
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
REVIEW article
Front. Med. , 30 March 2022
Sec. Healthcare Professions Education
Volume 9 - 2022 | https://doi.org/10.3389/fmed.2022.855403
This article is part of the Research Topic Insights in Healthcare Professions Education: 2021 View all 14 articles
Virtual simulation (VS) as an emerging interactive pedagogical strategy has been paid more and more attentions in the undergraduate medical education. Because of the fast development of modern computer simulation technologies, more and more advanced and emerging VS-based instructional practices are constantly increasing to promote medical education in diverse forms. In order to describe an overview of the current trends in VS-based medical teaching and learning, this scoping review presented a worldwide analysis of 92 recently published articles of VS in the undergraduate medical teaching and learning. The results indicated that 98% of included articles were from Europe, North America, and Asia, suggesting a possible inequity in digital medical education. Half (52%) studies reported the immersive virtual reality (VR) application. Evidence for educational effectiveness of VS in medical students’ knowledge or skills was sufficient as per Kirkpatrick’s model of outcome evaluation. Recently, VS has been widely integrated in surgical procedural training, emergency and pediatric emergency medicine training, teaching of basic medical sciences, medical radiation and imaging, puncture or catheterization training, interprofessional medical education, and other case-based learning experiences. Some challenges, such as accessibility of VS instructional resources, lack of infrastructure, “decoupling” users from reality, as well as how to increase students’ motivation and engagement, should be addressed.
As a positive, safe, and valid reality-based educational approach complementing the traditional teaching methods, simulation is increasingly used in the healthcare areas. Especially in the field of undergraduate education as the cornerstone and starting point of training medical professionals, an extensive body of published studies (1–5) have demonstrated that, when the learners act as they would respond under an environment that they believe to be real, simulation-based learning (SBL) experiences are helpful in integrating theoretical knowledge with practice, and gaining skills necessary for independent practice. As defined as “a dynamic process involving the creation of a hypothetical opportunity that incorporates an authentic representation of reality, facilitates active student engagement, and integrates the complexities of practical and theoretical learning with opportunity for repetition, feedback, evaluation, and reflection” (6), simulation used in undergraduate medical education often utilizes goal-based role-plays in the replicated clinical problematic scenarios or case settings in an interactive manner (1–5). Compared with real clinical learning experiences, SBL may be more efficient because the learners intentionally practice skills and higher order thinking. The use of SBL can expose medical students in ethically safe environments without risk of jeopardizing real patients/animals, let them feel safe to make mistakes, and can enhance their confidence while also developing professional knowledge, critical thinking skills, comprehensive decision-making skills, clinical judgment, better clinical preparation, as well as self-efficacy, satisfaction and emotions. Moreover, SBL as a form of education offers repeated practice opportunities especially for less common conditions, and reduces the time consuming to reach professional and clinical competence (1–5). Some previous systematic reviews (4, 7, 8) have shown that medical SBL is effective for the acquisition of clinical skills and contributes to better care of patients. SBL in clinical training such as the use of high-fidelity mannequins, partial task simulators, animal materials or standardized patients, etc. prepares future physicians with communication skills, physical diagnosis, medical interviewing, basic clinical procedures and basic surgical skills in safe and repeated manners, as well as without legal and ethical limits. In pre-clinical undergraduate medical education, the use of SBL serves to reinforce biomedical concepts and other professional knowledge via immediate feedback, and introduces low-risk clinical experiential learning amidst a shortage of qualified clinical preceptorships (1). Especially in a resource limited setting, SBL acts as a cost-effective, easily accessible, safe, feasible and promising educational tool that provides more opportunities for medical students to interact with “patients”/“animals” and engage in team work (3, 5). However, multiple factors including the shortages of funding and simulator technologies, the low supply of simulators, the lack of full-time trained staff, the poor motivation and experience limitations of instructors, the time intensive characteristic, etc. have been considered to have negative effects on effective implementation of current simulation-based undergraduate medical education (2, 9, 10).
Driven by the advanced innovations of modern computer and Internet technologies as well as the recent evolution of the medical profession and its teaching dynamics, SBL has conspicuously shifted to virtual platforms, on which simulation-based e-learning is accessible via a Web browser, and an upgraded SBL strategy named as virtual simulation (VS) has been produced (11, 12). VS is defined as “a screen-based simulation where the graphics, sound, and navigation emphasize the three-dimensional (3D) nature of the environment” (13). The boundaries between the term VS and other technologies such as virtual reality (VR), augmented reality (AR), and virtual standardized patient (VSP), etc. are difficult to define and these terms have been interchangeably used in academic research (13).
During the world wars, VS was initially used in the military area as an aviation training strategy based on a flight simulator. Subsequently, this innovative teaching and learning technological strategy was gainfully applied to more and more technical and workplace training interventions in equipment design, firefighting, law enforcement, lathe operation, vehicle prototyping, crane driving, automotive spray painting, hazard detection, and forestry equipment operation, etc. (9, 12). Sufficient practical learning opportunities are critical for the training of future physicians. However, it is paradoxical that the clinical instructional resources and opportunities for practice are often limited within a university setting due to a large number of undergraduate medical students and finite resources. The positive outcomes of VS in occupational practical training led to its use in undergraduate medical education. Through the re-creation of realistic clinical situations depicted on a computer screen, VS applied in medical teaching based on virtual patients/animals and AR simulations can create an immersive, interactive and risk-free environment for learning practical activities and procedures, thus provide the learners with multiple training possibilities for clinical practices (9, 13). So far, a global interest in VS-based medical teaching programs has been stimulated, and the use of VR, artificial intelligence, machine learning technologies and computer-based serious games is increasingly incorporated into undergraduate medical education practice.
However, because of the fast development of modern computer simulation technologies, more and more advanced and emerging VS teaching instruments, ideas, solutions and practical programs are installed to promote medical education in diverse forms. In order to describe an overview of the current trends in VS-based medical teaching and learning, we here review reports on the practice of using VS tools in medical education at the undergraduate level as documented in recently published literature.
In this study, we performed a bibliographic search on the electronic database MEDLINE via PubMed using key words “virtual simulation (VS) OR e-simulation OR computer simulation OR virtual reality (VR) AND medical education OR medical students”. Only peer-reviewed articles written in English involving undergraduate medical students and fully published online in recent 2 years (between January 2020 and December 2021) were included. The reviews, technical reports or study protocols without the practical outcomes were excluded. Full-texts of articles were obtained, screened, and underwent quality appraisal independently by two researchers then a consensus reached for included papers. Narrative data were extracted from each included article and downloaded into Excel using the categories listed in Supplementary Tables 1, 2. Data were thematically analyzed. Based the fact that the included studies are pitching at varied levels of outcome measurement, in order to evaluate the outcomes of VS practices, the Kirkpatrick evaluation model (14) was adopted in the present review to aid to segregate, analyze and present the findings of the included articles. Two independent researchers reviewed and grouped data within four levels of the Kirkpatrick model, which are as follow (14): Assessment of learners’ views/satisfaction (Level 1); Change in learners’ views or attitudes (Level 2a); Change in learners’ knowledge or skills (Level 2b); Change in learners’ behavior/practice (Level 3); Change in organizational practice (Level 4a); Change in benefit to patients/health outcome (Level 4b).
We identified a total of 92 articles reporting the application practice of VS in the undergraduate medical teaching and learning published since 2020 through our search strategy. In Supplementary Tables 1, 2, we summarized the study characteristics and main findings of these previous studies in detail. By and large, the annual numbers of related articles published during 2020 and 2021 were evenly split.
From the 92 published studies, VS was reported to be applied in the educational practice involving undergraduate medical students across 25 countries including the United States [26 studies (15–40)], the United Kingdom [9 studies (41–49)], Germany [7 studies (50–56)], China [6 studies (10, 57–61)], Denmark [6 studies (62–67)], France [4 studies (68–71)], Japan [4 studies (72–75)], Sweden [3 studies (76–78)], Canada [3 studies (79–81)], Netherlands [3 studies (82–84)], Spain [3 studies (85–87)], Australia [2 studies (88, 89)], Singapore [2 studies (90, 91)], Korea [2 studies (92, 93)], Finland [1 study (94)], Italy [1 study (95)], Ireland [1 study (96)], Colombia [1 study (97)], Pakistan [1 study (98)], Thailand [1 study (99)], Iran [1 study (100)], Poland [1 study (101)], Mexico [1 study (102)], Norway [1 study (103)], Saudi Arabia [1 study (104)], and Switzerland [1 study (105)]. The distribution of included studies among different continents was shown in Figure 1. Results showed that nearly half of studies (45%) were from Europe; one third (33%) from North America; 20% from Asia, while none was from Africa.
