- 1Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, China Medical University Hospital, Taichung, Taiwan
- 2School of Medicine, China Medical University, Taichung, Taiwan
- 3Management Office for Health Data, China Medical University Hospital, Taichung, Taiwan
- 4Intensive Care Unit, Chu Shang Show Chwan Hospital, Nantou, Taiwan
Background: Respiratory system infections commonly occur among individuals with asthma. However, whether asthma patients have a higher risk of pleural empyema development remains unclear.
Methods: This is a retrospective cohort study based on data from the National Health Insurance Research Database of Taiwan. The asthma cohort consisted of 48,360 newly diagnosed adult individuals from 2000 to 2012. The comparison cohort consisted of the same number of adults who did not have asthma and was matched for age, gender, comorbidity, and the year of diagnosis. The development of pleural empyema was followed up to 2013.
Results: Pleural empyema incidence was 2.03-fold higher in the asthma cohort compared to the comparison cohort (8.65 vs. 4.25 per 10,000 person-years), with an adjusted hazard ratio (HR) of 2.12 [95% confidence interval (CI) = 1.76–2.56]. Stratified analyses by age, gender, comorbidity, and corticosteroid use revealed that the crude and adjusted HRs of pleural empyema associated with asthma were all significant. Among patients with asthma, the risk of pleural empyema elevated with increased frequency of annual asthma-related emergency room visits and hospital admissions (≥1 vs. <1, aHR = 8.07, 95% CI = 4.31–15.1 and aHR = 9.31, 95% CI = 5.56–15.6).
Conclusion: An increased risk of pleural empyema occurrence was observed in adult patients with asthma than those without asthma. Furthermore, the risk of pleural empyema may increase with poor control of asthma.
Introduction
Asthma is a heterogeneous disease manifesting with airway inflammation (1). This disease is defined by the presence of respiratory symptoms that vary over time and in intensity, together with variable expiratory airflow limitation (2). Inadequate control of asthma may lead to frequent exacerbations, worse health status, and poor quality of life (3). Asthma is also found to be associated with respiratory system infections, but information on the underlying mechanism of this predisposition is limited (4). Altered epithelial microenvironment and impaired immune function may contribute to the susceptibility of respiratory system infections (5, 6).
Pleural empyema indicates the occurrence of frank pus within the pleural space (7). It is most commonly caused by respiratory system infections, such as pneumonia (8). Mortality rate among individuals having pneumonia with pleural empyema is far higher than in patients who do not have pleural empyema (9, 10). The crucial nature of pleural empyema and the need for removal have been identified for several centuries (11). Delayed diagnosis and poor drainage have been found to be linked with high mortality (12). Alcohol consumption, substance use, diabetes mellitus, immunosuppression, malignancy, pulmonary disease, and prior occurrence of pleural effusion are predictors of the development of pleural empyema (13, 14).
Several studies have investigated the association between asthma and respiratory system infections (15–18). However, the studies did not examine the incidence of pleural empyema in asthma patients. Pleural empyema is a noticeable infection of the respiratory system and requires timely treatments, such as antibiotic therapy, pleural drainage, intrapleural fibrinolysis, and surgery. Thus, investigating the risk of pleural empyema in patients with asthma is necessary. This study aimed to examine whether patients with asthma have a higher risk of pleural empyema development. In addition, we attempted to assess the effect of asthma control on the occurrence of pleural empyema.
Materials and Methods
Data Source
The Taiwan National Health Insurance (NHI) program was established in 1995. The National Health Insurance Research Database (NHIRD) is a nationwide database housing medical claims data of over 99.5% of people living in Taiwan (https://nhird.nhri.org.tw/en/). The database is updated and maintained by the National Health Research Institutes. The Longitudinal Health Insurance Database 2000 (LHID2000, a subset data of NHIRD) was used for this study. The database contains medical claims data of one million persons randomly selected from users registered in 2000. Data on their demographic characteristics, diagnostic codes, procedure claims, and medication claims were available from 1995 to 2013. All data were deidentified to protect their privacy; therefore, written informed consent from the participants involved was unnecessary. This study was approved by the Research Ethics Committee of the China Medical University and Hospital (CMUH-104-REC2-115).
