- 1Shengli Clinical Medical College of Fujian Medical University, Fuzhou, China
- 2Department of Surgical Oncology, Fujian Provincial Hospital, Fuzhou, China
- 3The First Affiliated Hospital of Fujian Medical University, Fuzhou, China
Idiopathic spontaneous intraperitoneal hemorrhage (ISIH) is a phenomenon caused by spontaneous rupture of intra-abdominal visceral vessels, and vascular malformations (VMs) leading to ISIH are rare in previously reported cases. VMs of the gastric wall, which are commonly located in the mucosa and submucosa, mostly lead to upper gastrointestinal bleeding rather than intraperitoneal hemorrhage. To our knowledge, this is the first report of ISIH caused by VMs in gastric muscularis. In the current case, a 22-year-old male patient presented with sudden abdominal pain for 4 h, accompanied by tachycardia and hypotension. CT revealed a hematoma in the omental bursa and fluids in abdominopelvic cavities. Then intraperitoneal hemorrhage was confirmed after abdominal paracentesis. Furthermore, ultrasonic gastroscopy indicated that vascular malformation in the muscularis of the stomach probably led to intraperitoneal hemorrhage. The patient recovered after conservative treatment based on fluid resuscitation and remained stable for 12 months of follow-up. This case suggests that VMs located in the gastrointestinal tract may lead to ISIH and ultrasonic gastroscopy is helpful in the diagnosis of VMs in the gastrointestinal tract.
Introduction
Idiopathic spontaneous intraperitoneal hemorrhage (ISIH), which was once labeled abdominal apoplexy, is a rare and potentially fatal condition caused by a spontaneous tear of intraperitoneal visceral vessels (1, 2). The presentation varies from non-specific abdominal pain to hemodynamic instability depending on the location and severity of bleeding (3). Surgical exploration remains a major diagnostic and therapeutic modality (4). In previously reported cases, ISIHs were commonly caused by atherosclerosis, aneurysms, vasculitis, etc. (2, 4). ISIH caused by vascular malformations (VMs) is rarely seen (5). VMs are congenital anomalies that can affect each part of the vasculature (6). About 90% of gastrointestinal VMs occur in the small intestine, leading to gastrointestinal bleeding (7, 8). To our knowledge, this is the first case of ISIH due to VMs in the muscularis of the stomach, which has some guidance for the etiology, diagnosis, and treatment of ISIH.
Case Presentation
A 22-year-old Asian man was admitted with “severe mid-upper abdomen pain for 4 h.” He presented persistent, severe pain in the upper abdomen and pain radiating to the left shoulder, accompanied by dizziness, palpitations, amaurosis, and cold sweats. He did not receive any treatment before the admission and denied surgery, trauma, alcohol intake, strenuous exercise, and use of non-steroidal anti-inflammatory drugs before the onset. No family history of related illness was reported. On physical examination, he was noted to have tachycardia (heart rate: 106 beats per min) and hypotension (blood pressure: 81/50 mmHg). Mild abdominal distension, epigastric tenderness, and rebound pain were also noted during physical examination.
