- 1Department of Thoracic and Cardiovascular Surgery, Dijon University Hospital, Dijon, France
- 2Service de Biostatistiques et d'Information Médicale (DIM), CHU Dijon Bourgogne, INSERM, Université de Bourgogne, CIC 1432, Module Épidémiologie Clinique, Dijon, France
- 3Université Paris-Saclay, Université de Versailles Saint-Quentin-en-Yvelines (UVSQ), Inserm, Centre de recherche en Epidémiologie et Santé des Populations (CESP), Villejuif, France
Introduction: The practice of thoracic surgery for lung cancer is subject to authorization in France. We evaluated the performance of hospitals using 30-day post-operative mortality as a quality indicator, estimating its distribution within each region and measuring its variability between regions.
Material and methods: All data for patients who underwent pulmonary resection for lung cancer in France (2013–2020) were collected from the national hospital administrative database. Thirty-day mortality was defined as any patient who died in hospital (including transferred patients) within the first 30 days after the operation and those who died later during the initial hospitalization. The Standardized Mortality ratio (SMR) was the smoothed, adjusted, hospital-specific mortality rate divided by the expected mortality. To describe the variation in hospital mortality between hospitals in each region, we used different commonly used indicators of variation such as coefficients of variation (CV), interquartile interval or range (IQR), extreme ratio, and systematic component of variance (SCV).
Results: In 2013–2020, 87,232 patients underwent lung resection for cancer in France. The number of deaths was 2,537, a rate of 2.91%. The median SMR of 199 hospitals was 0.99 with an IQR of 0.86 to 1.18 and a CV of 0.25. Among the regions that had the most hospitals performing lung resections for cancer, the extreme ratio was >2, which means that the maximum value is twice as high as the minimum value. The SCV between hospitals was >10 for two of these regions, which is considered indicative of very high variation. For the other regions (with few hospitals performing lung resections for cancer), the variation between hospitals was lower. Globally, the variability between regions concerning the SMR was moderate, 6% of the variance was due to differences across regions. On the contrary, the hospital volume was significantly related to the SMR (p = 0.003) with a negative linear trend, whatever the region.
Conclusion: This work shows significant differences in the practices of the various hospitals within regions. However, overall, the variability in the 30-day mortality rate between regions was moderate. Our findings raises questions regarding the regionalization of major surgical procedures in France.
Introduction
The practice of lung cancer surgery in France has been the subject of several publications using the national hospital (PMSI) medico-administrative database (1–3). Although the number of hospitals performing this surgery was reduced following the implementation of the French National Cancer Plan (4), the number still remains high. The corollary of this situation is that many surgical teams have relatively low surgical activity (1, 2). The number of lung resections performed per year, called hospital volume, is one of the indicators influencing post-operative mortality (2, 5). Post-operative mortality is one of the quality indicators of lung cancer surgery, as recently demonstrated by Fernandez et al. (6).
Thoracic surgery for lung cancer (LC) is a surgical act that is subject to authorization in France, and this authorization is granted to hospitals by the regional authorities (4). There is yet to be an evaluation of the quality of care of hospitals in different regions in France for this type of surgery.
Our work consisted of evaluating the performance of hospitals using one quality indicator, 30-day post-operative mortality, and then estimating the distribution of this indicator within each region. Our secondary objective was to measure the variability of this indicator from one region to another.
Materials and methods
Data source and study population
All data for patients who underwent pulmonary resection for LC in France from January 2013 to December 2020 were collected from the national hospital administrative database. This database, called PMSI for “Programme de Médicalisation des Systèmes d'Information,” was inspired by the US Medicare system. The reliability and validity of PMSI data have already been assessed (7). Routinely collected medical information includes the principal diagnosis, secondary diagnoses and procedures performed. Diagnoses identified during the hospital stay are coded according to the International Classification of Diseases, tenth revision (ICD-10) (8). We selected patients for whom a diagnosis of primary lung cancer was coded as the principal discharge diagnosis (all codes C34). Procedures are coded according to the CCAM (Classification Commune des Actes Médicaux). For all patients, LC was confirmed by pathology analyses according to the 2004 World Health Organization classification of LC (7). Surgery-related variables included the surgical approach [thoracotomy, video assisted thoracic surgery (VATS) or robot-assisted surgery], the type of resection (limited resection, lobectomy, bi-lobectomy and pneumonectomy), bronchioplasty, and the extent of the pulmonary resection (to the chest wall, the left atrium, the carina, the diaphragm, and the superior vena cava).
Patient consent was not required. Ethics approval for use of this database was obtained from the French National Commission for Data protection (Commission Nationale de l'Informatique et des Libertés: No 1576793), and this study adhered to the tenets of the Declaration of Helsinsksi.
Patient characteristics
Patient age and sex were included as baseline demographic characteristics. From the national administrative database, we included the following comorbidities: pulmonary disease (chronic bronchitis, emphysema), heart disease (coronary artery disease, cardiac arrhythmia, congestive heart failure, valvular heart disease, pulmonary artery hypertension, pulmonary embolism), peripheral vascular disease, liver disease, cerebrovascular events, neurological diseases (hemiplegia or paraplegia), renal disease, hematologic disease (leukemia, lymphoma), metabolic disease, anemia, other therapies (preoperative chemotherapy, steroids), and infectious disease. We also calculated the modified Charlson Comorbidity Index (CCI) as a marker of comorbidity (9).
