
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Med., 24 June 2022
Sec. Obstetrics and Gynecology
Volume 9 - 2022 | https://doi.org/10.3389/fmed.2022.905174
 Beshada Zerfu Woldegeorgis1*
Beshada Zerfu Woldegeorgis1* Mohammed Suleiman Obsa2
Mohammed Suleiman Obsa2 Lemi Belay Tolu3
Lemi Belay Tolu3 Efa Ambaw Bogino4
Efa Ambaw Bogino4 Tesfalem Israel Boda1
Tesfalem Israel Boda1 Henok Berhanu Alemu1
Henok Berhanu Alemu1Background: Episiotomy, a surgical procedure that enlarges the vaginal opening during childbirth, was common practice until the early 2000s. Other sources, including the World Health Organization (WHO), advocate for the selective use of episiotomy. Episiotomy rates, on the other hand, have remained high in developing countries, while declining in developed countries. As a result, the current study sought to determine the overall prevalence of episiotomy in Africa as well as the risk factors associated with its practice.
Methods: Articles were searched in international electronic databases. A standardized Microsoft Excel spreadsheet and STATA software version 14 were used for data extraction and analysis, respectively. The Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) checklist was used to write this report. A random-effects meta-analysis model was used to determine the pooled prevalence of episiotomy. A heterogeneity test was conducted using I-Squared (I2) statistics. Egger's test and funnel plots were conducted to detect publication bias. Subgroup analysis was also conducted. Association was expressed through a pooled odds ratio (OR) with a 95% Confidence Interval (CI).
Result: A total of 21 studies with 40,831 participants were included in the systematic review and meta-analysis. The pooled prevalence of episiotomy practice was 41.7% [95% CI (36.0–47.4), I2 = 99.3%, P < 0.001). Primiparity [OR: 6.796 (95% CI (4.862–9.498)), P < 0.001, I2: 95.1%], medical doctors- assisted delivery [OR: 3.675 (95% CI (2.034–6.640)), P < 0.001, I2: 72.6%], prolonged second stage of labor [OR: 5.539 (95% CI (4.252–7.199)), P < 0.001, I2: 0.0%], using oxytocin [OR: 4.207 (95% CI (3.100–5.709)), P < 0.001, I2: 0.0%], instrument -assisted vaginal delivery [OR: 5.578 (95% CI (4.285–7.260)), P < 0.001, I2: 65.1%], and macrosomia [OR: 5.32 (95% CI (2.738–10.339)), P < 0.001, I2: 95.1%] were factors associated with episiotomy practice.
Conclusion: In this review, the prevalence of episiotomy among African parturients was high. A selective episiotomy practice should be implemented to reduce the high episiotomy rates.
Systematic Review Registration: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42021293382, identifier: CRD42021293382.
An episiotomy is a vaginal and perineal surgical incision performed by a skilled birth attendant, to widen the vaginal opening (1, 2), late in the second stage when the perineum is stretched thin (3), and it is one of the most commonly performed surgical procedures all over the world (4). There are seven different ways to perform an episiotomy, with the two most common types in the literature and medical practice being “midline” and “mediolateral.” A midline (sometimes called “median”) episiotomy is a vertical incision from the posterior fourchette that runs along the midline through the central tendon of the perineal body. A mediolateral episiotomy is an incision beginning in the midline and directed laterally and downwards away from the rectum (2).
This surgical procedure is not without consequences as compared to permitting the perineum to tear. To begin with, episiotomy might be detrimental with respect to urinary incontinence symptoms (5). In a study conducted to assess the impact of episiotomy on the urogenital hiatus using transperineal ultrasound, the urogenital hiatal area was altered by episiotomy (6). In contrary, indicated use of episiotomy resulted in a significant decrease in third and fourth degree lacerations in a population-based observational study in Texas, United States of America (7).
According to a Cochrane database systematic review, women who had selective episiotomy experienced 30% less severe perineal trauma at birth than women who had a routine episiotomy policy. In terms of Apgar scores of <7 at 5 min, the number of women developing perineal infection, the number of women reporting painful sexual intercourse 6 months or more after delivery, and urinary incontinence 6 months or more after delivery, there was probably no or little difference reported. However, other significant long-term effects and outcomes were not reported in these trials (urinary fistula, rectal fistula, and fecal incontinence). As a result, the rationale for performing routine episiotomies to prevent severe perineal trauma was found to be unjustified, and there were no benefits to the baby or the mother from routine episiotomy (8).
Even when episiotomy technique is considered, mediolateral episiotomy does not appear to be protective against clinically or sonographically diagnosed obstetrical anal sphincter injuries (OASIS), and it was associated with decreased sexual functioning as well as sexual desire, arousal, and orgasm within the first 5 years after delivery (9). Furthermore, in a study conducted in 2015–2016 with the goal of describing the detailed epidemiology of labor and delivery in China, mediolateral episiotomy without indications more than doubled the risk of third and fourth degree perineal laceration in nulliparae without neonatal benefits, remembering the consequences of injudicious use of episiotomy (10). Prophylactic use of episiotomy in critical conditions such as shoulder dystocia, instrumental deliveries, occiput-posterior position, fetal macrosomia and non-reassuring fetal heart patterns don't prevent 3rd or 4th degree perineal tear (11). Nonetheless, a comparative, retrospective, mono-centric study in a university maternity unit in Besançon, France, found that selective episiotomy could reduce the incidence of perineal tears, particularly second-degree perineal tears, without increasing the rate of OASIS (12).
In order to combat the pain correlated with episiotomy, water birth has gained popularity globally, especially in midwifery- led care settings (13). Women's experiences with water birth matched groups in a prospective study by Lathrop et al. revealed that water birth was associated with a decreased likelihood of perineal lacerations (14). Furthermore, water immersion may reduce episiotomy rates (15, 16). Nonetheless, a lack of high-quality evidence clouded informed decisions about the advantages and disadvantages of water birth (17). Therefore, the merit and risks of water birth should be discussed thoroughly with the parturient during the process of informed decision making with mothers interested in this option (16).
Every year, ~140 million babies are born worldwide (18). In 2019, the United Nations (UN) estimated that the total fertility rate of Sub-Saharan Africa (SSA) would be at 4.7 births per woman from 2015 to 2020, which is more than double the level of any other region in the world (19). In concert with this, the rates of episiotomy practice have remained high worldwide, particularly in less industrialized countries and East Asia (20–22).
Reported rates of episiotomies vary greatly from one country to another across the globe. The lowest rate (1%) of episiotomy was reported in Sweden, whereas the highest (100%) was reported in Taiwan among primiparous parturients (23). Several countries have registered higher proportion of episiotomy practice.For instance, 58% in Italy in 1999; 66% in Oman in 2015; 67.5% in Poland in 2010; 68% in India in 2008; 75% in Cyprus;94 % in Cambodia; approximately 95% in Mexico among primiparous women (20, 23–28). In addition, significant number of women undergone episiotomy in Asian countries, 42–98% (23, 29, 30).
Furthermore, despite the standard recommendations that corroborate judicious use of episiotomy, increasing and variable patterns have been reported in Mexico: 41.8% in the state of Oaxaca and 77.2% in Mexico City (8, 25, 31). A sharp decline in episiotomy rates was reported in some countries like Turkey (93.3% in primipara women and 30.2% in multipara women in 2013) (1), France (18.6% from 2013 to 2017) (2), China (85.50% in 2003 to 41.7% in nulliparae and 21.5% in multiparae from 2015 to 2016) (3), the United States of America (20.3% in 2002 to 9.4% 2011 (4). Moreover, in Brazil episiotomy rate around the country declined from ~94% in 2000 (32) to 54% in 2014 (33) and 42% in 2019 (34), in Finland decreased from 71.5% in 1997–1999 to 54.9% in 2006–2007 among primiparous women, and from 21.5% in 1997–2001 to 9.2% in 2006–2007 among multiparous women (35). To summarize, the larger disparity in episiotomy rates around the world, as made evident by historical trends, is closely attributable to differences in episiotomy policies and resources (8, 20).
