- 1Division of Rheumatology, Columbia University Irving Medical Center, New York, NY, United States
- 2Columbia University Vagelos College of Physicians and Surgeons, New York, NY, United States
- 3Lupus Clinic and Rheumatology Clinical Research Center, University of California, San Francisco, San Francisco, CA, United States
- 4Feinstein Institutes for Medical Research, Manhasset, NY, United States
Background: The pandemic disrupted the care of patients with rheumatic diseases; difficulties in access to care and its psychological impact affected quality of life. Telemedicine as an alternative to traditional face-to-face office visits has the potential to mitigate this impact.
Objective: To evaluate patient and provider experience with telemedicine and its effect on care.
Methods: We surveyed patients with rheumatic diseases and their rheumatology providers. The surveys were conducted in 2020 and repeated in 2021. We assessed data on quality of care and health-related quality of life.
Results: Hundred patients and 17 providers responded to the survey. Patients reported higher satisfaction with telemedicine in 2021 compared to 2020 (94 vs. 84%), felt more comfortable with (96 vs. 86%), expressed a stronger preference for (22 vs. 16%), and higher intention to use telemedicine in the future (83 vs. 77%); patients thought physicians were able to address their concerns. While providers' satisfaction with telemedicine increased (18–76%), 14/17 providers believed that telemedicine visits were worse than in-person visits. There were no differences in annualized office visits and admissions. Mean EQ-5D score was 0.74, lower than general population (0.87) but equivalent to a subset of patients with SLE (0.74).
Conclusion: Our data showed a high level of satisfaction with telemedicine. The lower rheumatology provider satisfaction raises concern if telemedicine constitutes an acceptable alternative to in-person care. The stable number of office visits, admissions, and the similar quality of life to pre-pandemic level suggest effective management of rheumatic diseases using telemedicine/in-person hybrid care.
Introduction
Telemedicine, defined as the exchange of medical information through electronic communication to improve a patient's health, has long been utilized in rheumatology practice to maximize access to specialty care among populations in underserved areas and optimize healthcare delivery in routine clinical practice (1). Telemedicine encompasses a variety of formats using different technologies, including video conferences, telephone consultations, web-based conversations, and electronic messages (2).
During the height of the COVID-19 pandemic, rheumatic disease patients experienced significant health care interruption. Guaracha-Basáñez et al. reported that 51.3% patients with rheumatic diseases experienced health care interruption from March to June 2020 during the transition from in-person office visits to telemedicine (3). The increasing demand during the pandemic for healthcare resources, a soaring number of patients and limited physician availability galvanized the utilization of telemedicine in Rheumatology and other specialties (4). While in-person rheumatology practice was largely replaced by telemedicine to ensure the safety of both patients and providers, the implementation of telemedicine was challenging (5, 6).
It remains unclear whether telemedicine, especially the most commonly used video conference-based modality, can serve as a feasible alternative to conventional in-person clinical visits while achieving patient/provider satisfaction and maintaining the quality of care. Data on the quality of Rheumatology care delivered via telemedicine is sparse. De Thurah et al. randomized 294 patients to patient-reported outcome rheumatologist (PRO)-based telemedicine follow (PRO-TR), nurse PRO-based telemedicine follow up (PRO-TN), or conventional physician follow up (control) for 1 year. The PRO-telehealth interventions achieved similar disease control as compared to those in the control conventional follow-up group (7). Similarly, Taylor-Gjevre et al. randomized 85 rheumatoid arthritis (RA) patients into either in-person or video conference-based telehealth follow up over a 9-month period and found out there were not significant differences in disease activity measurements and quality of life (8). These data support the equivalence of telerheumatology to in-person visits in achieving quality of care.
The current study assessed the patient and provider experiences with virtual care and evaluated healthcare utilization and quality of life among patients receiving virtual care during and after the peak of COVID-19 pandemic to provide more information on the effectiveness of telemedicine in rheumatology practices.
Methods
This study is a longitudinal cohort study that evaluated the satisfaction with and effectiveness of telemedicine in a New York city Rheumatology academic practice. We designed two parallel seven-item questionnaires to evaluate the patient and provider experiences with virtual care. The question items were described in Tables 2, 3, respectively. The two questionnaires, despite evaluating different sides of virtual care, contain similar items.
Patients with rheumatic diseases who received virtual care in a video conference format from a single rheumatology clinic in New York city during April 2020 to September 2020 were invited to participate in the survey. The seven-item Patient Questionnaire was disseminated to patients shortly through telephone or web links after they completed the virtual visit to evaluate their satisfaction and experience with the encounter; the socio-demographic data were collected through medical record review. The survey was repeated October 2021 to January 2022 with additional and optional EQ-5D-3L questionnaire to evaluate the quality of life. The EQ-5D-3L descriptive system comprises the following five dimensions: mobility, self-care, usual activities, pain/discomfort, and anxiety/depression. Each dimension has 3 levels: no problems, some problems, and extreme problems. The patient is asked to indicate his/her health state by ticking the box next to the most appropriate statement in each of the five dimensions. This decision results into a 1-digit number that expresses the level selected for that dimension. The digits for the five dimensions can be combined into a 5-digit number that describes the patient's health state. The scoring algorithm for the EQ-5D index is based on US community preferences (9). Data on the total number of in-person and telemedicine office visits, admissions were collected from electronic medical records.