Region and hospital characteristics
Metropolitan France comprises 13 regions: Auvergne Rhones-Alpes (ARA), Bourgogne Franche-Comté (BFC), Bretagne (BRE), Centre Val-de-Loire (CVL), Corse (COR), Grand-Est (GE), Hauts-de-France (HdF), L'ile de France (IdF), Normandie (NOR), Nouvelle Aquitaine (NA), Occitanie (OC), Pays de Loire (PdL) and Provence Alpes Côte d'Azur (PACA). For each hospital within a region, we determined the number of times each type of pulmonary resection was performed from January 1, 2013, to December 31, 2020. Hospital volume was defined as the median number of procedures performed per year. For the purpose of the analysis, the hospital volume was represented as a continuous variable that was transformed into a logarithm.
Outcome measurements
Thirty-day mortality for a patient was defined as the occurrence of death in hospital (including transferred patients) either within the first 30-days after the operation or later on during the initial hospitalization. In other words, in the calculation of 30-day in-hospital mortality, we included deaths that occurred during the surgical stay, as well as any death that occurred during a subsequent hospitalization within 30-days of admission for the initial surgery.
Statistical analysis
To obtain a reliable measure of hospital quality, we used the hierarchical logistic regression model with “shrinkage” estimators. The adjusted Standardized Mortality ratio (SMR) was determined as the smoothed, adjusted, hospital-specific mortality rate divided by the expected mortality. The expected mortality was estimated from a fixed-effects component of hierarchical logistic model regression (10), using comorbidities, age, sex, modified CCI score, and the type of pulmonary resection (the approach and extent of resection) as adjustment factors. The hierarchical logistic regression model was developed using BUGS software (Bayesian Inference Using Gibbs Sampling, version 0.60; MRC Biostatistics Unit, Cambridge, United Kingdom). The credible 95% probability interval (PI) for each provider was then estimated.
In addition, we constructed funnel plots to determine outliers for 30-day mortality according to Spiegelhalter's methodology (11).
We used several methods to describe between-hospital differences in patient characteristics, the different procedures and the SMR of the hospitals within each region. Two groups of statistics of variation are commonly used: those that describe the distribution of rates, such as coefficients of variation (CV), interquartile, interval or range (IQR), extreme ratio, and those that use differences between expected and observed cases, such as the systematic component of variation (SCV) (12). The CV is the ratio of the standard deviation to the mean and measures how the data spreads around the average. The higher the coefficient of variation, the greater the level of dispersion around the mean. If the coefficient of variation is >1, it shows relatively high variability in the data sets. The IQR defines the interval or the range between the 1st and the 3rd quartile of the distribution, and measures how the data spreads around the average. The wider the range, the greater the level of dispersion around the mean. The extreme ratio corresponds to the ratio between the maximum and minimum values. An extreme ratio >2 implies that the maximum value is twice as high as the minimum value. Finally, SCV is the variation arising from the differences between the independent variable. A SCV >10 can be considered indicative of very high variation.
To estimate the potential influence of hospital volume on the SMR, we also studied the relationship between hospital volume and SMR by calculating a linear trend.
To estimate the variability of the SMR between regions, we used the intraclass correlation coefficient (ICC), which was calculated by fitting a multilevel regression model with a fixed coefficient for hospital volume and random intercept for the region.
The calculations for the hierarchical and multilevel logistics regression models were carried out using STATA 14 software (StataCorp, College Station, Tex), and for the full Bayesian analysis we used the R2jags module of R software (http://www.r-project.org).
Results
From 2013 to 2020, 87,232 patients underwent lung resection for cancer in France. The number of deaths was 2,537, resulting in a death rate of 2.91%. The variations in patient characteristics between the 199 hospitals in the 13 French regions is reported in Table 1. Regarding demographics, the median rate of female patients was 0.33, with an IQR of [0.28–0.37], and the median age was 65 years with IQR of [64–66 years] (Table 1). The pneumonectomy and bilobectomy rates varied highly across hospitals, resulting in a CV of 1.7 and 2.09, respectively (Table 1). Hospitals in the different regions had a VATS or robot-assisted surgery rate ranging from 0.075 to 0.47 with a CV of 0.89 (Table 1). The median hospital volume was 37, with an IQR of 9 to 87 procedures per year and a CV of 1.49. Figure 1 illustrates the high variability in hospital volume across the regions.
