- 1Department of Emergency and Critical Care Medicine, Nippon Medical School Hospital, Tokyo, Japan
- 2Department of Emergency Medicine, Hokkaido University Hospital, Sapporo, Japan
Background: Patients with blunt chest trauma have a high mortality rate. The assessment of blush in hepatic and splenic trauma is important for determining the need for emergency hemostatic interventions. However, the frequency and importance of blush in lung contusions are unknown. Therefore, this study aimed to evaluate the frequency of blush in patients with lung contusions and elucidate the relationship between blush and the clinical outcomes of patients with blunt chest trauma.
Materials and Methods: In this retrospective observational study, we enrolled patients with an injury severity score of 16 or higher and a chest abbreviated injury scale (AIS) score of 3 or higher who were admitted to the emergency department of Hokkaido University Hospital from January 1, 2003, to December 31, 2016. Blush was defined as active extravasation of an intravascular contrast agent recognized on contrast-enhanced computed tomography. The date of trauma, trauma severity, treatments, and outcomes were obtained from the patients’ electronic medical records.
Results: During the study period, 83 patients had severe lung contusions and 13 had blush. In-hospital mortality of patients with blush was significantly higher than that of patients without blush (53 vs. 10%, P < 0.001). Patients with blush required thoracic drainage more frequently (100 vs. 71%, P < 0.001) and support through mechanical ventilation more often (100 vs. 64%, P < 0.001) and for a longer duration (median duration, 0 vs. 25 days, P = 0.001) than patients without blush.
Conclusions: Our study revealed that blush in lung contusions was not rare and was associated with a high risk of mortality in patients with severe blunt chest trauma. Clinicians should not hesitate to intervene if blush is detected in a lung contusion of a patient with blunt chest trauma.
Introduction
For clinicians, reducing the number of preventable deaths among trauma patients in the emergency department is important. Chest trauma is the third most common cause of death in patients with multiple trauma, after abdominal and head trauma (1). Current studies report that the mortality rate of blunt chest trauma among patients with multiple trauma ranges from 5.5 to 25% (1–3). Severe lung contusion has a significant impact on clinical prognosis (2, 3). Severe lung contusions may also be associated with massive intrapulmonary bleeding, and severe cases requiring several clinical interventions are frequently reported (4, 5).
Blush, which has been frequently reported in hepatic and splenic trauma, is defined as active extravasation of the intravenous contrast agent recognized on computed tomography (6–8). Blush was reportedly observed in 6.6–17.1% of patients with severe hepatic and splenic trauma (6–11). The presence of blush in hepatic and splenic trauma indicates current progressive bleeding and implies the need for emergency hemostatic interventions such as transcatheter arterial embolization and abdominal surgery (6–11). Therefore, in some current management algorithms for hepatic and splenic trauma, blush has an important role in evaluating the necessity for emergency hemostatic interventions (6–11).
Although blush in lung contusions is sometimes observed in patients with severe blunt trauma in our clinical setting, its frequency and importance are unclear. Therefore, the present study was conducted to evaluate the frequency and relationship of blush in lung contusions with clinical outcomes in patients with blunt trauma.
Materials and Methods
Approval for this study was obtained from the Institutional Review Board of the Ethics Committee at Hokkaido University Hospital. The ethics board waived the need for informed consent owing to the retrospective design.
Patients
We retrospectively enrolled blunt injury patients with injury severity scores (ISS) ≥16 and chest abbreviated injury scale (AIS) scores ≥3 who were transported to the emergency department of Hokkaido University Hospital between January 1, 2003, and December 31, 2016. We excluded patients who had not undergone contrast-enhanced computed tomography (CECT) on admission to our emergency department. Furthermore, patients whose maximum diameter of lung contusion was less than 5 cm on computed tomography were excluded. Data on each patient’s age; sex; mechanism of injury; vital signs; respiratory Sequential Organ Failure Assessment, ISS, and AIS scores of each body part; in-hospital mortality; ventilator-free days; and specific treatments (such as mechanical ventilator support, thoracic drainage, isolated lung ventilation, extracorporeal membrane oxygenation support, and thoracic surgery) were obtained from the individual electronic medical records.
