- 1Department of Chinese Medicine, Chi Mei Medical Center, Tainan, Taiwan
- 2Department of Anesthesiology, Chi Mei Medical Center, Tainan, Taiwan
- 3Department of Neurosurgery, Chi Mei Medical Center, Tainan, Taiwan
- 4Department of Medical Research, Chi Mei Medical Center, Tainan, Taiwan
- 5Department of Recreation and Health-Care Management, College of Recreation and Health Management, Chia Nan University of Pharmacy and Science, Tainan, Taiwan
- 6Department of Anesthesiology, Chi Mei Medical Center, Liouying, Tainan, Taiwan
- 7Department of Emergency Medicine, E-Da Hospital, I-Shou University, Kaohsiung City, Taiwan
- 8School of Medicine for International Students, College of Medicine, I-Shou University, Kaohsiung City, Taiwan
Background: This meta-analysis aimed at investigating the efficacy of acupuncture for pain relief in patients receiving extracorporeal shock wave lithotripsy (ESWL).
Methods: Randomized controlled trials comparing the efficacy of acupuncture with conventional treatments were retrieved from major electronic databases (e.g., MEDLINE, EMBASE, and Cochrane Library) until August 28, 2022. The primary outcome was the response rate (i.e., rate of pain relief), while secondary outcomes included stone-free rate, satisfaction rate, duration of ESWL, peri-/post-procedural pain score, and risk of adverse events.
Results: Thirteen eligible studies involving 1,220 participants published between 1993 and 2022 were analyzed. Pooled results indicated that acupuncture had a better response rate compared to conventional treatments (RR = 1.17, 95% CI: 1.06–1.3, p = 0.003, seven trials, n = 832). Despite no difference in ESWL duration (MD = 0.02 min, 95% CI: −1.53 to 1.57, p = 0.98, three trials, n = 141), stone-free rate (RR = 1.11, 95% CI: 1–1.25, p = 0.06, six trials, n = 498), and satisfaction rate (RR = 1.51, 95% CI: 0.92–2.47, p = 0.1, three trials, n = 334) between the two groups, the acupuncture group had a lower risk of adverse events (RR = 0.51, 95% CI: 0.33–0.79, p = 0.003, five trials, n = 327), peri- (MD = −1.91 points, 94% CI: −3.53 to −0.28, p = 0.02, four trials, n = 258 patient) and post-procedural (MD = −1.07, 95% CI: −1.77 to −0.36, p = 0.003, four trials, n = 335) pain score.
Conclusion: The results of this meta-analysis showed that the use of acupuncture in patients receiving ESWL was associated with a higher pain relief rate and a lower risk of adverse events, suggesting feasibility of its use in this clinical setting.
Systematic review registration: https://www.crd.york.ac.uk/prospero/, identifier: CRD42022356327.
1. Introduction
Urolithiasis, which is one of the most prevalent diseases of the urinary system that affects more than 12% of the global population (1, 2), usually manifests with pain, urinary tract infections, and even hydronephrosis when the ureter is obstructed (3). In contrast to open nephrotomy, minimally invasive strategies such as extracorporeal shock wave lithotripsy (ESWL), ureteroscopic lithotripsy (URSL), percutaneous nephrolithotripsy (PCNL), and retroperitoneal ureterolithotripsy (RPUL) are the mainstream treatments in current clinical practice (3, 4). Extracorporeal shock wave lithotripsy (ESWL), which harnesses high-energy shock waves and pressure for stone fragmentation (5), has been described as an epoch-making therapeutic modality because of its simplicity, noninvasiveness (6), effectiveness, and low morbidity (7) especially for renal stones smaller than 2 cm in diameter or those located at the upper ureter (8). Nevertheless, the higher the energy used in ESWL, the more severe the adverse side-effects (9). Besides, patients may experience pain or anxiety (10) because of hematuria, stones retention and urinary tract infection after the procedure (11).
The sources of pain during ESWL can be two-folded. While somatic pain may be caused by shock waves penetrating through the superficial body structures (i.e., skin and muscle) (12), visceral pain can result from shock waves that reach the deeper structures (e.g., ribs, nerves, and the kidney capsule) (13). Although local anesthetics, non-steroidal anti-inflammatory drugs (NSAIDs), and opioids are the common analgesics being used during ESWL in daily practice (14), no consensus has been reached on the optimal analgesic regimen. Acupuncture has long been used as a mode of analgesia (15) that improves lower urinary tract symptoms (16, 17) through inducing ureteral smooth muscle relaxation (18), thereby achieving renal colic pain relief (19). Previous findings have shown that the use of acupuncture during ESWL could reduce analgesic requirement, alleviate anxiety (20–22), and improve the success rate of the procedure (23). Despite growing evidence in support of acupuncture as an analgesic measure during lithotripsy, the efficacy has not been systematically scrutinized. The aim of the current meta-analysis was to examine the role of acupuncture in lithotripsy through systematically reviewing currently available literature based on a comparison of treatment response rate, change in pain severity, stone-free rate, and satisfaction rate between patients receiving acupuncture and those undergoing other analgesic strategies during ESWL.
2. Methods
The registered protocol for this systematic review and meta-analysis can be accessed at https://www.crd.york.ac.uk/prospero/, number: CRD42022356327. The research was conducted based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Statement (PRISMA) guidelines.
2.1. Information sources and search strategy
Literature search was performed to identify eligible randomized controlled trials (RCTs) investigating the effectiveness of acupuncture for pain relief in patients receiving ESWL. Major databases, namely MEDLINE, Embase, and Cochrane CENTRAL register of controlled trials, were searched from their inception dates till August 28, 2022. The key words and medical subject headings (e.g., MeSH terms in Medline) that were used for searching included: (“extracorporeal shock wave lithotripsy” or “shock wave lithotripsy” or “urolithiasis” or “nephrolithiasis” or “Ureteral calculi”) and (“Acupuncture” or “Electro acupuncture” or “Laser acupuncture” or “Needle acupuncture” or “auricular acupuncture” or “manual acupuncture” or “acupoint injection” or “acupoint treatment”). In addition, we also searched the Google scholar, the China National Knowledge Infrastructure (CNKI) database, VIP Information Database, Chinese Biomedical Literature Database (CBM), and Wanfang Database to avoid omitting potentially eligible studies. The reference lists of the published systematic reviews and all of the included RCTs were also screened to identify relevant studies. We did not place restrictions on language, sample size, publication date, and country of publication. The search strategies for one of these databases (i.e., Medline) is provided in Supplementary Table 1.
2.2. Inclusion and exclusion criteria
Inclusion criteria were: (a) Patient population: Adult participants (≥18 years) receiving ESWL; (b) Intervention: Acupuncture therapies regardless of its location or type; (c) Comparison: Usual care (e.g., NSAIDS, opioids) or sham acupuncture; (d) Outcomes: Total response rate, treatment-related complications, pain score, and other procedure-related outcomes. Exclusion criteria included: (1) studies in which ESWL was not performed; (2) those that did not use acupuncture as the main therapeutic method; and (3) those that combined acupuncture with other conventional interventional strategies (e.g., NSAIDS, opioids).
2.3. Selection process and data collection
Two independent reviewers independently screened the literature for potentially eligible articles in accordance with the inclusion and exclusion criteria. A full text review of the selected trials was conducted to determine their eligibility. Disagreements were resolved through consulting with a third author. As part of the data extraction process, the two independent reviewers carried out separate data extraction processes that involved information pertinent to author information (e.g., first author), characteristics of participants (e.g., gender distribution), sample size, intervention details, drugs for conventional intervention, and country of origin.
2.4. Outcomes and definitions of data items
This study was designed to investigate the response rate, which referred to the percentage of participants experiencing effective pain relief after intervention (i.e., primary outcome). The definition of effective pain relief was based on that of each study. The secondary outcome included stone-free rate, risks of adverse events based on the definition of individual studies regardless of the timing of occurrence, satisfaction rate, duration of ESWL, hemodynamic profile (i.e., systolic and diastolic blood pressure, heart rate) during ESWL, as well as peri- and post-procedural pain score. For the current study, acupuncture encompassed all procedures involving the technique of acupuncture, namely conventional acupuncture, auricular acupuncture, laser acupuncture, electroacupuncture, acupuncture injection, and acupoint electrical stimulation.
2.5. Risks of bias assessment
Two independent reviewers appraised the methodological qualities of each included RCT according to the Cochrane risk-of-bias tool for RCTs (RoB 2.0), which comprises five domains for assessment, namely selection of the reported results, deviations from intended interventions, outcome measurement, randomization process, and missing outcome (24). The RoB categorized the risk in each domain into three categories: low risk, unclear risk, and high risk. Whenever there was a disagreement between the two reviewers, a third reviewer was consulted until consensus was reached.
