
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Med. , 04 August 2022
Sec. Intensive Care Medicine and Anesthesiology
Volume 9 - 2022 | https://doi.org/10.3389/fmed.2022.938005
This article is part of the Research Topic Clinical Teaching and Practice in Intensive Care Medicine and Anesthesiology View all 17 articles
 Ata Mahmoodpoor‡1*†
Ata Mahmoodpoor‡1*† Sarvin Sanaie‡1†
Sarvin Sanaie‡1† Seied Hadi Saghaleini‡2
Seied Hadi Saghaleini‡2 Zohreh Ostadi‡2
Zohreh Ostadi‡2 Mohammad-Salar Hosseini‡3
Mohammad-Salar Hosseini‡3 Naeeme Sheshgelani‡3
Naeeme Sheshgelani‡3 Amir Vahedian-Azimi‡4
Amir Vahedian-Azimi‡4 Abbas Samim‡5
Abbas Samim‡5 Farshid Rahimi-Bashar‡6*
Farshid Rahimi-Bashar‡6*Background: Modified Early Warning Score (MEWS) and National Early Warning Score (NEWS) are widely used in predicting the mortality and intensive care unit (ICU) admission of critically ill patients. This study was conducted to evaluate and compare the prognostic value of NEWS and MEWS for predicting ICU readmission, mortality, and related outcomes in critically ill patients at the time of ICU discharge.
Methods: This multicenter, prospective, observational study was conducted over a year, from April 2019 to March 2020, in the general ICUs of two university-affiliated hospitals in Northwest Iran. MEWS and NEWS were compared based on the patients’ outcomes (including mortality, ICU readmission, time to readmission, discharge type, mechanical ventilation (MV), MV duration, and multiple organ failure after readmission) using the univariable and multivariable binary logistic regression. The receiver operating characteristic (ROC) curve was used to determine the outcome predictability of MEWS and NEWS.
Results: A total of 410 ICU patients were enrolled in this study. According to multivariable logistic regression analysis, both MEWS and NEWS were predictors of ICU readmission, time to readmission, MV status after readmission, MV duration, and multiple organ failure after readmission. The area under the ROC curve (AUC) for predicting mortality was 0.91 (95% CI = 0.88–0.94, P < 0.0001) for the NEWS and 0.88 (95% CI = 0.84–0.91, P < 0.0001) for the MEWS. There was no significant difference between the AUC of the NEWS and the MEWS for predicting mortality (P = 0.082). However, for ICU readmission (0.84 vs. 0.71), time to readmission (0.82 vs. 0.67), MV after readmission (0.83 vs. 0.72), MV duration (0.81 vs. 0.67), and multiple organ failure (0.833 vs. 0.710), the AUCs of MEWS were significantly greater (P < 0.001).
Conclusion: National Early Warning Score and MEWS values of >4 demonstrated high sensitivity and specificity in identifying the risk of mortality for the patients’ discharge from ICU. However, we found that the MEWS showed superiority over the NEWS score in predicting other outcomes. Eventually, MEWS could be considered an efficient prediction score for morbidity and mortality of critically ill patients.
Readmission to the intensive care units (ICUs) is associated with poor patient outcomes, including higher mortality, a longer length of stay, and higher adverse event rates (1–3). In addition, ICU readmissions bring financial burden and wastefulness to the patient flow of the healthcare system (4, 5). Readmitted patients reduce ICU bed availability and, probably, the efficiency of the ICU facilities (6, 7). The intensivist usually decides to discharge patients from the ICU based on clinical evaluations (8, 9). However, several other non-clinical factors contribute to such decisions – including the high demand and need for ICU beds by emergency and surgical departments – making the discharge decision a complex, challenging, and risky care transfer process (10, 11). These factors may lead to an early and inadequate discharge of patients, which increases the risk of readmission, as up to 42% of patients discharged early are eventually readmitted to the ICU (12). Hence, several attempts have been made to optimize and prioritize ICU discharges, either by identifying risk factors associated with ICU readmission (9, 13) or developing readmission prediction models (14, 15). These models for mortality and readmission after ICU discharge have shown diverse accuracy. Although prospective validation is warranted for these scoring systems, they speculate that these models could be valuable assistance to clinicians for ICU discharge planning.
Several Early Warning Scores (EWSs) with different designs have been developed to diagnose early signs of deterioration in a patient’s conditions and initiate further medical care and possible ICU admission (16–18). Since a critical state usually follows specific deteriorations in the patient’s physiological signs, monitoring these signs could help the physicians predict the patient’s outcomes (19–21). One of the common EWSs is the Modified Early Warning Score (MEWS), validated in 2001 in the United Kingdom as a bedside tool to identify patients at risk for catastrophic events, including death or readmission to ICU (22). National Early Warning Score (NEWS) is another EWS introduced in 2012 by the Royal College of Physicians (23). The NEWS score identifies the patients at risk of deterioration and facilitates prompt critical care intervention. Also, many studies have shown the capability of NEWS in predicting the degree of illness (18, 24). Several studies have explored the association between these risk scores and hospital admission. The findings suggest that these risk scores could also be used as triage tools to identify patients requiring hospital admission (22, 25, 26).
Due to the lack of studies comparing NEWS and MEWS risk-scoring systems in ICU settings, it is still unclear which risk-scoring system is superior as a triage tool for ICU readmission and predicting mortality of critically ill patients. Considering the lack of information and the inconsistency in the cut-off values, this study was conducted to evaluate and compare the prognostic value of NEWS and MEWS for predicting ICU readmission, mortality, and related outcomes in critically ill patients at the time of ICU discharge.
This multicenter, prospective, observational study was conducted over a year, from April 2019 to March 2020, in the general intensive care units (ICUs) of two university-affiliated hospitals in Northwest Iran, to evaluate and compare the prognostic value of NEWS and MEWS scores for predicting ICU readmission, mortality and related outcomes in critically ill patients at the time of discharge from the ICU. All adult (over 18 years old) patients alive at the time of ICU discharge were eligible to enroll in this study, regardless of the medical diagnoses and underlying comorbidities. However, patients were excluded if they were: (a) stayed in the ICU for less than 48 h (such as postoperative patients), (b) patients directly discharged home or transferred to other medical centers, (c) patients discharged for palliative care, and (d) patients readmitted to the ICU for the second time. Patients who no longer needed mechanical ventilation (MV), vasopressor support, and renal replacement therapies were discharged from the ICU with appropriate levels of consciousness and transferred to general wards. Subsequently, all patients were followed up for 2 weeks to identify readmitted patients.
