- 1School of Midwifery, College of Health Science and Medicine, Wolaita Sodo University, Wolaita Sodo, Ethiopia
- 2School of Public Health, College of Health Sciences and Medicine, Wolaita Sodo University, Wolaita Sodo, Ethiopia
- 3Department of Nursing, College of Medicine and Health Sciences, Wollo University, Dessie, Ethiopia
Background: Disrespectful and abusive maternity care is a sign of poor treatment that influences women’s choice to deliver their babies in institutions. Such malpractices continue to go unreported and are rarely exposed in developing countries, despite their serious burden. Therefore, this meta-analysis study aimed to estimate disrespect and abuse of women during childbirth in East Africa.
Methods: PubMed, Google Scholar, Scopus, and Science Direct databases were searched. Data were extracted using Microsoft Excel and analyzed using STATA statistical software (v. 14). Publication bias was checked by forest plot, Begg’s rank test, and Egger’s regression test. To look for heterogeneity, I2 was computed, and an overall estimated analysis was carried out. Subgroup analysis was done by study region, sample size, and publication. The pooled odds ratio for associated factors was also computed.
Results: Out of 654 articles assessed, 18 met the criteria and were included in this study. There were a total of 12,434 study participants. The pooled prevalence of disrespect and abuse of women during childbirth in East Africa was 46.85% (95% CI: 45.26.72–66.98), I2 = 81.9%. It was lower in studies with sample size greater than 5000 (33%). The disrespect and abuse rates between community-based studies (44.96%) and institutional-based studies (47.35%) did not differ significantly, though. Instrumental delivery (AOR = 2.70; 95%CI: 1.79–4.08), presence of complications (AOR = 6.41; 95% CI: 1.36–30.14), receiving care at government hospitals (AOR = 3.66; 95% CI: 1.09–12.23), and poor wealth index (AOR = 2.16; 95% CI: 1.26–3.70) were associated factors.
Conclusion: In East Africa, disrespect and abuse of women during childbirth was high. Instrumental delivery, presence of complications during childbirth, receiving care at government hospitals and poor wealth index were predictors of maternal disrespect and abuse. Safe delivery practice should be promoted. Training in compassionate and respectful maternity care, particularly in public hospitals, has also been recommended.
Introduction
Maternal mortality and morbidity among women of reproductive age in poor nations are primarily caused by complications during pregnancy and childbirth (1). There is widespread agreement that professional birthing services provided within a formal healthcare system can reduce the risk of maternal fatalities (2). More than 162,000 women still lose their lives in pregnancy and childbirth each year in sub-Saharan Africa (SSA). Most such fatalities occur within a day of delivery (3).
The East African countries are Burundi, Ethiopia, Comoros, Uganda, Rwanda, Tanzania, Mozambique, Madagascar, Zimbabwe, Kenya, and Zambia are among the poorest in the world and have low access to and affordability of maternal healthcare services (4). Moreover, the risk of adverse effects on the mother and the child is increased by a lack of access to appropriate obstetric care, particularly during delivery. Due to this service gap, women end up having poor maternal outcomes. In East Africa, the risk of death for those mothers is 1 in 31, compared to 1 in 4,300 in a high-income country (5).
A woman’s rights during maternity care are violated by disrespect and abuse (D&A), which is also referred to as mistreatment, obstetric violence, or dehumanized care (6). Women’s human rights are violated when they are treated disrespectfully and violently while receiving facility-based maternity care. This also keeps women from using maternal health services, erodes their satisfaction and confidence in the healthcare system, and results in unfavorable pregnancy outcomes (7–10). Respectful maternal care during facility-based maternity care is recommended by the World Health Organization (WHO) as a fundamental method for improving the quality of maternity services, to decrease disrespect and abuse as well as maternal mortality and morbidity (11). The biggest obstacle to receiving quality maternity care globally, however, is the growing evidence of the disrespect, abuse, and mistreatment of women throughout labor, delivery, and the postpartum period (10, 12, 13).
Growing data demonstrates that disrespect and abuse of maternal care, to varied degrees and severity, happens globally (14). Additionally, this research demonstrates that women get disrespectful and harsh care during childbirth (14). To ensure physical safety during institutional delivery, the quality of maternal health services is constrained (15, 16). Many women, however, do not receive the medically and culturally appropriate treatment that they require (17).
According to the Universal Declaration of the Rights of the Childbearing Woman, every woman has the right to sexual and reproductive healthcare that is respectful and dignified, including during childbirth (18, 19). As a result, abuse during childbirth may constitute a violation of women’s fundamental human rights (20) and may act as a strong deterrent to women seeking care in facilities for subsequent pregnancies (21–23). A seven-category model was proposed by Bowser and Hill in a landscape analysis of the evidence for disrespect and abuse in facility-based childbirth that was published (24). This model was intended to generate discussion and a research agenda for implementation, not to provide a thorough analysis of the available evidence. Physical abuse, non-consented clinical care, non-confidential care, substandard care, discrimination, abandonment, and imprisonment in health facilities (23) have all been major themes in more recent research on this subject (25–28).
Stress, exhaustion, irritation, and a lack of job satisfaction all have an impact on a healthcare provider’s negative behavior. The working environment and conditions at the facility, as well as work-related issues like severe workloads, long working hours, lax supervision, strained relationships with coworkers, and inadequate pay, all have an impact on these problems (7, 24, 29). Disrespect and abusive at these facilities has reportedly been linked to women’s underuse of healthcare facilities during birthing (23, 30, 31).
Several negative effects of D&A on women’s health and wellbeing have been documented, including fear about using medical facilities (24), an increased chance of birth complications (32), low self-ratings of health, sleeping issues, and symptoms of post-traumatic stress disorder (33). The prevalence of disrespect and abuse ranged from 15% in Tanzania (28) to 98% in Nigeria (27).
There are no data at the country level, despite the fact that numerous primary researches have confirmed disrespect and abuse during child birth in East Africa. Therefore, the goal of this systematic review and meta-analysis study was to determine the prevalence of disrespect and abuse of women during childbirth in East Africa and its determinants. Clinicians and other stakeholders will be able to address gaps in disrespect and abuse of women during childbirth and operational plans based on the study’s findings, which will provide them with the fundamental knowledge they need to provide every child bearing women.
Methods
Data synthesis and reporting
We conducted data analysis based on a single measurement result (disrespect and abuse). Tables, text, and a forest plot are used to present the results. Using the standard PRISMA checklist guideline, this systematic review and meta-analysis study was carried out to assess the overall prevalence of disrespect and abuse of women during child birth in East Africa (34) (Supplementary Table 1).
Search strategy
Articles on the disrespect and abuse in East Africa were searched using international online databases (Pub Med, Science Direct, Scopus, EMBASE, and Google Scholar). The following keywords and search terms were used during the search: “prevalence,” “disrespect,” “abuse,” “delivery,” “obstetric,” “parturition,” “maternity care,” “mistreatment during pregnancy,” “attitude of health personnel,” “professional misconduct,” and “East Africa.” Boolean operators like “OR” and “AND” were used to combine the search phrases as well as use them separately. The Population Exposure Controls and Outcome (PECO) searching guidelines were used to perform the search strategy and retrieve relevant articles from the databases specified above. The search was carried out from October 1, 2022, until November 1, 2022.
Study outcome
Any act of physical abuse, non-confidential care, non-consented care, non-dignified care, abandonment of care, discrimination, or detention in the facilities during childbirth is considered disrespectful and abusive behavior (35).
Inclusion and exclusion criteria
The papers that were included in this meta-analysis were those that were conducted in East African nations, were published in English, and had full texts that could be searched. Studies that included data on the disrespect and abuse of child birth were also reported on. Qualitative studies, studies from developed countries, research from duplicated sources, and articles missing the complete text were all omitted from this systematic review and meta-analysis. The eligibility of the included articles in this study was determined using the COCOPOP (Condition, Context, and Population) paradigm. Laboring women made up the study population (POP), with the prevalence of disrespect and abuse serving as the condition (CO), and only studies carried out in East-Africa serving as the context (CO).
Quality assessment
Two authors (NG and KT) independently assessed the standard of the research using the Joanna Briggs Institute (JBI) standardized quality appraisal checklist (36). The disagreement raised during the quality assessment was resolved through a discussion led by the third author (GA). The critical analysis checklist has eight parameters with yes, no, unclear, and not applicable options. The parameters involve the following questions:
(1) Where were the criteria for inclusion in the sample clearly defined?
(2) Were the study subjects and, therefore, the setting described in detail?
(3) Was the exposure measured result validly and reliably?
(4) Were the main objective and standard criteria used to measure the event?
(5) Were confounding factors identified?
(6) Were strategies to affect confounding factors stated?
(7) Were the results measured indeed and dependably? And (8) Was the statistical analysis suitable? Studies were considered low risk when they scored 50% and above on the quality assessment indicators, as reported in a Supplementary file (Supplementary Table 2).
Risk of bias assessment
Through the Hoy et al. (37) established bias assessment tool, which consists of 10 items that assess four domains of bias as well as internal and external validity, two writers (NG and GA) independently evaluated included papers for risk of bias. Any disagreement raised during the risk of bias assessment was resolved through a discussion led by the third author (KT). Finally, the argument was solved and reached with an agreement. The first four questions (items 1–4) assess whether there is selection bias, non–response bias, and external validity. The last six questions (items 5–10) evaluate the presence of measurement bias, analysis-related bias, and internal validity. Studies were labeled as having a “low risk of bias” if they answered “yes” to eight or more of the ten questions. Studies classed as “moderate risk” if they answered “yes” to six to seven of the ten questions, whereas studies classified as “high risk” if they answered “yes” to five or fewer of the ten questions, according to information in a Supplementary file (Supplementary Table 3).
Data extraction
Data extraction and analysis were carried out using STATA 14 software and a Microsoft Excel spreadsheet from 2016, respectively. Using a standardized Joanna Briggs Institute data extraction format, two authors (NG and KT) separately extracted all pertinent data. The disagreement raised during data extraction was resolved through a discussion led by the third author (GA). Finally, the argument was solved and reached with an agreement. Due to this study’s lack of a paper form, the data automation tool was not employed (manual data). The first author’s name, the year of publication, the study region, the study setting, the study design, the sample size, the prevalence of the prevalence of disrespect and abuse, the unadjusted odd ratio for variables, and the quality of each paper were retrieved.
Data analysis
The data were exported to STATA software version 14 for analysis after being extracted from all pertinent findings in a Microsoft Excel spreadsheet. A weighted inverse variance random-effects model was used in a meta-analysis to produce a pooled OR. The presence of heterogeneity was visually evaluated using a forest plot, which was then utilized to analyze and estimate the pooled estimate of disrespect and abuse. Analysis of subgroups was done based on the study setting and sample size. Sensitivity analysis was used to determine the impact of a single study on the meta-analysis estimate of prevalence as a whole. The funnel plot was used to examine potential publication bias, and Begg and Egger’s regression tests were used to examine it more objectively. The trim-and-fill method proposed by Duval and Tweedie (38) was used to control publication bias. Cochran’s Q X2 test and I2 statistics were used to test for heterogeneity, estimate the amount of total/residual heterogeneity, and measure variability caused by heterogeneity, respectively (39). A Univar ate meta-regression analysis was used to examine the effects of sample size and publication year variations on between-study heterogeneity (40).