2.6. Evidence quality assessment
Two independent reviewers evaluated the degree of certainty of the evidence that was categorized into high, moderate, low, and very low through assessing the probability of study limitations, publication bias, effect consistency, imprecision, and indirectness according to GRADE (grading of recommendations assessment, development and evaluation) guidance. All disagreements regarding ratings were resolved through discussion.
2.7. Data analysis
All data analyses were performed with the Review Manager (RevMan) version 5.4.1 software (The Nordic Cochrane Center, The Cochrane Collaboration, Copenhagen, Denmark). Continuous variables that were assessed with the same scale are expressed as mean difference (MD) with a 95% confidence interval (CI), while other data are presented as standardized mean difference (SMD). For a dichotomous variable (i.e., efficacy and complication rate), the effect size is expressed as risk ratio (RR) with 95% confidence interval (CI). Overlapping in sample size assessment in studies with more than two intervention arms was prevented by dividing participants in the control group into separate subgroups to compare with their counterparts in the corresponding specific treatment arm as previously described (25). While the means and SDs were preserved in spite of division of the total number of participants on encountering continuous variables, both the event number and the total number of participants were divided for categorical outcomes. In view of the heterogeneity of the clinical and population parameters involved, the Mantel–Haenszel random effects model was chosen for outcome analysis. The degree of heterogeneity was considered significant when I2 statistics was >50% (26) where a leave-one-out sensitivity analysis was conducted to test robustness of the result. A funnel plot was examined to detect the possibility of publication bias when at least 10 trials were involved. A p-value of < 0.05 was deemed statistically significant. The statistical approach adopted in the present meta-analysis was as previously described (27–29).
3. Results
3.1. Selection, characteristics, and quality of studies
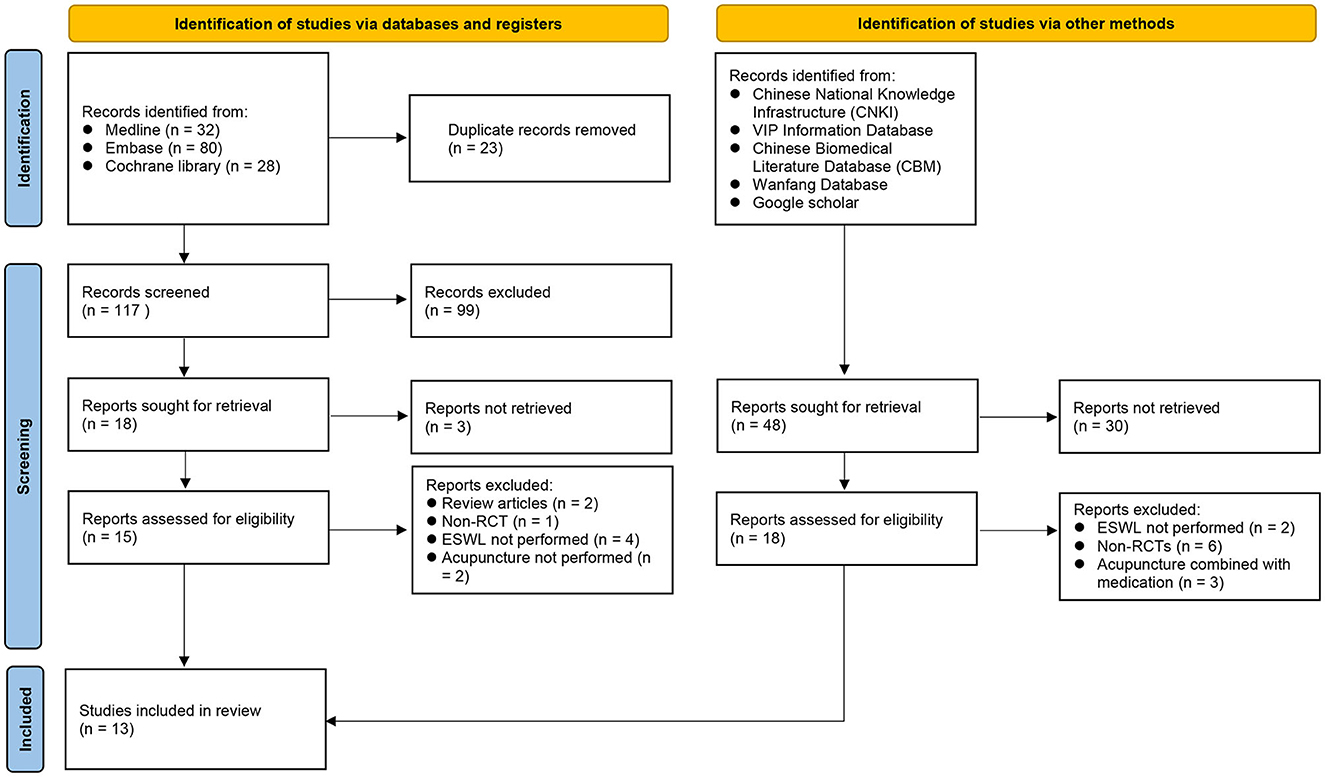