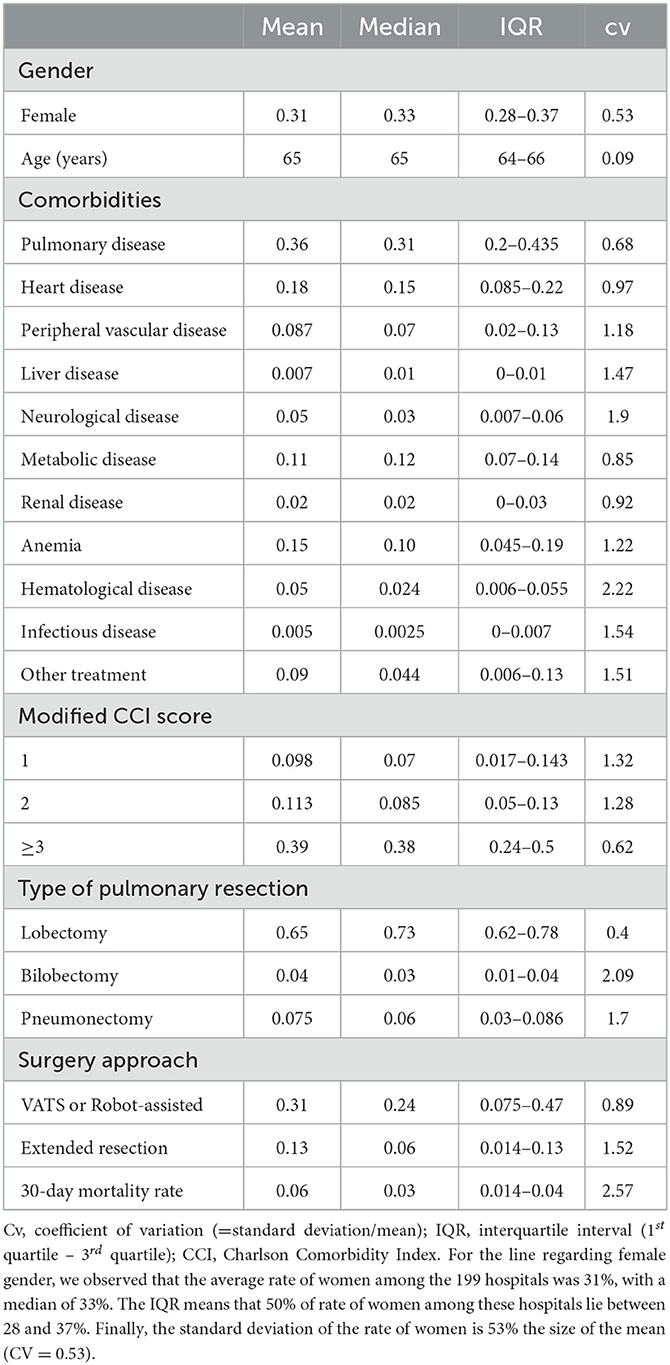
Table 1. Between hospital variation in the characteristics of patients undergoing lung cancer surgery in France, January 2013 to December 2020.
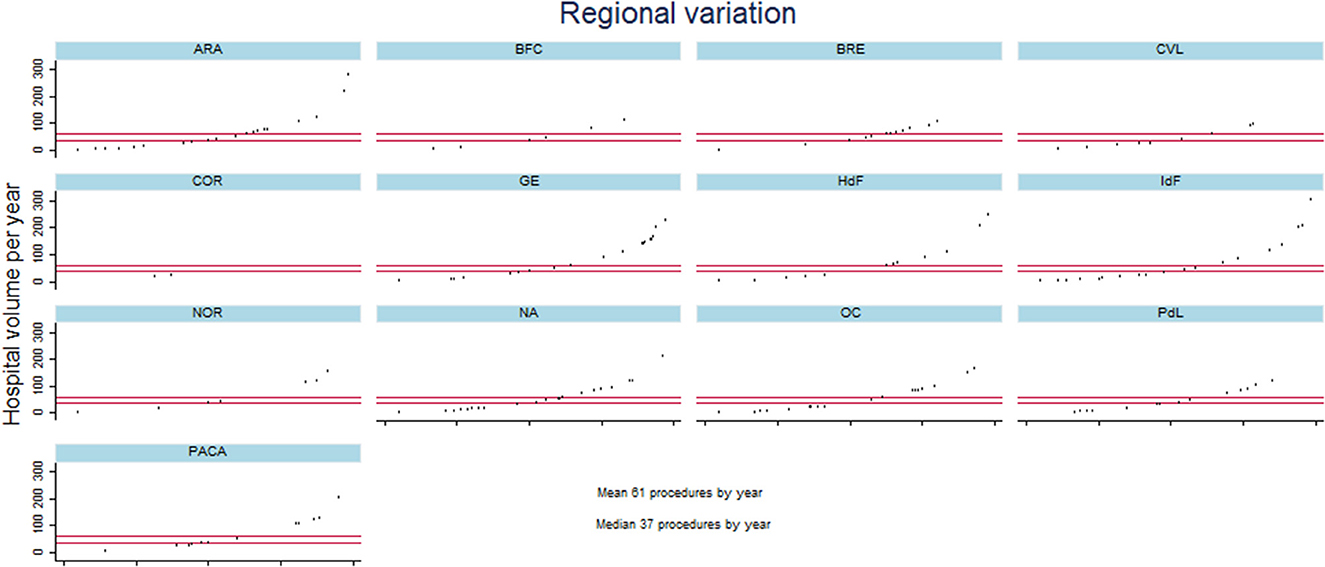
Figure 1. Description of hospital volume per year for the different hospitals in each French region from January 2013 to December 2020. Metropolitan France comprises 13 regions: ARA, Auvergne Rhones-Alpes; BFC, Bourgogne Franche-Comté; BRE, Bretagne; CVL, Centre Val-de-Loire; COR, Corse; GE, Grand-Est; HdF, Hauts-de-France; IdF, L'ile de France; NOR, Normandie; NA, Nouvelle Aquitaine; OC, Occitanie; PdL, Pays de Loire; and PACA, Provence Alpes Côte d'Azur. The X axis of each figure represents the different hospitals per region and the Y axis the hospital volume.