Concurrently we surveyed 17 rheumatology healthcare providers from Columbia University Irving Medical Center who delivered virtual care in 2020 and in 2021 with the seven-item Provider Questionnaire.
The study protocol was approved by the Columbia University Irving Medical Center (CUIMC) Institutional Review Board (IRB).
Results
Socio-Demographic Information
100 out of 110 (91%) consecutive patients were able to complete the survey in 2020, and 100 out of 108 (92%) consecutive patients responded to the repeat survey in 2021. Additionally, 71 (66%) patients completed the EQ-5D-3L.
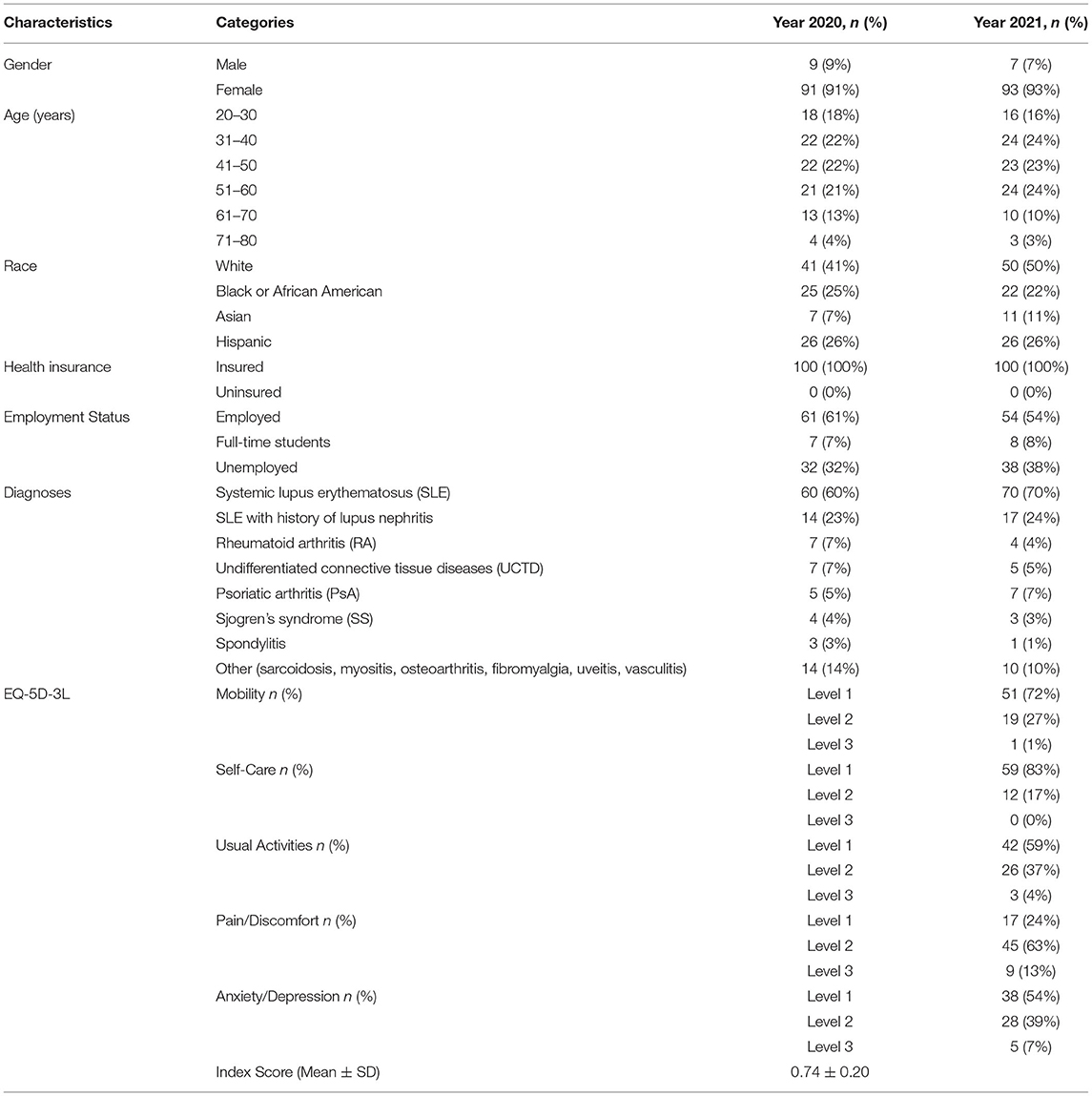
The socio-demographics of the 100 (90.9% of 110 and 92.6% out of 108) patients that responded to the survey in 2020 and 2021 are summarized in Table 1. Sixty-seven patients responded to both surveys in 2020 and 2021.