Of the 140 records retrieved from the three main databases, 23 were removed because of duplications. Of the remaining 117 records, 99 were deemed ineligible based on their titles and abstracts. After a further exclusion of nine reports after a full-text screening of the remaining 15 trials, six RCTs were considered eligible for inclusion in the current study (Figure 1). Moreover, seven additional RCTs were identified through the examination of other databases (e., CNKI). In total, 13 RCTs being conducted in China (n = 7) (30–36), Taiwan (n = 1) (23), Iran (n = 1) (37), Turkey (n = 1) (38), Germany (n = 1) (20), Italy (n = 1) (21), and America (n = 1) (22) published from 1993 to 2022 were included.
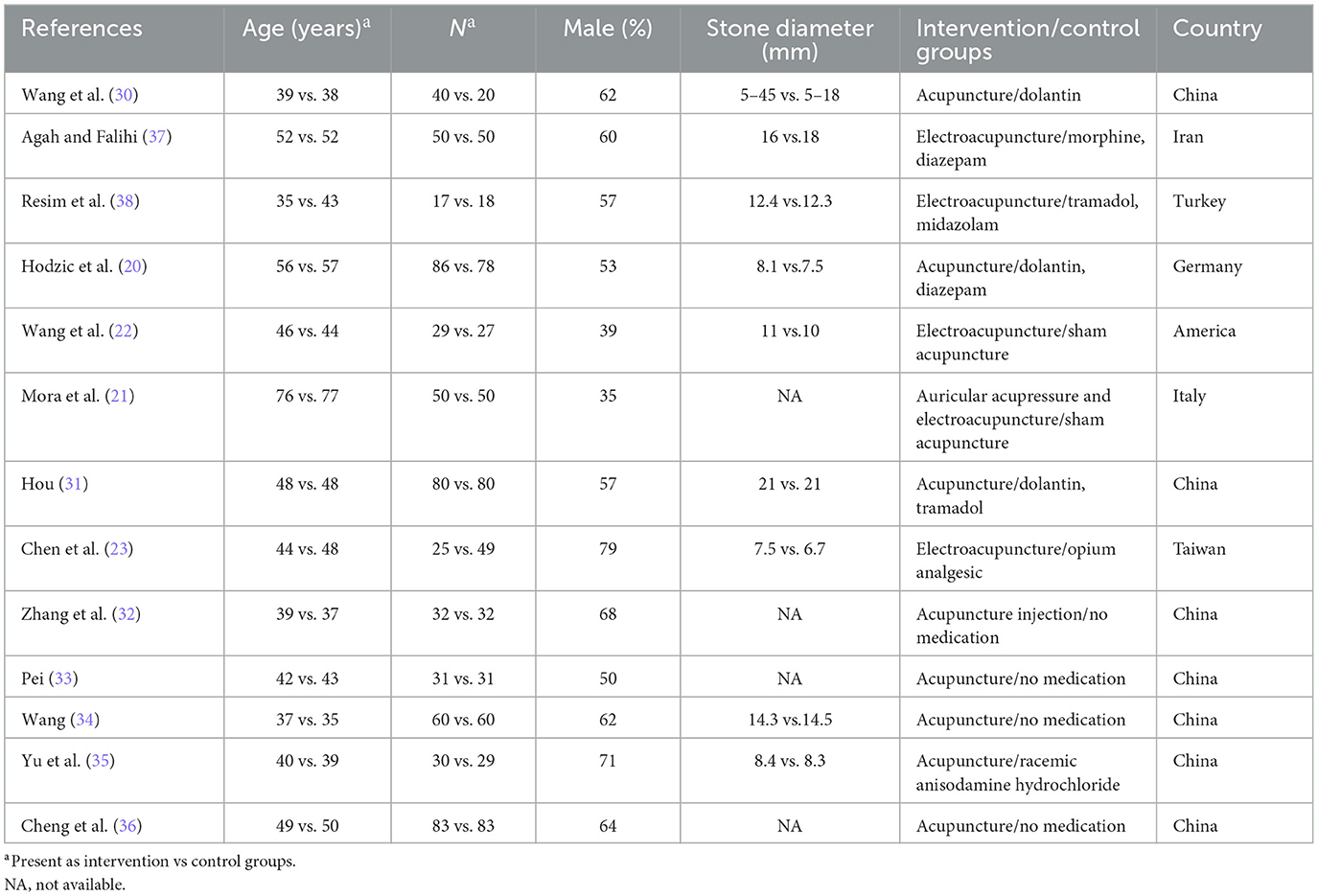
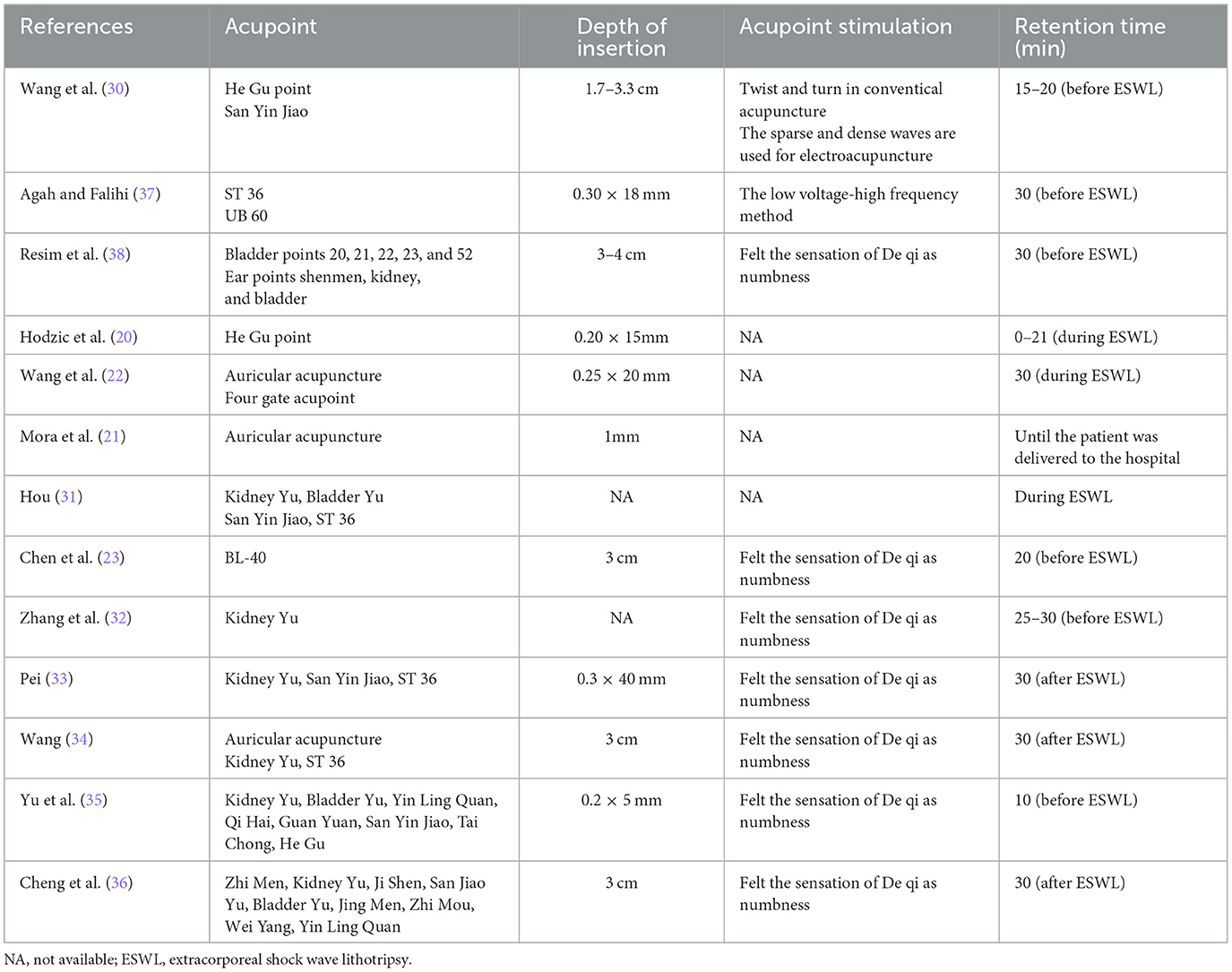
The characteristics of the included studies are summarized in Table 1. The 13 studies included 1,220 patients, of whom 613 were in the acupuncture group, and 607 belonged to the control group. The proportion of male gender ranged from 35 to 79%. The age of participants ranged from 35 to77 years. In the acupuncture group, three types of acupuncture techniques were involved: acupuncture (seven trials) (20, 30, 31, 33–36), electroacupuncture (four trials) (22, 23, 37, 38), electroacupuncture combine with auricular acupressure (one trial) (21), and acupuncture injection (one trial) (32). One study randomized the patients into three groups, namely two intervention groups (i.e., acupuncture and electroacupuncture) and one control group (i.e., dolantin) (30). The details for acupuncture technique are demonstrated in Table 2. In terms of controls, opioids (n = 6) (20, 23, 30, 31, 37, 38), sham acupuncture (n = 2) (21, 22), no intervention (n = 4) (32–34, 36), and racemic anisodamine hydrochloride (n = 1) (35) were adopted.
Of the five studies (23, 30, 33, 34, 38) that reported information about adverse events, only one (30) mentioned three cases of nausea and two cases of palpitations in the acupuncture analgesia group. Two other trials (34) identified poor stone evacuation after ESWL as the underlying cause of adverse complications. Two studies (23, 38) noted that none of the patients receiving acupuncture experienced adverse reactions.
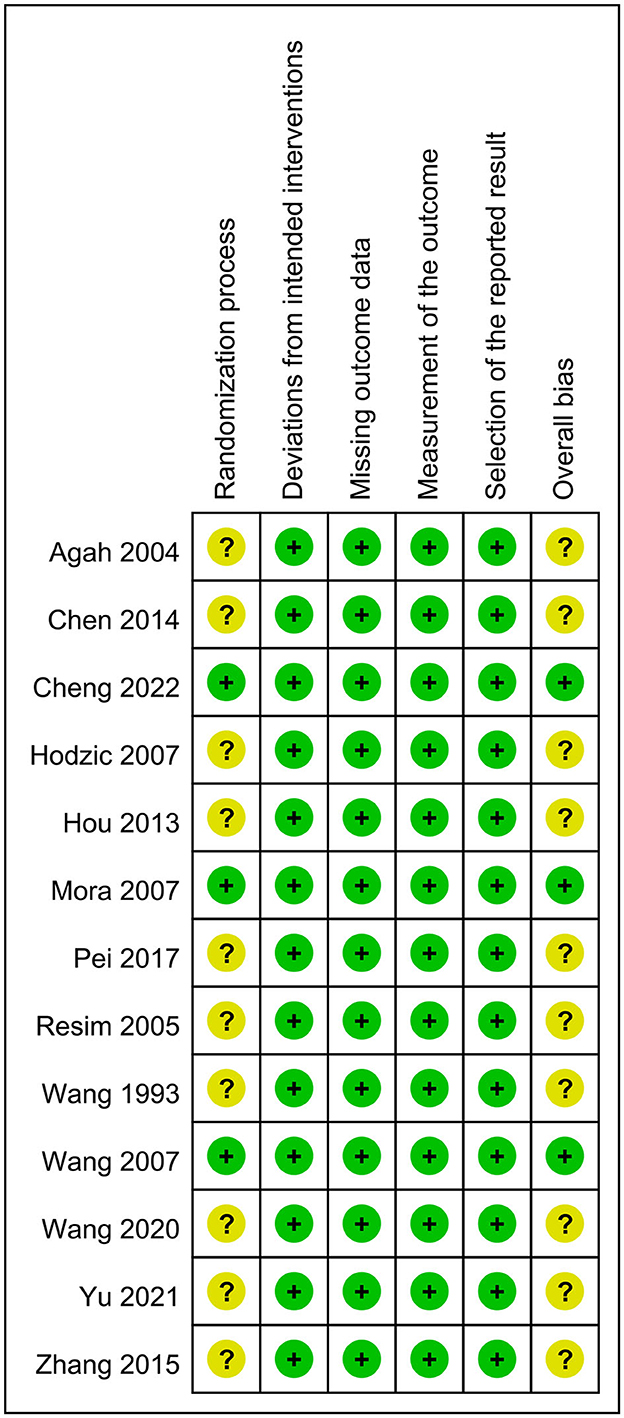
The results of risk of bias assessment are summarized in Figure 2. The rating of “having some concerns” was given to the risk of bias for the randomization process in ten trials that failed to disclose details about allocation sequence concealment. The overall bias was graded as “low” and “having some concerns” in three and 10 studies, respectively.
