not include women who had early abortion, infertility, and did not receive services from our hospital, so the data collection was not comprehensive enough. Another reason may be that Shenzhen is one of the largest cities in China and attracts many people from various provinces, so it leads to a slightly lower infection rate than the overall rate in Guangdong Province. Basically, consistent with previous reports in the relevant literature (11, 12), the maternal age of HBsAg carriers was slightly higher than that in the non-exposed group. The prevalence of infection in the <25 years age group was about 6.6%, slightly lower than in the 25–35 years and > 35 years age groups, which should be related to the introduction of hepatitis B vaccination in China since 1992 (13).
We found that pregnant women with HBsAg carriers had a higher risk of ICP compared with the non-exposed group (aOR = 2.888). This is consistent with past studies that HBsAg carrier is a high risk factor for the development of ICP, but the results of this study showed that the risk of ICP in pregnant women with HBsAg carriage was 2.888 times higher than that of normal mothers, which is higher than previous studies (14–16). Jiang et al. Meta-analyses showed that not only were pregnant women infected with HBV at increased risk of developing ICP, but also patients with ICP were at increased risk of HBV infection (17). Therefore, in clinical practice, we should pay more attention to the serum total bile acid level and clinical manifestations of HBsAg carriers, and do a good job in the early prevention, diagnosis and treatment of ICP.
Pregnant women with HBsAg carriers have a lower risk of PIH (aOR = 0.699). Zhang et al. found that maternal HBsAg carrier group had a reduced risk of pre-eclampsia, premature rupture of membranes and PIH (OR = 0.83) (18). William et al. also found the risk of infecting PIH in HBsAg positive mothers (OR = 0.55) is lower than the in HBsAg negative mothers (19). However, in a case–control study, HBV-infected women reported a higher risk of PIH than the normal group (OR = 4.2) (20). The bias in these results may be due to differences in research methods and the cohort used in the study. Although the mechanism of the relationship between maternal HBsAg carrier and the incidence of PIH is unknown, PIH may be associated with an altered maternal immune response to fetal allograft, resulting in increased immune tolerance and decreased incidence of PIH.
Pregnant women with HBsAg carrier had a lower risk of developing hypothyroidism in pregnancy (aOR = 0.779). In contrast, no effect of hepatitis B virus status on thyroid status was found in the study by Testa and Percy et al. (21, 22). But instead of pregnant women, they studied people with autoimmune thyroid disease and the elderly, so the effect of hepatitis B virus on thyroid function may vary between study subjects. The liver is the target organ of thyroid hormone and it also plays an important role in hormone metabolism (23). In the study of Wu and Feng et al. showed that liver disorders were negatively correlated with TSH (24) and TT4 and FT4 were positively correlated (25). In turn, FSH, TT4, FT4 are important indicators for the diagnosis of hypothyroidism, so HBsAg carrier has a protective effect against hypothyroidism in pregnancy, which is worthy of clinical attention.
Birth weight of newborns in the HBsAg carrier group was lower than in the unexposed group (OR = 1.14). Unal et al. also found that HBV infection could lead to the decrease of newborn weight (26). Secondly, a retrospective cohort study in Thailand also found that HBsAg-positive women had a higher risk of having low birth weight babies (RR = 1.258) (27). Taken together, these studies suggest that HBsAg carriers are a high risk factor for neonatal weight, and clinical monitoring of neonatal weight in HBsAg carriers should be strengthened.
Some studies have reported that there is no association between GDM and HBV infection. For example, Cui et al. showed that there was no difference between the probability of HBV carriers suffering from GDM and the non-exposed group (28). The research results of Chen et al. also confirmed this point (7). However, some studies have shown an association between maternal HBV infection and GDM. For example, Giles et al.’s study showed that women with HBV infection had an increasing risk of developing GDM (OR = 1.2) (29). Consistenting with the former, we found that maternal HBsAg carriers were not associated with the risk of GDM infection.
