- 1Women's Health Development Unit, School of Medical Sciences, Universiti Sains Malaysia, Kubang Kerian, Malaysia
- 2Department of Family Medicine, School of Medical Sciences, Universiti Sains Malaysia, Kubang Kerian, Malaysia
Introduction: Maternal mortality and severe maternal morbidity remain major public health problems globally. Understanding their risk factors may result in better treatment solutions and preventive measures for maternal health. This review aims to identify the prevalence and risk factors of severe maternal morbidity (SMM) and maternal near miss (MNM).
Methods: A systematic review and meta-analysis was conducted to assess the prevalence and risk factors of SMM and MNM. The study adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis guidelines. A systematic search was performed in the MEDLINE (PubMed), CINAHL (EBSCOhost), and Science Direct databases for articles published between 2011 and 2020.
Results: Twenty-four of the 44 studies included were assessed as being of good quality and having a low risk of bias. The prevalence of SMM and MNM was 2.45% (95% CI: 2.03, 2.88) and 1.68% (95% CI: 1.42, 1.95), respectively. The risk factors for SMM included history of cesarean section (OR [95% CI]: 1.63 [1.43, 1.87]), young maternal age (OR [95% CI]: 0.71 [0.60, 0.83]), singleton pregnancy (OR [95% CI]: 0.42 [0.32, 0.55]), vaginal delivery (OR [95% CI]: 0.11 [0.02, 0.47]), coexisting medical conditions (OR [95% CI]: 1.51 [1.28, 1.78]), and preterm gestation (OR [95% CI]: 0.14 [0.08, 0.23]). The sole risk factor for MNM was a history of cesarean section (OR [95% CI]: 2.68 [1.41, 5.10]).
Conclusions: Maternal age, coexisting medical conditions, history of abortion and cesarean delivery, gestational age, parity, and mode of delivery are associated with SMM and MNM. This helps us better understand the risk factors and their strength of association with SMM and MNM. Thus, initiatives such as educational programs, campaigns, and early detection of risk factors are recommended. Proper follow-up is important to monitor the progression of maternal health during the antenatal and postnatal periods.
Systematic Review Registration: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42021226137, identifier: CRD42021226137.
Introduction
Severe maternal morbidity (SMM) refers to “potentially life-threatening conditions during pregnancy, childbirth or after pregnancy, from which maternal near miss (MNM) cases would emerge” (1, 2). The standard definition and internationally accepted identification criteria for SMM by the World Health Organization (WHO) Working Group on Maternal Mortality Morbidity Classifications (1, 2) incorporate clinical disorders (hemorrhagic, hypertensive, and other systemic disorders) and severe management indicators to assess the severity of SMM and to strengthen the ability of health care professionals to detect SMM (1).
However, maternal mortality and SMM remain major public health problems for global healthcare systems despite substantial progress (3). Between 1990 and 2015, the global maternal mortality ratio (MMR) declined by 44% but failed to meet the 75% reduction set by Millennium Development Goal 5. Sustainable Development Goal 3 aims to ensure healthy living, promote well-being for people of all ages, and reduce global MMR to <70 per 100,000 live births by 2030. The average reduction of 7.5% each year between 2016 and 2030 is more than three times the 2.3% annual rate of decline observed globally between 1990 and 2015.
Prior to 2011, the literature varied in its definitions and criteria used to classify SMM and MNM cases. In a review, the prevalence of SMM based on various disease-specific, management-based, and organ system dysfunction-based criteria ranged from 0.04 to 15% (4). Meanwhile, the prevalence according to organ-based dysfunction using the Mantel criteria and emergency hysterectomy was 0.42 and 0.039%, respectively. With a 98.3% I2 value for the Mantel-based criteria and 95.5% for the emergency hysterectomy criteria, the heterogeneity among studies was large and significant (4).
While maternal mortality has been commonly used as a benchmark for maternal health status, there is evidence that it is just the “tip of the iceberg” for adverse maternal outcomes (5, 6). The SMM literature has revealed several contributing factors. Employment status (7), low household income (8), history of abortion (8), multiple births (9), and inadequate antenatal care (8) were documented as contributing factors for SMM. However, mixed findings were reported for the factors of age (10–12), race (9, 13), educational level (8, 13), co-existing medical conditions (14), parity (15), gestational period (10), mode of delivery (12, 16), previous cesarean section (14), and pre-pregnancy body mass index (9, 14).
Determining the pooled prevalence of SMM at a global level gives a better indication of its severity than discrete primary studies. The identification of factors associated with SMM allows a clearer understanding of the issue and serves as a basis for appropriate preventive strategies to be established. This pertains to primary prevention at the institutional, provider, and client levels, such as screening or preventive that could potentially avoid death or severe morbidity from a disorder. Therefore, to inform clinical policy and enhance patient care, planning beyond maternal mortality and direct, focused evaluation of the strength of each risk factor's association with SMM is required. This systematic review aims to ascertain the prevalence and risk factors of SMM based on the WHO standard definition and criteria (1). The evidence, effect estimates, and strength of statistical association between SMM and its risk factors will be summarized in this review.
Methods
Study Design and Search Strategy
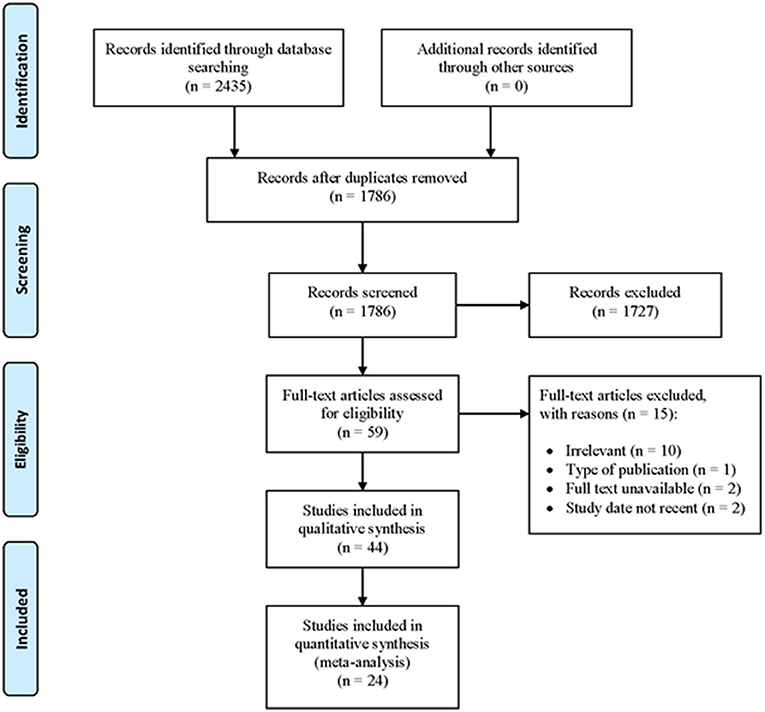
To determine the prevalence and risk factors, researchers conducted a systematic review and meta-analysis of studies on SMM. The study followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Figure 1).