Definition
Blush was defined as active extravasation of intravenous contrast recognized on CECT, similar to previous reports (6–8). A typical blush is shown in Figure 1. Severe lung contusion was defined as ≥5 cm of maximum diameter on computed tomography.
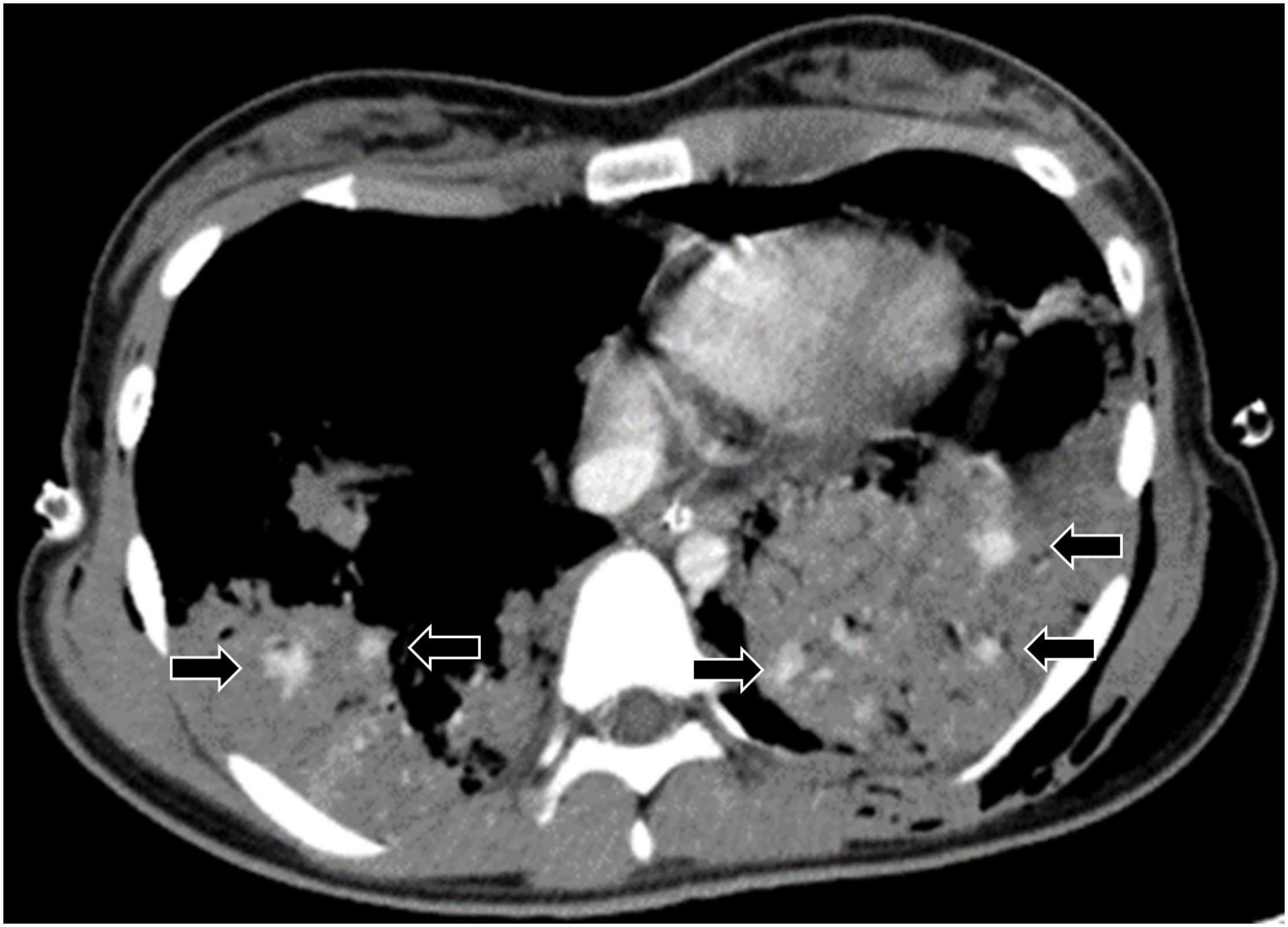
Figure 1. Typical blush in lung contusion. Arrows indicate extravasation of contrast media in the lung contusion, which is defined as blush.