Individual and clinical factors related to mothers; individual and clinical factors related to the newborn; as well as the socio-demographic profiles of the parturient in Africa and other countries influence episiotomy practice (36). In studies conducted in Brazil (37, 38), Nigeria (39–42),Turkey (43), the United States (44), and Ethiopia (45, 46), the odds of episiotomy practice were positively correlated with younger age at delivery. Nonetheless, advanced maternal age (≥35) was reported as an attributable factor in some studies (37, 47–49).
According to Macleod et al. (50), Koskas et al. (51), Giannella et al. (52), Cromi et al. (48), Beyene et al. (53), Tobiaw Tefera et al. (54), Teshome et al. (46), and Pebolo et al. (55) episiotomy was significantly associated with a prolonged second stage of labor. Furthermore, macrosomia (42, 51, 53, 54, 56–58), advanced gestational age (49, 59, 60), breech presentation (50, 51, 57, 60–62), primiparity (40–42, 45, 46, 53, 56–58, 61, 63–65), oxytocin use (45, 53, 59, 62, 66, 67), meconium-stained amniotic fluid (49, 50), reduced apgar score (67), assisted breech vaginal delivery or vaginal operative delivery (forceps) (41, 42, 53, 54, 56, 58, 61, 63, 66), analgesia (49, 67, 68), non-reassuring fetal heart rate pattern (68), persistent occipito posterior position (41), post-term pregnancy (45), fetal distress (47, 69), perineal tear (66), private character of the mother (41), a history of gestational hypertension (45), birth spacing <2 years (66), vaginal birth after cesarean section (41), maternal under nutrition (64), history of episiotomy in their index delivery (70), and delivery attended by obstetricians and gynecologists (40, 57, 61) were found to be the risk factors documented in these studies. That said, the odds of episiotomy practice may vary within the African context and around the globe, and hence midwifes and obstetricians must better weigh the risks and benefits in order to predict and curb the impacts associated with liberal use of episiotomy (8).
Banta and his associate found four advantages to episiotomy. To begin with, it is claimed that a clean, straight incision is easier to repair and heals faster than a laceration or tear. Second, it is claimed that episiotomy results in fewer third-degree lacerations. Third, episiotomy is said to prevent fetal brain injury by lowering the fetal head's pressure on the pelvic floor. Fourth, episiotomy is said to shorten the second stage of labor, which helps to avoid pelvic floor damage (71). Additionally, episiotomy is justified in preeclampsia (72), in the event of abnormal cardiotocography, inability to control maternal blood pressure, imminent eclampsia, worsening biochemistry, or worsening maternal symptoms, for expeditious delivery of the newborn by shortening the second stage of labor and avoiding suffering for the baby (73). Finally, episiotomy requires laboring mothers to provide informed consent (74). Performing episiotomy without informed consent or with coerced consent is deemed to be instances of obstetric violence (16).
In Africa, although there has been no representative data, the reported rate of episiotomy ranged from 9.3% in a study conducted in South East Nigeria (40) to 73% in Uganda (55). Understanding the magnitude and risks associated with episiotomy can help adhere to existing or develop new protocols that are consistent with World Health Organization (WHO) (75) and American College of Obstetricians and Gynecologists (ACOG) recommendations that emphasize the judicious use of episiotomy (3). To date, there has been no systematic review and meta-analysis conducted to estimate the pooled prevalence and identify risk factors associated with episiotomy practice in Africa. Therefore, the current study aimed to address these two questions: (i) what is the continent's overall estimate of episiotomy practices? (ii) What are the factors that may influence episiotomy practices among African women who give birth in health facilities?
The goal of this systematic review and meta-analysis was to determine the pooled prevalence of episiotomy practice and the factors associated with it among African parturients who gave birth in public health facilities. The study protocol for this study was prepared and registered in the International Prospective Register of Systematic Reviews (PROSPERO) databases on 25/12/2021 (available from: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42021293382) we confirmed the absence of ongoing systematic reviews on this topic by following the guidance note for registering a Systematic Review Protocol to avoid duplication. The meta-analysis was reported using the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA)-Statement (76) (Supplementary File 1).
The inclusion criteria for this review were determined using the CoCoPop mnemonic (condition, context, and population). Population/Participants -parturient mothers who were reported to have undergone episiotomy at health facilities in Africa. Context-Observational Studies (descriptive and analytic cross-sectional studies, cohort studies, and case control studies) published in English between January 1, 2000 and December 31, 2021, spanning more than two decades due to a scarcity of primary studies. Condition-Studies that reported the outcome of interest based on the prevalence and risk factors associated with episiotomy practice were included in this review.
We excluded studies without full text access; articles that contained insufficient information; findings from personal opinions; articles reported outside the scope of the outcome of interest; qualitative study design; case reports; case series; letters; and previous systematic review.
It is an obstetric surgical procedure in which incisions are made in the vulva and perineum to allow for a smooth delivery of the newborn by creating enough space (3).
If the labor lasts longer than 2 h without epidural analgesia or 3 h with epidural analgesia in nulliparous women, or 1 h without or 2 h with epidural analgesia in multiparous women (77).
A new born birth weight ≥4,000 g (78).
Is a drug prescribed for laboring mothers for induction or augmentation of labor by enhancing uterine contraction (78).
Parity is determined by the number of pregnancies reaching the age of viability. A woman who has been delivered only once of a fetus or fetuses born alive or dead with an estimated length of gestation of above the age of viability is termed primiparity. Whereas, multipara is a woman who has completed two or more pregnancies to the age of viability (78).
When the fetal presenting part is the vertex or occiput in a laboring mother, labor begins spontaneously and the delivery is accomplished with minimal assistance (78).
Our search was restricted to articles published in English from January 1, 2000 to December 31, 2021. The electronic databases of PubMed, Hinari, Science Direct, Web of Science, African Journal of Online (AJOL), Cumulative Index to Nursing and Allied Health Literature (CINAHL), Excerpta Medica database (EMBASE), Google, Journal Storage (JSTOR), and Google scholar were searched. Using the snowballing method, the reference lists of the identified studies were also scrutinized to identify other relevant articles that were not captured during the initial search. We used key concepts to build a search strategy while conducting a comprehensive PubMed search. Initially, Medical Subject Headings (MeSH) terms relevant to our search were identified and added to the search builder. Next, we identified every possible keyword for each key concept and thoroughly used a combination of MeSH and keywords, truncating (*) of stems that are four letters or longer, putting double quotes ("“) around any multi-phrase, and adding field tags [tiab] and [tw] for each concept. Finally, after double checking that syntax was correct and Boolean operators were in all caps, we started running a search in the PubMed search box using a building block approach, which means we built the search one concept at a time and then combined concepts together at the end [“women*” (text word) OR “pregnant mother” (text word) OR “birth” (text word) OR (“pregnant women” (MeSH Terms) AND “women” (MeSH Terms)] AND [“episiotomy” (text word) OR “episiotomy practice” (text word) OR (“obstetric surgical procedures” MeSH Terms)] AND “episiotomy.” From January 1st to February 30th, 2022, two authors (BW and EA) participated in a double blinded search. The full search results were included as an additional file (Supplementary File 2).
The retrieved studies were exported to EndNote X7, which was then used to remove duplicate studies. After removal of duplicates, two authors (BW and MO) independently screened the titles and abstracts to determine the eligibility of studies. To describe the extent to which assessments by multiple authors are similar, the Cochrane handbook for systematic reviews of interventions was consulted. Values of kappa 0.75 (75 percent) were considered in this way, indicating excellent agreement. The screened articles were then subjected to a full article review by two independent authors (TI and HB). The inclusion and exclusion criteria were used to screen the articles.