A systematic search was performed in the MEDLINE (PubMed), CINAHL (EBSCOhost), and Science Direct databases for articles published between 2011 and 2020 inclusive. The search was done using the following Medical Subject Headings (MeSH) and generic free-text search terms as follows: ((Prevalence [MeSH Terms]) OR (risk factors[MeSH Terms])) AND (severe maternal morbidity[Text Word])) OR (maternal near miss[Text Word])) OR (potentially life-threatening[Text Word])) OR (maternal complications[Text Word])) OR (severe acute maternal morbidity[Text Word])) OR (pregnancy complications[Text Word])) AND ((“2011” [Date - Publication]: “2022” [Date - Publication])) The search terms were flexible and tailored to the various electronic databases. All studies published starting from 2011 were retrieved to assess their eligibility for inclusion in this study. The search was limited to full-text articles written in English. The reference lists of the included studies were cross-checked to locate additional potentially acceptable studies.
Eligibility Criteria
The main inclusion criterion was the reporting of prevalence or risk factors of SMM. Studies that were written in English, published in 2011 or later, had cross-sectional, case-control, or cohort designs, and were conducted in the community or health institutions were included. Case series/reports, conference papers, proceedings, abstract-only articles, editorial reviews, letters of communications, commentaries, systematic reviews, and qualitative studies were excluded.
Study Selection and Screening
All records identified using our search strategy were exported to the EndNote X8 (Clarivate Analytics). Duplicate articles were removed. Two independent reviewers (MKHR, NMN) screened the titles and abstracts of the identified articles. The full texts of eligible studies were obtained and thoroughly read to assess their suitability for the meta-analysis. A consensus discussion was held in the event of a conflict between the two reviewers, and a third reviewer was consulted. The search method is presented in the PRISMA flow chart showing the number of studies that were included and excluded, along with reasons for exclusion (Figure 1). The primary outcomes of this study were the prevalence and risk factors of SMM.
Quality Assessment and Bias
A critical appraisal was done to assess data quality using the Joanna Briggs Institute Meta-Analysis for cross-sectional, case-control, and cohort studies (17). Independent bias assessments were carried out by two reviewers. When more than 70% of the responses were “yes,” moderate when 50–69% of the answers were “yes,” and high when <50% of the answers were “yes,” the risk of bias was rated low. Studies that showed a high or moderate risk of bias were excluded from the review.
Data Extraction
Two reviewers independently extracted data into Microsoft Excel (Microsoft Office Professional Plus 2016). The data included the name of the first author, publication year, study location, study design, setting, study population, sample size, SMM definition, prevalence, risk factors, and data for calculation of effect estimates. The data for risk factors included sociodemographic characteristics, medical and gynecological histories, and past and present obstetric performance.
Result Synthesis and Statistical Analysis
Outcomes were reported using odds ratios (ORs) and 95% confidence intervals (CIs). The analysis was performed with the Review Manager software (v.5.4; Nordic Cochrane Centre, Copenhagen, Denmark). A random-effects model was used to pool data. The I2 statistic was used to assess heterogeneity, which was stratified as follows: 0–40%, might not be important; 30–60%, moderate heterogeneity; 50–90% substantial heterogeneity; and 75–100%, considerable heterogeneity (18). Funnel plots and Egger's test were used to assess publication bias if indicated, and a p < 0.05 was declared as statistically significant.
Results
Characteristics of the Included Studies
A total of 2,435 articles were retrieved through an electronic search using the aforementioned search terms, of which 1,786 were eligible for the title and abstract assessment after removing 649 duplicate records. Of the 1,786 articles screened for eligibility, 1,727 were excluded after evaluating their titles and abstracts. A total of 59 articles underwent full-text assessment for eligibility, of which 15 were excluded due to irrelevancy (n = 10), not suitable type of publication (n = 1), unavailability of full text (n = 2), and not recent (n = 2) (Figure 1).
In this review, 44 articles underwent quality assessment, of which 24 with good quality and low risk of bias were included and the remaining poor-quality articles excluded. Nineteen studies were cross-sectional, two were case-control, and three were cohort. A variety of countries were represented in this systematic review and meta-analysis. The smallest sample size was 262 women, and the largest was 3,162,303 (Table 1). The source of funding of included articles was tabulated in the Supplementary File.