Statistical Analysis
Statistical analysis was conducted using JMP 12.0.1 for Windows (SAS Institute Inc., Cary, NC, United States). Statistical significance was assessed at the 0.05 level unless otherwise noted. Data were summarized using medians and interquartile ranges (25th–75th percentile) or counts and percentages, where appropriate. Univariate comparisons were compared using chi-square tests for categorical variables and Wilcoxon rank-sum tests for continuous variables.
Results
From January 1, 2003, to December 31, 2016, 247 patients with ISS ≥16 and chest AIS scores ≥3 were admitted to the emergency department. Of these, 82 patients who had not undergone CECT on admission, 35 without lung contusion injuries, and 67 without severe lung contusion injuries were excluded. Among 83 patients with severe lung contusion injuries, 13 patients with blush in the lung contusions were identified (Figure 2). The patients with blush in the lung contusions were 10% of patients with lung contusions and 15% of patients with severe lung contusions.
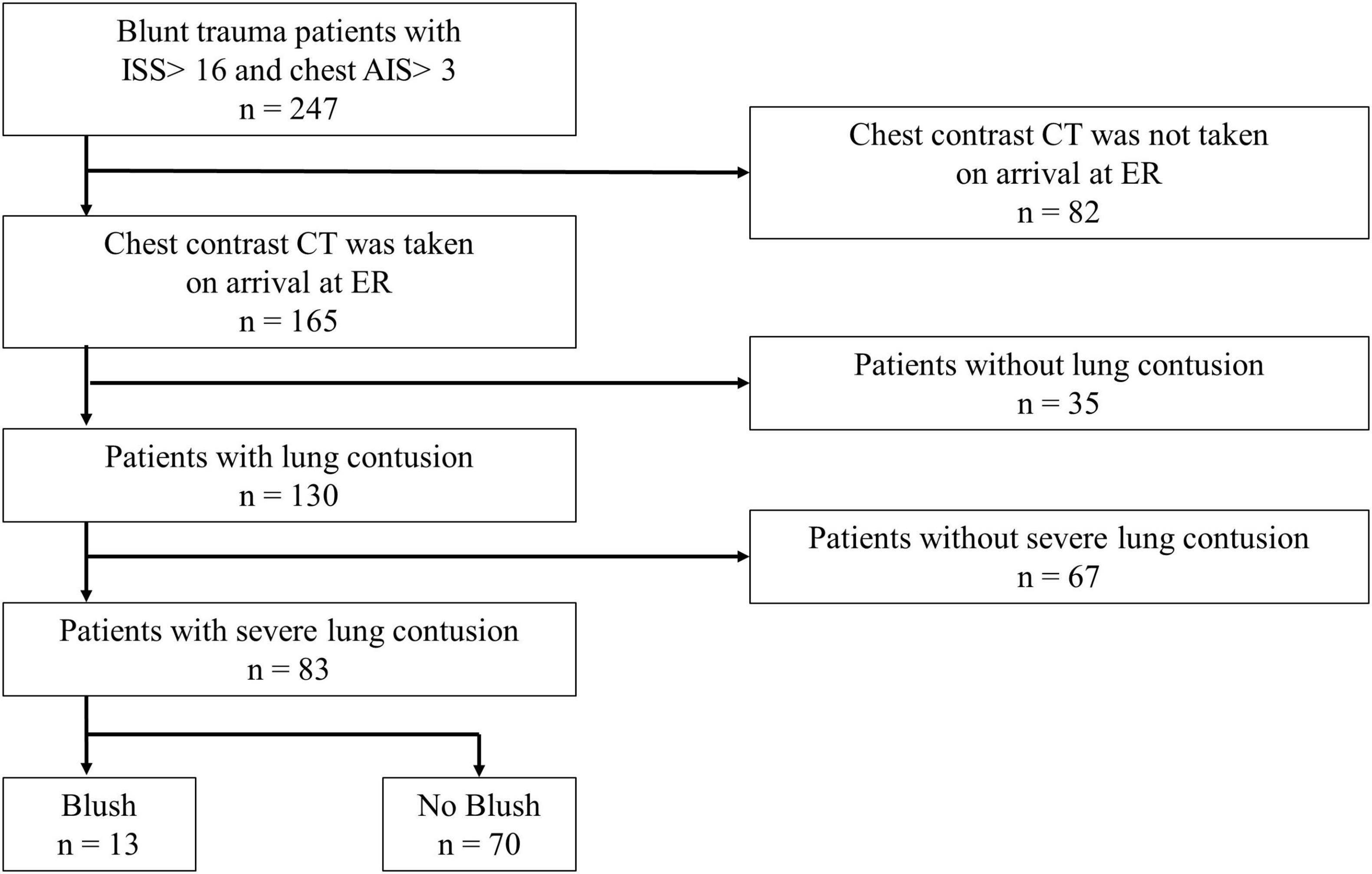