The Joana Briggs Institute (JBI) critical appraisal checklists (79) were used to assess the quality of the studies. The methodological quality of each study was independently evaluated by two reviewers (EA and LT). Discrepancies were solved through discussion with a third independent reviewer (MS.O.). Hence, studies scoring 7 or above after evaluation against these criteria were included in this systematic review and meta-analysis. In this manner, for studies reporting only prevalence data, the following major components were evaluated: appropriateness of the sample frame for addressing the target population, sample size adequacy, study setting and participants, whether the data analysis was conducted with sufficient coverage of the identified sample, validity and reliability of the measurement, appropriateness of the statistical analysis, and adequacy and management of response rate (Supplementary File 3). For the analytical cross-sectional studies, the JBI checklist assessed the following main components: inclusion criteria, participants and settings, whether the exposure was measured in a valid and reliable way, whether the standard and objective criteria were used for measuring the outcome, confounding factors and strategies used to deal with them, whether the outcome was measured in a valid and reliable manner, and appropriateness of the statistical analysis (Supplementary File 4).
Using a standard Microsoft Excel spreadsheet, BW and MO independently extracted the relevant data. For data extraction, the JBI adopted formats were used (80). The author's name, study period and year of publication, methods and settings, age of the mothers, sample size and sampling procedure, data collection instrument, estimate of episiotomy practice with 95 percent confidence interval, response rate, and factors associated with episiotomy were all extracted. After retrieving data from 30% of the studies, the reliability agreement among the data extractors was assessed and confirmed using Cohan's kappa coefficient. As a result, the kappa coefficient's strength of agreement was classified as poor (≤ 0.20), fair (0.21–0.40), moderate (0.41–0.60), good (0.61–0.80), and almost perfect agreement (0.81–1) (81) and a kappa statistic value ≥0.5 was considered congruent and accepted. In the case of disagreements between the two data extractors, LT was involved in resolving them through discussion and re-checking of the original articles.
The number of parturients who received episiotomy was divided by the total number of parturients and multiplied by one hundred to calculate the pooled episiotomy practice among African parturients. The pooled effect was investigated using the OR. Furthermore, variables identified as a risk factor for episiotomy in at least three studies were taken into account.
To check for publication bias, we used Egger's statistical tests and funnel plots. The presence of publication bias was thus declared with a statistical significance of 5%. The I2-test was also used to determine heterogeneity. When the I2-test value was 25, 50, and 75%, heterogeneity was classified as mild, moderate, and high, respectively, across the studies.
All the extracted data was exported to STATA version 14 software for analysis. Due to the high heterogeneity among the included studies, the random-effects model was used for analysis. To find the source of heterogeneity, we used subgroup analysis based on African regions and meta-regression based on year of publication and sample size. The impact of the retrieved associated factors on the outcome variable was also investigated. Texts, forest plots, and tables were used to illustrate the findings of this systematic review and meta-analysis. The characteristics of the included studies were described using the OR with a 95% CI.
Our search was restricted to articles published in English between January 1, 2000 and December 31, 2021 in the electronic databases PubMed, Hinari, Science Direct, Web of Science, CINAHL, and EMBASE. In addition, Google, Google scholar, and AJOL were used. Through systematic and manual searching, 934 primary articles were found. Due to duplication, 770 articles were removed. The remaining 164 were screened based on their title and abstract, with 130 being eliminated as unrelated to our study. Finally, 34 full-text primary articles were evaluated against eligibility criteria, and 21 were selected for quantitative analysis (Figure 1).
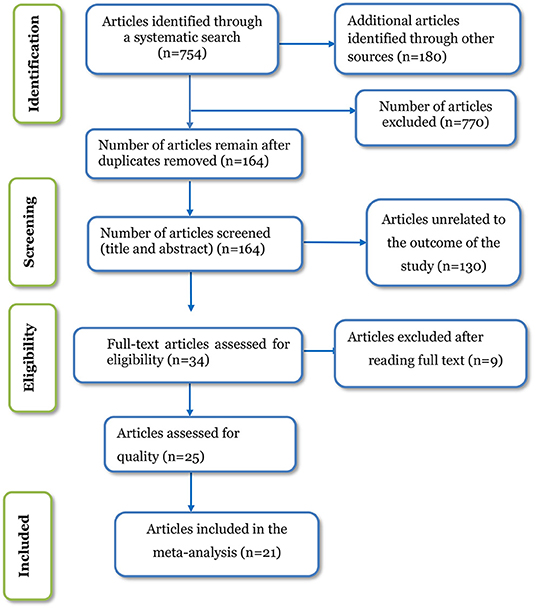
Figure 1. PRISMA flow diagram of included studies in the systematic review and meta-analysis of episiotomy practice and its associated factors in Africa, 2022.
This systematic review and meta-analysis included a total of 21 articles from seven African countries. Eighteen primary studies employed an analytical cross-sectional study design, while the remaining three studies employed a descriptive cross-sectional study design. Regarding the settings in which the studies were conducted eight studies were conducted in Ethiopia (45, 46, 54, 57, 61, 64, 66), eight in Nigeria (40–42, 58, 63, 65, 82), and the remainder of the studies were conducted in the Democratic Republic of the Congo (DRC) (69), Zimbabwe (83), Uganda (55), Ghana (84), and Burkina Faso (85). The majority of the studies, 16 (76.2%), were reported from Eastern and Western African countries. The number of study participants ranged from 249 (55), in a study conducted in Uganda to 12,168 (56) in Nigeria. Out of 40,831 women, episiotomy was practiced on 15,437 of them. The highest prevalence of episiotomy practice was reported in a study from Uganda, at 73% (55), followed by Ethiopia, at 68% (64). On the contrary, the lowest rate of episiotomy, 9.3%, was reported in a study from Nigeria (40). In this meta-analysis, 17 of the 21 studies reported a percentage of episiotomy practice in primiparous and multiparous women (40–42, 45, 46, 53, 54, 56–58, 61, 63–66, 69, 83), while the other four studies did not (55, 82, 84, 85). The mean age of the study participants was not reported in ~66.7% of the studies (40, 46, 55, 56, 58, 63, 64, 66, 69, 82–84). Among the studies that reported the age of the study subjects, the mean age of women for whom episiotomy was performed was 25.57 years (41, 45, 53, 54, 57, 61, 85). The year of publication of the included studies ranged from 2003 to 2021 (Table 1).
Regarding the sampling techniques and data collection tools, nine studies employed systematic random sampling methods (45, 46, 53–55, 57, 61, 64, 66), eleven studies employed either retrospective (40–42, 56, 58, 63, 65, 82–84) or prospective (85) analysis of delivery notes, while the remaining one study employed stratified sampling methods (69). Furthermore, pre-tested questionnaires and refined checklists were used to collect data (Supplementary File 5).
This systematic review and meta-analysis included 21 studies to estimate the pooled prevalence of episiotomy practice among African parturients who gave birth in health facilities. The heterogeneity (I2) of the included studies was (I2 = 99.3%; P < 0.001) when using the fixed effect model. Due to the high heterogeneity of the data, we used a random effects model to estimate the pooled prevalence of episiotomy practice, which was 41.7% [95% CI (36.0–47.4)] (Figure 2).
In addition, supplementary analysis was performed on 17 of the 21 studies that reported the magnitude of episiotomy in primiparous (n = 11,555) and multiparous women (n = 24,252) to estimate the percentage of episiotomy practiced. As a result, the combined prevalence of episiotomy among primiparous and multiparous women was 64.4% [(95% CI: 55.6–73.1), I2 = 99.2%, P < 0.001] and 26.3% [(95% CI: 20.6–31.9), I2 = 99.1%, P < 0.001] among primiparous (Figure 3) and multiparous (Figure 4) respectively.
We used subgroup analysis based on African regions, as well as meta-regression based on year of publication and sample size, to find the source of heterogeneity.