The protocol study was reviewed and approved by the Research Ethics Committees of Islamic Azad University-Tabriz Branch (IR.TBZMED.REC.1397.994), following the Declaration of Helsinki of the World Medical Association (27). Written informed consent was obtained from the patients or their legally accepted representatives. In addition, the study was conducted and reported in accordance with the recommendations of the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement (28).
Demographic characteristics and clinical data, including comorbidities, reasons for admission (medical, surgical, or emergency), the severity of illness [based on Acute Physiology and Chronic Health Evaluation IV (APACHE-IV) and Sequential Organ Failure Assessment (SOFA) scores], consciousness state, and vital signs (respiratory rate, peripheral oxygen saturation (SpO2), systolic/diastolic blood pressure, heart rate, pulse rate, and body temperature) upon ICU admission were recorded for all patients. Additionally, we collected the information, including the status and type of multiple organ failure, mechanical ventilation (MV) status, MV duration, length of stay (LOS) in the ICU, and the NEWS and MEWS scores at the time of ICU discharge. All data were collected and analyzed by researchers completely independent of the clinical decision-makers.
A trained nurse calculated the NEWS and MEWS scores for all patients who were alive at the time of ICU discharge using physiological parameters. NEWS scores were obtained by nursing staff at the ICUs, including the following seven common vital signs parameters: Respiratory rate (RR), peripheral oxygen saturation (SpO2) measured by pulse oximetry, supplementary oxygen, systolic arterial blood pressure (SBP), pulse rate (PR), body temperature (T), and AVPU (Alert, responds to Voice, responds to Pain, Unresponsive) score based on the Glasgow Coma Scale (GCS) [The AVPU score was derived from the GCS as follows: A = 14–15, V = 9–13, P = 4–8, U = 3] (29). Patients with a score between 0 and 4 are considered low risk, those with a score of 5 or 6 are considered medium risk, and patients with a score ≥ 7 are considered high risk (29). The MEWS consists of five physiological variables, including systolic blood pressure (SBP), heart rate (HR), respiratory rate (RR), body temperature (T), and AVPU score based on the GCS. Determining a MEWS score involves assigning a number between 0 and 3 to each of the six vital signs. Patients with scores between 2 and 4 are considered at medium risk and should remain under specialized care and be assessed again in 2 to 8 h. Those with a score ≥ 5 are considered at high risk for mortality and being moved to ICU (22).
The primary outcomes were mortality and readmission to the ICU. The secondary outcomes were the type of discharge from ICU and subgroups of consequences related to the readmission, such as mechanical ventilation, duration of mechanical ventilation, and multiple organ failure.
Data were expressed as mean ± standard division (SD) or median with interquartile range (IQR) for continuous variables, and frequencies with percentages (%) for categorical characteristics. The Shapiro-Wilk test was used to determine whether data were normally distributed. To compare the NEWS and MEWS scores according to the outcomes and subgroups of outcomes, we used Mann–Whitney as a non-parametric test for non-normal distributions. Univariate and multivariate binary logistic regression analyses were performed to evaluate associations of NEWS and MEWS scores with the outcomes. Each variable was first tested by univariate analysis with odds ratios (OR) and 95% confidence intervals (95% CI). In multivariate analysis, based on conditional logistic regression, variables with a p-value < 0.05 in the univariate analyses were proposed for entry into the model. To assess the predictive prognostic efficacy of the NEWS and MEWS scores, we performed receiver operating characteristic (ROC) curves and calculated the area under the curves (AUC). AUC figures were calculated alongside sensitivity (SN), specificity (SP), positive likelihood ratio (LR +), negative likelihood ratio (LR-), positive predictive value (PPV), negative predictive value (NPV), and Youden index to find appropriate cut-offs. In addition, we compared the ROC of NEWS and MEWS scores using the DeLong test. According to the general guide, AUC between (0.9-1.0), (0.8-0.9), (0.7-0.8), and (0.6-0.7) was considered as excellent, good, fair, and poor, respectively. Statistical analysis was performed using SPSS Statistics 21.0 (SPSS Inc., Chicago, IL, United States) and MedCalc.1 In all analyses, p-values less than 0.05 were considered significant.
In total, 410 patients were selected for this study. The basic information and clinical characteristics of the patient population are listed in Table 1. The median age (IQR) of the patients was 59 (49.75–69) years, and 223 (56.8%) patients were male. Nearly half of the patients (n = 185, 45.1%) had comorbidities, and 25 (6.1%) had more than two underlying diseases. The most common reason of admission was surgical (n = 272, 66.3%) followed by medical (n = 102, 24.9%) and emergency (n = 36, 8.8%). The median (IQR) of APACHE IV and SOFA scores of the patients were 23.5 (21–26) and 9 (6–13.25), respectively. More than half of patients had multiple organ failure (n = 286, 69.8%) and underwent MV (n = 273, 66.6%). The median (IQR) length of stay in the ICU and MV duration were 9 (6–13.25) and 8 (5–12) days, respectively.
A total of 50 (12.2%) ICU patients discharged to the general ward were readmitted within 2 to 12 days, with a median (IQR) time of 4 (3–4) days. Clinical characteristics of readmitted patients and the main reasons for readmission are presented in Table 2. Of 50 patients readmitted to the ICU, 39 (78%) underwent MV. The median (IQR) MV duration in readmitted patients was 6 (5–6) days. Organ failure was present in 48 (96%) readmitted patients.
Table 3 presents the detailed comparison of NEWS and MEWS scores among the patients regarding mortality, type of discharge, readmission, time to readmission, MV status, MV duration, and organ failure after readmission. Comparing NEWS and MEWS scores between outcomes showed statistically significant differences, as the median scores of NEWS and MEWS were significantly higher in non-survivors, readmitted patients, patients with lower (<4) days to readmission, those who underwent MV, patients with higher (≥6) days of MV, and patients with multiple organ failure. However, no significant differences were observed between median scores of NEWS (p-value = 0.332) and MEWS (p-value = 0.447) in the patients with planned and unplanned types of discharge.