3.2. Results of syntheses
Regarding the primary outcome, pooled results indicated a better response rate associated with acupuncture compared to usual care (RR = 1.17; 95% CI: 1.06 to 1.3; p = 0.003; I2 = 71%; seven trials, 832 patients; Figure 3) with consistent findings on sensitivity analysis. For secondary outcomes, there was a significantly lower pain score in the acupuncture group than that in the control group (MD = −1.91 points, 94% CI: −3.53 to −0.28, p = 0.02, I2 = 96%, four trials, 258 patients; Figure 4A) with inconsistent findings on sensitivity analysis. Despite no difference in the duration of ESWL in both groups (MD = 0.02 min, 95% CI: −1.53 to 1.57, p = 0.98, I2 = 0, three trials, 141 patients, sensitivity analysis: consistent; Figure 4B), the acupuncture group exhibited a non-significantly higher stone-free rate compared to that in the control group (RR = 1.11, 95% CI: 1–1.25, p = 0.06, I2 = 52%, six trials, 498 patients; Figure 4C). Sensitivity analysis showed a statistically significant higher stone-free rate in the acupuncture group than that in the control group when two studies (30, 38) were removed one at a time. The hemodynamic changes during ESWL in both groups are demonstrated in Figure 5, suggesting no significant difference with or without acupuncture.
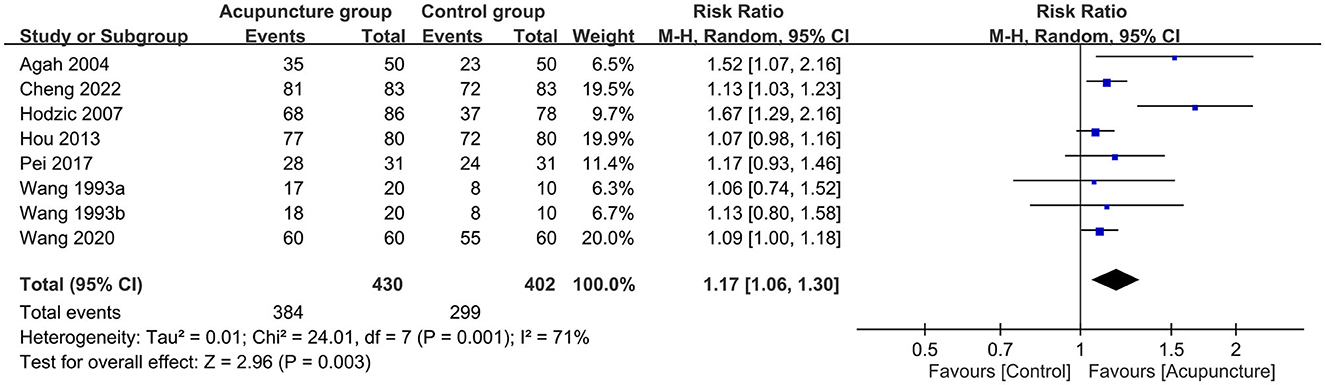
Figure 3. Forest plot comparing response rate between acupuncture and control groups. RR, risk ratio; M-H, Mantel–Haenszel; CI, confidence interval.
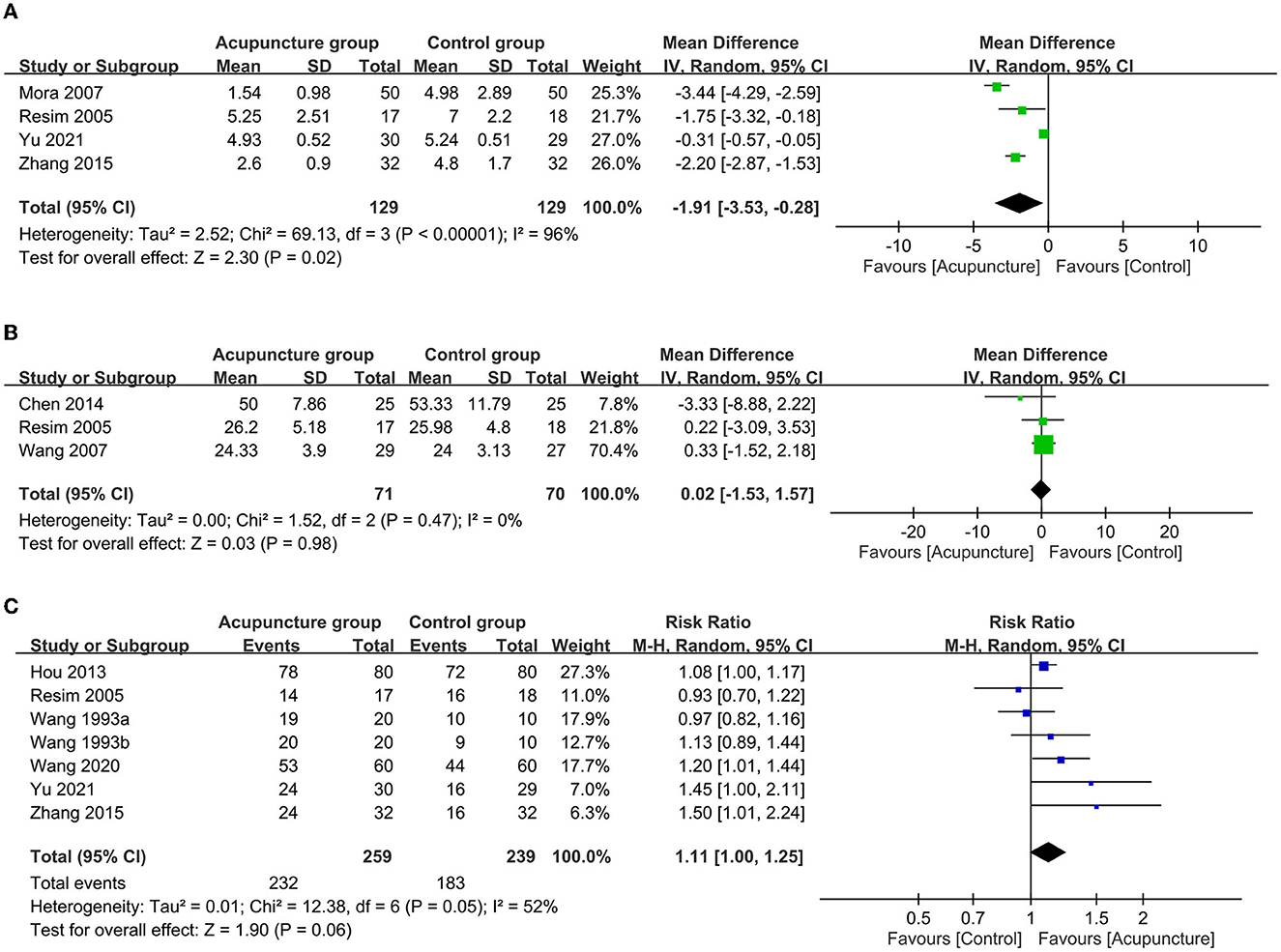
Figure 4. Forest plot comparing the (A) peri-procedural pain score; (B) duration of extracorporeal shock wave lithotripsy (ESWL); and (C) stone-free rate between acupuncture and control groups. CI, confidence interval; IV, inverse variance.