Pregnant women with HBsAg carrier have a lower risk of antepartum hemorrhage and (aOR = 0.294) hyperthyroidism in pregnancy (aOR = 0.388). The liver is necessary for coagulation because it is the organ that produces prothrombin and other coagulation factors, and the liver is the target organ for thyroid hormones. HBsAg carrier was found to be a protective factor for prenatal hemorrhage and hyperthyroidism in pregnancy in this study, which is different from (30–32). However, since the sample size of both in this study was less than 1%, there are some limitations in the results and more studies are needed to prove it if it needs to be practiced in the clinic.
The study also found no association between preterm delivery, premature rupture of membranes, cesarean section, meconium-stained amniotic fluidis and HBV infection, consistent with studies (7, 9, 33, 34). Interestingly, it has been shown in some studies (35–37) that maternal HBsAg carriers may have an increased risk of preterm birth. And in an Israeli study it was noted that HBV/HCV infected pregnant women have higher rates of premature rupture of membranes, placental abruption, labor induction, cesarean section, rates of perinatal mortality, and congenital malformations (38). The reasons for the inconsistent results of the studies are unclear and may be due, on the one hand, to the fact that the studies were based on different sites and different populations and, secondly, may be related to the viral load of pregnant women with HBsAg carriers.
We studied the relationship between maternal HBsAg carriers and pregnancy complications among pregnant women in Longhua District, Shenzhen City. Although the sample size of our study is relatively large, there are still some limitations. First, although our sample size is large, this sample size only represents the Longhua District of Shenzhen. Even though the resident population of Longhua District in Shenzhen has exceeded 2.5 million, which is well above the level of a large city. Second, the study did not include potential confounding factors that could affect pregnancy outcome. For example, risk factors such as smoking and alcohol consumption should be taken into consideration. In addition, our data on viral load in HBV carriers is poorly documented, so whether viral load affects adverse pregnancy complications and outcomes is uncertain.
In conclusion, the prevalence rate of HBsAg carriers in pregnant women in Longhua District, Shenzhen City, China was 8.34%. Compared with normal pregnant women, HBsAg carriers have a higher risk of ICP, a lower risk of gestational hypothyroidism and PIH, and a lower birth weight of their infants. Maternal HBsAg carriers were not associated with the occurrence of these adverse pregnancy outcomes or complications, including GDM, anemia of pregnancy, pelvic adhesion, thrombocytopenia, oligohydramnios, premature birth, postpartum hemorrhage, cesarean section, obstructed labor, meconium-staining amniotic fluid and premature rupture of fetal membranes.
Data availability statement
The datasets presented in this article are not readily available because Data cannot be shared publicly because of restrictions apply to the availability of these data, which were used under license for the current study. Data are available from corresponding author for researchers who meet the criteria for access to confidential data. Requests to access the datasets should be directed to HH, 2422190004@qq.com.
Ethics statement
The studies involving human participants were reviewed and approved by Medical Ethics Committee of Shenzhen Longhua District People's Hospital. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements. No potentially identifiable images or data are included in this article.
Author contributions
MW: methodology, data analysis, and writing–original draft. JW: conceptualization, resources, and writing–review. JY: methodology and writing–review. WR and CW: data analysis and writing–review. WY: conceptualization and writing–review. HH: resources, writing–review, and supervision. All authors contributed to the article and approved the submitted version.
Funding
This research was funded by Department of Higher Education, Ministry of Education of China, 2021 Second Batch of Industry-University Cooperative Education Project (202102490073).
Acknowledgments
We would like to thank all the staff in the Department of Obstetrics and medical record at Longhua District People’s Hospital in Shenzhen for their efforts in diagnosing and recording HBV-positive and sero-negative mothers and babies.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
HBV, Hepatitis B virus; HBsAg, Hepatitis B surface antigen; GDM, Gestational diabetes mellitus; PIH, pregnancy induced hypertension; OR, odds ratio; aOR, adjusted odds ratio; CI, confidence intervals; ICP, intrahepatic cholestasis of pregnancy; Ivf, If the patient is in vitro fertilization; SD, Standard deviation.