Results
Search results and study characteristics
We retrieved a total of 654 articles from various international online databases, such as PubMed, Scopus, EMBASE, Science Direct, and Google Scholar. After excluding duplicate research, we were left with 503 studies that were chosen for full title and abstract screening. The remaining 154 studies were screened for full text articles after 349 studies were eliminated because of the titles and abstracts. After reviewing the full text, 136 articles were excluded for further reasons. Finally, this systematic review and meta-analysis study’s inclusion criteria included 18 articles (26, 28, 35, 41–56) with 12,434 study participants (Figure 1).
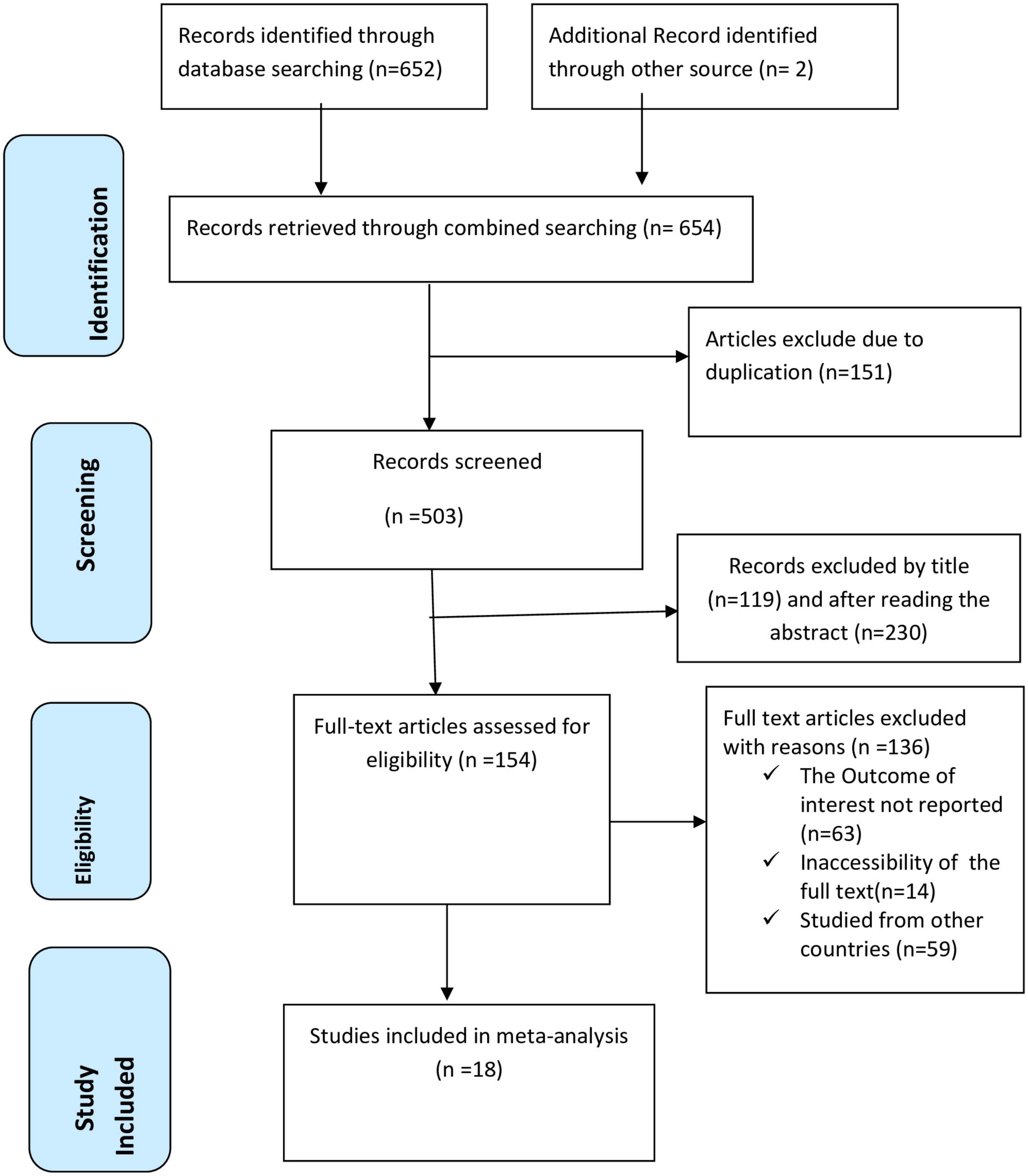
Figure 1. PRISMA flow chart displays the article selection process for the prevalence of disrespect and abuse of women during childbirth in East Africa.
Each of the included studies yielded low risk results and used a cross-sectional study methodology. The remaining studies were community-based, while 14 were cross-sectional studies carried out at healthcare facilities. Thirteen studies were carried out in Ethiopia (41, 43–48, 50–56), three in Tanzania (26, 28, 42), one in Kenya (49), and one in Sudan (51). Sample sizes varied from 204 to 2109. Disrespect and abuse of women during childbirth varied in prevalence from 1.9 to 98.9% (Table 1).
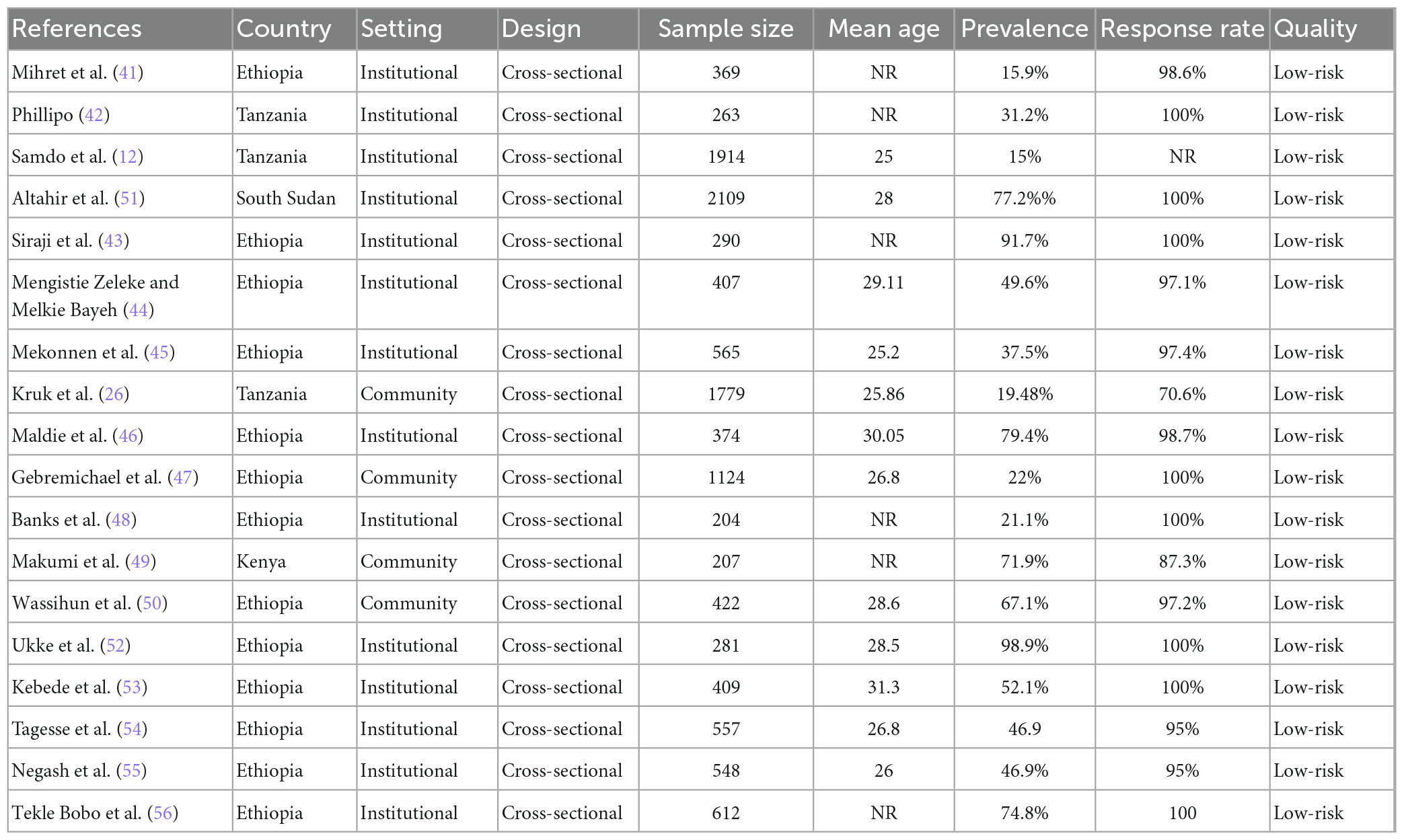
Table 1. Characteristics of studies included in the systematic review and meta-analysis of disrespect and abuse of women during childbirth in East Africa.
Meta-analysis
Prevalence of disrespect and abuse during childbirth
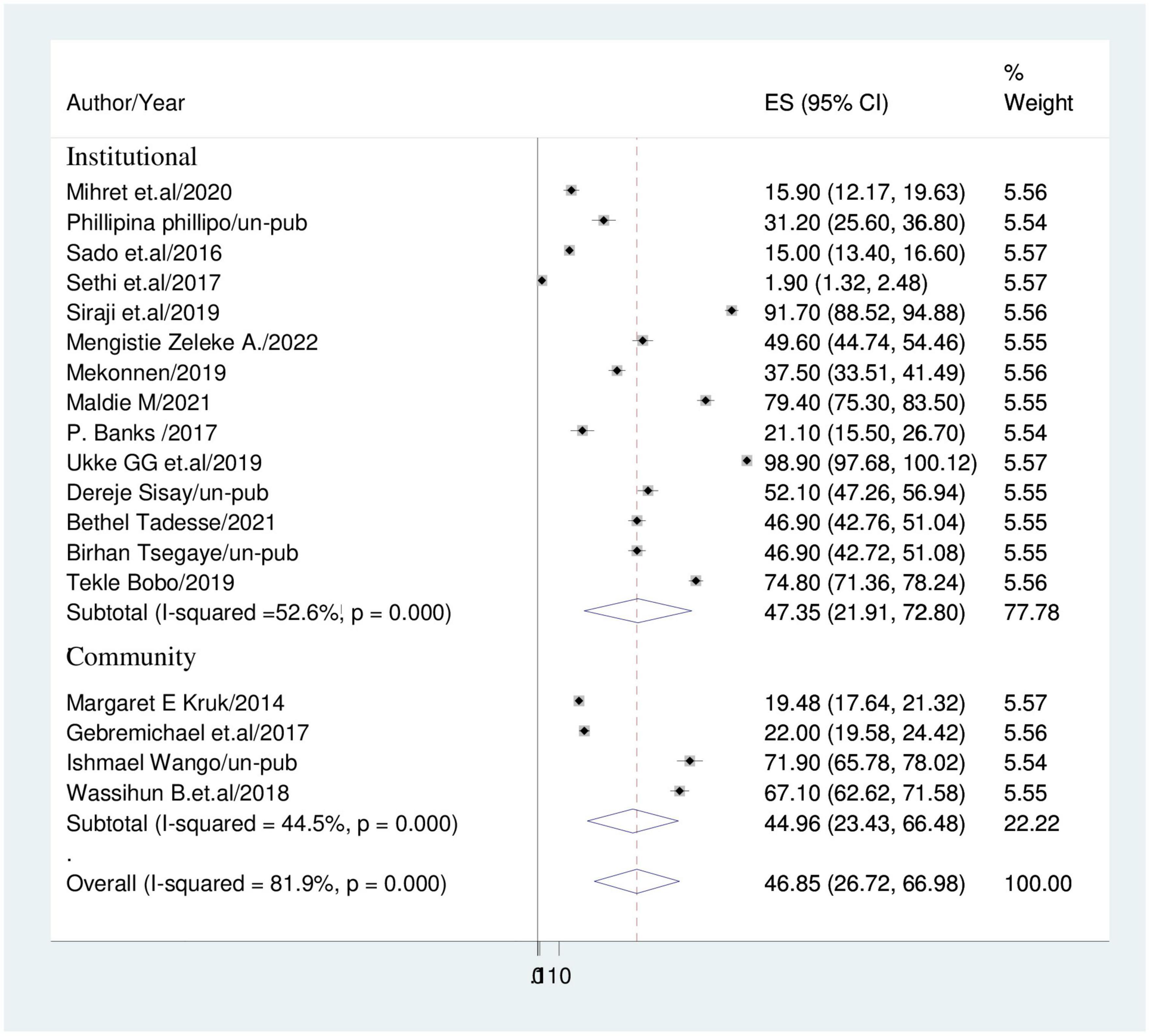
The overall estimate of disrespect and abuse during childbirth was computed using a DerSimonian and Laird random-effects model. As a result, the heterogeneity index (I2) was 81.9% (p < 0.001) and the pooled prevalence of disrespect and abuse of women during childbirth among women in East Africa was 46.85% (95% CI: 26.72, 66.97) (Figure 2).
