- 1Department of Obstetrics and Gynecology, The Fourth Hospital of Hebei Medical University, Shijiazhuang, Hebei, China
- 2Department of Neurology, Children’s Hospital of Hebei Province, Shijiazhuang, Hebei, China
- 3Department of Gynecology, Obstetrics and Gynecology Hospital of Fudan University, Shanghai, China
This study aimed to assess the effect of excessive gestational weight gain (GWG) before and after 28 weeks on the mode of delivery in women who attempted a trial of labor after cesarean (TOLAC), stratified by pre-pregnancy BMI. A retrospective analysis of the outcomes of eligible women who attempted trial of labor after cesarean (TOLAC) in a Chinese hospital from January 2016 to October 2022 was performed. GWG before and after 28 weeks was categorized as ‘excessive’ or ‘non-excessive’ based on the guideline of Institute of Medicine (IOM). Multivariable logistic regression analyses were used to estimate the effect of excessive GWG before and after 28 weeks on mode of delivery in women who underwent TOLAC, stratified by pre-pregnancy BMI. Of the 512 women who underwent term trial of labor, 71.1% achieved a vaginal birth. No correlation was found between excessive GWG before 28 weeks and the rate of vaginal birth after cesarean (VBAC). Among women with or without excessive GWG before 28 weeks, excessive GWG after 28 weeks was significantly associated with a reduced rate of VBAC. When stratified by pre-pregnancy BMI, women who had excessive gestational weight gain after 28 weeks gestation had lower rates of VBAC than those who did not, regardless of being underweight, normal or overweight (aOR 0.23, 95% CI 0.06–0.88; aOR 0.42, 95% CI 0.25, 0.70; and aOR 0.12, 95% CI 0.04–0.36; respectively). Excessive weight gain after 28 weeks of pregnancy was related to decreased rates of VBAC, irrespective of pre-pregnancy weight status and weight gain before 28 weeks.
1. Introduction
Women who have had a prior cesarean section can choose either vaginal birth after cesarean section (VBAC) or repeat cesarean section (RCS) for their subsequent deliveries. However, globally, most women with a previous cesarean opt for a repeat cesarean. The rate of trial of labor after cesarean (TOLAC) differs across countries, with lower rates in China (10%) and the US (13%) and a higher rate in Germany (36.0–49.8%) (1–3). Although successful TOLAC is associated with lower overall morbidity rates than RCS (4), concerns about its safety and associated liability continues to limit its availability (5–8).
The factors that impact VBAC rates include onset of labor, previous vaginal birth or VBAC, multiple cesarean sections, body mass index (BMI), and interpregnancy interval (9–12). Gestational weight gain (GWG) is a potential risk factor for the global obesity crisis, and unlike most of the other factors, it can be modified during pregnancy (13, 14). Excessive GWG can lead to complications of a kind that cesarean section (CS), preeclampsia, gestational diabetes, large for gestational age babies (LGA), and macrosomia (15–17). Only a handful of studies have examined the link between GWG and VBAC, and these studies have yielded inconsistent results. Two studies from the USA and New Zealand indicated that excessive GWG could lower the chances of vaginal birth (18, 19), while another study from the USA detected no variation in TOLAC success rates with excessive GWG (20).
The Institute of Medicine (IOM) guideline proposed fitting GWG classified by pre-pregnancy BMI in 2009 (21). Maternal metabolic changes and GWG differ throughout pregnancy (22); therefore, some studies specifically examined the association between excessive GWG during the first or second trimester and pregnancy complications (16, 23, 24). However, the association between excessive GWG at different stages of pregnancy and VBAC remains unclear. This study aims to explore the relationship between weight gain before and after 28 weeks and VBAC stratified by pre-pregnancy BMI.
2. Participants and methods
2.1. Study setting
This was a retrospective study performed at the Fourth affiliated Hospital of Hebei Medical University, which is a comprehensive regional medical center located in northeast China that performs approximately 1,800 deliveries per year. Before week 8 of gestation, a specific electronic file was created for each pregnant woman at their first antenatal visit. They then received regular follow-up visits every 2–4 weeks until delivery. The study was approved by the Ethics Committee of the Fourth affiliated Hospital of Hebei medical university (2022KS010).
2.2. Eligibility criteria
The study population consisted of women who registered at their first prenatal visit before week 8 of gestation and attempted TOLAC and delivered between January 1, 2016 and October 31, 2022. We excluded women with malpresentation in the current pregnancy, previous uterine scar other than low transverse incision scar, multiple gestation, more than one prior cesarean delivery, placenta previa, delivery before week 37 (37 0/7 weeks), and incomplete information. We also omitted obese women (BMI > 30 kg/m2) from the study, as this group had an insufficient sample size for representation.
2.3. Data collection
For the analysis, the clinical characteristics of women attempting TOLAC were obtained from electronic files, including maternal age, maternal height, labor induction, gestational age at delivery, maternal hypertension or diabetes in pregnancy, previous vaginal birth or VBAC, pre-pregnancy weight, maternal weight at 28 weeks, maternal weight at delivery, and mode of delivery. Meanwhile, the weight of each participant was recorded at each visit; they wore light clothing without shoes during the measurement.
2.4. Determination of gestational weight gain
During the first antenatal care visit, each participant reported their pre-pregnancy weight. Maternal weight at 28 weeks was determined as the latest weight measured within 1 week around 28 weeks. Maternal weight at delivery was that measured within 2 days before the delivery date. By dividing the self-reported pre-pregnancy weight (25, 26) (in kilograms) of each participant by their height squared (in meters), the pre-pregnancy BMI was calculated (27). GWG was calculated as follows: GWG before 28 weeks = maternal weight at 28 weeks - pre-pregnancy weight; GWG after 28 weeks = maternal weight at delivery - maternal weight at 28 weeks.
We applied the recommendation of IOM for weight gain during pregnancy based on pre-pregnancy BMI (underweight: < 18.5 kg/m2, normal: 18.5–24.9 kg/m2, overweight: 25.0–29.9 kg/m2) (21) (Table 1) to calculate the suitable range of gestational weight gain before and after 28 weeks (Table 2). Using this standard, we categorized women as having ‘excessive GWG’ if they exceeded the recommended upper limit for their BMI group, and ‘non-excessive GWG’ if they gained weight within or below the recommended range.