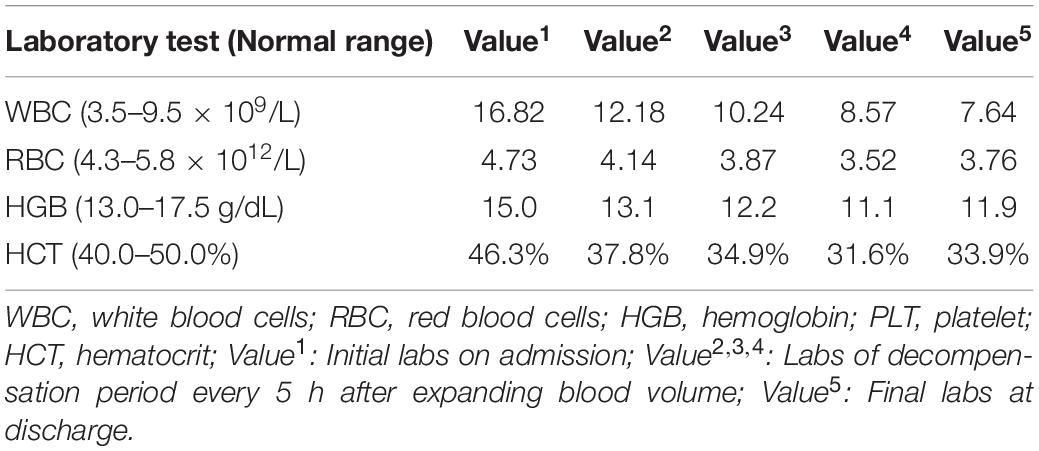
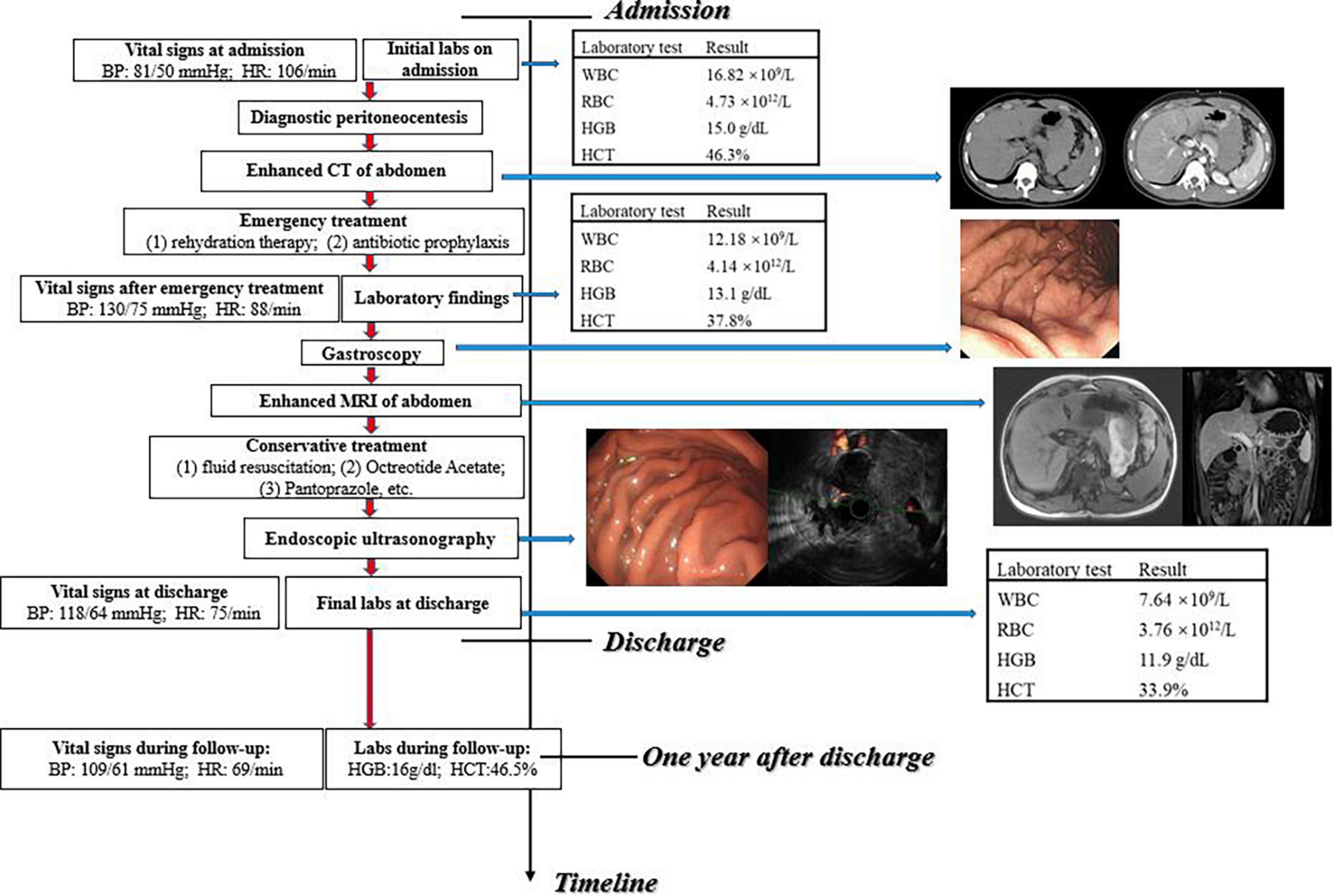
Initial laboratory evaluation revealed a white cell count (WBC) of 16.82 × 109/L, hemoglobin (HGB) of 15 g/dL, and hematocrit (HCT) of 46.3% (Table 1). Abdominal enhanced computed tomography (CT) showed a 10 × 5.2 cm2 hemoperitoneum in the gastro-pancreatic gap in addition to the massive hemoperitoneum around the spleen and in the rectovesical space, which was connected with the hemoperitoneum around the liver through the Winslow foramen (Figure 1A); and the size and density of each solid organ were normal. Subsequently, the patient underwent diagnostic abdominal paracentesis, which further confirmed that the intraperitoneal fluid was blood. Gastroscopy showed that the gastric mucosa was smooth, and no ulcer or bleeding spot was observed in the upper digestive tract (Figure 1B). Fluid resuscitation