As shown in Figure 5, a significant variation in episiotomy practice can be seen across the three regions in Africa. Episiotomy was most performed in central Africa 50 % [(95% CI: 47.74–52.26), I2 = .%, P < 0.001] (69). East Africa came in second with 47.7% [(95% CI: 36.55–58.44), I2 = 98.7 %, p < 0.001] (45, 46, 53, 54, 57, 61, 64, 66, 83). In western African countries, episiotomy was performed in 35.01% [(95% CI: 26.99–43.02), I2 = 99.6%, p < 0.001] (40–42, 56, 58, 63, 65, 82, 84, 85) of parturients. Of the 21 included studies, 10 studies were reprorted from East African countries, while ten studies and one study were reported from westAfrican, and central African countries respectively.
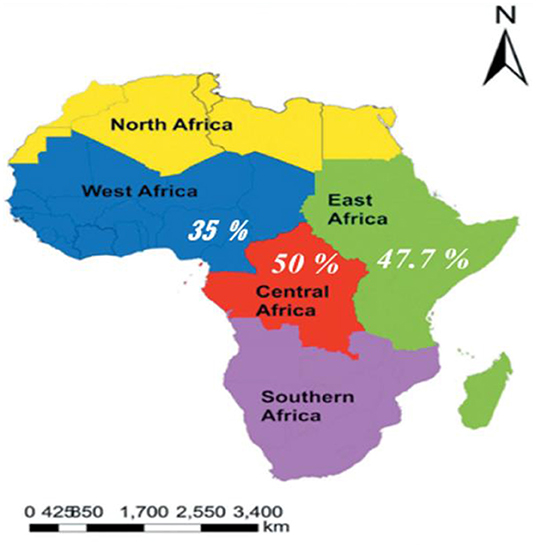
Figure 5. Subgroup analyses on the pooled prevalence of episiotomy practice by African regions, 2022 (source: https://en.wikipedia.org/wiki/List_of_regions_of_Africa).
Based on sample size and publication year, we used random-effects meta regression to find the source of heterogeneity at a 5% significance level. As shown in Table 2, these covariates were not found to be the source of heterogeneity.
We used the random-effects model to perform sensitivity analysis to determine the impact of a single study on the overall meta-analysis. The results of the analysis revealed that single study estimates are closer to the combined estimate, implying that a single study has no effect on the final pooled prevalence of episiotomy practice (Table 3).
All studies fell within the funnel plot based on subjective inspection (Figure 6). Furthermore, neither Egger's linear regression test (t = 0.16, P = 0.260) nor Begg's rank correlation test (z = 0.15, P = 0.880) were statistically significant (Table 4).
The pooled odds ratio was used to identify factors linked to episiotomy practice, and the association with the outcome variable was declared at a 5% significant level. As a result, eight variables were extracted from at least three studies. Six variables were found to be predictors of episiotomy performance: birth attendant, mode of delivery, oxytocin use, prolonged second stage of labor, birth weight, and parity.
This study revealed that primiparous women had 6.78 times more likelihood of incurring an episiotomy as compared to multiparous women [OR: 6.796 (95% CI (4.862–9.498)), P < 0.001, I2: 95.1%].Furthermore, episiotomy was 3.7 times more likely to be practiced when medical doctors attended the delivery compared to midwives [OR: 3.675 (95% CI (2.034–6.640)), P < 0.001, I2: 72.6%]. In this study, the second stage of labor delayed for more than 2 h was 5.5 times more likely to end up with an episiotomy [OR: 5.539 (95% CI (4.252–7.199)), P < 0.001, I2: 0.0%].
In the current review, laboring mothers who were given oxytocin for labor augmentation were 4.21 times more likely to undergo episiotomy when compared to their counterparts [OR: 4.207 (95% CI (3.100–5.709)), P < 0.001, I2: 0.0%]. Regarding the mode of delivery, mothers whose labor was assisted by instrumental vaginal delivery were 5.58 times more likely to undergo episiotomy compared to those delivered by spontaneous vertex delivery [OR: 5.578 (95% CI (4.285–7.260)), P < 0.001, I2: 65.1%]. Furthermore, the findings from the current review revealed that the odds of episiotomy practice were 5.32 times more likely when the fetal birth weight was ≥4,000 g [OR: 5.32 (95% CI (2.738–10.339)), P < 0.001, I2: 95.1%] compared to the normal birth weight (Table 5).
The aim of this meta-analysis was to find out how common episiotomy was and what factors were linked to it. This review included twenty-one studies in order to summarize the extent of episiotomy use and identify associated factors among African women who gave birth in public health facilities. These results have been obtained from research conducted in a number of African countries. The routine use of episiotomy, according to researchers, increases the risk of perineal trauma (27). All international organizations, including the WHO, agree with the body of evidence that routine episiotomy has no place in the modern era of advanced maternal care (75). Furthermore, the 2006 ACOG bulletin did not recommend the routine use of episiotomy (3).
Nonetheless, a remarkable spectrum of episiotomy practice has been observed among countries around the globe (82). The current review found that the pooled prevalence of episiotomy practices among laboring mothers in Africa was 41.7 [95% CI (36.0–47.4)] for all vaginal deliveries. There is a wide difference in episiotomy practice from region to region within the African continent. The sample size, year of publication, and settings where the studies were conducted might have contributed to a high and uneven spectrum of episiotomy. Furthermore, such disparities may indicate a lack of evidence-based standardized policy, training, and practice across the continent. Another possible explanation for the variation in episiotomy practices among African countries could be the preference to employ episiotomy frequently because of the simultaneous belief that allowing even minor perineal tears is more cumbersome than repair when an episiotomy cut is performed.
In the current review, the rate of episiotomy for all vaginal deliveries is by far higher than previous studies carried out in Denmark, 4.9% (20), Sweden, 6.6% (20), Nigeria, 7% (40), the United States in 2011, 9.4% (20), Ghana, 17% (84), United Kingdom (UK) in 2011/2012, 15.20% (20), Burkina Faso, 21% (85), in rural Zimbabwe, 26% (83), Hong Kong, 27% (86), Vietnamese-born women living in Australia, 29.9% (30), Slovania, 31.3% in 2013 (87), and 14.3% in France (88). A significant and continuing decline in the rate of episiotomy practices in some countries over the years may be attributed to the adoption of clinical practice guidelines advocating the policy of restricted episiotomy use. Clesse et al. (88), for instance, found a remarkable and persistent decline in the episiotomy figure 7.3 of percentage points and a rate of change of 34% from 2013.
Similarly, the episiotomy rate in all vaginal deliveries in the United States fell from 60.9% in 1979 to 24.5% in 2004 (89), and the rate in Hong Kong fell from 73% in 2003 to 27% in 2008 (86). In contrast, the pooled estimate for episiotomy practice, in all vaginal deliveries, in this meta-analysis was lower than in a study conducted in India, where 63.4% (90), Oman, 66% (27), Portugal, 72.9% in 2010 (20), Mexico City, 77.2% (25), Turkey, 93.3% (91), Phnom Penh, Cambodia, 94.5% (28), and Taiwan, 100% (23), which may suggest liberal use in these countries.
This systematic review and meta-analysis also identified potential determinants of episiotomy practices among parturients in Afrika. Thus, primiparity was found to be significantly associated with the use of episiotomy, which is supported by the findings of other previous studies (30, 68). Another study also found that primiparas were more likely to undergo episiotomy than multiparas (28). The results of this review are also in line with those of previous studies conducted in Ethiopia (45, 46, 53, 57, 61, 64), Nigeria (40–42, 56, 58, 63, 65), Brazil (92), Vietnam (93), Iran (67), Saudi Arabia (94), Latin America (59), France (68), East African migrants in Australia (95), Taiwan (96), and Vietnam born women in Australia (30). The potential explanation may be that episiotomies are thought to speed up the second stage of labor and reduce the risk of spontaneous perineal tears, but such perceptions among obstetricians or midwives have not been supported by evidence.