References
1. Organization, W.H, Global progress report on HIV, viral hepatitis and sexually transmitted infections, (2021). Available at: https://www.who.int/publications/i/item/9789240027077 (Accessed July 15, 2021).
2. Liu, J, Liang, W, Jing, W, and Liu, M. Countdown to 2030: eliminating hepatitis B disease. China Bull World Health Organ. (2019) 97:230–8. doi: 10.2471/blt.18.219469
3. Yue, T, Zhang, Q, Cai, T, Xu, M, Zhu, H, Pourkarim, MR, et al. Trends in the disease burden of HBV and HCV infection in China from 1990-2019. Int J Infect Dis. (2022) 122:476–85. doi: 10.1016/j.ijid.2022.06.017
4. Liu, J, Wang, X, Wang, Q, Qiao, Y, Jin, X, Li, Z, et al. Hepatitis B virus infection among 90 million pregnant women in 2853 Chinese counties, 2015-2020: a national observational study. Lancet Reg Health West Pac. (2021) 16:100267. doi: 10.1016/j.lanwpc.2021.100267
5. Pawlowska, M, Pniewska, A, Pilarczyk, M, Kozielewicz, D, and Domagalski, K. Prophylaxis of vertical HBV infection. Expert Opin Drug Saf. (2016) 15:1361–8. doi: 10.1080/14740338.2016.1211106
6. Thio, CL, Guo, N, Xie, C, Nelson, KE, and Ehrhardt, S. Global elimination of mother-to-child transmission of hepatitis B: revisiting the current strategy. Lancet Infect Dis. (2015) 15:981–5. doi: 10.1016/s1473-3099(15)00158-9
7. Chen, YM, Ning, WW, Wang, X, Chen, YJ, Wu, B, and Tao, J. Maternal hepatitis B surface antigen carrier status and pregnancy outcome: a retrospective cohort study. Epidemiol Infect. (2022) 150:1–22. doi: 10.1017/s0950268822000681
8. Wan, ZH, Zhou, AF, Zhu, HP, Lin, XF, Hu, D, Peng, SX, et al. Maternal hepatitis B virus infection and pregnancy outcomes: a hospital-based case-control study in Wuhan. China J Clin Gastroenterol. (2018) 52:73–8. doi: 10.1097/mcg.0000000000000842
9. Sun, Q, Lao, TT, Du, MY, Xie, M, Sun, YH, Bai, B, et al. Chronic maternal hepatitis B virus infection and pregnancy outcome-a single center study in Kunming, China. BMC Infect Dis. (2021) 21:21. doi: 10.1186/s12879-021-05946-7
10. Huang, X, Tan, H, Li, X, Zhou, S, Wen, SW, and Luo, M. Maternal chronic HBV infection would not increase the risk of pregnancy-induced hypertension –results from pregnancy cohort in Liuyang rural China. PLoS One. (2014) 9:e114248. doi: 10.1371/journal.pone.0114248
11. Zhao, Y, Chen, Y-L, Song, H-Q, Huang, P-Y, Wang, L-Y, Liu, W, et al. Effects of maternal hepatitis B surface antigen positive status on the pregnancy outcomes: a retrospective study in Xiamen, China, 2011-2018. PLoS One. (2020) 15:e0229732. doi: 10.1371/journal.pone.0229732
12. Katamba, PS, Mukunya, D, Kwesiga, D, and Nankabirwa, V. Prenatal hepatitis B screening and associated factors in a high prevalence district of lira, northern Uganda: a community based cross sectional study. BMC Public Health. (2019) 19:1004. doi: 10.1186/s12889-019-7344-6
13. Luo, ZB, Li, LJ, and Ruan, B. Impact of the implementation of a vaccination strategy on hepatitis B virus infections in China over a 20-year period. Int J Infect Dis. (2012) 16:E82–8. doi: 10.1016/j.ijid.2011.10.009