was conducted immediately after admission. Although blood routine tests revealed a downward trend of hemoglobin and hematocrit (HGB 13.1 g/dL, HCT of 37.8%), the patient’s condition tended to be stabilized (heart rate: 88 beats per min; blood pressure: 130/75 mmHg). Given the success of rehydration therapy and ambiguous source of hemorrhage, conservative medical treatment (Fluid resuscitation, Octreotide Acetate, Pantoprazole, etc.) was initially adopted. Meanwhile, the patient was under close observation, and emergency surgical exploration would be conducted if necessary.
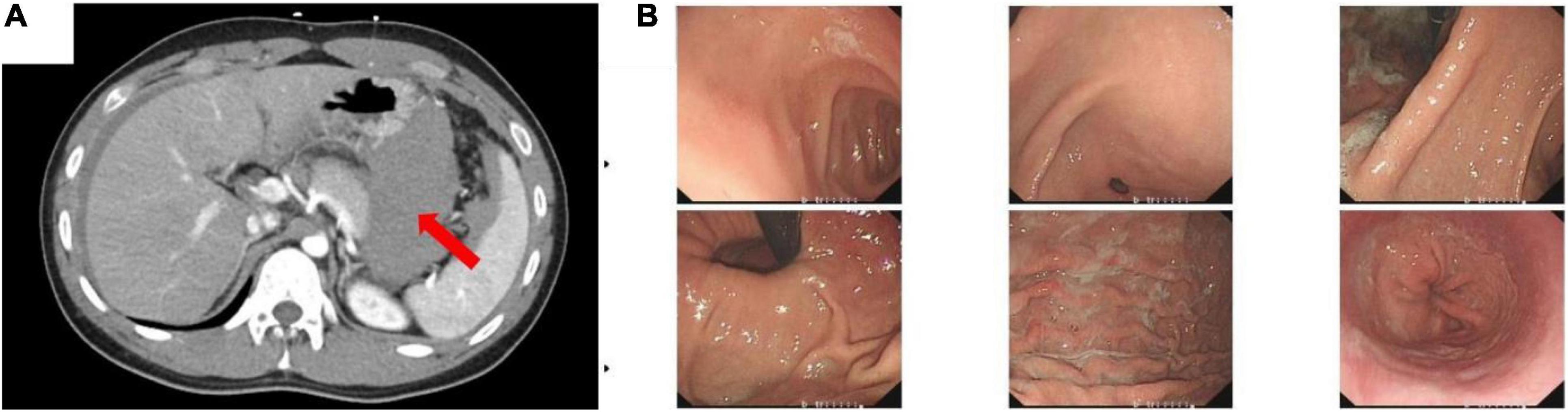
Figure 1. (A) Enhanced computed tomography (CT) of the abdomen. Red arrow showed a 10 × 5.2 cm2 high-density shadow in the gastro-pancreatic gap. (B) Gastroscopy showed that the gastric mucosa was smooth and had no ulcer or bleeding spot in the upper digestive tract.