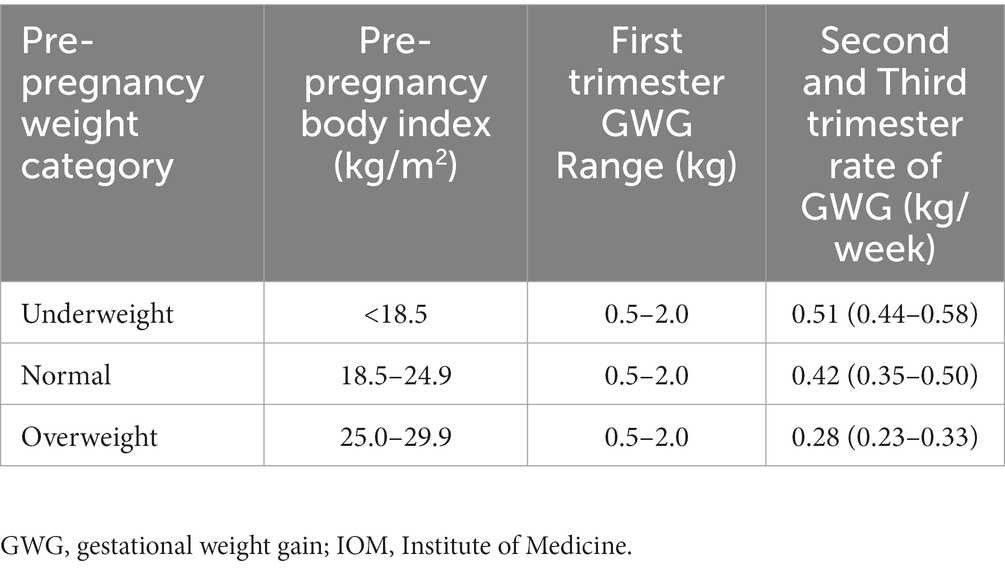
Table 1. Gestational weight gain recommended by the IOM guideline (21).
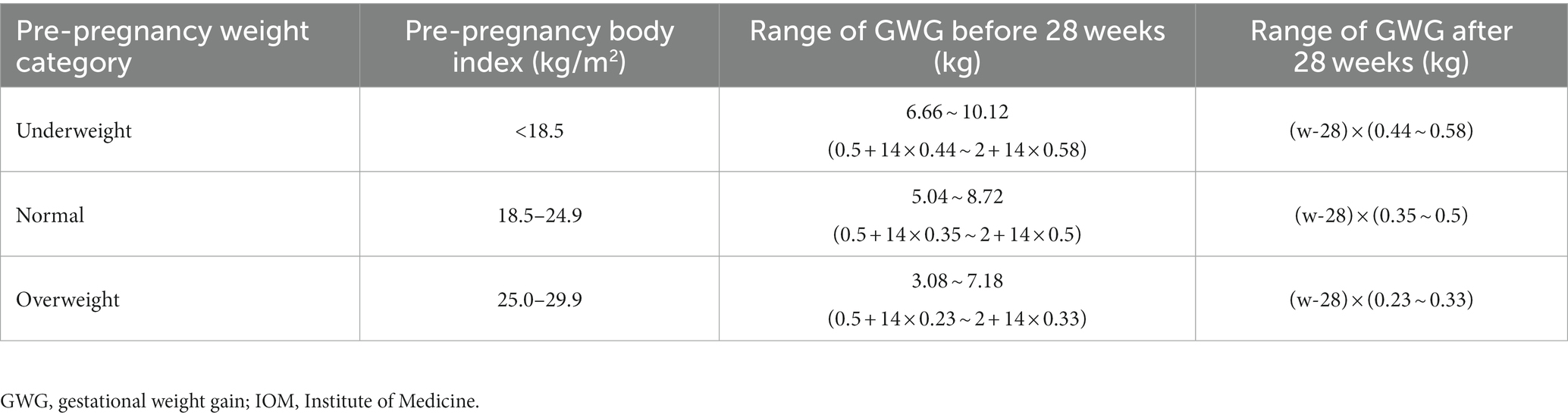
Table 2. Gestational weight gain of included pregnant women according to IOM standard (21).
2.5. Data analysis
We evaluated participant characteristics across GWG before and after 28 weeks by frequency (percentage), and used the Chi-squared or Fisher exact tests to compare the distribution of differences. We analyzed continuous variables using the Student’s t test. Predictors of VBAC success were evaluated using univariate logistic regression analyses. Then, we adjusted for potential confounders that were statistically significant in the univariate analysis (those with p < 0.05) and generated multivariable logistic regression models to investigate the association between gestational weight gain before and after 28 weeks and VBAC.
To understand how GWG before and after 28 weeks affects VBAC, a stratified analysis was performed to examine the relation between GWG after 28 weeks and the rate of VBAC in groups of GWG before 28 weeks (classified into excessive and non-excessive). The non-excessive GWG group was used as the reference group.
We also generated multivariable logistic regression models for the three subgroups (underweight, normal weight, and overweight) to further explore the relation between excessive gestational weight gain before and after 28 weeks and VBAC rate among women with different pre-pregnancy BMI categories, adjusting for the same confounders except pre-pregnancy BMI. The adjusted OR with 95% CI are shown in Figure 1. SPSS version 19.0 software was used for all statistical analyses, and GraphPad Prism version 6.0 was used to draw the figure. A two-tailed p < 0.05 indicated statistical significance for analyses.