Tables 4, 5 present the univariable and multivariable binary logistic regression analyses to evaluate associations of NEWS and MEWS scores to predict outcomes. In univariable analysis, an increase in mortality risk was observed in a higher NEWS score (OR: 18.58, 95% CI: 8.45–40.86, p-value < 0.001) and MEWS score (OR: 12.19, 95% CI: 6.43–23.11, p-value < 0.001). However, multivariable analysis showed that the higher NEWS was only associated with mortality (OR: 6.51, 95% CI: 1.81–23.43, p-value = 0.004). In addition, the multivariable binary logistic regression model identified that the higher NEWS and MEWS scores upon discharge were associated with readmission, lower time to readmission, the risk of undergoing MV after readmission, higher MV duration, and the risk of multiple organ failure after readmission.
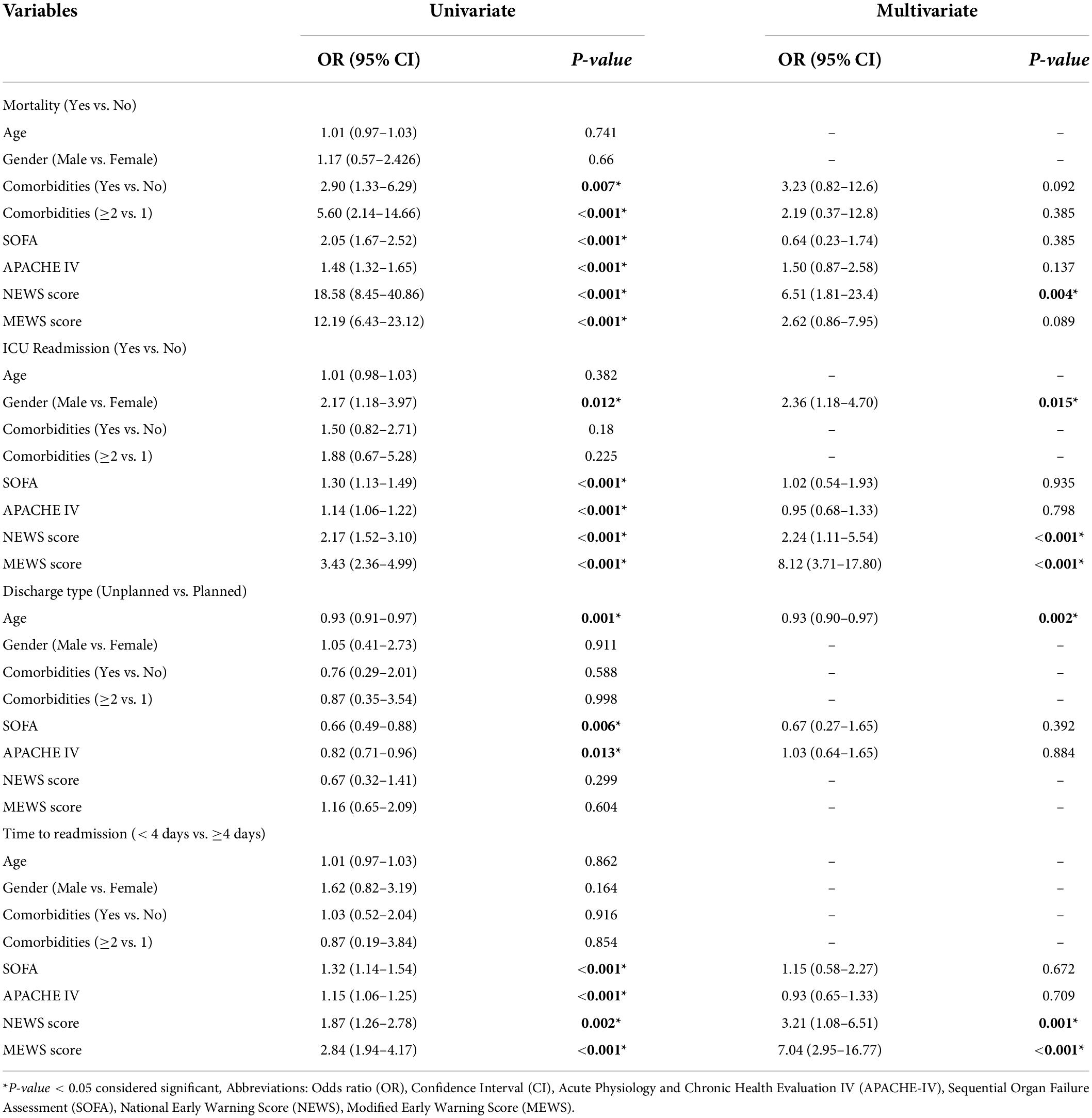
Table 4. Univariable and multivariable binary logistic regression analysis to evaluate associations of NEWS and MEWS scores to predict mortality, readmission, discharge type, and time to readmission.