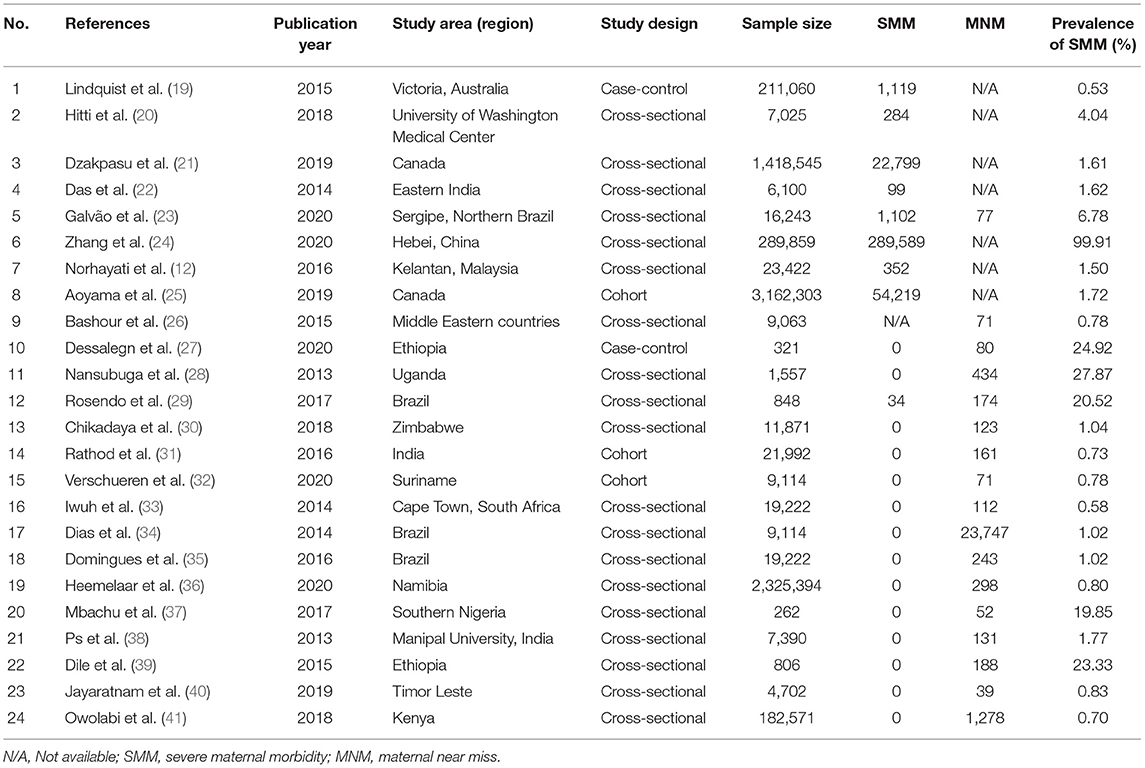
Table 1. Summary of research articles included in the systemic review and meta-analysis for SMM and MNM (n = 24).
Severe Maternal Morbidity
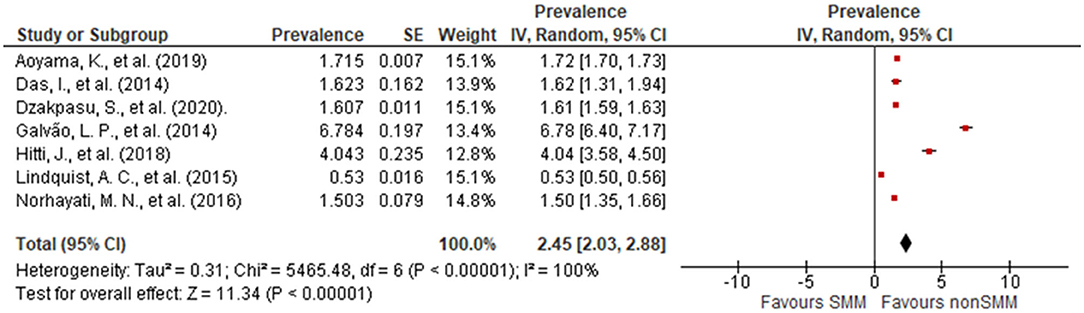
We observed significant variations in the prevalence of SMM in this review (Figure 2). The lowest reported prevalence of SMM was 0.53% (19), and the highest was 6.78% (23). Eight articles were included, with the overall pooled prevalence of SMM at 2.45% (95% CI: 2.03, 2.88). Egger's test showed statistically insignificant publication bias (P = 0.162).
Various factors such as age, parity, history of cesarean section, previous history of abortion, singleton pregnancy, and coexisting medical conditions were evaluated for their association with SMM. Two studies (12, 19) reported an association between a history of cesarean section and SMM with an OR of 1.63 (95% CI: 1.43, 1.87) when compared to women with only a history of vaginal delivery. Four studies (12, 19, 20, 25) showed a significant association between young maternal age and SMM with an OR of 0.71 (95% CI: 0.60, 0.83) when compared with older women. Additionally, three studies (12, 19, 20) showed a significant association between singleton pregnancies and SMM with an OR of 0.42 (95% CI: 0.32, 0.55) when compared to twin pregnancies (Figure 3).
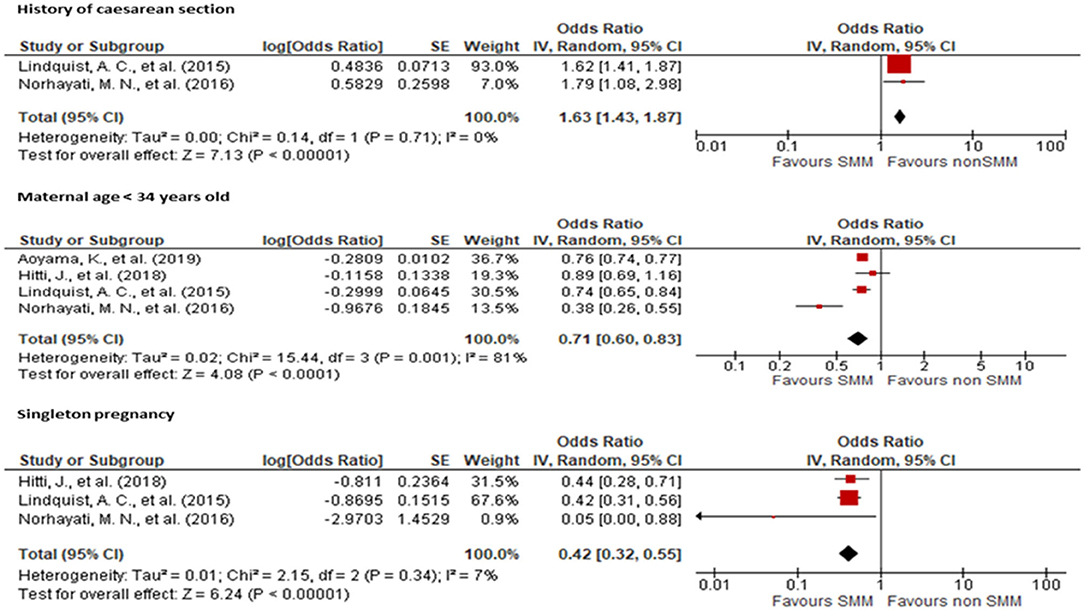
Figure 3. Forest plot showing the association of history of cesarean section, maternal age, and singleton pregnancy with severe maternal morbidity.