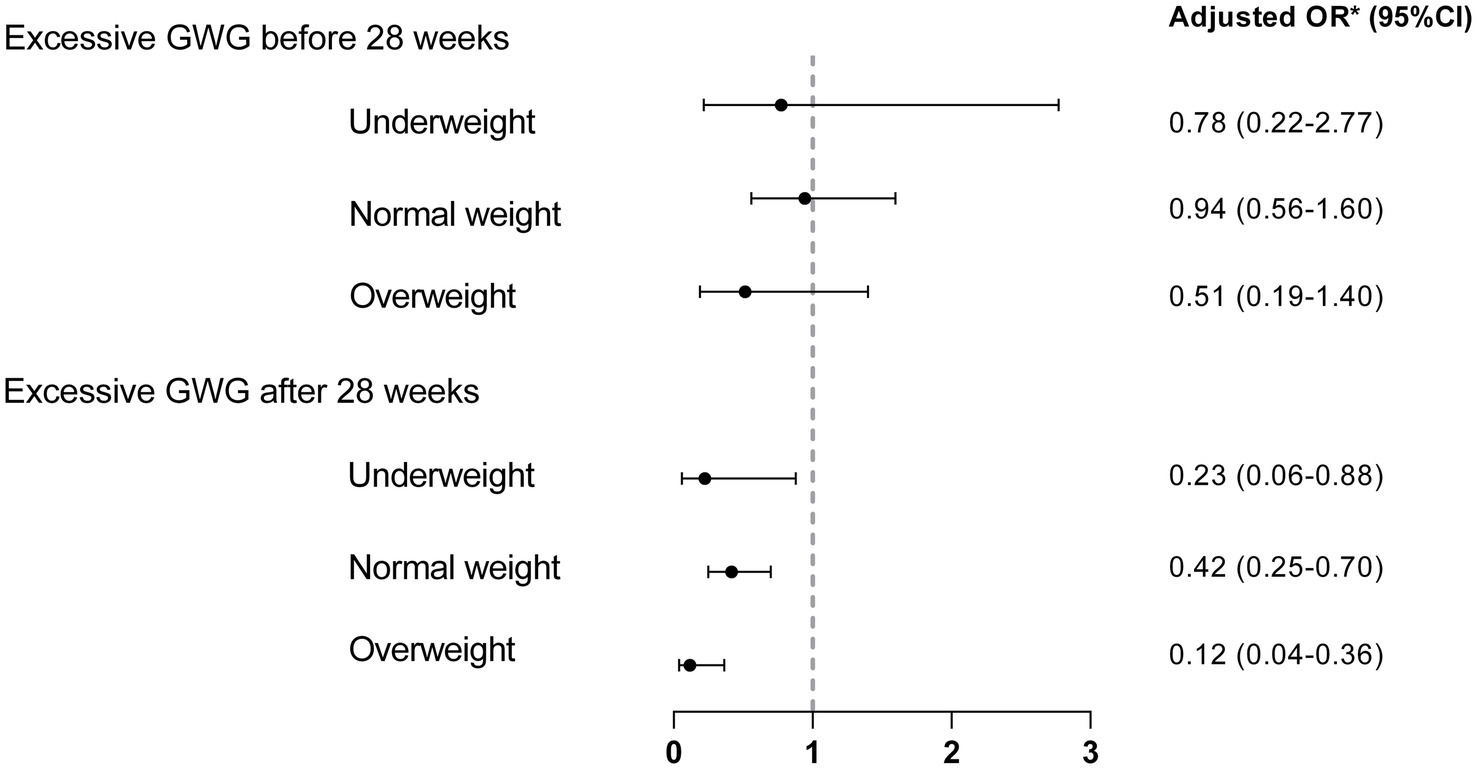
Figure 1. Association between excessive GWG before and after 28 weeks and VBAC stratified by pre-pregnancy BMI. Non-excessive GWG was used as the reference group. *Adjusted for induction of labor, hypertension in pregnancy, previous vaginal birth or VBAC.
3. Results
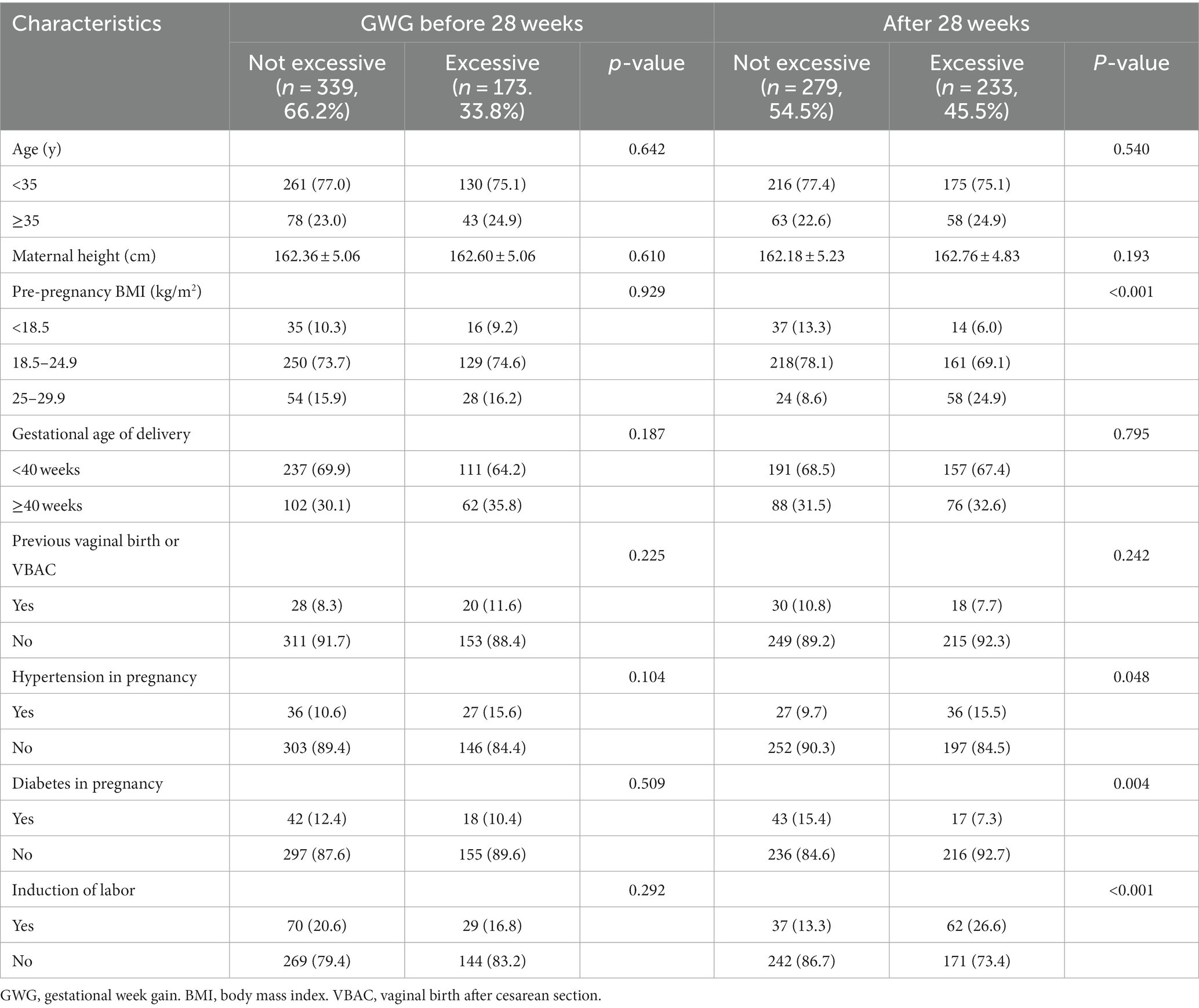
We examined 552 women who attempted TOLAC for eligibility during the study period. Thirty-one women who did not fulfil the eligibility criteria and 9 women were obese were excluded. In total, 512 (92.7%) women were included in the analysis. Nearly half of the 512 women who met the inclusion criteria exceeded the IOM recommendations for GWG after 28 weeks (45.5%), while 33.8% had excessive GWG before 28 weeks. The demographics of the participants are summarized in Table 3, stratified by GWG before and after 28 weeks. GWG before 28 weeks was not significantly influenced by hypertension or diabetes in pregnancy, maternal age, previous vaginal birth or VBAC, maternal height, gestational age at delivery, pre-pregnancy