- 1Department of Anesthesiology and Perioperative Medicine, Xijing Hospital, Fourth Military Medical University, Xi’an, China
- 2Department of Traditional Chinese Medicine, Xijing Hospital, Fourth Military Medical University, Xi’an, China
- 3Department of Anesthesiology and Perioperative Medicine, Translational Research Institute of Brain and Brain-Like Intelligence, Shanghai Fourth People’s Hospital Affiliated to Tongji University School of Medicine, Shanghai, China
Background: Postoperative delirium is common in elderly patients following major surgery. This study aimed to assess the effect of transcutaneous electrical acupoint stimulation combined with auricular acupressure on the incidence of postoperative delirium among older patients undergoing major abdominal surgery.
Methods: In this single-center, randomized controlled clinical trial, 210 patients aged 65 years or older undergoing major abdominal surgery were randomized to receive either intervention treatment (transcutaneous electrical acupoint stimulation started at 30 min before anesthesia until the end of the surgery, followed by intermittent auricular acupressure in the first three postoperative days; n = 105) or standard care (n = 105). The primary outcome was the incidence of delirium at the first seven postoperative days or until hospitalization depended on which came first. Secondary outcomes included delirium severity, opioid consumption, postoperative pain score, sleep quality, length of postoperative hospital stay, and postoperative 30-day complications. Enrollment was from April 2019 to March 2020, with follow-up ending in April 2020.
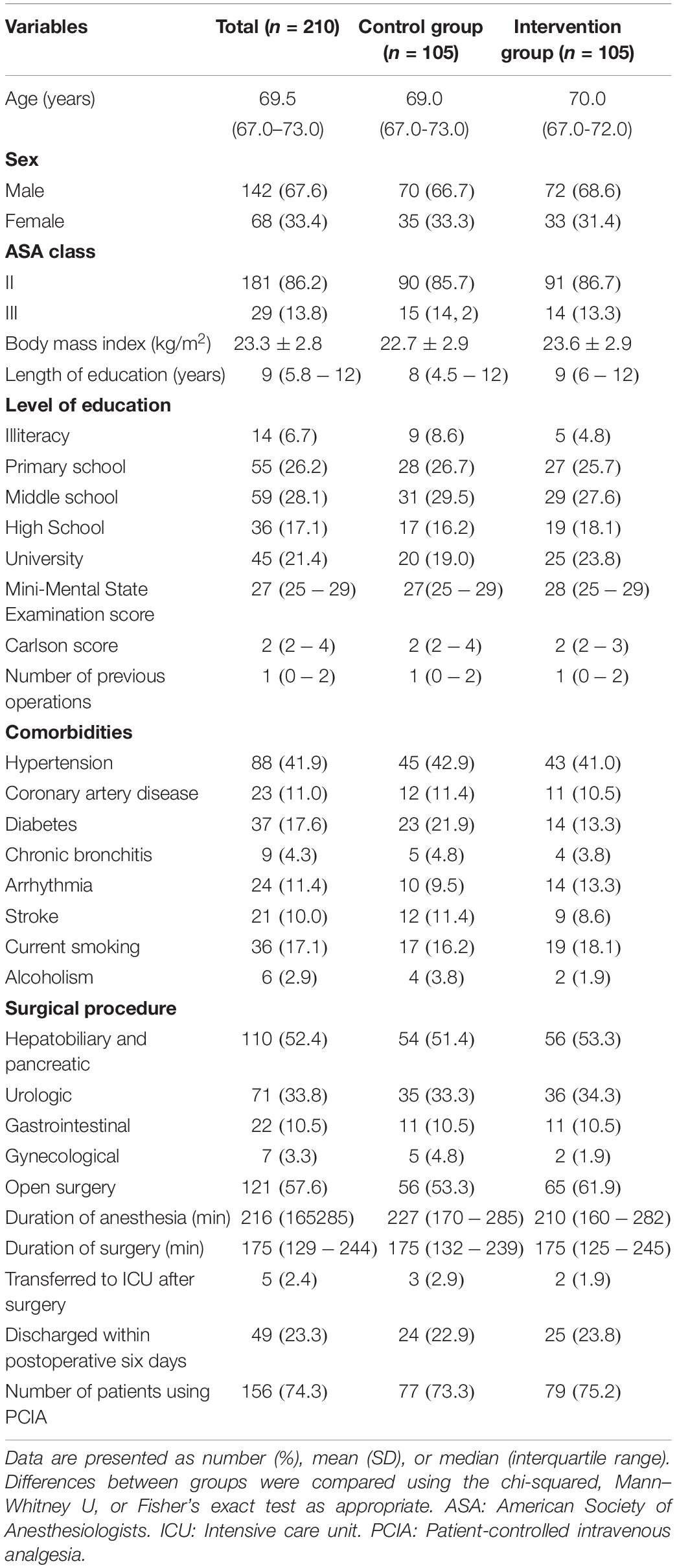
Results: All of the 210 randomized patients [median age, 69.5 years, 142 (67.6%) male] completed the trial. The incidence of postoperative delirium was significantly reduced in patients received intervention treatment (19/105 (18.1%) vs. 8/105 (7.6%), difference, –10.5% [95% CI, –1.5% to –19.4%]; hazard ratio, 0.41 [95% CI, 0.18 to 0.95]; P= 0.023). Patients in the control group had a higher postoperative Memorial Delirium Assessment Scale (4 vs. 3; difference, –1; 95% CI, –1 to 0; P = 0.014) and a greater increase in Pittsburgh Sleep Quality Index score from baseline to postoperative day three (2.5 vs. 2.0; difference, –1; 95% CI, –2 to –1; P < 0.001) than patients in the intervention group. No significant difference was observed as of other secondary outcomes.
Conclusion: In elderly patients undergoing major abdominal surgery, transcutaneous electrical acupoint stimulation combined with auricular acupressure reduced the incidence of postoperative in-hospital delirium compared with standard care. A multicenter, randomized clinical trial with a larger sample size is necessary to verify these findings.
Clinical Trial Registration: [https://clinicaltrials.gov], identifier [NCT03726073].
Introduction
Postoperative delirium is an acute neurological disorder that commonly occurs within the first three days after the operation (1, 2). Delirium prevalence ranges from 18 to 35% in general medical services and reaches 50% in elderly patients after high-risk surgery (3). It has been documented that postoperative delirium is associated with increased mortality, morbidity, and healthcare costs (4, 5). Despite efforts to decrease its occurrence, the incidence of postoperative delirium remains at 15%–54% in elderly patients after major abdominal surgery (6, 7).
The etiology of postoperative delirium is multifactorial and not fully elucidated. Cumulative evidence has shown that it may be associated with neuroinflammation, alteration in neurotransmitters, subclinical cerebral vascular events, and can be precipitated by factors such as pain, hypotension, and electroencephalogram suppression during surgery (1, 8). Acupuncture, a traditional Chinese medicine, has been reported to have anti-inflammatory and neuroprotective properties (9, 10). It also alleviates perioperative hypotension, reduces anesthetic and analgesic consumption, and improves sleep disorders (9, 11). Therefore, acupuncture and related techniques might exert a beneficial influence in reducing postoperative delirium.
Evidence supporting the use of acupuncture on delirium prevention is limited. A pilot study has shown that transcutaneous electrical acupoint stimulation applied on pre-and intraoperative has a trend of alleviating postoperative delirium in elderly patients with silent lacunar infarction undergoing spinal surgery (6.3% vs. 25.0%; relative risk, 0.25; 95% CI, 0.06 to 1.09) (12). Since the effect of a single session of electronic acupuncture only lasted for two or 3 h (9, 13), the transitory acupuncture protocol in the study may attribute to the limited effect of acupuncture on delirium prevention. Previous studies reported that delirium mainly occurs within postoperative three days (14, 15); thus, adding acupuncture interventions on postoperative three days may augment its preventive effects. Postoperative auricular acupuncture has shown its effect on relieving anxiety in post-cesarean section women (16) and preventing postoperative agitation in geriatric patients (17). In clinical practice, body and auricular acupuncture have been combined for synergistic effects, such as sleep improvement and opioid rescue (18, 19). However, the combined effects of body acupuncture and auricular acupuncture for delirium prevention in elderly patients have not been explored.
This study hypothesized that pre-and intra-operative transcutaneous electrical acupoint stimulation combined with auricular acupressure treatment for the first three postoperative days compared with standard care would reduce the incidence of postoperative delirium among elderly patients undergoing major abdominal surgery.