Two studies (19, 25) showed no association between parity and SMM occurrence with an OR of 1.17 for primiparous women (95% CI: 0.92, 1.50) when compared to multiparous women. Likewise, two studies (12, 19) showed no association between history of abortion and SMM occurrence with an OR of 1.17 (95% CI: 0.86, 1.61) (Figure 4) when compared to women without a history of abortion.
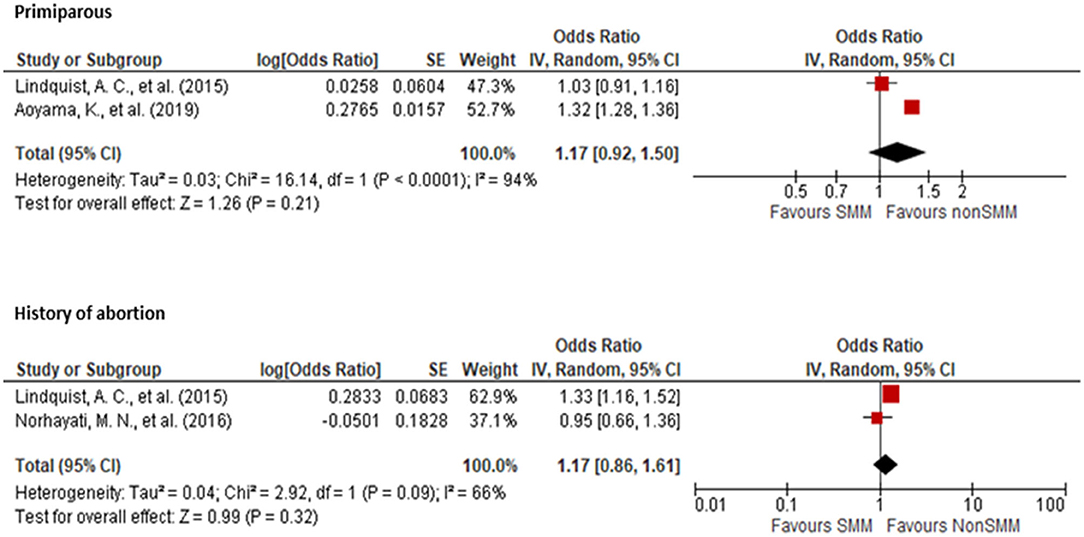
Figure 4. Forest plot showing the association of parity and history of abortion with severe maternal morbidity.
Two studies (12, 19) showed a significant association between coexisting medical conditions and SMM with an OR of 1.51 (95% CI: 1.28, 1.78) when compared to mothers without medical conditions. Three studies (12, 19, 25) showed an association between vaginal delivery and SMM with an OR of 0.11 (95% CI: 0.02, 0.47) when compared to cesarean delivery. Lastly, one study showed an association between full-term delivery and SMM with an OR of 0.14 (95% CI: 0.08, 0.23) when compared to pre-term delivery (Figure 5).
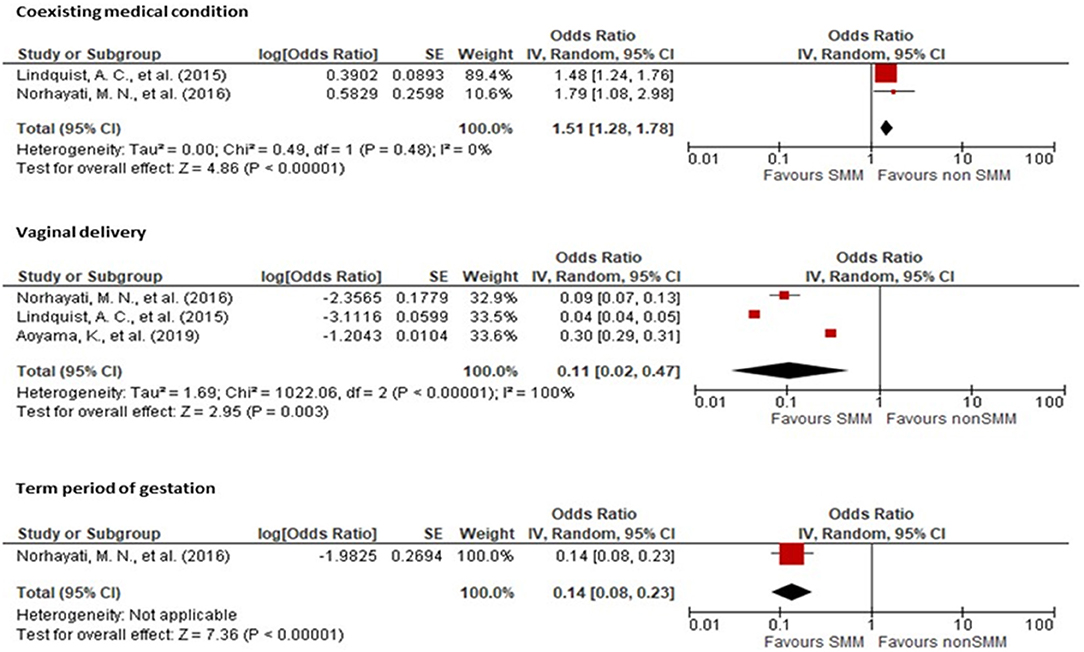
Figure 5. Forest plot showing the association of history of coexisting medical conditions, vaginal delivery, and gestational period with severe maternal morbidity.