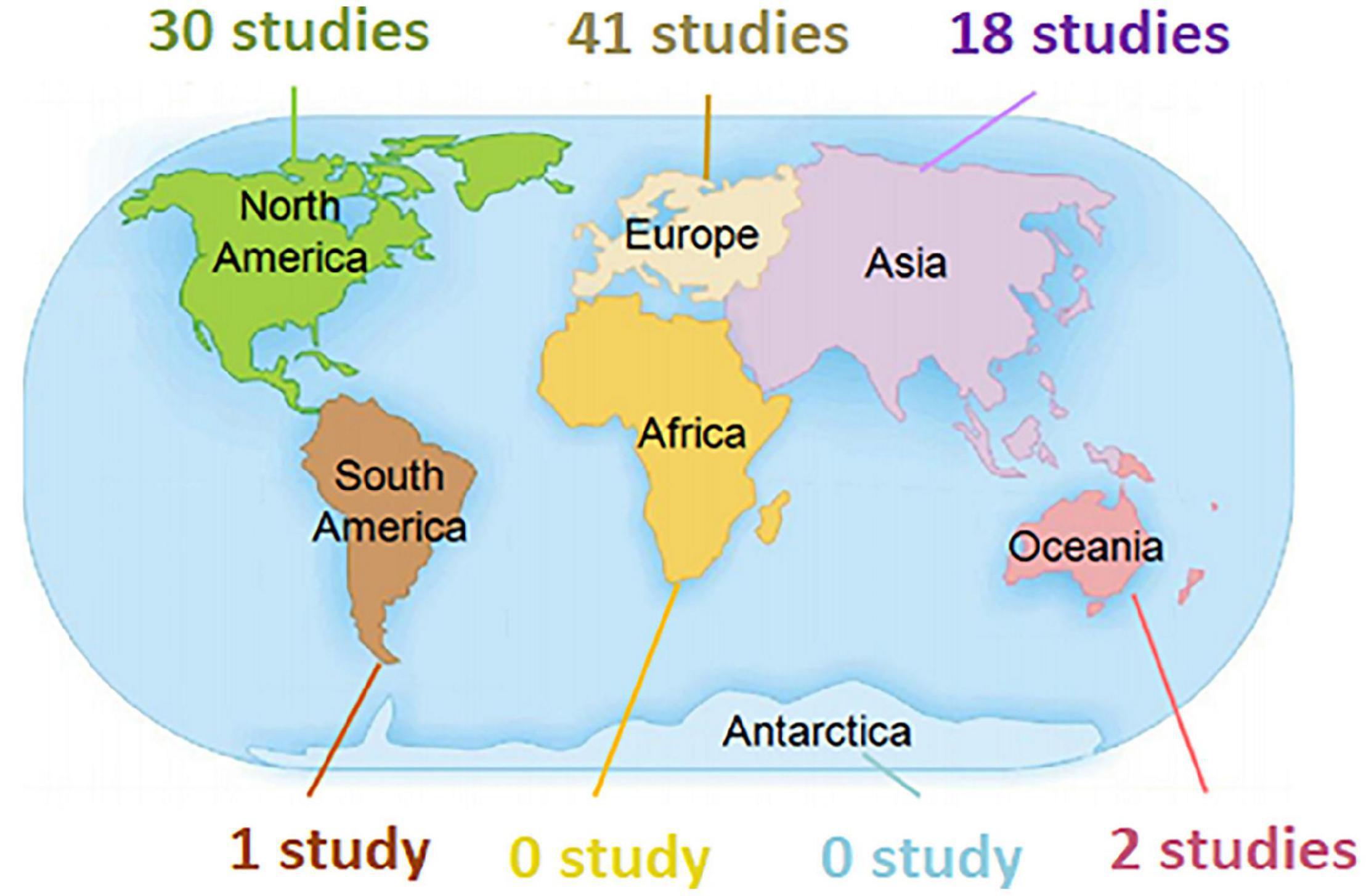
Figure 1. Graph showing the distribution of included studies reporting the use of VS in undergraduate medical education among different continents.
Despite the diversification of virtual simulators/platforms/systems used in undergraduate medical education, we found that 48 (52%) studies (18, 22, 23, 27–31, 33–35, 37–39, 42, 44–48, 50, 52, 54, 57–67, 71, 72, 75, 78, 81–84, 93, 96, 99, 101, 103, 105) reported the immersive VR application, which is characterized by the use of VR equipment consisting of head-mounted displays (headsets or goggles) and/or hand controllers. This finding suggested that VR might be a typical and popular representative of modern VS technology used in medical education. Moreover, only one third of (31) articles (15, 16, 22, 26, 31–33, 38, 47, 48, 52, 53, 56, 58, 60–62, 64, 65, 67, 71, 73, 75, 76, 78–80, 95, 96, 101, 105) included in this review were based on the commercially available or free VS softwares/platforms, the rest used the self-developed ones.
All the included studies involved the outcome evaluation that can be mapped to Kirkpatrick’s four-level model. Using the Kirkpatrick’s evaluation model to structure the analysis of evidence from these studies, a lens was afforded for integrating the findings to identify that a vast majority of included studies (67 studies; 73%) evaluated at Level 2b of the Kirkpatrick’s model, included the changes in learners’ knowledge or skills. In addition, 23 studies included the Kirkpatrick Level 1 evaluation of learner satisfaction, and two studies reported the changes in learners’ views or attitudes (Level 2a). No study met the Level 3 (practice change) and Level 4 (health outcome) of Kirkpatrick’s model.
These findings suggested that evidence for educational effectiveness of VS in medical students’ knowledge or skills was sufficient. There was no study particularly presenting the students’ performance change in clinical practice or the possible benefit to patient/health outcome. More pedagogical research might be merited to inform effective evaluation of the effect of VS used in undergraduate medical education on learners’ behavior/practice as well as its clinical effectiveness.
In spite of the varied study purposes of included articles, these previous attempts at least open up possibility and suggest potential for VS application in undergraduate medical education. Based on the studies included for review, we summarized that, in the recent 2 years, VS has been integrated in the following learning contexts and practical aspects of undergraduate medical education (Figure 2).
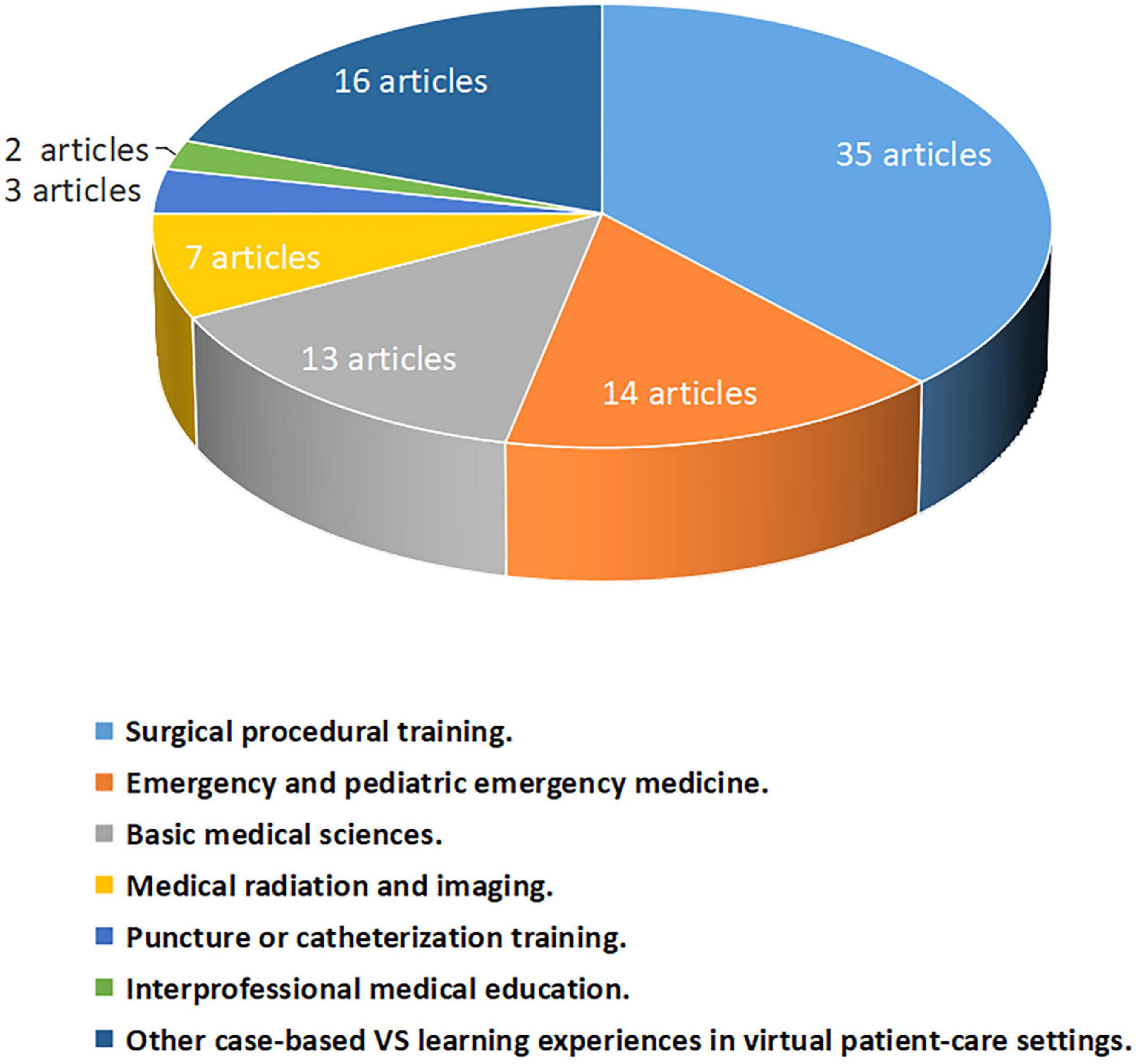
Figure 2. Graph showing the distribution of 92 articles included in this review among learning contexts and practical aspects of undergraduate medical education.