14. Tan, J, Liu, X, Mao, X, Yu, J, Chen, M, Li, Y, et al. HBsAg positivity during pregnancy and adverse maternal outcomes: a retrospective cohort analysis. J Viral Hepat. (2016) 23:812–9. doi: 10.1111/jvh.12545
15. Cai, Q, Liu, H, Han, W, Liu, L, Xu, Y, He, Y, et al. Maternal HBsAg carriers and adverse pregnancy outcomes: a hospital-based prospective cohort analysis. J Viral Hepat. (2019) 26:1011–8. doi: 10.1111/jvh.13105
16. Arthuis, C, Diguisto, C, Lorphelin, H, Dochez, V, Simon, E, Perrotin, F, et al. Perinatal outcomes of intrahepatic cholestasis during pregnancy: an 8-year case-control study. PLoS One. (2020) 15:e0228213. doi: 10.1371/journal.pone.0228213
17. Jiang, R, Wang, T, Yao, Y, Zhou, F, and Huang, X. Hepatitis B infection and intrahepatic cholestasis of pregnancy: a systematic review and meta-analysis. Medicine. (2020) 99:e21416. doi: 10.1097/MD.0000000000021416
18. Zhang, YL, Chen, JC, Liao, TT, Chen, SW, Yan, JY, and Lin, XQ. Maternal HBsAg carriers and pregnancy outcomes: a retrospective cohort analysis of 85,190 pregnancies. BMC Pregnancy Childbirth. (2020) 20:724. doi: 10.1186/s12884-020-03257-4
19. To, W.W.KCheung, W, and Mok, K-M. Hepatitis B surface antigen carrier status and its correlation to gestational hypertension. Aust N Z J Obstet Gynaecol. (2003) 43:119–22. doi: 10.1046/j.0004-8666.2003.00029.x
20. Saleh-Gargari, S, Hantoushzadeh, S, Zendehdel, N, Jamal, A, and Aghdam, H. The Association of Maternal HBsAg carrier status and perinatal outcome. Hepat Mon. (2009) 9:180–4.
21. Testa, A, Castaldi, P, Fant, V, Fiore, GF, Grieco, V, De Rosa, A, et al. Prevalence of HCV antibodies in autoimmune thyroid disease. Eur Rev Med Pharmacol Sci. (2006) 10:183–6.
22. Percy, ME, Potyomkina, Z, Dalton, AJ, Fedor, B, Mehta, P, Andrews, DF, et al. Relation between apolipoprotein E genotype, hepatitis b virus status, and thyroid status in a sample of older persons with down syndrome. Am J Med Genet A. (2003) 120A:191–8. doi: 10.1002/ajmg.a.20099
23. Malik, R, and Hodgson, H. The relationship between the thyroid gland and the liver. QJM: Int J Med. (2002) 95:559–69. doi: 10.1093/qjmed/95.9.559
24. Wu, YC, You, SL, Zang, H, Liu, HT, Mao, YL, Mao, PY, et al. Usefulness of serum thyroid-stimulation hormone (TSH) as a prognostic indicator for acute-on-chronic liver failure. Ann Hepatol. (2015) 14:218–24. doi: 10.1016/s1665-2681(19)30784-7
25. Feng, H-L, Li, Q, Cao, W-K, and Yang, J-M. Changes in thyroid function in patients with liver failure and their clinical significance: a clinical study of non-thyroidal illness syndrome in patients with liver failure. Hepatobiliary Pancreat Dis Int. (2020) 19:561–6. doi: 10.1016/j.hbpd.2020.05.001
26. Unal, C, Tanacan, A, Ziyadova, G, Fadiloglu, E, and Beksac, MS. Effect of viral load on pregnancy outcomes in chronic hepatitis B infection. J Obstet Gynaecol Res. (2019) 45:1837–42. doi: 10.1111/jog.14065
27. Sirilert, S, Traisrisilp, K, Sirivatanapa, P, and Tongsong, T. Pregnancy outcomes among chronic carriers of hepatitis B virus. Int J Gynecol Obstet. (2014) 126:106–10. doi: 10.1016/j.ijgo.2014.02.019