Standardized mortality rate
In order to calculate the SMR, the model used to obtain the expected 30-day mortality included 16 comorbidities, age, sex, modified CCI score, and the type of pulmonary resection (the approach and extent of resection). The reliability of 30-day mortality was 0.43 with 95% confidence interval (CI) of 0.32 to 0.53. The median SMR of 199 hospitals was 0.99 with an IQR of 0.86 to 1.18 and a CV of 0.25.
Identification of quality-of-care outliers
The funnel plot for the SMR describing hospital performance is displayed in Figure 2. It shows that out of 199 hospitals, 13 lie below the lower limit of the central 95% region, indicating performance that was better than expected. The thirteen hospitals that lie above the upper limit performed significantly worse than expected.
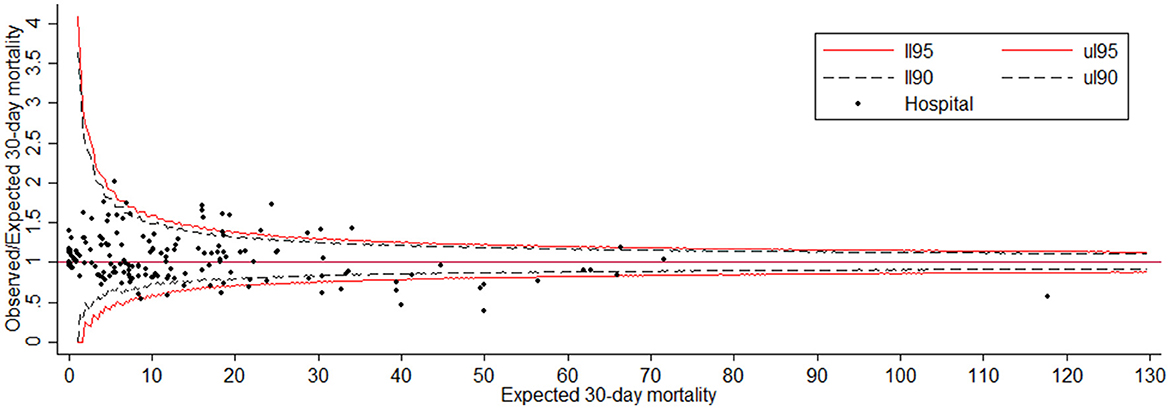
Figure 2. Funnel plot for the 30-day mortality with adjusted Observed/Expected ratio (SMR). The red line corresponds to the 95% control limit and the dash black line corresponds to the 90% control limit.
Regional variation
Out of the 13 regions, four regions (COR, BFC, CVL and NOR) had less than ten hospitals performing lung resections for cancer, five regions (HdF, BRE, PdL, PACA and OC) had between 10 and 20 hospitals, and four regions (GE, NA, IdF and ARA) had between twenty and thirty hospitals.
The variation in the SMR between hospitals in different regions is reported in Table 2, which shows the following measures: mean, CV, extreme ratio, interquartile ratio and SCV. Amongst the regions with the highest number of hospitals performing lung resections for cancer, the extreme ratio (i.e., the ratio of the highest SMR to the lowest SMR) was >2. On the other hand, the SCV was >10 in four regions (ARA, IdF, NOR, and PdL), which can be considered indicative of very high variation in these regions. For the OC region, the SCV was 4.9, while the extreme ratio was 4.45. Some regions with few hospitals, such as BRE, CVL, NOR and PdL had a high variability with an extreme ratio around 2. For the other regions, the variation between hospitals was smaller.
