
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
COMMUNITY CASE STUDY article
Front. Med. , 21 October 2022
Sec. Healthcare Professions Education
Volume 9 - 2022 | https://doi.org/10.3389/fmed.2022.966193
 Eraka P. Bath1,2
Eraka P. Bath1,2 Kathleen Brown1,3
Kathleen Brown1,3 Christina Harris1,4
Christina Harris1,4 Alma Guerrero1,5
Alma Guerrero1,5 Daniel Kozman1,6,7
Daniel Kozman1,6,7 Charles C. Flippen II1,8
Charles C. Flippen II1,8 Isla Garraway1,9
Isla Garraway1,9 Karol Watson1,6
Karol Watson1,6 Langston Holly1,8
Langston Holly1,8 Sarah M. Godoy10*
Sarah M. Godoy10* Keith Norris1,7
Keith Norris1,7 Gail Wyatt1,2
Gail Wyatt1,2The woefully low proportion of scientists and clinicians underrepresented in medicine (UIM), including members of African-American/Black, Hispanic/Latinx, American Indian/Alaska Native or Native Hawaiian/Pacific Islander communities, is well characterized and documented. Diversity in medicine is not only just, but it improves quality and outcomes. Yet, diversity in academic medicine remains stagnant, despite national recognition and urgent calls to improve diversity, equity, and inclusion across health sciences. One strategy that has shown to improve diversity in many sectors is high quality mentoring. While many institutions have adopted mentoring programs, there remains a lack of mentorship that is equitable, individualized, and sets a clear timeline for academic milestones that will position UIM mentees at the optimal trajectory for promotion and retention. A barrier to assembling these programs is the small number of UIM among the senior faculty ranks who are able to serve in this role, given the disproportionate burden to serve on a multitude of academic committees, task forces, and workgroups to fulfill institutional mandates to diversify representation. These time-consuming services, documented in the literature as the “minority tax,” are generally uncompensated and unaccounted for in terms of consideration for promotion, leadership positions, and other measures of career advancement. The Justice, Equity, Diversity, and Inclusion Academic Mentors (JAM) Council represents a novel, culturally responsive, and anti-racist approach to achieve a more equitable and inclusive institutional environment. This approach strategically leverages the intergenerational wisdom and experience of senior UIM faculty via time-protected effort with the overall goals of improving rates of promotion, retention, and career satisfaction of early career UIM colleagues. This community case study describes the rationale, resources needed, processes, and proposed workflow required to launch the JAM Council, as well as the major roles and responsibilities for JAM mentors and mentees, which may be considered by academic medical centers focused on improving diversity among the faculty ranks.
The COVID-19 pandemic, the demand for racial and health justice in response to the brutal murders of George Floyd, Breonna Taylor, and many others, and the uprisings that emerged around the country signaled a shift in the collective consciousness around the naming of structural and institutional racism in various sectors, including health (1). Nationally, numerous jurisdictions cited racism as a public health crisis, including several of the most prominent organizations within organized medicine (2). Additionally, the National Academy of Medicine, the American Medical Association, and the National Institutes of Health, as well as multiple scientific journals publicly affirmed the support for Black Lives Matter and the need for racial reckoning, highlighting urgent calls for equity in opportunity and representation among all ranks including the highest within each institution (3, 4). These conversations echoed throughout academic medical centers around the country and prompted faculty members who are underrepresented in medicine (UIM) to build community around shared and lived experiences of isolation, and historic and ongoing aspects of internalized, interpersonal, and structural racism, while simultaneously rallying to create actionable steps to counter these visible and invisible practices of discrimination and denigration (5).
The low proportion of UIM faculty is well characterized and documented (6–8). As demands for racial justice in health science and medicine amplify, workforce diversity has been called out as an ongoing challenge and urgent necessity for achieving health equity. Diversity in medicine is not only just, but it improves health outcomes, perceived quality of care, productivity and innovation (9–12). In fact, the Association of American Medical Colleges (AAMC) has underscored that increasing diversity of the biomedical workforce is a key strategy to mitigate health inequity nationally (13). Unfortunately, despite national recognition and urgent calls to improve diversity, equity, and inclusion in health sciences, vast underrepresentation is evident across many racial/ethnic and gender groups (10, 11).
One strategy that has improved diversity in many sectors is quality mentoring (12–15). In most academic institutions, there is insufficient effective mentorship of early career UIM faculty with these faculty typically receiving less mentorship than their white colleagues (12–14). While many institutions offer mentoring programs of some type, few offer mentorship that is culturally responsive, equity-centered, individualized, and sets a clear timeline for academic milestones that will position the UIM mentee at the optimal trajectory for promotion and retention (16).
Mentoring is extensively documented as a key component to professional development, satisfaction with personal achievement and work environment, and successful promotion in academic medicine (12–14, 17, 18). Yet, consensus on best practice varies by institution, discipline, and perspectives from mentees and mentors (12, 13). Popular mentoring models include dyadic mentoring by an experienced investigator or team-based models where a mentoring team brings different expertise. The mentorship relationship often includes support related to scientific writing and grantsmanship, teaching, promotion, and tenure processes, maintaining work-life balance, time management, and managing and leading a team. Institutional components, including the support of key leaders and dedicated resources, are also critical for sustaining mentorship programs (14). There is well-established evidence that investing in faculty mentoring programs ultimately benefits the academic institutions at the organizational level through improved faculty satisfaction, retention, and institutional climate (12, 13, 19).
Although effective mentoring is critical for academic success, there are limited studies documenting the structure and effectiveness of mentoring programs for UIM faculty (12, 13). More recently, studies that include the implementation or evaluation of UIM mentoring programs that explicitly addresses common obstacles rooted in racist or biased practices and structures have been described (20–24). Research has found that mentorship programs for UIM faculty must assess for relevant elements that include mentors' potential for bias and discrimination, previous mentorship training, experience with intersectionality and isolation, and service on diversity committees, among other factors (20, 21). Yet, most UIM “specific” mentoring programs follow traditional content and structure of general mentoring programs with the only difference being a focus of implementation with UIM faculty.