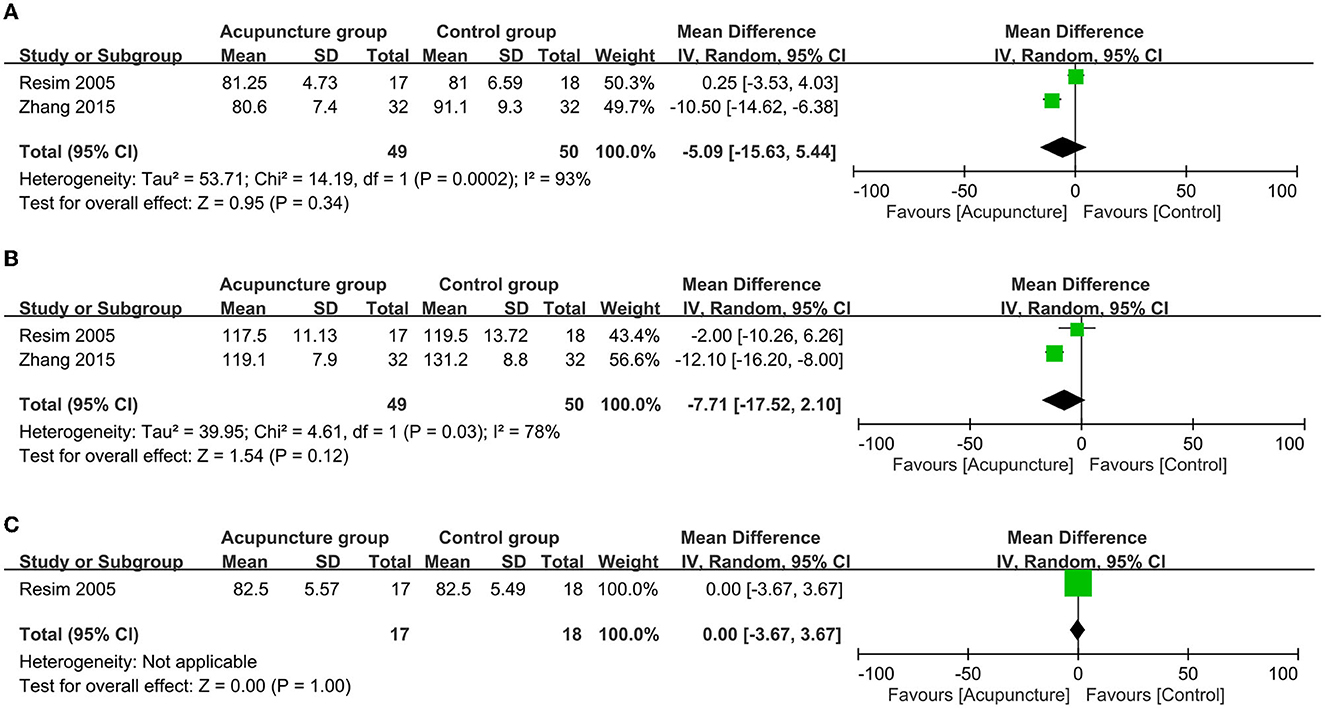
Figure 5. Forest plot comparing the (A) heart rate; (B) systolic blood pressure and (C) diastolic blood pressure during extracorporeal shock wave lithotripsy (ESWL) between acupuncture and control groups. CI, confidence interval; IV, inverse variance.
Following ESWL, the acupuncture group showed a reduced risk of adverse events (RR = 0.51, 95% CI: 0.33 to 0.79, p = 0.003, I2 = 51%; five trials, 327 patients; sensitivity analysis: consistent; Figure 6A) and a lower pain score (MD = −1.07, 95% CI: −1.77 to −0.36, p = 0.003, I2 = 91%; four trials, 335 patients; sensitivity analysis: inconsistent; Figure 6B) compared to those in the control group. There was a non-significantly higher satisfaction rate in patients receiving acupuncture compared to that in those without (RR = 1.51, 95% CI: 0.92 to 2.47, p = 0.1, I2 = 92%, three trials, 334 patients; Figure 6C). Sensitivity analysis revealed a significantly higher satisfaction rate in the acupuncture group compared to the control group when the one study (34) was removed.
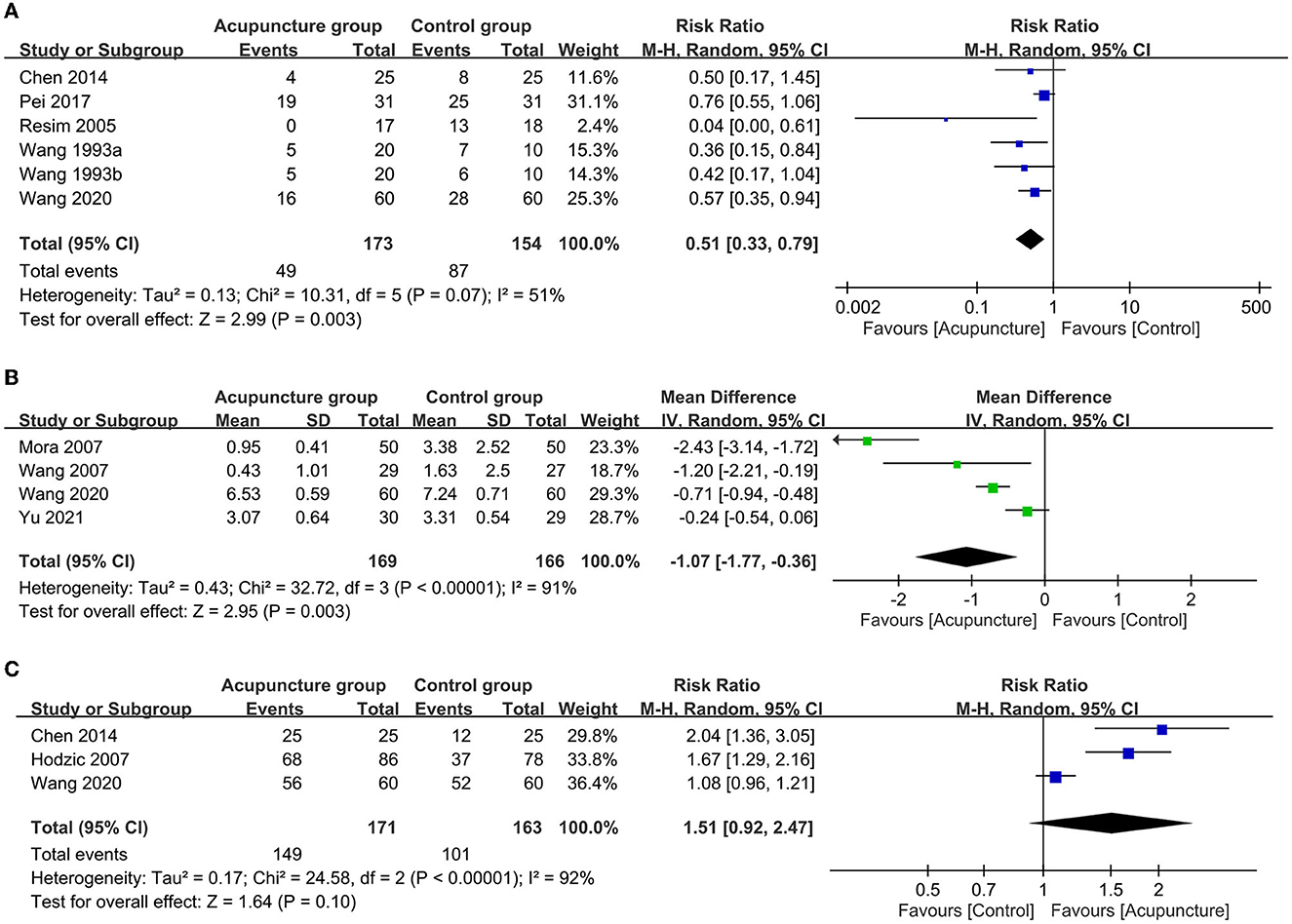
Figure 6. Forest plot comparing the (A) risk of adverse events; (B) post-procedural pain score and (C) satisfaction rate between acupuncture and control groups. RR, risk ratio; M-H, Mantel–Haenszel; CI, confidence interval.
3.3. Certainty of evidence
Analysis of the quality of evidence for outcome measures based on the GRADE system demonstrated a low level of evidence in most outcomes because of downgrading due to a high degree of inconsistency and imprecision, except for diastolic blood pressure, risk of adverse events, and duration of ESWL that were all graded as high (Supplementary Table 2).
4. Discussion
The current meta-analysis demonstrated the effectiveness of acupuncture not only during ESWL as reflected by a higher percentage of participants experiencing effective pain relief and a reduced ESWL-related pain severity compared to those in the controls, but also after the procedure when a lower postoperative pain score and a higher stone-free rate were noted despite a lack of significant difference compared to the control group in the latter. Although there was no difference in the duration of ESWL and hemodynamic changes between the two groups, our results showed a lower risk of adverse events associated with the acupuncture approach and a non-significantly higher satisfaction rate in patients who received acupuncture.
Despite the established role of extracorporeal shock wave lithotripsy (ESWL) as an effective therapeutic approach to lithotripsy, sedation and analgesics measures are required to alleviate the considerable pain triggered by the energy dissipated as the electrical (magnetic) shock waves penetrate different tissue densities of the body (6). For pain relief in this setting, previous studies have reported the use of opiate analgesics (39), patient-controlled analgesia (PCA) (40), general anesthesia (41), epidural injection (42), local anesthesia (43), and oral analgesics. Nevertheless, drug addiction and other side effects related to conventional analgesics such as dizziness, somnolence, respiratory depression, nausea, vomiting (44), and even delayed hospital discharge (45, 46) remain an important clinical concern. In contrast to medication-induced analgesia, previous studies have explored the analgesic efficacy of the other means such as acupuncture-assisted anesthesia (AAA) (47) (including electroacupuncture, auricular acupuncture, acupuncture point injection and acupressure), transcutaneous electrical nerve stimulation (TENS) (48), massage (49), relaxation therapy, hypnosis, aromatherapy, music, and audiovisual distraction (50). One recent large-scale systematic review including 23 RCTs and 2,439 participants evaluated the efficacy of complementary therapies (i.e., music, acupuncture, acupressure, TENS, and audiovisual transfer) for pain relief in patients receiving ESWL (51). Although that study also systematically reviewed five RCTs focusing on acupuncture and related techniques in patients undergoing ESWL and described their efficacy for reducing pain score and anxiety in this patient population (51), no pooled evidence was generated to support their findings. The analgesic efficacy of acupuncture was also demonstrated in previous studies that showed a decrease in sedative and painkiller requirements during lithotripsy associated with the application of acupuncture (21, 22).