Fetal macrosomia is common in obstetrics with problems in both the mother and newborn. The current review also showed that newborn birth weight ≥4,000 g was another risk factor associated with the practice of episiotomy compared with normal birth weight, which coincides with the findings reported in studies carried out in Ethiopia (53, 54, 57), France (51), and Nigeria (42, 56, 82). Other than newborns', fetal macrosomia causes maternal complications during delivery, such as 3rd or 4th degree perineal tears (97, 98). Rates of episiotomy, and other morbidities and mortality associated with predicted macrosomia could be reduced by cesarean deliveries (99). However, when such prenatal screening is not available as in underdeveloped countries, it contributes to high magnitudes of episiotomy.
Statistical analysis of this result also indicates that a protracted second stage of labor is among the important risk factors positively associated with episiotomy. This finding is also supported by studies conducted in Iran (67), Spain (100), and Brazil (92). When mothers exert themselves in labor for more than 2 h, they usually become exhausted. Moreover, inadequate provision of maternal support will also result in prolonged labor. This time, the attending healthcare professional is forced to perform an episiotomy cut to alleviate or reduce morbidity to the fetus (53).
In present study, laboring mothers who had used oxytocin for the induction or augmentation of labor had higher odds of being exposed to episiotomy than their counterparts. Our results concur with the findings in Iran (67), Brazil (92), Vietnam (30), and Latin America (32). Similarly this review is congruent with a study conducted in Shroud City, northeast Iran (67). The potential explanation could be due to oxytocin induced uterine hyper stimulation which in turn which may affect the normal beat to beat variability during labor resulting in non-reassuring fetal heart rate patterns. In such cases episiotomy is usually performed for expeditious delivery of the baby in an attempt to shorten labor time.
None spontaneous vertex deliveries (vacuum-assisted, forceps, and assisted breech deliveries) were another risk factor for episiotomy practice in laboring mothers compared with spontaneous vertex delivery and it is in line with previous studies conducted in other settings (32, 37, 67, 94). Such a correlation may arise from tertiary hospitals' endeavors to handle abnormal labor, complex and advanced maternity care. Therefore, doctors and midwives may perform an episiotomy to decrease perineal tears in such a situation.
The other finding from this study is that deliveries attended by doctors were positively associated with episiotomy practice compared with deliveries attended by midwives. Similar findings have been observed in other settings (40, 57, 61). One of the reasons might be that abnormal labors are frequently attended by medical doctors and, hence, episiotomies are performed liberally to support and assist the labor process with forceps or vacuum delivery.
The limitations of this systematic review have been acknowledged. Some studies did not contain sufficient predictor variables to adequately determine the degree of prediction. However, attempts were made to include all other potential variables across the identified databases. Furthermore, in this review, the study method used in all included articles was a cross-sectional design. As a result, the outcome variable might be affected by other confounding variables, which would decrease the power of the study and the causal conclusion between episiotomy and its associated factors. In the current meta-analysis, all included studies were conducted in African countries in three regions: Eastern Africa, Central Africa, and Western Africa. Therefore, it might lack continental representativeness because no information was found in the northern and southern regions of the African continent. However, the maternal health care and health care facilities in these regions are not different from those in other regions of the continent. Furthermore, the results of this review should be interpreted cautiously as there is significant heterogeneity in pooled effect estimates.
The protocol for this study has been registered. More than seven online databases were searched to avoid missing published studies, including articles published in African journals. In addition, a manual search was performed to retrieve the article using Google Scholar. During the selection of articles, the PRISMA guidelines were strictly followed, and the articles were closely assessed for their quality using the newly amended JBI critical appraisal tool. Furthermore, we used broader inclusion criteria to include articles published from 2000 to 2021GC. In studies that reported percent of episiotomy in both primiparous and multiparous parturients, additional analysis was performed. A sensitivity analysis was also carried out.
The pooled random effect meta-analysis revealed that the prevalence of episiotomy practice among laboring mothers in Africa was high when compared to existing global recommendations, including those from the WHO. Furthermore, primiparity, macrosomia, prolonged second stage of labor, instrument assisted vaginal deliveries, augmented or induced labor using oxytocin, and deliveries attended by medical doctors were independent predictors of episiotomy practice in African health facilities.
As a result, we recommend that African countries adopt a restrictive episiotomy policy to lower their rates and limit morbidity associated with injudicious episiotomy practice. To reduce the risks associated with macrosomia, prenatal screening with obstetric ultrasound and cesarean section delivery should be encouraged. Countries should either follow international guidelines like WHO and ACOG recommendations or create their own protocols. To change current beliefs about episiotomy in primiparous women, more in-service training for midwives and obstetricians is required. Episiotomy should only be performed when there is a clear indication or when evidence supports it.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
BW and MO involved in selection of study, data extraction, quality assessment, statistical analysis, results interpretation and writing the initial, and final drafts of the manuscript. EB, LT, TB, and HA were involved in data extraction, quality assessment, statistical analysis, and writing drafts of the manuscript. All authors proofread and approved the final manuscript.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
We would like to express our gratitude to all of the authors of the articles included in this study.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2022.905174/full#supplementary-material
ACOG, American College of Obstetricians and Gynecologists; CI, Confidence Interval; JBI, Johanna Briggs Institute; OR, Odds Ratio; PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses; USA, United States of America; WHO, World Health Organization.
1. Thacker S, Banta H. Benefits and risks of episiotomy: an interpretive review of the English language literature, 1860-1980. Obstet Gynecol Survey. (2003) 38:322–38. doi: 10.1097/00006254-198306000-00003
2. Kalis V, Laine K, de Leeuw JW, Ismail KM, Tincello DG. Classification of episiotomy: towards a standardisation of terminology. BJOG. (2012) 119:522–6. doi: 10.1111/j.1471-0528.2011.03268.x
3. American College of Obstetricians-Gynecologists. ACOG practice bulletin. episiotomy. Clinical management guidelines for obstetrician-gynecologists. number 71, April 2006. Obstet Gynecol. (2006) 107:957–62.
4. Löwenstein L, Drugan A, Gonen R, Itskovitz-Eldor J, Bardicef M, Jakobi P. Episiotomy: beliefs, practice and the impact of educational intervention. Euro J Obstetr Gynecol Reprod Biol. (2005) 123:179–82. doi: 10.1016/j.ejogrb.2005.04.006
5. Frigerio M, Mastrolia SA, Spelzini F, Manodoro S, Yohay D, Weintraub AY. Long-term effects of episiotomy on urinary incontinence and pelvic organ prolapse: a systematic review. Arch Gynecol Obstet. (2019) 299:317–25. doi: 10.1007/s00404-018-5009-9
6. Cassado Garriga J, Carmona Ruiz A, Pessarrodona Isern A, Rodriguez Carballeira M, Esteve Serena E, Garcia Manau P, et al. Impact of episiotomy on the urogenital hiatus using transperineal ultrasound. Neurourol Urodyn. (2018) 37:434–9. doi: 10.1002/nau.23322
7. Dillon SJ, Nelson DB, Spong CY, McIntire DD, Leveno KJ. Episiotomy: evolution of a common obstetric practice at a public hospital. Am J Perinatol. (2021) 1620–35. doi: 10.1055/s-0041-1739410
8. Jiang H, Qian X, Carroli G, Garner P. Selective versus routine use of episiotomy for vaginal birth. Cochrane Database Syst Rev. (2017) 2:Cd000081. doi: 10.1002/14651858.CD000081.pub3
9. Dogan B, Gün I, Özdamar Ö, Yilmaz A, Muhçu M. Long-term impacts of vaginal birth with mediolateral episiotomy on sexual and pelvic dysfunction and perineal pain. J Mater Fetal Neonatal Med. (2017) 30:457–60. doi: 10.1080/14767058.2016.1174998
10. Ye J, Chen Y, Yang H, Chen Q, Huang Y, Zhao J, et al. A nationwide cross-sectional survey of episiotomy practice in China. Lancet Reg Health West Pac. (2022) 19:100345. doi: 10.1016/j.lanwpc.2021.100345
11. Steiner N, Weintraub AY, Wiznitzer A, Sergienko R, Sheiner E. Episiotomy: the final cut? Arch Gynecol Obstet. (2012) 286:1369–73. doi: 10.1007/s00404-012-2460-x
12. Forey P-L, Lallemant M, Bourtembourg-Matras A, Eckman-Lacroix A, Ramanah R, Riethmuller D, et al. Impact of a selective use of episiotomy combined with Couder's maneuver for the perineal protection. Arch Gynecol Obstet. (2020) 302:77–83. doi: 10.1007/s00404-020-05572-9
13. Cluett ER, Burns E, Cuthbert A. Immersion in water during labour and birth. Cochrane Database Syst Rev. (2018) 5:CD000111. doi: 10.1002/14651858.CD000111.pub4
14. Lathrop A, Bonsack CF, Haas DM. Women's experiences with water birth: a matched groups prospective study. Birth. (2018) 45:416–23. doi: 10.1111/birt.12362
15. Aughey HK, Jardine J, Moitt N, Fearon K, Hawdon J, Pasupathy D, et al. Waterbirth: a national retrospective cohort study of factors associated with its use in 46,088 women in England. Res Square. (2020) 2–9. doi: 10.21203/rs.3.rs-93490/v1
16. Zaami S, Stark M, Beck R, Malvasi A, Marinelli E. Does episiotomy always equate violence in obstetrics? Routine and selective episiotomy in obstetric practice and legal questions. Eur Rev Med Pharmacol Sci. (2019) 23:1847–54. doi: 10.26355/eurrev_201903_17219
17. Zaami S, Zupi E, Lazzeri L, Centini G, Stark M, Malvasi A, et al. Episiotomy: a medicolegal vicious cycle. Panminerva Med. (2020) 63:224–31. doi: 10.23736/S0031-0808.20.03946-4
18. Olusanya BO, Teeple S, Kassebaum NJ. The contribution of neonatal jaundice to global child mortality: findings from the GBD 2016 study. Pediatrics. (2018) 141:e20171471. doi: 10.1542/peds.2017-1471
19. United Nations Department Department of Economics and Social Affairs Population Division. World Population Prospects: The 2019 Revision. Volume 1. Comprehensive Tables. United Nations, Department of Economics and Social Affairs, Population Division, New York (2019).