Figure 2. Flowchart of the study selection process. The blush group included patients in whom blush was detected in the severe lung contusion (≥5 cm of maximum diameter) on contrast-enhanced CT on arrival at the ER. The no blush group included patients who had severe lung contusions but for whom blush was not detected. ISS, injury severity score; AIS, abbreviated injury scale; CT, computed tomography; ER, emergency room.
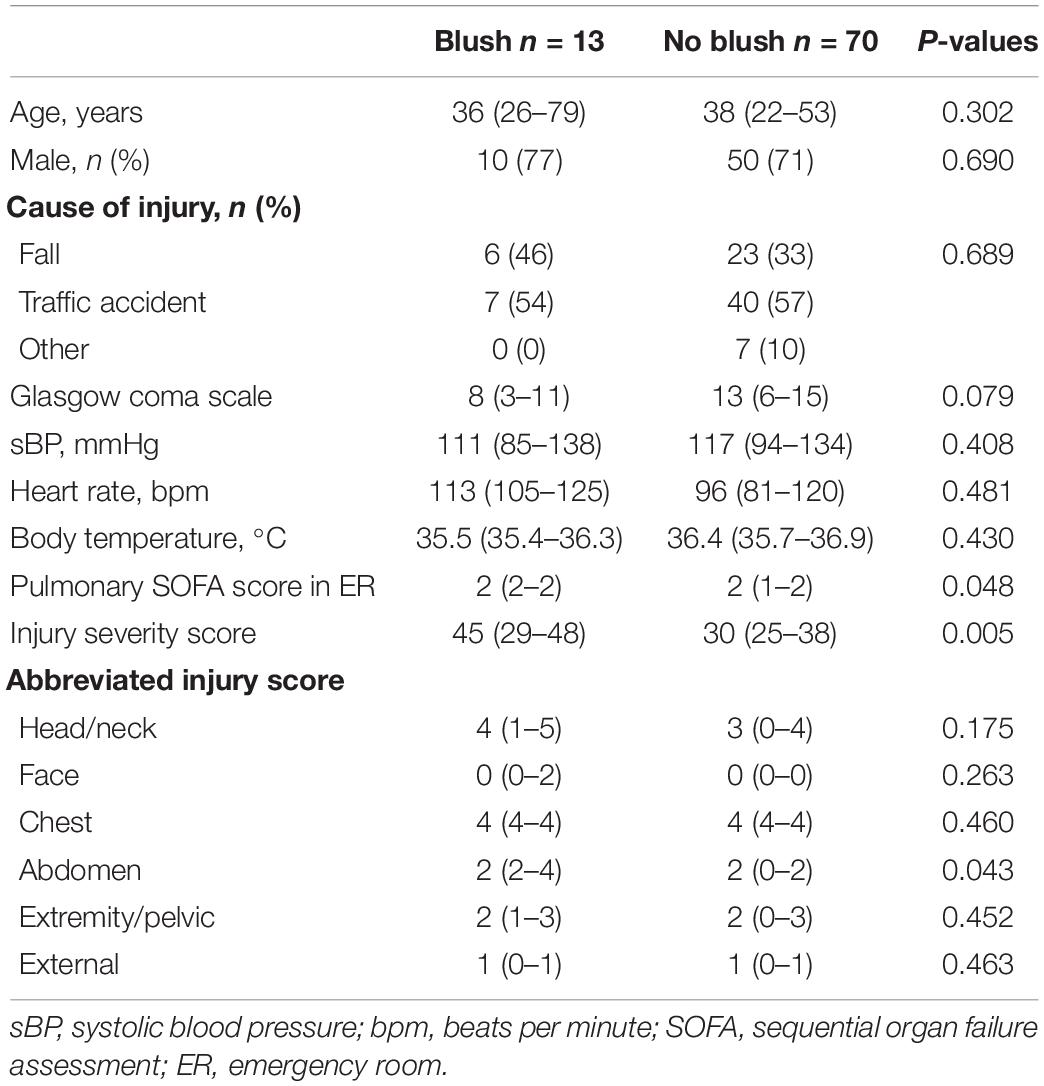
The patients with blush did not show any difference in age, sex, or cause of injury from the patients without blush. There was no significant difference in individual chest AIS scores between the two groups; however, the abdomen AIS and ISS scores in patients with blush were higher than those in patients without blush (Table 1).
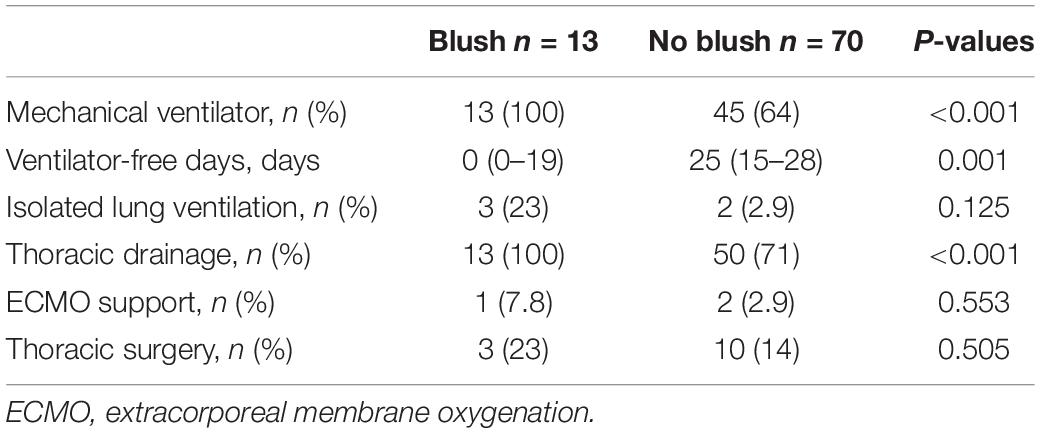
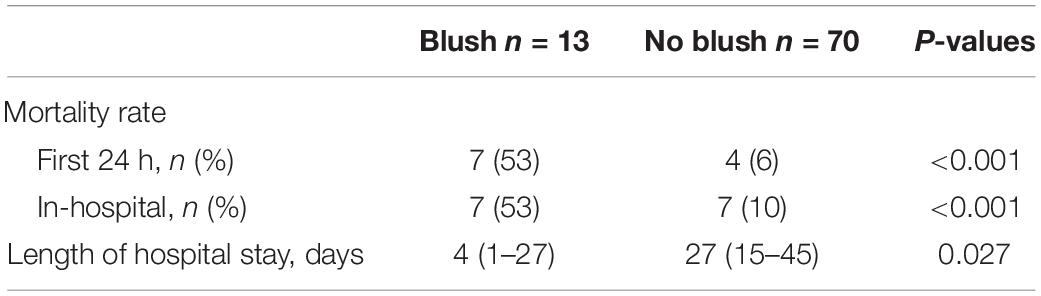
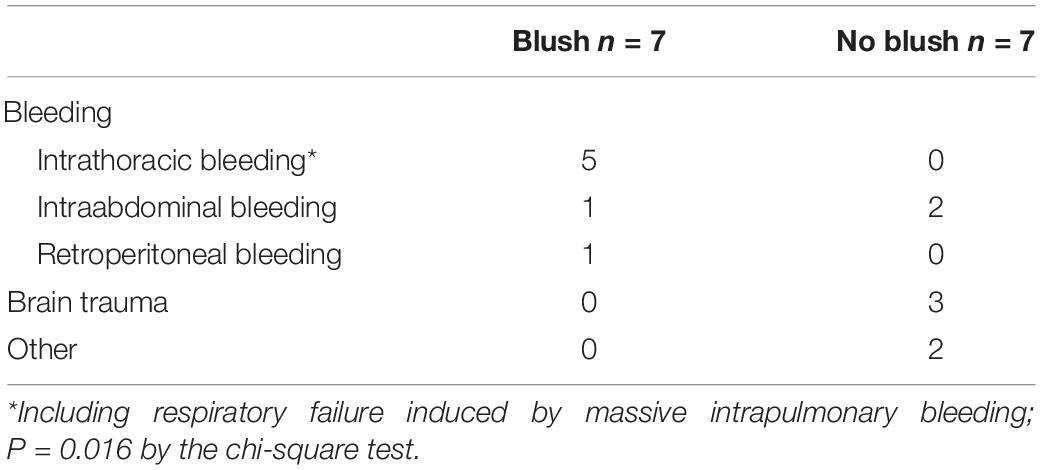
Tables 2, 3 show, respectively, the clinical interventions and outcomes of patients with and without blush. In patients with blush, the in-hospital and first 24-h mortality rates were significantly higher than those in patients without blush. Furthermore, the frequency of use of mechanical ventilator support in patients with blush was higher than that in patients without blush. Ventilator-free