The main finding of the current meta-analysis was the analgesic efficacy of acupuncture as demonstrated by a higher percentage of participants achieving effective pain relief and a reduced ESWL-related pain severity compared to those in the control groups. Consistent with our findings, other systematic reviews have supported the promising outcomes of conventional acupuncture and related methods (e.g., auricular acupuncture, electroacupuncture, or acupoint electrical stimulation) in postoperative pain management (52) among patients undergoing back surgery (53), cardiac surgery (54), total knee replacement (55), and laparoscopic surgery (56). Therefore, our results suggested that acupuncture may be an effective analgesic strategy for patients receiving ESWL.
This study presented a significantly lower pain score in the acupuncture group than that in the control group (MD = −1.91 points, 94% CI: −3.53 to −0.28). Five of the included studies used electroacupuncture for pain relief. The analgesic mechanism of electroacupuncture may be attributed to the activation of different endogenous opioid peptides and their receptors through different frequencies of electroacupuncture stimulation (57). A previous experimental study suggested that the analgesic effect of low frequency (2 Hz) electroacupuncture stimulation in the rat spinal cord may be mediated by met-enkephalin and dynorphin acting simultaneously on the μ-, δ-, and κ-receptors, while that of high frequency (l00 Hz) electroacupuncture stimulation is mediated by dynorphin acting on the κ-receptor (58). It has been proposed that the release of opioid substances may produce an endogenous enkephalin-like inhibition on the projection neuron in the dorsal horn, which in turn suppresses the transmission of nociception (59).
Postoperative discomfort experienced during ESWL originates from superficial and deep somatic pain as well as visceral pain. For pain relief, previous studies have suggested the use of topical anesthetic creams such as EMLA (6), which can penetrate the skin to a depth of 4 mm. However, the analgesic effect of topical anesthetics did not reduce the need for analgesia as shown in previous RCT (60) and meta-analysis (61). The result may be explained by the inadequacy of topical anesthesia to alleviate both deep somatic pain and visceral pain (62). In contrast, previous review articles (14, 63) and meta-analysis (43) have demonstrated an effective pain relief in patients undergoing ESWL despite a similar depth of skin manipulation, suggesting the involvement of other analgesic mechanisms. The current study incorporated six conventional acupuncture studies (20, 30, 31, 33–36). Compared to other acupuncture-related techniques, conventional acupuncture induces a characteristic “grabbing needle” biomechanics known as the “de qi” reaction (64, 65). So far, de qi has been proven crucial to the effectiveness of acupuncture anesthesia (66, 67). The stronger the gripping force, the more it enhances the antinociceptive activity (68). It partially supports the theory that mechanical signals are transmitted through the connective tissue during manipulation.
For the current meta-analysis, the definition of adverse events was according to that of individual studies. Among the 13 included studies, five including six datasets provided information about the definitions and incidence of adverse events (Figure 6A) that included nausea/vomiting (23, 30, 38), dizziness (23, 30, 38), palpitation (30), orthostatic hypotension (38), renal colic (30, 33, 34), and gross hematuria (33). Of the six datasets, four adopted opioids (23, 30, 38) and two used no medication (33, 34) in their control groups. Although opioids have been shown to be effective against ESWL-related pain (69), opioid-derived analgesics are known to be associated with side effects such as nausea, vomiting, dizziness, and pruritus (70, 71). Therefore, our pooled result showing a lower risk of adverse events in the acupuncture group than that in the controls was consistent with the reported risks of adverse events associated with opioid use. Moreover, the description of a higher incidence of recurrent renal colic as the major adverse event among the recruited individuals in the two studies that enrolled control subjects with no medication (33, 34) may further imply the efficacy of acupuncture for pain relief in patients receiving ESWL.
Our study had some limitations. First, because only a small number of the included studies recruited patients undergoing sham acupuncture or sham site electrical stimulation as controls, the mechanism underlying the observed acupuncture-related analgesic effect (e.g., “de qi”) could not be elucidated. Second, insufficient information about allocation concealment as well as randomization methods and blinding in the majority of studies (i.e., eight out of 13) may have affected our results. Third, the relatively small sample size of the included studies, inconsistent interventions, different sites of intervention, and variations in study design, duration of treatment, and lithotripters were all sources of heterogeneity that may obscure the significance of our findings. Fourth, of the 48 potentially eligible articles initially retrieved, up to 30 that were included in the CNKI database could not be read in full text because of the early date of publication, illegible text from poor quality of scanning, as well as publication as posters or abstracts. As a result, those questionable articles were excluded to preserve the quality of the present study. Finally, variations in disease-related inclusion criteria (i.e., site, size, shape, hardness, and severity of obstruction) may contribute to biases in outcome interpretation. More high-quality RCTs are warranted to address these issues.
In conclusion, the results of the current meta-analysis and systematic review supported the efficacy of conventional acupuncture and related techniques for pain relief during and after ESWL. The procedures were also associated with a reduced risk of adverse events despite the lack of significant beneficial effects on stone-free rate, and patient satisfaction. Further large-scale clinical studies are required to verify our findings.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
Author contributions
Conceptualization and literature search: H-TC, I-WC, and C-KS. Methodology: Y-CH and I-WC. Trial selection: J-RK and K-CH. Data analysis: K-CH. Data extraction and writing—original draft preparation: H-TC and K-CH. Writing—review and editing: H-TC, K-CH, and C-KS. All authors have read and agreed to the published version of the manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2023.1114485/full#supplementary-material
References
1. Sorokin I, Mamoulakis C, Miyazawa K, Rodgers A, Talati J, Lotan Y. Epidemiology of stone disease across the world. World J Urol. (2017) 35:1301–20. doi: 10.1007/s00345-017-2008-6
2. Brener ZZ, Winchester JF, Salman H, Bergman M. Nephrolithiasis: evaluation and management. South Med J. (2011) 104:133–9. doi: 10.1097/SMJ.0b013e318206f6bd
3. Yasui T, Okada A, Hamamoto S, Taguchi K, Ando R, Mizuno K, et al. Efficacy of retroperitoneal laparoscopic ureterolithotomy for the treatment of large proximal ureteric stones and its impact on renal function. Springerplus. (2013) 2:600. doi: 10.1186/2193-1801-2-600
4. Bozkurt IH, Yonguc T, Arslan B, Degirmenci T, Gunlusoy B, Aydogdu O, et al. Minimally invasive surgical treatment for large impacted upper ureteral stones: ureteroscopic lithotripsy or percutaneous nephrolithotomy? Can Urol Assoc J. (2015) 9:E122–5. doi: 10.5489/cuaj.2280