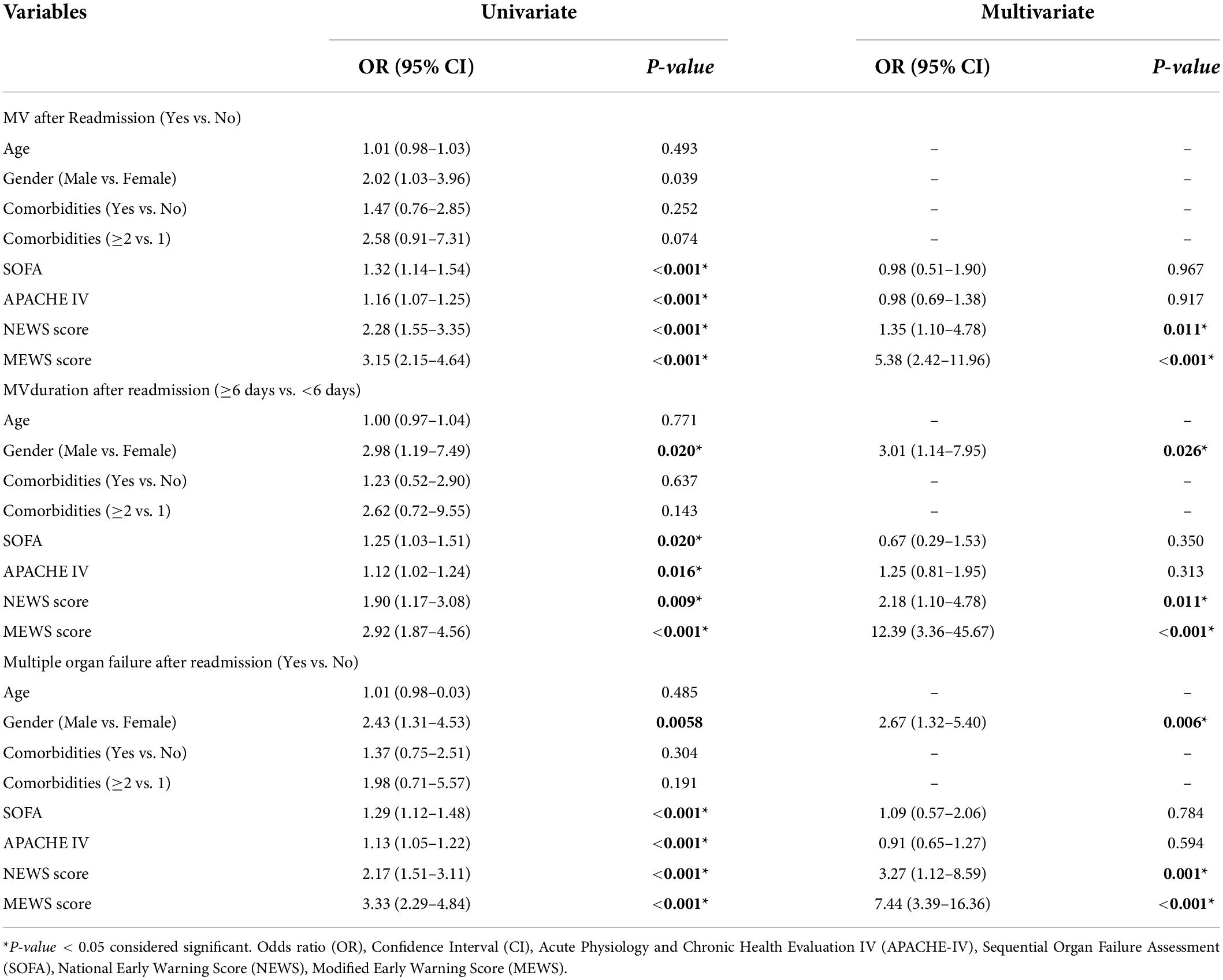
Table 5. Univariable and multivariable binary logistic regression analysis to evaluate associations of NEWS and MEWS scores to predict MV status, MV duration, and organ failure after readmission.
Table 6 shows the performance of NEWS and MEWS scores to predict outcomes with cut-off points. Excellent predictive performance of the NEWS score was found regarding mortality, with an AUC of 0.91 (95% CI: 0.88–0.94, p-value < 0.0001). The best cut-off value (>4) had a sensitivity of 71.87%, specificity of 95.5%, LR + of 15.98, LR- of 0.29, PPV of 57.5%, NPV of 97.6%, and 0.67% of Yuden index. The AUC values of the NEWS scores for ICU readmission, MV status, and multiple organ failure after readmission were considered fair. However, the poor predictive performance of the NEWS score was observed regarding the time to readmission and MV duration after readmission (Supplementary Figure 1).
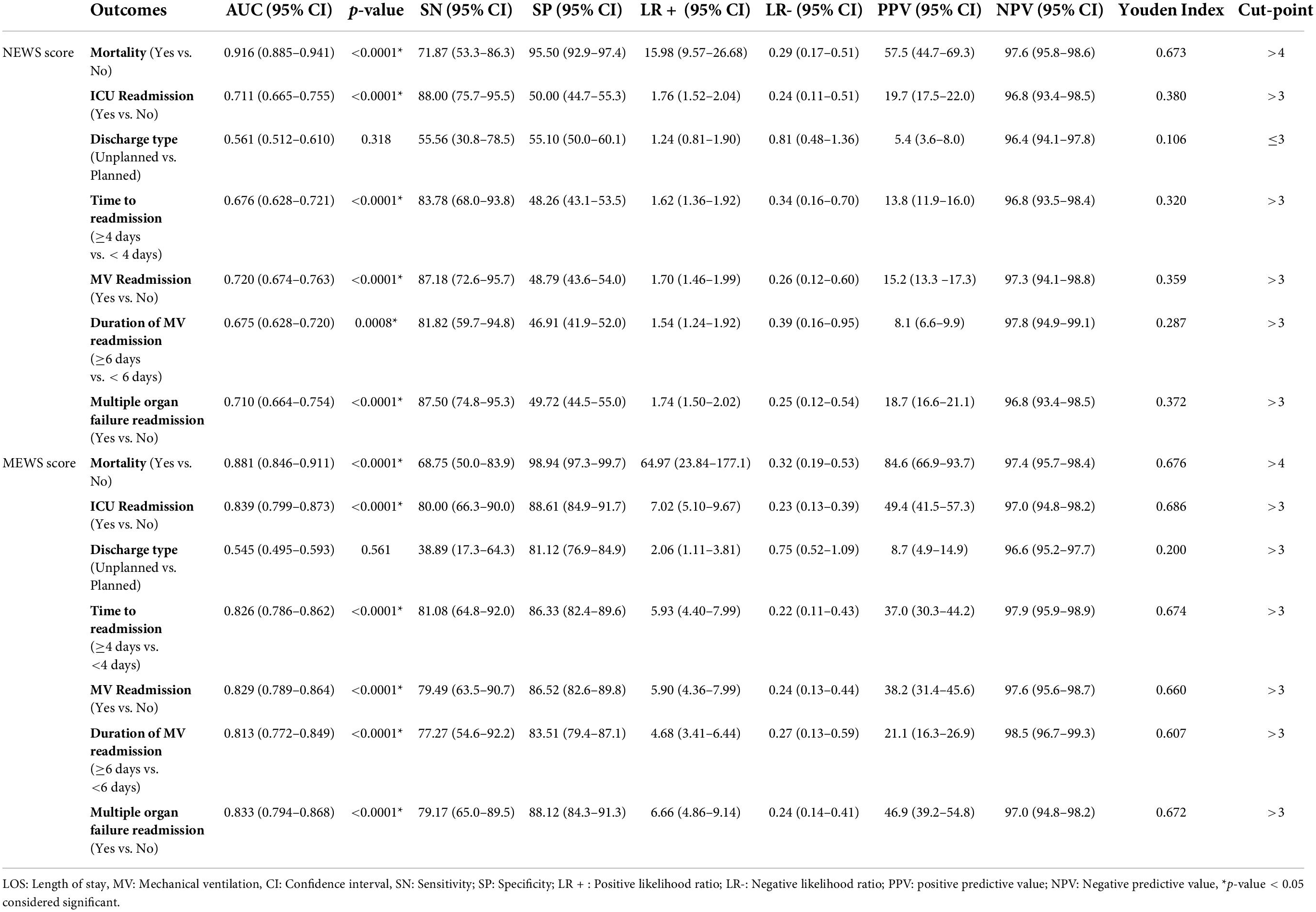
Table 6. Receiver operating characteristic curve results of NEWS and MEWS scores to predicting outcomes.