Few programs are sufficiently adapted and tailored for the specific needs and perspectives of UIM faculty. For example, an adapted program may include pairing mentors and early career faculty who may or may not have similar social characteristics and personal experiences, but often lack a culturally-responsive, intersectional, and equity-centered approach (2). Mentoring programs for UIM faculty are also typically evaluated with general mentoring outcomes, such as career satisfaction and climate assessments (2) but fail to include salient measures related to inclusion and belonging. Effective evaluation tools for UIM mentorship programs should include assessment of belonging and connectedness, reduced clinical responsibilities when engaging in diversity, inclusion, justice, and equity focused service, and other factors that disproportionately burden and tax UIM faculty (24). In short, there is a critical need for a new genre of mentoring that explicitly addresses UIM-specific challenges with mentees and is supported by institutional leadership (13).
While many institutions have adopted mentorship programs for early career faculty, there remains a persistent lack of formal mentorship programs created with an equitable lens for UIM faculty. In particular, there is a lack of mentorship programming that equips UIM faculty with the specific skills needed to navigate the culture of academic medicine that has historically centered and favored the professional organization and socialization of white supremacy values and ideology (25). This set of white supremacy values and ideologies that typically center on the heteronormativity of white, male faculty shapes the discriminatory and oppressive experiences of UIM faculty (26, 27) and other marginalized groups who are often few within their departments and situated in predominantly white institutions.
The numerous obstacles encountered by UIM and women faculty are well documented and include: (a) explicit and insidious racism; (b) microaggressions; (c) devaluation of scholarly contributions, merit, and skillset by colleagues and administrators; (d) the burden of representing all minoritized populations; and (e) the continuous and disproportionate requests to serve on committees, task forces, and workgroups to fulfill institutional mandates to diversify representation that are generally uncompensated, undervalued and unaccounted for, in terms of promotion consideration and career advancement (i.e., minority tax) (24, 25, 27–29). These experiences of both blatant and perceived discrimination, vocational strain, role overload, and adverse life events have also been shown to impact the physical and mental health of UIM faculty (27, 28). Available studies underscore how work-related stress and resulting health conditions may contribute to early morbidity and premature departures of UIM faculty from the academy, further highlighting the urgent need for robust institutional interventions to retain these faculty (19, 27). Additionally, UIM faculty are less likely to be promoted, have leadership positions, and be awarded National Institutes of Health R01 level grants compared to their white peers even after adjusting for multiple potential confounders (30, 31).
Specific mentoring practices and strategies for UIM and other marginalized groups are essential to help navigate these barriers to academic success and promotion. Mentoring programs should be tailored to the multitude of barriers UIM faculty face that non-UIM faculty are unaware of or may deny (25). The mentoring needs and demands for early career UIM faculty far exceed the limited supply of UIM mid-career and senior faculty, and this paucity of senior person-power exacerbates the gap in available mentorship opportunities and networks for those most at risk for attrition (19). Thus, it is important that institutional leadership intentionally create a culture of inclusive excellence by acknowledging the UIM specific challenges that require support and investment for effective mitigation. Therefore, it is critical for institutions to invest in mentoring infrastructure as reliance on grants to run such programs constitutes an unfunded mandate, typically shouldered by UIM mid-career and senior faculty that aggravates the minority tax (24).
At the David Geffen School of Medicine, the University of California, Los Angeles (UCLA) a newly formed collective of Black, Latinx, and Native American (BLNA) faculty engaged in a more explicit dialogue with executive leadership centered on the plight of retention and attrition of UIM faculty, who are often traversing spaces with racism, bias, microaggressions, and exclusion. Together, the collective recognized the need for both top-down and bottom-up antiracist strategies to address the invisible and opaque and the visible dimensions of structural racism in the academic setting. Several potential initiatives emerged from the BLNA faculty collective, including a mentorship program for early career UIM faculty that builds on promising practices.
Institutionalization of an innovative mentoring program was identified as one of several strategies that could be leveraged to address the high attrition, low career satisfaction, and obstacles encountered in the promotion process for UIM faculty, particularly early career faculty. Specifically, a mentoring program that explicitly addresses racism, biased practices, and evaluation structures that adversely impact UIM faculty was identified as a key solution. Institutional investment and structural accountability with concrete measures and resources to address historical and ongoing oppression and discrimination is required to support an antiracist and equity-minded mentoring program.
To address common but harmful experiences for UIM faculty, strategies were envisioned by BLNA faculty to create an innovative approach to a mentoring program that would: (1) be driven and developed by UIM faculty and non-UIM faculty allies, using an antiracist and intersectional lens to provide the tools and strategies to navigate UIM-specific barriers to success in academia; (2) credit, value, and monetarize the lived experience and expertise of UIM mid-career and senior medical faculty; (3) hold academic centers structurally accountable in taking steps to address the historic and ongoing oppression and discrimination of UIM faculty; and (4) formalize and institutionalize the program into a critical component of an academic medical center through the sustained investment of monetary and non-monetary resources. We hypothesize that expanding the number of culturally sensitive mentors, improving their visibilities, and enhancing skill development through an institutional initiative will benefit career development and strengthen the onramps and pathways toward promotion and retention of underrepresented and/or traditionally marginalized faculty. The long-term goal is to observe a longitudinal decrease in attrition of underrepresented and/or traditionally marginalized faculty, thereby expanding their overall representation and success at the associate and full professor levels.
The Justice, Equity, Diversity, and Inclusion Academic Mentors (JAM) Council at UCLA is a mentorship program designed to offer an intensive 1-year training program with extensive coaching in mentorship for UIM faculty in academic medicine. The JAM Council is anchored in building a sense of community, networking, and sponsorship opportunities for UIM faculty. The JAM Council targets mentees at the instructor and assistant professor levels who desire a sustainable and rewarding career in academic medicine and/or health leadership. In addition to offering traditional academic career development mentoring, the JAM Council program pairs early career UIM faculty with middle career and senior UIM and non-UIM allied faculty to curate a sense of belonging and connection by equipping them with the skills needed to explicitly navigate effects of racism, discrimination, and biased practices on their professional development and socialization within academic medicine. These include understanding and evaluating structural barriers that adversely impact UIM faculty.