Study Cohorts
Patients with newly diagnosed asthma [International Classification of Disease, 9th Revision, Clinical Modification (ICD-9-CM) code 493 and asthma medication (bronchodilator or corticosteroid)] from January 1, 2000, to December 31, 2012, were selected in the asthma cohort. The date of the diagnosis was defined as the index date. Individuals with a diagnosis of pleural empyema before the index date and those with incomplete data were excluded from the analysis. The individuals in the comparison cohort included people free from asthma. The exclusion criteria for the comparison cohort were the same as for the asthma cohort. The comparison cohort was 1:1 frequency-matched with the asthma cohort by age, gender, comorbidity, and index year. All subjects were monitored until any of the following occurred: (1) development of pleural empyema, (2) withdrawal from NHI system, (3) death, and (4) the date of 31st of December 2013.
Outcome and Variables
All diseases were recorded in accordance with the ICD-9-CM in the NHIRD. The primary outcome was pleural empyema (based on ICD-9-CM code 510 and related antibiotic treatment). We also determined the related baseline comorbidities between 1995 and index date, including chronic obstructive pulmonary disease (COPD, ICD-9-CM code 496), diabetes mellitus (ICD-9-CM code 250), chronic kidney disease (CKD, ICD-9-CM code 585), chronic liver disease and cirrhosis (CLD, ICD-9-CM code 571), rheumatic disease (ICD-9-CM codes 446.5, 710.0–710.4, 714.0–714.2, 714.8, and 725), stroke (ICD-9-CM codes 433–438), cancer (ICD-9-CM codes 140–209), and malnutrition (ICD-9-CM codes 260–269). We selected only diagnoses from the outpatient department that appeared at least twice within 1 year or had a diagnosis of hospitalization to increase the accuracy for asthma, pleural empyema, and all comorbidities. In addition, we evaluated the related medication, corticosteroid use.
Statistical Analysis
We used the Chi-squared test to examine the proportion distribution of age group, gender, comorbidity, and medication between asthma and comparison cohorts. The means of age in the two cohorts were compared using a student's t-test. The estimation of cumulative incidence of pleural empyema in asthma and comparison cohorts was performed by the Kaplan–Meier method. A log-rank test was utilized to determine the significance. The incidence rates of pleural empyema were calculated by asthma, age group, gender, comorbidities, and medication. Univariable and multivariable Cox proportional hazard regression models were used to estimate hazard ratios (HRs) and 95% confidence intervals (CIs). Moreover, we calculated the incidence rates and relative risk of pleural empyema by stratification with age, gender, comorbidities, and medication between asthma and comparison cohorts. Among patients with asthma, we further evaluated the impact of the annual number of asthma-related emergency room visits and hospital admissions and cumulative corticosteroid doses on pleural empyema development. Data analysis was performed with the SAS statistical software (Version 9.4 for Windows; SAS Institute, Inc., Cary, NC, USA). Statistical significance was considered at a p-value < 0.05.
Results
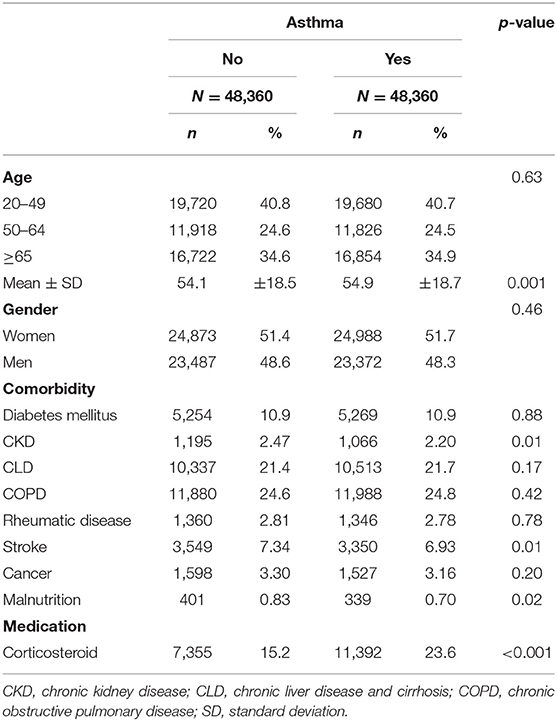
We recruited an asthma group comprising 48,360 patients and a comparator group of 48,360 individuals (Table 1). Age and gender did not significantly differ between asthma and comparator group. The mean age ± standard division of asthma and comparator group was 54.9 ± 18.7 and 54.1 ± 18.5 years, respectively. Approximately 52% of the individuals were women in both groups. The major comorbidities of the asthma group were COPD (24.8%), CLD (21.7%), followed by diabetes mellitus (10.9%), stroke (6.93%), and cancer (3.16%). The mean follow-up periods were 7.72 ± 4.15 years in the asthma group and 8.03 ± 4.02 years in the comparator group. The proportion of corticosteroid use were 23.6% in the asthma group and 15.2% in the comparator group. Figure 1 showed that patients with asthma had a higher cumulative incidence of pleural empyema than individuals without asthma throughout the 14-year study period.