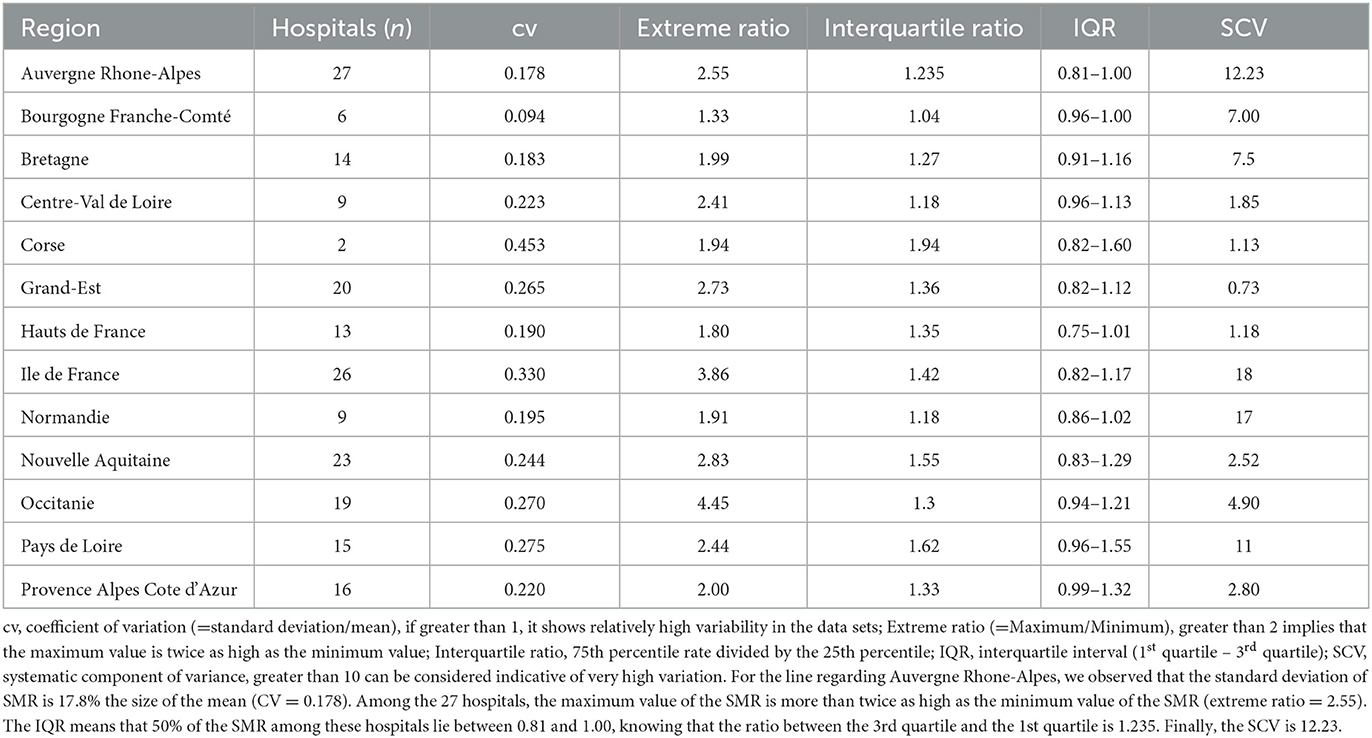
Table 2. Between hospital variation in adjusted standardized mortality rates in each region of France.
Figure 3 shows the relationship between the hospital volume (i.e., the median number of procedures performed per year) and SMR. The hospital volume was significantly related to the SMR (p = 0.003) with a negative linear trend, whatever the region (Figure 3). However, we noted a difference in the slope of the linear trend of the SMR between regions. The variability between regions was globally moderate with an ICC of 0.06 (95% CI: 0.014–0.23), indicating that 6% of the SMR variance is due to differences across regions. This is consistent with the value of IQRs observed from one region to another, seeing as the intervals overlap (Table 2). Statistically, this means that the SMRs are not different from one region to another.
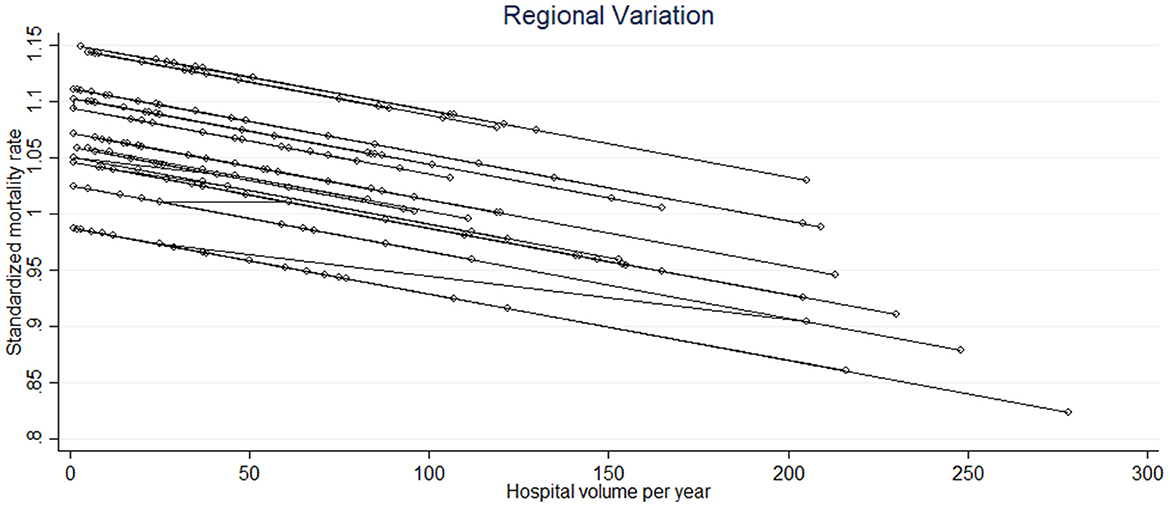
Figure 3. The significant linear relationship between the standardized mortality rate and the hospital volume of the different hospitals in each region (each circle corresponds to a hospital and each line to a region).