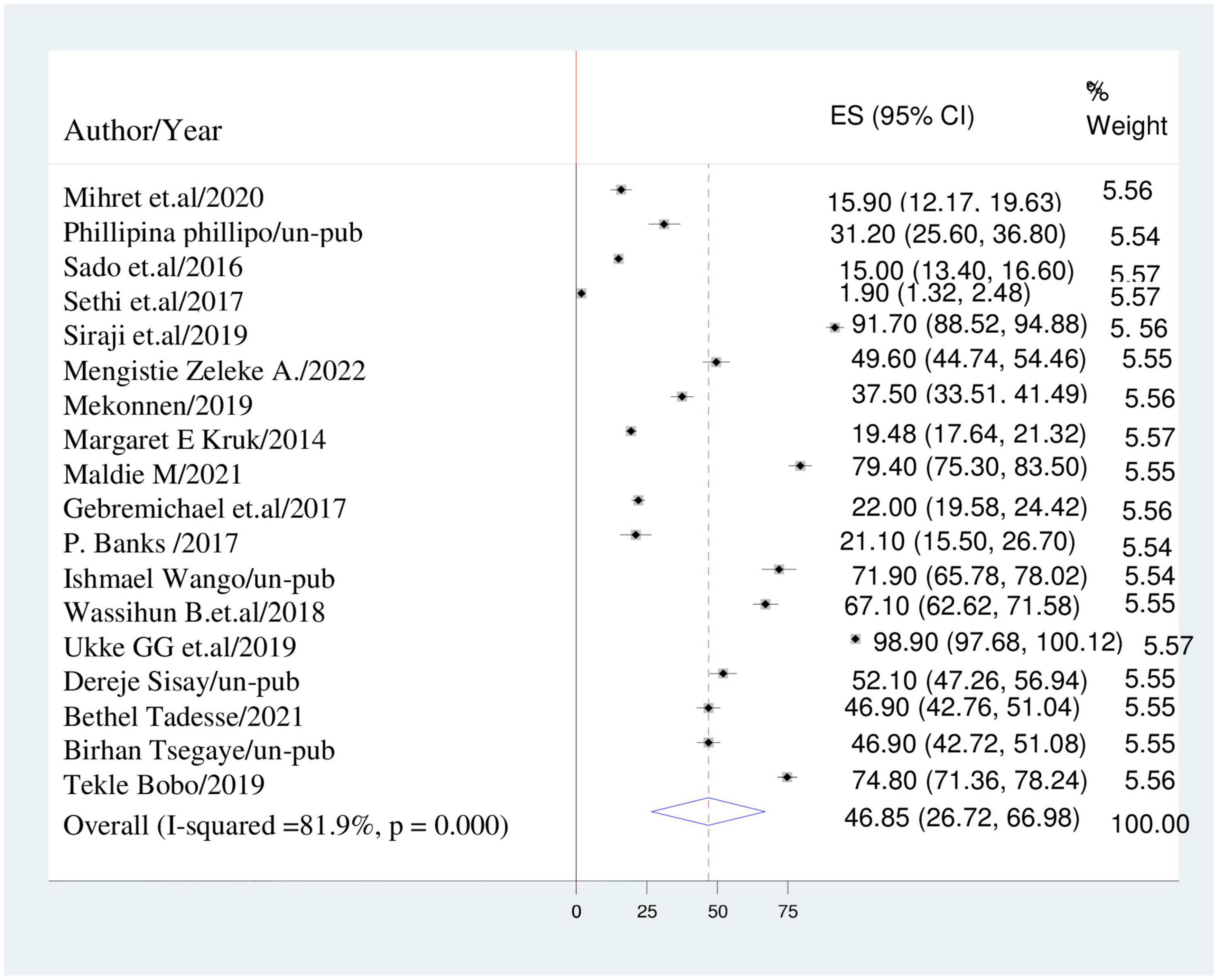
Figure 2. Forest plot displaying the pooled prevalence of disrespect and abuse of women during childbirth in East-Africa.
Subgroup analysis
Subgroup analysis based on sample size and study setting was carried out because this meta-analysis revealed a notable heterogeneity. Because of this, community based studies had the lower prevalence of disrespect and abuse during childbirth (44.96%; 95% CI: 23.43, 66.48); I2 = 44.5% than institutional based studies (47.35%; 95% CI: 21.91, 72.80); I2 = 52.6% (Figure 3). Studies with sample sizes of less than 500 had a prevalence of disrespect and abuse of women (57.92%; 95% CI: 36.83, 79.01); I2 = 29.3% while studies with sample sizes of more than 500 had a prevalence of (33%; 95% CI: 18.54, 47.44); I2 = 19.8% (Figure 4).
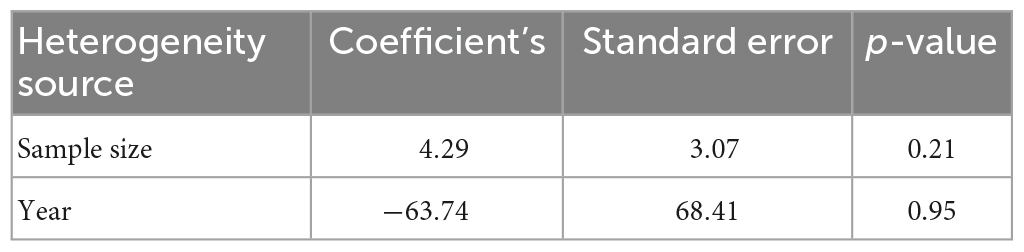
Heterogeneity and publication bias
We calculated a sub-group analysis based on sample size, and study setting to correct the reported heterogeneity of this study (I2 = 81.9%). Additionally, a univariate meta-regression utilizing the sample size and year as covariates was conducted to determine the root cause of heterogeneity. It demonstrated that the variability between research was unaffected by sample size or the year (Table 2).
A funnel plot was used to analyze the presence of publication bias visually, while the Egger’s test and Begg’s test were used to assess it objectively. The funnel plot shows an unequal distribution of studies upon visual observation (Figure 5). The Egger test (p = 0.002) and Begg test (p = 0.041) suggested a significant publication bias, thus we conducted Duval and Tweedie trim-and-fill analysis to address it across the studies. The pooled prevalence of disrespect and abuse of women during facility childbirth was revised to 1.7% after the inclusion of eight studies within the fill and trim analysis. Therefore, trim fill analysis was employed to correct publication bias when eight papers were included in the funnel plot (Figure 6).
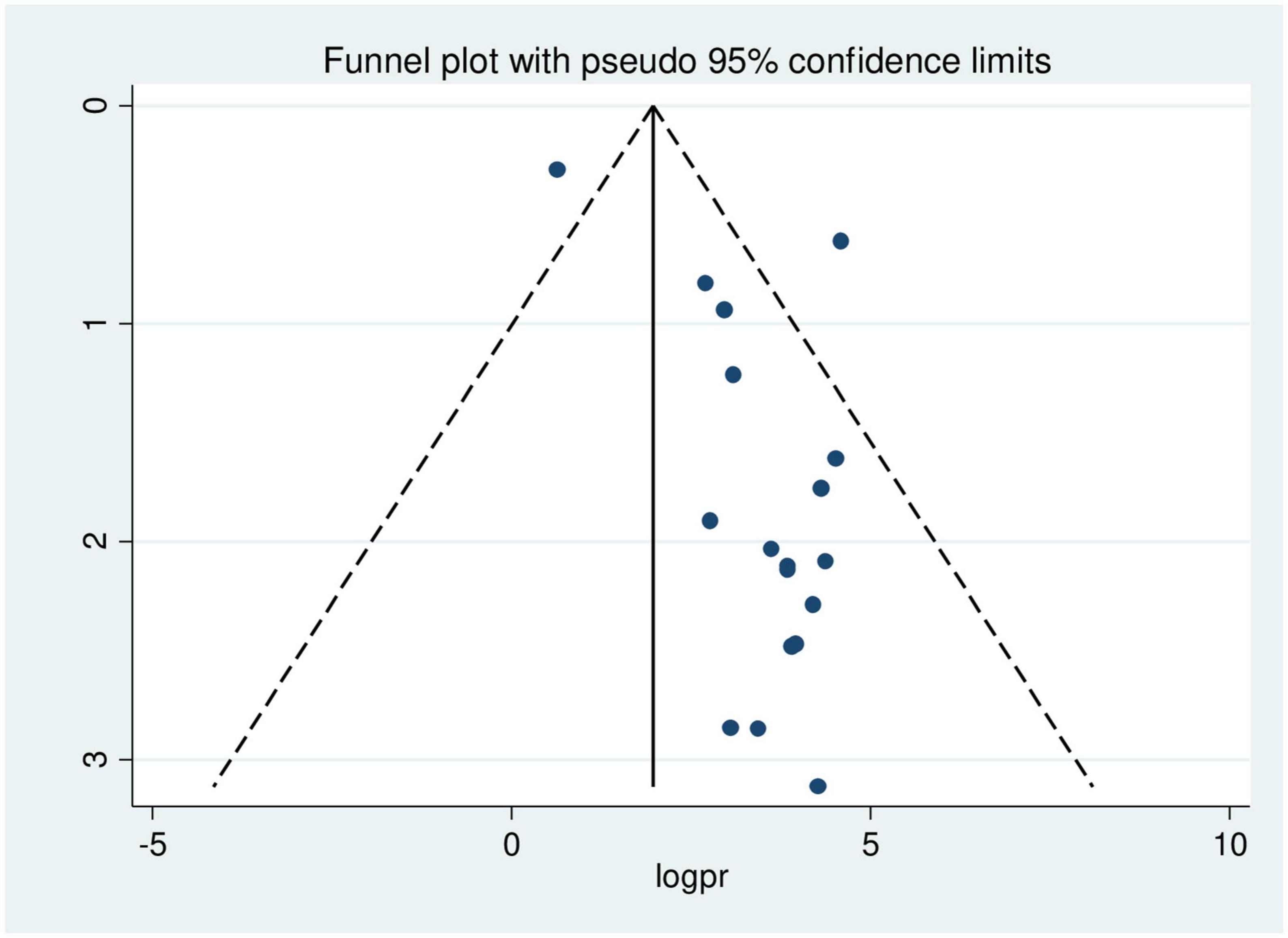
Figure 5. Funnel plot showing asymmetrical distribution of studies indicating the presence of publication bias.