Of the 100 patients surveyed in 2020, 91 (91%) were women with a mean ± standard deviation (SD) age of 44.3 ± 12.9 years; 41 (41%) were White, 25 (25%) African American, 26 (26%) Hispanic, and 7% Asian; 60 (60%) of the patients had a diagnosis of Systemic Lupus Erythematosus (SLE), and the remaining 40 (40%) had other systemic autoimmune diseases [undifferentiated connective tissue disorder (UCTD), rheumatoid arthritis (RA), psoriatic arthritis (PsA), and spondyloarthritis (SpA)].
Of the 100 patients surveyed in 2021, 93 (93%) were women with a mean ± SD age of 44.8 ± 13.0 years; 50 (50%) were White, 22 (22%) African American, 26 (26%) Hispanic, and 11% Asian; 70 (70%) of the patients had a diagnosis of Systemic Lupus Erythematosus (SLE), and the remaining 30 (30%) had other systemic autoimmune diseases [undifferentiated connective tissue disorder (UCTD), rheumatoid arthritis (RA), psoriatic arthritis (PsA), and spondyloarthritis (SpA)].
Interestingly, in these two cohorts of patients with rheumatic diseases and a large proportion of SLE patients, over 60% patients were employed or full-time students (Table 1).
Seventeen providers responded to the survey both in 2020 and 2021. The providers included 15 physicians and two nurse practitioners from Columbia University Irving Medical Center Division of Rheumatology; of the 15 physicians, nine were board-certified rheumatologists and six were rheumatology fellows in training.
Survey Data
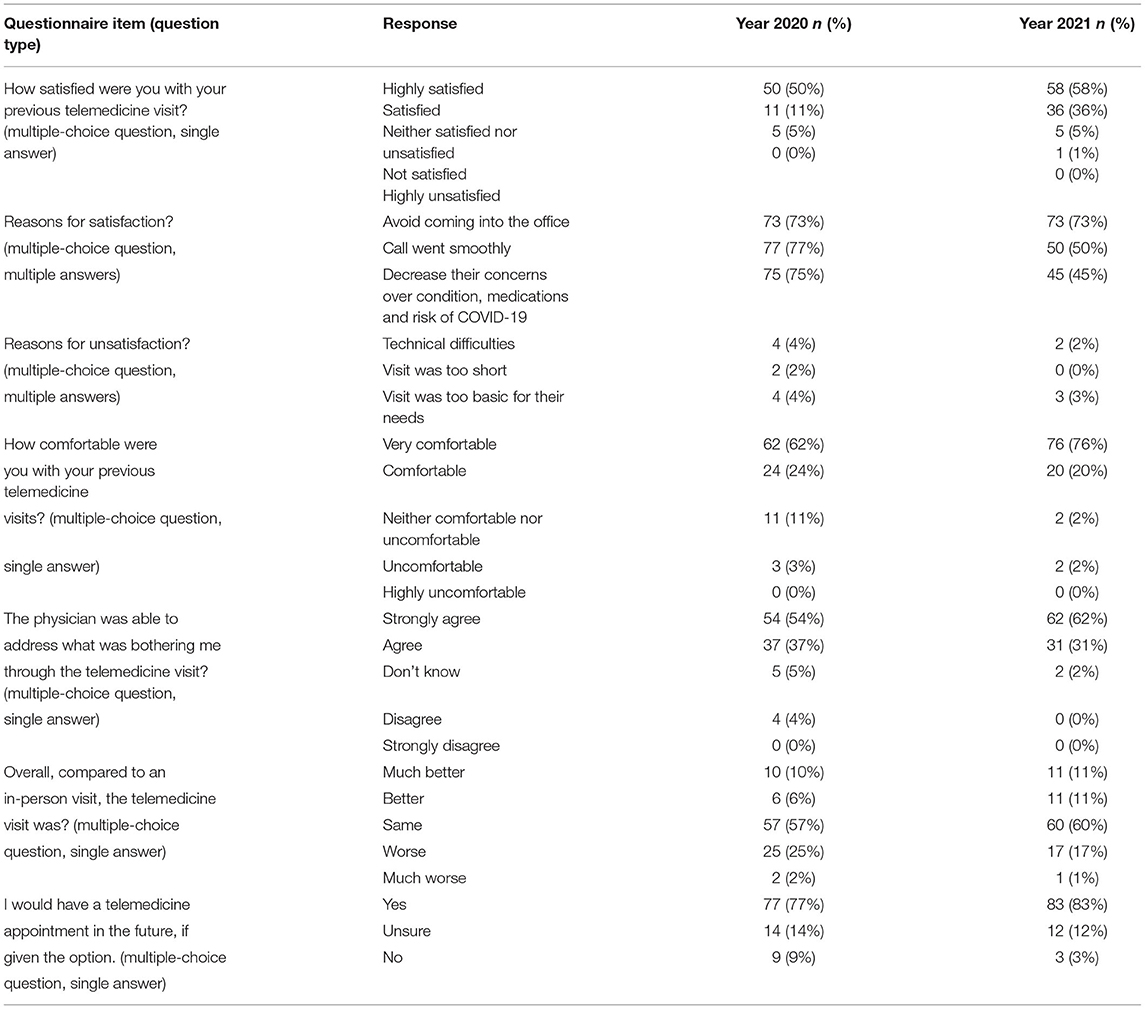
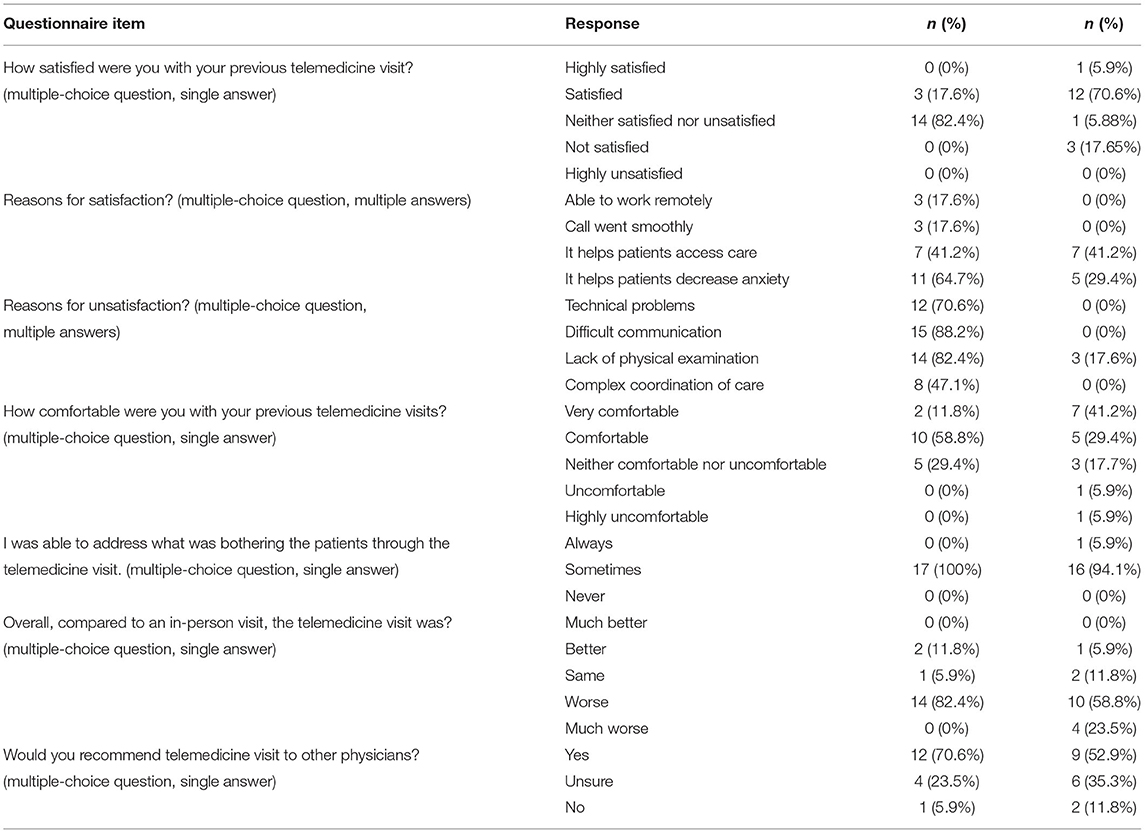
The survey results for patients and providers are shown in Tables 2, 3.
Compared to 2020, patient respondents in 2021 reported a higher level of satisfaction (94 vs. 84%, p < 0.05). As expected, respondents felt more comfortable in 2021 with the telemedicine format (96 vs. 86%, p < 0.05). The majority of respondents (91% in 2020 and 93% in 2021) acknowledged that physicians were able to satisfactorily address the issues and concerns that prompted the visit. The percentage of respondents who considered the experience to be the same as the in-person experience remained high (57% in 2020 and 60% in 2021), more respondents in 2021 reported that telemedicine was better than in-person visit (22 vs. 16%). Finally, when asked whether they would use telemedicine in the future, 77% of 2020 respondents and 83% of 2021 respondents responded “yes.” In the 2021 survey we also asked if telemedicine was an acceptable or preferred alternative to the in-person visits; it was acceptable to 94 (94%) and preferred by 45 patients (45%).