Discussion
To the best of our knowledge, this is the first study of this type to be carried out in France. The literature on the study of regional variations in surgical practice in hospitals is fairly poor (13–15). Our work underscores the fact that there is currently a large number of French hospitals performing resections for lung cancer. Surgical practice is dispersed and in-hospital mortality varies considerably from one hospital to another. The mean SMR was similar across regions, but with great variability between hospitals within regions. Nevertheless, the variability was more marked for certain regions, particularly those in which many hospitals perform the surgery.
Our work reveals that there is variability in the practices of the different hospitals as well as in the different regions. There are still many low-volume hospitals in France despite the required authorization. One of the characteristics of French health care is the dispersed supply of care, which is also seen in other European countries (16–19). However, the number of hospitals per region practicing this type of surgery is not in line with the needs of the population in regions such as in Auvergne Rhône-Alpes or Nouvelle Aquitaine.
To our knowledge, the variation in hospital comorbidities within regions has not yet been described in the literature. Our work reveals a considerable variation in the rate of certain comorbidities, such as peripheral vascular disease, liver disease, anemia and hematological disease. The coefficient of variation was 1.18, 1.47, 1.22, and 2.22, respectively. It is possible that the patients managed in the different hospitals are different in terms of comorbidities or that the coding for the associated PMSI diagnoses is not consistent from one hospital to another. Because of our data source, it is not possible to know which of these hypotheses is most likely to explain the differences observed.
The type of lung resection also varied from one hospital to another, particularly bilobectomies and pneumonectomies, and we cannot compare our results with the literature because lung cancer surgery has not been published using the same methodology as ours. Pneumonectomies are complex procedures more often performed by specialized teams in high volume units, which may explain the variability observed between hospitals.
The median 30-day mortality rate was 3%, which appears to be higher than in some European countries, which is consistent with a recent systematic review (20) comparing mortality following lung cancer resection in France with other European countries. The systematic review showed that France has a higher rate than some other European countries, including England, Denmark, Holland or Finland. Our work confirms the great variability in post-operative mortality between hospitals, as shown by the interquartile values and the coefficient of variation. It is a complex issue to understand why France (20) has a higher rate of post-operative mortality than other European countries.
The fact that volume of hospital activity is significantly related to excess mortality (21–25) has been demonstrated many times in the literature. Countries in which fewer centers offer thoracic surgery, such as in the UK, have a lower overall post-operative mortality rate than France. On average, their centers also have a higher volume of activity than French centers (16–19), and an interesting English study showed that high-volume centers had better survival after lung cancer surgery (23). The literature unanimously illustrates that high-volume centers have better results in terms of mortality, confirmed by our study, whatever the French region. Obviously, hospital volume is not the only component of quality of care that can have a role in hospital mortality, and we know that the nurse to patient staffing ratio or the processes in the different units could have an important role. For example, in a study by Aiken et al. (26) in nine European countries, the authors showed that an increase of one patient per nurse is associated with a 7% increase in the risk of a surgical patient dying within 30-days of admission. Further studies are needed to assess these additional factors, but we unfortunately do not have access to such data in the PMSI database.
Our work provides an estimation of the variability in post-operative mortality between regions, a subject for which the literature is scarce (27). We have shown that the difference in 30-day mortality between regions is ultimately moderate, and the most striking variability was observed between hospitals within regions. Our findings raise questions regarding current regionalization policies for major surgical procedures such as lung cancer surgery. Some countries have moved toward the centralization of complex surgeries in selected hospitals in an attempt to group together the technical skills needed to improve quality of care (28, 29). This idea seems attractive, especially if we want to be able to measure hospital performance reliably. Compared with other countries, France offers dispersed care for major interventions like thoracic surgery or pancreatic surgery, which could be one of the reasons that the death rate is higher in France than in other countries (20).
The differences in the 30-day mortality of hospitals in France could also be explained by the lack of quality measurement, in contrast to certain European countries (16–19). European surgical teams that undertake regular assessments of their practice are informed of their level of performance and can thus implement actions to improve their results.
We recognize that our study has some limitations. In particular, the choice of mortality as the key outcome is a limitation because we did not assess the overall quality of care but only one indicator, the 30-day mortality rate, which is only one of several potential indicators. Other indicators, for instance post-operative complications after lung resection, such as pneumopathy or atelectasis, which are good quality indicators, cannot be obtained through the PMSI. We only had access to in-hospital mortality data, but it is nevertheless a relevant indicator for this type of surgery. Another limitation concerns the TNM stage, which is not recorded in the PMSI, but is a factor that can influence mortality. The final limitation concerns the risk of underestimating certain comorbidities because of the quality of the coding. Indeed, coding practices may vary among institutions since the people who perform the coding of diagnoses can be clinicians or information system technicians. Nevertheless, the quality of coding is checked in a standardized way by medical information professionals in each hospital in order to correct diagnoses (internal quality assessment), and the level of re-cording of co-morbidities has increased significantly in recent years, following its impact on the tariff of hospital stays. Because of the impact on hospital budget allocation, it has been shown that hospital claims data are becoming more accurate. In addition, a national external quality assessment program has been implemented to verify the quality of discharge abstracts in each hospital.