Our conceptual model (see Figure 1) depicts how the JAM Council program aims to promote community building and belonging by connecting UIM faculty through a community of practice based on shared lived experience and intersectional identities. The program teaches UIM faculty how to navigate negative workplace climates, including experiences of discrimination and workplace isolation, the latter of which can result in a thwarted sense of belonging and lack of connectedness. Research has found that unequitable practices such as slower rates of promotion for UIM faculty, hostile workplace environments due to institutionalized racism and discrimination, and challenges finding effective mentorship are potent drivers of feelings of isolation, racial battle fatigue, and attrition (32–35) for faculty. Our goal is to increase retention and decrease attrition among UIM faculty, who are known to leave their institutions sooner at the assistant and associate professor level than their white colleagues, by specifically addressing belonging and promoting connectedness and inclusivity (19, 30). The white-UIM attrition gap is especially problematic given that UIM faculty are already severely underrepresented (36, 37) and face additional obstacles in academic structures, including workplace stress, distress of not fitting in, and imposter syndrome, which further exacerbate feeling unwanted in the workplace and social isolation (11, 26, 27). We posit that increasing creating affirming affinity spaces that enable connectedness based on shared racial and gendered minoritized statuses will help UIM faculty have a heightened sense of belonging and inclusion within their institutions and result in improved recruitment and retention of UIM faculty at various ranks.
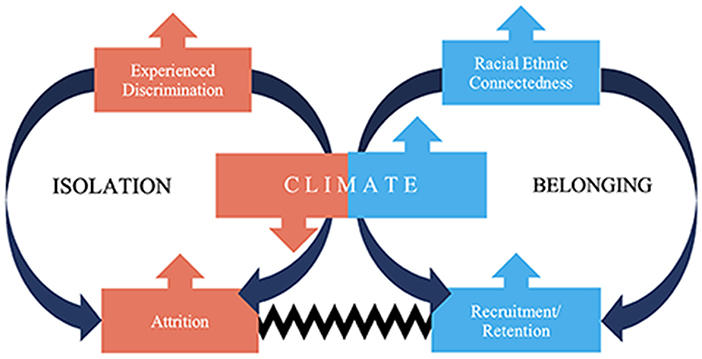
Figure 1. Model depicting how the JAM council can address negative workplace climates while promoting recruitment and retention, connectedness, and belonging.
The JAM Council is composed of mentors within senior faculty positions from the various UCLA academic series and medical specialties. Mentors will serve 3-year terms as advisors and leaders of mentorship teams that will support early career UIM faculty appointed to departments within the UCLA David Geffen School of Medicine (DGSOM). JAM Council mentors include a group of faculty who represent a breadth of disciplines (e.g., surgical, non-surgical, biobehavioral, basic science) and academic series (e.g., research, clinician-educator). Mentors must fulfill several predetermined competencies to be considered for the position and will report directly to the Vice Dean of Faculty with Ad Hoc reporting to the Vice Dean of Justice, Equity, and Diversity Inclusion at the DGSOM.
Mentors must commit to supporting the scholarly productivity of prospective mentees and facilitate the development and advancement of their career goals. In addition to their assigned departmental mentors distinct from the JAM program, JAM council mentors will assist faculty mentees in preparation and development of a portfolio of research, teaching, service, and/or other scholarly activities to support promotion through the ranks, and to navigate an institutional environment still mired in racism and sexism, macro and microaggressions, conscious and unconscious biases. Mentor positions will be compensated by the Dean's Office within the medical school, rather than individual departments or other funding sources, with a stipend payable to the individual mentor at 10% of 2021 NIH cap (including benefits) depending on available effort, not too dissimilar from a NIH K-24 award mechanism for mentoring.
There are several competencies and expectations for our JAM Council mentors (Table 1). Mentors must hold the rank of associate or full professor and must be supported by their Departmental leadership. The curriculum includes mentor training from National Research Mentoring Network, Center for the Improvement of Mentored Experiences in Research, as well as training in culturally responsive mentorship (20, 38). JAM Council mentors are responsible for: (1) providing personalized academic guidance and mentoring, (2) coordinating additional mentorship, sponsorship, and endorsement opportunities for UIM faculty from the time of their academic appointment, (3) assisting faculty mentees in preparation of a substantial portfolio of research, teaching, service, and other scholarly activities as needed for their series that will support promotion through the ranks, and (4) serving as a liaison with department promotion committee chairs to address any concerns about the dossier preparation.
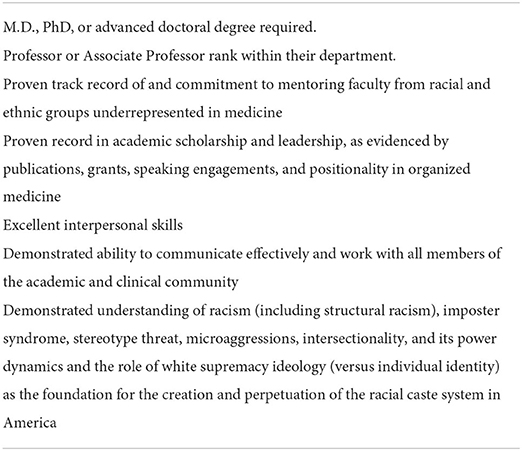
Table 1. Competencies required for Justice, Equity, Diversity, and Inclusion Academic Mentors (JAM) Council Mentors.
The responsibilities span from general faculty development to focused preparation for early career faculty with expanded teaching roles, and activities that support those pursuing advanced training as education leaders, researchers, master clinicians, public health leaders, and scholars. This role is supplemental to the required departmental/divisional responsibilities for faculty success. JAM council mentors will participate in monthly meetings with their assigned mentee, monthly meetings with their mentoring team, and quarterly meetings with JAM Council. Expected time commitment for JAM mentors is ~4 h per week but could be more depending on the number of mentees.