Among the 17 providers surveyed in 2020, 3 (17.6%) expressed satisfaction with telemedicine while 14 (82.4%) felt that the telemedicine visits were inferior to conventional in-person clinic visits. In contrast, 13 (76.5%) of 17 providers in 2021 reported satisfaction with telemedicine but 14 (82.3%) still thought the telemedicine visits were worse or much worse than in-person visits. Noticeably, technical difficulties, unsatisfactory communications, and insufficient physical examinations were reported by 12 (71%), 15 (88%), and 14 (82%) providers in 2020 as reasons for dissatisfactions with virtual care. The lack of physical examination was the most reported reason for dissatisfaction with telemedicine among providers in 2021. However, 12 (70.6%) in 2020 and 9 (52.9%) in 2021 still chose to recommend telemedicine visits to other physicians.
Quality of Care
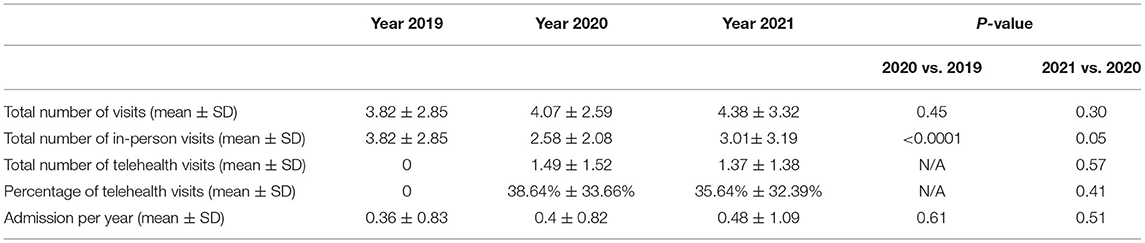
The average number of in-person office visits, telemedicine visits, and admissions per survey respondent for 2019, 2020, and 2021 were shown in Table 4. There was no significant difference among the total number of visits per patient in 2019 (3.82 ± 2.85), 2020 (4.07 ± 2.59), and 2021 (4.38 ± 3.32). During 2020, the peak of COVID-19 pandemic, telemedicine visits constituted over 1/3 of total visits per year (1.49 ± 1.52), and their percentage (38.64% ± 33.66%) remained stable beyond the peak of pandemic into 2021 (35.64% ± 32.39%). There was no increase in the number of admissions, during and after the peak of pandemic (0.36 ± 0.83 in 2019, 0.4 ± 0.82 in 2020, and 0.48 ± 1.09 in 2021) despite the increased burden on the healthcare system in 2020 and 2021.
Quality of Life
The data on quality of life was collected only in 2021 using the EQ-5D-3L questionnaire. The numbers and percentages of patients (n = 71) reporting each level of problem on each dimension of the EQ-5D-3L are shown as Table 1. Our cohort has a mean EQ-5D-3L index score (± SD) of 0.74 ± 0.20, which is significantly lower than the US population norm (0.87) but similar to the pre-pandemic level reported among patients with SLE and connective tissue disorders (0.74) in the nationally representative Medical Expenditure Panel Survey (MEPS) (10). Additionally, 43 (60.6%) patients acknowledged that “telemedicine helped me when I was feeling down during the pandemic last year” and 46 (64.8%) agreed that “telemedicine helped to decrease my everyday stress over the past year.” Interestingly, only 5 of these 71 (7.0%) patients were “neither satisfied nor dissatisfied” or “not satisfied” with telemedicine and their mean EQ-5D index score was 0.70 ± 0.15 slightly lower than those who felt satisfied or highly satisfied with telemedicine (0.75 ± 0.20); additionally, 3 of 5 (60%) were unsure that telemedicine helped to address their anxiety or depression.
Discussion
Telemedicine has now been extensively used in the management of rheumatology patients but literature examining its outcomes has been scarce. Before the COVID-19 pandemic, a few randomized clinical trials investigating the role of telemedicine were conducted in RA patients, which consistently reported high satisfaction rates of 80–90% (7, 8). More recently, six studies conducted among patients with rheumatic diseases during the COVID-19 pandemic indicated high acceptance and satisfaction with telemedicine for the delivery of rheumatology care (5). Multiple studies investigated factors associated with the acceptance of telemedicine by patients with rheumatic diseases. Ferucci et al. surveyed 56 patients seen by telemedicine (TM group) vs. 66 patients seen in-person (in-person only group), and reported factors associated with the use of telemedicine included a higher disease activity, a higher number of rheumatologist visits in the preceding year, a more positive perception of telehealth, and a visit with a physician who used telehealth more often (11). Breslau et al. found in a survey study of 2080 adults that participants were generally willing to use video visits but preferred in-person care (12). More recently, Moskowitz et al. proposed that patients have different expectations of providers in telemedicine based on their locus of control; and delivering tailored communication in telemedicine could enhance satisfaction (13).