Of the included 92 papers, 38% (35 paper) reported the integration of VS in surgical training for medical undergraduates, among which 12 studies focused on the instructional application of virtual endoscopic [including laparoscopic (31, 36, 37, 56, 73, 76, 78, 98), arthroscopic (26, 47, 48), and otoscopic (53)] simulators; 7 studies were for learning procedures or concepts of orthopedic and bone surgery (32, 33, 35, 45, 57, 66, 70); 5 studies were based on VS system or platform as a primary mode of teaching neurosurgical procedures, neuroanatomy and pathologies (22, 28, 71, 80, 81); 4 papers (38, 61, 75, 84) reported the exposure of medical undergraduates as novice surgeons to the robotic surgery simulators; 2 studies conducted by the same team (64, 65) explored the VR simulation-based training in Cochlear Implant surgery; the other 2 were for learning basic motor skills in liver surgery (50, 52); 1 in minimally invasive surgery (97), and 1 in vitreoretinal surgery (67). In addition, Fukuta et al. (46) generated a virtual operating theater orientation to improve knowledge and confidence of medical undergraduates. Except five validation studies of virtual simulators (26, 47, 53, 65, 81) in which the undergraduates acted as the novice group for comparison with the skilled group, the findings of all the other included studies positively supported the usability and its feasibility of integrating VS in surgical training.
As one of crucial links in medical education, competence-based training of surgical skills is important from the undergraduate phase. Sufficient and high-quality training, deliberate practice, as well as mastery of surgical techniques and instruments are imperative for future surgeons. However, the high risks of injury, the slow learning curves, as well as the limited opportunities to practice, etc. are challenging the modern surgical training. Compared with the traditional master-apprentice surgical education, VS-integrated surgical training can provide desirable alternative allowing an active, independent, repeated and safe learning for students to become familiar with procedures, instruments, and equipment before performing surgeries on patients. In particular, VS-based learning has been found to be conducive to the development of complex psychomotor skills, such as hand-eye coordination that endoscopic and robotic surgery sets particular demands on (64, 65, 97). A recently published article conducted by Petersen et al. (67) found no positive skill transfer from basic skills pre-training in a VR vitreoretinal simulator to the procedure-specific modules, suggesting that, compared than spending valuable training time on basic skills VS pre-training, proceeding directly to VS-based training of procedures was more meaningful for learners.
The second focus of VS-integrated learning contexts in undergraduate medical education was emergency and pediatric emergency medicine training, with 14 articles (10, 16–18, 29, 30, 34, 39, 51, 55, 68, 79, 93, 101) published recently. Among them, eight studies (10, 16–18, 30, 34, 39, 68) used VS-based teaching in pediatric emergencies. The VS simulators used in these studies were mainly based on virtual patient cases, and simulated the clinical critical events.
Emergencies especially pediatric and neonatal emergencies are relatively rare, but potentially catastrophic. However, the life-saving emergency management skills are difficult to master, and accordingly used uncommonly enough to make skill acquisition a challenge (18). In order to provide a safe environment for unlimited exposure to rare clinical events and training in high-risk procedures, SBL has long been considered as a cornerstone of emergency medicine training (16).Unfortunately, as a frequent approach to traditional SBL, standardized patients for emergencies especially for pediatric emergencies are not on option. Many available mannequin-type patient simulators cannot fully display the realistic conditions for training and assessment of competency, as well as critical physical examination findings, such as work of breathing and mental status, in clinical emergency events (30). The above studies showed the integration of VS in emergency medicine training provided promising zero-risk training for undergraduates. In particular, seven studies (18, 29, 30, 34, 39, 93, 101) used the VR simulation systems consisting of VR headsets or goggles to realistically and immersively replicate clinical settings and findings, allowing students to deliberately practice and receive vivid feedback on their assessment.
As the foundation of medical practice, basic or pre-clinical sciences are considered as the “core component” for clinical education. The active and efficient learning experiences in pre-clinical years for in-depth mastery of the basic medical knowledge shape up clinically competent and scientifically grounded physicians (106). Modern pre-clinical curricula lay emphasis on practical-oriented, laboratory-based hands-on training. However, most basic medical curricula are highly information-intensive. Especially facing the reduction of contact hours and limited resources, the use of VS in teaching of basic medical sciences has been paid more and more attentions (106).
We found that, since 2020, there were 13 articles reporting the application of VS for teaching basic medical sciences, including anatomy (23, 42, 44, 49, 59, 60, 69, 72, 82, 104), physiology (92, 94) and pharmacology (19). Obviously, VS-enhanced anatomy training is a focused program as a powerful supplement in conventional anatomy teaching settings. Traditional methods for understanding anatomy include lectures, textbooks, cadaveric dissection, the viewing of prosections, illustrations, photographs, physical models, etc. (42). However, the teaching efficiency may be lacking because of traditional 2D images, as well as limited and expensive cadaver or mannequin resources. As the revolution of anatomy education through digital media, VS has been demonstrated to provide vivid and dynamic imagery that the students can interact with an active learning experience without having to study in an anatomy laboratory (23, 42, 44, 49, 59, 60, 69, 72, 82, 104). Especially for some topics that are challenging to teach because of complex 3D nature, VS-integrated teaching facilitated the 3D spatial perception of anatomy, and helped the students learn more efficiently. Among the included 10 articles reporting VS application in anatomy education, 6 (42, 49, 59, 60, 72, 104) used virtual simulators to help students see the details of muscle and bones; 1 (44) for neuro-anatomy; 1 (23) for cerebrovascular anatomy; and 1 (69) for prostate. The other study conducted by Bogomolova et al. (82) developed a virtual 3D assessment scenario for undergraduate anatomical education. Similarly, the other reports about teaching practices on the use of VS in the pre-clinical phase were in the fields of neurophysiology (94), cardiac physiology (92) and psychopharmacology (19), respectively.
Medical radiation and imaging data such as CT, MRI, and ultrasound are indispensable for the clinical diagnosis. Undergraduate medical education is responsible for pedagogical preparation of medical radiation practitioners. However, being limited by radiation safety reasons, the exposure of medical undergraduates to clinical imaging teaching materials is generally insufficient (88, 96). With the technological development of digital radiographic reconstruction with geometric as well as density characteristic accuracy (107), more and more VS computer software programs have been designed and used in undergraduate medical education, allowing students gain more hands-on experience and develop their clinical skills without worrying about exposing to any unnecessary radiation. In the recent 2 years, we found five studies (20, 85, 86, 88, 96) used VS serious games or systems simulating a radiologist’s practice in the real world among medical undergraduates for radiology learning. The results collectively showed that, for medical undergraduates, the integration of VS as a valuable learning resource had the potential to improve preparation for the clinical environment and increase student confidence (20, 85, 86, 88, 96).
The other two studies (58, 62) demonstrated the effectiveness of VR learning integrated in ultrasonography training for improving students’ ultrasound skills, and students reported they wanted more VS learning. As the VR educational tool is not as space demanding or as expensive as ultrasound simulators, it could be appealing for medical schools with limited resources for basic ultrasound training (62).
Mastering the skill and procedures of puncture or catheterization is essential across many medical specialties. However, as an invasive operation that may cause patients discomfort and have the risk of complications, puncture or catheterization has been considered as a challenge for medical training (63, 99). In the recent 2 years, three published articles reported the application of VR in VS training among medical undergraduates for lumbar puncture (25), ultrasound-guided peripheral venous catheter placement (63), and endotracheal intubation (99), respectively. The results collectively suggested that, as a teaching method well-received by students, VS training can engage learners, develop their practical competencies and proficiency in performing procedures under safe and controlled environments, facilitate spatial recognition and anatomic visualization, thus enhance medical education and skills training (25, 63, 99).
As a critical component of modern patient-centered healthcare practices, the interprofessional team–based model of care in which multiple healthcare professionals including physicians, nurses and pharmacists, etc. work together has been associated with enhanced patient satisfaction and better quality in patient care (108, 109). It has been well-accepted that interprofessional team training should commence at the undergraduate level and continue into clinical practice (91). Simulation-based experiential learning methods represented by role-play have been widely used in undergraduate medical education, and proven to be effective for interprofessional team training (91, 108, 109). Nevertheless, traditional simulation-based interprofessional education in undergraduate stage is confronted with challenges, such as difficulties in getting together different professions of healthcare students as well as the lack of simulation facilities and interprofessional facilitators (90, 91). Importantly, based on its multi-user feature, VS offers an opportunity for healthcare undergraduates from different professions and different institutions to efficiently participate in interprofessional education. In 2020, Liaw et al. (91) reported an integration of computer-based VR into interprofessional team training curriculum among undergraduate medical and nursing students. No difference between virtual and live simulations was found in terms of students’ attitudes toward teamwork and communication skill performances, suggesting the potential use of VR to substitute conventional simulation training in interprofessional education. Subsequently, under the background of COVID-19 pandemic, the same study team applied the Internet-based 3D virtual world mimicking the real hospital environment for VS-integrated interprofessional training, and geographically dispersed undergraduate students from six different healthcare professions (medicine, nursing, pharmacy, occupational therapy, physiotherapy, and medical social work) experienced this VS-based learning using their own avatar roles (90). Results also showed that this immersive and realistic VS tool offered opportunity for high-quality interprofessional medical education delivery.