20. Clesse C, Lighezzolo-Alnot J, De Lavergne S, Hamlin S, Scheffler M. Statistical trends of episiotomy around the world: comparative systematic review of changing practices. Health Care Women Int. (2018) 39:644–62. doi: 10.1080/07399332.2018.1445253
21. Danilack VA, Nunes AP, Phipps MG. Unexpected complications of low-risk pregnancies in the United States. Am J Obstet Gynecol. (2015) 212:809. e1–809. e6. doi: 10.1016/j.ajog.2015.03.038
22. Chandraharan E. Intrapartum care: an urgent need to question historical practices and ‘non-evidence'-based, illogical foetal monitoring guidelines to avoid patient harm. J Pat Saf Risk Manage. (2019) 24:210–7. doi: 10.1177/2516043519878583
23. Graham ID, Carroli G, Davies C, Medves JM. Episiotomy rates around the world: an update. Birth. (2005) 32:219–23. doi: 10.1111/j.0730-7659.2005.00373.x
24. Friedman AM, Ananth CV, Prendergast E, D'Alton ME, Wright JD. Variation in and factors associated with use of episiotomy. JAMA. (2015) 313:197–9. doi: 10.1001/jama.2014.14774
25. Garcia-Cerde R, Torres-Pereda P, Olvera-Garcia M, Hulme J. Health care workers' perceptions of episiotomy in the era of respectful maternity care: a qualitative study of an obstetric training program in Mexico. BMC Pregnancy Childbirth. (2021) 21:549. doi: 10.1186/s12884-021-04022-x
26. Seijmonsbergen-Schermers A, Geerts C, Prins M, Van Diem M, Klomp T, Lagro-Janssen A, et al. The use of episiotomy in a low-risk population in the Netherlands: a secondary analysis. Birth. (2013) 40:247–55. doi: 10.1111/birt.12060
27. Al-Ghammari K, Al-Riyami Z, Al-Moqbali M, Al-Marjabi F, Al-Mahrouqi B, Al-Khatri A, et al. Predictors of routine episiotomy in primigravida women in Oman. Appl Nurs Res. (2016) 29:131–5. doi: 10.1016/j.apnr.2015.05.002
28. Schantz C, Sim KL, Ly EM, Barennes H, Sudaroth S, Goyet S. Reasons for routine episiotomy: a mixed-methods study in a large maternity hospital in phnom Penh, Cambodia. Reprod Health Matters. (2015) 23:68–77. doi: 10.1016/j.rhm.2015.06.012
29. Lam K, Wong H, Pun T. The practice of episiotomy in public hospitals in Hong Kong. Hong Kong Med J. (2006) 12:94.
30. Trinh AT, Khambalia A, Ampt A, Morris JM, Roberts CL. Episiotomy rate in vietnamese-born women in Australia: support for a change in obstetric practice in Viet Nam. Bull World Health Organ. (2013) 91:350–6. doi: 10.2471/BLT.12.114314
31. Hartmann K, Viswanathan M, Palmieri R, Gartlehner G, Thorp J, Lohr KN. Outcomes of routine episiotomy: a systematic review. JAMA. (2005) 293:2141–8. doi: 10.1001/jama.293.17.2141
32. Althabe F, Belizán JM, Bergel E. Episiotomy rates in primiparous women in Latin America: hospital based descriptive study. BMJ. (2002) 324:945–6. doi: 10.1136/bmj.324.7343.945
33. Lansky S, Friche AAL, Silva AAM, Campos D, Bittencourt SDA, Carvalho ML, et al. Birth in Brazil survey: neonatal mortality, pregnancy and childbirth quality of care. Cad Saude Publica. (2014) 30:S192–207. doi: 10.1590/0102-311X00133213
34. Cunha CMP, Katz L, Lemos A, Amorim MKnowledge M. Attitude and practice of brazilian obstetricians regarding episiotomy. Rev Bras Ginecol Obstet. (2019) 41:636–46. doi: 10.1055/s-0039-3400314
35. Räisänen S, Vehviläinen-Julkunen K, Gisler M, Heinonen S. A population-based register study to determine indications for episiotomy in Finland. Int J Gynecol Obstet. (2014) 115:26–30. doi: 10.1016/j.ijgo.2011.05.008
36. Clesse C, Lighezzolo-Alnot J, De Lavergne S, Hamlin S, Scheffler M. Factors related to episiotomy practice: an evidence-based medicine systematic review. J Obstet Gynaecol. (2019) 39:737–47. doi: 10.1080/01443615.2019.1581741
37. de Carvalho CCM, Souza ASR, Moraes Filho OB. Prevalence and factors associated with practice of episiotomy at a maternity school in Recife, Pernambuco, Brazil. Rev Assoc Med Bras. (2010) 56:333–9. doi: 10.1590/S0104-42302010000300020
38. da Silva FM, de Oliveira SM, Bick D, Osava RH, Tuesta EF, Riesco ML. Risk factors for birth-related perineal trauma: a cross-sectional study in a birth centre. J Clin Nurs. (2012) 21:2209–18. doi: 10.1111/j.1365-2702.2012.04133.x
39. Ezegwui H, Ikeako L, Ogbuefi F. Obstetric outcome of teenage pregnancies at a tertiary hospital in Enugu, Nigeria. Niger J Clin Pract. (2012) 15:147–50. doi: 10.4103/1119-3077.97289
40. Owa O, Eniowo A, Ilesanmi O. Factors associated with episiotomy among parturients delivering in a tertiary care centre in Nigeria. Int J Res Med Sci. (2015) 3:836. doi: 10.5455/2320-6012.ijrms20150403
41. Chigbu B, Onwere S, Aluka C, Kamanu C, Adibe E. Factors influencing the use of episiotomy during vaginal delivery in South Eastern Nigeria. East Afr Med J. (2008) 85:240–3. doi: 10.4314/eamj.v85i5.9618
42. Alayande BT, Amole IO, Akin D. Relative frequency and predictors of episiotomy in Ogbomoso, Nigeria. Internet J Med Update. (2012) 7:41–4. Available online at: http://www.akspublication.com/ijmu
43. Demirci O, Yilmaz E, Tosun Ö, Kumru P, Arinkan A, Mahmutoglu D, et al. Effect of young maternal age on obstetric and perinatal outcomes: results from the tertiary center in Turkey. Balkan Med J. (2016) 33:344–9. doi: 10.5152/balkanmedj.2015.150364
44. Kozhimannil KB, Karaca-Mandic P, Blauer-Peterson CJ, Shah NT, Snowden JM. Uptake and utilization of practice guidelines in hospitals in the United States: the case of routine episiotomy. Joint Comm J Qual Pat Saf. (2017) 43:41–8. doi: 10.1016/j.jcjq.2016.10.002
45. Kidane GG, Gebrehiwot H, Abay M, Darie Getachew TW. Episiotomy practice and its associated factors among mothers who gave birth vaginally at public health institutions of Shire Town, Northern Ethiopia. Res Rev J Health Prof. (2016) 6:1–8.