Materials and Methods
Study Design
This was a single-center, prospective, randomized, assessor-blinded trial. Ethical approval was obtained from the Institutional Review Board of Xijing Hospital (No. KY20182080-F-1) in Xi’an, Shaanxi Province of China. The trial was registered at ClinicalTrials.gov before patient enrollment (NCT03726073, October 31, 20181). Written informed consent was obtained from all patients before randomization.
Participants
Participants 65 years or older with American Society of Anesthesiologists physical status class ≤ III and scheduled for elective, major abdominal surgery (including hepatobiliary and pancreatic, urologic, gastrointestinal, or gynecological) were eligible for trial inclusion. Major surgery was defined by a planned more than two days hospitalization (20). Participants were required to complete a Mini-Mental State Examination and have a score higher than 20. Patients were excluded if they had a severe visual or auditory impairment, literacy deficits, mental illness, history of brain injury or neurosurgery, with a history of alcohol or drug abuse, history of acupuncture treatment, or contradicted to transcutaneous electrical acupoint stimulation or auricular acupressure (for example, planted with pacemakers, with skin lesions, or allergy to surface electrodes).
Randomization and Blinding
Participants were recruited into the study from the electronic medical record system of our hospital by research staff. After giving consent and completing the baseline assessment, eligible participants were randomly assigned to either the intervention group (transcutaneous electrical acupoint stimulation combined with auricular acupressure) or the control group (standard care) in a 1:1 ratio using simple randomization. The random allocation sequence was generated by the statistician.
Study-group assignments were concealed in opaque envelopes and revealed by a research nurse upon patients’ arrival at the operation room. The investigators including the research coordinator, outcome assessors, data collectors, and the statistician were blinded to treatment allocation. The acupuncturist and participants were not blinded. The care team (surgeons, anesthesiologists, and nurses) were aware that an acupuncture study was undergoing but were blinded to study hypothesis and intervention protocol. Participants were informed not to discuss the group allocation or the aim of the study with investigators (except the acupuncturist) during the whole process of the study. Assessors would communicate with the ward nurses, and ask the nurses to let the patients wear an earmuff (loose enough to ensure patients could hear the assessors’ questions) before every postoperative evaluation. In addition, interactions between the assessors, participants and their family members were limited to the questions on the case report form. To assess the frequency of unblinding to group allocation, the assessors were asked to guess which treatment this patient had received after a patient was discharged from the hospital.
Intervention
The acupressure protocol used in the present study was based on previous publications relating to acupoint selection in symptom management (12), investigators’ previous publications (9), and clinical experience of the acupuncturist in the team who is specializing in acupuncture clinical practice with seven years.
In the intervention group, participants received transcutaneous electrical acupoint stimulation through bilateral Hegu (LI4), Neiguan (PC6), and Zusanli (ST36) acupoints after entering the operation room. The neuroprotective effects and the exact locations of these three acupoints have been previously described (12, 21, 22). After entering the operation room, Hwato brand disposable electronic pads (size 50 mm × 50 mm) were placed on these acupoints after skin disinfection and then simultaneously connected to a transcutaneous electroacupuncture apparatus (SDZ-V, Suzhou Medical Appliance Company, Suzhou, Jiangsu, China). The transcutaneous electroacupuncture apparatus was set to provide a disperse-dense wave with an alternating frequency of 2/10 Hz. The current intensity was modulated between 5 and 20 mA (5 to 10 mA for the upper limbs, 10 to 20 mA for the lower limbs) and the final stimulus current of each acupoint was regulated individually until the De Qi sensation (a composite of sensations including soreness, numbness, distention, heaviness, and others such as coldness, warmness, and pain electric-shock feeling) was achieved at each acupoint. The electrostimulation was started from 30 min before anesthesia induction and up to the end of surgery.
Postoperatively, after arriving at the post-anesthesia care unit, patients in the intervention group were tapped Vaccaria seeds (Hebei Heshi Medical Apparatus and Instruments Co., LTD, Hengshui, China) at seven auricular points (Shenmen, Point Zero, Sympathetic, Subcortex, Heart, Liver, and Endocrine) located on the right ear by the acupuncturist. These auricular acupoints were previously used alone or combined to manage postoperative agitation and sleep disturbances (17, 23, 24). From postoperative day one to day three, participants were instructed to manually stimulate each auricular acupoint for 30 s, five times a day, for three days (From nine AM to nine PM, around every 3 h). Participants were instructed on the procedure, stimulation techniques, duration and intensity of auricular acupressure, the methods of keeping acupressure patches in the right place and protecting them, and were asked to document the time of auricular acupressure application and any side-effects in a diary sheet. The acupuncturist verified the quality of auricular acupressure daily. The pastes with seeds were removed after three days.
Participants in the standard care group did not receive any acupuncture intervention during the study period.
Anesthesia Protocol
Anesthesia was induced with intravenous propofol (1–2 mg/kg) or etomidate (0.2–0.3 mg/kg), sufentanil (3 μg/kg), and rocuronium (1 mg/kg). After the loss of consciousness, an endotracheal tube was intubated. Anesthesia was maintained with sevoflurane inhalation (0.7–1.7 minimum alveolar concentration) and remifentanil infusion (0.05–0.2μg/kg/min). Rocuronium was administered as indicated (0.2 mg/kg). The depth of anesthesia was adjusted based on the hemodynamic indices and bispectral index (BIS). The BIS was maintained at 40–60 during surgery. Use of dexmedetomidine, midazolam, anticholinergic drugs, and haloperidol was avoided unless they were indicated for delirium rescue therapy. Standard monitoring procedures included electrocardiography, pulse oximetry, capnography, and inspiratory and expiratory sevoflurane concentrations. Invasive blood pressure monitoring was applied when necessary. A lung-protective ventilation strategy and multimodal analgesia were applied intraoperatively. Analgesia was assisted by intravenous administration of parecoxib sodium (40 mg) and oxycodone (0.1 mg/kg) preoperatively and local anesthetic infiltration in the surgical wound (0.5% ropivacaine) postoperatively. Postoperative intravenous patient-controlled analgesia was applied to patients during postoperative three days based on anesthesiologists’ clinical experience. Patient-controlled intravenous analgesia was established with 100 ml of 1 μg/ml sufentanil and 80 μg/ml butorphanol, programmed to deliver a background infusion of 0.015 ml/kg/h and 0.5 mL bolus with a lockout interval of 10 min. Parecoxib sodium (40 mg) was given intravenously every 12 h during the postoperative three days. An intravenous bolus of rescue oxycodone (0.05–0.1 mg/kg) was available every 6 h if the pain was intolerable.
Outcomes
Two trained investigators who were not involved in the study intervention, anesthesia, and clinical care of patients performed outcome assessment. The primary outcome was the incidence of delirium during the first seven postoperative days or hospitalization if patients were discharged within seven days postoperatively. The diagnosis of delirium and its subtype were based on the Confusion Assessment Method or Confusion Assessment Method-intensive care unit for intubated patients, the Richmond Agitation Sedation Scale, reports from family members, and medical records review (5, 25, 26). Delirium was assessed daily at around 6 PM. The Confusion Assessment Method algorithm required the identification of both an acute onset and fluctuating course and inattention and either disorganized thinking or an impaired level of consciousness (25). As ward nurses and surgeons would assess patients’ mental status at least once daily and describe the results in their notes, medical records would be reviewed. For delirium patients in the ward, a mix-type delirium would be diagnosed if the patients manifested a fluctuation of mental status and behaviors during the day. Delirium patients in the intensive care unit were classified using the Richmond Agitation Sedation Scale score (RASS) (26): (1) hyperactive type, consistently positive RASS score remains at + 1 to + 4; (2) hypoactive type, consistently neutral or negative Richmond Agitation Sedation Scale remains at –3 to 0; (3) mixed type, alternative positive and negative.
Secondary outcomes included delirium severity measured by the Memorial Delirium Assessment Scale, intraoperative opioid consumption, pain intensity both at rest and at movement assessed by the Numeric Rating Scale at 24 h, 48 h, and 72 h after surgery, sleep quality within the first three postoperative days by the Pittsburgh Sleep Quality Index, length of postoperative hospitalization, the occurrence of non-delirium and complications within postoperative 30 days.