The JAM Council advisory board will select mentor applicants based on their availability to devote the time necessary to participate in the program and their experience in mentoring those who identify as historically underrepresented in medicine and/or with historically marginalized identities. Mentors' applications will include answering a series of questions in the following areas: (i) self-reflection on interpersonal strengths and weaknesses as a potential mentor, (ii) history of mentoring and mentoring facilitation and how they might apply those skills to the JAM Council program, (iii) self-reflection on navigating identity and intersectionality and how/if they have impacted their academic journey thus far (whether as a student, trainee or faculty), and (iv) how they have supported the academic or career development for UIM mentees. The JAM Council advisory board reviewed all applications with a rubric that ranks their applicant responses across these four domains.
All newly and recently appointed faculty at the instructor or assistant professor level are invited and eligible to apply as mentees to the program. Acceptance as a mentee into the JAM program is determined through an annual competitive selection process, in which ~20–25 candidates are chosen each year. Like the mentors, mentees are required to have the support of their departmental leadership. Mentees will participate in monthly seminars, monthly meetings with their assigned mentor and their mentoring cohort, and quarterly meetings with JAM Council advisory board. Expected time commitment for JAM mentees is estimated at ~4–6 h per month.
Similar to the process for selecting mentors, the JAM Council advisory board will select mentee applicants. Mentees will be evaluated based on their availability to devote the time necessary to participate in the program, overall career goals, and consideration of their experience in mentoring those who identify as historically underrepresented in medicine identities and/or with historical marginalized identities. Because one of the goals of the program is to expand workforce and build mentoring skills, consideration of mentee applicants' previous mentoring experience is included in application review. Mentee's applications included answering a series of questions in the following areas: (i) self-reflection on how they would benefit from the program, self-reflection on strengths and weakness and what they need to be successful in their current academic environment, (ii) scholarship and professional development goals, (iii) self-reflection on navigating identity and intersectionality and how/if they have impacted their academic journey thus far (whether as a student, trainee or faculty), and (iv) how they have been supported in the academic or career development as an underrepresented mentees. The JAM Council advisory board will review all applications with a rubric that ranks applicant responses across these four domains.
The JAM Council advisory board is a six-member group of multidisciplinary faculty from the UCLA DGSOM Justice, Equity, Diversity, and Inclusion Oversight Committee that serve multiple critical roles. Their roles include: (a) the selection of mentees and mentors, (b) developing the core curriculum for the academic year, (c) meeting with mentees and mentors on a semi-annual basis for feedback about the program, (d) establishing metrics of success and deliverables for the program, and (e) interfacing with decanal leadership regarding resource requirements and progress of the program.
Thematically, the overarching content of the JAM Council focuses on mentoring early career UIM faculty to navigate invisible and visible acts of racism in academia, creating racial and ethnic connectedness, and establishing a safeguard and form of advocacy for non-UIM who are unaware of or deny the presence of barriers for the retention of UIM faculty. The JAM council and its multiple components were intentionally created around four programmatic themes derived from a series of meetings driven by BLNA faculty members and supported by decanal leadership. These themes are as follows: (a) it takes a village: creating a team of sponsors and champions, (b) level setting with transparent expectations: learning the rules of the game, (c) building bias resistance and resilience, and (e) fostering community, through team-building practices that promote connectedness and interdependence (Table 2).
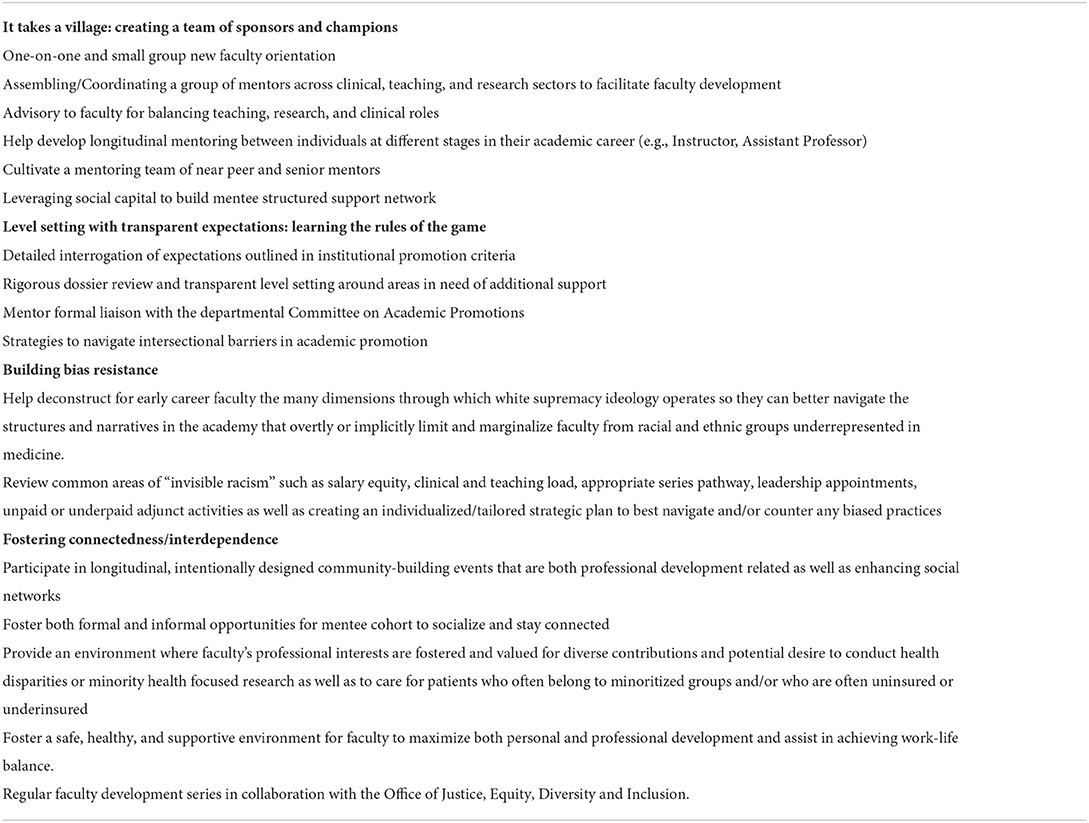
Table 2. Key programmatic themes of the Justice, Equity, Diversity, and Inclusion Academic Mentors (JAM) program.
