
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
EDITORIAL article
Front. Med., 18 July 2022
Sec. Intensive Care Medicine and Anesthesiology
Volume 9 - 2022 | https://doi.org/10.3389/fmed.2022.973679
This article is part of the Research TopicBedside Visual Image Technologies for Respiratory and Circulatory Management in Intensive Care SettingsView all 10 articles
Editorial on the Research Topic
Bedside Visual Image Technologies for Respiratory and Circulatory Management in Intensive Care Settings
Cardiovascular and pulmonary systems are the major systems that suffer from critical diseases and injuries among patients. Accessible and accurate tools providing diagnosis and monitoring information are warranted to assist individualized therapy and decision making. Up-to-date, novel imaging techniques emerge thanks to the advancement in the field, including novel imaging modalities that have not been widely used in clinical practice. Bedside visual image technologies, including electrical impedance tomography (EIT) for ventilation and perfusion, and critical care ultrasound for alveolar atelectasis and cardiac output assessments, have gained great attentions in ICU/operating theater. In the current Research Topic, we are happy to collect one review, two case reports, one simulation, and five clinical studies investigated in more than 250 subjects to update our knowledge in the field.
Interactions among cardiovascular, pulmonary and other systems are often complicated. Many diseases could lead to multiple-organ failure. One example is hepatopulmonary syndrome, which causes pulmonary vascular dysfunction secondary to liver cirrhosis (1). Evidence of intrapulmonary vascular dilatation is one of the diagnostic criteria for hepatopulmonary syndrome. Therefore, imaging examination could be one of the critical measures to identify pulmonary vasodilatation. In the current Research Topic, Luo and Du reviewed the recent advance diagnostic imaging techniques for hepatopulmonary syndrome, including ultrasound, dynamic pulmonary perfusion imaging, pulmonary angiography, and computed tomography. They discussed the pros and cons of the current techniques and pointed out the need and room for further development of imaging techniques.
In addition to the multiple-organ interactions, treatment of cardiopulmonary diseases may introduce some psychological impairments (2). Some studies indicated that revisiting the ICU treatment period could be helpful via providing patients with necessary information (3). Vlake et al. demonstrated in a patient recovered from COVID-19 that virtual reality intervention provided a valuable adjunct to improve patient's psychological status. The development and application of the virtual reality module require an interdisciplinary cooperation. To increase the effectiveness, the module might need to be constructed individually to meet the experience of the patient groups. Therefore, it is a promising field that requires further investigation.
The rest of the papers in the Research Topic are either ultrasound or EIT related, which implicates rapid development in these two imaging modalities. The use of medical ultrasound for cardiovascular system can date back to 1960s (4). To date, ultrasound is used as a diagnostic tool as well as guiding tool for certain maneuvers. To evaluate the right ventricle filling state, Zhao et al. used echocardiography to dynamically monitor central venous pressure and the size of right ventricle. They were able to clarify the correlation between left ventricle stroke volume and negative fluid balance in 71 patients with elevated central venous pressure via comparing hemodynamic and echo parameters at baseline and after negative fluid balance. Ultrasound-guided catheterization has been used for a decade but the success rate may depend on arterial depth (5). Tian et al. retrospectively analyzed 119 patients and demonstrated a potential correlation between first-attempt success and arterial depth.
EIT is a novel non-invasive bedside imaging modality (6). EIT can be used to monitor the ventilation distributions during the entire ventilation support period. A recently important milestone is the evidence from two randomized-controlled trials that EIT-guided positive end-expiratory pressure (PEEP) settings may improve outcomes (length of hospital stay, mortality etc.) in patients with acute respiratory distress syndrome (ARDS) (7, 8). Li et al. evaluated the possibility to predict weaning outcome in patients with delayed upper abdominal surgery. Another team tested the ability of EIT to predict outcome of high flow nasal cannula therapy. These studies broadened the use of EIT to support the respiratory management in ICU. Lung perfusion assessed with EIT helps physicians to understand the ventilation-perfusion matching status and identify the potential reasons for respiratory failure (9). Hypertonic saline bolus is injected via central venous catheter to augment the impedance signal. Wang et al. shared their experience in managing a patient with high-risk pulmonary embolism. Not only adult patients can benefit from EIT. Ren et al. compared PEEP titration with global and regional compliance calculated with EIT data in pediatric ARDS. We believe more and more EIT applications in pediatric patients may be published when the device manufactures provide EIT for such patient group. Various requirements need to be considered for different applications and different patient groups, such as electrode size, position, noise suppression, baseline drift and moving artifacts. Yang et al. presented mathematical method to overcome some of the issues during practical EIT measurements. Although the effectiveness was only validated in limited patient data but the results were promising.
Although medical ultrasound has been reported since several decades, due to the lack of bedside tools, lung ultrasound became one of the hot topics in recent years (10, 11). Lung and heart ultrasound provides different information compared to EIT: ultrasound could provide morphology information of cardiopulmonary lesions, cardiac systolic and diastolic function, special signs of etiologies, whereas EIT could make a rapid functional assessment of regional lung ventilation, perfusion and the corresponding matching. Development of personalized medicine and clinical decision may benefit from the information of both bedside techniques. In clinical practice, we propose to combine these two techniques to manage patients with cardiopulmonary dysfunctions (Figure 1). By combining EIT and ultrasound, we can make a holistic management for the circulatory and respiratory failure. Further studies are warranted to examine whether the proposed workflow can improve patient outcomes.