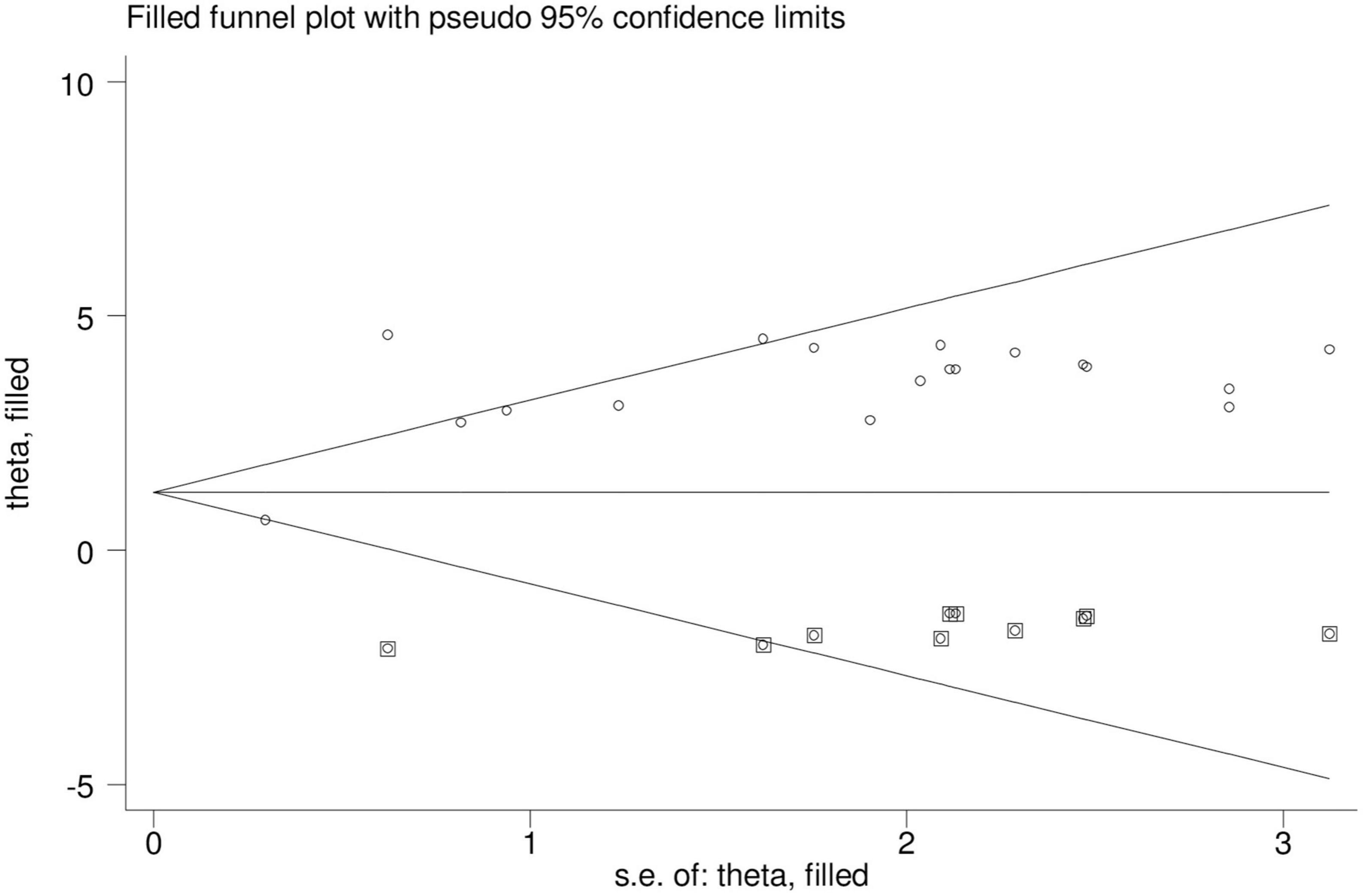
Figure 6. Trim and fill methods of analysis displaying the presence of eight missing studies causing for funnel plot asymmetry.
We also did a counter-enhanced funnel plot to identify potential causes of the funnel plot’s asymmetry. Given that the majority of this area contains regions with statistically significance, publication bias is more likely to be the main cause of this funnel asymmetry (P < 0.01). Different shaded patches are present to show statistical significance. In particular, p-values higher than 0.10 correspond to the center white shaded area, p-values between 0.10 and 0.05 to the heavy gray shaded region, p-values between 0.05 and 0.01 to the medium gray shaded region, and p-values less than 0.01 to the area outside the funnel (Figure 7).
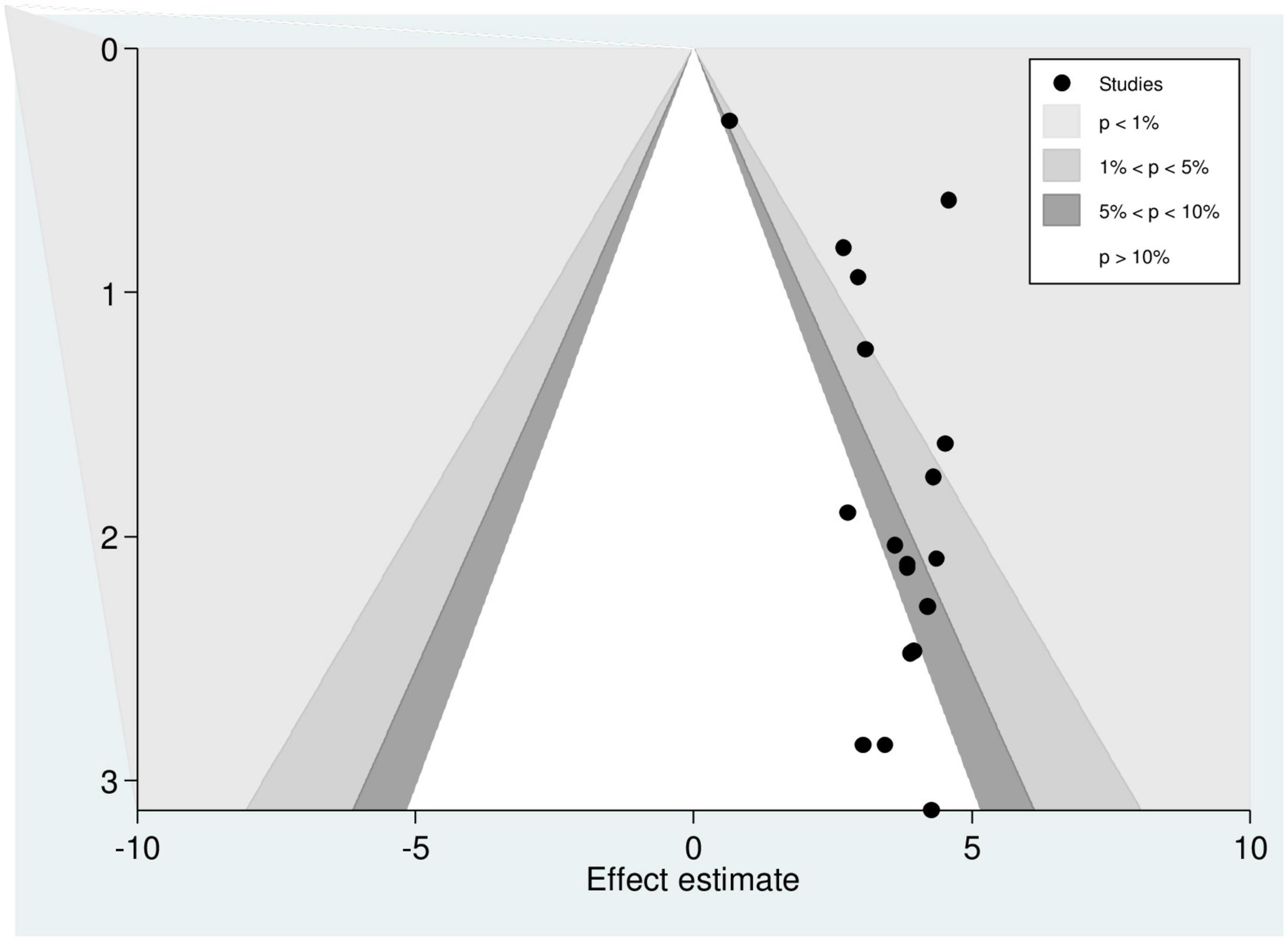
Figure 7. Counter-enhanced funnel plot showing that funnel plot asymmetry is due to the presence of publication bias.
Leave –one-out-sensitivity analysis
A leave-one-out sensitivity analysis was carried out to detect the effect of each study on the overall prevalence of disrespect and abuse of women during childbirth by excluding one study at a time. In the sensitivity analysis, both Altahir et al. and Ukke et al. showed an impact on the pooled prevalence of disrespect and abuse of women during childbirth at health facility (Table 3).