Our cohort, with a high number of SLE patients, showed similar satisfaction rates (84% in 2020 and 94% in 2021) to those reported in the literature. However, the high level of frustration with telemedicine visits among healthcare providers in our center raises concerns as to whether disease activity can be assessed adequately using this format. In 2017, McDougall et al. published a systematic literature review which examined the use of telemedicine (video conferences and telephone consultations) in the diagnosis and/or management of inflammatory/autoimmune rheumatic diseases that included one randomized controlled trial and 19 observational studies. They concluded that there was limited evidence to support the effectiveness of telemedicine (14). Additionally, Han et al. reviewed data from three randomized clinical trials and three observational studies evaluating the role of virtual care in the management of patients with RA and reported equivalent control of disease activity and good patient experiences compared to conventional follow-up strategies (15).
Alexander et al. conducted a cross-sectional analysis of the US National Disease and Therapeutic Index Audit of 125.8 million primary care visits between January 2018 and June 2020. The authors reported that the pandemic was associated with a 25% decrease in primary care in-person office visits, which was in part due to the increase in telemedicine that accounted for 35.3% of encounters during the second quarter of 2020 (16). A similar percentage of telemedicine visits (38.6%) were observed in our cohort without a significant change in the total number of encounters. George et al. examined trends in in-person vs. telehealth visits among 300 rheumatology providers from 92 offices during COVID-19 and post-COVID-19 transition (May–August 2020); the authors found that telehealth increased substantially during the peak of the pandemic-−41.4% of all follow up visits (March to May 2020), and slightly decreased during the post-COVID-19 transition (27.7% of visits). In our cohort the percentage of telehealth visits remained stable in 2021 at 35.6% (17).
In a 2017 prospective study of hospitalizations among 155 Danish SLE patients, Busch et al. reported a crude hospitalization rate of 25% of the cohort per year and an annual admissions rate of 0.50 (18). Lawson et al. brought up a model of assessing outcomes of interest in SLE, which include healthcare utilization such as hospitalizations, disease activity, disease damage, mortality, and quality of life (19). Given the susceptibility of SARS-CoV-2 infection among patients with rheumatic diseases, the rate of hospitalization had the potential to be higher during the pandemic (20). Our cohort with a large proportion of SLE patients showed a stable hospitalizations rate (0.36, 0.40, 0.48/year in 2019, 2020, and 2021). Given the fact that 91% and 93% patients agreed or strongly agreed that “physicians were able to address what was bothering me during the telehealth visits,” we propose that the stable hospitalization rate during the COVID-19 pandemic may reflect the effectiveness of telehealth visits in addressing the medical needs of our patients; however, this assumption needs further investigation. Patients with rheumatic diseases in our cohort maintained a relatively stable outpatient healthcare utilization during the COVID-19 pandemic despite public health policies with non-significant increases in the total number of visits (3.82, 4.07, and 4.38 in year 2019, 2020, and 2021), which was almost all contributed by telerheumatology. However, it should be noted that the actual healthcare utilization rates might be underestimated given that both patients and physicians might attempt to maximally reduce the time spent in the hospital during the COVID-19 pandemic (21).
Patients with rheumatic diseases were reported to have significant impairment of health-related quality of life (HR-QoL) during the COVID-19 pandemic, especially in psycho-emotional dimension due to health care interruptions (22). However, our cohort showed quality of life similar to that reported pre-pandemic, as indicated by a stable EQ-5D-3L index score; and over 60% of survey respondents acknowledged that telemedicine helped to stabilize and improve their psycho-emotional status. Our clinic responded rapidly during the peaks of COVID-19 pandemic in 2020 and 2021; 96 % of total visits were switched to telemedicine as early as the last 2 weeks of March 2020. In fact, research personnel and medical students all helped keep patients connected with our clinic and optimized the transition to telemedicine. This swift transition to telemedicine in our rheumatology practice minimized the health care interruption experienced by other medical systems. While these data did not provide direct comparisons, we submit that telemedicine might have helped to improve patients' quality of life by increasing their access to rheumatology care and addressing their anxiety and/or depression about healthcare interruption.
As rheumatology clinical practices change, it is becoming clear that telemedicine will complement traditional face-to-face clinical encounters in care delivery and clinical trials. Disease activity indices such as the British Isles Lupus Assessment Group Index (BILAG) and the Systemic Lupus Erythematosus Disease Activity Index-2000 (SLEDAI-2K) for SLE, and the RA Disease Activity Score 28 (DAS-28) for RA are critical in clinical studies, and require physician assessments (23–25). Virtual disease activity indices have not yet been compared to face-to-face measures. Moreover, the physical examinations, especially musculoskeletal and cutaneous examinations, as essential components of patient evaluations, are difficult to conduct virtually (26, 27). The ability of current technology to allow for accurate evaluations by virtual visits is not yet fully understood. Accordingly, we and others have embarked on the task to further evaluate the role of telemedicine in disease activity assessments as virtual outcome measures might provide meaningful targets for optimizing treatment and assessing response in clinical trials.