5. Moon KB, Lim GS, Hwang JS, Lim CH, Lee JW, Son JH, et al. Optimal shock wave rate for shock wave lithotripsy in urolithiasis treatment: a prospective randomized study. Korean J Urol. (2012) 53:790–4. doi: 10.4111/kju.2012.53.11.790
6. Gupta NP, Kumar A. Analgesia for pain control during extracorporeal shock wave lithotripsy: current status. Indian J Urol. (2008) 24:155–8. doi: 10.4103/0970-1591.40607
7. Qiang YC, Guo YG, Wang YQ. The effectiveness and safety of extracorporeal shock wave lithotripsy for the management of kidney stones: a protocol of systematic review and meta-analysis. Medicine. (2020) 99:e19915. doi: 10.1097/MD.0000000000019915
8. Nielsen TK, Jensen JB. Efficacy of commercialised extracorporeal shock wave lithotripsy service: a review of 589 renal stones. BMC Urol. (2017) 17:59. doi: 10.1186/s12894-017-0249-8
9. McAteer JA, Evan AP. The acute and long-term adverse effects of shock wave lithotripsy. Semin Nephrol. (2008) 28:200–13. doi: 10.1016/j.semnephrol.2008.01.003
10. Ortiz CT, Blanco LLR, Vicente FD, Satué CG, Pérez LMM, Herrera ET, et al. [Extracorporeal shock-wave lithotripsy: anxiety and pain perception]. Actas Urol Esp. (2000) 24:163–8. doi: 10.1016/S0210-4806(00)72423-5
11. Dobrowiecka K, Przekora J, Jobs K, Kowalczyk K, Plewka K, Paturej A, et al. Early complications of extracorporeal shockwave lithotripsy in the records of the Department of Paediatrics, Nephrology and Allergology of the Military Institute of Medicine - preliminary results. Dev Period Med. (2018) 22:260–4. doi: 10.34763/devperiodmed.20182203.260264
12. Bovelander E, Weltings S, Rad M, van Kampen P, Pelger RCM, Roshani H. The influence of pain on the outcome of extracorporeal shockwave lithotripsy. Curr Urol. (2019) 12:81–7. doi: 10.1159/000489424
13. Williams CM, Kaude JV, Newman RC, Peterson JC, Thomas WC. Extracorporeal shock-wave lithotripsy: long-term complications. AJR Am J Roentgenol. (1988) 150:311–5. doi: 10.2214/ajr.150.2.311
14. Bach C, Zaman F, Kachrilas S, Kumar P, Buchholz N, Masood J. Drugs for pain management in shock wave lithotripsy. Pain Res Treat. (2011) 2011:259426. doi: 10.1155/2011/259426
15. Hao JJ, Mittelman M. Acupuncture: past, present, and future. Glob Adv Health Med. (2014) 3:6–8. doi: 10.7453/gahmj.2014.042
16. Kim J-I, Choi T-Y, Jun JH, Kang H, Lee MS. Acupuncture for management of lower urinary tract symptoms in Parkinson's disease: a protocol for the systematic review of randomized controlled trials. Medicine. (2018) 97:e9821. doi: 10.1097/MD.0000000000009821
17. Lee H-Y, Bae G-E, Lee S-D, Nam J-K, Yun Y-J, Han J-Y, et al. Moxibustion as an adjunct for lower urinary tract symptoms associated with benign prostate enlargement: a randomized controlled pilot trial. Medicine. (2020) 99:e18918. doi: 10.1097/MD.0000000000018918
18. Tu J-F, Cao Y, Wang L-Q, Shi G-X, Jia L-C, Liu B-L, et al. Effect of adjunctive acupuncture on pain relief among emergency department patients with acute renal colic due to urolithiasis: a randomized clinical trial. JAMA Netw Open. (2022) 5:e2225735. doi: 10.1001/jamanetworkopen.2022.25735
19. Cao Y, Tu J-F, Shi G-X, Wang L-Q, Jia L-C, Li B, et al. Acupuncture as adjunctive therapy for acute renal colic caused by urinary calculi: study protocol for a randomized controlled trial. Trials. (2021) 22:652. doi: 10.1186/s13063-021-05600-2
20. Hodzic J, Golka K, Selinski S, Pourvali H, Sommerfeld H-J. [Analgesia with acupuncture in extracorporeal shock wave lithotripsy of kidney stones–first results]. Urologe A. (2007) 46:740, 742–4, 746–7. doi: 10.1007/s00120-007-1362-1
21. Mora B, Iannuzzi M, Lang T, Steinlechner B, Barker R, Dobrovits M, et al. Auricular acupressure as a treatment for anxiety before extracorporeal shock wave lithotripsy in the elderly. J Urol. (2007) 178:160–4; 164. doi: 10.1016/j.juro.2007.03.019
22. Wang S-M, Punjala M, Weiss D, Anderson K, Kain ZN. Acupuncture as an adjunct for sedation during lithotripsy. J Altern Complement Med. (2007) 13:241–6. doi: 10.1089/acm.2006.6262
23. Chen W-T, Chang F-C, Chen Y-H, Lin J-G. An evaluation of electroacupuncture at the weizhong acupoint (BL-40) as a means of relieving pain induced by extracorporeal shock wave lithotripsy. Evid Based Complement Alternat Med. (2014) 2014:592319. doi: 10.1155/2014/592319
24. Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. (2019) 366:l4898. doi: 10.1136/bmj.l4898
25. Chang C-C, Yen W-T, Lin Y-T, Wang L-K, Hung K-C, Wu Z-F, et al. Perioperative pregabalin for preventive analgesia in breast cancer surgery: a meta-analysis of randomized controlled trials. Clin J Pain. (2020) 36:968–77. doi: 10.1097/AJP.0000000000000883
26. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. (2003) 327:557–60. doi: 10.1136/bmj.327.7414.557
27. Hung K-C, Yew M, Lin Y-T, Chen J-Y, Wang L-K, Chang Y-J, et al. Impact of intravenous and topical lidocaine on clinical outcomes in patients receiving propofol for gastrointestinal endoscopic procedures: a meta-analysis of randomised controlled trials. Br J Anaesth. (2022) 128:644–54. doi: 10.1016/j.bja.2021.08.036
28. Hung KC, Chang YJ, Chen IW, Soong TC, Ho CN, Hsing CH, Chu CC, Chen JY, Sun CK. Efficacy of high flow nasal oxygenation against hypoxemia in sedated patients receiving gastrointestinal endoscopic procedures: a systematic review and meta-analysis. J Clin Anesth. (2022) 77:110651. doi: 10.1016/j.jclinane.2022.110651
29. Hung K-C, Chang Y-J, Chen I-W, Lin C-M, Liao S-W, Chin J-C, et al. Comparison of video-stylet and video-laryngoscope for endotracheal intubation in adults with cervical neck immobilisation: a meta-analysis of randomised controlled trials. Anaesth Crit Care Pain Med. (2021) 40:100965. doi: 10.1016/j.accpm.2021.100965
30. Wang S-j, Zhang S-Y, Feng S-P, Li F-Z, Ma J-G, Sun L-H, et al. [Acupuncture anaesthesia in treating urinary tract stone with extracorporeal shock wave lithotripsy]. World J Acupuncture-Moxibust. (1993) 14:34–6.
31. Hou B-D. [Extracorporeal lithotripsy combined with acupuncture to relieve pain and promote urinary calculi in 80 cases]. Chin Med Mod Dist Educ China. (2013) 11:55–55.
32. Zhang S-H, Zhao Z-X, Li X, Wand J, Su X-J. [Impacts of the injection with flurphen mixture at Shenshu(BL 23)on hemodynamics and analgesia in patients with extracorporeal shock wave lithotripsy]. Chinese Acupunct Moxibust. (2015) 35:233–6.
33. Pei J-W. [Effect of acupuncture plus massotherapy on post-lithotripsy stone discharging in urinary stone patients]. Shanghai J Acupunct Moxibust. (2017) 36:825–7.
34. Wang J-N. [An analysis of curative effect of chinese medicine special nursing measures combined with conventional interventions in treating patients with urinary calculi after extracorporeal shock wave lithotripsy]. J New Chinese Med. (2020) 52:145–8.
35. Yu W-X, Pei X-H, Sun Ning Y, Li-Jie YY, Zhou G-J. [Study on the clinical efficacy of sacral acupuncture combined with extracorporeal shock wave lithotripsy in the treatment of lower ureteral calculi]. World J Integrat Trad West Med. (2021) 16:715–8.
36. Cheng Q-q, Cai K, Wang L-p, Fen Q, Hamu RJM. [A clinical study of extracorporeal shock wave lithotripsy (ESWL) combined with acupuncture therapy for pain relief and stone removal in urinary tract stones]. Xinjiang J Trad Chinese Med. (2022) 40:27–29.
37. Agah M, Falihi A. The efficacy of acupuncture in extracorporeal shock wave lithotripsy. Urol J. (2004) 1:195–9.
38. Resim S, Gumusalan Y, Ekerbicer HC, Sahin MA, Sahinkanat T. Effectiveness of electro-acupuncture compared to sedo-analgesics in relieving pain during shockwave lithotripsy. Urol Res. (2005) 33:285–90. doi: 10.1007/s00240-005-0473-7
39. Plutchok JJ, Kortis HI, Amory DW, Wagner BK. Use of a continuous alfentanil infusion for extracorporeal shock wave lithotripsy in the treatment of renal calculi. J Stone Dis. (1992) 4:235–42.