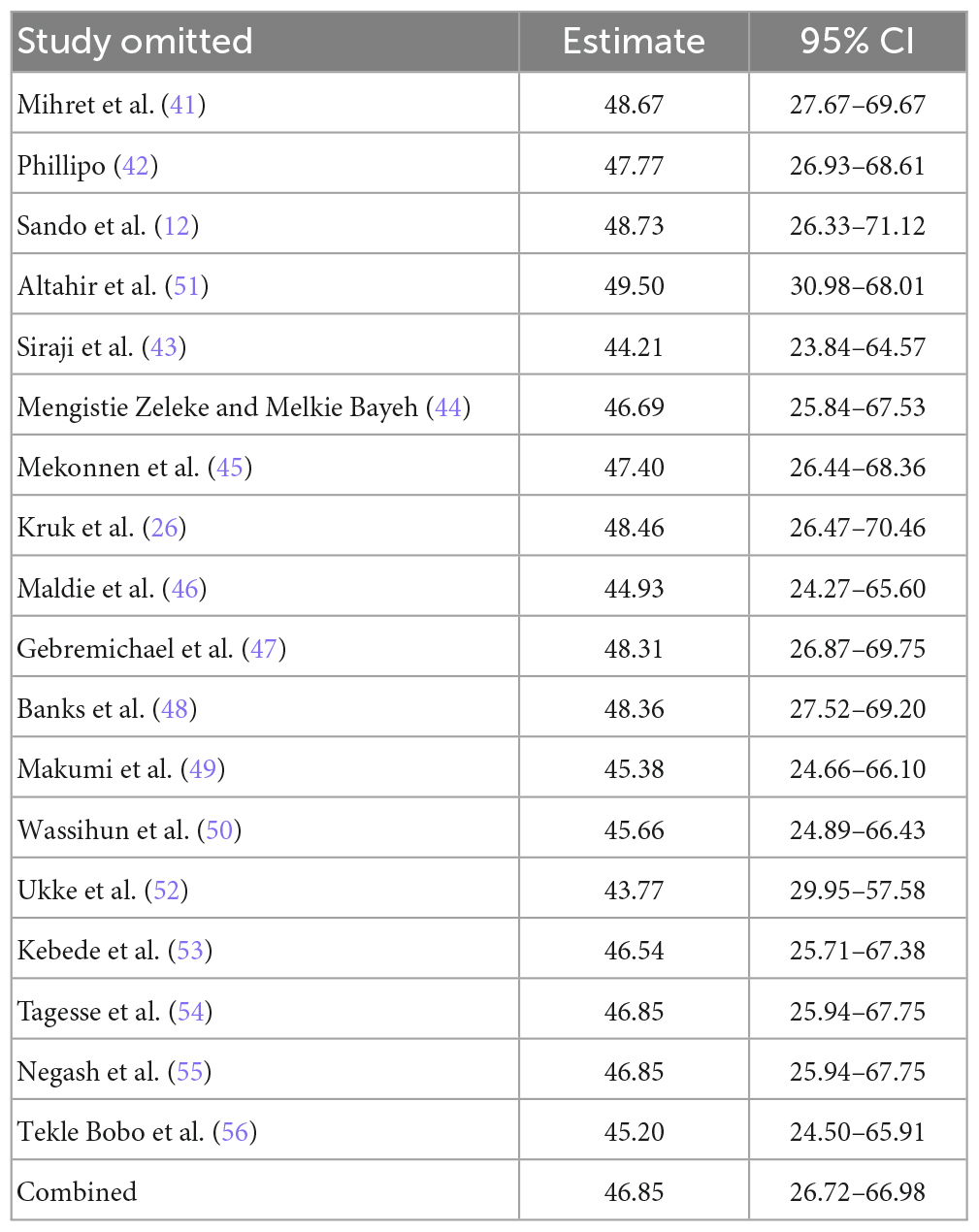
Table 3. The pooled prevalence of disrespect and abuse of women during childbirth in East Africa when one study omitted from the analysis a step at a time.
Factors associated with disrespect and abuse during childbirth
In this study, presence of complication during childbirth, receiving care at government hospitals, instrumental delivery, and poor wealth index were candidate variables of disrespect and abuse. Therefore, maternal disrespect and abuse were significantly associated with the presence of complications during childbirth, instrumental delivery, receiving of care at public hospitals and poor wealth index.
Instrumental delivery
According to this study, women who gave birth with instrumental delivery were 2.7 times more likely to be disrespected and abused as compared to women who gave birth with spontaneous vaginal delivery (stocktickerAOR = 2.70; 95%CI: 1.79,4.08). Random effect model was applied because of the existence of heterogeneity between studies (I2 = 57.3%) (Figure 8).
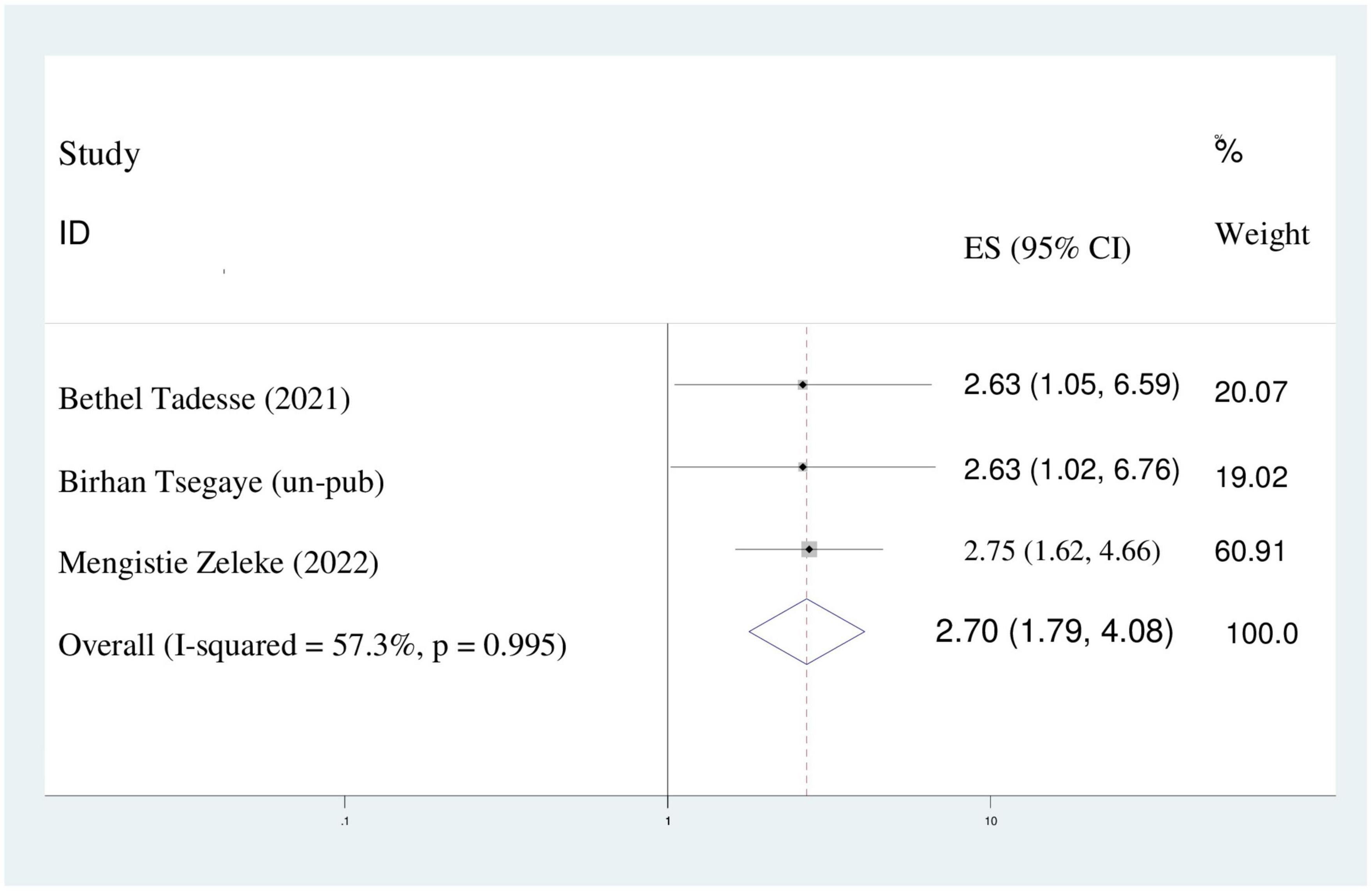
Figure 8. The pooled odds ratio displaying the association of instrumental delivery with disrespect and abuse of women.
Presence of complication during childbirth
This meta-analysis found that women who had complications during childbirth were six times more likely to be disrespected and abused than women who didn’t have complication during childbirth (AOR = 6.41%;95%CI: 1.36–30.14). A random effect model was assumed because the value of I2 was 71.6% (Figure 9).
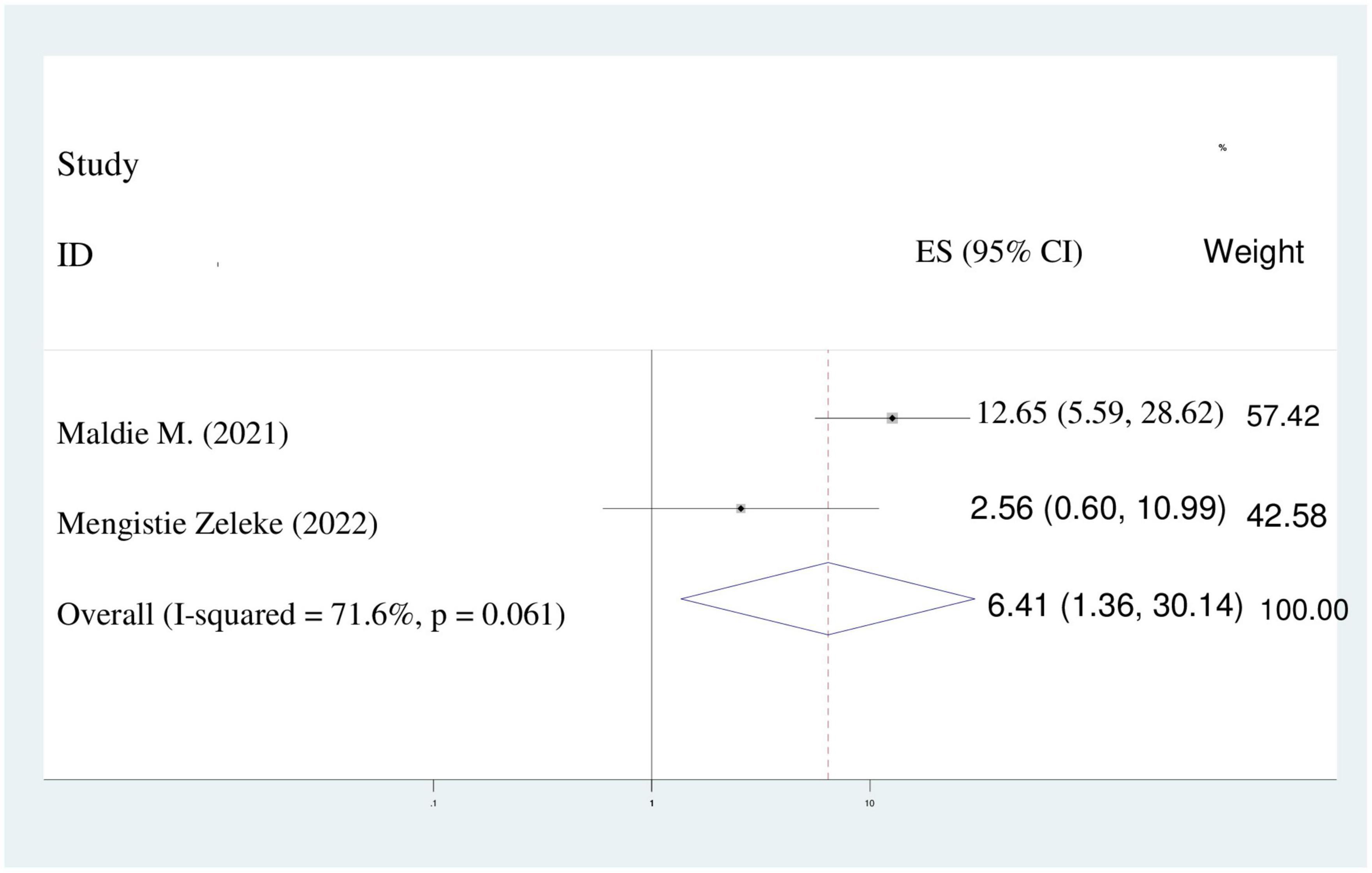
Figure 9. Pooled odds ratio displaying the association of presence of complications during childbirth with disrespect and abuse.
Receiving of care at government hospitals
In this study, the odds of maternal disrespect and abuse during childbirth in government hospitals were 3.6 times higher than their counterparts (AOR = 3.66; 95%CI: 1.09–12.23). Because of I2 static indicated heterogeneity (89.6%), a random effect model was selected for the analysis (Figure 10).