To clarify the reason for the hemorrhage, enhanced magnetic resonance imaging (MRI) was performed, which revealed a hematoma in the gastro-pancreatic gap, without signs of space-occupying lesion and other indications about the source of bleeding (Figure 2A). Later, we performed endoscopic ultrasonography (EUS) on him. A mixed hypoechoic and anechoic lesion was seen between the pancreatic tail and the gastric wall, which was closely related to the peripheral blood vessels and was considered to be a hematoma combined with the previous imaging reports. Part of the muscularis propria was connected to the hematoma. In addition, Doppler ultrasonography showed that the blood flow signal was continuous between the muscularis propria and hematoma, which was considered as the vascular malformation in the muscularis of the stomach (Figure 2B). He was ultimately diagnosed with “intraperitoneal hemorrhage due to VMs in the muscularis of the stomach” based on the CT images and the EUS results, combined with the clinical manifestation. The patient was young and had fertility demands shortly. He was reluctant to accept CTA and interventional therapy due to the radiation dose of CTA and endovascular treatment. Also, considering that no obvious bleeding site was found on enhanced CT, we were concerned that the intervention would not be able to locate the lesion, so we did not conduct invasive treatment, such as endovascular management or surgery. The patient recovered gradually after conservative treatment without signs of continuous bleeding, and he was discharged after 4 days (the final laboratory data are shown in Table 1). We performed follow-ups for the patient at the hospital outpatient department at 6 months intervals. The follow-up after 1 year showed that the patient had no signs of recurrence (Figure 3). The timeline from emergency to follow-up is presented in Figure 3.
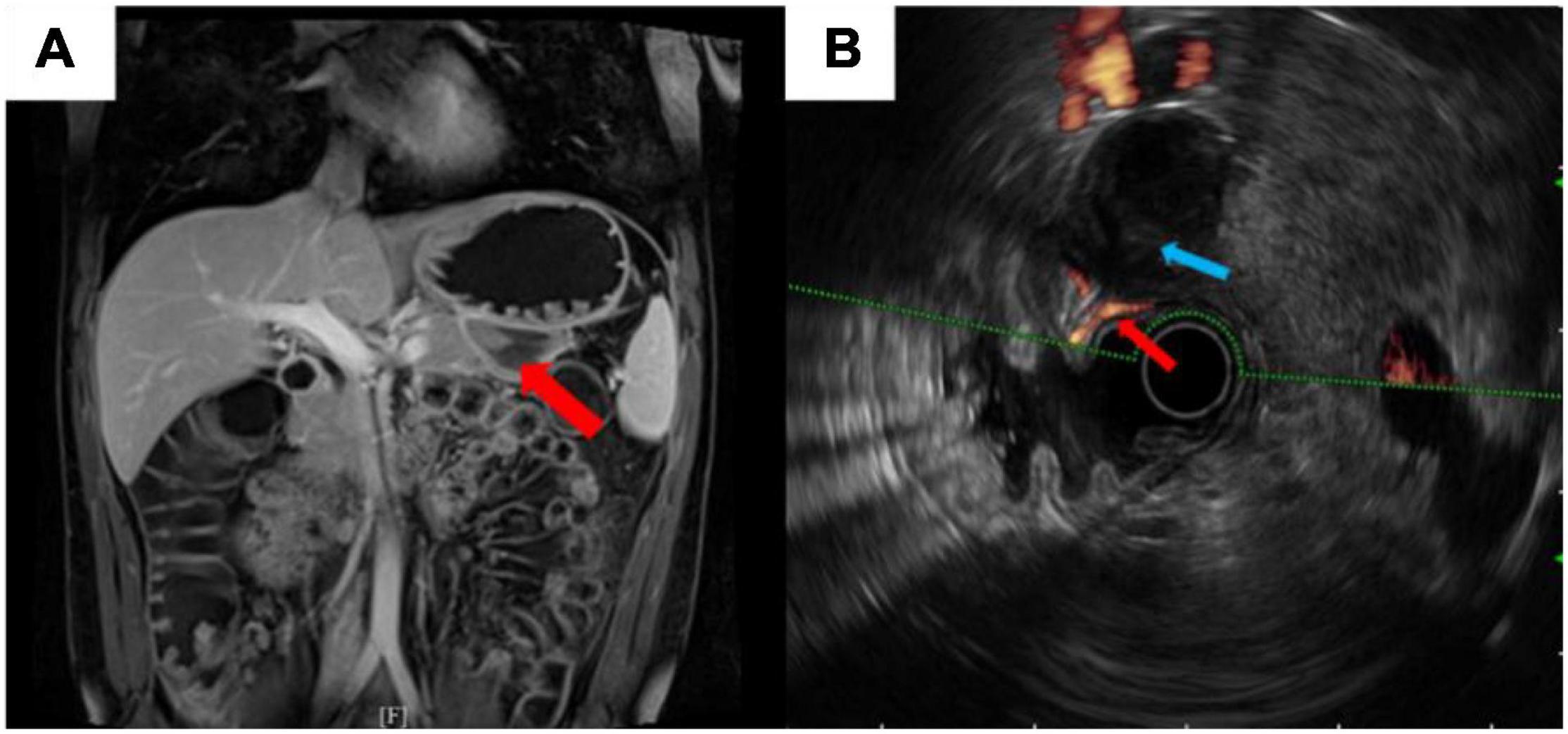
Figure 2. (A) Enhanced magnetic resonance imaging (MRI) revealed no sign of space-occupying lesion. Red arrow showed a hematoma in the gastro-pancreatic gap. (B) Endoscopic ultrasonography (EUS) illustrated the vascular malformation in the muscularis of the stomach. Blue arrow showed a hypoechoic shadow. Red arrow showed a 1.3-mm diameter blood flow signal was continuous between the muscularis propria and the hypoechoic shadow.