days in patients with blush were fewer than those for patients without blush. In terms of specific treatment, the use of isolated lung ventilation supports was frequent in patients with blush. In patients with blush, the major cause of death was severe intrathoracic bleeding, including respiratory failure induced by massive intrapulmonary bleeding (Table 4).
Discussion
In this single-institute retrospective observational study, blush in lung contusions occurred in 15% of patients with severe lung contusions. Furthermore, the blush in lung contusions was associated with the necessity for various interventions and with a high mortality rate. In addition, the blush group had more acute deaths than the no blush group. Therefore, the length of hospital stay in the blush group was shorter than that in the no blush group because of survival bias.
Treatment strategies have been established for blush in hepatic and splenic trauma, and the mortality rate of these patients has been reported to be 0–8.4% (6, 8–10). However, to the best of our knowledge, no investigation into the urgency of blush in lung contusion has previously been reported. In the present study, blush in the lung contusion was more frequently observed than in previous hepatic and splenic trauma (6, 8–10). Furthermore, blush in lung contusions was clearly associated with poor patient outcomes. However, the urgency of seeing blush in a lung contusion CECT had not been recognized by attending physicians in our institution before the present study. Therefore, because no management strategy had also been established, patients with blush in lung contusion would have a high mortality rate. Similar to blush in hepatic or splenic trauma, blush in lung contusion will be a good indicator to guide the management strategy for patients with chest trauma.
Blush in lung contusions indicates ongoing hemorrhage, similar to blush in hepatic and splenic injuries. However, the effects of ongoing hemorrhages are much different between lung contusions and hepatic/splenic injuries, because the hemorrhages in lung contusions are also frequently intra-airway hemorrhages. Intra-airway hemorrhages from lung contusions exacerbate respiratory conditions, even if the amount of hemorrhage is small (4, 12, 13). Therefore, when blush is detected in lung contusions, clinicians need to intervene more aggressively to stop the hemorrhage.