Maternal Near Miss
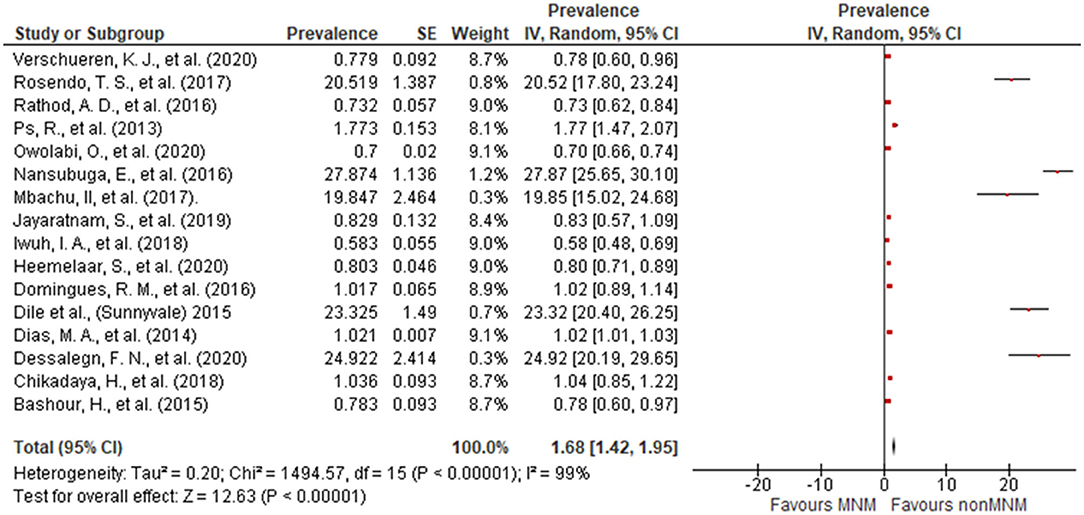
Sixteen articles were included in the estimation of the pooled prevalence of MNM. A wide variance in the prevalence of MNM was observed. The lowest reported prevalence was 0.58% (33) and the highest was 27.87% (28). The overall pooled prevalence of MNM was 1.68% (95% CI: 1.42, 1.95) (Figure 6).
One study (23) reported an association between a history of cesarean section and MNM with an OR of 2.68 (95% CI: 1.41, 5.10) compared to women without a history of cesarean section. Additionally, the same study (23) showed an association between a history of abortion and MNM with an OR of 1.64 (95% CI: 0.92, 2.93) when compared to women with no history of abortion (Figure 7).
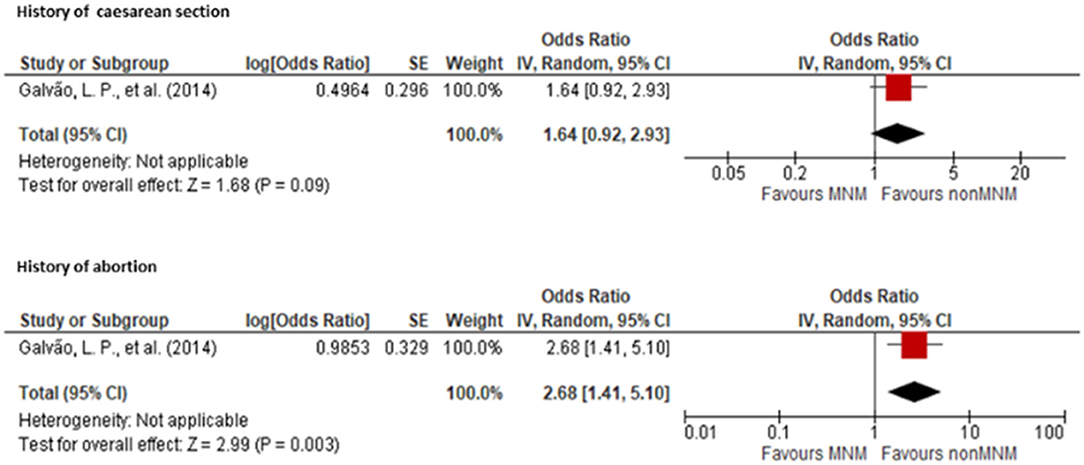
Figure 7. Forest plot showing the association of history of cesarean section and abortion with maternal near miss.
Discussion
In our analysis, the worldwide prevalence of SMM and MNM was 2.45 and 1.68%, respectively. The risk factors of history of cesarean section, advanced maternal age, multiple pregnancies, co-existing medical conditions, and cesarean birth were associated with SMM, while the sole reported risk factor for MNM was a history of cesarean section.
Older maternal age has been associated with a greater likelihood of having pre-existing medical conditions, a higher risk of obstetric complications, maternal morbidity, and an increased risk of progression from SMM to death (42). In our review, it can be concluded that advanced maternal age increases the risk of SMM. Contrary to the results of other reviews, we found that maternal morbidity was higher in mothers at both ends of the age spectrum, such as those of age >35 years and adolescents (43).
According to a review (43), national estimates from vital registration in the United States suggest that adolescents have a lower MMR than women of age >20 years. The same review also reported statistics from the United Kingdom showing that the MMR for women of age under 20 years is slightly higher than that of women of age 20–24 years but lower than that of women of age >25 years. Conversely, data from Australia suggest that the MMR for women of age under 20 years is higher than those of all other age groups apart from women of age >40 years. Evidence from both developing and developed countries also suggests that risks are greater for younger adolescents, with girls of age 15 years or younger having higher mortality rates than older adolescents. In most countries, adolescent births are concentrated among poorer, less educated women, which further compounds their disadvantaged situation by disrupting school attendance and limiting future livelihood opportunities.
In terms of physiological risk, the evidence is somewhat conflicting. Still, some evidence suggests that young women are at increased risk of several direct causes of maternal mortality, such as eclampsia, and indirect causes, such as obstructed labor. A study in Latin America also showed increased risks of hemorrhage and sepsis in young women, particularly those under 16 years of age (43).
According to a report by the Centers for Disease Control and Prevention, the MMR in the United States increased gradually with increasing maternal age and particularly in women older than 35 years, specifically, a 3.5-fold increase in MMR. This increased rate of maternal mortality is mostly attributed to comorbidities and coexisting medical conditions, such as metabolic syndrome, past and current cancer, cardiovascular, renal, and autoimmune diseases, which are more prevalent among older pregnant women. For instance, hypertension and Type II diabetes are more common in older women, and women older than 35 years have a 2- to 4-fold higher risk of having hypertension compared to women aged 30–34 years (44).