In addition to the above learning contexts and practical aspects, the remaining 18 articles (15, 21, 24, 27, 40, 41, 43, 54, 73, 77, 83, 87, 89, 95, 100, 102, 103, 105) reported the integration of VS into other case-based learning experiences in virtual patient-care settings. Despite the diversity of virtual patient systems and clinical scenarios, these studies generally showed that VS-integrated case-based learning as a feasible teaching approach (54) could result in students’ learning gains, retention of information, and transfer of knowledge to clinical application (89, 95, 100, 102), help future physicians improve diagnostic accuracy thus enhance the clinical reasoning teaching (15, 27, 43), extend students’ preparedness level for their future clinical experiences (40, 83), facilitate empathy (24), cultural competence (77) and comprehensive clinical skills such as communication-based skills (21), clinical decision-making skills (78) within undergraduate medical education, and improve students’ confidence in managing clinical scenarios (41), thus was highly received by students (89, 95, 105).
Especially during the COVID-19 pandemic, this pedagogical modality avoided training interruption and was highly valued (41, 87, 95, 105). Due to risk of COVID-19 exposure and required social distancing, the students’ clinical placements, face-to-face teaching and practical/lab sessions have all been limited even canceled in the pandemic situations, and a sudden and complete disruption in medical education has occurred (15, 16, 106, 110). The restrictions due to COVID-19 raise the need for innovative medical VS teaching methods, which provide educational contents in a learning environment where lecturers and students separated by space or time or both (41). However, the sudden outbreak of COVID-19 poses the difficulties in altering medical training modality during an extremely short period of time. In this situation, VS-based learning that has been widely adopted in medical schools is considered as a prompt turning point in medical education to overcome the educational gap due to COVID-19 (16, 17, 41, 79, 111). Through the application of VS, it is potential to digitally reconstruct the clinical environment, simulate the clinical learning and ensure the continuation of practical examinations, in spite of widely dispersed student or faculty placements (112). After outbreak of COVID-19, De Ponti et al. (95) conducted a questionnaire-based survey among 115 pre-graduated medical students, and showed that 97 students (84%) considered the future use of VS training useful in addition to the traditional apprenticeship at patient’s bedside, suggesting medical students’ appreciation for the application of VS in post-pandemic medical education. The integration of emergent technology represented by VS into medical curriculum has been considered as an indispensable component of the transformative change and post-COVID undergraduate medical education to keep the medical education on stream (106). Especially in the face of the current ongoing COVID-19 crisis, VS could act as a flexible teaching and learning modality in response to further pandemic waves.
In addition, the students’ performance on learning tasks can be well-assessed using VSPs (21), or a computer-based case simulation objective structured clinical examination (OSCE) (87). However, a study (103) compared a fully immersive, interactive, multiplayer VR application in the group self-practice of systematic clinical observation using the airway, breathing, circulation, disability and exposure (ABCDE) approach to the physical equipment, and the results showed that group self-practice of the ABCDE approach in VR application was non-inferior to practice with physical equipment. Therefore, further practice and research on the integration of different virtual patient VS systems in case-based learning experiences under various clinical scenarios might be required to identify the role of VS in undergraduate medical education.
This study reviewed the recent practice of VS in the undergraduate medical teaching and learning reporting in 92 articles since 2020. Evidence for educational effectiveness of VS in medical students’ knowledge or skills was sufficient as per Kirkpatrick’s model of outcome evaluation. We found that VS was applied in the educational practice involving undergraduate medical students across 25 countries. However, an overwhelming majority of (97%) involved studies were form Europe, North America, and Asia. This regional bias might be due to the uneven distribution of digital medical education resources across the world, which would influence the local medical students’ access to education in underdeveloped areas. However, the highly shareable feature of digital resources has been considered to provide an opportunity to address the need for a fair learning system for medical students and promote equity in medical education globally (113, 114). Even in resource limited settings, the application of VS educational systems/platforms could help to promote medical learning by reducing instructor costs and laboratory materials. Along with the advancement and expansion of computer technology, VS has been believed as a less expensive and more accessible alternative for undergraduate medical education, allowing for its wide application in low-and-middle-income countries (85, 115). So far, increased availability and affordability of technology-based commercial platforms, such as Google, Apple, and Microsoft, allow any medical educational institution to share VS resources, or engage in research and development of VS projects to improve their efficiencies within curricula. For example, as an international virtual community with more than 1,500 million square meters allowing tens of thousands of users connected at the same time around the world, Second Life1 created by Linden Laboratories in 2003 has become the most active virtual world in higher education. Currently, hundreds of universities around the world have used it to support teaching and learning activities. As an educational tool, Second Life has been dedicated to the training of medical undergraduate students in areas such as radiology (85, 116) and anatomy (86, 115, 117). Therefore, once being promoted to more medical schools around the world, VS learning produces based on platforms such as Second Life will help promote greater equity in global medical education. Similarly, the University of Southern California, United States, developed a freeware virtual patient community, the University of Southern California Standard Patient Studio platform, with funding from the Department of Defense. This platform allows for the creation of personalized VSP software for different teaching and learning purposes, and has been shared by other US medical schools (19). In addition, a company (Oxford Medical Simulation) is offering a VR medical education platform where undergraduate students can take medical histories, examine, diagnose and treat digitally simulated patients within a virtual clinical environment (118). Nowadays, Human Patient Simulators and Virtual Reality Laparoscopic Trainers have been well-developed by manufacturers and are available on the market (120, 121). Therefore, professional teaching materials that were previously limited to certain settings or world-renowned medical schools are now being released on VS-based platforms that can be employed by any user across institutions, areas and countries (122). In China, a profile file-sharing website named the National Virtual Simulation Experiment Teaching Project Sharing Platform2 is readily available with minimal setup and free access, in which the abundant medical VS teaching resources contribute greatly to the nationwide equity in undergraduate medical education. To date (1 October 2021), the VS teaching resources in the areas of pre-clinical and clinical medicine have been visited near 350,000 times. If the language barrier can be overcome, these VS medical teaching materials may be shared by more medical schools around the world.
Lack of infrastructure such as computer hardware and network has been considered as one of major challenges to establishing VS-integrated curricula (90). It has been found that computer self-efficacy might affect the learners’ willingness to adopt the VS as part of learning (90). For remote VS experiences, the Internet connection bandwidth could impact the learning experience, and contribute to the technical issues (90). Here, we found the immersive VR approach is the currently popular VS tool used in undergraduate medical education, the application of which was reported in half (52%) involved studies. However, the cost and the provision of satisfactory VR equipment such as head-mounted displays and hand controllers might limit final implementation of VR-integrated educational practice in low- and middle income countries. Some studies (75, 105) showed that, during the VR-simulation, “visually-induced motion sickness” shown as nausea, headache, blurred vision, and dizziness might cause a disturbing impact on some learners at the physical level. Moreover, because the headsets and other VR equipment are used communally among undergraduate medical students, it should be necessary to disinfect the VR simulation tools for public use between uses, especially during the COVID-19 pandemic (105). In addition, we found only one third of involved studies used the commercially available or free-accessible VS softwares/platforms for the undergraduate medical teaching and learning. Actually, designing and developing new VS instructional simulators or creating VS educational scenarios require significant inputs of time, funds and effort for educators. Currently, due to the excessive rapid change of VS technology, there are no standardized or well described VS design approaches (13). Continued back-and-forth collaboration among educators, clinicians and engineers in design and development teams is critical to advancing the establishment and implementation of VS-integrated undergraduate medical training (57). It had been estimated that at least 1 year need to be spent to achieve an acceptable VR simulator for medical undergraduates (57). These barriers might provide incentive for educators to centralize VS medical educational resources. However, only through increasing availability and awareness of developed VS instructional tools among larger audiences, individual costs can be shared and the above barriers will be minimized. If possible, freely sharing online VS educational resources may help equalize global medical education.