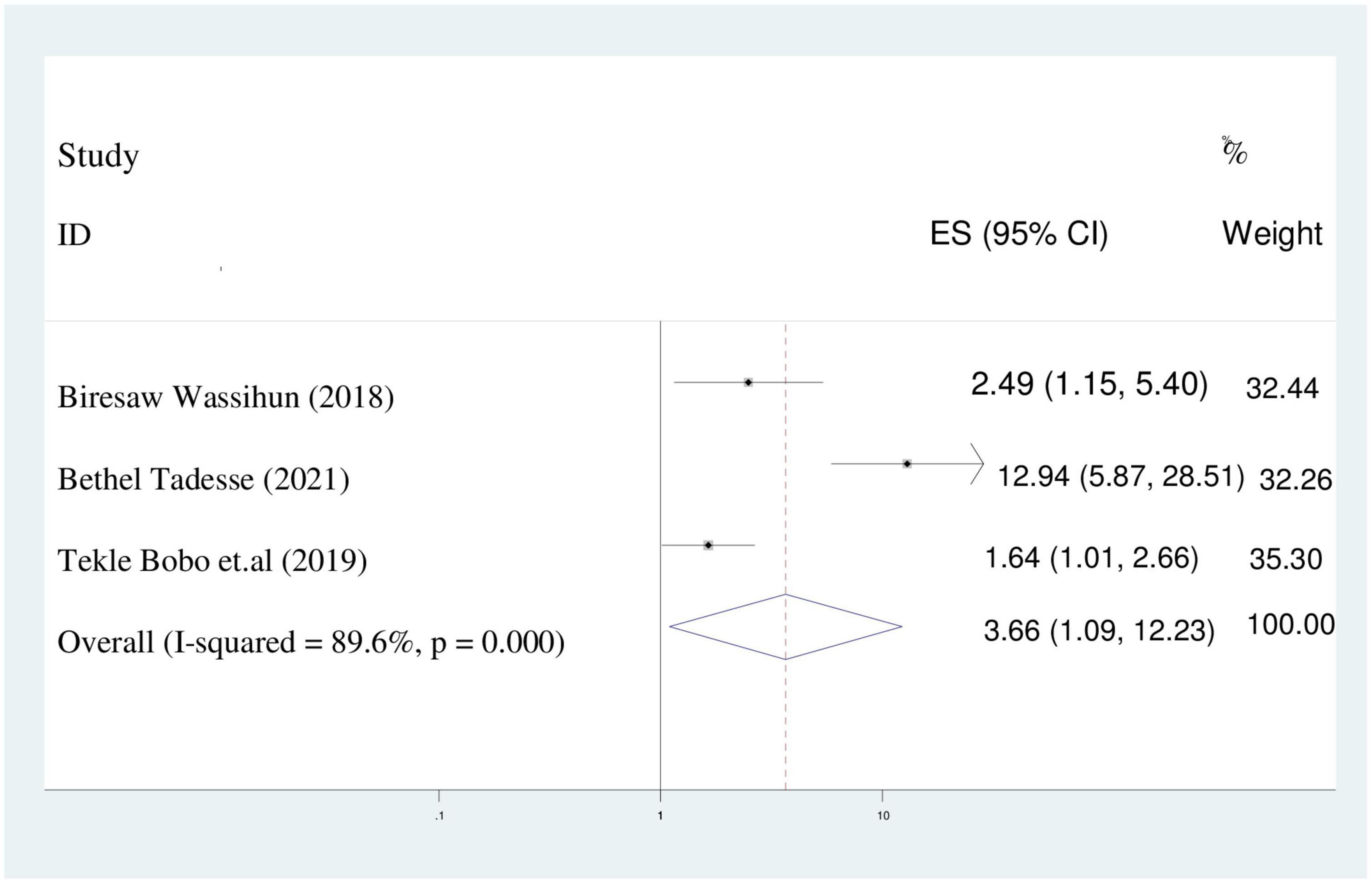
Figure 10. Pooled odds ratio displaying the association of receiving care at government hospitals with disrespect and abuse of women.
Poor wealth index
The chance of maternal disrespect and abuse of women who had poor wealth index were two times higher than women who had rich wealth index (AOR = 2.16; 95%CI: 1.26–3.70). We utilized random effect model because of the presence of heterogeneity (I2 = 46.2%) (Figure 11).
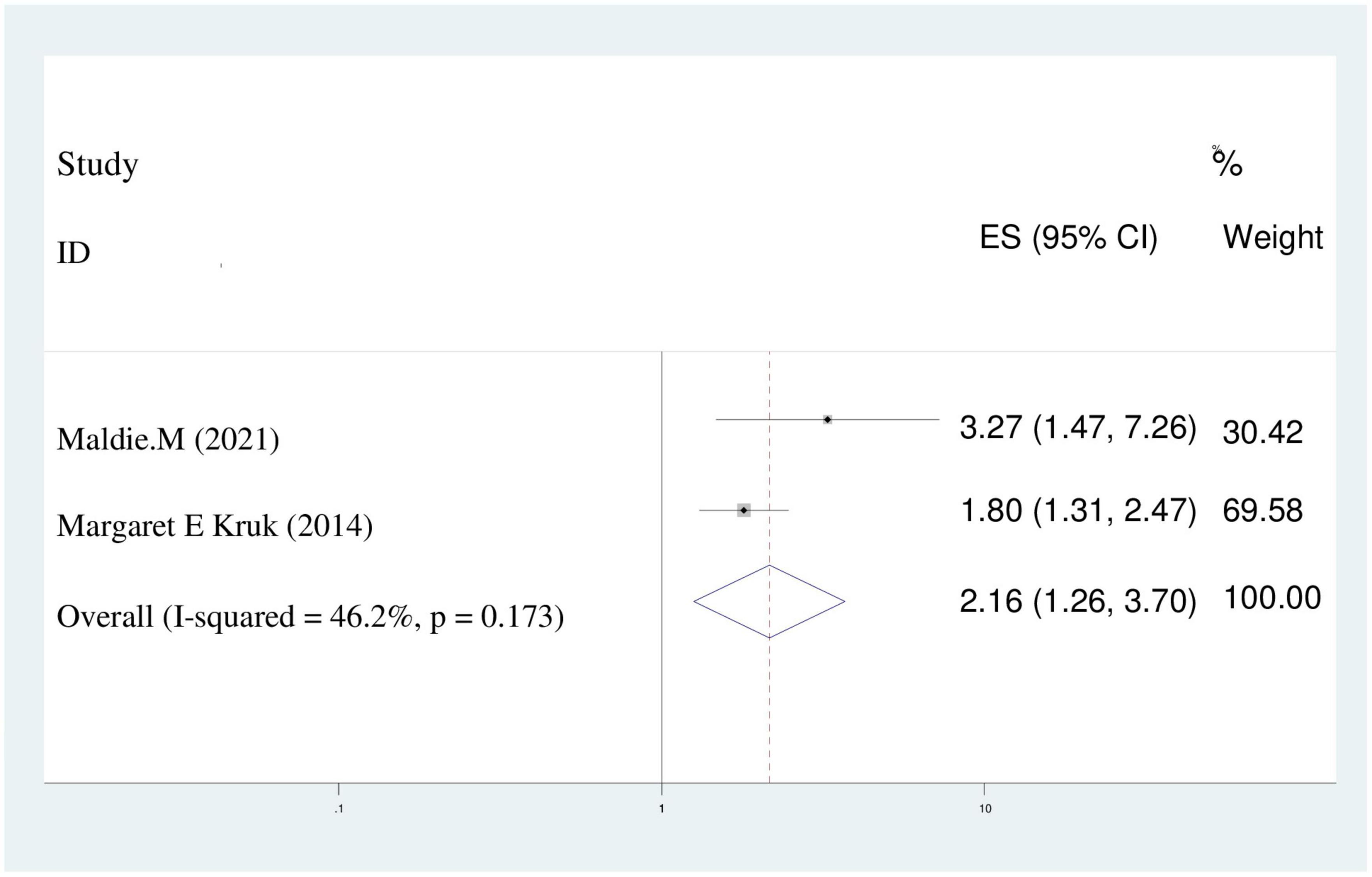
Figure 11. Pooled odds ratio displaying the association of poor wealth index with disrespect and abuse of women.
Discussion
The fundamental rights of women, newborns, and families are violated when women are treated disrespectfully or violently when giving birth at a medical facility. One of the world’s biggest problems is the mistreatment of women who are giving birth in medical facilities. Due to the focus on reducing both maternal and newborn morbidity and mortality through the implementation of various measures such boosting institutional delivery and woman-friendly care. Meanwhile, using institutional delivery is difficult because of the disrespect and mistreatment of women while they are giving birth in a medical facility.
Three areas are highlighted in the World Health Organization’s (WHO) vision for the quality of maternal and newborn health under the experience component of quality of care: communication, emotional support, and dignity and respect (57). Dignity and respect place a premium on providing care that upholds women’s rights to privacy, confidentiality, and freedom from mistreatment such physical and verbal abuse and discrimination (58). In poor nations where a big proportion of clients are served by a small number of care professionals, disrespect and abuse are frequently more of an issue (58).
To improve the standard of care and the use of expert delivery services, respectful care during labor must be promoted (59). Abuse and disrespect have a negative impact on the use of competent delivery services, an intervention that has been shown to significantly lower maternal mortality across the globe (60). The key findings were that the estimate of disrespect and abuse of women during childbirth and disrespect and abuse of women were significantly related to the maternal wealth status, receiving at governmental hospitals, presence of complication during childbirth and instrumental delivery. The purpose of this systematic review and meta-analyses was to ascertain the general prevalence of disrespect and abuse among East African women as well as the factors that contribute to it. Therefore, the overall prevalence of disrespect and abuse of women during childbirth was 46.85% (95% CI: 26.72–66.98) in this study. The results of the current study are in line with meta-analysis studies conducted in Ethiopia (49.4%) (36) and Sub-Saharan African nations (44.09%) (61). This could be as a result of the research locations’ shared socioeconomic traits.
The results of this study are lower than those from studies done in Nepal (70.1%) (62), India (60%, 84.3%) (63, 64), Iran (75.5%) (65), Pakistan 97.4% (66), Pakistan 99.7% (67), and Peru 97.4% (68). The study population, the different health facility set up, and the definition of disrespect and abuse all may have an impact.
The results of this study was higher than those of studies conducted in Mexico (18.8%) (69), Brazil (18.3%) (70) and India (28%) (71) in comparison. Socioeconomic differences, variations in healthcare providers’ knowledge, attitudes, and skills, variations in healthcare facilities and systems, variations in study time and sampling methods, and differences in how disrespect and abuse of women during childbirth are defined at various healthcare facilities could all be contributing factors.
In thesis meta-analysis, presence of complication during childbirth, receiving care at governmental hospitals, poor wealth index, and instrumental delivery were predictors of maternal disrespect and abuse during childbirth. Women who utilized an instrument had a 2.7 higher likelihood of being disrespected and abused than those who gave delivery naturally vaginally. Studies from Pakistan (66) and India (64, 72) and their findings are in agreement with this one. The greater patient load and unfavorable patient-provider ratio in medical facilities may be the cause. The current study’s findings may be explained by the fact that, in comparison to higher-level settings, the delivery of health services in low-level settings is hampered by a lack of standards, leadership, supervision, and quality clinical care, as well as by a severe lack of multidisciplinary teams and training.