BMI, or induction of labor. However, GWG after 28 weeks was associated with pre-pregnancy BMI, hypertension in pregnancy, diabetes in pregnancy, and induction of labor. Pre-pregnancy overweight women had a higher likelihood of exceeding the IOM recommendations after 28 weeks (p < 0.001). Hypertension in pregnancy and induction of labor was more likely to occur in women with excessive GWG after 28 weeks (p = 0.048, p < 0.001, respectively), while women with diabetes in pregnancy tended not to exceed the IOM recommendations after 28 weeks (p = 0.004).
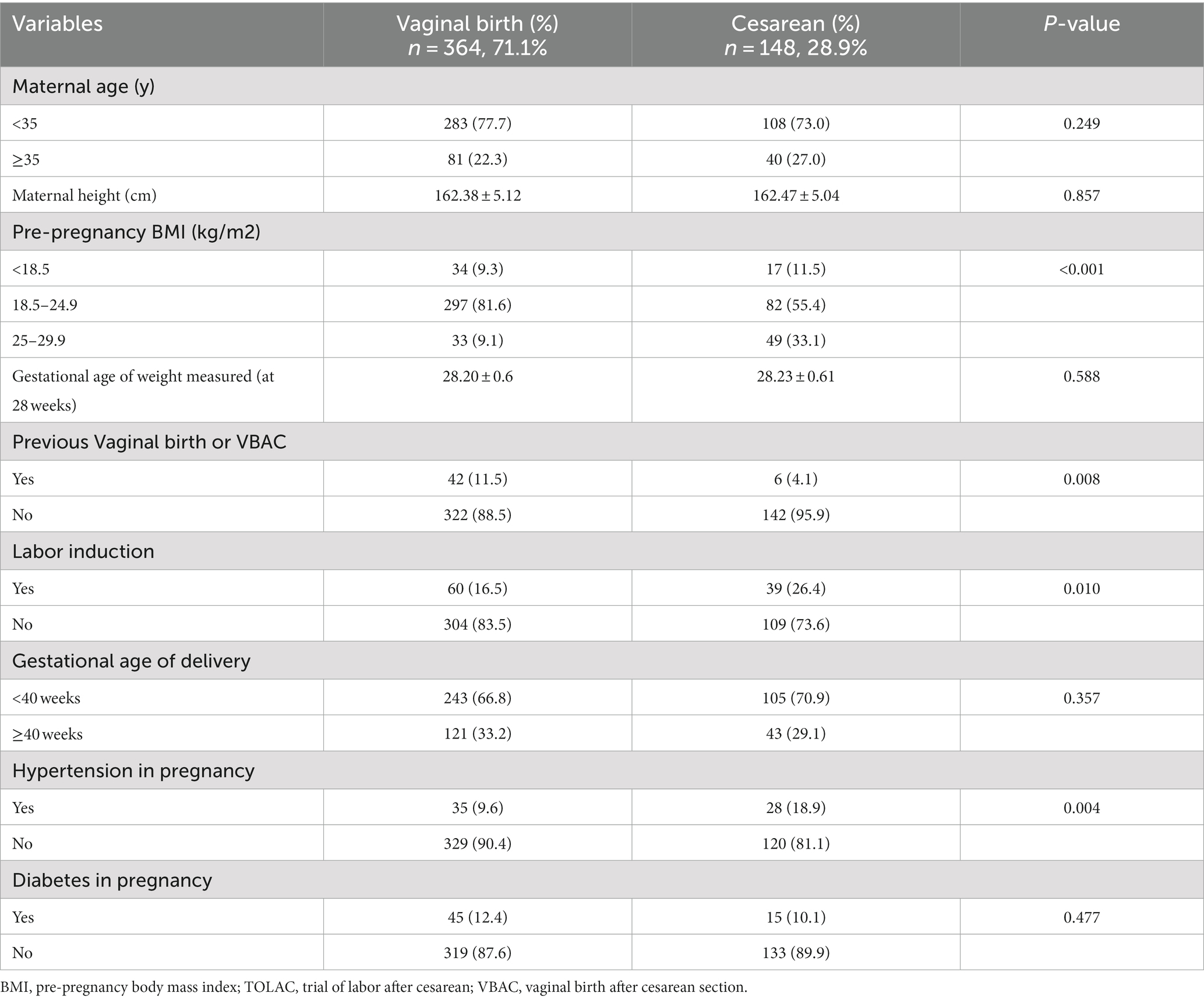
Among all women who attempted TOLAC, vaginal delivery occurred in 71.1%. The timing of weight measurement at 28 weeks did not significantly differ between the cesarean section and the vaginal delivery groups (p = 0.588). In the unadjusted model, women were more likely undergo a successful TOLAC if they were nonobese (p < 0.001), had a previous vaginal birth or VBAC (p = 0.008), had spontaneous labor (p = 0.010), and did not have hypertension in pregnancy (p = 0.004) (Table 4).