According to the results, the MEWS score had a good predictive performance for all outcomes, except for the type of discharge, which was insignificant. Best performing predictive value of MEWS score was related to the mortality with AUC of 0.88 (95% CI: 0.84–0.91, p-value < 0.0001), and the best cut-off value (>4) had a value sensitivity of 68.75%, specificity of 98.94%, LR + of 64.97, LR- of 0.32, PPV of 84.6%, NPV of 97.4%, and 0.67% of Yuden index. The AUCs for predicting readmission, time to readmission, MV status, MV duration, and multiple organ failure varied between 0.81 and 0.83 (Supplementary Figure 2). The cut-off values for predicting readmission, time to readmission, MV status, MV duration, and multiple organ failure were three or more scores.
A comparison of NEWS and MEWS AUCs was performed to predict the outcomes using the DeLong test, and the results are presented in Table 7. To predict mortality, the AUCs of NEWS and MEWS scores were 0.916 and 0.881, respectively, but this difference was not statistically significant (p-value = 0.082) (Figure 1A). However, the AUCs of the MEWS were significantly greater than NEWS for readmission (0.83 vs. 0.71, p-value < 0.0001) (Figure 1B), no significant difference for unplanned discharge types (Figure 1C), time to readmission (0.82 vs. 0.67, p-value < 0.0001) (Figure 1D), MV status, (0.82 vs. 0.72, p-value < 0.0001) (Figure 1E), MV duration (0.81 vs. 0.67, p-value < 0.0001) (Figure 1F), and multiple organ failure (0.83 vs. 0.71, p-value < 0.0001) (Figure 1G).
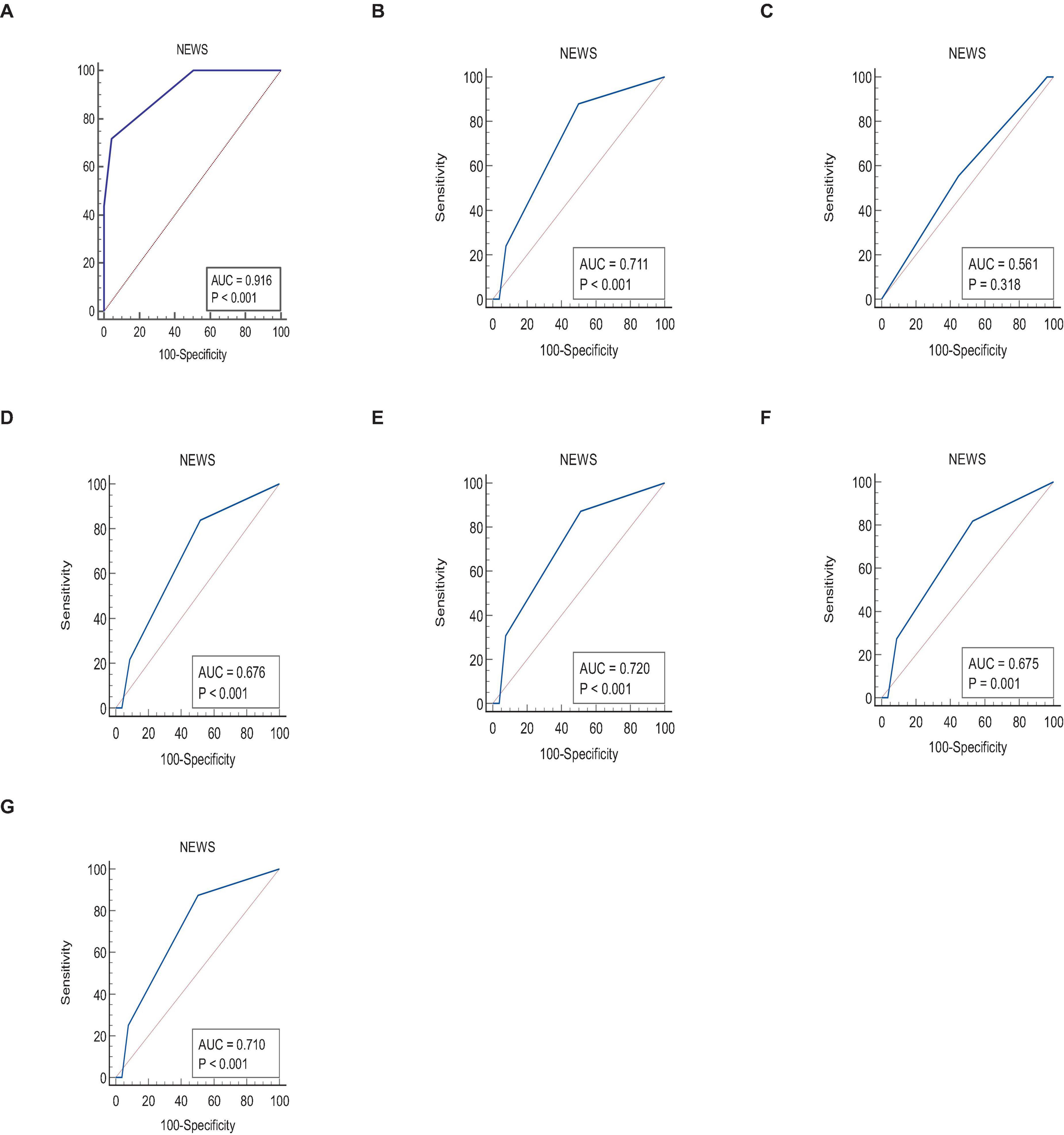
Figure 1. Comparison of ROC curves between NEWS and MEWS scores to predict (A) mortality, (B) ICU readmission, (C) unplanned discharge type, (D) time to readmission ≥ 4 days, (E) MV after readmission, (F) duration of MV ≥ 6 days, and (G) multiple organ failure after readmission.