Recently, VS has been widely integrated in various learning contexts and practical aspects of undergraduate medical education, including surgical procedural training, emergency and pediatric emergency medicine training, teaching of basic medical sciences, medical radiation and imaging, puncture or catheterization training, interprofessional medical education, and other case-based learning experiences. Among them, the most focused field of study is the application of VS tools in training of surgical skills; however, more attempts are needed to apply VS in interprofessional medical education and training of puncture/catheter skills. Generally, VS has been well-accepted as a valuable pedagogical approach for undergraduate medical education. Through providing computer-generated immersive learning scenes being highly realistic, diversified, dynamic and customized, VS used in undergraduate medical education offers an opportunity for students to achieve first-person experiences in life-like and complex clinical scenarios that they may not normally be exposed to, or when it is hard to access patients, and makes learning effective and appealing to students. However, content provided on a screen using a digital device might “decouple” users from reality. Hands-on experience is essential for medical students to master clinical skills, for example, surgical techniques. Several previous studies (18, 123) have suggested that improved performance in the VS environment might not always transfer to the clinical setting. Therefore, VS is insufficient to replace hands-on experiential practice for medical students to master clinical skills, which might be another important challenge. The current VS simulators act as only part of the medical comprehensive training to supplement the hands-on experience but not the only training technique. In addition, an interesting study (86) explored the impact of compulsory participation on the VS learning experiences of medical undergraduates. The results showed that the learning performance and acceptance of VS technology were lower with a compulsory participation, and the opinion toward VS-based study was even worse if dropouts were not allowed. Therefore, learning in VS environments should be voluntary (86). And how to increase students’ motivation and engagement is an important issue for medical educators to achieve the effective integration of VS into undergraduate education.
QW and JW substantially contributed to the conception and the design of the work. All authors have contributed to the interpretation of the data and the drafting of the work, they revised several versions of it and have approved the submitted version.
This work was supported by the Educational Science Planning Project in Hubei province (2019GB019) and the Teaching Research Project in Wuhan University of Science and Technology (2019Z004).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2022.855403/full#supplementary-material
1. Jabaay MJ, Marotta DA, Aita SL, Walker DB, Grcevich LO, Camba V, et al. Medical simulation-based learning outcomes in pre-clinical medical education. Cureus. (2020) 12:e11875. doi: 10.7759/cureus.11875
2. Nara N, Beppu M, Tohda S, Suzuki T. The introduction and effectiveness of simulation-based learning in medical education. Intern Med. (2009) 48:1515–9. doi: 10.2169/internalmedicine.48.2373
3. Najjuma JN, Bajunirwe F, Twine M, Namata T, Kyakwera CK, Cherop M, et al. Stakeholder perceptions about the establishment of medical simulation-based learning at a university in a low resource setting: a qualitative study in Uganda. BMC Med Educ. (2020) 20:379. doi: 10.1186/s12909-020-02301-3
4. Theodoulou I, Nicolaides M, Athanasiou T, Papalois A, Sideris M. Simulation-based learning strategies to teach undergraduate students basic surgical skills: a systematic review. J Surg Educ. (2018) 75:1374–88. doi: 10.1016/j.jsurg.2018.01.013
5. Koh J, Dubrowski A. Merging problem-based learning with simulation-based learning in the medical undergraduate curriculum: the PAIRED framework for enhancing lifelong learning. Cureus. (2016) 8:e647. doi: 10.7759/cureus.647
6. Kaldheim HKA, Bergland Å, Ølnes MA, Hofsø K, Dihle A, Creutzfeldt J, et al. Use of simulation-based learning among perioperative nurses and students: a scoping review. Nurse Educ Today. (2019) 73:31–7. doi: 10.1016/j.nedt.2018.09.013
7. Murphy JG, Cremonini F, Kane GC, Dunn W. Is simulation based medicine training the future of clinical medicine? Eur Rev Med Pharmacol Sci. (2007) 11:1–8.
8. McGaghie WC, Issenberg SB, Cohen ER, Barsuk JH, Wayne DB. Does simulation-based medical education with deliberate practice yield better results than traditional clinical education? A meta-analytic comparative review of the evidence. Acad Med. (2011) 86:706–11. doi: 10.1097/ACM.0b013e318217e119
9. Coyne E, Calleja P, Forster E, Lin F. A review of virtual-simulation for assessing healthcare students’ clinical competency. Nurse Educ Today. (2021) 96:104623. doi: 10.1016/j.nedt.2020.104623
10. Hu L, Zhang L, Yin R, Li Z, Shen J, Tan H, et al. NEOGAMES: a serious computer game that improves long-term knowledge retention of neonatal resuscitation in undergraduate medical students. Front Pediatr. (2021) 9:645776. doi: 10.3389/fped.2021.645776
11. Borg Sapiano A, Sammut R, Trapani J. The effectiveness of virtual simulation in improving student nurses’ knowledge and performance during patient deterioration: a pre and post test design. Nurse Educ Today. (2018) 62:128–33. doi: 10.1016/j.nedt.2017.12.025
12. Tinôco JDS, Enders BC, Sonenberg A, Lira ALBC. Virtual clinical simulation in nursing education: a concept analysis. Int J Nurs Educ Scholarsh. (2021) 18:20200001. doi: 10.1515/ijnes-2020-0001
13. McGrath JL, Taekman JM, Dev P, Danforth DR, Mohan D, Kman N, et al. Using virtual reality simulation environments to assess competence for emergency medicine learners. Acad Emerg Med. (2018) 25:186–95. doi: 10.1111/acem.13308
14. Campbell K, Taylor V, Douglas S. Effectiveness of online cancer education for nurses and allied health professionals; a systematic review using kirkpatrick evaluation framework. J Cancer Educ. (2019) 34:339–56. doi: 10.1007/s13187-017-1308-2
15. Dekhtyar M, Park YS, Kalinyak J, Chudgar SM, Fedoriw KB, Johnson KJ, et al. Use of a structured approach and virtual simulation practice to improve diagnostic reasoning. Diagnosis. (2021) 9:69–76. doi: 10.1515/dx-2020-0160
16. Austin A, Rudolf F, Fernandez J, Ishimine P, Murray M, Suresh P, et al. COVID-19 educational innovation: hybrid in-person and virtual simulation for emergency medicine trainees. AEM Educ Train. (2021) 5:e10593. doi: 10.1002/aet2.10593
17. Yang T, Buck S, Evans L, Auerbach M. A telesimulation elective to provide medical students with pediatric patient care experiences during the COVID pandemic. Pediatr Emerg Care. (2021) 37:119–22. doi: 10.1097/PEC.0000000000002311
18. Putnam EM, Rochlen LR, Alderink E, Augé J, Popov V, Levine R, et al. Virtual reality simulation for critical pediatric airway management training. J Clin Transl Res. (2021) 7:93–9.
19. Rakofsky JJ, Talbot TB, Dunlop BWA. Virtual standardized patient-based assessment tool to evaluate psychiatric residents’ psychopharmacology proficiency. Acad Psychiatry. (2020) 44:693–700. doi: 10.1007/s40596-020-01286-x
20. Shu L, Bahri F, Mostaghni N, Yu G, Javan R. The time has come: a paradigm shift in diagnostic radiology education via simulation training. J Digit Imaging. (2021) 34:212–27. doi: 10.1007/s10278-020-00405-2
21. O’Rourke SR, Branford KR, Brooks TL, Ives LT, Nagendran A, Compton SN. The emotional and behavioral impact of delivering bad news to virtual versus real standardized patients: a pilot study. Teach Learn Med. (2020) 32:139–49. doi: 10.1080/10401334.2019.1652180
22. Greuter L, De Rosa A, Cattin P, Croci DM, Soleman J, Guzman R. Randomized study comparing 3D virtual reality and conventional 2D on-screen teaching of cerebrovascular anatomy. Neurosurg Focus. (2021) 51:E18. doi: 10.3171/2021.5.FOCUS21212
23. Galvez R, Wallon RC, Shackelford L, Amos JR, Rowen JL. Use of virtual reality to educate undergraduate medical students on cardiac peripheral and collateral circulation. Med Sci Educ. (2020) 31:19–22. doi: 10.1007/s40670-020-01104-x