Statistical Analysis
The incidence of postoperative delirium was reported to be up to 23.9% in elderly patients after major surgery (5, 7). We assumed that the incidence of postoperative delirium would be reduced from 23.9% in the control group to 8.9% in the intervention group based on the effect reported in a small randomized controlled trial (12). With significance set at 0.05 and a power of 80%, 95 patients in each group were required (PASS 15.0 software, NCSS, Kaysville, UT) to detect the differences. Considering a loss to follow-up rate of 10%, we planned to enroll 210 participants, with 105 in each group.
Analyses of primary and secondary outcomes were performed both in the intention-to-treat and per-protocol populations. We did not plan an interim analysis. We did not conduct the missing data imputation as there were no missing data for the primary outcome and less than 5% for all secondary outcomes.
Categorical variables are presented as frequencies or proportions and analyzed using the chi-squared test or Fisher exact test. Continuous variables are presented as mean (standard deviation) or median (interquartile range) depending on distribution (the Shapiro-Wilk test was used to assess normality) and analyzed with independent samples t-test or Mann–Whitney U test. The relative risk and 95% confidence interval (CI) are used to describe the differences in dichotomous outcomes. The difference (and 95% CI) between medians were calculated with the Hodges–Lehmann estimator.
The primary endpoint was analyzed using the chi-squared test. The cumulative postoperative delirium incidence was calculated with the Kaplan–Meier estimator, with differences between groups assessed using the log-rank test. The hazard ratio and 95% CI estimated with a Cox regression model were used to describe differences if the proportional assumption was not violated. The Cox regression model was adjusted for age and sex.
The Memorial Delirium Assessment Scale within seven postoperative days was compared using a generalized linear mixed-effect model, with results presented as mean and 95% CI. Treatment assignment, time, and interaction between treatment assignment and time effects were included as fixed effects. Participants were included as random effects. The model covariates were unadjusted.
Sensitivity analysis included analysis of the primary and secondary outcomes in the per-protocol populations. We performed post hoc subgroup analyses using a Cox proportional hazards model to investigate the intervention effects on the cumulative delirium incidence in specific subgroups, including sex (male vs. female), age (< 70 years old vs. ≥ 70 years old), the education level (≤ 9 years of schooling or no qualification vs. >9 years of schooling), surgery type (upper abdominal surgery vs. lower abdominal surgery), and history of operation. We tested for treatment effect heterogeneity across various subgroups and reported the corresponding P values for interaction.
Statistical analyses were performed using SPSS 24.0 (IBM Corp., Armonk NY). Two-tailed tests were used in all analyses, and P < 0.05 was considered statistically significant.
Results
Trial Population and Baseline Characteristics
From April 17, 2019, to March 10, 2020, 334 patients scheduled for major abdominal surgery were screened for eligibility at Xijing Hospital, Xi’an, Shaanxi Province of China. Among them, 210 patients were enrolled and randomly assigned to either the intervention group (n = 105) or the standard care group (n = 105). Eight patients (two in the intervention group and three in the standard care group violated anesthesia protocol, three in the intervention group violated acupuncture protocol) were excluded from the per-protocol analysis (Figure 1).
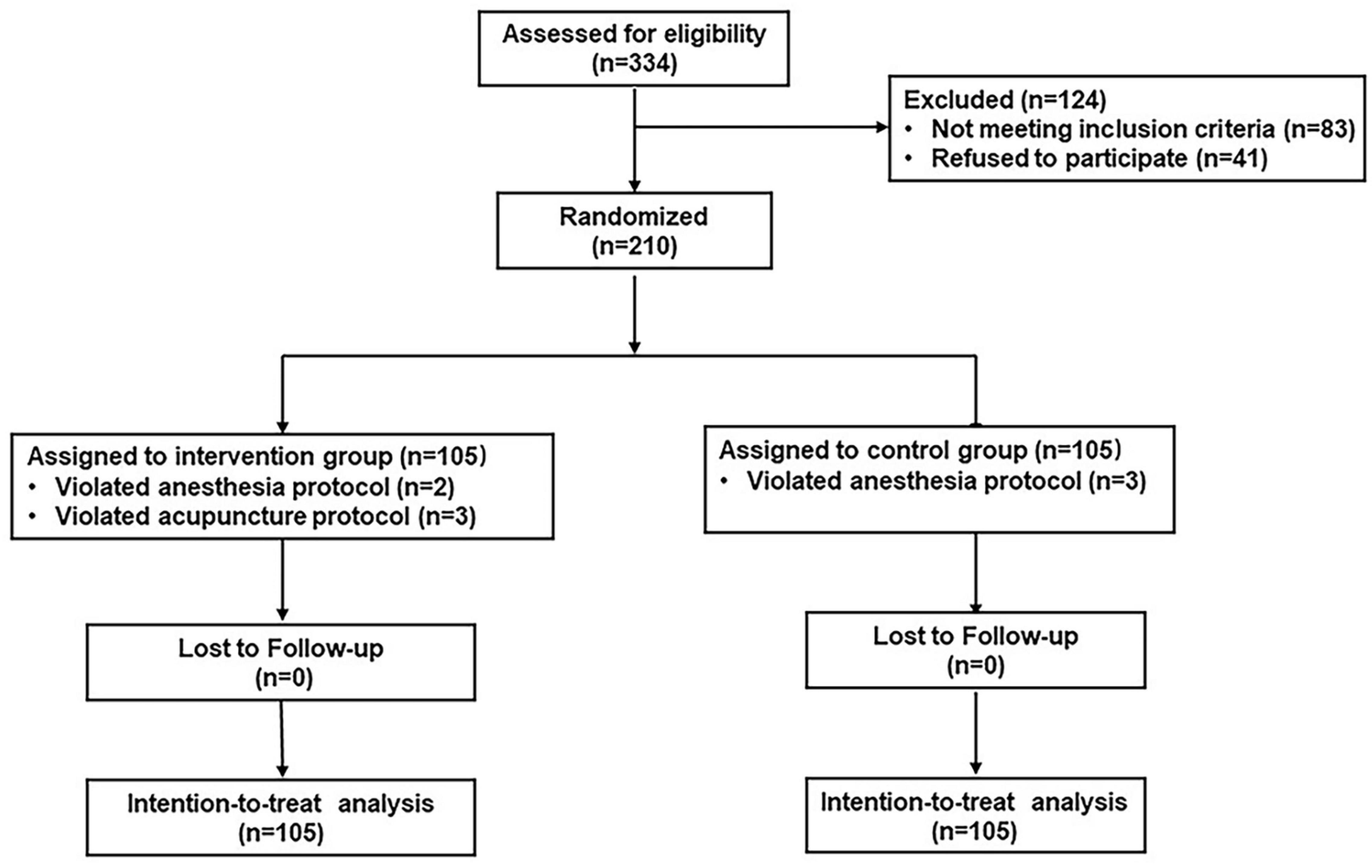
Figure 1. Trial profile. The intention-to-treat analysis included all randomized patients in the groups in which they were randomly assigned.
Overall, most of the patients were male (142/210, 67.6%), and the median age was 69.5 (interquartile range, 67.0–73.0) years (Table 1). The types of surgery included hepatobiliary and pancreatic (52.4%), urologic (33.8%), gastrointestinal (10.5%), and gynecological (3.3%) procedures (Table 1). Baseline characteristics and surgical parameters did not differ between the two groups (Table 1). Forty-nine (23.3%) patients were discharged within postoperative six days, five (2.4%) patients (three in the control group and two in the intervention group) were transferred to the intensive care unit after surgery, and there were no differences between groups. The final visit of the last randomized patient took place on April 10, 2020.