Discussion
Idiopathic spontaneous intraperitoneal hemorrhage (ISIH), originally known as abdominal apoplexy, is used to describe atypical and non-traumatic spontaneous intraperitoneal or retroperitoneal bleeding, excluding typical intraperitoneal bleeding caused by ectopic pregnancy, malignant tumor, aortic aneurysm or dissection, visceral rupture, trauma, and iatrogenic injury (9, 10). Abdominal aneurysm is the main reason of ISIH, of which splenic aneurysm is the most common (60%) and the gastric and gastroepiploic aneurysms are responsible for only 3% (2). The rupture of a splenic aneurysm is mostly caused by the erosion of the vessel wall owing to pancreatic enzymes released in pancreatitis (in about 50% of cases) and results in over 90% mortality (11). Besides abdominal aneurysms, atherosclerosis is considered to be another important cause of ISIH. The presumed mechanism is the weakness of the tunica media in the injured vessel, which ruptures when blood pressure suddenly rises (2). As described in the report, a patient was presented to our hospital with sudden, non-specific abdominal pain and, was finally diagnosed with ISIH caused by VMs in gastric muscularis mainly relying on EUS.
VMs are diseases with unpredictable clinical evolution and manifestations, which lead to life-threatening conditions in severe cases (12). The splenic artery is the most common vessel responsible for ISIH, while the gastric or gastroepiploic artery accounts for only 4% (13). The VMs of the gastric wall generally occur in the gastric mucosa and submucosa, so it usually causes intragastric hemorrhage (14–16). We checked the relevant literature and found that this is the first case of a vessel in the muscularis of the stomach inducing intraperitoneal bleeding, which suggests that the blood vessels of the gastric serosal surface, and even the entire stomach wall, should be considered when looking for the bleeding sites of ISIH.