24. Elzie CA, Shaia JA. Pilot study of the impact of virtually embodying a patient with a terminal illness. Med Sci Educ. (2021) 31:665–75. doi: 10.1007/s40670-021-01243-9
25. Roehr M, Wu T, Maykowski P, Munter B, Hoebee S, Daas E, et al. The feasibility of virtual reality and student-led simulation training as methods of lumbar puncture instruction. Med Sci Educ. (2020) 31:117–24. doi: 10.1007/s40670-020-01141-6
26. Bishop ME, Ode GE, Hurwit DJ, Zmugg S, Rauck RC, Nguyen JT, et al. The arthroscopic surgery skill evaluation tool global rating scale is a valid and reliable adjunct measure of performance on a virtual reality simulator for hip arthroscopy. Arthroscopy. (2021) 37:1856–66. doi: 10.1016/j.arthro.2021.01.046
27. Kim B, Loke YH, Mass P, Irwin MR, Capeland C, Olivieri L, et al. Novel virtual reality medical image display system for group discussions of congenital heart disease: development and usability testing. JMIR Cardio. (2020) 4:e20633. doi: 10.2196/20633
28. Atli K, Selman W, Ray AA. Comprehensive multicomponent neurosurgical course with use of virtual reality: modernizing the medical classroom. J Surg Educ. (2021) 78:1350–6. doi: 10.1016/j.jsurg.2020.11.003
29. Lowe J, Peng C, Winstead-Derlega C, Curtis H. 360 virtual reality pediatric mass casualty incident: a cross sectional observational study of triage and out-of-hospital intervention accuracy at a national conference. J Am Coll Emerg Physicians Open. (2020) 1:974–80. doi: 10.1002/emp2.12214
30. Zackoff MW, Young D, Sahay RD, Fei L, Real FJ, Guiot A, et al. Establishing objective measures of clinical competence in undergraduate medical education through immersive virtual reality. Acad Pediatr. (2021) 21:575–9. doi: 10.1016/j.acap.2020.10.010
31. Melnyk R, Campbell T, Holler T, Cameron K, Saba P, Witthaus MW, et al. See like an expert: gaze-augmented training enhances skill acquisition in a virtual reality robotic suturing task. J Endourol. (2021) 35:376–82. doi: 10.1089/end.2020.0445
32. Orland MD, Patetta MJ, Wieser M, Kayupov E, Gonzalez MH. Does virtual reality improve procedural completion and accuracy in an intramedullary tibial nail procedure? a randomized control trial. Clin Orthop Relat Res. (2020) 478:2170–7. doi: 10.1097/CORR.0000000000001362
33. Wang KC, Bernardoni ED, Cotter EJ, Levine BR, Frank RM. The impact of unguided trauma simulation practice on novice performance: a randomized controlled trial. J Am Acad Orthop Surg. (2021) 29:255–62. doi: 10.5435/JAAOS-D-19-00225
34. Zackoff MW, Real FJ, Sahay RD, Fei L, Guiot A, Lehmann C, et al. Impact of an immersive virtual reality curriculum on medical students’ clinical assessment of infants with respiratory distress. Pediatr Crit Care Med. (2020) 21:477–85. doi: 10.1097/PCC.0000000000002249
35. Blumstein G, Zukotynski B, Cevallos N, Ishmael C, Zoller S, Burke Z, et al. Randomized trial of a virtual reality tool to teach surgical technique for tibial shaft fracture intramedullary nailing. J Surg Educ. (2020) 77:969–77. doi: 10.1016/j.jsurg.2020.01.002
36. Fu Y, Cavuoto L, Qi D, Panneerselvam K, Arikatla VS, Enquobahrie A, et al. Characterizing the learning curve of a virtual intracorporeal suturing simulator VBLaST-SS©. Surg Endosc. (2020) 34:3135–44. doi: 10.1007/s00464-019-07081-6
37. Lesch H, Johnson E, Peters J, Cendán JCVR. Simulation leads to enhanced procedural confidence for surgical trainees. J Surg Educ. (2020) 77:213–8. doi: 10.1016/j.jsurg.2019.08.008
38. Gurung PMS, Campbell T, Wang B, Joseph JV, Ghazi AE. Accelerated skills acquisition protocol (ASAP) in optimizing robotic surgical simulation training: a prospective randomized study. World J Urol. (2020) 38:1623–30. doi: 10.1007/s00345-019-02858-9
39. Young D, Real FJ, Sahay RD, Zackoff M. Remote virtual reality teaching: closing an educational gap during a global pandemic. Hosp Pediatr. (2021) 11:e258–62. doi: 10.1542/hpeds.2021-005927
40. Chaffkin J, Ray JM, Goldenberg M, Wong AH. Impact of a virtual simulation-based educational module on managing agitation for medical students. Acad Psychiatry. (2021). [Online ahead of print]. doi: 10.1007/s40596-021-01521-z
41. Morgan G, Melson E, Davitadze M, Ooi E, Zhou D, Hanania T, et al. Utility of Simulation via Instant Messaging - Birmingham Advance (SIMBA) in medical education during COVID-19 pandemic. J R Coll Physicians Edinb. (2021) 51:168–72. doi: 10.4997/JRCPE.2021.218
42. Kolla S, Elgawly M, Gaughan JP, Goldman E. Medical student perception of a virtual reality training module for anatomy education. Med Sci Educ. (2020) 30:1201–10. doi: 10.1007/s40670-020-00993-2
43. Plackett R, Kassianos AP, Timmis J, Sheringham J, Schartau P, Kambouri M. Using virtual patients to explore the clinical reasoning skills of medical students: mixed methods study. J Med Internet Res. (2021) 23:e24723. doi: 10.2196/24723
44. Pickering JD, Panagiotis A, Ntakakis G, Athanassiou A, Babatsikos E, Bamidis PD. Assessing the difference in learning gain between a mixed reality application and drawing screencasts in neuroanatomy. Anat Sci Educ. (2021). [Online ahead of print]. doi: 10.1002/ase.2113
45. Wilson G, Zargaran A, Kokotkin I, Bhaskar J, Zargaran D, Trompeter A. Virtual reality and physical models in undergraduate orthopaedic education: a modified randomised crossover trial. Orthop Res Rev. (2020) 12:97–104. doi: 10.2147/ORR.S252274
46. Fukuta J, Gill N, Rooney R, Coombs A, Murphy D. Use of 360° video for a virtual operating theatre orientation for medical students. J Surg Educ. (2021) 78:391–3. doi: 10.1016/j.jsurg.2020.08.014
47. Mulligan A, Vaghela KR, Jeyaseelan L, Lee J, Akhtar K. Transferable global rating scales in the validation of the ArthroSim™ virtual reality arthroscopy simulator. Surg Technol Int. (2020) 37:306–11.
48. Bartlett JD, Lawrence JE, Yan M, Guevel B, Stewart ME, Audenaert E, et al. The learning curves of a validated virtual reality hip arthroscopy simulator. Arch Orthop Trauma Surg. (2020) 140:761–7. doi: 10.1007/s00402-020-03352-3
49. Lo S, Abaker ASS, Quondamatteo F, Clancy J, Rea P, Marriott M, et al. Use of a virtual 3D anterolateral thigh model in medical education: augmentation and not replacement of traditional teaching? J Plast Reconstr Aesthet Surg. (2020) 73:269–75. doi: 10.1016/j.bjps.2019.09.034
50. Kenngott HG, Pfeiffer M, Preukschas AA, Bettscheider L, Wise PA, Wagner M, et al. IMHOTEP: cross-professional evaluation of a three-dimensional virtual reality system for interactive surgical operation planning, tumor board discussion and immersive training for complex liver surgery in a head-mounted display. Surg Endosc. (2021) 36:126–34. doi: 10.1007/s00464-020-08246-4
51. Middeke A, Anders S, Raupach T, Schuelper N. Transfer of clinical reasoning trained with a serious game to comparable clinical problems: a prospective randomized study. Simul Healthc. (2020) 15:75–81. doi: 10.1097/SIH.0000000000000407
52. Huettl F, Saalfeld P, Hansen C, Preim B, Poplawski A, Kneist W, et al. Virtual reality and 3D printing improve preoperative visualization of 3D liver reconstructions-results from a preclinical comparison of presentation modalities and user’s preference. Ann Transl Med. (2021) 9:1074. doi: 10.21037/atm-21-512
53. Albrecht T, Nikendei C, Praetorius M. Face, content, and construct validity of a virtual reality otoscopy simulator and applicability to medical training. Otolaryngol Head Neck Surg. (2021). [Online ahead of print]. doi: 10.1177/01945998211032897
54. Klemm P, Kleyer A, Tascilar K, Schuster L, Meinderink T, Steiger F, et al. Virtual reality-based app to educate health care professionals and medical students about inflammatory arthritis: feasibility study. JMIR Serious Games. (2021) 9:e23835. doi: 10.2196/23835
55. Issleib M, Kromer A, Pinnschmidt HO, Süss-Havemann C, Kubitz JC. Virtual reality as a teaching method for resuscitation training in undergraduate first year medical students: a randomized controlled trial. Scand J Trauma Resusc Emerg Med. (2021) 29:27. doi: 10.1186/s13049-021-00836-y
56. Huettl F, Huber T, Duwe M, Lang H, Paschold M, Kneist W. Higher quality camera navigation improves the surgeon’s performance: evidence from a pre-clinical study. J Minim Access Surg. (2020) 16:355–9. doi: 10.4103/jmas.JMAS_143_19