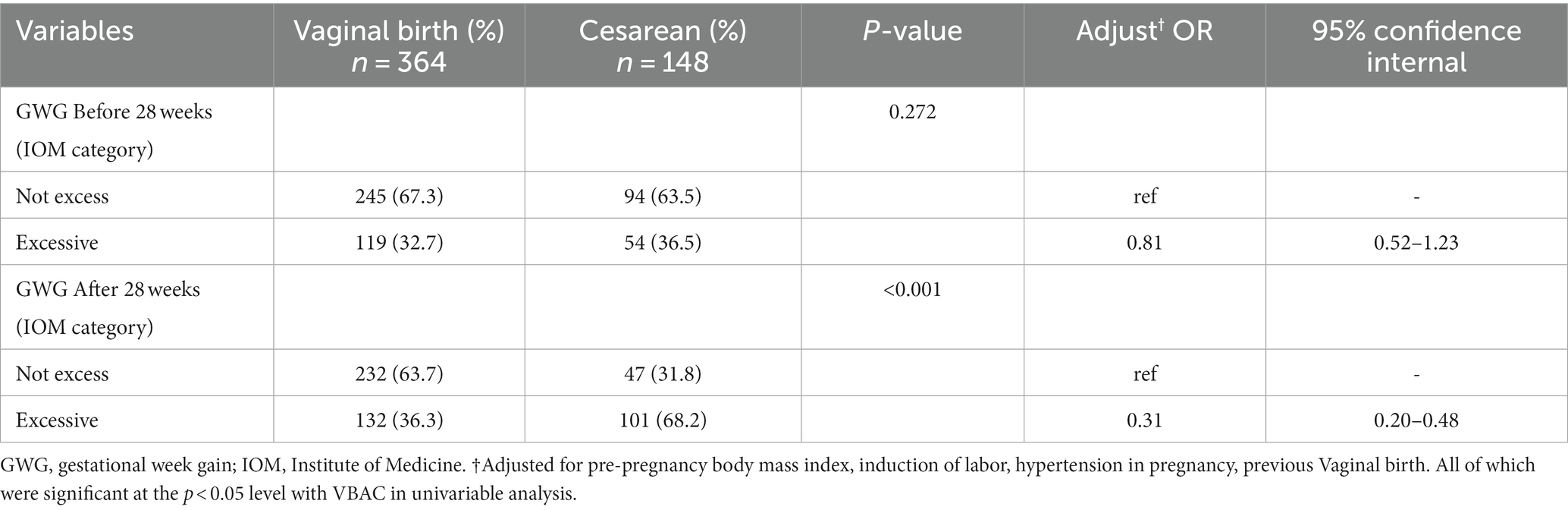
After adjusting for pre-pregnancy body mass index, induction of labor, previous vaginal birth or VBAC, hypertension in pregnancy, and other potential confounders, women who gained excessive weight after 28 weeks had significantly lower odds of vaginal birth than those who did not (Adjusted odds ratio [aOR] 0.31, 95% CI 0.20–0.48); however, excessive weight gain before 28 weeks had no significant effect on the VBAC rate (aOR 0.81, 95% CI 0.52–1.23) (Table 5).
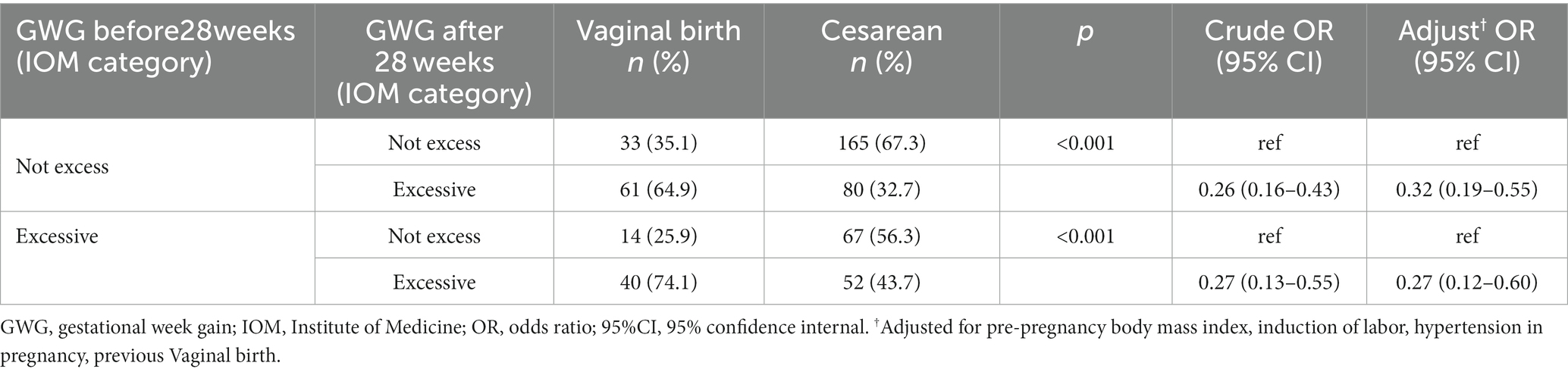
Table 6 shows the association between GWG after 28 weeks and the VBAC rate stratified by GWG before 28 weeks. We found that among women with excessive or non-excessive GWG before 28 weeks, the non-excessive GWG after 28 weeks group had less risk of failed TOLAC than the excessive GWG after 28 weeks group (aOR 0.27, 95% CI 0.12–0.60; aOR 0.32, 95% CI 0.19–0.55; respectively).
The aORs from the multivariable logistic regression models stratified by pre-pregnancy BMI are shown in Figure 1. We found that excessive gestational weight gain after 28 weeks was associated with a lower success rate of TOLAC than non-excessive weight gain in underweight, normal weight, and overweight women (aOR 0.23, 95% CI 0.06–0.88; aOR 0.42, 95% CI 0.25–0.70; and aOR 0.12, 95% CI 0.04–0.36; respectively). Gestational weight gain before 28 weeks was not associated with VBAC in any BMI category in this study.
4. Discussion
Among Chinese women in this study, excessive GWG after 28 weeks was linked to a higher risk of failed TOLAC among women with or without excessive GWG before 28 weeks. Compared with non-excessive GWG, excessive GWG after 28 weeks also reduces the VBAC rate among underweight, normal, and overweight women.