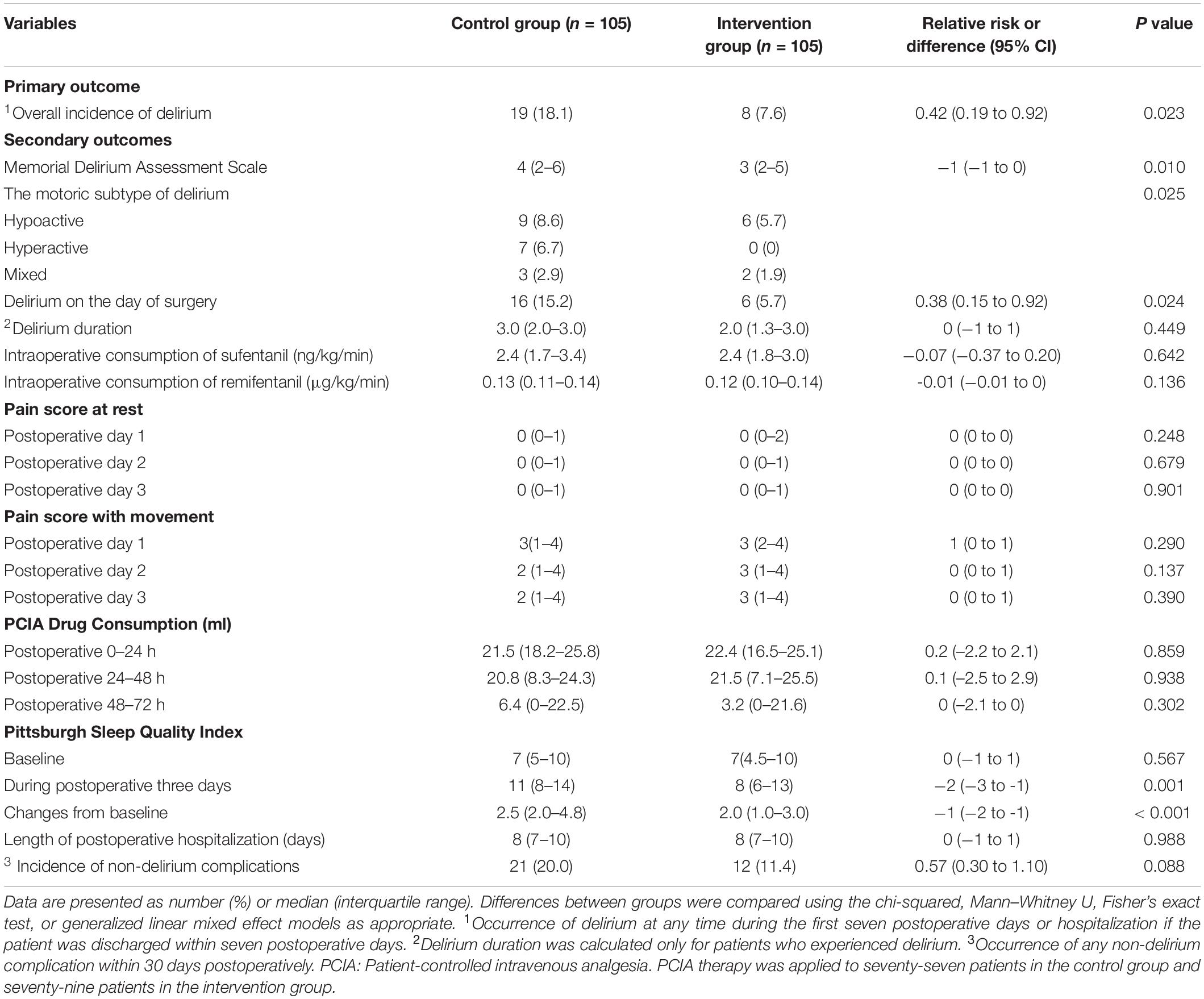
Primary and Secondary Outcomes
In the intention-to-treat population, the incidence of postoperative delirium during postoperative seven days was 7.6% (8/105) in the intervention group and 18.1% (19/105) in the control group (difference, −10.5% [95% CI, −1.5% to −19.4%]; relative risk, 0.42 [95% CI, 0.19 to 0.92]; P = 0.023; number needed to treat = 10 [95% CI, 5 to 64]; Table 2). The proportion of postoperative delirium-free patients significantly differed between the two groups (hazard ratio, 0.41; 95% CI, 0.18 to 0.95; P = 0.023) (Figure 2).
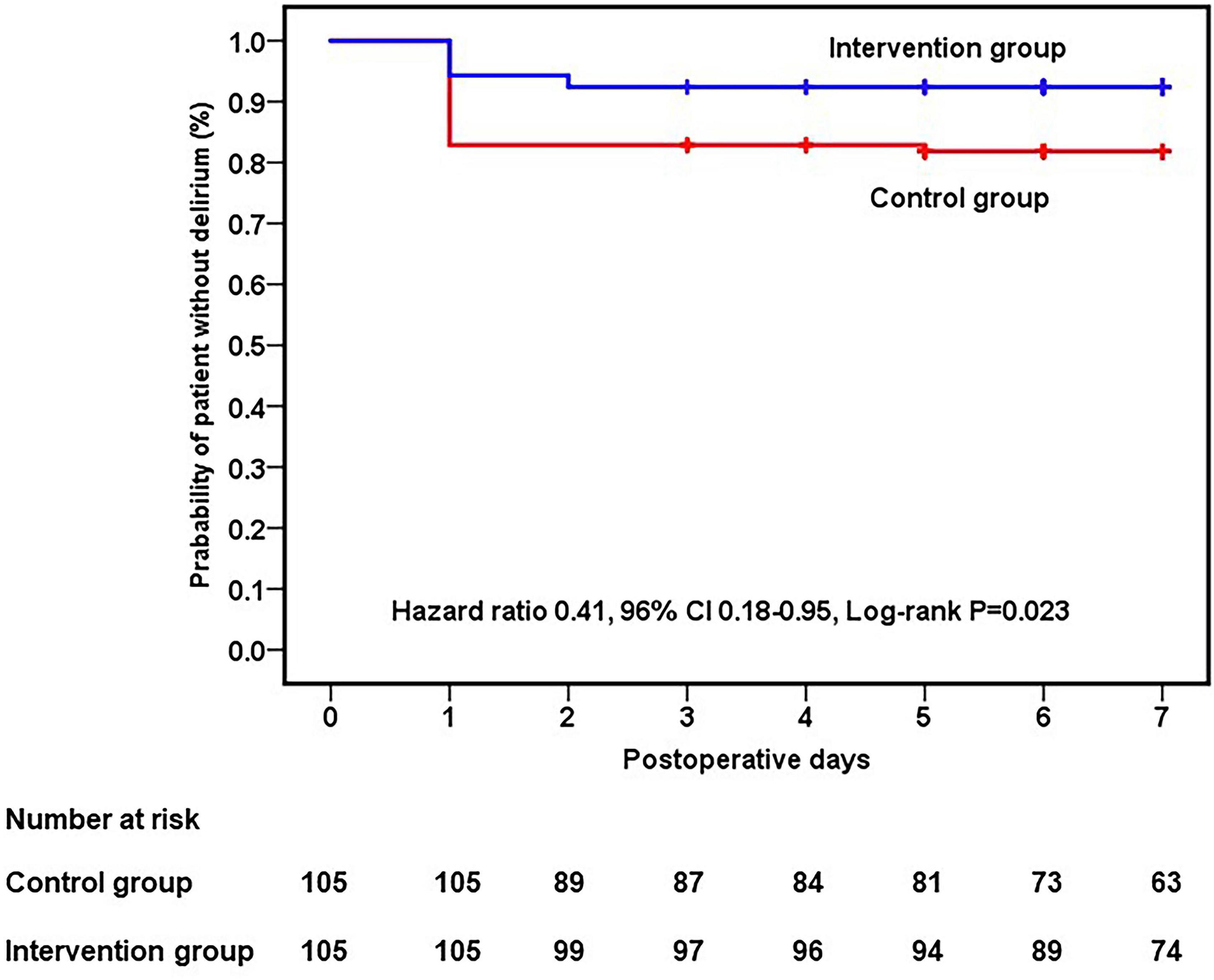
Figure 2. Kaplan–Meier curve showing the probability of a patient being delirium-free within seven postoperative days.