46. Teshome Y, Mekonen M, Sisay T, Chala G, Mengistu A, Shewasinad S, et al. Prevalence of episiotomy and its associated factors in university of gondar comprehensive specialized referral hospital: a retrospective study from Ethiopia. Am J Life Sci. (2020) 8:9. doi: 10.11648/j.ajls.20200801.12
47. Wu LC, Malhotra R, Lie D, Tan TC, Østbye T. Risk factors and midwife-reported reasons for episiotomy in women undergoing normal vaginal delivery. Arch Gynecol Obstet. (2014) 288:1249–56. doi: 10.1007/s00404-013-2897-6
48. Cromi A, Bonzini M, Uccella S, Serati M, Bogani G, Pozzo N, et al. Provider contribution to an episiotomy risk model. J Mater Fetal Neonatal Med. (2015) 28:2201–6. doi: 10.3109/14767058.2014.982087
49. Shmueli M, Gabbay Benziv R, Hiersch L, Ashwal E, Aviram R, Yogev Y, et al. Episiotomy–risk factors and outcomes. J Mater Fetal Neonatal Med. (2017) 30:251–6. doi: 10.3109/14767058.2016.1169527
50. Macleod M, Strachan B, Bahl R, Howarth L, Goyder K, Van de Venne M, et al. A prospective cohort study of maternal and neonatal morbidity in relation to use of episiotomy at operative vaginal delivery. BJOG. (2008) 115:1688–94. doi: 10.1111/j.1471-0528.2008.01961.x
51. Koskas M, Caillod A, Fauconnier A, Bader G. Maternal and neonatal consequences induced by the French recommendations for episiotomy practice. Monocentric study about 5409 vaginal deliveries. Gynecol Obstet Fertil. (2009) 37:697–702. doi: 10.1016/j.gyobfe.2009.06.003
52. Giannella L, Mfuta K, Pedroni D, Delrio E, Venuta A, Bergamini E, et al. Delays in the delivery room of a primary maternity unit: a retrospective analysis of obstetric outcomes. J Mater Fetal Neonatal Med. (2013) 26:593–7. doi: 10.3109/14767058.2012.745500
53. Beyene F, Nigussie AA, Limenih SK, Tesfu AA, Wudineh KG. Factors associated with episiotomy practices in Bahirdar city, Ethiopia: a cross-sectional study. Risk Manag Healthc Policy. (2020) 13:2281–9. doi: 10.2147/RMHP.S277657
54. Tobiaw Tefera MBK, Mekonen T. Prevalence of episiotomy and factors associated with practice of episiotomy at Saint Paul's hospital millennium medical college: a cross sectional study. Ethiop J Reproduct Health. (2019) 11:1–8.
55. Pebolo F, Judith A, Kabonge Dan K. Prevalence and factors associated with episiotomy practice among primiparous women in mulago national referral hospital Uganda. Int J Preg Child Birth. (2019) 5:197–201. doi: 10.15406/ipcb.2019.05.00176
56. Ayyuba R, Garba I, Ozegya M, Abubakar I. Episiotomy at aminu kano teaching hospital, Kano, Nigeria: a 3-year review. Arch Int Surg. (2016) 6:17. doi: 10.4103/2278-9596.187202
57. Worku SA, Mitku YM, Getahun SA. Episiotomy-practice-and-its-associated-factor-among-women-who-gave-birth-at-public-health-institutions-of-akaki-kality. Clin Mother Child Health. (2019) 16:1–6. doi: 10.4172/2090-7214.1000318
58. Okeke T, Ugwu E, Okezie O, Enwereji J, Ezenyeaku C, Ikeako L. Trends and determinants of episiotomy at the University of nigeria teaching hospital (UNTH), Enugu, Nigeria. Niger J Med. (2012) 21:304–7. Available online at: https://www.ajol.info/index.php/njm/article/view/91062
59. Ballesteros-Meseguer C, Carrillo-García C, Meseguer-de-Pedro M, Canteras-Jordana M, Martínez-Roche M. Episiotomy and its relationship to various clinical variables that influence its performance. Rev Lat Am Enfermagem. (2016) 24:e2793. doi: 10.1590/1518-8345.0334.2686
60. Lesieur E, Blanc J, Loundou A, Dubuc M, Bretelle F. Can the rate of episiotomy still be lowered? Status update in PACA region (south of France). Gynecol Obstet Fertil Senol. (2017) 45:146–51. doi: 10.1016/j.gofs.2017.01.007
61. Yemaneh Y, Sahile E, Alehegn A, Girma A, Robles C. Assessment of the proportion and associated factors of episiotomy at public health institutions of Axum town, Tigray Region, North Ethiopia. Crit Care Obst Gyne. (2015) 11:1–7. doi: 10.21767/2471-9803.1000152
62. Chuilon A, Le Ray C, Prunet C, Blondel B. Episiotomy in France in 2010: Variations according to obstetrical context and place of birth. J Gynecol Obstet Biol Reprod. (2016) 45:691–700. doi: 10.1016/j.jgyn.2015.10.005
63. Enyindah C, Fiebai P, Anya S, Okpani A. Episiotomy and perineal trauma prevalence and obstetric risk factors in Port Harcourt, Nigeria. Niger J Med. (2007) 16:242–5.
64. Fikadu K, Boti N, Tadesse B, Mesele D, Aschenaki E, Toka E, et al. Magnitude of episiotomy and associated factors among mothers who give birth in arba minch general hospital, southern ethiopia: observation-based cross-sectional study. J Pregnancy. (2020) 2020:8395142. doi: 10.1155/2020/8395142
65. Onah HE, Akani CI. Rates and predictors of episiotomy in Nigerian women. Trop J Obstet Gynaecol. (2004) 21:44–5. doi: 10.4314/tjog.v21i1.14463
66. Woretaw E, Teshome M, Alene M. Episiotomy practice and associated factors among mothers who gave birth at public health facilities in Metema district, northwest Ethiopia. Reprod Health. (2021) 18:142. doi: 10.1186/s12978-021-01194-9
67. Rasouli M, Keramat A, Khosravi A, Mohabatpour Z. Prevalence and factors associated with episiotomy in Shahroud City, northeast of Iran. Int J Womens Health Reprod Sci. (2016) 4:125–9. doi: 10.15296/ijwhr.2016.29
68. Goueslard K, Cottenet J, Roussot A, Clesse C, Sagot P, Quantin C. How did episiotomy rates change from 2007 to 2014? Population-based study in France. BMC Pregnancy Childbirth. (2018) 18:208. doi: 10.1186/s12884-018-1747-8
69. Innocent N, Philémon MM, Prince I, Justine Y, Ntakwinja M, Olivier N, et al. Factors associated with episiotomy practice in Bukavu, Democratic Republic of the Congo. Int J Reprod Contracept Obstet Gynecol. (2018) 7:2553. doi: 10.18203/2320-1770.ijrcog20182860
70. Zilberman A, Sheiner E, Barrett O, Hamou B, Silberstein T. Once episiotomy, always episiotomy? Arch Gynecol Obstet. (2018) 298:121–4. doi: 10.1007/s00404-018-4783-8
71. Banta D, Thacker SB. The risks and benefits of episiotomy: a review. Birth. (1982) 9:25–30. doi: 10.1111/j.1523-536X.1982.tb01599.x
72. Steegers EA, Von Dadelszen P, Duvekot JJ, Pijnenborg R. Pre-eclampsia. Lancet. (2010) 376:631–44. doi: 10.1016/S0140-6736(10)60279-6
73. English FA, Kenny LC, McCarthy FP. Risk factors and effective management of preeclampsia. Integr Blood Press Control. (2015) 8:7. doi: 10.2147/IBPC.S50641
74. Malvasi A, Trojano G, Tinelli A, Marinelli E, Zaami S. Episiotomy: an informed consent proposal. J Matern Fetal Neonatal Med. (2021) 34:948–951. doi: 10.1080/14767058.2019.1622677
76. EQUATOR Network. PRISMA 2009 checklist for reporting systematic reviews and meta-analyses. J ASEAN Fed Endocr Soc. (2015) 30:196–6.