The MEWS and NEWS are relatively new scoring systems capable of predicting the prognosis of ICU patients. Few studies employ and compare the MEWS or NEWS as outcome predictors in ICU patients. In this multicenter, prospective, observational study, we compared the NEWS and MEWS scores to predict the outcomes in critically ill patients at the time of ICU discharge. The analysis from the multivariable logistic model showed that high MEWS and NEWS were the risk factors for readmission occurrences, time to readmission, mortality, MV status, MV duration, and multiple organ failure after readmission. By comparing these two scoring systems, we identified that there was no significant difference between the AUCs of the NEWS and the MEWS for predicting mortality (P-value = 0.082). In contrast, the prognostic accuracy of MEWS in other outcomes such as readmission occurrence, time to readmission, MV status, MV duration, and multiple organ failure excels the prognostic accuracy of NEWS score (P-value < 0.001). Such a result can be due to the fact that most problems that directly or indirectly affect the readmission of critically ill patients are related to respiratory dysfunction. The rate of readmission due to respiratory dysfunction in this study was almost 50%. In addition, our results show that male patients are more likely to be readmitted, have multiple organ failures, and have a longer MV duration. From a clinical perspective, these findings suggest that gender may also be an important consideration in discharge planning in addition to the use of NEWS and MEWS. However, further studies are needed to confirm this finding. Based on the findings of this study, we conclude that MEWS can be considered an effective prognostic tool for predicting all outcomes, and the NEWS score is a good predictor of mortality and ICU readmission in critically ill patients at the time of ICU discharge. Hence, we advocate for determining the MEWS and NEWS at ICU discharge as an assistive tool to make a better-informed decision.
Scoring systems can be used to measure the performance of one ICU over a time period, or used to compare the performance of different ICUs which allows ICUs to understand more about the quality of delivered care, audit themselves and assist them in decision-making, resource allocation, quality assessment programs and teaching. Each physician should consider that the decision regarding to whether the patients should or should not be admitted to the ICU is dependent on some other factors. These include the risk and complications of ICU admission/readmission, patients’ wishes, and the time lag when scores are calculated (usually 24 h after admission to the ICU), which means that clinical intervention may precede the calculation of the score. As the MEWS and NEWS scores includes all qSOFA variables, so they can serve as an accurate score in prediction of outcome even in patients with infection. Using a scores that includes a points-based risk score, such as the NEWS/MEWS, may improve teaching, the integration, and incorporation of early warning scores into clinical practice focused on identifying and managing patients at risk for poor outcome (30, 31). Our findings coincide with many similar studies. Consistent with this study, many previous studies have shown the NEWS and MEWS scores to be a decisive tool for the early identification of patients with a high risk of poor outcomes, including mortality and ICU readmission (32–34). Balshi et al. reported that the MEWS is associated with ICU readmission, and a score > 6 has an excellent accuracy as a prognostic predictor (32). A prospective observational study by Xie et al. showed good performance of MEWS for in-hospital mortality prediction, with AUC values at 0.83 in patients presenting to the emergency department (35). MEWS also helps predict the mortality of COVID-19 patients, with AUC values of 0.913 and 0.833 (36, 37). Lv et al. found that MEWS shows superiority over the quick Sequential Organ Function Assessment (qSOFA), Combination of Confusion, Urea, Respiratory Rate, Blood Pressure, and Age ≥ 65 (CURB-65), and NEWS scores in predicting hospital mortality, and NEWS showed superiority over the other scores in predicting ICU admission in patients with community-acquired pneumonia (CAP) (38). Klepstad et al. showed that the higher NEWS in gastrointestinal surgical patients at ICU discharge was the predictive factor of ICU readmission (33). Moreover, the study by Doðu et al. demonstrated that a NEWS value of >7.5 at the time of discharge from ICU estimates a high probability of ICU readmission within the first 48 h after discharge (34). However, in contrast to these findings, a study by Reini et al. showed that the MEWS at ICU discharge is not a predictor of ICU readmission (39). On the other hand, this finding might be influenced (as acknowledged by the authors) by the decision to withhold ICU readmission for 10 out of 15 patients discharged with a MEWS of 5 or more. MEWS and NEWS are widely used scoring systems in many countries, but differences between these studies, including study setting, population, and disease type, have led to differences in the predictive ability of these scoring systems.
The most important advantage of MEWS and NEWS scores compared with other scoring systems, such as APACHE IV, SOFA, and Simplified Acute Physiology Score (SAPS), are their simplicity. They consist of basic physiological measurements in contrast to APACHE IV, SOFA, and SAPS, which, for instance, need documentation of laboratory results, making them a simpler tool with facilitated assessment procedures (38, 39). The advantage of these simple scoring systems could be the early identification of patients who were becoming increasingly unstable. In addition, they could facilitate the discharge decision by the intensivist. Early identification of critically ill patients with poor outcomes at the time of discharge from the ICU can enable the appropriate allocation of limited resources, such as intensive care beds.
The strengths of this study were the multicenter prospective design with heterogeneous patients from the general ICUs of two hospitals, which adjusted the confounding variables and made the findings more generalizable. However, our study has several limitations. First, the patient selection criteria were inclusive (all patients aged 18 years and above admitted to general ICU); this creates a rather heterogeneous cohort, and due to the wide range of ICU admission causes, we could not see the reason for admission evaluated as a variable. Second, we have not presented the individual physiological parameters included in the MEWS and NEWS; identifying whether any of these parameters had a better predictive value than the others would be interesting. Third, we could not use multiple parametric models like MANOVA to adjust the potential correlation among outcomes due to the lack of normal distribution of outcomes as the pre-assumption required for multiple testing. Fourth, to deal with multiple outcomes, we considered mortality and ICU readmission as primary outcomes. However, secondary outcomes are then subsidiary, and the results concerning them can only have an exploratory rather than a confirmatory interpretation. In addition, the frequency of readmission in the ICU was low (50 from 410), so interpreting results related to secondary outcomes such as readmission time, MV readmission, and duration of MV readmission should be interpreted with caution. Nevertheless, due to the varied performance of MEWS and NEWS in other studies, future disease-specific studies are required to improve the accuracy and applicability of MEWS and NEWS.