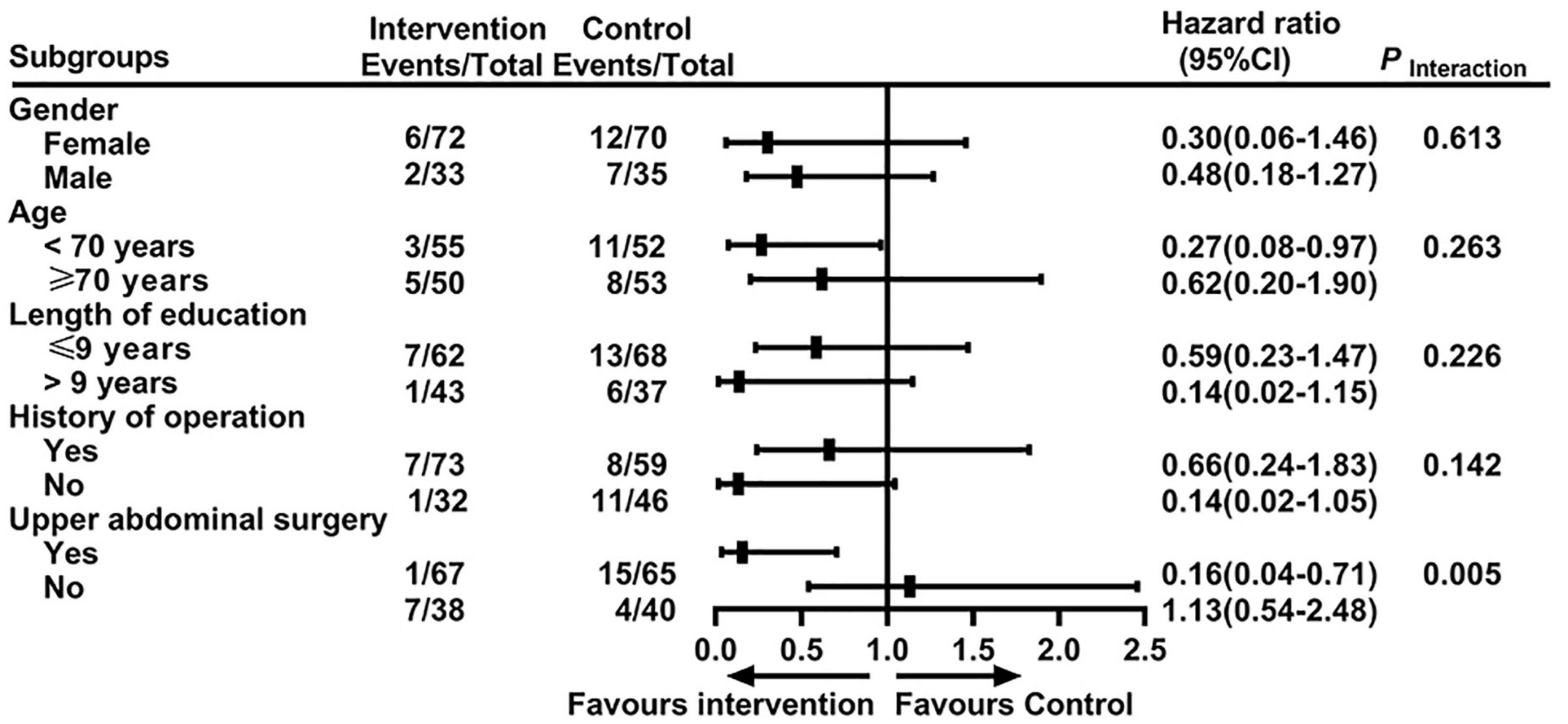
Subgroup analyses using the Cox model showed that the interaction between surgery sites and treatment was statistically significant (P = 0.005, Figure 3). Patients who underwent upper abdominal surgery benefited more from the intervention than those who underwent lower abdominal surgery (hazard ratio, 0.16; 95% CI, 0.04 to 0.71).
The incidence of delirium on the day of surgery was 5.7% (6/105) in the intervention group and 15.2% (16/105) in the control group (relative risk, 0.38; 95% CI, 0.15 to 0.92; P = 0.024). Delirium severity measured by Memorial Delirium Assessment Scale was lower in the intervention group than in the control group (3 vs. 4; difference, –1; 95% CI,–1 to 0; P = 0.010), with significant differences on postoperative day two (P = 0.007), day three (P < 0.001) and day four (P = 0.037) (Figure 4). The control group had a significantly greater increase regarding Pittsburgh Sleep Quality Index score change from baseline to postoperative day three than the intervention group (2.5 vs. 2.0; difference, –1; 95% CI, –2 to –1; P < 0.001). The two groups did not differ significantly with respect to the duration of delirium, the intraoperative consumption of sufentanil and remifentanil, the Numeric Pain Rating Scale at rest and movement at postoperative 24 h, 48 h, and 72 h, the patient-controlled intravenous analgesia drug consumption during postoperative 0–24 h, 24–48 h, and 48–72 h, and the length of postoperative hospitalization (Table 2).
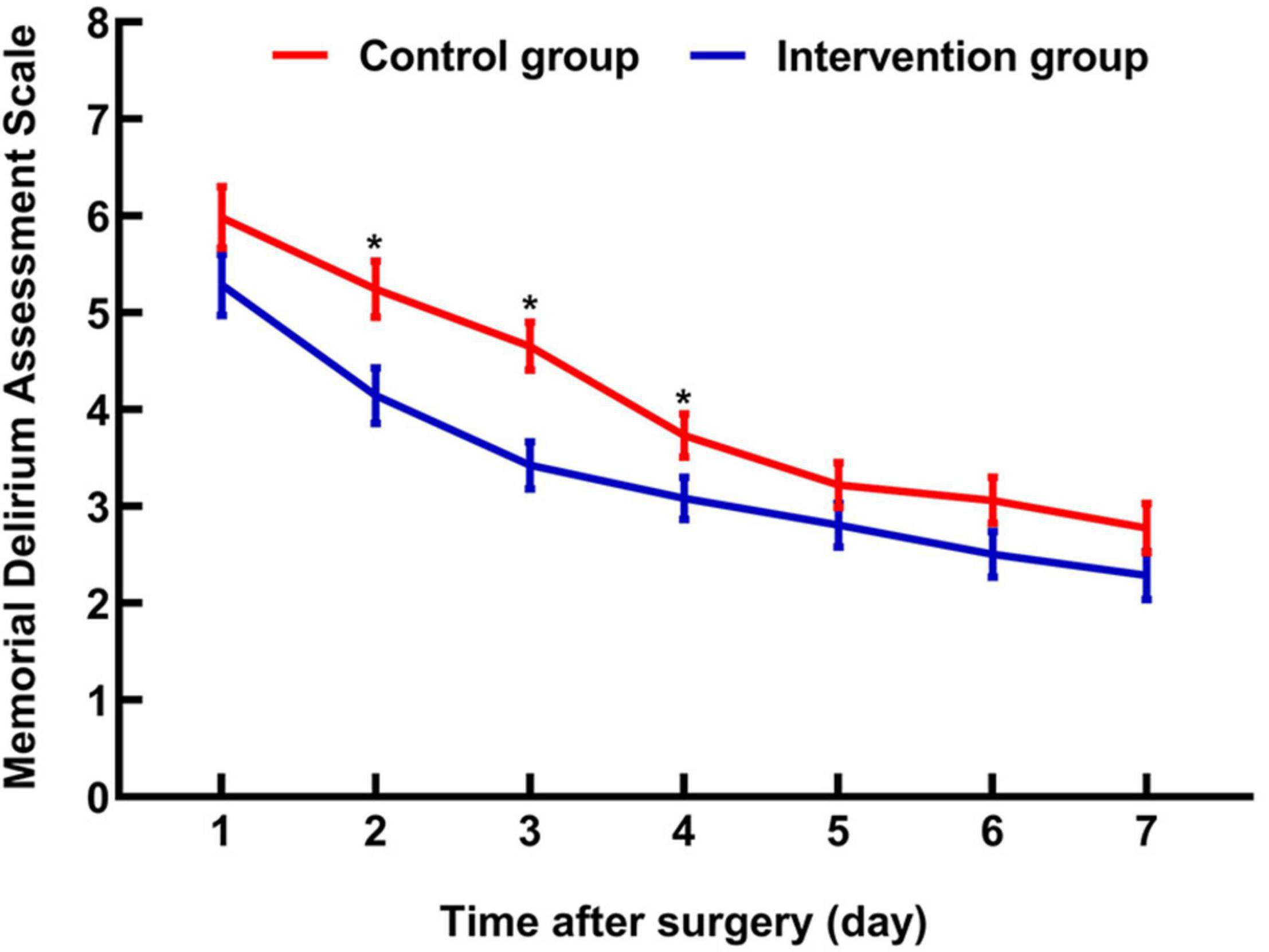
Figure 4. Changes in Memorial Delirium Assessment Scale during the first postoperative seven days. Makers indicate means, and error bars indicate standard errors. *Significant difference between groups.
The per-protocol analysis yielded similar results (Supplementary Table 1).