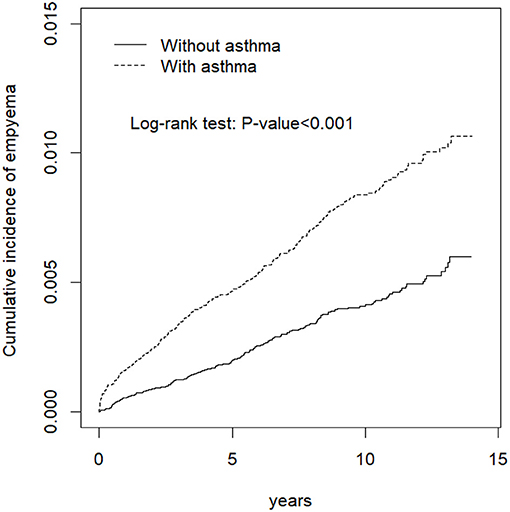
Figure 1. Cumulative incidence of pleural empyema in the asthma group (dashed line) and in the comparison group (solid line).
The overall incidence density rates of pleural empyema were 8.65 and 4.25 per 10,000 person-years in asthma and comparator groups, respectively (Table 2). Compared with the comparator group, the corresponding adjusted HR (aHR) of pleural empyema was 2.12 (95% CI = 1.76–2.56) in the asthma group after adjusting for age, gender, COPD, diabetes mellitus, CKD, CLD, stroke, cancer, and corticosteroid use. Compared with persons aged 20–49, the aHRs of pleural empyema were 2.43-fold higher in those aged 50–64 (95% CI = 1.80–3.29) and 4.10-fold higher in those aged ≥65 (95% CI = 3.09–5.44). The aHR of pleural empyema was 2.55-fold higher for men relative to women (95% CI = 2.09–3.12). Moreover, the risk of pleural empyema was higher in persons with stroke (aHR = 2.68, 95% CI = 2.12–3.38), diabetes mellitus (aHR = 1.86, 95% CI = 1.50–2.31), and COPD (aHR = 1.48, 95% CI = 1.22–1.79) compared with subjects without these comorbidities.