77. Cheng YW, Caughey AB. Defining and managing normal and abnormal second stage of labor. Obstet Gynecol Clin North Am. (2017) 44:547–66. doi: 10.1016/j.ogc.2017.08.009
78. Gary Cunningham KJLF, Bloom SL, Spong CY, Dashe JS, Hoffman BL, Casey BM, et al. Williams Obstetrics. 26th edition. New York: Mc Graw Hill Education.
79. Buccheri RK, Sharifi C. Critical appraisal tools and reporting guidelines for evidence-based practice. Worldviews Evid.-Based Nurs. 14:463–72. doi: 10.1111/wvn.12258
80. Aromataris E, Munn Z editors. JBI Manual for Evidence Synthesis. (2020). doi: 10.46658/JBIMES-20-01. Available online at: https://synthesismanual.jbi.global
81. Sim J, Wright CC. The kappa statistic in reliability studies: use, interpretation, and sample size requirements. Phys Ther. (2005) 85:257–68. doi: 10.1093/ptj/85.3.257
82. Izuka E, Dim C, Chigbu C, Obiora-Izuka C. Prevalence and predictors of episiotomy among women at first birth in Enugu, south east Nigeria. Ann Med Health Sci Res. (2014) 4:928–32. doi: 10.4103/2141-9248.144916
83. Bergh JE, Sueters M, Segaar M, Roosmalen JV. Determinants of episiotomy in rural Zimbabwe. Acta Obstet Gynecol Scand. (2003) 82:966–8. doi: 10.1080/j.1600-0412.2003.00323.x
84. Morhe ES, Sengretsi S, Danso KA. Episiotomy in Ghana. Int J Gynaecol Obstet. (2004) 86:46–7. doi: 10.1016/j.ijgo.2004.04.006
85. Adama O, Natacha LB, Smaila O, Alexis SY, Francoise MT, Charlemagne OM, et al. Episiotomy: epidemiological aspects, indications and prognosis in the bogodogo health district. Open J Obstet Gynecol. (2018) 08:1354–63. doi: 10.4236/ojog.2018.813137
86. Lai CY, Cheung HW, Hsi Lao TT, Lau TK, Leung TY. Is the policy of restrictive episiotomy generalisable? A prospective observational study. J Matern Fetal Neonatal Med. (2009) 22:1116–21. doi: 10.3109/14767050902994820
87. Jug Došler A, Mivšek AP, Verdenik I, Škodič Zakšek T, Levec T, Petročnik P. Incidence of episiotomy in Slovenia: the story behind the numbers. Nurs Health Sci. (2017) 19:351–7. doi: 10.1111/nhs.12352
88. Clesse C, Cottenet J, Lighezzolo-Alnot J, Goueslard K, Scheffler M, Sagot P, et al. Episiotomy practices in France: epidemiology and risk factors in non-operative vaginal deliveries. Sci Rep. (2020) 10:20208. doi: 10.1038/s41598-020-70881-7
89. Frankman EA, Wang L, Bunker CH, Lowder JL. Episiotomy in the United States: has anything changed? Am J Obstet Gynecol. (2009) 200:573.e1–7. doi: 10.1016/j.ajog.2008.11.022
90. Singh S, Thakur T, Chandhiok N, Dhillon BS. Pattern of episiotomy use & its immediate complications among vaginal deliveries in 18 tertiary care hospitals in India. Indian J Med Res. (2016) 143:474–80. doi: 10.4103/0971-5916.184304
91. Kartal B, Kizilirmak A, Calpbinici P, Demir G. Retrospective analysis of episiotomy prevalence. J Turk German Gynecol Assoc. (2017) 18:190. doi: 10.4274/jtgga.2016.0238
92. Braga GC, Clementino STP, Luz PFN, Scavuzzi A, Noronha Neto C, Amorim MMR. Fatores de risco para a episiotomia: um estudo de caso-controle. Rev Assoc Méd Bras. (2014) 60:465–72. doi: 10.1590/1806-9282.60.05.015
93. Trinh AT, Khambalia A, Ampt A, Morris JM, Roberts CL. Providing evidence to support obstetric practice change in Vietnam: episiotomy use among Vietnamese-born women living in Australia. Bull. World Health Organ. (2013) 91:350–356.
94. Ogunyemi D, Manigat B, Marquis J, Bazargan M. Demographic variations and clinical associations of episiotomy and severe perineal lacerations in vaginal delivery. J Natl Med Assoc. (2006) 98:1874–81.
95. Belihu FB, Small R, Davey MA. Episiotomy and severe perineal trauma among eastern African immigrant women giving birth in public maternity care: a population based study in Victoria, Australia. Women Birth. (2017) 30:282–90. doi: 10.1016/j.wombi.2016.11.008
96. Hsieh W-C, Liang C-C, Wu D, Chang S-D, Chueh H-Y, Chao A-S. Prevalence and contributing factors of severe perineal damage following episiotomy-assisted vaginal delivery. Taiwan J Obstet Gynecol. (2014) 53:481–5. doi: 10.1016/j.tjog.2013.07.002
97. Abolfazl M, Hamidreza TS, Narges M, Maryam Y. Gestational diabetes and its association with unpleasant outcomes of pregnancy. Pak J Med Sci. (2008) 24:566–70. Available online at: https://pjms.com.pk/issues/julsep08/abstract/article
98. Bjørstad AR, Irgens-Hansen K, Daltveit AK, Irgens LM. Macrosomia: mode of delivery and pregnancy outcome. Acta Obstet Gynecol Scand. (2010) 89:664–9. doi: 10.3109/00016341003686099
99. Vitner D, Bleicher I, Kadour-Peero E, Lipworth H, Sagi S, Gonen R. Does prenatal identification of fetal macrosomia change management and outcome? Arch Gynecol Obstet. (2019) 299:635–44. doi: 10.1007/s00404-018-5003-2
Keywords: Africa, associated factors, delivery, episiotomy, parturient, perineum
Citation: Woldegeorgis BZ, Obsa MS, Tolu LB, Bogino EA, Boda TI and Alemu HB (2022) Episiotomy Practice and Its Associated Factors in Africa: A Systematic Review and Meta-Analysis. Front. Med. 9:905174. doi: 10.3389/fmed.2022.905174
Received: 26 March 2022; Accepted: 23 May 2022;
Published: 24 June 2022.
Edited by:
Simona Zaami, University of Rome Sapienza, ItalyReviewed by:
Timothy Abiola Olusesan Oluwasola, University of Ibadan, NigeriaCopyright © 2022 Woldegeorgis, Obsa, Tolu, Bogino, Boda and Alemu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Beshada Zerfu Woldegeorgis, YmVzaGFkYXplcmZ1QGdtYWlsLmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.