According to the available literature, optimal diagnostic and therapeutic evidence of ISIH remain controversial (12). CT angiography (CTA) or digital subtraction angiography (DSA) is considered to be a primary tool for diagnosing ISIH, localizing the bleeding vessel if the hemodynamic and clinical status of patients enables it (3, 17). The non-invasiveness and short acquisition time of CTA give it more advantages for acute bleeding and a higher priority than DSA (18, 19). However, some literature points out that CTA may have false-negative results which can occur if the bleeding is not obvious at the time of the scan due to the short acquisition time (19–21). Considering that the patient had no indication of active bleeding, and it was difficult to locate the culprit vessel using CTA, we did not perform CTA in this case. EUS can provide real-time images of the gastrointestinal wall and blood vessels of adjacent tissues and has been applied to diagnostic interventions (22, 23). VMs can appear as a persistent blood flow signal in the parietal layer of the gastrointestinal tract under EUS guidance (24).
Surgery and embolization are methods for the treatment of VMs. Endovascular embolization is less invasive and recommended in most cases (9). However, it is difficult to locate culprit vessels in cases without active bleeding, so endovascular embolization was not selected in this case. Exploratory surgery is usually employed when CTA cannot be performed or failed to identify the culprit vessel (17). Exploratory laparotomy or laparoscopic exploration can detect the bleeding site, achieve initial hemostasis (25), and take tissue for pathological diagnosis. However, nearly 40% of operations failed in finding the bleeding site of the patient (9, 26). Therefore, due to the lack of continuous bleeding, we did not surgically explore and treat the patient. For younger patients without immediate surgical management, we suggest close attention and a conservative administration, including somatostatin or somatostatin analogs (such as octreotide), which have been concluded as an effective therapy for hemorrhage of gastrointestinal VMs (27, 28). However, for patients with decompensated or life-threatening conditions, we recommend emergency surgery; for patients with recurrent bleeding, surgery may be also finally required (29).
The limitations of our study include the lack of objectivity of imaging and the ambiguous assessment of therapeutic effect. Different from CT or MRI, EUS is operator dependent, and the analysis of the images is subjective. There is a risk of recurrence because the patient did not receive surgical treatment and EUS revealed that VMs still existed, though he is currently in stable condition. The length of follow-up time is not sufficient to accurately evaluate the effect of conservative treatment up to now.
Conclusion
For patients with spontaneous intraperitoneal hemorrhage, particularly ISIH, VM rupture should be considered when the disease cannot be identified after excluding the common causes. VMs in the gastric wall may lead to intraperitoneal hemorrhage in addition to intragastric bleeding. If it is speculated that the vascular malformation is located in the gastric wall, EUS may be a new alternative diagnostic approach for CTA. Due to the lack of evidence, it is difficult to standardize the treatment of such patients. Conservative treatment can be chosen temporarily for patients without immediate surgery or indication of embolism.
Data Availability Statement
The original contributions presented in this study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Ethics Statement
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author Contributions
YHZ, YCZ, WL, and SL participated in the diagnosis and treatment of patients. YHZ and YCZ wrote the manuscript. WL provided professional opinions on diagnosis. SL reviewed and revised the manuscript. All authors contributed to manuscript revision, read, and approved the submitted version.
Funding
This work was supported by three grants from the Scientific Research Foundation of Fujian Provincial Hospital, China (No. 2020YJ04), Youth Scientific Research Project of Fujian Provincial Health Commission, China (No. 2020QN01010175), and Science and Innovation Project for Youth Talent of Natural Science Foundation of Fujian Province, China (No. 2020J01223150).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We thank the patient who was presented in the case and the team at the Endoscopy Center of Fujian Provincial Hospital.