Women with a prior cesarean delivery had almost two times the risk (CI: 1.93, 2.23) of SMM compared to those without a prior cesarean delivery. Prior cesarean delivery is known to be associated with preeclampsia, placenta previa, placenta accreta, placental abruption, uterine rupture, postpartum infection, transfusion, and admission to the intensive care unit (14). The risks of placenta previa and morbidly adherent placenta in subsequent pregnancies increased markedly with an increasing number of prior cesarean sections. Compared with those without a history of cesarean section, pregnant women with a history of cesarean section were significantly more likely to experience uterine rupture, morbidly adherent placenta, MNM, severe maternal outcomes, and placenta previa. Uterine rupture during pregnancy and delivery is one of the most devastating obstetric complications, as it frequently results in life-threatening maternal and fetal compromises (45).
According to the 2018 annual report by the National Perinatal Epidemiology Center of Ireland, 45.4% of women who experienced an SMM in 2016 were nulliparous (46). The SMM rate for multiparous women was 6.46 per 1,000, 32% higher than that of primiparous women. However, nulliparous women had the highest SMM of 7.66 per 1,000 births, 56% higher than primiparous women at 4.91 per 1,000 births.
A French study found that the risk for SMM was significantly higher for unplanned cesarean deliveries at all maternal ages. In contrast, the planned delivery mode analysis showed an increased risk of SMM associated with planned cesarean delivery compared with planned vaginal delivery in only women aged 35 years and older (42).
According to a secondary analysis by the WHO Multicountry Survey on Maternal and Newborn Health (WHOMCS), a cross-sectional study performed in 29 countries, it was found that twin pregnancies had a higher risk of contributing to SMM and mortality in all regions (47). Using the new WHO diagnostic criteria for severe maternal conditions, another recent WHOMCS study identified that twin pregnancies doubled the risk of SMM, tripled the risk of MNM, and increased the risk of maternal death 4-fold when compared to singleton pregnancies. The current review found a higher occurrence of preterm deliveries in SMM, which correlates with the underlying etiology of the women's medical conditions.
According to the WHO, maternal deaths have been described as the tip of the iceberg and maternal morbidity as the base (5). For every woman who dies from pregnancy-related reasons, another 20 to 30 women suffer from acute or chronic morbidity, frequently with long-term consequences that impair their ability to function normally. Women's physical, mental, and sexual health, as well as their ability to perform in particular areas (e.g., cognition, mobility, and social involvement), body image, and socioeconomic position, are all affected by these consequences. Maternal morbidity, like maternal mortality, is expected to be the highest in low- and middle-income nations, particularly among the poorest women. There are no proper standardized results on the implications of SMM. However, it is well-known that it can lead to short- and long-term consequences, which are preventable.
The studies in the current review underwent quality assessment, and only good-quality studies with a low risk of bias were included. There were only a few studies that compared women with and without maternal complications, which did not allow us to identify population risk factors. The heterogeneity in the outcomes ranged from low to high, possibly due to the participants' sociodemographic characteristics. However, subgroup analysis was not possible because of the limited number of studies that had substantial heterogeneity. We involved only three databases for searching. However, MEDLINE is the most extensive database for social and medical sciences and the inclusion of 24 papers is strong enough to conclude the outcome. Moreover, we have displayed the cumulative effect estimates in forest plots that consolidate the findings.
Conclusions
Notably, identifying the risk factors for severe maternal morbidity and maternal near miss is pertinent to prevent maternal death. Quantifying the strength of association of the risk factors and surveillance of the presence of these factors at primary and tertiary care levels helps to identify the interventions required that can be performed during antenatal care and childbirth. Initiatives such as educational programs, campaigns, and early detection of risk factors contributing to SMM and MNM are recommended. Proper follow-up is important to monitor the progression of maternal health during the antenatal and postnatal periods. We recommend additional studies comparing women with and without SMM and MNM using the WHO definition and criteria.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Author Contributions
NHNH, MNN, and ISB: conceptualization, methodology, and visualization. MNN and NHNH: validation, resources, and data curation. MNN and HRMK: formal analysis and writing of original draft preparation. HRMK: investigation. NHNH, MNN, ISB, and HRMK: writing of review and editing. NHNH: project administration. All authors have read and agreed to the published version of the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors would like to thank Madam Nurul Azurah Mohd Roni, a librarian from Hamdan Tahir Library, for her assistance with the database searches.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2022.861028/full#supplementary-material
References
1. WHO. Evaluating the Quality of Care for Severe Pregnancy Complications: The WHO Near-Miss Approach for Maternal Health. Geneva: World Health Organization (2011).
2. Say L, Souza JP, Pattinson RC. Maternal near miss–towards a standard tool for monitoring quality of maternal health care. Best Pract Res Clin Obstet Gynaecol. (2009) 23:287–96. doi: 10.1016/j.bpobgyn.2009.01.007
3. WHO. Trends in Maternal Mortality: 1990 to 2015: Estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division. Geneva: World Health Organization (2015).