We acknowledge several weaknesses of the study. First of all, the questionnaires used in the current study were not previously validated. Second, 67 of the 100 survey respondents in 2020 completed the survey again in 2021, the two cohorts in 2020 and 2021 were not the same, which limited our ability to perform a pairwise comparison. Third, EQ-5D-3L questionnaire was only disseminated to patients in 2021; as such, we were unable to directly compare 2020 and 2021 quality of life data of our survey respondents, which might bring in more persuasive data on the effectiveness of telerheumatology.
The data presented here support a high level of patient satisfaction with telerheumatology and suggest effectiveness in disease control and quality of care. More in depth evaluations of disease control, quality of care, and quality of life are needed to fully define the role of telemedicine in everyday rheumatology care.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Columbia University Irving Medical Center Institutional Review Board. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author Contributions
WT and SI wrote the first draft of the manuscript. AA, CA, MM, and MD contributed to the conception and design of the study. SI, JW, JB, and LK collected the data. WT, SI, JB, and LK performed the statistical analysis. All authors contributed to the manuscript revision, read, and approved the submitted version.
Funding
This research was partially supported by the United States Department of Defense (DoD).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Davis P, Howard R, Brockway P. An evaluation of telehealth in the provision of rheumatologic consults to a remote area. J Rheumatol. (2001) 28:1910–3. Available online at: https://www.jrheum.org/content/28/8/1910.tab-article-info
2. Solomon DH, Rudin RS. Digital health technologies: opportunities and challenges in rheumatology. Nat Rev Rheumatol. (2020) 16:525–35. doi: 10.1038/s41584-020-0461-x
3. Guaracha-Basanez GA, Contreras-Yanez I, Hernandez-Molina G, Gonzalez-Marin A, Pacheco-Santiago LD, Valverde-Hernandez SS, et al. Clinical and bioethical implications of health care interruption during the COVID-19 pandemic: a cross-sectional study in outpatients with rheumatic diseases. PLoS ONE. (2021) 16:e0253718. doi: 10.1371/journal.pone.0253718
4. Hollander JE, Carr BG. Virtually Perfect? Telemedicine for Covid-19. N Engl J Med. (2020) 382:1679–81. doi: 10.1056/NEJMp2003539
5. Tang W, Khalili L, Askanase A. Telerheumatology: a narrative review. Rheumatol Immunol Res. (2021) 2:139–45. doi: 10.2478/rir-2021-0020
6. Song Y, Bernard L, Jorgensen C, Dusfour G, Pers YM. The challenges of telemedicine in rheumatology. Front Med. (2021) 8:746219. doi: 10.3389/fmed.2021.746219
7. de Thurah A, Stengaard-Pedersen K, Axelsen M, Fredberg U, Schougaard LMV, Hjollund NHI, et al. Tele-health followup strategy for tight control of disease activity in rheumatoid arthritis: results of a randomized controlled trial. Arthritis Care Res. (2018) 70:353–60. doi: 10.1002/acr.23280
8. Taylor-Gjevre R, Nair B, Bath B, Okpalauwaekwe U, Sharma M, Penz E, et al. Addressing rural and remote access disparities for patients with inflammatory arthritis through video-conferencing and innovative inter-professional care models. Musculoskelet Care. (2018) 16:90–5. doi: 10.1002/msc.1215
9. Shaw JW, Johnson JA, Coons SJ. US valuation of the EQ-5D health states: development and testing of the D1 valuation model. Med Care. (2005) 43:203–20. doi: 10.1097/00005650-200503000-00003
10. Sullivan PW, Lawrence WF, Ghushchyan V. A national catalog of preference-based scores for chronic conditions in the United States. Med Care. (2005) 43:736–49. doi: 10.1097/01.mlr.0000172050.67085.4f
11. Ferucci ED, Holck P, Day GM, Choromanski TL, Freeman SL. Factors associated with use of telemedicine for follow-up of rheumatoid arthritis. Arthrit Care Res. (2020) 72:1404–9. doi: 10.1002/acr.24049
12. Predmore ZS, Roth E, Breslau J, Fischer SH, Uscher-Pines L. Assessment of patient preferences for telehealth in post-COVID-19 pandemic health care. JAMA Netw Open. (2021) 4:e2136405. doi: 10.1001/jamanetworkopen.2021.36405
13. Gabay G, Ornoy H, Moskowitz H. Patient-centered care in telemedicine—an experimental-design study. Int J Med Inform. (2021) 159:104672. doi: 10.1016/j.ijmedinf.2021.104672
14. McDougall JA, Ferucci ED, Glover J, Fraenkel L. Telerheumatology: a systematic review. Arthritis Care Res. (2017) 69:1546–57. doi: 10.1002/acr.23153
15. Han L, Hazlewood GS, Barnabe C, Barber CEH. Systematic review of outcomes and patient experience with virtual care in rheumatoid arthritis. Arthritis Care Res. (2021). doi: 10.1002/acr.24586. [Epub ahead of print].