The JAM Council is composed of a 16-session curriculum combined with individual, small team, and group mentoring delivered throughout the year (Table 3). The curriculum includes didactics, multimedia presentations, breakout sessions, group work, and role playing. Senior faculty mentors are part of a mentoring team with up to two to three mentees each. Early career mentees will be supported in a scholarly project that helps them develop and advance skills aligned with attaining their individual career goals. The JAM council curriculum addresses the following well-described threats to UIM faculty retention as well as key elements identified by the BLNA faculty group. Key curricular topics include but are not limited to: (a) the minority tax and service obligation—what it looks like and how to manage it; (b) promotion–important milestones and anticipating invisible criteria (e.g., the hidden curriculum) (39); (c) salary negotiations and personal wealth differential; (d) sponsorship; (e) intersectionality, isolation, code-switching, stereotype threat, and imposter syndrome; (f) gate blocking—anticipating biased, institutional factors at various levels of your career; and (g) negotiating equity in clinical spaces for UIM faculty. For example, UIM are more likely to care for financially marginalized patients (40), and also generate less income than their white counterparts (41). Although this fulfills institutional commitments to address health equity, this often results in lower compensation despite providing mission critical care that is more time-intensive.
Measurement tools specifically designed to evaluate formal mentorship programs in academic settings will be used. Because the goal of the JAM Council is to explicitly address the effects of racism, biased practices, and structures that adversely impact UIM faculty, in addition to traditional outcome measures such as career satisfaction, attrition and length to promotion, measurement of minority tax burden, belonging, connectedness, wellbeing, and impostor syndrome will be conducted. Evaluations will be conducted at multiple time points and include mixed methods of qualitative and quantitative measures with the goal of generating a holistic perspective to provide robust assessment of program processes, outcomes and lessons learned (20, 21).
In most institutions, there are few programs designed to increase diverse faculty in academic medicine with insufficient or incomplete mentorship available to early career UIM faculty (13, 15). While many institutions have adopted mentoring programs of some type, there remains a lack of mentorship for UIM faculty that is inclusive and equitable, culturally responsive, and anti-racist in explicitly addressing historic and ongoing aspects of racism (internalized, interpersonal, and structural). Also lacking are strategies on how to best cope with these same issues outside of the academic institution that further impact faculty wellness and productivity. Thus, the JAM Council was designed to leverage the experience and wisdom of senior UIM faculty to positively impact promotion, retention, and career satisfaction of early career UIM colleagues and to recognize and address the complex interaction of these factors.
In recognition of this critical need, the BLNA secured institutional support and commitment to the monetary and non-monetary resources necessary to conduct this activity. Institutional support has been repeatedly cited as a way to sustain mentorship programs, so they become embedded within academic health centers (13, 25). Institutional support is imperative to dismantling racism in medicine and academic by supporting programs and efforts that explicitly work against exclusionary practices that unfairly advantage white faculty by hiring, promoting, assigning higher value to their work, and enabling access to resources while disadvantaging UIM faculty (19, 25, 42, 43). Thus, by leveraging the power and privilege embedded in a predominately white institution to change the academic climate to be more supportive of advancement and productivity of UIM faculty the JAM Council fosters greater justice, equity, diversity, and inclusion (25, 44).
To ensure the success of the program, we have considered addressing structural and institutional threats that UIM faculty face over their academic careers. The first threat directly relates to the lack of racial and ethnic representation in academia. Given the consistently low number of UIM faculty in most academic settings, it is highly likely that their colleagues and administration will be of a differing race and/or ethnicity, and belong to a dominant group with conscious and unconscious negative biases toward the UIM faculty. This discordance has the potential to produce strained cross-cultural communications, due to differing lived experiences as well as professional and social frames of references. This can result in the UIM faculty member lacking the social connections necessary to build the supportive and collaborative environment needed to succeed in academia. Negative workplace environments and resultant social isolation can have a profound impact on mental wellness and ultimately academic productivity (45, 46).
The JAM Council was intentionally designed to counteract the threats posed by the lack of diversity and representation in academic medicine. The social isolation and lack of sense of belonging experienced by UIM faculty in academic medicine can have detrimental impact on their overall health, career progression, and success (27, 48–50). By ensuring that some mentors are also UIM faculty, we are attempting to bridge potential cross-cultural communication divides to facilitate trusted relationship rooted in the shared experience of membership in historically marginalized racial and ethnic groups in our racialized society. This racial concordance portends a lower likelihood of assumptions based on stereotypes, bias, or prejudice, thus allowing for a more genuine and trusted relationship (47). In fact, we posit that the connections formed by the JAM Council can serve as a form of bias resistance that can build bias resilience, both individually and as a collective. A unique aspect of the mentoring program will be its ability to promote racial and ethnic connectedness, and collectivism through a shared learning community.
It is important to highlight that although a goal of the JAM council is to build community and promote connections among UIM faculty mentors and early career/junior faculty scholars, the JAM Council program also includes non-UIM faculty mentors, who are equally pivotal to its successful implementation and sustainability. An overarching goal of the JAM Council program is to enhance workforce development and capacity in the area of inclusive and culturally mentoring practices, with an emphasis on groups who identify as UIM and/or have historically marginalized identities. The JAM Council program's curriculum intentionally embeds antiracism, and culturally responsive and informed mentoring techniques in its implementation (20). These include but are not limited to creating shared learning space where both mentor and mentees reflecting on their positionality along axes of power and privilege (20), and anchoring the program within historical context of understanding structural racism and bias in academy. Examples include using vignettes and videos to create reflective dialogue and role playing to address microaggressions.
The JAM Council may also catalyze research that advances health equity and potentially increase successful grant funding for UIM researchers. This may be especially salient given that prior research has shown that topic choice contributes to the significantly lower rate of NIH awards to African American/Black scientists compared to their white colleagues (31, 47). Further, funded UIM research scientists are more likely to conduct research that centers UIM communities. Their mentorship may lead to increases in funding for early career colleagues that share a research interest relevant to their community but may not understand the nuances of NIH and other study sections around funding priorities within the space of health equity research (13, 47).