We found that nearly half of the women gained more weight than recommended after 28 weeks (45.5%), which was higher than that before 28 weeks (33.8%), contrary to the findings of a previous study which showed the GWG between the second and third trimesters was approximately the same in the underweight, normal, and overweight groups (28). Overweight women overweight women had a higher rate of excessive weight gain after 28 weeks of gestation, and other studies have shown that overweight and obese women are more likely to gain too much weight during pregnancy than women with a normal BMI (20, 29). We also revealed that women who exceeded the IOM recommended weight gain after 28 weeks had a higher likelihood of having induced labor and gestational hypertension, which is consistent with previous studies (20, 23). Interestingly, we found that women with diabetes in pregnancy tended not to exceed the IOM recommendations for GWG after 28 weeks. This result is consistent with previous studies, Shi et al. also found that less than the recommended amount of weight gain by the IOM was observed in more than one-third of the pregnant women who had GDM (17). A potential explanation for this finding is that the women with GDM who received the diagnosis between the 24th and 28th week of pregnancy managed to lower their blood glucose levels and curb their excessive weight gain by following a healthy diet and engaging in physical activity (30). Moreover, women who were prone to GDM were more likely to receive education about appropriate weight gain throughout pregnancy during prenatal care, in order to reduce the occurrence of known pregnancy complications, such as preeclampsia and fetal macrosomia. Therefore, these women might pay more attention to their dietary habits, have more physical activity, and ultimately have less GWG than women without GDM (31).
The overall chance of a successful TOLAC was 71.1%. Previous findings found that women who had delivered vaginally had a higher chance of vaginal birth (30). Our study also confirmed most prior reports that abnormal pre-pregnancy weight is linked to an increased rate of failed TOLAC (32, 33). Shi and his colleagues performed a retrospective cohort study that encompassed all TOLAC cases in the US from 2012 to 2020 to determine if overweight women were significantly less likely to undergo TOLAC (32). Herman and his colleagues found a link between maternal BMI and TOLAC utilization in a trial involving 536 pregnant women (33). In addition, consistent with previous studies (34, 35), we found that induction of labor and gestational hypertension were associated with failed TOLAC.
There is limited research on GWG and TOLAC outcomes. The likelihood of successful VBAC was reported to be 40% lower in patients who gained over 40 pounds by Juhasz and his colleagues (20), and Shi Hanxu and his team also found that weight gain exceeding 20 pounds during pregnancy was linked to a lower VBAC rate (32). In contrast, Jenny and her colleagues did not observe any effect of excessive GWG on TOLAC success rates (19). However, these studies did not performed a stratified analysis by pre-pregnancy BMI and gestational stage, which are potential modifiers of the relationship between GWG and TOLAC outcomes. Our results revealed that excessive GWG after 28 weeks was association with failed TOLAC. Further analysis found that increased risk of failed TOLAC was linked to excessive GWG after 28 weeks among women with or without excessive GWG before 28 weeks. Inconsistent with our study findings, IS et al. (24) suggested that trimester-specific GWG was not significantly associated with cesarean delivery in general outside the framework of TOLAC.
Two population-based studies analyzed the association between GWG and cesarean section stratified by pre-pregnancy BMI in pregnant women generally and arrived at different conclusions. Xu and his colleagues conducted a population-based cohort study with 174,953 singleton pregnancies and found that high GWG was associated with a higher overall risk of cesarean delivery for all BMI groups (36). On the other hand, a population-based cohort study which included 245,526 singleton term pregnancies, suggested that high weight gain during pregnancy increased the risk of cesarean delivery for obese women (37). In our study, we found that excessive GWG after 28 weeks was associated with a higher chance of cesarean delivery for all BMI groups (underweight, normal weight, and overweight), whereas the vaginal delivery was not influenced by excessive weight gain before 28 weeks.
The associations between excessive GWG after 28 weeks and the increased risks of failed TOLAC in our study might owing to several mechanisms. Excessive GWG after 28 weeks is positively related to pre-pregnancy overweight, induction of labor, and hypertension in pregnancy, which in turn could contribute to the increased risks of failing TOLAC (20, 23, 29). Moreover, excessive GWG may impair uterine contraction by increasing the amount of fat and cholesterol in the uterine muscle, resulting in reduced uterine contractility, longer labor duration, and more cesarean deliveries (38). However, it is unknown if the distribution of excessive fat differs before and after 28 weeks of gestation. Since fat distribution is an important factor in uterine contraction, whether excessive weight gain in the third trimester is more likely to lead to a relative increase in the distribution of fat in the uterus requires further research.
Some limitations of our study should be acknowledged. First, our study was conducted in a single center and excluded obese women, which may affect the applicability of our findings to other populations. Second, this was a retrospective study, which may lead to selection bias. It is possible that women with a high pre-pregnancy BMI were counseled toward choosing elective repeat cesarean delivery, and this may be one of the reasons why there were so few obese people in this study. Third, due to data limitations, we were unable to perform further analyses based on metabolic-related laboratory indicators (blood glucose, hemoglobin, etc.) and physical examination indicators (abdominal circumference, subcutaneous fat, etc.). Fourth, although our analysis stratified by different pre-conception BMI groups, there may be other unknown confounding variables which may influenced VBAC we did not account for in our analysis. Moreover, we did not further analyze women with gestational diabetes, such as whether exercise would affect their weight. Therefore, more studies are needed to explore this issue in depth in the future.
5. Conclusion
To sum up, our findings showed that regardless of pre-pregnancy weight status and weight gain before 28 weeks, excessive weight gain after 28 weeks of pregnancy was associated with decreased rates of VBAC. This finding suggests the importance of weight management in the third trimester to improve the chance of VBAC, especially in overweight women, who were more likely to gain excessive weight after 28 weeks. Our results suggest that women can increase their likelihood of achieving VBAC by managing their weight during pregnancy. Based on our results, we recommend that TOLAC women should be counseled to avoid excessive GWG after 28 weeks, no matter their pre-pregnancy BMI, to increase their possibility of VBAC success.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The study was approved by the Ethics Committee of the Fourth affiliated Hospital of Hebei Medical University (2022KS010). The patients/participants provided their written informed consent to participate in this study.