In conclusion, this work shows significant differences in the practices of the various hospitals within each French region. However, between regions, there were only moderate variations in the 30-day mortality rate. These results should encourage surgical teams in France to implement quality of care measures based on the analysis of outcomes. Finally, our findings call into question the current policies relative to the regionalization of major surgical procedures in France.
Data availability statement
The datasets presented in this article are not readily available because the use of these data by our department was approved by the National Committee for data protection. We are not allowed to transmit these data. PMSI data are available for researchers who meet the criteria for access to these French confidential data (this access is submitted to the approval of the National Committee for data protection) from the national agency for the management of hospitalization (ATIH-Agence technique de l'information sur l'hospitalisation). Requests to access the datasets should be directed to Agence technique de l'information sur l'hospitalisation 117 boulevard Marius Vivier Merle 69329 Lyon Cedex 03.
Author contributions
AB was involved in the conception and design of the study, in charge of the analysis, involved in the interpretation, wrote the first draft, and approved the final version. JC was responsible for the data collection, accessed and verified the data, involved in the interpretation, critically reviewed the first draft, and approved the final version. P-BP was involved in the conception and design of the study, involved in the interpretation, critically reviewed the first draft, and approved the final version. CQ was the coordinator of the study, responsible for the data collection, accessed and verified the data, involved in the interpretation, and critically reviewed the first draft. All authors approved the final version.
Acknowledgments
The authors thank Harbajan Chadha-Boreham for reviewing the English and Gwenaëlle Periard for her help with the layout and management of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Pagès PB, Cottenet J, Mariet AS, Bernard A, Quantin C. In-hospital mortality following lung cancer resection: nationwide administrative database. Eur Respir J. (2016) 47:1809–17. doi: 10.1183/13993003.00052-2016
2. Bernard A, Cottenet J, Mariet AS, Quantin C, Pagès PB. Is an activity volume threshold really realistic for lung cancer resection? J Thorac Dis. (2018) 10:5685–94. doi: 10.21037/jtd.2018.09.77
3. Bernard A, Pagès PB, Mariet AS, Pforr A, Madelaine L, Cottenet J, et al. Evaluation de la pratique du cancer bronchique en France à partir de la base nationale du PMSI. evaluation of surgical practice in the treatment of lung cancer in france from the pmsi national database. Revue des Mal Respir. (2018) 36:31–8. doi: 10.1016/j.rmr.2018.01.014
4. Ministère de l'Enseignement Supérieur et de la, Recherche, Ministère de la Santé et des, Sports. Plan Cancer 2009– 2013. Available online at: http://www.e-cancer.fr/Plan-cancer/Les-Plans-cancer-de-2003-a-2013/Le-Plancancer-2009-2013 (accessed March 2016).
5. Kozower BD, Stukenborg GJ. The relationship between hospital lung cancer resection volume and patient mortality risk. Ann Surg. (2011) 254:1032–7. doi: 10.1097/SLA.0b013e31821d4bdd
6. Fernandez FG, Kosinski AS, Burfeind W, Park B, DeCamp MM, Seder C, et al. STS lung cancer resection risk model: higher quality data and superior outcomes. Ann Thorac Surg. (2016) 102:370–7. doi: 10.1016/j.athoracsur.2016.02.098
7. World Health Organization. International Statistical Classification of Diseases and Related Health Problems 10th Revision. Available online at: http://apps.who.int/classifications/icd10/browse/2016/en (accessed March 1, 2016).