There was a 6-fold increase in the likelihood of disrespect and maltreatment among women who experienced complications during labor. This result agrees with the findings of the Indian study (72). She may have become susceptible to disrespect and abuse because of the risk of labor complications, which might have put the midwives on edge. Alternatively, the abuse or perceived disrespect may have been an effort by the midwives to shift the burden for the complications to her. There may be a statistically significant correlation between the lack of access to high-quality maternity care and disrespect and abuse of women. This is a crucial discovery since maternal stress of any kind slows down the labor process and raises the risk of problems (73). Therefore, in order to enhance maternal health outcomes, it is necessary to address the types of abusive provider behavior that can lead to difficulties.
According to this study, women with low wealth indices were twice as likely to experience abuse and contempt as women with high wealth indices. This result is in line with research conducted in Pakistan (74). The explanation could be because facility-based healthcare personnel treat wealthier women with greater respect and consideration than impoverished ones.
In contrast to women receiving care at private hospitals, the current study found that women receiving care at public hospitals were 3.7 times more likely to experience abuse and contempt.
The possible explanation for this is that, in contrast to health centers where there may be relatively fewer complicated cases and care providers are less stretched, hospitals with higher case loads and overflowing referrals of complicated cases that cause overcrowding may push care providers to provide abusive care.
In this study, a random-effect model was utilized to address a sizable variance that occurred in between-study heterogeneity. No single study significantly influenced the overall prevalence of disrespect and abuse of women, according to the results of a leave-one-out sensitivity analysis. To determine the presence of heterogeneity, sub-group analysis based on sample size, and study settings was conducted. The considerable heterogeneity may result from variations in the sample populations, variations in the paper’s properties, or variations in socio-cultural factor.
Conclusion
To sum up, there was a significant frequency of abuse and disrespect toward women in East Africa after childbirth. The prevalence of disrespect and abuse of women during childbirth also varied depending on the study location and sample size. Significantly contributing factors to disrespect and abuse of women during childbirth included the presence of maternal difficulties during childbirth, low wealth index, receiving care at a government hospital, and instrumental delivery. It is advised that medical professionals adhere to the concepts of compassionate and respectful maternity care. Additionally, spontaneous vaginal birth and safe delivery practices have been recommended.
Strength and limitations
This study has some limitations. First, the study protocol was not registered in the prospective international register of systematic reviews (PROSPERO). Second, articles were restricted to only being published in the English language. Third, all of the included studies were cross-sectional, which might affect the outcome variable because of other confounding factors.
This research has some strength. First, compressive electronic online international searching engines were used. Second, the predictors of disrespect and abuse were discovered.
Data availability statement
The original contributions presented in this study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
NG conceptualized the study. NG and GA contributed to during data extraction and analysis. NG and KT wrote result interpretation. NG, GA, and KT prepared the first draft, contributed during the conceptualization and interpretation of results and substantial revision, and revised and finalized the final draft manuscript. All the authors read and approved the final version of the manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2023.1117116/full#supplementary-material
Supplementary Table 1 | Prisma checklist.
Supplementary Table 2 | Methodological quality assessment of included studies using Joanna Brigg’s Institute quality appraisal criteria scale (JBI). The eight item questions assessing inclusion criteria, study setting and participant, exposure measurement, objectives, confounder, statically analysis, outcome measurement and dealing confounder were used.
Supplementary Table 3 | Risk of bias assessment for the included studies. The ten item questions of which four items assess external and six items assess internal validity were used.
References
1. Kassebaum N, Bertozzi-Villa A, Coggeshall M, Shackelford K, Steiner C, Heuton K, et al. Global, regional, and national levels and causes of maternal mortality during 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. (2014) 384:980–1004. doi: 10.1097/01.aoa.0000472714.57328.86
2. Campbell O, Calvert C, Testa A, Strehlow M, Benova L, Keyes E, et al. The scale, scope, coverage, and capability of childbirth care. Lancet. (2016) 388:2193–208. doi: 10.1016/S0140-6736(16)31528-8
3. Darega B, Dida N, Tafese F, Ololo S. Institutional delivery and postnatal care services utilizations in Abuna Gindeberet District, West Shewa, Oromiya Region, Central Ethiopia: A community-based cross sectional study. BMC Pregnancy Childbirth. (2016) 16:149. doi: 10.1186/s12884-015-0735-5
4. World Health Organization [WHO]. World health statistics 2010. Geneva: World Health Organization (2010).
5. Zere E, Tumusiime P, Walker O, Kirigia J, Mwikisa C, Mbeeli T. Inequities in utilization of maternal health interventions in Namibia: implications for progress towards MDG 5 targets. Int J Equity Health. (2010) 9:16.14. doi: 10.1186/1475-9276-9-16
6. Manning A, Schaaf M. Amy Manning 1 & Marta Schaaf 1, with gracious input from members of the respectful maternity care council guideline. Geneva: Maternal Health Task Force/WHO (2015). p. 1–6.
7. Bohren M, Vogel J, Hunter E, Lutsiv O, Makh S, Souza J, et al. The mistreatment of women during childbirth in health facilities globally: a mixed-methods systematic review. PLoS Med. (2015) 12:e1001847. doi: 10.1371/journal.pmed.1001847
8. Moran A, Jolivet R, Chou D, Dalglish S, Hill K, Ramsey K, et al. A common monitoring framework for ending preventable maternal mortality, 2015–2030: phase I of a multi-step process. BMC Pregnancy Childbirth. (2016) 16:250. doi: 10.1186/s12884-016-1035-4
9. Afulani P, Phillips B, Aborigo R, Moyer C. Articles Person-centred maternity care in low-income and middle-income countries: analysis of data from Kenya. Lancet Glob Health. (2018) 7:e96–109. doi: 10.1016/S2214-109X(18)30403-0
10. Miller S, Abalos E, Chamillard M, Ciapponi A, Colaci D, Comande D, et al. Beyond too little, too late and too much, too soon: a pathway towards evidence-based, respectful maternity care worldwide. Lancet. (2016) 388:2176–92. doi: 10.1016/S0140-6736(16)31472-6
11. World Health Organization [WHO]. The prevention and elimination of disrespect and abuse during facility based childbirth: WHO statement. Geneva: World Health Organization (2015).
12. Sando D, Abuya T, Asefa A, Banks K, Freedman L, Kujawski S, et al. Methods used in prevalence studies of disrespect and abuse during facility based childbirth: lessons learned. Reprod Health. (2017) 14:127. doi: 10.1186/s12978-017-0389-z
13. Sadler M, Santos M, Ruiz-Berdun D, Rojas G, Skoko E, Gillen P, et al. Moving beyond disrespect and abuse: addressing the structural dimensions of obstetric violence. Reprod Health Matt. (2016) 24:47–55. doi: 10.1016/j.rhm.2016.04.002
14. World Health Organization [WHO]. Fact sheet maternal mortality. Geneva: World Health Organization (2016).
15. Milman school of public health, C.U. Disrespect and abuse during child birth. New York: Averting Maternal Death and Disability. (2012).
16. University Reserch Co., Llc. Maternal and newborn health. Uganda: University Reserch Co., LLC (2012).
17. Margaret E, Greene O. Delivering success scaling up solutions for maternal health. London: Willesden Centre for Health & Care (2013).
18. United Nations Human Rights Council. Technical guidance on the application of a human rights based approach to the implementation of policies and programmes to reduce preventable maternal morbidity and mortality: report of the Office of the United Nations High Commissioner for Human Rights. New York, NY: United Nations Human Rights Council (2012).
19. White Ribbon Alliance. Respectful maternity care: the universal rights of child bearing women. Washington, DC: White Ribbon Alliance (2011).
20. World Health Organization [WHO]. The prevention and elimination of disrespect and abuse during facility based childbirth: WHO statement. Geneva: World Health Organization (2014).
21. Bohren M, Hunter E, Munthe-Kaas H, Souza J, Vogel J, Gulmezoglu A. Facilitators and barriers to facility-based delivery in low-and middle-income countries: a qualitative evidence synthesis. Reprod Health. (2014) 11:71. doi: 10.1186/1742-4755-11-71
22. Chadwick R, Cooper D, Harries J. Narratives of distress about birth in South African public maternity settings: a qualitative study. Midwifery. (2014) 30:862–8. doi: 10.1016/j.midw.2013.12.014
23. Moyer C, Adongo P, Aborigo R, Hodgson A, Engmann C. They treat you like you are not a human being: maltreatment during labour and delivery in rural northern Ghana. Midwifery. (2014) 30:262–8. doi: 10.1016/j.midw.2013.05.006
24. Bowser D, Hill K. Exploring evidence for disrespect and abuse in facility-based childbirth: report of a landscape analysis. Washington DC: United States Agency for International Development (2010).
25. Warren C, Njuki R, Abuya T, Ndwiga C, Maingi G, Serwanga J, et al. Study protocol for promoting respectful maternity care initiative to assess measure and design interventions to reduce disrespect and abuse during childbirth in Kenya. BMC Pregnancy Childbirth. (2013) 13:21. doi: 10.1186/1471-2393-13-21
26. Kruk M, Kujawski S, Mbaruku G, Ramsey K, Moyo W, Freedman L. Disrespectful and abusive treatment during facility delivery in Tanzania: a facility and community survey. Health Policy Plan. (2014) 33:e26–33. doi: 10.1093/heapol/czu079
27. Okafor I, Ugwu E, Obi S. Disrespect and abuse during facility-based childbirth in a low-income country. Int J Gynaecol Obstet. (2015) 128:110–3. doi: 10.1016/j.ijgo.2014.08.015
28. Sando D, Kendall T, Lyatuu G, Ratcliffe H, McDonald K, Mwanyika-Sando M, et al. Disrespect and abuse during childbirth in Tanzania: are women living with HIV more vulnerable? J Acquir Immune Defic Syndr. (2014) 67:S228–34. doi: 10.1097/QAI.0000000000000378
29. Mannava P, Durrant K, Fisher J, Chersich M, Luchters S. Attitudes and behaviours of maternal health care providers in interactions with clients: a systematic review. Glob Health. (2015) 11:36. doi: 10.1186/s12992-015-0117-9
30. Mselle L, Moland K, Mvungi A, Evjen-Olsen B, Kohi T. Why give birth in health facility? Users’ and providers’ accounts of poor quality of birth care in Tanzania. BMC Health Serv Res. (2013) 13:174. doi: 10.1186/1472-6963-13-174
31. Larson E, Hermosilla S, Kimweri A, Mbaruku G, Kruk M. Determinants of perceived quality of obstetric care in rural Tanzania: a cross-sectional study. BMC Health Serv Res. (2014) 14:483. doi: 10.1186/1472-6963-14-483
32. Rance S, McCourt C, Rayment J, Mackintosh N, Carter W, Watson K, et al. Women’s safety alerts in maternity care: is speaking up enough? BMJ Qual Saf. (2013) 22:348–55. doi: 10.1136/bmjqs-2012-001295
33. Swahnberg K, Schei B, Hilden M, Halmesmäki E, Sidenius K, Steingrimsdottir T, et al. Patients’ experiences of abuse in health care: a Nordic study on prevalence andassociated factors in gynaecological patients. J Psychosom Obstet Gynaecol. (2007) 86:349–56. doi: 10.1080/00016340601185368
34. Moher D, Liberati A, Tetzlaff J, Altman D, The Prisma Group. The preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. (2009) 6:e1000097. doi: 10.1371/journal.pmed.1000097
35. Kassa Z, Husen S. Disrespectful and abusive behavior during childbirth and maternity care in Ethiopia: a systematic review and meta-analysis. BMC Res Notes. (2019) 12:83. doi: 10.1186/s13104-019-4118-2
36. Moola S, Munn Z, Tufanaru C, Aromataris E, Sears K, Sfetcu R, et al. Checklist for analytical cross-sectional studies. Adelaide. (2017) 6:6–23.