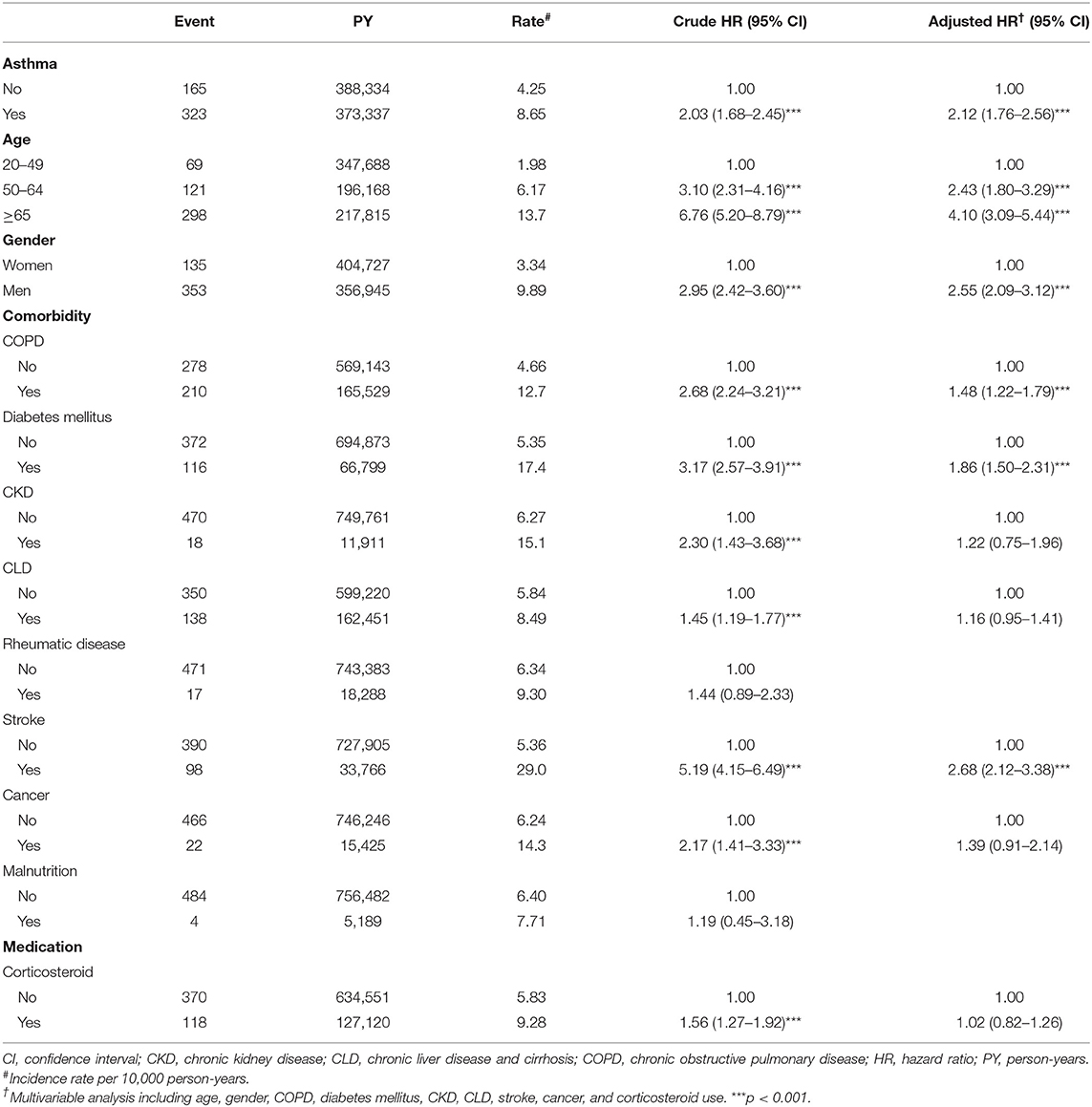
Table 2. Incidences and hazard ratios of pleural empyema by asthma, age, gender, comorbidity, and corticosteroid use among all participants.
Further analyses revealed that the incidences and aHRs of pleural empyema for the asthma group were all significantly higher compared with the comparator group after stratification for age, gender, presence of comorbidities, and corticosteroid use (Table 3). In addition, we assessed the impact of the frequency of asthma-related emergency room visits and hospital admissions on the development of pleural empyema among the asthma group (Table 4). A higher frequency of annual asthma-related emergency room visits and hospital admissions raised the risk of pleural empyema development (both p for trend <0.001). Moreover, we analyzed cumulative corticosteroid doses on pleural empyema development among the asthma group (Table 4). The incidence of pleural empyema was higher in those with corticosteroid use; however, the p value for trend was not significant (p = 0.25).