4. Tuncalp O, Hindin MJ, Souza JP, Chou D, Say L. The prevalence of maternal near miss: A systematic review. BJOG. (2012) 119:653–61. doi: 10.1111/j.1471-0528.2012.03294.x
5. Firoz T, Chou D, von Dadelszen P, Agrawal P, Vanderkruik R, Tunçalp O, et al. Measuring maternal health: focus on maternal morbidity. Bull World Health Organ. (2013) 91:794–6. doi: 10.2471/BLT.13.117564
6. King JC. Maternal mortality in the United States–why is it important and what are we doing about it? Semin Perinatol. (2012) 36:14–8. doi: 10.1053/j.semperi.2011.09.004
7. Van Hanegem N, Miltenburg AS, Zwart JJ, Bloemenkamp KW, Van Roosmalen J. Severe acute maternal morbidity in asylum seekers: a two-year nationwide cohort study in the Netherlands. Acta Obstet Gynecol Scand. (2011) 90:1010–6. doi: 10.1111/j.1600-0412.2011.01140.x
8. de Moraes AP, Barreto SM, Passos VM, Golino PS, Costa JE, Vasconcelos MX. Severe maternal morbidity: a case-control study in Maranhao, Brazil. Reprod Health. (2013) 10:11. doi: 10.1186/1742-4755-10-11
9. Lindquist A, Knight M, Kurinczuk JJ. Variation in severe maternal morbidity according to socioeconomic position: a UK national case-control study. BMJ Open. (2013) 3:6. doi: 10.1136/bmjopen-2013-002742
10. Liu S, Joseph KS, Hutcheon JA, Bartholomew S, León JA, Walker M, et al. Gestational age-specific severe maternal morbidity associated with labor induction. Am J Obstet Gynecol. (2013) 209:209.e1-8. doi: 10.1016/j.ajog.2013.05.033
11. van Mello NM, Zietse CS, Mol F, Zwart JJ, van Roosmalen J, Bloemenkamp KW, et al. Severe maternal morbidity in ectopic pregnancy is not associated with maternal factors but may be associated with quality of care. Fertil Steril. (2012) 97:623–9. doi: 10.1016/j.fertnstert.2011.12.021
12. Norhayati MN, Nik Hazlina NH, Aniza AA, Sulaiman Z. Factors associated with severe maternal morbidity in Kelantan, Malaysia: A comparative cross-sectional study. BMC Pregnancy Childbirth. (2016) 16:185. doi: 10.1186/s12884-016-0980-2
13. Oliveira FC Jr, Costa ML, Cecatti JG, Pinto e Silva JL, Surita FG. Maternal morbidity and near miss associated with maternal age: the innovative approach of the 2006 Brazilian demographic health survey. Clinics. (2013) 68:922–7. doi: 10.6061/clinics/2013(07)06
14. Gray KE, Wallace ER, Nelson KR, Reed SD, Schiff MA. Population-based study of risk factors for severe maternal morbidity. Paediatr Perinat Epidemiol. (2012) 26:506–14. doi: 10.1111/ppe.12011
15. Roost M, Altamirano VC, Liljestrand J, Essen B. Does antenatal care facilitate utilization of emergency obstetric care? A case-referent study of near-miss morbidity in Bolivia. Acta Obstet Gynecol Scand. (2010) 89:335–42. doi: 10.3109/00016340903511050
16. van Dillen J, Zwart JJ, Schutte J, Bloemenkamp KW, van Roosmalen J. Severe acute maternal morbidity and mode of delivery in the Netherlands. Acta Obstet Gynecol Scand. (2010) 89:1460–5. doi: 10.3109/00016349.2010.519018
17. Aromataris E, Munn Z. JBI Manual for Evidence Synthesis. The Joanna Briggs Institute. Adelaide (2020). doi: 10.46658/JBIMES-20-01
18. Higgins JPT TJ, Chandler J, Cumpston M, Li T, Page MJ, Welch VA. Cochrane Handbook for Systematic Reviews of Interventions version 6.1 (updated September 2020). Cochrane (2020). doi: 10.1002/9781119536604
19. Lindquist AC, Kurinczuk JJ, Wallace EM, Oats J, Knight M. Risk factors for maternal morbidity in Victoria, Australia: a population-based study. BMJ Open. (2015) 5:e007903. doi: 10.1136/bmjopen-2015-007903
20. Hitti J, Sienas L, Walker S, Benedetti TJ, Easterling T. Contribution of hypertension to severe maternal morbidity. Am J Obstet Gynecol. (2018) 219:405.e1-405. doi: 10.1016/j.ajog.2018.07.002
21. Dzakpasu S, Deb-Rinker P, Arbour L, Darling EK, Kramer MS, Liu S, et al. Severe maternal morbidity surveillance: Monitoring pregnant women at high risk for prolonged hospitalisation and death. Paediatr Perinat Epidemiol. (2020) 34:427–439. doi: 10.1111/ppe.12574
22. Das I, Datta M, Samanta S, Mahapatra B, Mukherjee P. A cross-sectional study on post-partum severe acute maternal morbidity and maternal deaths in a Tertiary Level Teaching Hospital of Eastern India. Int J Women Health Reproduct Sci. (2014) 2:113–8. doi: 10.15296/ijwhr.2014.18
23. Galvão LP Alvim-Pereira F de Mendonça CM Menezes FE Góis KA Ribeiro RF , et al., The prevalence of severe maternal morbidity and near miss and associated factors in Sergipe, Northeast Brazil. BMC Pregnancy Childbirth. (2014) 14:25. doi: 10.1186/1471-2393-14-25
24. Zhang T, Wang H, Wang X, Yang Y, Zhang Y, Tang Z, et al. The adverse maternal and perinatal outcomes of adolescent pregnancy: a cross sectional study in Hebei, China. BMC Pregnancy Childbirth. (2020) 20:339. doi: 10.1186/s12884-020-03022-7
25. Aoyama K, Pinto R, Ray JG, Hill AD, Scales DC, Lapinsky SE, et al. Association of maternal age with severe maternal morbidity and mortality in Canada. JAMA network open. (2019) 2:e199875. doi: 10.1001/jamanetworkopen.2019.9875
26. Bashour H, Saad-Haddad G, DeJong J, Ramadan MC, Hassan S, Breebaart M, et al. A cross sectional study of maternal “near-miss” cases in major public hospitals in Egypt, Lebanon, Palestine and Syria. BMC Pregnancy Childbirth. (2015) 15:296. doi: 10.1186/s12884-015-0733-7