Therapeutic interventions for hemorrhage in lung contusions are twofold: protection of the contralateral lung from pulmonary hemorrhage and hemostatic intervention (13). One simple form of protection of the contralateral lung from intra-airway hemorrhage is isolated lung ventilation. When blush in the lung contusion is detected, it may be necessary to isolate the contralateral lung before the exacerbation of the respiratory condition by intra-airway hemorrhage from the lung injury. Although lung resection and lobectomy are definitive hemostatic procedures for lung injury, they are highly invasive. Therefore, trans-arterial embolization is frequently selected for pulmonary hemorrhage, similar to the treatment of hepatic and splenic injuries (13, 14). However, the lungs have blood supply from two vessel systems: the tracheal and pulmonary artery systems. Furthermore, blood flow in the pulmonary artery is more than that in the tracheal artery in the lung. Therefore, control of blood flow in the pulmonary artery by, for example, balloon occlusion, is necessary to stop the pulmonary hemorrhage (15, 16). When blush in lung contusions is detected, there is potential to improve prognosis by actively protecting the contralateral lung and performing hemostatic interventions to prevent further bleeding and worsening of the respiratory status.
Strengths and Limitations
The strength of our study lies in the fact that it is the first one to report the frequency of blush in lung contusions and its relationship with the outcomes. However, there are inherent limitations in any retrospective evaluation. Additionally, the numbers in this study may be considered small, hence precluding broad generalization. Furthermore, the observation period was so long that the treatment algorithm might have changed and contributed to the patients’ outcomes. Also, the significant difference in in-hospital stay between groups was affected by survival bias. However, to the best of our knowledge, this is the first report about blush in lung contusions and its characteristics. More extensive research is needed to confirm our results.
Our study revealed that blush in lung contusions was not rare and was associated with the necessity for various interventions and a high mortality rate. When blush in lung contusions is detected in patients with blunt chest trauma, clinicians must be aware of the dangers of the sign. Immediate protection of the contralateral lung from pulmonary hemorrhage and performing hemostatic interventions may improve outcomes, but further large-scale.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics Statement
This study was approved by Hokkaido University Hospital, and the requirement for informed consent was waived.
Author Contributions
NT collected and interpreted the data and drafted the manuscript. MH conceived the study, analyzed and interpreted the data, and drafted the manuscript. SY read the manuscript and revised it for important intellectual content. All authors read and approved the final manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We thank Editage (www.editage.com) for English language editing.
References
1. Chrysou K, Halat G, Hoksch B, Schmid RA, Kocher GJ. Lessons from a large trauma center: impact of blunt chest trauma in polytrauma patients-still a relevant problem? Scand J Trauma Resusc Emerg Med. (2017) 25:42. doi: 10.1186/s13049-017-0384-y
2. Mahmood I, El-Menyar A, Younis B, Ahmed K, Nabir S, Ahmed MN, et al. Clinical significance and prognostic implications of quantifying pulmonary contusion volume in patients with blunt chest trauma. Med Sci Monit. (2017) 23:3641–8. doi: 10.12659/msm.902197
3. Dogrul BN, Kiliccalan I, Asci ES, Peker SC. Blunt trauma related chest wall and pulmonary injuries: an overview. Chin J Traumatol. (2020) 23:125–38. doi: 10.1016/j.cjtee.2020.04.003