37. Hoy D, Brooks P, Woolf A, Blyth F, March L, Bain C, et al. Assessing risk of bias in prevalence studies: modification of an existing tool and evidence of inter-rater agreement. J Clin Epidemiol. (2012) 65:934–9. doi: 10.1016/j.jclinepi.2011.11.014
38. Duval S, Tweedie R. Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. (2000) 56:455–63. doi: 10.1111/j.0006-341X.2000.00455.x
39. Higgins J, Thompson S. Quantifying heterogeneity in a meta-analysis. Stat Med. (2002) 21:1539–58. doi: 10.1002/sim.1186
40. Viechtbauer W. Conducting meta-analyses in R with the metaphor package. J Stat Softw. (2010) 36:1–48. doi: 10.18637/jss.v036.i03
41. Mihret H, Atnafu A, Gebremedhin T, Dellie E. Reducing disrespect and abuse of women during antenatal care and delivery services at Injibara general hospital, Northwest Ethiopia: a pre–post interventional study. Int J Womens Health. (2020) 12:835–47. doi: 10.2147/IJWH.S273468
42. Phillipo P. Assessment of magnitude and factors associated with disrespectful and abusive maternity care during childbirth in health facilities in tabora municipality. Tanzania: Muhimbili University of Health and Allied Sciences. (2016).
43. Siraj A, Teka W, Hebo H. Prevalence of disrespect and abuse during facility based child birth and associated factors, Jimma University Medical Center, Southwest Ethiopia. BMC Pregnancy Childbirth. (2019) 19:185. doi: 10.1186/s12884-019-2332-5
44. Mengistie Zeleke A, Melkie Bayeh G. Maternal disrespect and abuse among mothers who gave childbirth at public health facilities and associated factors in Gondar town, Northwest, Ethiopia. J Midwifery Reprod Health. (2022) 10:3165-3174.
45. Mekonnen A, Fikadu G, Esmeal A. Disrespectful and abusive maternity care during childbirth in Bale zone Public Hospitals, Southeast Ethiopia: cross-sectional study. Clin. Pract. (2019) 16:1273–80. doi: 10.37532/fmcp.2019.16(5).1273-1280
46. Maldie M, Egata G, Chanie M, Muche A, Dewau R, Worku N, et al. Magnitude and associated factors of disrespect and abusive care among laboring mothers at public health facilities in Borena District, South Wollo, Ethiopia. PLoS One. (2021) 16:e0256951. doi: 10.1371/journal.pone.0256951
47. Gebremichael M, Worku A, Medhanyie A, Berhane Y. Mothers’ experience of disrespect and abuse during maternity care in northern Ethiopia. Glob Health Action. (2018) 11:1465215. doi: 10.1080/16549716.2018.1465215
48. Banks K, Karim A, Ratcliffe H, Betemariam W, Langer A. Jeopardizing quality at the frontline of healthcare: prevalence and risk factors for disrespect and abuse during facility-based childbirth in Ethiopia. Health Policy Plan. (2018) 33:317–27. doi: 10.1093/heapol/czx180
49. Makumi, Wango I. Disrespect and abuse of women during facility based Deliveries and its effects on intent to use maternity services in uringu division meru county. Ph.D. thesis. Kenya: University of Nairobi (2015).
50. Wassihun B, Deribe L, Worede N, Gultie T. Prevalence of disrespect and abuse of women during child birth and associated factors in Bahir Dar town, Ethiopia. Epidemiol Health. (2018) 40:e2018029. doi: 10.4178/epih.e2018029
51. Altahir A, Abd Alaal A, Mohammed A, Eltayeb D. Proportion of disrespectful and abusive care during childbirth among women in Khartoum State-2016. Am J. Public Health Rese. (2018) 6:237–42.
52. Ukke G, Gurara M, Boynito W. Disrespect and abuse of women during childbirth in public health facilities in Arba Minch town, south Ethiopia – a cross-sectional study. PLoS One. (2019) 14:e0205545. 0205545 doi: 10.1371/journal.pone.0205545
53. Kebede D, Dachew A, Abota T. Maternal disrespect and abuse by health care providers among postpartum women attending Mizan-Tepi University teaching hospital, south west Ethiopia. medRxiv. [Preprint]. (2022). doi: 10.1101/2022.01.28.22269996
54. Tagesse B, Tamiso A, Rodamo K, Zenebe A. Prevalence and associated factors of disrespectful and abusive care during childbirth among women who gave birth in health facilities in Hawassa city, southern Ethiopia: Ethiop. J. Health Biomed Sci. (2021) 11:67–82. doi: 10.21203/rs.3.rs-107805/v1
55. Negash B, Yoseph A. Status of disrespectful and abusive maternity care among women who delivered in hospitals of Sidama zone, South Ethiopia, in 2019. Res Squ. [Preprint]. (2020). doi: 10.21203/rs.3.rs-49456/v1
56. Tekle Bobo F, Kebebe Kasaye H, Etana B, Woldie M, Feyissa T. Disrespect and abuse during childbirth in Western Ethiopia: should women continue to tolerate? PLoS One. (2019) 14:e0217126. doi: 10.1371/journal.pone.0217126
57. Tunçalp ö, Were W, MacLennan C, Oladapo O, Gülmezoglu A, Bahl R. Quality of care for pregnant women and newborns the WHO vision. BJOG. (2015) 122:1045–91. doi: 10.1111/1471-0528.13451
58. World Health Organization [WHO]. WHO recommendations: intrapartum care for a positive childbirth experience. Geneva: World Health Organization (2018).
59. Abuya T, Waren C, Miller N, Njuki R, Ndwiga C, Maranga A, et al. Exploring the prevalence of disrespect and abuse during childbirth in Kenya. PLoS One. (2015) 10:e0123606. doi: 10.1371/journal.pone.0123606
60. Vo Isola F, Owolabi O, Fjillippi V. Disrespect and abuse of women during childbirth in Nigeria: a systematic review. PLoS One. (2017) 12:e0174084. 0174084 doi: 10.1371/journal.pone.0174084
61. Kassa Z, Tsegaye B, Abeje A. Disrespect and abuse of women during the process of childbirth at health facilities in sub-Saharan Africa: a systematic review and meta-analysis. BMC Int Health Hum Rights. (2020) 20:23. doi: 10.1186/s12914-020-00242-y
62. Thapaliya R, Paudel K, Shrestha S. Disrespect and abuse during facility- based childbirth in Pokhara metropolitan city. JGMC Nepal. (2021) 14:39–44. doi: 10.3126/jgmcn.v14i1.30572
63. Yadav A, Singh T, Sachan S. Prevalence of disrespect and abuse and its determinants during antenatal care services in Rural Uttar Pradesh India. Int J Health Sci Res. (2022) 12:115. doi: 10.52403/ijhsr.20220216
64. Nawab T, Erum U, Amir A, Khalique N, Ansari M, Chauhan A. Disrespect and abuse during facility-based childbirth and its socio-demographic determinants – A barrier to healthcare utilization in rural population. J Family Med Prim Care. (2019) 8:239–45. doi: 10.4103/jfmpc.jfmpc_247_18
65. Hajizadeh K, Vaezi M, Meedya S, Mohammad Alizadeh Charandabi S, Mirghafourvand M. Prevalence and predictors of perceived disrespectful maternity care in postpartum Iranian women: a cross-sectional study. BMC Pregnancy Childbirth. (2020) 20:463. doi: 10.1186/s12884-020-03124-2
66. Hameed W, Avan B. Women’s experiences of mistreatment during childbirth: a comparative view of home-and facility-based births in Pakistan. PLoS One. (2018) 13:e0194601. doi: 10.1371/journal.pone.0194601
67. Azhar Z, Oyebode O, Masud H. Disrespect and abuse during childbirth in district Gujrat, Pakistan: a quest for respectful maternity care. PLoS One. (2018) 13:e0200318. doi: 10.1371/journal.pone.0200318
68. Montesinos-Segura R, Urrunaga-Pastor D, Mendoza-Chuctaya G, Taype- Rondan A, Helguero-Santin L, Martinez-Ninanqui F, et al. Disrespect and abuse during childbirth in fourteen hospitals in nine cities of Peru. Int J Gynecol Obstet. (2018) 140:184–90. doi: 10.1002/ijgo.12353
69. Brenes Monge A, Fernández Elorriaga M, Poblano Verástegui O, Valdez Santiago R, Martínez Nolasco M. Disrespect and abuse in obstetric care in Mexico: an observational study of deliveries in four hospitals. Matern Child Health J. (2021) 25:565–73. doi: 10.1007/s10995-020-03052-9
70. Mesenburg M, Victora C, Serruya S, de León R, Damaso A, Domingues M, et al. Disrespect and abuse of women during the process of childbirth in the 2015 Pelotas birth cohort. Reprod Health. (2018) 15:54. doi: 10.1186/s12978-018-0495-6
71. Afulani P, Diamond-Smith N, Phillips B, Singhal S, Sudhinaraset M. Validation of the person-centered maternity care scale in India. Reprod Health. (2018) 15:147. doi: 10.1186/s12978-018-0591-7
72. Bhattacharya S, Sundari Ravindran T. Silent voices: institutional disrespect and abuse during delivery among women of Varanasi district, Northern India. BMC Pregnancy Childbirth (2018) 18:338. doi: 10.1186/s12884-018-1970-3
73. Freedman L, Ramsey K, Abuya T, Bellows B, Ndwiga C, Warren C, et al. Defining disrespect and abuse of women in childbirth: a research, policy and rights agenda. Bull World Health Organ. (2014) 92:915–7. doi: 10.2471/BLT.14.137869
Keywords: disrespect, abuse, mistreatment, childbirth, meta-analysis, East Africa
Citation: Gebeyehu NA, Adella GA and Tegegne KD (2023) Disrespect and abuse of women during childbirth at health facilities in Eastern Africa: systematic review and meta-analysis. Front. Med. 10:1117116. doi: 10.3389/fmed.2023.1117116
Received: 06 December 2022; Accepted: 03 April 2023;
Published: 20 April 2023.
Edited by:
Zaleha Abdullah Mahdy, National University of Malaysia, MalaysiaReviewed by:
Timothy Abiola Olusesan Oluwasola, University of Ibadan, NigeriaAida Kalok, National University of Malaysia, Malaysia
Copyright © 2023 Gebeyehu, Adella and Tegegne. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Natnael Atnafu Gebeyehu, am9zc3lhdG5hZnUyMDIwQGdtYWlsLmNvbQ==
 Natnael Atnafu Gebeyehu
Natnael Atnafu Gebeyehu Gtachew Asmare Adella
Gtachew Asmare Adella Kirubel Dagnaw Tegegne
Kirubel Dagnaw Tegegne