40. Tokumine J, Iha H, Okuda Y, Shimabukuro T, Shimabukuro T, Ishigaki K, et al. Appropriate method of administration of propofol, fentanyl, and ketamine for patient-controlled sedation and analgesia during extracorporeal shock-wave lithotripsy. J Anesth. (2000) 14:68–72. doi: 10.1007/s005400050069
41. Daly KM, Chaker K, Rhouma SB, Chehida MAB, Ouanes Y, Sellami A, et al. [Evaluation of protocols on the use of analgesics for pain management in patients with extracorporeal shock wave lithotripsy (ESWL)]. Pan Afr Med J. (2019) 32:109. doi: 10.11604/pamj.2019.32.109.18211
42. Zhu H, Xiao X, Chen X, Feng G, Zhang Q, Wang H, et al. Ureteroscopic treatment of urological calculi under sacral block anesthesia. Urol Res. (2012) 40:361–3. doi: 10.1007/s00240-011-0417-3
43. Laksita TB, Soebadi MA, Wirjopranoto S, Hidayatullah F, Kloping YP, Rizaldi F. Local anesthetics versus systemic analgesics for reducing pain during Extracorporeal Shock Wave Lithotripsy (ESWL): a systematic review and meta-analysis. Turk J Urol. (2021) 47:270–8. doi: 10.5152/tju.2021.21143
44. Waelkens P Alsabbagh E Sauter A Joshi GP Beloeil H PROSPECT PROSPECT Working group** of the European Society of Regional Anaesthesia and Pain therapy (ESRA). Pain management after complex spine surgery: a systematic review and procedure-specific postoperative pain management recommendations. Eur J Anaesthesiol. (2021) 38:985–94. doi: 10.1097/EJA.0000000000001448
45. Hutchison RW. Challenges in acute post-operative pain management. Am J Health Syst Pharm. (2007) 64(6 Suppl 4):S2–5. doi: 10.2146/ajhp060679
46. Rawal N. Analgesia for day-case surgery. Br J Anaesth. (2001) 87:73–87. doi: 10.1093/bja/87.1.73
47. Sun Y, Gan TJ, Dubose JW, Habib AS. Acupuncture and related techniques for postoperative pain: a systematic review of randomized controlled trials. Br J Anaesth. (2008) 101:151–60. doi: 10.1093/bja/aen146
48. Kararmaz A, Kaya S, Karaman H, Turhanoglu S. Effect of the frequency of transcutaneous electrical nerve stimulation on analgesia during extracorporeal shock wave lithotripsy. Urol Res. (2004) 32:411–5. doi: 10.1007/s00240-004-0438-2
49. Koşar A, Oztürk A, Serel TA, Akkuş S, Unal OS. Effect of vibration massage therapy after extracorporeal shockwave lithotripsy in patients with lower caliceal stones. J Endourol. (1999) 13:705–7. doi: 10.1089/end.1999.13.705
50. Cift A, Benlioglu C. Effect of different musical types on patient's relaxation, anxiety and pain perception during shock wave lithotripsy: a randomized controlled study. Urol J. (2020) 17:19–23.
51. Saraogi M, Geraghty RM, Hameed B, Rob S, Pietropaolo A, Sarica K, et al. Role of complementary medicine (music, acupuncture, acupressure, TENS and audio-visual distraction) in shockwave lithotripsy (SWL): a systematic review from EAU Sections of Urolithiasis (EULIS) and Uro-Technology (ESUT). Urology. (2020) 145:38–51. doi: 10.1016/j.urology.2020.06.035
52. Wu M-S, Chen K-H, Chen I-F, Huang SK, Tzeng P-C, Yeh M-L, et al. The Efficacy of acupuncture in post-operative pain management: a systematic review and meta-analysis. PLoS ONE. (2016) 11:e0150367. doi: 10.1371/journal.pone.0150367
53. Cho Y-H, Kim C-K, Heo K-H, Lee MS, Ha I-H, Son DW, et al. Acupuncture for acute postoperative pain after back surgery: a systematic review and meta-analysis of randomized controlled trials. Pain Pract. (2015) 15:279–91. doi: 10.1111/papr.12208
54. Liu X-L, Tan J-Y, Molassiotis A, Suen LKP, Shi Y. Acupuncture-point stimulation for postoperative pain control: a systematic review and meta-analysis of randomized controlled trials. Evid Based Complement Alternat Med. (2015) 2015:657809. doi: 10.1155/2015/657809
55. Ko HF, Chen C-H, Dong K-R, Wu H-C. Effects of acupuncture on postoperative pain after total knee replacement: systematic literature review and meta-analysis. Pain Med. (2021) 22:2117–27. doi: 10.1093/pm/pnab201
56. Zhao D-Q, Qian G-Y, Jin J, Yao Y-P, Bian X-M, Zhang W-P. Acupuncture therapy strategy options in postoperative management after laparoscopic cholecystectomy: a protocol for systematic review and Bayesian meta-analysis. Medicine. (2021) 100:e24199. doi: 10.1097/MD.0000000000024199
57. Han JS. Acupuncture: neuropeptide release produced by electrical stimulation of different frequencies. Trends Neurosci. (2003) 26:17–22. doi: 10.1016/S0166-2236(02)00006-1
58. Chen XH, Han JS. Analgesia induced by electroacupuncture of different frequencies is mediated by different types of opioid receptors: another cross-tolerance study. Behav Brain Res. (1992) 47:143–9. doi: 10.1016/S0166-4328(05)80120-2
59. Han JS. Acupuncture analgesia: areas of consensus and controversy. Pain. (2011) 152:S41–8. doi: 10.1016/j.pain.2010.10.012
60. Tiselius HG. Cutaneous anesthesia with lidocaine-prilocaine cream: a useful adjunct during shock wave lithotripsy with analgesic sedation. J Urol. (1993) 149:8–11. doi: 10.1016/S0022-5347(17)35983-9
61. Wang Z, Chen G, Wang J, Wei W. Eutectic mixture of local anaesthetics for pain reduction during extracorporeal shockwave lithotripsy: a systematic review and meta-analysis. PLoS ONE. (2020) 15:e0237783. doi: 10.1371/journal.pone.0237783
62. Leung CC, Chan YM, Ngai SW, Ng KF, Tsui SL. Effect of pre-incision skin infiltration on post-hysterectomy pain–a double-blind randomized controlled trial. Anaesth Intensive Care. (2000) 28:510–6. doi: 10.1177/0310057X0002800504
63. Chaussy CG, Tiselius HG. How can and should we optimize extracorporeal shockwave lithotripsy? Urolithiasis. (2018) 46:3–17. doi: 10.1007/s00240-017-1020-z
64. Langevin HM, Churchill DL, Fox JR, Badger GJ, Garra BS, Krag MH. Biomechanical response to acupuncture needling in humans. J Appl Physiol. (2001) 91:2471–8. doi: 10.1152/jappl.2001.91.6.2471
65. Yang X-Y, Shi G-X, Li Q-Q, Zhang Z-H, Xu Q, Liu C-Z. Characterization of deqi sensation and acupuncture effect. Evid Based Complement Alternat Med. (2013) 2013:319734. doi: 10.1155/2013/319734
66. Acar HV. Acupuncture and related techniques during perioperative period: a literature review. Complement Ther Med. (2016) 29:48–55. doi: 10.1016/j.ctim.2016.09.013
67. Kong J, Gollub R, Huang T, Polich G, Napadow V, Hui K, et al. Acupuncture de qi, from qualitative history to quantitative measurement. J Altern Complement Med. (2007) 13:1059–70. doi: 10.1089/acm.2007.0524
68. Hsu C-Y, Lee K-H, Huang H-C, Chang Z-Y, Chen H-Y, Yang T-H. Manipulation therapy relieved pain more rapidly than acupuncture among lateral epicondylalgia (tennis elbow) patients: a randomized controlled trial with 8-week follow-up. Evid Based Complement Alternat Med. (2016) 2016:3079247. doi: 10.1155/2016/3079247
69. Aboumarzouk OM, Hasan R, Tasleem A, Mariappan M, Hutton R, Fitzpatrick J, et al. Analgesia for patients undergoing shockwave lithotripsy for urinary stones - a systematic review and meta-analysis. Int Braz J Urol. (2017) 43:394–406. doi: 10.1590/s1677-5538.ibju.2016.0078
70. Issa MM, El-Galley R, McNamara DE, Segall S. Analgesia during extracorporeal shock wave lithotripsy using the Medstone STS lithotriptor: a randomized prospective study. Urology. (1999) 54:625–8. doi: 10.1016/S0090-4295(99)00231-9
Keywords: acupuncture, extracorporeal shock wave lithotripsy, meta-analysis, pain, urolithiasis
Citation: Chen H-T, Hung K-C, Hsu Y-C, Kuo J-R, Chang Y-J, Chen I-W and Sun C-K (2023) Efficacy of acupuncture for pain relief in patients receiving extracorporeal shock wave lithotripsy: a meta-analysis of randomized controlled studies. Front. Med. 10:1114485. doi: 10.3389/fmed.2023.1114485
Received: 02 December 2022; Accepted: 15 May 2023;
Published: 02 June 2023.
Edited by:
Haoran Liu, Stanford University, United StatesReviewed by:
Yiloren Tanidir, Marmara University, TürkiyeBrent Wagner, United States Department of Veterans Affairs, United States
Copyright © 2023 Chen, Hung, Hsu, Kuo, Chang, Chen and Sun. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Cheuk-Kwan Sun, cmVzZWFyY2hnYXRlMDAwQGdtYWlsLmNvbQ==; I-Wen Chen, bWF2aXNpbmdAZ21haWwuY29t
†These authors have contributed equally to this work and share first authorship
‡These authors have contributed equally to this work
 Hsiao-Tien Chen
Hsiao-Tien Chen Kuo-Chuan Hung
Kuo-Chuan Hung Yao-Chin Hsu1
Yao-Chin Hsu1 Jinn-Rung Kuo
Jinn-Rung Kuo I-Wen Chen
I-Wen Chen Cheuk-Kwan Sun
Cheuk-Kwan Sun