16. Alexander GC, Tajanlangit M, Heyward J, Mansour O, Qato DM, Stafford RS. Use and content of primary care office-based vs. telemedicine care visits during the COVID-19 pandemic in the US. JAMA Netw Open. (2020) 3:e2021476. doi: 10.1001/jamanetworkopen.2020.21476
17. George MD, Danila MI, Watrous D, Reddy S, Alper J, Xie F, et al. Disruptions in rheumatology care and the rise of telehealth in response to the COVID-19 pandemic in a community practice-based network. Arthritis Care Res. (2021) 73:1153–61. doi: 10.1002/acr.24626
18. Busch RW, Kay SD, Voss A. Hospitalizations among Danish SLE patients: a prospective study on incidence, causes of admission and risk factors in a population-based cohort. Lupus. (2018) 27:165–71. doi: 10.1177/0961203317734919
19. Lawson EF, Yazdany J. Healthcare quality in systemic lupus erythematosus: using Donabedian's conceptual framework to understand what we know. Int J Clin Rheumtol. (2012) 7:95–107. doi: 10.2217/ijr.11.65
20. Askanase AD, Khalili L, Buyon JP. Thoughts on COVID-19 and autoimmune diseases. Lupus Sci Med. (2020) 7:e000396. doi: 10.1136/lupus-2020-000396
21. Nguyen JL, Benigno M, Malhotra D, Khan F, Angulo FJ, Hammond J, et al. Pandemic-related declines in hospitalization for non-COVID-19-related illness in the United States from January through July 2020. PLoS ONE. (2022) 17:e0262347. doi: 10.1371/journal.pone.0262347
22. Guaracha-Basanez GA, Contreras-Yanez I, Hernandez-Molina G, Estrada-Gonzalez VA, Pacheco-Santiago LD, Valverde-Hernandez SS, et al. Quality of life of patients with rheumatic diseases during the COVID-19 pandemic: the biopsychosocial path. PLoS ONE. (2022) 17:e0262756. doi: 10.1371/journal.pone.0262756
23. Symmons DP, Coppock JS, Bacon PA, Bresnihan B, Isenberg DA, Maddison P, et al. Development and assessment of a computerized index of clinical disease activity in systemic lupus erythematosus. Members of the British Isles Lupus Assessment Group (BILAG). Q J Med. (1988) 69:927–37.
24. Gladman DD, Ibanez D, Urowitz MB. Systemic lupus erythematosus disease activity index 2000. J Rheumatol. (2002) 29:288–91. Available online at: https://www.jrheum.org/content/29/2/288.tab-article-info
25. Prevoo ML. van 't Hof MA, Kuper HH, van Leeuwen MA, van de Putte LB, van Riel PL. Modified disease activity scores that include twenty-eight-joint counts. Development and validation in a prospective longitudinal study of patients with rheumatoid arthritis. Arthritis Rheum. (1995) 38:44–8. doi: 10.1002/art.1780380107
26. Mikuls TR, Johnson SR, Fraenkel L, Arasaratnam RJ, Baden LR, Bermas BL, et al. American college of rheumatology guidance for the management of rheumatic disease in adult patients during the COVID-19 pandemic: version 3. Arthritis Rheumatol. (2021) 73:e1–e12. doi: 10.1002/art.41596
Keywords: autoimmune diseases (AD), telemedicine, quality of life, quality of care/care delivery, survey, telerheumatology
Citation: Tang W, Inzerillo S, Weiner J, Khalili L, Barasch J, Gartshteyn Y, Dall'Era M, Aranow C, Mackay M and Askanase A (2022) The Impact of Telemedicine on Rheumatology Care. Front. Med. 9:876835. doi: 10.3389/fmed.2022.876835
Received: 15 February 2022; Accepted: 03 May 2022;
Published: 20 May 2022.
Edited by:
Dario Roccatello, University of Turin, ItalyReviewed by:
Anabela Barcelos, New University of Lisbon, PortugalVittorio Modena, SC Nephrology and Dialysis San Giovanni Bosco Hospital, Italy
Copyright © 2022 Tang, Inzerillo, Weiner, Khalili, Barasch, Gartshteyn, Dall'Era, Aranow, Mackay and Askanase. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Anca Askanase, YWRhMjBAY3VtYy5jb2x1bWJpYS5lZHU=
†These authors have contributed equally to this work
 Wei Tang
Wei Tang Sean Inzerillo1†
Sean Inzerillo1† Yevgeniya Gartshteyn
Yevgeniya Gartshteyn Anca Askanase
Anca Askanase