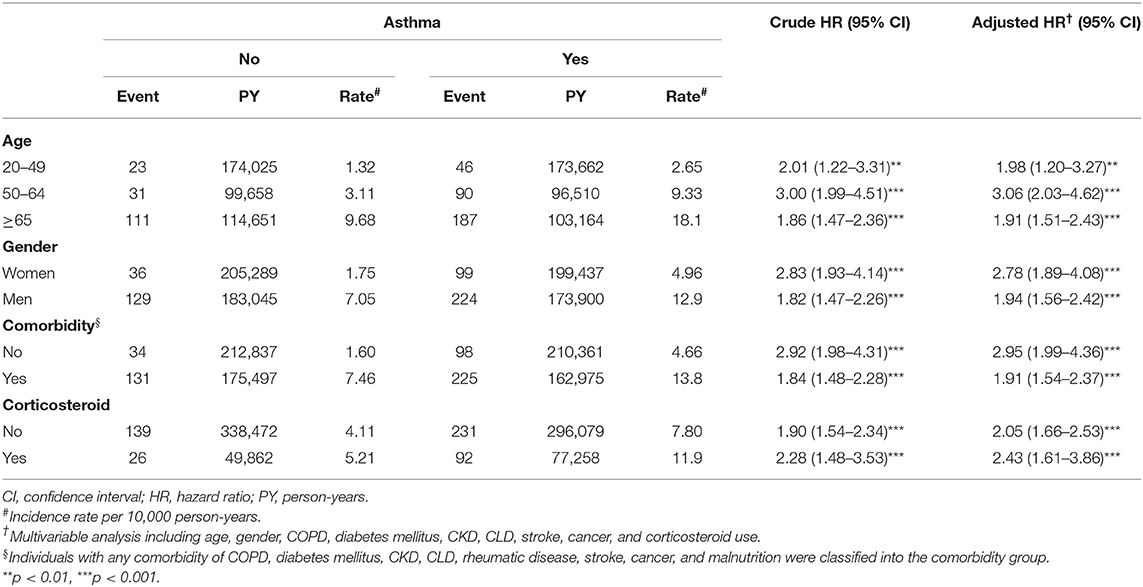
Table 3. Incidences and hazard ratios of pleural empyema by age, gender, comorbidity, and corticosteroid use between asthma and non-asthma cohorts.
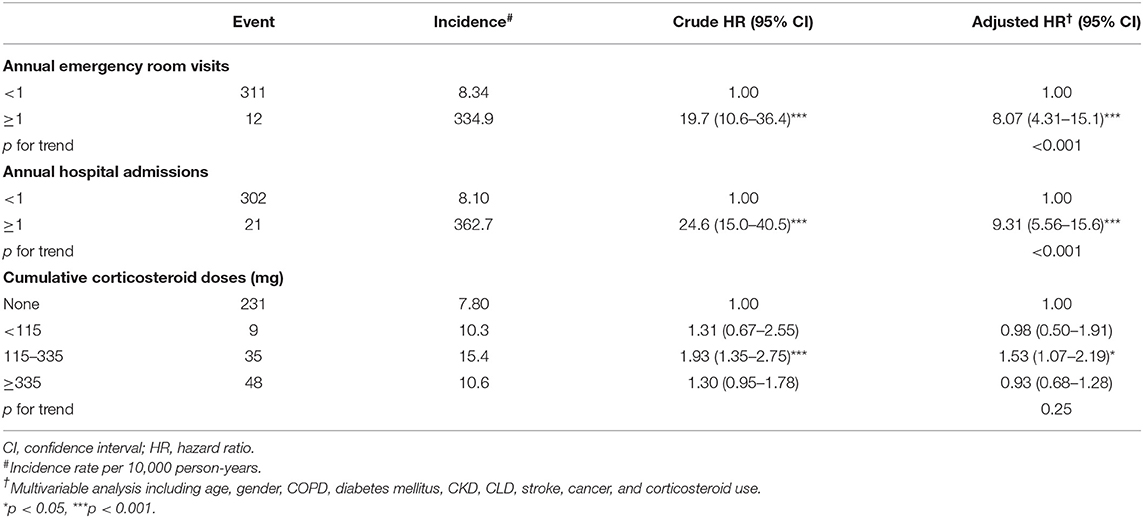
Table 4. Incidences and hazard ratios of pleural empyema by emergency room visits, hospital admissions, and cumulative corticosteroid doses among asthma cohort.
Discussion
We believed that this investigation is the first population-based retrospective cohort study to evaluate the incidence of pleural empyema in patients with asthma. Our findings revealed that patients with asthma have a significantly higher risk of developing pleural empyema than those without asthma. The risk of pleural empyema was also larger in older people, in males, those with comorbidities. Furthermore, the hazards of pleural empyema were significantly larger in the asthma cohort compared with the comparison cohort under stratification by age, gender, comorbidity, and corticosteroid use. Moreover, we found that the risk of pleural empyema was higher in asthma patients with an increased number of asthma-related emergency medical demands and hospital admissions, indicating that the level of asthma control may influence the occurrence of pleural empyema.