57. Mok TN, Chen J, Pan J, Ming WK, He Q, Sin TH, et al. Use of a virtual reality simulator for tendon repair training: randomized controlled trial. JMIR Serious Games. (2021) 9:e27544. doi: 10.2196/27544
58. Hu KC, Salcedo D, Kang YN, Lin CW, Hsu CW, Cheng CY, et al. Impact of virtual reality anatomy training on ultrasound competency development: a randomized controlled trial. PLoS One. (2020) 15:e0242731. doi: 10.1371/journal.pone.0242731
59. Chen S, Zhu J, Cheng C, Pan Z, Liu L, Du J, et al. Can virtual reality improve traditional anatomy education programmes? A mixed-methods study on the use of a 3D skull model. BMC Med Educ. (2020) 20:395. doi: 10.1186/s12909-020-02255-6
60. Du YC, Fan SC, Yang LC. The impact of multi-person virtual reality competitive learning on anatomy education: a randomized controlled study. BMC Med Educ. (2020) 20:343. doi: 10.1186/s12909-020-02155-9
61. Chiu HY, Kang YN, Wang WL, Tong YS, Chang SW, Fong TH, et al. Gender differences in the acquisition of suturing skills with the da Vinci surgical system. J Formos Med Assoc. (2020) 119:462–70. doi: 10.1016/j.jfma.2019.06.013
62. Rosenfeldt Nielsen M, Kristensen EQ, Jensen RO, Mollerup AM, Pfeiffer T, Graumann O. Clinical ultrasound education for medical students: virtual Reality versus e-Learning, a randomized controlled pilot trial. Ultrasound Q. (2021) 37:292–6. doi: 10.1097/RUQ.0000000000000558
63. Andersen NL, Jensen RO, Posth S, Laursen CB, Jørgensen R, Graumann O. Teaching ultrasound-guided peripheral venous catheter placement through immersive virtual reality: an explorative pilot study. Medicine. (2021) 100:e26394. doi: 10.1097/MD.0000000000026394
64. Frendø M, Frithioff A, Konge L, Sørensen MS, Andersen SAW. Cochlear implant surgery: learning curve in virtual reality simulation training and transfer of skills to a 3D-printed temporal bone - A prospective trial. Cochlear Implants Int. (2021) 22:330–7. doi: 10.1080/14670100.2021
65. Frendø M, Frithioff A, Konge L, Foghsgaard S, Mikkelsen PT, Sørensen MS, et al. Assessing competence in cochlear implant surgery using the newly developed cochlear implant surgery assessment tool. Eur Arch Otorhinolaryngol. (2021) 279:127–36. doi: 10.1007/s00405-021-06632-9
66. Andersen SAW, Mikkelsen PT, Sørensen MS. The effect of simulator-integrated tutoring for guidance in virtual reality simulation training. Simul Healthc. (2020) 15:147–53. doi: 10.1097/SIH.0000000000000414
67. Petersen SB, Vestergaard AH, Thomsen ASS, Konge L, Cour M, Grauslund J, et al. Pretraining of basic skills on a virtual reality vitreoretinal simulator: a waste of time. Acta Ophthalmol. (2021). [Online ahead of print]. doi: 10.1111/aos.15039
68. Michelet D, Barre J, Truchot J, Piot MA, Cabon P, Tesniere A. Effect of computer debriefing on acquisition and retention of learning after screen-based simulation of neonatal resuscitation: randomized controlled trial. JMIR Serious Games. (2020) 8:e18633. doi: 10.2196/18633
69. Fiard G, Selmi SY, Maigron M, Bellier A, Promayon E, Descotes JL, et al. validating the transfer of skills acquired on a prostate biopsy simulator: a prospective, randomized, controlled study. J Surg Educ. (2020) 77:953–60. doi: 10.1016/j.jsurg.2020.01.008
70. Bouaoud J, El Beheiry M, Jablon E, Schouman T, Bertolus C, Picard A, et al. a 3D virtual reality platform, improves undergraduate craniofacial trauma education. J Stomatol Oral Maxillofac Surg. (2021) 122:367–71. doi: 10.1016/j.jormas.2020.09.009
71. Ros M, Debien B, Cyteval C, Molinari N, Gatto F, Lonjon N. Applying an immersive tutorial in virtual reality to learning a new technique. Neurochirurgie. (2020) 66:212–8. doi: 10.1016/j.neuchi.2020.05.006
72. Nakai K, Terada S, Takahara A, Hage D, Tubbs RS, Iwanaga J. Anatomy education for medical students in a virtual reality workspace: a pilot study. Clin Anat. (2021) 35:40–4. doi: 10.1002/ca.23783
73. Watari T, Tokuda Y, Owada M, Onigata K. the utility of virtual patient simulations for clinical reasoning education. Int J Environ Res Public Health. (2020) 17:5325. doi: 10.3390/ijerph17155325
74. Wada Y, Nishi M, Yoshikawa K, Higashijima J, Miyatani T, Tokunaga T, et al. Usefulness of virtual three-dimensional image analysis in inguinal hernia as an educational tool. Surg Endosc. (2020) 34:1923–8. doi: 10.1007/s00464-019-06964-y
75. Takata R, Kanehira M, Kato Y, Matsuura T, Kato R, Maekawa S, et al. Improvement of three-dimensional motion sickness using a virtual reality simulator for robot-assisted surgery in undergraduate medical students: a prospective observational study. BMC Med Educ. (2021) 21:498. doi: 10.1186/s12909-021-02872-9
76. Oussi N, Renman P, Georgiou K, Enochsson L. Baseline characteristics in laparoscopic simulator performance: the impact of personal computer (PC)-gaming experience and visuospatial ability. Surg Open Sci. (2020) 4:19–25. doi: 10.1016/j.sopen.2020.06.002
77. Rothlind E, Fors U, Salminen H, Wändell P, Ekblad S. Virtual patients reflecting the clinical reality of primary care - a useful tool to improve cultural competence. BMC Med Educ. (2021) 21:270. doi: 10.1186/s12909-021-02701-z
78. Oussi N, Enochsson L, Henningsohn L, Castegren M, Georgiou E, Kjellin A. Trainee performance after laparoscopic simulator training using a Blackbox versus LapMentor. J Surg Res. (2020) 250:1–11. doi: 10.1016/j.jss.2019.12.039
79. Foohey S, Nagji A, Yilmaz Y, Sibbald M, Monteiro S, Chan TM. Developing the virtual resus room: fidelity, usability, acceptability, and applicability of a virtual simulation for teaching and learning. Acad Med. (2021). [Online ahead of print]. doi: 10.1097/ACM.0000000000004364
80. Mirchi N, Bissonnette V, Yilmaz R, Ledwos N, Winkler-Schwartz A, Del Maestro RF. The virtual operative assistant: an explainable artificial intelligence tool for simulation-based training in surgery and medicine. PLoS One. (2020) 15:e0229596. doi: 10.1371/journal.pone.0229596
81. Siyar S, Azarnoush H, Rashidi S, Del Maestro RF. Tremor assessment during virtual reality brain tumor resection. J Surg Educ. (2020) 77:643–51. doi: 10.1016/j.jsurg.2019.11.011
82. Bogomolova K, Sam AH, Misky AT, Gupte CM, Strutton PH, Hurkxkens TJ, et al. Development of a virtual three-dimensional assessment scenario for anatomical education. Anat Sci Educ. (2021) 14:385–93. doi: 10.1002/ase.2055
83. Arents V, de Groot PCM, Struben VMD, van Stralen KJ. Use of 360° virtual reality video in medical obstetrical education: a quasi-experimental design. BMC Med Educ. (2021) 21:202. doi: 10.1186/s12909-021-02628-5
84. Beulens AJW, Hashish YAF, Brinkman WM, Umari P, Puliatti S, Koldewijn EL, et al. Training novice robot surgeons: proctoring provides same results as simulator-generated guidance. J Robot Surg. (2021) 15:397–428. doi: 10.1007/s11701-020-01118-y
85. Rudolphi-Solero T, Jimenez-Zayas A, Lorenzo-Alvarez R, Domínguez-Pinos D, Ruiz-Gomez MJ, Sendra-Portero FA. team-based competition for undergraduate medical students to learn radiology within the virtual world Second Life. Insights Imaging. (2021) 12:89. doi: 10.1186/s13244-021-01032-3
86. Rudolphi-Solero T, Lorenzo-Alvarez R, Ruiz-Gomez MJ, Sendra-Portero F. Impact of compulsory participation of medical students in a multiuser online game to learn radiological anatomy and signs within the virtual world Second Life. Anat Sci Educ. (2021). [Online ahead of print]. doi: 10.1002/ase.2134
87. García-Seoane JJ, Ramos-Rincón JM, Lara-Muñoz JP. CCS-OSCE working group of the CNDFME. Changes in the Objective Structured Clinical Examination (OSCE) of University Schools of Medicine during COVID-19. Experience with a computer-based case simulation OSCE (CCS-OSCE). Rev Clin Esp. (2021) 221:456–63. doi: 10.1016/j.rceng.2021.01.006
88. Gunn T, Rowntree P, Starkey D, Nissen L. The use of virtual reality computed tomography simulation within a medical imaging and a radiation therapy undergraduate programme. J Med Radiat Sci. (2021) 68:28–36. doi: 10.1002/jmrs.436
89. Torda ACLASSIE. teaching - using virtual reality to incorporate medical ethics into clinical decision making. BMC Med Educ. (2020) 20:326. doi: 10.1186/s12909-020-02217-y
90. Liaw SY, Choo T, Wu LT, Lim WS, Choo H, Lim SM, et al. “Wow, woo, win”: healthcare students’ and facilitators’ experiences of interprofessional simulation in three-dimensional virtual world: a qualitative evaluation study. Nurse Educ Today. (2021) 105:105018. doi: 10.1016/j.nedt.2021.105018