References
1. Green WT, Powers JH. Intra-abdominal apoplexy. Ann Surg. (1931) 93:1070–4. doi: 10.1097/00000658-193105000-00013
2. Wang H, Xiu D. Abdominal apoplexy because of the rupture of gastroduodenal artery and inferior pancreaticoduodenal artery: a case report. Medicine. (2017) 96:e8264. doi: 10.1097/MD.0000000000008264
3. Qaraqe TM, Abou Daher A, Alami RS. Abdominal apoplexy: a rare case of spontaneous middle colic artery rupture with transverse colectomy. Int J Surg Case Rep. (2021) 81:105835. doi: 10.1016/j.ijscr.2021.105835
4. Zeinalpour A, Aghili A, Gholizadeh B. Abdominal apoplexy due to rupture of inferior pancreaticoduodenal artery: a rare case of acute abdomen. Caspian J Intern Med. (2021) 12(Suppl 2):S479–81. doi: 10.22088/cjim.12.0.479
5. Saeed Y, Farkas Z, Azeez S. Idiopathic spontaneous intraperitoneal hemorrhage due to rupture of short gastric artery presenting as massive gastrointestinal bleeding: a rare case presentation and literature review. Cureus. (2020) 12:e11499. doi: 10.7759/cureus.11499
6. Della Rosa N, Bertozzi N, Adani R. Vascular malformation and their unpredictable evolution: a true challenge for physicians. Acta Biomed. (2020) 91:e2020067. doi: 10.23750/abm.v91i3.8298
7. Redondo-Cerezo E, Gomez-Ruiz CJ, Sanchez-Manjavacas N, Vinuelas M, Jimeno C, Perez-Vigara G, et al. Long-term follow-up of patients with small-bowel angiodysplasia on capsule endoscopy. determinants of a higher clinical impact and rebleeding rate. Rev Esp Enferm Dig. (2008) 100:202–7. doi: 10.4321/s1130-01082008000400002
8. Chen H, Fu S, Feng N, Chen H, Gao Y, Zhao Y, et al. Bleeding recurrence in patients with gastrointestinal vascular malformation after thalidomide. Medicine. (2016) 95:e4606. doi: 10.1097/MD.0000000000004606
9. Cawyer JC, Stone CK. Abdominal apoplexy: a case report and review. J Emerg Med. (2011) 40:e49–52. doi: 10.1016/j.jemermed.2007.11.080
10. Harbour LN, Koch MS, Louis TH, Fulmer JM, Guileyardo JM. Abdominal apoplexy: two unusual cases of hemoperitoneum. Proceedings. (2012) 25:16–9. doi: 10.1080/08998280.2012.11928772
11. Corvino F, Giurazza F, Ierardi AM, Lucatelli P, Basile A, Corvino A, et al. Splenic artery pseudoaneurysms: the role of Ce-Ct for diagnosis and treatment planning. Diagnostics. (2022) 12:1012. doi: 10.3390/diagnostics12041012
12. Cucuruz B, Koller M, Pfleiderer R, Geisthoff U, Meyer L, Kapp F, et al. Towards a better treatment of patients with vascular malformations: certified interdisciplinary centers are mandatory. Z Evid Fortbild Qual Gesundhwes. (2022) 168:1–7. doi: 10.1016/j.zefq.2021.11.003
13. Negmadjanov U, Ohanisian L, Rubay D, Hristov B, Belizon A. Abdominal apoplexy: a case study of idiopathic spontaneous lesser sac hematoma. Cureus. (2019) 11:e4937. doi: 10.7759/cureus.4937
14. Athanasoulis CA, Galdabini JJ, Waltman AC, Novelline RA, Greenfield AJ, Ezpeleta ML. Angiodysplasia of the colon: a cause of rectal bleeding. Cardiovasc Radiol. (1977) 1:3–13. doi: 10.1007/BF02551967
15. Gordon FH, Watkinson A, Hodgson H. Vascular malformations of the gastrointestinal tract. Best Pract Res Clin Gastroenterol. (2001) 15:41–58. doi: 10.1053/bega.2000.0155
16. Handra-Luca A, Montgomery E. Vascular malformations and hemangiolymphangiomas of the gastrointestinal tract: morphological features and clinical impact. Int J Clin Exp Pathol. (2011) 4:430–43.