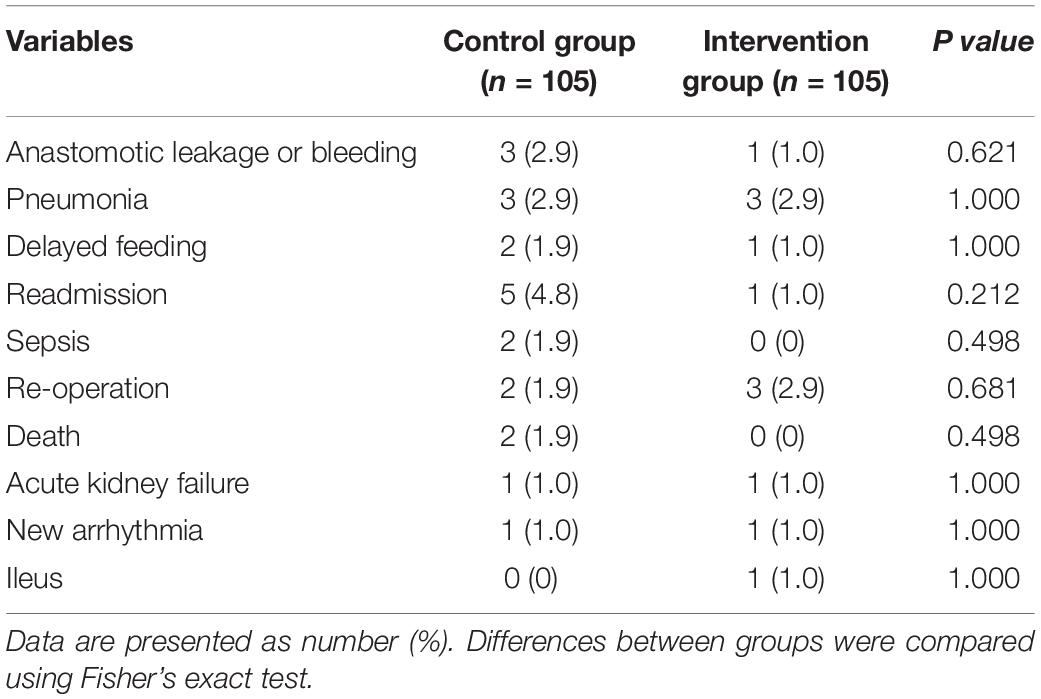
Adverse Events
Thirty-three surgery-related adverse events (12 in the intervention group and 21 in the control group) were documented within 30 days postoperatively. Adverse events (anastomotic leakage or bleeding, pneumonia, delayed feeding, readmission, sepsis, re-operation, death, acute kidney failure, new arrhythmia, and ileus), whether viewed individually (P for each > 0.20) or collectively (11.4% vs. 20.0%; relative risk, 0.57; 95% CI, 0.30 to 1.10; P = 0.088), did not significantly differ between the two groups (Table 3). Two patients in the control group died of postoperative septic shock, but no difference was found in all-cause 30-day mortality between groups.
Skin temporary pain or paranesthesia was considered an expected adverse event with transcutaneous electrical acupoint stimulation and auricular acupressure treatment. One patient in the intervention group reported mild leg numbness, which was alleviated within three days. There was no withdrawal from adverse events.
The Effectiveness of Assessor-Blinded
Outcome assessors were able to get a 54.3% rate for correctly guessing patients’ received therapy (59.0% for the intervention group and 49.5% for the control group). Outcome assessors’ perception of patients’ accepted treatment did not affect the primary outcome (Supplementary Table 2).
Discussion
In this single-center, prospective, randomized trial, transcutaneous electrical acupoint stimulation combined with auricular acupressure reduced the incidence and severity of postoperative delirium and improved postoperative sleep quality in elderly patients undergoing major abdominal surgery.
Postoperative delirium developed in 18.1% of patients in the standard care group. This was in line with previous studies for non-cardiac surgeries, which range from 13 to 50% (3), but slightly lower than the reported rate that we used to estimate sample size (23.9%) (5). There are several reasons for this. First, compared with those in the previous study (5), patients in the current study were younger (median age: 69.5 years vs. 77.0 years) and higher delirium risk patients (such as American Society of Anesthesiologists physical status class > III and Mini-Mental State Examination score ≤ 20) were excluded. Second, anesthesia management was different between the two studies. Delirium risk factors such as midazolam, anticholinergic drugs, and haloperidol were avoided, and Bis-guided anesthesia management was applied during surgery in the present study. These reasons may explain the slightly lower incidence of delirium in this trial (1, 3).
A trend of reduced incidence of postoperative delirium (6.3% vs. 25%; relative risk, 0.25; 95% CI, 0.06 to 1.09) was reported when transcutaneous electrical acupoint stimulation was applied pre- and intraoperatively to 64 geriatric patients with silent lacunar infarction undergoing spine surgery (12). This was consistent with the delirium-prevention effect observed in our study (relative risk, 0.42; 95% CI, 0.19 to 0.92). The mechanisms of the delirium-sparing effect produced by transcutaneous electrical acupoint stimulation and auricular acupressure remain undetermined. Gao et al. demonstrated that transcutaneous electrical acupoint stimulation at bilateral LI4 and PC6 reduced neuroinflammation by lowering the permeability of the blood-brain barrier (12). Studies reported that one potential mechanism by which auricular acupressure may exert its anti-delirium effect is activating the locus coeruleus noradrenergic system, which is one of the central vagal relay centers and plays a critical role in the generating and regulating of delirium (27, 28). By stimulating the ear branch of the vagus nerve, auricular acupressure may exert an add-on neuroprotective effect by direct and indirect modulation of the activity and connectivity of the locus coeruleus noradrenergic system, thus modulating the release and uptake of noradrenaline and dopamine in some key brain regions, including the prefrontal cortex and hippocampus, which are postulated to be associated with attention, memory, and other cognitive dysfunction (27–29). As postoperative delirium has been speculated to be a harbinger for postoperative cognitive dysfunction, the mechanism of acupuncture to prevent postoperative delirium may be similar to those of acupuncture to prevent postoperative cognitive dysfunction, which is by attenuating systemic inflammation and neuroinflammation, reducing oxidative stress levels, improving synaptic plasticity, and reducing neuronal injury (10, 12, 30).
Subgroup analysis of our data suggested that patients who underwent upper abdominal surgery benefitted more from the intervention than patients who underwent lower abdominal surgery. It is unclear why this occurred, but this heterogeneity may be related to the acupoints we selected and the individual response differences toward acupuncture treatment. Kim et al. suggested that individual differences in acupuncture analgesia are associated with inherited genetic factors, adenosine monophosphate-activated protein kinase expression in the hypothalamus, spinal levels of neurotransmitters and pro-inflammatory cytokines, and the density of cholecystokinin receptors (31). The difference of acupuncture’s delirium-prevention effects between upper and lower abdominal surgery may share similar mechanisms and warrant further study. Our results also raise the question of whether the specificity of needling sites is essential to the therapeutic benefits of acupuncture.
Psychological distress, pain, and insomnia are often intertwined (32). Pain and sleep disorders are possible confounders of delirium severity, and thus attenuated the extent of postoperative pain and improved sleep quality might reduce the incidence of postoperative delirium (1, 33). Inconsistent with the previous studies (34, 35), acupuncture did not decrease intraoperative opioid consumption and postoperative pain in this trial. This may be related to the high opioid doses and a multi-model analgesia protocol adopted in the present trial.
The change from baseline to postoperative day three in the Pittsburgh Sleep Quality Index score was more significant in the control group than in the intervention group (2.5 vs. 2.0; between-group difference, –1; 95% CI, –2 to –1; P < 0.001), indicating that the acupuncture intervention in the present study has a beneficial effect on postoperative sleep quality. The improved sleep quality within the first three postoperative days in the present study may be attributed to auricular acupressure, as indicated in the previous studies that auricular acupoint stimulation improves sleep quality (36). The rationale of the auricular acupoints selected in this trial was based on their effects of calming the mind, relieving anxiety, and improving sleep quality (23). Hou et al. showed that auricular acupressure normalized disturbed sleep patterns and improved sleep quality via regulating the neuroendocrine system, neuroimmunological factors, neuroinflammation, and neural reflex, as well as antioxidation (37). However, whether auricular acupressure reduces postoperative delirium directly or indirectly by improving postoperative sleep quality is unclear, which needs to be elucidated in future studies.