8. Iezzoni LI. Assessing quality using administrative data. Ann Intern Med. (1997) 127:666–74. doi: 10.7326/0003-4819-127-8_Part_2-199710151-00048
9. Charlson M, Szatrowski TP, Peterson J, Gold J. Validation of a combined comorbidity index. J Clin Epidemiol. (1994) 47:1245–51. doi: 10.1016/0895-4356(94)90129-5
10. Normand SLT, Shahian DM. Statistical and clinical aspects of hospitals outcomes profiling. Stat Sci. (2007) 22:206–26. doi: 10.1214/088342307000000096
11. Spiegelhalter D. Funnel plots for comparing institutional performance. Statist Med. (2005) 24:1185–202. doi: 10.1002/sim.1970
12. Ibáñez B, Librero J, Bernal-Delgado E, Peiró S, López-Valcarcel BG, Martínez N, et al. Is there much variation in variation? revisiting statistics of small area variation in health services research. BMC Health Serv Res. (2009) 9:60. doi: 10.1186/1472-6963-9-60
13. Wouters MW, Siesling SS, Jansen-Landheer ML, et al. variation in treatment and outcome in patients with nonsmall cell lung cancer by region, hospital type and volume in the Netherlands. Eur J Surg Oncol. (2010) 36:S83–92. doi: 10.1016/j.ejso.2010.06.020
14. Zettervall SL, Soden PA, Buck DB, Cronenwett JL, Goodney PP, Eslami MH, et al. Significant regional variation exists in morbidity and mortality after repair of abdominal aortic aneurysm. J Vasc Surg. (2017) 65:1305–12. doi: 10.1016/j.jvs.2016.08.110
15. Gurney JK, McLeod M, Stanley J, Robson B, Campbell D, Dennett E, et al. Regional variation in post-operative mortality in New Zealand. ANZ J Surg. (2022) 92:1015–25. doi: 10.1111/ans.17510
16. Jakobsen E, Green A, Oesterlind K, Rasmussen TR, Iachina M, Palshof T. Nationwide quality improvement in lung cancer care: the role of the danish lung cancer group and registry. J Thorac Oncol. (2013) 8:1238–47. doi: 10.1097/JTO.0b013e3182a4070f
17. Beck N, Hoeijmakers F, van der Willik EM, Heineman DJ, Braun J, Tollenaar RAEM, et al. National comparison of hospital performances in lung cancer surgery: the role of case mix adjustment. Ann Thorac Surg. (2018) 106:412–20. doi: 10.1016/j.athoracsur.2018.02.074
18. Helminena O, Valoa J, Andersenb H, Lautamäkia A, Vuohelainena V, Sihvoa E. Real-world guideline-based treatment of lung cancer improves short- and long-term outcomes and resection rate: a population-based study. Lung Cancer. (2020) 140:1–7. doi: 10.1016/j.lungcan.2019.12.002
19. Royal College of Physicians. Lung Cancer Clinical Outcomes Publication 2018 (for surgical operations performed in 2016). London: RCP (2018).
20. Bernard AA, Riviere A, Cottenet J, Madeleine L, Quantin C, Pages PB. Comparison of mortality of lung cancer resections in France to other European countries. Rev Mal Respir. (2022) 39:669–75. doi: 10.1016/j.rmr.2022.08.002
21. Lien YC, Huang MT, Lin HC. Association between surgeon and hospital volume and in-hospital fatalities after lung cancer resections: the experience of an Asian contry. Ann Thorac Surg. (2007) 83:1837–43. doi: 10.1016/j.athoracsur.2006.12.008
22. Sioris T, Sihvo E, Sankila R, Salo J. effect of surgical volume and hospital type on outcome in non-small cell lung cancer surgery: a finnish population-based study. Lung Cancer. (2008) 59:119–25. doi: 10.1016/j.lungcan.2007.07.020
23. Lüchtenborg M, Riaz SP, Coupland VH, Lim E, Jakobsen E, Krasnik M, et al. High procedure volume is strongly associated with improved survival after lung cancer surgery. J Clin Oncol. (2013) 31:3141–6. doi: 10.1200/JCO.2013.49.0219
24. Ross JS, Normand S-LT, Wang Y, Ko DT, Chen J, Drye EE, et al. Hospital volume and 30-day mortality for three common medical conditions. N Engl J Med. (2010) 362:1110–8. doi: 10.1056/NEJMsa0907130
25. von Meyenfeldt EM, Gooiker GA, Van Gijn W, Post PN, van de Velde CJH, Tollenaar RAEM, et al. The relationship between volume or surgeon speciality and outcome in the surgical treatment of lung cancer. a systematic review and meta-analysis. J Thorac Oncol. (2012) 7:1170–8. doi: 10.1097/JTO.0b013e318257cc45
26. Aiken LH, Sloane DM, Bruyneel L, Van den Heede K, Griffiths P, Busse R, et al. Nurse staffing and education and hospital mortality in nine European countries: a retrospective observational study. Lancet. (2014) 383:1824–30. doi: 10.1016/S0140-6736(13)62631-8
27. Birkmeyer JD, Reames BN, McCulloch P, Carr AJ, Campbell WB, Wennberg JE, et al. Understanding regional variation in the use of surgery health public. Lancet. (2013) 382:1121–9. doi: 10.1016/S0140-6736(13)61215-5
28. Bendzsak AM, Baxter NN, Darling GE, Austin PC, Urbach DR. Regionalization and outcome of lung cancer surgery in Ontario Canada. J Clin Oncol. (2017) 35:2772–80. doi: 10.1200/JCO.2016.69.8076
Keywords: lung cancer surgery, standardized mortality rate, variation, region, quality of care
Citation: Bernard A, Cottenet J, Pages P-B and Quantin C (2023) Is there variation between hospitals within each region in postoperative mortality for lung cancer surgery in France? A nationwide study from 2013 to 2020. Front. Med. 10:1110977. doi: 10.3389/fmed.2023.1110977
Received: 29 November 2022; Accepted: 27 February 2023;
Published: 14 March 2023.
Edited by:
Shuibang Wang, National Institutes of Health (NIH), United StatesReviewed by:
Gunnar N. Hillerdal, Karolinska University Hospital, SwedenDong Xie, Tongji University, China
Copyright © 2023 Bernard, Cottenet, Pages and Quantin. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Catherine Quantin, Y2F0aGVyaW5lLnF1YW50aW5AY2h1LWRpam9uLmZy
 Alain Bernard
Alain Bernard Jonathan Cottenet2
Jonathan Cottenet2 Catherine Quantin
Catherine Quantin