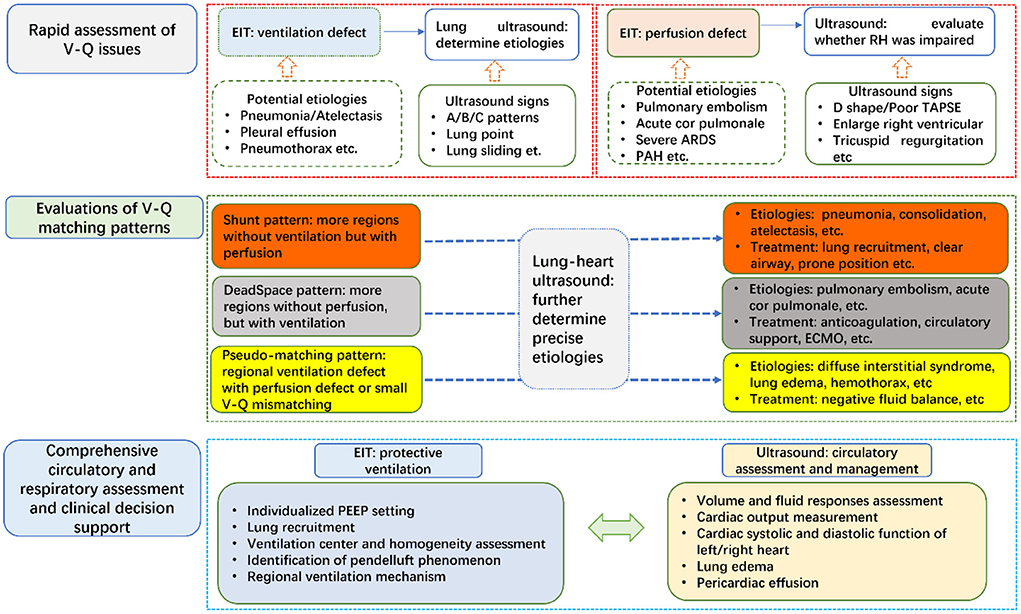
Figure 1. Combination of chest EIT and lung ultrasound for respiratory and circulatory managements in ICU. TAPSE, Tricuspid annular plane systolic excursion; PAH, pulmonary arterial hypertension; ARDS, acute respiratory distress syndrome; V-Q, ventilation-perfusion; PEEP, positive end-expiratory pressure; ECMO, extracorporeal membrane oxygenation.
HH and ZZ drafted the manuscript. YL and KM critically revised the manuscript. All authors have approved the final version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Kennedy TC, Knudson RJ. Exercise-aggravated hypoxemia and orthodeoxia in cirrhosis. Chest. (1977) 72:305–9. doi: 10.1378/chest.72.3.305
2. Bienvenu OJ, Friedman LA, Colantuoni E, Dinglas VD, Sepulveda KA, et al. Psychiatric symptoms after acute respiratory distress syndrome: a 5-year longitudinal study. Intensive Care Med. (2017) 44:38–47. doi: 10.1007/s00134-017-5009-4
3. Vlake JH, van Genderen ME, Schut A, Verkade M, Wils E-J, et al. (2020) Patients suffering from psychological impairments following critical illness are in need of information. J Intensive Care 8. doi: 10.1186/s40560-019-0422-0
4. Gramiak R, Shah PM. Echocardiography of the aortic root. Invest Radiol. (1968) 3:356–66. doi: 10.1097/00004424-196809000-00011
5. Nakayama Y, Nakajima Y, Sessler DI, Ishii S, Shibasaki M, et al. A novel method for ultrasound-guided radial arterial catheterization in pediatric patients. Anesthesia Analgesia. (2014) 118:1019–26. doi: 10.1213/ANE.0000000000000164
6. Frerichs I, Amato MB, van Kaam AH, Tingay DG, Zhao Z, et al. Chest electrical impedance tomography examination, data analysis, terminology, clinical use and recommendations: consensus statement of the TRanslational EIT developmeNt stuDy group. Thorax. (2017) 72:83–93. doi: 10.1136/thoraxjnl-2016-208357
7. He H, Chi Y, Yang Y, Yuan S, Long Y, et al. Early individualized positive end-expiratory pressure guided by electrical impedance tomography in acute respiratory distress syndrome: a randomized controlled clinical trial. Crit Care. (2021) 25:230. doi: 10.1186/s13054-021-03645-y
8. Hsu HJ, Chang HT, Zhao Z, Wang PH, Zhang JH, et al. Positive end-expiratory pressure titration with electrical impedance tomography pressure-volume curve: a randomized trial in moderate to severe ARDS. Physiol Meas. (2021) 42:014002. doi: 10.1088/1361-6579/abd679
9. He H, Chi Y, Long Y, Yuan S, Zhang R, et al. Three broad classifications of acute respiratory failure etiologies based on regional ventilation and perfusion by electrical impedance tomography: a hypothesis-generating study. Ann Intensive Care. (2021) 11:134. doi: 10.1186/s13613-021-00921-6
10. Blanco PA, Cianciulli TF. Pulmonary edema assessed by ultrasound: impact in cardiology and intensive care practice. Echocardiography. (2016) 33:778–87. doi: 10.1111/echo.13182
Keywords: critical EIT, critical ultrasound, lung ventilation, lung perfusion, respiratory and circulatory management
Citation: He H, Long Y, Möller K and Zhao Z (2022) Editorial: Bedside visual image technologies for respiratory and circulatory management in intensive care settings. Front. Med. 9:973679. doi: 10.3389/fmed.2022.973679
Received: 20 June 2022; Accepted: 04 July 2022;
Published: 18 July 2022.
Edited and reviewed by: Zhongheng Zhang, Sir Run Run Shaw Hospital, China
Copyright © 2022 He, Long, Möller and Zhao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Huaiwu He, aGVodWFpd3VAcHVtY2guY24=; Zhanqi Zhao, emhhbnFpLnpoYW9AaHMtZnVydHdhbmdlbi5kZQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.