Although we expect the JAM Council to significantly enhance justice, equity, diversity, and inclusion efforts within our institution, there are potential challenges and limitations with this nascent program. Due to limitations in resources and available mentors, a finite number of mentee positions are available. Presently, there is no other program available to early career faculty that are not selected for the mentorship program. Lastly, there are a relatively small number of senior UIM faculty available to participate as mentors. This potential concern is manifested in two distinct ways: (a) the program could add to the minority tax burden already carried by most of the senior UIM faculty; and (b) the need for a breadth of clinical disciplines and academic series among the senior mentors may be difficult to achieve with a relatively small number of mentors. These concerns are partially mitigated by decreasing the percentage effort required for the mentors, as well as including some non-UIM senior faculty to serve as senior mentors and add additional clinical discipline and academic series diversity.
Enhancing retention of UIM faculty hinges upon improving positioning for leadership and advancement pathways, and this requires mentorship, sponsorship, and coaching that are institutionally supported and championed. Inadequate time and support must be addressed for UIM faculty to mitigate minority tax and other systemic barriers to provide and receive the critical guidance for producing the scholarship and innovation required for promotion (25, 49, 50). This requires true institutional commitment, from recognition of the problem to supplying the needed support and resources for programmatic success. This is not something that arises de novo within an institution and is unlikely to happen if championed by only a few faculty. The BLNA faculty collective sent a strong message to (a) identify the problem, (b) provide rationale for the solution, and (c) underscore likely outcomes of no action and action and were supported by executive and decanal leadership to operationalize this program. Fortunately, the JAM Council program has received significant support, resources, and executive sponsorship from the Dean's office who have included the JAM Council's program within their larger program of antiracism and addressing systemic racism across the medical school and health system. The JAM Council was co-created by the executive leadership in the Dean's office and has multiple touchpoints with the Deans of JEDI and the Deans for faculty, the latter of which are specifically attuned the requirements for advancement and promotion. The Dean's office has provided vital and necessary support which includes dedicated administrative staff, protected time for senior faculty to administer the program, space for holding in person meetings, IT support, public announcements, and resources (e.g., space, food, technology, and scheduling support) for hosting community building events. Broad dissemination by the Dean's office describing the program's significance and purpose has been an important part of the implementation strategy and buy-in has been communicated across the decanal and administrative structure. Updates on the JAM Council Program's progress will be embedded in standing executive meetings. This support is an essential element that reflect the institution's overall commitment to addressing structural racism and underscore their investment and buy-in to the process at the most senior ranks. It is important to note that the JAM Council is also launching within the medical school's larger Antiracism Roadmap, an overarching planned commitment to create structural accountability in antiracism in academic medicine. This includes but is not limited to updated guidelines to address bias and discrimination in the workplace and learning environment.
While it seems implicit, it can be challenging for majority groups to understand the isolation of marginalized and underrepresented groups in the same environment, let alone appreciate the need for community building. BLNA recognized that community is the cure for this isolation. Thus, there is a high need for community and affinity group spaces to be cultivated for UIM faculty within the academic medicine institutional environment. While affinity group spaces exist, they are not well recognized or structurally enfranchised. For instance, there may be research communities, including clinical research or global research, or education communities where people with shared needs come together. Doing the same for people of shared racial/ethnic identities is often labeled as reverse racism when in fact it is a response to implicit and explicit racism and discrimination that the majority are either unaware of or refuse to acknowledge. The implementation of the JAM Council will hopefully push the field of mentoring and anti-racism in medicine forward using an existing but unrecognized approach of cultivating microenvironments dedicated to faculty success. The JAM Council's evaluation will hopefully move such programs beyond perspective pieces by applying them and putting them into action.
The original contributions presented in the study are included in the article/supplementary materials, further inquiries can be directed to the corresponding author/s.
EPB, CH, KB, AG, and KN contributed to conception and design of the article. EPB, CH, KB, AG, SMG, and KN wrote the first draft of the manuscript. All authors contributed to manuscript revision, read, and approved the submitted version.
Funds for Open Access publication fees were received from UCLA DGSOM office of JEDI.
The authors are grateful for the support of the UCLA David Geffen School of Medicine Black Latinx Native American Faculty Collective for their thought partnership and the Office of the Dean at the UCLA David Geffen School of Medicine, and mentors and mentees of the JAM Council. The authors wish to specifically thank Ms. Isadora Avendano for her administrative support at all stages to operationalize the program and ensure its successful launch. The authors wish to thank to Drs. Clarence Braddock, Steve Dubinett, Jonathan Hiatt, Kelsey Martin, Emilie Markus, David McIntosh, and Anja Paardekooper for their executive sponsorship and thought partnership. The authors also thank Ms. Georgia Perris for editorial assistance.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Krieger N. Enough: COVID-19, structural racism, police brutality, plutocracy, climate change-and time for health justice, democratic governance, and an equitable, sustainable future. Am J Public Health. (2020) 110:1620–3. doi: 10.2105/AJPH.2020.305886
2. Paine L, de la Rocha P, Eyssallenne AP, Andrews CA, Loo L, Jones CP, et al. Declaring racism a public health crisis in the United States: cure, poison, or both? Front Public Health. (2021) 9:676784. doi: 10.3389/fpubh.2021.676784
3. O'Reilly KB. Racism is a Threat to Public Health. Chicago, IL: American Medical Association (2020).
4. Collins FS. NIH Stands Against Structural Racism in Biomedical Research. Bethesda: National Institutes of Health. (2021).
5. Wilkins CH, Williams M, Kaur K, DeBaun MR. Acad Med's journey toward racial equity must be grounded in history: recommendations for becoming an antiracist academic medical center. Acad Med J Assoc Am Med Coll. (2021) 96:1507–12. doi: 10.1097/ACM.0000000000004374
6. Association of American Medical Colleges (AAMC). Faculty roster: U.S. medical school faculty. (2019). Available online at: https://www.aamc.org/data-reports/faculty-institutions/report/faculty-roster-us-medical-school-faculty (accessed on June 6, 2022).