The mechanism between asthma and pleural empyema remains largely unknown. Patients with asthma who are susceptible to pneumonia may still play a major role. This condition may be driven by the following: (1) a large prevalence of carriage of the bacteria, (2) a disordered immune response from exposure to the bacteria, (3) impaired bacterial clearance, and (4) a suboptimal response to vaccination (5). Parapneumonic pleural effusions are known to represent a common complication of pneumonia and can be found in approximately 40% of bacterial pneumonia cases (11). In addition, inhaled or systemic corticosteroid use, shared comorbidities, cigarette smoking, alcohol consumption, unhealthy lifestyle, poor self-care, and poor physical health are commonly noted among asthma patients. These factors are also related to the development of pneumonia and pleural empyema (9).
Inconsistent evidence was found between chronic inflammatory airway disease and the development of pleural empyema. Lu et al. (19) conducted a case-control study to evaluate the potential risk factors of pleural empyema. They enrolled 1,851 pleural empyema cases and 7,404 non-empyema controls and found significant factors that lead to pleural empyema include the following: aspiration history [odds ratio (OR) = 7.28, 95% CI = 5.00–10.6)], human immunodeficiency virus infection (OR = 5.66, 95% CI = 1.38–23.2), malnutrition (OR = 2.86, 95% CI = 2.07–3.95), cancer (OR = 2.74, 95% CI = 2.28–3.30), diabetes mellitus (OR = 2.25, 95% CI = 1.96–2.59), stroke (OR = 1.99, 95% CI = 1.70–2.34), CKD (OR = 1.78, 95% CI = 1.42–2.25), chronic obstructive pulmonary disease (COPD, OR = 1.72, 95% CI = 1.47–2.01), asthma (OR = 1.34, 95% CI = 1.15–1.57), and CLD (OR = 1.20, 95% CI = 1.06–1.35). In another study, Lu et al. evaluated COPD and the subsequent development of pleural empyema (20). They enrolled 55,136 COPD cases and 98,769 non-COPD controls and found that the incidence of pleural empyema was 3.64-fold higher in the COPD cohort than in the comparison cohort (15.8 vs. 4.34 per 10,000 person-years), with a corresponding aHR of 3.25 (95% CI = 2.73–3.87). These findings may suggest that chronic inflammatory airway disease may contribute to the development of pleural empyema. By contrast, Dusemund et al. (21) performed a case-control study in Switzerland to investigate outcomes of community-acquired pneumonia in patients with chronic lung disease. They found that the incidence of pleural empyema was insignificant in asthma [0.5% (asthma) vs. 0.9% (controls), p = 0.141] and COPD [0.5% (COPD) vs. 0.5% (controls), p = 0.817]. In addition, Elemraid et al. (22) assessed predictors of pleural empyema development in children. They found that age, sex, mother's age, smoking among the child's parents, poverty, nursery attendance, asthma, and household characteristics (bedrooms and number of occupants) were not significantly related. Therefore, we may need additional investigations to clarify this issue.
Strength
The strength of this study lies in the establishment of a population-based asthma cohort to assess the risk of developing pleural empyema. Conducting a prospective cohort study is expensive. Therefore, a retrospective cohort study based on insurance claims data may be a suitable and economical alternative. Regardless of socioeconomic background and/or residential location, the universal coverage by the NHI program lowers access barriers to health care all citizens (23). This study was able to reflect a “real world” scenario in which asthma, pleural empyema, and comorbidities were assessed during medical evaluation.
Limitation
Several limitations exist and need to be considered in interpreting the study findings. First, the ICD-9-CM algorithm was used to define asthma, pleural empyema, and comorbidities. All diagnoses were dependent on the competence of clinical physicians in diagnosing; however, asthma has been carefully validated in the NHIRD (24). In addition, an ad hoc committee established by the insurance authority monitored the evaluation of claims data to prevent errors and violations. We selected only diagnoses from the outpatient department that appeared at least twice within 1 year or had a diagnosis of hospitalization to increase the accuracy. In addition, we applied the medication used to improve the diagnosis of asthma and empyema. Second, the NHIRD does not provide detailed information regarding smoking habits, drinking habits, and other environmental factors, which are potentially confounding factors in the current study. In addition, relevant clinical variables, such as serum laboratory data, image reports, and culture results, were unavailable in the database.