The Confusion Assessment Method and Confusion Assessment Method-intensive care unit were used in this study to diagnose delirium as they are commonly used for postoperative delirium identification and easy to learn for non-psychiatrists, with high sensitivity (94% to 100%) and high specificity (90% to 95%) (25). As each assessment may take 20 min to 30 min, and assessments were conducted for postoperative seven days, a once-daily assessment was chosen in this study to improve participants’ compliance. However, it is possible that short periods of fluctuating mental status, inattention, disorganized thinking, or altered consciousness level may not be detected at the time of assessment. Additional medical records review was used in this study to minimize the risk of delirium misclassification, which has been accepted in previous studies (5, 38). Further research should add other screening methods such as the Consortium to Establish a Registry of Alzheimer’s Disease (39) and the Montreal Cognitive Assessment tests (40) to assess other diverse cognitive domains and verify the robustness of anti-delirium effects exerted from electrical acupoint stimulation combined with auricular acupressure.
This study has several limitations. First, this is a single-center study, while internal validity is not impacted, the external validity and generalizability of the results may be affected by clinical practice and therapeutic measures in various medical centers. The sample size is relatively small, the power of this intervention should be tested in a clinical trial with a larger sample size. Second, the enrolled patients and the acupuncturist were not blinded. Thus, an inherent risk of the Hawthorne effect cannot be ruled out in this study. The outcome assessors, data collectors and the statistician were blinded to reduce the risk of bias. Third, a sham acupuncture group was not used to eliminate the placebo effect. Future studies are needed to distinguish the specific and non-specific effects of acupuncture intervention for postoperative delirium. Fourth, the subgroup analysis was post hoc. Therefore, these findings should be interpreted as exploratory. In addition, the number of events in most subgroups was relatively small, which may limit the power to detect the difference among subgroups. Fifth, the dosage of postoperative rescue analgesic drugs was not recorded. However, perioperative pain management was strictly controlled, postoperative pain scores were lower, and the analgesic effect was comparable between the two groups. Standardized perioperative pain management and preservation of randomization would be expected to minimize the confounding from rescue drug consumption differences. Furthermore, although anesthesia management was conducted under the guidance of the BIS, the BIS and frequencies of burst suppression during surgery were not recorded and compared, potentially confounding and biasing the results (41).
Acupuncture is an important supplementary strategy for perioperative management (9), applications of acupuncture before, during, and after surgery as an adjuvant therapy will have a great clinical application. Future acupuncture studies should investigate how to best implement acupuncture in real-world clinical settings, such as setting up an acupuncture protocol and selecting the appropriate acupoints for specific surgeries and populations. To investigate the mechanisms of how acupuncture prevents postoperative delirium could provide essential insights in preventing postoperative delirium. As postoperative delirium and postoperative cognitive dysfunction share risk factors (30), a long-term follow-up to investigate the preventive effects of acupuncture intervention on postoperative cognitive dysfunction should also be included in future studies.
In conclusion, in this single-center, prospective, randomized study, transcutaneous electrical acupoint stimulation combined with auricular acupressure reduced the incidence of postoperative delirium in elderly patients undergoing major abdominal surgery. A multicenter randomized clinical trial with a larger sample size is necessary to verify these findings.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by the Institutional Review Board of Xijing Hospital (No. KY20182080-F-1) in Xi’an, Shaanxi Province of China. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
QF, CL, ZL, HD, and LX contributed to the concept and design of the study and data interpretation. QF and ZL performed the study registration. QF and JF performed the screen of patients. NY performed the acupuncture intervention. YW and LW performed the outcome assessment and data collection. CL performed the data analysis. QF, CL, ZL, and HD prepared the primary manuscript. All the authors read and approved the final version of the manuscript.
Funding
This work was supported by the National Natural Science Foundation of China under grant numbers 81970448 and 81590954; the Natural Science Foundation of Shaanxi Province under grant numbers 2018SF-277 and 2019KW-069.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We thank Chen Li, Department of Health Statistics, School of Preventive Medicine, Fourth Military Medical University, Xi’an, Shaanxi, China, for her support with the data analysis.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2022.855296/full#supplementary-material
Footnotes
References
1. Jin Z, Hu J, Ma D. Postoperative delirium: perioperative assessment, risk reduction, and management. Br J Anaesth. (2020) 125:492–504. doi: 10.1016/j.bja.2020.06.063
2. Lopez MG, Hughes CG, DeMatteo A, O’Neal JB, McNeil JB, Shotwell MS, et al. Intraoperative oxidative damage and delirium after cardiac surgery. Anesthesiology. (2020) 132:551–61. doi: 10.1097/aln.0000000000003016
3. Inouye SK, Westendorp RG, Saczynski JS. Delirium in elderly people. Lancet. (2014) 383:911–22. doi: 10.1016/s0140-6736(13)60688-1
4. Su X, Meng Z-T, Wu X-H, Cui F, Li H-L, Wang D-X, et al. Dexmedetomidine for prevention of delirium in elderly patients after non-cardiac surgery: a randomised, double-blind, placebo-controlled trial. Lancet. (2016) 388:1893–902. doi: 10.1016/s0140-6736(16)30580-3
5. Gleason LJ, Schmitt EM, Kosar CM, Tabloski P, Saczynski JS, Robinson T, et al. Effect of delirium and other major complications on outcomes after elective surgery in older adults. JAMA Surg. (2015) 150:1134–40. doi: 10.1001/jamasurg.2015.2606
6. Chen CC, Li HC, Liang JT, Lai IR, Purnomo JDT, Yang YT, et al. Effect of a modified hospital elder life program on delirium and length of hospital stay in patients undergoing abdominal surgery: a cluster randomized clinical trial. JAMA Surg. (2017) 152:827–34. doi: 10.1001/jamasurg.2017.1083
7. Scholz AF, Oldroyd C, McCarthy K, Quinn TJ, Hewitt J. Systematic review and meta-analysis of risk factors for postoperative delirium among older patients undergoing gastrointestinal surgery. Br J Surg. (2016) 103:e21–8. doi: 10.1002/bjs.10062
8. Aldecoa C, Bettelli G, Bilotta F, Sanders RD, Audisio R, Borozdina A, et al. European society of anaesthesiology evidence-based and consensus-based guideline on postoperative delirium. Eur J Anaesthesiol. (2017) 34:192–214. doi: 10.1097/eja.0000000000000594
9. Lu Z, Dong H, Wang Q, Xiong L. Perioperative acupuncture modulation: more than anaesthesia. Br J Anaesth. (2015) 115:183–93. doi: 10.1093/bja/aev227
10. Ho YS, Zhao FY, Yeung WF, Wong GT, Zhang HQ, Chang RC. Application of acupuncture to attenuate immune responses and oxidative stress in postoperative cognitive dysfunction: what do we know so far? Oxid Med Cell Longev. (2020) 2020:9641904. doi: 10.1155/2020/9641904
11. Garland SN, Xie SX, DuHamel K, Bao T, Li Q, Barg FK, et al. Acupuncture versus cognitive behavioral therapy for insomnia in cancer survivors: a randomized clinical trial. J Natl Cancer Inst. (2019) 111:1323–31. doi: 10.1093/jnci/djz050
12. Gao F, Zhang Q, Li Y, Tai Y, Xin X, Wang X, et al. Transcutaneous electrical acupoint stimulation for prevention of postoperative delirium in geriatric patients with silent lacunar infarction: a preliminary study. Clin Interv Aging. (2018) 13:2127–34. doi: 10.2147/cia.s183698