7. Ogunyemi D, Okekpe CC, Barrientos DR, Bui T, Au MN, Lamba S. United States Medical School Academic Faculty Workforce Diversity, Institutional Characteristics, and Geographical Distributions From 2014-2018. Cureus. (2022) 14:e22292. doi: 10.7759/cureus.22292
8. Schor NF. The decanal divide: women in decanal roles at US medical schools. Acad Med. (2018) 93:237–40. doi: 10.1097/ACM.0000000000001863
9. Acosta DA, Poll-Hunter NI. Diversity and inclusion in the Acad Med workforce. In:Sanchez JP, , editor. Succeeding in Acad Med. Switzerland: Springer, Cham (2020). p.1–14
10. Eckstrand KL, Eliason J, St Cloud T, Potter J. The priority of intersectionality in Acad Med. Acad Med. (2016) 91:904–7. doi: 10.1097/ACM.0000000000001231
11. Wingard D, Trejo J, Gudea M, Goodman S, Reznik V. Faculty equity, diversity, culture and climate change in Acad Med: a longitudinal study. J Natl Med Assoc. (2019) 111:46–53. doi: 10.1016/j.jnma.2018.05.004
12. Bonifacino E, Ufomata EO, Farkas AH, Turner R, Corbelli JA. Mentorship of underrepresented physicians and trainees in Acad Med: a systematic review. J Gen Intern Med. (2021 A) 36:1023–34. doi: 10.1007/s11606-020-06478-7
13. Beech BM, Calles-Escandon J, Hairston KG, Langdon MS, Latham-Sadler BA, Bell RA. Mentoring programs for underrepresented minority faculty in academic medical centers: a systematic review of the literature. Acad Med. (2013) 88:541–9. doi: 10.1097/ACM.0b013e31828589e3
14. Daley SP, Broyles SL, Rivera LM, Brennan JJ, Lu ER, Reznik V, et al. conceptual model for faculty development in academic medicine: the underrepresented minority faculty experience. J Natl Med Assoc. (2011) 103:816–21. doi: 10.1016/S0027-9684(15)30435-1
15. Gutierrez-Wu J, Lawrence C, Jamison S, Wright ST, Steiner MJ, Orr CJ. An evaluation of programs designed to increase representation of diverse faculty at academic medical centers. J Natl Med Assoc. (2022) 114:278–89. doi: 10.1016/j.jnma.2022.01.012
16. Association of American Medical Colleges. Assessing Institutional Culture and Climate Webcast Supplemental Guide. (2013). Available online at: https://www.aamc.org/media/21031/download (accessed on June 6, 2022).
17. Efstathiou JA, Drumm MR, Paly JP, Lawton DM, O'Neill RM, Niemierko A, et al. Long-term impact of a faculty mentoring program in academic medicine. PLoS ONE. (2018) 13:e0207634. doi: 10.1371/journal.pone.0207634
18. Orr CJ, McLaurin-Jiang S, Jamison SD. Diversity of mentorship to increase diversity in academic pediatrics. Pediatrics. (2021) 147:e20193286. doi: 10.1542/peds.2019-3286
19. Zambrana RE, Ray R, Espino MM, Castro C, Douthirt Cohen B, Eliason J. “Don't leave us behind” The importance of mentoring for underrepresented minority faculty. Am Educ Res J. (2015 F) 52:40–72. doi: 10.3102/0002831214563063
20. Wyatt GA, Chin D, Milburn N, et al. Mentoring the mentors of students from diverse backgrounds for research. Am J Orthopsychiatry. (2019) 89:321–8. doi: 10.1037/ort0000414
21. Trejo JA, Wingard D, Hazen V, et al. A system-wide health sciences faculty mentor training program is associated with improved effective mentoring and institutional climate. J Clin Transl Sci. (2021) 6:E18. doi: 10.1017/cts.2021.883
22. Kalet A, Libby AM, Jagsi R, Brady K, Chavis-Keeling D, Pillinger MH, et al. Mentoring underrepresented minority physician-scientists to success. Acad Med. (2022) 97:497–502. doi: 10.1097/ACM.0000000000004402
23. Amaechi O, Foster KE, Tumin D, Campbell KM. Addressing the gate blocking of minority faculty. J Natl Med Assoc. (2021) 113:517–21. doi: 10.1016/j.jnma.2021.04.002
24. Rodríguez JE, Campbell KM, Pololi LH. Addressing disparities in academic medicine: what of the minority tax? BMC Med Educ. (2015) 15:1–5. doi: 10.1186/s12909-015-0290-9
25. Rodríguez JE, Tumin D, Campbell KM. Sharing the power of white privilege to catalyze positive change in Acad Med. J Racial Ethnic Health Disparities. (2021) 8:539–42. doi: 10.1007/s40615-020-00947-9
26. Aguirre A. Women and Minority Faculty in the Academic Workplace: Recruitment, Retention, and Academic Culture. ASHE-ERIC Higher Education Report, Volume 27, Number 6. Jossey-Bass Higher and Adult Education Series. Jossey-Bass, 350 Sansome St., San Francisco, CA 94104-1342 (2000).