Author contributions
GL and HS conceived and designed the study and drafted the manuscript. GL, JZ, and HZ collected the clinical data. GL and CZ analyzed the data. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the Shanghai Educational Science Research Project (C2023160), Shanghai Clinical Research Center for Gynecological Diseases (22MC1940200), and Shanghai Urogenital System Diseases Research Center (2022ZZ01012).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Mu, Y, Li, X, Zhu, J, Liu, Z, Li, M, Deng, K, et al. Prior caesarean section and likelihood of vaginal birth, 2012-2016. China Bull World Health Organ. (2018) 96:548–57. doi: 10.2471/BLT.17.206433
2. Osterman, MJK. Recent trends in vaginal birth after cesarean delivery: United States, 2016-2018. NCHS Data Brief. (2020) 359:1–8.
3. Gross, MM, Matterne, A, Berlage, S, Kaiser, A, Lack, N, Macher-Heidrich, S, et al. Interinstitutional variations in mode of birth after a previous caesarean section: a cross-sectional study in six German hospitals. J Perinat Med. (2015) 43:177–84. doi: 10.1515/jpm-2014-0108
4. Landon, MB, Hauth, JC, Leveno, KJ, Spong, CY, Leindecker, S, Varner, MW, et al. Maternal and perinatal outcomes associated with a trial of labor after prior cesarean delivery. N Engl J Med. (2004) 351:2581–9. doi: 10.1056/NEJMoa040405
5. Lundgren, I, Morano, S, Nilsson, C, Sinclair, M, and Begley, C. Cultural perspectives on vaginal birth after previous caesarean section in countries with high and low rates – a hermeneutic study. Women Birth. (2020) 33:e339–47. doi: 10.1016/j.wombi.2019.07.300
6. Keedle, H, Schmied, V, Burns, E, and Dahlen, HG. The journey from pain to power: a meta-ethnography on women's experiences of vaginal birth after caesarean. Women Birth. (2018) 31:69–79. doi: 10.1016/j.wombi.2017.06.008
7. Basile Ibrahim, B, Kennedy, HP, and Whittemore, R. Women's perceptions of barriers and facilitators to vaginal birth after cesarean in the United States: an integrative review. J Midwifery Womens Health. (2020) 65:349–61. doi: 10.1111/jmwh.13083
8. Chan, MH, Hauck, Y, Kuliukas, L, and Lewis, L. Women's experiences of their involvement around care decisions during a subsequent pregnancy after a previous caesarean birth in Western Australia. Women Birth. (2021) 34:e442–50. doi: 10.1016/j.wombi.2020.09.007
9. Yao, R, Crimmins, SD, Contag, SA, Kopelman, JN, and Goetzinger, KR. Adverse perinatal outcomes associated with trial of labor after cesarean section at term in pregnancies complicated by maternal obesity. J Matern Fetal Neonatal Med. (2019) 32:1256–61. doi: 10.1080/14767058.2017.1404023
10. Trojano, G, Damiani, GR, Olivieri, C, Villa, M, Malvasi, A, Alfonso, R, et al. VBAC: antenatal predictors of success. Acta Biomed. (2019) 90:300–9. doi: 10.23750/abm.v90i3.7623
11. Tahseen, S, and Griffiths, M. Vaginal birth after two caesarean sections (VBAC-2)-a systematic review with meta-analysis of success rate and adverse outcomes of VBAC-2 versus VBAC-1 and repeat (third) caesarean sections. BJOG. (2010) 117:5–19. doi: 10.1111/j.1471-0528.2009.02351.x
12. Place, K, Kruit, H, Tekay, A, Heinonen, S, and Rahkonen, L. Success of trial of labor in women with a history of previous cesarean section for failed labor induction or labor dystocia: a retrospective cohort study. BMC Pregnancy Childbirth. (2019) 19:176. doi: 10.1186/s12884-019-2334-3
13. Lau, EY, Liu, J, Archer, E, McDonald, SM, and Liu, J. Maternal weight gain in pregnancy and risk of obesity among offspring: a systematic review. J Obes. (2014) 2014:524939. doi: 10.1155/2014/524939
14. Rasmussen, KM, Abrams, B, Bodnar, LM, Butte, NF, Catalano, PM, and Maria, S-RA. Recommendations for weight gain during pregnancy in the context of the obesity epidemic. Obstet Gynecol. (2010) 116:1191–5. doi: 10.1097/AOG.0b013e3181f60da7
15. Goldstein, RF, Abell, SK, Ranasinha, S, Misso, ML, Boyle, JA, Harrison, CL, et al. Gestational weight gain across continents and ethnicity: systematic review and meta-analysis of maternal and infant outcomes in more than one million women. BMC Med. (2018) 16:153. doi: 10.1186/s12916-018-1128-1
16. Qi, Y, Sun, X, Tan, J, Zhang, G, Chen, M, Xiong, Y, et al. Excessive gestational weight gain in the first and second trimester is a risk factor for gestational diabetes mellitus among women pregnant with singletons: a repeated measures analysis. J Diabetes Investig. (2020) 11:1651–60. doi: 10.1111/jdi.13280
17. Shi, P, Liu, A, and Yin, X. Association between gestational weight gain in women with gestational diabetes mellitus and adverse pregnancy outcomes: a retrospective cohort study. BMC Pregnancy Childbirth. (2021) 21:508. doi: 10.1186/s12884-021-03982-4
18. Juhasz, G, Gyamfi, C, Gyamfi, P, Tocce, K, and Stone, JL. Effect of body mass index and excessive weight gain on success of vaginal birth after cesarean delivery. Obstet Gynecol. (2005) 106:741–6. doi: 10.1097/01.AOG.0000177972.32941.65
19. McDonald, ACE, Wise, MR, and Thompson, JM. Effect of excessive gestational weight gain on trial of labour after caesarean: a retrospective cohort study. Aust N Z J Obstet Gynaecol. (2018) 58:64–71. doi: 10.1111/ajo.12664
20. Mei, JY, Havard, AL, Mularz, AJ, Maykin, MM, and Gaw, SL. Impact of gestational weight gain on trial of labor after cesarean success. Am J Perinatol. (2019) 36:1023–30. doi: 10.1055/s-0038-1675624