The MEWS and NEWS at the time of ICU discharge are independent predictors of ICU readmission and mortality. NEWS and MEWS scores greater than 4 have excellent and good accuracy in predicting mortality with 91 and 82% AUCs, respectively. In addition, scores greater than 3 have good and fair accuracy in predicting ICU readmission with AUCs of 83 and 71%, respectively. We found that the MEWS showed superiority over the NEWS score in predicting ICU readmission, time to readmission, MV readmission, MV duration, and multiple organ failure.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by the Ethics Committees of Islamic Azad University-Tabriz Branch (IR.TBZMED.REC.1397.994). The patients/participants provided their written informed consent to participate in this study.
FR-B, AM, SS, NS, and AV-A: study concept and design. SHS, ZO, M-SH, and SS: analysis and interpretation of data. SHS and AS: acquisition of data and drafting of the manuscript. FR-B, ZO, and SS: critical revision of the manuscript for important intellectual content. FR-B and AM: statistical analysis. All authors contributed to the article and approved the submitted version.
This study was supported by the Vice-chancellor for Research and Technology, Islamic Azad University-Tabriz Branch.
We thank the “Clinical Research Development Unit of Baqiyatallah Hospital” for guidance and advice.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2022.938005/full#supplementary-material
1. Brown SE, Ratcliffe SJ, Kahn JM, Halpern SD. The epidemiology of intensive care unit readmissions in the United States. Am J Respir Crit Care Med. (2012) 185:955–64. doi: 10.1164/rccm.201109-1720OC
2. Ponzoni CR, Corrêa TD, Filho RR, Serpa Neto A, Assunção MSC, Pardini A, et al. Readmission to the intensive care unit: incidence, risk factors, resource use, and outcomes. a retrospective cohort study. Ann Am Thoracic Soc. (2017) 14:1312–9. doi: 10.1513/AnnalsATS.201611-851OC
3. Grochla M, Saucha W, Borkowski J, Knapik P. [Readmission to the intensive care unit - epidemiology, prediction and clinical consequences]. Wiadomosci Lekarskie. (2019) 72:1387–96.
4. Jo YS, Lee YJ, Park JS, Yoon HI, Lee JH, Lee CT, et al. Readmission to medical intensive care units: risk factors and prediction. Yonsei Med J. (2015) 56:543–9. doi: 10.3349/ymj.2015.56.2.543
5. van Sluisveld N, Bakhshi-Raiez F, de Keizer N, Holman R, Wester G, Wollersheim H, et al. Variation in rates of ICU readmissions and post-ICU in-hospital mortality and their association with ICU discharge practices. BMC Health Serv Res. (2017) 17:281. doi: 10.1186/s12913-017-2234-z
6. Kramer AA, Higgins TL, Zimmerman JE. The association between ICU readmission rate and patient outcomes. Crit Care Med. (2013) 41:24–33. doi: 10.1097/CCM.0b013e3182657b8a
7. Marquet K, Claes N, De Troy E, Kox G, Droogmans M, Schrooten W, et al. One fourth of unplanned transfers to a higher level of care are associated with a highly preventable adverse event: a patient record review in six Belgian hospitals. Crit Care Med. (2015) 43:1053–61. doi: 10.1097/ccm.0000000000000932
8. Hosein FS, Bobrovitz N, Berthelot S, Zygun D, Ghali WA, Stelfox HT. A systematic review of tools for predicting severe adverse events following patient discharge from intensive care units. Crit Care. (2013) 17:R102. doi: 10.1186/cc12747
9. Elliott M, Worrall-Carter L, Page K. Intensive care readmission: a contemporary review of the literature. Intensive Crit Care Nurs. (2014) 30:121–37. doi: 10.1016/j.iccn.2013.10.005
10. Tanaka Gutiez M, Ramaiah R. Demand versus supply in intensive care: an ever-growing problem. Crit Care. (2014) 18:P9. doi: 10.1186/cc13199
11. Mathews KS, Long EFA. Conceptual framework for improving critical care patient flow and bed use. Ann Am Thoracic Soc. (2015) 12:886–94. doi: 10.1513/AnnalsATS.201409-419OC
12. van Sluisveld N, Zegers M, Westert G, van der Hoeven JG, Wollersheim H. A strategy to enhance the safety and efficiency of handovers of ICU patients: study protocol of the pICUp study. Implement Sci. (2013) 8:67. doi: 10.1186/1748-5908-8-67
13. Kareliusson F, De Geer L, Tibblin AO. Risk prediction of ICU readmission in a mixed surgical and medical population. J Intensive Care. (2015) 3:30. doi: 10.1186/s40560-015-0096-1
14. Badawi O, Breslow MJ. Readmissions and death after ICU discharge: development and validation of two predictive models. PLoS One. (2012) 7:e48758. doi: 10.1371/journal.pone.0048758
15. Ouanes I, Schwebel C, Français A, Bruel C, Philippart F, Vesin A, et al. A model to predict short-term death or readmission after intensive care unit discharge. J Crit Care. (2012) 27:422.e1–9. doi: 10.1016/j.jcrc.2011.08.003
16. Alam N, Hobbelink EL, van Tienhoven AJ, van de Ven PM, Jansma EP, Nanayakkara PW. The impact of the use of the Early Warning Score (EWS) on patient outcomes: a systematic review. Resuscitation. (2014) 85:587–94. doi: 10.1016/j.resuscitation.2014.01.013
17. Chapman SM, Maconochie IK. Early warning scores in paediatrics: an overview. Arch Dis. Child. (2019) 104:395–9. doi: 10.1136/archdischild-2018-314807
18. Kramer AA, Sebat F, Lissauer M. A review of early warning systems for prompt detection of patients at risk for clinical decline. J Trauma Acute Care Surg. (2019) 87:S67–73. doi: 10.1097/ta.0000000000002197
19. Petersen JA. Early warning score challenges and opportunities in the care of deteriorating patients. Danish Med J. (2018) 65:B5439.