27. Dessalegn FN, Astawesegn FH, Hankalo NC. Factors associated with maternal near miss among women admitted in West Arsi Zone Public Hospitals, Ethiopia: unmatched case-control study. J Pregnancy. (2020) 2020:6029160. doi: 10.1155/2020/6029160
28. Nansubuga E, Ayiga N, Moyer CA. Prevalence of maternal near miss and community-based risk factors in Central Uganda. Int J Gynaecol Obstet. (2016) 135:214–20. doi: 10.1016/j.ijgo.2016.05.009
29. Rosendo TS, Roncalli AG, Azevedo GD. Prevalence of maternal morbidity and its association with socioeconomic factors: a population-based survey of a city in Northeastern Brazil. Rev Bras Ginecol Obstet. (2017) 39:587–95. doi: 10.1055/s-0037-1606246
30. Chikadaya H, Madziyire MG, Munjanja SP. Incidence of maternal near miss in the public health sector of Harare, Zimbabwe: a prospective descriptive study. BMC Pregnancy Childbirth. (2018) 18:458. doi: 10.1186/s12884-018-2092-7
31. Rathod AD, Chavan RP, Bhagat V, Pajai S, Padmawar A, Thool P. Analysis of near-miss and maternal mortality at tertiary referral centre of rural India. J Obstet Gynaecol India. (2016) 66:295–300. doi: 10.1007/s13224-016-0902-2
32. Verschueren KJ, Kodan LR, Paidin RR, Samijadi SM, Paidin RR, Rijken MJ, et al. Applicability of the WHO maternal near-miss tool: a nationwide surveillance study in Suriname. J Glob Health. (2020) 10:020429. doi: 10.7189/jogh.10.020429
33. Iwuh IA, Fawcus S, Schoeman L. Maternal near-miss audit in the Metro West maternity service, Cape Town, South Africa: a retrospective observational study. S Afr Med J. (2018) 108:171–5. doi: 10.7196/SAMJ.2018.v108i3.12876
34. Dias MA, Domingues RM, Schilithz AO, Nakamura-Pereira M, Diniz CS, Brum IR, et al. Incidence of maternal near miss in hospital childbirth and postpartum: data from the Birth in Brazil study. Cad Saude Publica. (2014) 30(Suppl. 1):S1–12. doi: 10.1590/0102-311X00154213
35. Domingues RM, Dias MA, Schilithz AO, Leal MD. Factors associated with maternal near miss in childbirth and the postpartum period: findings from the birth in Brazil National Survey, 2011-2012. Reprod Health. (2016) 13:115. doi: 10.1186/s12978-016-0232-y
36. Heemelaar S, Josef M, Diener Z, Chipeio M, Stekelenburg J, van den Akker T, et al. Maternal near-miss surveillance, Namibia. Bull World Health Organ. (2020) 98:548–57. doi: 10.2471/BLT.20.251371
37. Mbachu II, Ezeama C, Osuagwu K, Umeononihu OS, Obiannika C, et al. A cross sectional study of maternal near miss and mortality at a rural tertiary centre in southern Nigeria. BMC Pregnancy Childbirth. (2017) 17:251. doi: 10.1186/s12884-017-1436-z
38. Ps R, Verma S, Rai L, Kumar P, Pai MV, Shetty J. “Near miss” obstetric events and maternal deaths in a tertiary care hospital: an audit. J Pregnancy. (2013) 2013:393758. doi: 10.1155/2013/393758
39. Dile M, Seyum T. Proportion of maternal near misses and associated factors in referral hospitals of Amhara regional state, Northwest Ethiopia: institution based cross sectional study. Gynecol Obstet. (2015) 5:2161. doi: 10.4172/2161-0932.1000308
40. Jayaratnam S, Soares M, Jennings B, Thapa AP, Woods C. Maternal mortality and 'near miss' morbidity at a tertiary hospital in Timor-Leste. Aust N Z J Obstet Gynaecol. (2019) 59:567–72. doi: 10.1111/ajo.12940
41. Owolabi O, Riley T, Juma K, Mutua M, Pleasure ZH, Amo-Adjei J, et al. Incidence of maternal near-miss in Kenya in 2018: findings from a nationally representative cross-sectional study in 54 referral hospitals. Sci Rep. (2020) 10:15181. doi: 10.1038/s41598-020-72144-x
42. Korb D, Goffinet F, Seco A, Chevret S, Deneux-Tharaux C. Risk of severe maternal morbidity associated with cesarean delivery and the role of maternal age: a population-based propensity score analysis. Can Med Assoc J. (2019) 191:E352–60. doi: 10.1503/cmaj.181067
43. Nove A, Matthews Z, Neal S, Camacho AV. Maternal mortality in adolescents compared with women of other ages: evidence from 144 countries. Lancet Global Health. (2014) 2:e155–64. doi: 10.1016/S2214-109X(13)70179-7
44. Attali E, Yogev Y. The impact of advanced maternal age on pregnancy outcome. Best Pract Res Clin Obstet Gynaecol. 70:2–9. doi: 10.1016/j.bpobgyn.2020.06.006
45. Kietpeerakool C, Lumbiganon P, Laopaiboon M, Rattanakanokchai S, Vogel JP, Gülmezoglu AM. Pregnancy outcomes of women with previous caesarean sections: secondary analysis of World Health Organization Multicountry Survey on Maternal and Newborn Health. Sci Rep. (2019) 9:9748. doi: 10.1038/s41598-019-46153-4
Keywords: severe maternal morbidity, maternal near miss, prevalence, risk factor, meta-analysis
Citation: Nik Hazlina NH, Norhayati MN, Shaiful Bahari I and Mohamed Kamil HR (2022) The Prevalence and Risk Factors for Severe Maternal Morbidities: A Systematic Review and Meta-Analysis. Front. Med. 9:861028. doi: 10.3389/fmed.2022.861028
Received: 24 January 2022; Accepted: 18 February 2022;
Published: 17 March 2022.
Edited by:
Elisa Bevilacqua, Fondazione Policlinico Agostino Gemelli IRCCS, ItalyReviewed by:
Nigussie Tadesse Sharew, University of Groningen, NetherlandsMohd Faizal Ahmad, National University of Malaysia, Malaysia
Copyright © 2022 Nik Hazlina, Norhayati, Shaiful Bahari and Mohamed Kamil. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mohd Noor Norhayati, aGF5YXRpa2tAdXNtLm15
 Nik Hussain Nik Hazlina
Nik Hussain Nik Hazlina Mohd Noor Norhayati
Mohd Noor Norhayati Ismail Shaiful Bahari2
Ismail Shaiful Bahari2