27. Zambrana RE, Harvey Wingfield A, Lapeyrouse LM, Dávila BA, Hoagland TL, Valdez RB. Blatant, subtle, and insidious: URM faculty perceptions of discriminatory practices in predominantly White institutions. Sociol Inq. (2017) 87:207–32. doi: 10.1111/soin.12147
28. Embrick DG, Dominguez S, Karsak B. More than just insults: rethinking sociology's contribution to scholarship on racial microaggressions. Sociol Inq. (2017) 87:193–206. doi: 10.1111/soin.12184
29. Borlik MF, Godoy SM, Wadell PM, Petrovic-Dovat L, Cagande CC, Hajirnis A, et al. Women in academic psychiatry: Inequities, barriers, and promising solutions. Acad Psychiatry. (2021) 45:110–9. doi: 10.1007/s40596-020-01389-5
30. Liu CQ, Alexander H. Promotion rates for first-time assistant and associate professors appointed from 1967 to 1997. AAMC Anal Brief. (2010) 9:9–10. doi: 10.1089/jwh.2015.5608
31. Ginther DK, Schaffer WT, Schnell J, Masimore B, Liu F, Haak LL, et al. Race, ethnicity, and NIH research awards. Science. (2011) 333:1015–9. doi: 10.1126/science.1196783
32. Hardeman RR, Murphy KA, Karbeah JM, Kozhimannil KB. Naming institutionalized racism in the public health literature: a systematic literature review. Public Health Rep. (2018) 133:240–9. doi: 10.1177/0033354918760574
33. Nunez-Smith M, Curry LA, Bigby J, Berg D, Krumholz HM, Bradley EH. Impact of race on the professional lives of physicians of African descent. Ann Intern Med. (2007) 146:45–51. doi: 10.7326/0003-4819-146-1-200701020-00008
34. Nunez-Smith M, Ciarleglio MM, Sandoval-Schaefer T, Elumn J, Castillo-Page L, Peduzzi P, et al. Institutional variation in the promotion of racial/ethnic minority faculty at US medical schools. Am J Public Health. (2012) 102:852–8. doi: 10.2105/AJPH.2011.300552
35. Spence JP, Buddenbaum JL, Bice PJ, Welch JL, Carroll AE. Independent investigator incubator (I3): a comprehensive mentorship program to jumpstart productive research careers for junior faculty. BMC Med Educ. (2018) 18:1–1. doi: 10.1186/s12909-018-1290-3
36. Lett E, Orji WU, Sebro R. Declining racial and ethnic representation in clinical academic medicine: a longitudinal study of 16 US medical specialties. PLoS ONE. (2018) 13:e0207274. doi: 10.1371/journal.pone.0207274
37. Xierali IM, Nivet MA, Rayburn WF. Full-time faculty in clinical and basic science departments by sex and underrepresented in medicine status: a 40-year review. Acad Med. (2021) 96:568–75. doi: 10.1097/ACM.0000000000003925
38. Javier D, Stinson K, Zavala M, Ahmed T, Vishwanatha JK. NRMNet: Building a national resource for mentorship, networking and professional development to enhance diversity. Ethn Dis. (2021) 31:469. doi: 10.18865/ed.31.3.469
39. Sarikhani Y, Shojaei P, Rafiee M, Delavari S. Analyzing the interaction of main components of hidden curriculum in medical education using interpretive structural modeling method. BMC Med Educ. (2020) 20:1–9. doi: 10.1186/s12909-020-02094-5
40. Komaromy M, Grumbach K, Drake M, Vranizan K, Lurie N, Keane D, et al. The role of black and Hispanic physicians in providing health care for underserved populations. N Engl J Med. (1996) 334:1305–10. doi: 10.1056/NEJM199605163342006
41. Toretsky C, Mutha S, Coffman J. Breaking Barriers for Underrepresented Minorities in the Health Professions. University of California San Francisco: Healthforce Center (2018).
42. Romano MJ. White privilege in a white coat: how racism shaped my medical education. Ann Family Med. (2018) 16:261–3. doi: 10.1370/afm.2231
43. Alang S, Hardeman R, Karbeah JM, Akosionu O, McGuire C, Abdi H, et al. White supremacy and the core functions of public health. Am J Public Health. (2021) 111:815–9. doi: 10.2105/AJPH.2020.306137
44. Krieger N, Boyd RW, De Maio F, Maybank A. Medicine's privileged gatekeepers: producing harmful ignorance about racism and health. Health Affairs Blog. (2021) 10. doi: 10.1377/forefront.20210415.305480
45. Pololi L, Cooper LA, Carr P. Race, disadvantage and faculty experiences in academic medicine. J Gen Intern Med. (2010) 25:1363–9. doi: 10.1007/s11606-010-1478-7
46. Hardeman RR, Przedworski JM, Burke S, Burgess DJ, Perry S, Phelan S, et al. Association between perceived medical school diversity climate and change in depressive symptoms among medical students: a report from the medical student CHANGE study. J Natl Med Assoc. (2016) 108:225–35. doi: 10.1016/j.jnma.2016.08.005
47. Yehia BR, Cronholm PF, Wilson N, Palmer SC, Sisson SD, Guilliames CE, et al. Mentorship and pursuit of Acad Med careers: a mixed methods study of residents from diverse backgrounds. BMC Med Educ. (2014) 14:1–8. doi: 10.1186/1472-6920-14-26
48. Holloway-Friesen H. The role of mentoring on Hispanic graduate students' sense of belonging and academic self-efficacy. J Hispanic High Educ. (2021) 20:46–58. doi: 10.1177/1538192718823716
49. Coe C, Piggott C, Davis A, Hall M, Goodell K, Joo P, et al. Leadership pathways in academic family medicine: focus on underrepresented minorities and women. Fam Med. (2020) 52:104–11. doi: 10.22454/FamMed.2020.545847
Keywords: mentoring, academic medicine, underrepresented in medicine (UIM), diversity equity and inclusion (DEI), antiracism
Citation: Bath EP, Brown K, Harris C, Guerrero A, Kozman D, Flippen CC II, Garraway I, Watson K, Holly L, Godoy SM, Norris K and Wyatt G (2022) For us by us: Instituting mentorship models that credit minoritized medical faculty expertise and lived experience. Front. Med. 9:966193. doi: 10.3389/fmed.2022.966193
Received: 20 July 2022; Accepted: 27 September 2022;
Published: 21 October 2022.
Edited by:
Kathryn Toy Knecht, Loma Linda University, United StatesReviewed by:
Elizabeth Walker, Emory University, United StatesCopyright © 2022 Bath, Brown, Harris, Guerrero, Kozman, Flippen, Garraway, Watson, Holly, Godoy, Norris and Wyatt. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sarah M. Godoy, c2dvZG95QGVtYWlsLnVuYy5lZHU=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.