20. Nannan Panday RS, Minderhoud TC, Alam N, Nanayakkara PWB. Prognostic value of early warning scores in the emergency department (ED) and acute medical unit (AMU): a narrative review. Eur J Internal Med. (2017) 45:20–31. doi: 10.1016/j.ejim.2017.09.027
21. Padilla RM, Mayo AM. Clinical deterioration: a concept analysis. J Clin Nurs. (2018) 27:1360–8. doi: 10.1111/jocn.14238
22. Subbe CP, Kruger M, Rutherford P, Gemmel L. Validation of a modified early warning score in medical admissions. Qjm. (2001) 94:521–6. doi: 10.1093/qjmed/94.10.521
23. Royal College of Physicians. National Early Warning Score (NEWS): Standardising the Assessment of Acute-Illness Severity in the NHS. Report of Working Party. London: Royal College of Physicians (2012).
24. Pirneskoski J, Kuisma M, Olkkola KT, Nurmi J. Prehospital national early warning score predicts early mortality. Acta Anaesthesiol Scand. (2019) 63:676–83. doi: 10.1111/aas.13310
25. Burch VC, Tarr G, Morroni C. Modified early warning score predicts the need for hospital admission and inhospital mortality. Emerg Med J. (2008) 25:674–8. doi: 10.1136/emj.2007.057661
26. Cei M, Bartolomei C, Mumoli N. In-hospital mortality and morbidity of elderly medical patients can be predicted at admission by the Modified Early Warning Score: a prospective study. Int J Clin Pract. (2009) 63:591–5. doi: 10.1111/j.1742-1241.2008.01986.x
27. World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. (2013) 310:2191–4. doi: 10.1001/jama.2013.281053
28. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. (2008) 61:344–9. doi: 10.1016/j.jclinepi.2007.11.008
29. Jones M. NEWSDIG: the national early warning score development and implementation group. Clin Med. (2012) 12:501–3. doi: 10.7861/clinmedicine.12-6-501
30. Liu VX, Lu Y, Carey KA, Gilbert ER, Afshar M, Akel M, et al. Comparison of early warning scoring systems for hospitalized patients with and without infection at risk for in-hospital mortality and transfer to the intensive care unit. JAMA Netw Open. (2020) 3:e205191. doi: 10.1001/jamanetworkopen.2020.5191
31. Desai N, Gross J. Scoring systems in the critically ill: uses, cautions, and future directions. BJA Educ. (2019) 19:212–8. doi: 10.1016/j.bjae.2019.03.002
32. Balshi AN, Huwait BM, Noor ASN, Alharthy AM, Madi AF, Ramadan OE, et al. Modified Early Warning Score as a predictor of intensive care unit readmission within 48 hours: a retrospective observational study. Rev Bras Terapia Intensiva. (2020) 32:301–7. doi: 10.5935/0103-507x.20200047
33. Klepstad PK, Nordseth T, Sikora N, Klepstad P. Use of national early warning score for observation for increased risk for clinical deterioration during post-ICU care at a surgical ward. Therapeut Clin Risk Manag. (2019) 15:315–22. doi: 10.2147/tcrm.s192630
34. Doğu C, Doğan G, Kayir S, Yağan Ö. Importance of the National Early Warning Score (NEWS) at the time of discharge from the intensive care unit. Turk J Med Sci. (2020) 50:1203–9. doi: 10.3906/sag-1906-78
35. Xie X, Huang W, Liu Q, Tan W, Pan L, Wang L, et al. Prognostic value of Modified Early Warning Score generated in a Chinese emergency department: a prospective cohort study. BMJ Open. (2018) 8:e024120. doi: 10.1136/bmjopen-2018-024120
36. Wang L, Lv Q, Zhang X, Jiang B, Liu E, Xiao C, et al. The utility of MEWS for predicting the mortality in the elderly adults with COVID-19: a retrospective cohort study with comparison to other predictive clinical scores. PeerJ. (2020) 8:e10018. doi: 10.7717/peerj.10018
37. Aygun H, Eraybar S. The role of emergency department triage early warning score (TREWS) and modified early warning score (MEWS) to predict in-hospital mortality in COVID-19 patients. Ir J Med Sci. (2021) 191:997–1003. doi: 10.1007/s11845-021-02696-y
38. Lv C, Chen Y, Shi W, Pan T, Deng J, Xu J. Comparison of different scoring systems for prediction of mortality and ICU admission in elderly CAP population. Clin Intervent Aging. (2021) 16:1917–29. doi: 10.2147/cia.s335315
Keywords: intensive care unit, National Early Warning Score, Modified Early Warning Score, readmission, mortality, prognosis
Citation: Mahmoodpoor A, Sanaie S, Saghaleini SH, Ostadi Z, Hosseini M-S, Sheshgelani N, Vahedian-Azimi A, Samim A and Rahimi-Bashar F (2022) Prognostic value of National Early Warning Score and Modified Early Warning Score on intensive care unit readmission and mortality: A prospective observational study. Front. Med. 9:938005. doi: 10.3389/fmed.2022.938005
Received: 06 May 2022; Accepted: 19 July 2022;
Published: 04 August 2022.
Edited by:
Longxiang Su, Peking Union Medical College Hospital (CAMS), ChinaReviewed by:
Jian-cang Zhou, Sir Run Run Shaw Hospital, ChinaCopyright © 2022 Mahmoodpoor, Sanaie, Saghaleini, Ostadi, Hosseini, Sheshgelani, Vahedian-Azimi, Samim and Rahimi-Bashar. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ata Mahmoodpoor, YW1haG1vb2Rwb29yQHlhaG9vLmNvbQ==; Farshid Rahimi-Bashar, ZnJfcmFoaW1pYmFzaGFyQHlhaG9vLmNvbQ==
†These authors have contributed equally to this work and share first authorship
‡ORCID: Ata Mahmoodpoor, orcid.org/0000-0002-4361-6230; Sarvin Sanaie, orcid.org/0000-0003-2325-5631; Seied Hadi Saghaleini, orcid.org/0000-0003-4996-4372"; Zohreh Ostadi, orcid.org/0000-0003-0437-4192; Mohammad-Salar Hosseini, orcid.org/0000-0003-2765-5018; Amir Vahedian-Azimi, orcid.org/0000-0002-1678-7608; Farshid Rahimi-Bashar, orcid.org/0000-0001-8276-1425
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.