4. Park JM, Kim CW, Cho HM, Son BS, Kim DH. Induced airway obstruction under extracorporeal membrane oxygenation during treatment of life-threatening massive hemoptysis due to severe blunt chest trauma. J Thorac Dis. (2014) 6:E255–8. doi: 10.3978/j.issn.2072-1439.2014.10.22
5. Nagashima F, Inoue S, Ohta M. A patient with severe polytrauma with massive pulmonary contusion and hemorrhage successfully treated with multiple treatment modalities: a case report. J Med Case Rep. (2020) 14:69. doi: 10.1186/s13256-020-02406-9
6. Ingram MCE, Siddharthan RV, Morris AD, Hill SJ, Travers CD, McKracken CE, et al. Hepatic and splenic blush on computed tomography in children following blunt abdominal trauma: is intervention necessary? J Trauma Acute Care Surg. (2016) 81:266–70. doi: 10.1097/TA.0000000000001114
7. Alarhayem AQ, Myers JG, Dent D, Lamus D, Lopera J, Liao L, et al. “Blush at first sight”: significance of computed tomographic and angiographic discrepancy in patients with blunt abdominal trauma. Am J Surg. (2015) 210:1104–10; discussion 1110. doi: 10.1016/j.amjsurg.2015.08.009
8. Omert LA, Salyer D, Dunham CM, Porter J, Silva A, Protetch J. Implications of the ‘contrast blush’ finding on computed tomographic scan of the spleen in trauma. J Trauma. (2001) 51:272–7; discussion 277. doi: 10.1097/00005373-200108000-00008
9. Teuben MPJ, Spijkerman R, Blokhuis TJ, Pfeifer R, Teuber H, Pape HC, et al. Safety of selective nonoperative management for blunt splenic trauma: the impact of concomitant injuries. Patient Saf Surg. (2018) 12:32. doi: 10.1186/s13037-018-0179-8
10. Bhullar IS, Frykberg ER, Tepas JJ, Siragusa D, Loper T, Kerwin AJ. At first blush: absence of computed tomography contrast extravasation in Grade IV or V adult blunt splenic trauma should not preclude angioembolization. J Trauma Acute Care Surg. (2013) 74:105–11; discussion 111. doi: 10.1097/TA.0b013e3182788cd2
11. Burlew CC, Kornblith LZ, Moore EE, Johnson JL, Biffl WL. Blunt trauma induced splenic blushes are not created equal. World J Emerg Surg. (2012) 7:8. doi: 10.1186/1749-7922-7-8
12. Ogawa F, Sakai T, Takahashi K, Kato M, Yamaguchi K, Okazaki S, et al. A case report: veno-venous extracorporeal membrane oxygenation for severe blunt thoracic trauma. J Cardiothorac Surg. (2019) 14:88. doi: 10.1186/s13019-019-0908-9
13. Radchenko C, Alraiyes AH, Shojaee S. A systematic approach to the management of massive hemoptysis. J Thorac Dis. (2017) 9(Suppl. 10):S1069–86. doi: 10.21037/jtd.2017.06.41
14. Panda A, Bhalla AS, Goyal A. Bronchial artery embolization in hemoptysis: a systematic review. Diagn Interv Radiol. (2017) 23:307–17. doi: 10.5152/dir.2017.16454
15. Fortin M, Turcotte R, Gleeton O, Bussières JS. Catheter-induced pulmonary artery rupture: using occlusion balloon to avoid lung isolation. J Cardiothorac Vasc Anesth. (2006) 20:376–8. doi: 10.1053/j.jvca.2006.02.008
Keywords: lung contusion, pulmonary contusion, blush, chest trauma, contrast enhanced computed tomography, blunt trauma
Citation: Tominaga N, Hayakawa M and Yokobori S (2022) Blush in Lung Contusions Is Not Rare and Has a High Risk of Mortality in Patients With Blunt Chest Trauma. Front. Med. 9:858511. doi: 10.3389/fmed.2022.858511
Received: 20 January 2022; Accepted: 18 May 2022;
Published: 09 June 2022.
Edited by:
Philipp Störmann, University Hospital Frankfurt, GermanyReviewed by:
Cora Rebecca Schindler, University Hospital Frankfurt, GermanyKlemens Horst, University Hospital RWTH Aachen, Germany
Copyright © 2022 Tominaga, Hayakawa and Yokobori. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mineji Hayakawa, bWluZWppQGRyZWFtLmNvbQ==
 Naoki Tominaga
Naoki Tominaga Mineji Hayakawa2*
Mineji Hayakawa2* Shoji Yokobori
Shoji Yokobori