17. Law EK, Lee RK, Hung EH, Ng AW. Radiological diagnosis and management of idiopathic spontaneous intra-abdominal haemorrhage (abdominal apoplexy): a case series. Abdom Imaging. (2015) 40:343–51. doi: 10.1007/s00261-014-0220-z
18. Jansen IGH, Berkhemer OA, Yoo AJ, Vos JA, Lycklama ANGJ, Sprengers MES, et al. Comparison of Cta- and Dsa-based collateral flow assessment in patients with anterior circulation stroke. AJNR Am J Neuroradiol. (2016) 37:2037–42. doi: 10.3174/ajnr.A4878
19. Wortman JR, Landman W, Fulwadhva UP, Viscomi SG, Sodickson AD. Ct angiography for acute gastrointestinal bleeding: what the radiologist needs to know. Br J Radiol. (2017) 90:20170076. doi: 10.1259/bjr.20170076
20. O’Brien AC, Healy GM, Rutledge N, Patil A, McCann JWJ, Cantwell CP. Conventional angiography findings in hemodynamically unstable patients with acute abdominal hemorrhage and a negative Ct bleeding study. CVIR Endovasc. (2020) 3:22. doi: 10.1186/s42155-020-00112-7
21. Wong H, Hodgson L, Banfield J, Shankar JJS. Digital subtraction angiography for Ct angiogram negative haemorrhages. Can J Neurol Sci. (2018) 45:522–6. doi: 10.1017/cjn.2018.75
22. Chapman CG, Waxman I. Eus-guided portal vein sampling. Endosc Ultrasound. (2018) 7:240–5. doi: 10.4103/eus.eus_28_18
23. Yang J, Zhou Y. Combined Ercp and endoscopic ultrasonography: a new treatment for rare hemorrhage from a duodenal papillary vascular malformation. Endoscopy. (2021) 53:E108–9. doi: 10.1055/a-1202-9858
24. Vila JJ, Perez-Miranda M, Basterra M, Gomez M, Fernandez-Urien I, Jimenez FJ. Endoscopic ultrasound-guided therapy of a rectal dieulafoy lesion. Endoscopy. (2014) 46(Suppl 1):E84–5. doi: 10.1055/s-0033-1344776
25. Jakob DA, Liasidis P, Schellenberg M, Matsushima K, Lam L, Demetriades D, et al. Intra-abdominal hemorrhage control: the need for routine four-quadrant packing explored. World J Surg. (2021) 45:1014–20. doi: 10.1007/s00268-020-05906-3
26. Hassani KI, Bounekar A, Gruss JM. Spontaneous rupture of the right gastroepiploic artery: unusual cause of acute abdomen and shock. World J Emerg Surg. (2009) 4:24. doi: 10.1186/1749-7922-4-24
27. Bauditz J. Effective treatment of gastrointestinal bleeding with thalidomide–chances and limitations. World J Gastroenterol. (2016) 22:3158–64. doi: 10.3748/wjg.v22.i11.3158
28. Iannone A, Principi M, Barone M, Losurdo G, Ierardi E, Di Leo A. Gastrointestinal bleeding from vascular malformations: is octreotide effective to rescue difficult-to-treat patients? Clin Res Hepatol Gastroenterol. (2016) 40:373–7. doi: 10.1016/j.clinre.2016.02.003
Keywords: idiopathic spontaneous intraperitoneal hemorrhage, abdominal apoplexy, vascular malformation, endoscopic ultrasonography, case report
Citation: Zhou Y, Zhou Y, Li W and Lin S (2022) Idiopathic Spontaneous Intraperitoneal Hemorrhage Due to Vascular Malformations in the Muscularis of the Stomach: A Case Report. Front. Med. 9:927899. doi: 10.3389/fmed.2022.927899
Received: 25 April 2022; Accepted: 20 June 2022;
Published: 01 September 2022.
Edited by:
Gopal Krishna Dhali, Institute of Post Graduate Medical Education and Research (IPGMER), IndiaReviewed by:
Antonio Corvino, University of Naples Parthenope, ItalyEgidio Imbalzano, University of Messina, Italy
Copyright © 2022 Zhou, Zhou, Li and Lin. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Weihua Li, bGl3aEBmam11LmVkdS5jbg==; Shengtao Lin, ZHJsaW5zdEAxNjMuY29t
†These authors have contributed equally to this work
 Yuhang Zhou
Yuhang Zhou Yuchen Zhou3†
Yuchen Zhou3† Weihua Li
Weihua Li