91. Liaw SY, Ooi SW, Rusli KDB, Lau TC, Tam WWS, Chua WL. Nurse-physician communication team training in virtual reality versus live simulations: randomized controlled trial on team communication and teamwork attitudes. J Med Internet Res. (2020) 22:e17279. doi: 10.2196/17279
92. Jeon YK, Youm JB, Ha K, Woo J, Yoo HY, Leem CH, et al. Teaching cardiac excitation-contraction coupling using a mathematical computer simulation model of human ventricular myocytes. Adv Physiol Educ. (2020) 44:323–33. doi: 10.1152/advan.00093.2019
93. Han SG, Kim YD, Kong TY, Cho J. Virtual reality-based neurological examination teaching tool (VRNET) versus standardized patient in teaching neurological examinations for the medical students: a randomized, single-blind study. BMC Med Educ. (2021) 21:493. doi: 10.1186/s12909-021-02920-4
94. Björn MH, Laurila JM, Ravyse W, Kukkonen J, Leivo S, Mäkitalo K, et al. Learning impact of a virtual brain electrical activity simulator among neurophysiology students: mixed-methods intervention study. JMIR Serious Games. (2020) 8:e18768. doi: 10.2196/18768
95. De Ponti R, Marazzato J, Maresca AM, Rovera F, Carcano G, Ferrario MM. Pre-graduation medical training including virtual reality during COVID-19 pandemic: a report on students’ perception. BMC Med Educ. (2020) 20:332. doi: 10.1186/s12909-020-02245-8
96. O’Connor M, Stowe J, Potocnik J, Giannotti N, Murphy S, Rainford L. 3D virtual reality simulation in radiography education: the students’ experience. Radiography. (2021) 27:208–14. doi: 10.1016/j.radi.2020.07.017
97. Alvarez-Lopez F, Maina MF, Arango F, Saigí-Rubió F. Use of a low-cost portable 3D virtual reality simulator for psychomotor skill training in minimally invasive surgery: task metrics and score validity. JMIR Serious Games. (2020) 8:e19723. doi: 10.2196/19723
98. Sattar MU, Palaniappan S, Lokman A, Shah N, Riaz Z, Khalid U. User experience design in virtual reality medical training application. J Pak Med Assoc. (2021) 71:1730–5. doi: 10.5455/JPMA.22992
99. Khundam C, Sukkriang N, Noël F. No difference in learning outcomes and usability between using controllers and hand tracking during a virtual reality endotracheal intubation training for medical students in Thailand. J Educ Eval Health Prof. (2021) 18:22. doi: 10.3352/jeehp.2021.18.22
100. Mansoory MS, Khazaei MR, Azizi SM, Niromand E. Comparison of the effectiveness of lecture instruction and virtual reality-based serious gaming instruction on the medical students’ learning outcome about approach to coma. BMC Med Educ. (2021) 21:347. doi: 10.1186/s12909-021-02771-z
101. Jaskiewicz F, Kowalewski D, Starosta K, Cierniak M, Timler D. Chest compressions quality during sudden cardiac arrest scenario performed in virtual reality: a crossover study in a training environment. Medicine. (2020) 99:e23374. doi: 10.1097/MD.0000000000023374
102. López Chávez O, Rodríguez LF, Gutierrez-Garcia JOA. comparative case study of 2D, 3D and immersive-virtual-reality applications for healthcare education. Int J Med Inform. (2020) 141:104226. doi: 10.1016/j.ijmedinf.2020.104226
103. Berg H, Steinsbekk A. The effect of self-practicing systematic clinical observations in a multiplayer, immersive, interactive virtual reality application versus physical equipment: a randomized controlled trial. Adv Health Sci Educ Theory Pract. (2021) 26:667–82. doi: 10.1007/s10459-020-10019-6
104. Alharbi Y, Al-Mansour M, Al-Saffar R, Garman A, Alraddadi A. Three-dimensional virtual reality as an innovative teaching and learning tool for human anatomy courses in medical education: a mixed methods study. Cureus. (2020) 12:e7085. doi: 10.7759/cureus.7085
105. Birrenbach T, Zbinden J, Papagiannakis G, Exadaktylos AK, Müller M, Hautz WE, et al. Effectiveness and utility of virtual reality simulation as an educational tool for safe performance of COVID-19 diagnostics: prospective, randomized pilot trial. JMIR Serious Games. (2021) 9:e29586. doi: 10.2196/29586
106. Gaur U, Majumder MAA, Sa B, Sarkar S, Williams A, Singh K. Challenges and opportunities of preclinical medical education: COVID-19 crisis and beyond. SN Compr Clin Med. (2020) 2:1992–7. doi: 10.1007/s42399-020-00528-1
107. Wu Z, Yu J, Wu Q, Hou P, Sun J. Validation of radiographic quality of simulation software - ImaSim. J Xray Sci Technol. (2021) 29:453–62. doi: 10.3233/XST-210860
108. Wang J, Hu X, Liu J, Li L. Pharmacy students’ attitudes towards physician-pharmacist collaboration: intervention effect of integrating cooperative learning into an interprofessional team-based community service. J Interprof Care. (2016) 30:591–8. doi: 10.1080/13561820.2016.1185095
109. Wang J, Guo J, Wang Y, Yan D, Liu J, Zhang Y, et al. Use of profession-role exchange in an interprofessional student team-based community health service-learning experience. BMC Med Educ. (2020) 20:212. doi: 10.1186/s12909-020-02127-z
110. Nieto-Escamez FA, Roldán-Tapia MD. Gamification as online teaching strategy during COVID-19: a mini-review. Front Psychol. (2021) 12:648552. doi: 10.3389/fpsyg.2021.648552
111. Hoopes S, Pham T, Lindo FM, Antosh DD. Home surgical skill training resources for obstetrics and gynecology trainees during a pandemic. Obstet Gynecol. (2020) 136:56–64. doi: 10.1097/AOG.0000000000003931
112. Park JC, Kwon HE, Chung CW. Innovative digital tools for new trends in teaching and assessment methods in medical and dental education. J Educ Eval Health Prof. (2021) 18:13. doi: 10.1097/AOG.0000000000003931
113. Posever N, Sehdev M, Sylla M, Mashar R, Mashar M, Abioye A. addressing equity in global medical education during the COVID-19 pandemic: the global medical education collaborative. Acad Med. (2021) 96:1574–9. doi: 10.1097/ACM.0000000000004230
114. Olszewski AE, Daniel DA, Stein DR, McCulloch MI, Su SW, Hames DL, et al. Teaching pediatric peritoneal dialysis globally through virtual simulation. Clin J Am Soc Nephrol. (2018) 13:900–6. doi: 10.2215/CJN.10460917
115. Maresky HS, Oikonomou A, Ali I, Ditkofsky N, Pakkal M, Ballyk B. Virtual reality and cardiac anatomy: exploring immersive three-dimensional cardiac imaging, a pilot study in undergraduate medical anatomy education. Clin Anat. (2019) 32:238–43. doi: 10.1002/ca.23292
116. Lorenzo-Alvarez R, Rudolphi-Solero T, Ruiz-Gomez MJ, Sendra-Portero F. Game-based learning in virtual worlds: a multiuser online game for medical undergraduate radiology education within second life. Anat Sci Educ. (2020) 13:602–17. doi: 10.1002/ase.1927
117. Richardson A, Hazzard M, Challman SD, Morgenstein AM, Brueckner JKA. “Second Life” for gross anatomy: applications for multiuser virtual environments in teaching the anatomical sciences. Anat Sci Educ. (2011) 4:39–43. doi: 10.1002/ase.195
118. Virtual Reality Medical Simulation. Oxford Medical Simulation. (2020). Available online at: http://oxfordmedicalsimulation.com/product/vr-medical-simulation/ (Accessed June 18, 2020)
119. Klosiewicz T, Zalewski R, Faferek J, Zawiejska A. Application of medical simulation in the education of medical students in the area of gynecology and obstetrics. Ginekol Pol. (2020) 91:281–6. doi: 10.5603/GP.2020.0046
120. Brinkmann C, Fritz M, Pankratius U, Bahde R, Neumann P, Schlueter S, et al. Box- or virtual-reality trainer: which tool results in better transfer of laparoscopic basic skills?-A prospective randomized trial. J Surg Educ. (2017) 74:724–35. doi: 10.1016/j.jsurg.2016.12.009
121. Tabatabai S. Simulations and virtual learning supporting clinical education during the COVID 19 pandemic. Adv Med Educ Pract. (2020) 11:513–6. doi: 10.2147/AMEP.S257750
Keywords: virtual simulation, virtual reality, undergraduate medical education, simulation-based learning, computer simulation
Citation: Wu Q, Wang Y, Lu L, Chen Y, Long H and Wang J (2022) Virtual Simulation in Undergraduate Medical Education: A Scoping Review of Recent Practice. Front. Med. 9:855403. doi: 10.3389/fmed.2022.855403
Received: 15 January 2022; Accepted: 10 March 2022;
Published: 30 March 2022.
Edited by:
Lynn Valerie Monrouxe, The University of Sydney, AustraliaCopyright © 2022 Wu, Wang, Lu, Chen, Long and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jun Wang, d2FuZ2p1bkB3dXN0LmVkdS5jbg==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.