21. Voerman, E, Santos, S, Inskip, H, Amiano, P, Barros, H, Charles, MA, et al. Association of gestational weight gain with adverse maternal and infant outcomes. JAMA. (2019) 321:1702–15. doi: 10.1001/jama.2019.3820
22. Schiavone, M, Putoto, G, Laterza, F, and Pizzol, D. Gestational diabetes: an overview with attention for developing countries. Endocr Regul. (2016) 50:62–71. doi: 10.1515/enr-2016-0010
23. Dude, AM, Kominiarek, MA, Haas, DM, Iams, J, Mercer, BM, Parry, S, et al. Weight gain in early, mid, and late pregnancy and hypertensive disorders of pregnancy. Pregnancy Hypertens. (2020) 20:50–5. doi: 10.1016/j.preghy.2020.03.001
24. Gonzalez-Ballano, I, Saviron-Cornudella, R, Esteban, LM, Sanz, G, and Castan, S. Pregestational body mass index, trimester-specific weight gain and total gestational weight gain: how do they influence perinatal outcomes? J Matern Fetal Neonatal Med. (2021) 34:1207–14. doi: 10.1080/14767058.2019.1628942
25. Niquini, RP, Bittencourt, SA, and Leal, MC. Conformity of pre-gestational weight measurement and agreement of anthropometric data reported by pregnant women and those recorded in prenatal cards, City of Rio de Janeiro, 2007-2008. Rev Bras Epidemiol. (2013) 16:670–81. doi: 10.1590/S1415-790X2013000300011
26. Rangel Bousquet Carrilho, T, MR, K, Rodrigues Farias, D, Freitas Costa, NC, Araújo Batalha, M, ER, M, et al. Agreement between self-reported pre-pregnancy weight and measured first-trimester weight in Brazilian women. BMC Pregnancy Childbirth. (2020) 20. doi: 10.1186/s12884-020-03354-4
27. Mamun, AA, Callaway, LK, O'Callaghan, MJ, Williams, GM, Najman, JM, Alati, R, et al. Associations of maternal pre-pregnancy obesity and excess pregnancy weight gains with adverse pregnancy outcomes and length of hospital stay. BMC Pregnancy Childbirth. (2011) 11:62. doi: 10.1186/1471-2393-11-62
28. Xu, MY, Guo, YJ, Zhang, LJ, and Lu, QB. Effect of individualized weight management intervention on excessive gestational weight gain and perinatal outcomes: a randomized controlled trial. PeerJ. (2022) 10:e13067. doi: 10.7717/peerj.13067
29. Haugen, M, Brantsaeter, AL, Winkvist, A, Lissner, L, Alexander, J, Oftedal, B, et al. Associations of pre-pregnancy body mass index and gestational weight gain with pregnancy outcome and postpartum weight retention: a prospective observational cohort study. BMC Pregnancy Childbirth. (2014) 14:201. doi: 10.1186/1471-2393-14-201
30. Gitas, G, Alkatout, I, Ertan, KA, Rody, A, Proppe, L, Kocaer, M, et al. Risk factor analysis in women who underwent trial of labor after cesarean section: a multicenter study in Germany. J Turk Ger Gynecol Assoc. (2022) 23:137–44. doi: 10.4274/jtgga.galenos.2022.2022-1-2
31. Chuang, YC, Huang, L, Lee, WY, Shaw, SW, Chu, FL, and Hung, TH. The association between weight gain at different stages of pregnancy and risk of gestational diabetes mellitus. J Diabetes Investig. (2022) 13:359–66. doi: 10.1111/jdi.13648
32. Shi, H, Li, S, Lv, J, Wang, HHX, Hou, Q, and Jin, Y. Maternal and neonatal characteristics associated with clinical outcomes of TOLAC from 2012-20 in the USA: evidence from a retrospective cohort study. EClinicalMedicine. (2022) 54:101681. doi: 10.1016/j.eclinm.2022.101681
33. Ganer Herman, H, Kogan, Z, Shevach Alon, A, Stern, T, Bar, J, and Kovo, M. Trial of labor after cesarean in women in their second delivery - labor characteristics and postpartum factors which influence a patient's choice. J Matern Fetal Neonatal Med. (2022) 35:384–8. doi: 10.1080/14767058.2020.1719064
34. Wingert, A, Hartling, L, Sebastianski, M, Johnson, C, Featherstone, R, Vandermeer, B, et al. Clinical interventions that influence vaginal birth after cesarean delivery rates: Systematic Review & Meta-Analysis. BMC Pregnancy Childbirth. (2019) 19:529. doi: 10.1186/s12884-019-2689-5
35. He, X, Dai, Q, Wu, X, Zhou, J, and Li, J. Outcomes and risk factors for failed trial of labor after cesarean delivery (TOLAC) in women with one previous cesarean section: a Chinese population-based study. BMC Pregnancy Childbirth. (2022) 22:676. doi: 10.1186/s12884-022-05005-2
36. Xu, H, Arkema, EV, Cnattingius, S, Stephansson, O, and Johansson, K. Gestational weight gain and delivery outcomes: a population-based cohort study. Paediatr Perinat Epidemiol. (2021) 35:47–56. doi: 10.1111/ppe.12709
37. Cedergren, M. Effects of gestational weight gain and body mass index on obstetric outcome in Sweden. Int J Gynaecol Obstet. (2006) 93:269–74. doi: 10.1016/j.ijgo.2006.03.002
Keywords: trial of labor, weight gain, cesarean section, body mass index, pregnancy
Citation: Liu G, Zhang J, Zhou C, Zhang H and Shen H (2023) Effect of excessive gestational weight gain before and after 28 weeks on trial of labor after cesarean stratified by pre-pregnancy body mass index: a retrospective cohort study. Front. Med. 10:1157967. doi: 10.3389/fmed.2023.1157967
Edited by:
Simcha Yagel, Hadassah Medical Center, IsraelReviewed by:
Jinrong Li, Sichuan University, ChinaReyna Sámano, Instituto Nacional de Perinatología (INPER), Mexico
Copyright © 2023 Liu, Zhang, Zhou, Zhang and Shen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Haoran Shen, c2hlbmhhb3JhbkBmdWRhbi5lZHUuY24=
 Guangpu Liu
Guangpu Liu Jingya Zhang1
Jingya Zhang1 Haoran Shen
Haoran Shen