28. Cui, AM, Cheng, XY, Shao, JG, Li, HB, Wang, XL, Shen, Y, et al. Maternal hepatitis B virus carrier status and pregnancy outcomes: a prospective cohort study. BMC Pregnancy Childbirth. (2016) 16:87. doi: 10.1186/s12884-016-0884-1
29. Giles, M, Davey, M-A, and Wallace, E. Chronic hepatitis B infection and the risk of gestational diabetes: a cross-sectional study. BJOG Int J Obstet Gynaecol. (2020) 127:1147–52. doi: 10.1111/1471-0528.16217
30. Reddick, KLB, Jhaveri, R, Gandhi, M, James, AH, and Swamy, GK. Pregnancy outcomes associated with viral hepatitis. J Viral Hepat. (2011) 18:e394–8. doi: 10.1111/j.1365-2893.2011.01436.x
31. Chen, B, Wang, Y, Lange, M, and Kushner, T. Hepatitis C is associated with more adverse pregnancy outcomes than hepatitis B: a 7-year national inpatient sample study. Hepatol Commun. (2022) 6:2465–73. doi: 10.1002/hep4.2002
32. Cui, W, Deng, B, Wang, W, and Liu, P. Graves’ hyperthyroidism accompanied with acute hepatitis B virus infection: an extrahepatic manifestation? Virol J. (2016) 13:80. doi: 10.1186/s12985-016-0537-z
33. Huang, Q-T, Wei, S-S, Zhong, M, Hang, L-L, Xu, Y-Y, Cai, G-X, et al. Chronic hepatitis B infection and risk of preterm labor: a meta-analysis of observational studies. J Clin Virol. (2014) 61:3–8. doi: 10.1016/j.jcv.2014.06.006
34. Wong, S, Chan, LY, Yu, V, and Ho, L. Hepatitis B carrier and perinatal outcome in singleton pregnancy. Am J Perinatol. (1999) 16:0485–8. doi: 10.1055/s-1999-6802
35. Ma, X, Sun, D, Li, C, Ying, J, and Yan, Y. Chronic hepatitis B virus infection and preterm labor(birth) in pregnant women—an updated systematic review and meta-analysis. J Med Virol. (2018) 90:93–100. doi: 10.1055/s-1999-6802
36. Peng, S, Chen, H, Li, X, Du, Y, and Gan, Y. Maternal age and educational level modify the association between chronic hepatitis B infection and preterm labor. BMC Pregnancy Childbirth. (2020) 20:38. doi: 10.1186/s12884-020-2729-1
37. Xu, C, Bao, Y, Zuo, J, Li, Y, Tang, Y, Qu, X, et al. Maternal chronic hepatitis B virus infection and the risk of preterm birth: a retrospective cohort analysis in Chinese women. J Viral Hepat. (2021) 28:1422–30. doi: 10.1111/jvh.13585
Keywords: HBsAg carrier, pregnancy complications, pregnancy induced hypertension, intrahepatic cholestasis of pregnancy, hypothyroidism of pregnancy
Citation: Weng M, Wang J, Yin J, Ren W, Wei C, Yang W and He H (2023) Effects of HBsAg carriers on pregnancy complications in pregnant women: a retrospective cohort study. Front. Med. 10:1166530. doi: 10.3389/fmed.2023.1166530
Edited by:
Soheil Tavakolpour, Dana–Farber Cancer Institute, United StatesReviewed by:
Alberto Puertas, Virgen de las Nieves University Hospital, SpainNaim Abu-Freha, Soroka Medical Center, Israel
Copyright © 2023 Weng, Wang, Yin, Ren, Wei, Yang and He. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Huimin He, MjQyMjE5MDAwNEBxcS5jb20=
†These authors have contributed equally to this work and share first authorship
 Mengqing Weng
Mengqing Weng Jie Wang2,3†
Jie Wang2,3†