13. Coura LEF, Manoel CHU, Poffo R, Bedin A, Westphal GA. Randomised, controlled study of preoperative eletroacupuncture for postoperative pain control after cardiac surgery. Acupunct Med. (2011) 29:16–20. doi: 10.1136/aim.2010.003251
14. Ely EW, Inouye SK, Bernard GR, Gordon S, Francis J, May L, et al. Delirium in mechanically ventilated patients: validity and reliability of the confusion assessment method for the intensive care unit (CAM-ICU). JAMA. (2001) 286:2703–10. doi: 10.1001/jama.286.21.2703
15. Robinson TN, Raeburn CD, Tran ZV, Angles EM, Brenner LA, Moss M. Postoperative delirium in the elderly: risk factors and outcomes. Ann Surg. (2009) 249:173–8. doi: 10.1097/SLA.0b013e31818e4776
16. Kuo SY, Tsai SH, Chen SL, Tzeng YL. Auricular acupressure relieves anxiety and fatigue, and reduces cortisol levels in post-caesarean section women: a single-blind, randomised controlled study. Int J Nurs Stud. (2016) 53:17–26. doi: 10.1016/j.ijnurstu.2015.10.006
17. Arai YC, Ito A, Hibino S, Niwa S, Ueda W. Auricular acupunctures are effective for the prevention of postoperative agitation in old patients. Evid Based Complement Altern Med. (2010) 7:383–6. doi: 10.1093/ecam/nep172
18. Chung YC, Tsou MY, Chen HH, Lin JG, Yeh ML. Integrative acupoint stimulation to alleviate postoperative pain and morphine-related side effects: a sham-controlled study. Int J Nurs Stud. (2014) 51:370–8. doi: 10.1016/j.ijnurstu.2013.06.007
19. Zhang J, Qin Z, So TH, Chen H, Lam WL, Yam LL, et al. Electroacupuncture plus auricular acupressure for chemotherapy-associated insomnia in breast cancer patients: a pilot randomized controlled trial. Integr Cancer Ther. (2021) 20:15347354211019103. doi: 10.1177/15347354211019103
20. Deiner S, Luo X, Lin HM, Sessler DI, Saager L, Sieber FE, et al. Intraoperative infusion of dexmedetomidine for prevention of postoperative delirium and cognitive dysfunction in elderly patients undergoing major elective noncardiac surgery: a randomized clinical trial. JAMA Surg. (2017) 152:e171505. doi: 10.1001/jamasurg.2017.1505
21. Tao J, Zheng Y, Liu W, Yang S, Huang J, Xue X, et al. Electro-acupuncture at LI11 and ST36 acupoints exerts neuroprotective effects via reactive astrocyte proliferation after ischemia and reperfusion injury in rats. Brain Res Bull. (2016) 120:14–24. doi: 10.1016/j.brainresbull.2015.10.011
22. Wang H, Xie Y, Zhang Q, Xu N, Zhong H, Dong H, et al. Transcutaneous electric acupoint stimulation reduces intra-operative remifentanil consumption and alleviates postoperative side-effects in patients undergoing sinusotomy: a prospective, randomized, placebo-controlled trial. Br J Anaesth. (2014) 112:1075–82. doi: 10.1093/bja/aeu001
23. Suen LK, Wong TK, Leung AW. Effectiveness of auricular therapy on sleep promotion in the elderly. Am J Chin Med. (2002) 30:429–49. doi: 10.1142/s0192415x0200051x
24. Chen HY, Shi Y, Ng CS, Chan SM, Yung KK, Zhang QL. Auricular acupuncture treatment for insomnia: a systematic review. J Altern Complement Med. (2007) 13:669–76. doi: 10.1089/acm.2006.6400
25. Inouye SK, Leo-Summers L, Zhang Y, Bogardus ST Jr, Leslie DL, Agostini JV. A chart-based method for identification of delirium: validation compared with interviewer ratings using the confusion assessment method. J Am Geriatr Soc. (2005) 53:312–8. doi: 10.1111/j.1532-5415.2005.53120.x
26. Sessler CN, Gosnell MS, Grap MJ, Brophy GM, O’Neal PV, Keane KA, et al. The Richmond agitation-sedation scale: validity and reliability in adult intensive care unit patients. Am J Respir Crit Care Med. (2002) 166:1338–44. doi: 10.1164/rccm.2107138
27. Hansen N, Rediske AI. The locus coeruleus noradrenaline system in delirium. Front Aging Neurosci. (2021) 13:784356. doi: 10.3389/fnagi.2021.784356
28. Farmer AD, Strzelczyk A, Finisguerra A, Gourine AV, Gharabaghi A, Hasan A, et al. International consensus based review and recommendations for minimum reporting standards in research on transcutaneous vagus nerve stimulation (version 2020). Front Hum Neurosci. (2020) 14:568051. doi: 10.3389/fnhum.2020.568051
29. Butt MF, Albusoda A, Farmer AD, Aziz Q. The anatomical basis for transcutaneous auricular vagus nerve stimulation. J Anat. (2020) 236:588–611. doi: 10.1111/joa.13122
30. Daiello LA, Racine AM, Yun Gou R, Marcantonio ER, Xie Z, Kunze LJ, et al. Postoperative delirium and postoperative cognitive dysfunction: overlap and divergence. Anesthesiol. (2019) 131:477–91. doi: 10.1097/aln.0000000000002729
31. Kim YK, Park JY, Kim SN, Yeom M, Lee S, Oh JY, et al. What intrinsic factors influence responsiveness to acupuncture in pain: a review of pre-clinical studies that used responder analysis. BMC Compl Altern Med. (2017) 17:281. doi: 10.1186/s12906-017-1792-2
32. Morphy H, Dunn KM, Lewis M, Boardman HF, Croft PR. Epidemiology of insomnia: a longitudinal study in a UK population. Sleep. (2007) 30:274–80.
33. Lu Y, Li YW, Wang L, Lydic R, Baghdoyan HA, Shi XY, et al. Promoting sleep and circadian health may prevent postoperative delirium: a systematic review and meta-analysis of randomized clinical trials. Sleep Med Rev. (2019) 48:101207. doi: 10.1016/j.smrv.2019.08.001
34. Huang S, Peng W, Tian X, Liang H, Jia Z, Lo T, et al. Effects of transcutaneous electrical acupoint stimulation at different frequencies on perioperative anesthetic dosage, recovery, complications, and prognosis in video-assisted thoracic surgical lobectomy: a randomized, double-blinded, placebo-controlled trial. J Anesth. (2017) 31:58–65. doi: 10.1007/s00540-015-2057-1
35. Asmussen S, Przkora R, Maybauer DM, Fraser JF, Sanfilippo F, Jennings K, et al. Meta-analysis of electroacupuncture in cardiac anesthesia and intensive care. J Intens Care Med. (2019) 34:652–61. doi: 10.1177/0885066617708558
36. Hmwe NTT, Browne G, Mollart L, Allanson V, Chan SW. An integrative review of acupressure interventions for older people: a focus on sleep quality, depression, anxiety, and agitation. Int J Geriatr Psychiatry. (2019) 34:381–96. doi: 10.1002/gps.5031
37. Hou P-W, Hsu H-C, Lin Y-W, Tang N-Y, Cheng C-Y, Hsieh C-L. The history, mechanism, and clinical application of auricular therapy in traditional chinese medicine. Evid Based Complement Altern Med. (2015) 2015:495684. doi: 10.1155/2015/495684
38. Krewulak KD, Hiploylee C, Ely EW, Stelfox HT, Inouye SK, Fiest KM. Adaptation and validation of a chart-based delirium detection tool for the ICU (CHART-DEL-ICU). J Am Geriatr Soc. (2021) 69:1027–34. doi: 10.1111/jgs.16987
39. Watne LO, Torbergsen AC, Conroy S, Engedal K, Frihagen F, Hjorthaug GA, et al. The effect of a pre- and postoperative orthogeriatric service on cognitive function in patients with hip fracture: randomized controlled trial (oslo orthogeriatric trial). BMC Med. (2014) 12:63. doi: 10.1186/1741-7015-12-63
40. Zhuang L, Yang Y, Gao J. Cognitive assessment tools for mild cognitive impairment screening. J Neurol. (2021) 268:1615–22. doi: 10.1007/s00415-019-09506-7
Keywords: transcutaneous electric acupoint stimulation, auricular acupressure, elderly, abdominal surgery, delirium
Citation: Fan Q, Lei C, Wang Y, Yu N, Wang L, Fu J, Dong H, Lu Z and Xiong L (2022) Transcutaneous Electrical Acupoint Stimulation Combined With Auricular Acupressure Reduces Postoperative Delirium Among Elderly Patients Following Major Abdominal Surgery: A Randomized Clinical Trial. Front. Med. 9:855296. doi: 10.3389/fmed.2022.855296
Received: 15 January 2022; Accepted: 16 May 2022;
Published: 15 June 2022.
Edited by:
Vincenza Frisardi, Santa Maria Nuova Hospital, ItalyReviewed by:
Niels Hansen, University Medical Center Göettingen, GermanyJiaqiang Zhang, Zhengzhou University, China
Copyright © 2022 Fan, Lei, Wang, Yu, Wang, Fu, Dong, Lu and Xiong. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chong Lei, Y3J5c3RhbGxlaWNob25nQDEyNi5jb20=; Lize Xiong, bXpreGx6QDEyNi5jb20=
 Qianqian Fan
Qianqian Fan Chong Lei
Chong Lei Yonghui Wang
Yonghui Wang Nannan Yu
Nannan Yu Lini Wang
Lini Wang Jingwen Fu
Jingwen Fu Hailong Dong
Hailong Dong Zhihong Lu
Zhihong Lu Lize Xiong
Lize Xiong