Conclusion
An increased risk of pleural empyema occurrence was observed in adult patients with asthma compared to those without asthma. Furthermore, the risk of pleural empyema may increase with the degree of asthma control.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author Contributions
W-CL, T-CS, C-YT, T-CH, and W-HH: conception and design. C-YT, T-CH, and W-HH: administrative support. W-CL, C-LL, and T-CS: collection and assembly of data and data analysis and interpretation. All authors: manuscript writing and final approval of manuscript.
Funding
This study was supported by China Medical University Hospital (DMR-110-033).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Borish L, Culp JA. Asthma: a syndrome composed of heterogeneous diseases. Ann Allergy Asthma Immunol. (2008) 101:1–8. doi: 10.1016/S1081-1206(10)60826-5
2. Menzies-Gow A, McBrien CN, Baker JR, Donnelly LE, Cohen RT. Update in asthma and airway inflammation 2018. Am J Respir Crit Care Med. (2019) 200:14–9. doi: 10.1164/rccm.201902-0321UP
3. Stanescu S, Kirby SE, Thomas M, Yardley L, Ainsworth B. A systematic review of psychological, physical health factors, and quality of life in adult asthma. NPJ Prim Care Respir Med. (2019) 29:37. doi: 10.1038/s41533-019-0149-3
4. Tracy MC, Mathew R. Complicated pneumonia: current concepts and state of the art. Curr Opin Pediatr. (2018) 30:384–92. doi: 10.1097/MOP.0000000000000619
5. Zaidi SR, Blakey JD. Why are people with asthma susceptible to pneumonia? a review of factors related to upper airway bacteria. Respirology. (2019) 24:423–30. doi: 10.1111/resp.13528
6. Christou EAA, Giardino G, Stefanaki E, Ladomenou F. Asthma: an undermined state of immunodeficiency. Int Rev Immunol. (2019) 38:70–8. doi: 10.1080/08830185.2019.1588267
7. Redden MD, Chin TY, van Driel ML. Surgical versus non-surgical management for pleural empyema. Cochrane Database Syst Rev. (2017) 3:CD010651. doi: 10.1002/14651858.CD010651.pub2
8. Bedawi EO, Hassan M, Rahman NM. Recent developments in the management of pleural infection: a comprehensive review. Clin Respir J. (2018) 12:2309–20. doi: 10.1111/crj.12941
9. Hasley PB, Albaum MN, Li YH, Fuhrman CR, Britton CA, Marrie TJ, et al. Do pulmonary radiographic findings at presentation predict mortality in patients with community-acquired pneumonia? Arch Intern Med. (1996) 156:2206–12. doi: 10.1001/archinte.156.19.2206
10. Menéndez R, Torres A, Zalacaín R, Aspa J, Martín Villasclaras JJ, Borderías L, et al. Risk factors of treatment failure in community acquired pneumonia: implications for disease outcome. Thorax. (2004) 59:960–5. doi: 10.1136/thx.2003.017756
11. Feller-Kopman D, Light R. Pleural disease. N Engl J Med. (2018) 378:740–51. doi: 10.1056/NEJMra1403503
12. Ashbaugh DG. Empyema thoracis. factors influencing morbidity and mortality. Chest. (1991) 99:1162–5. doi: 10.1378/chest.99.5.1162
13. Strange C, Sahn SA. The definitions and epidemiology of pleural space infection. Semin Respir Infect. (1999) 14:3–8.
14. Sahn SA. Diagnosis and management of parapneumonic effusions and empyema. Clin Infect Dis. (2007) 45:1480–6. doi: 10.1086/522996
15. Talbot TR, Hartert TV, Mitchel E, Halasa NB, Arbogast PG, Poehling KA, et al. Asthma as a risk factor for invasive pneumococcal disease. N Engl J Med. (2005) 352:2082–90. doi: 10.1056/NEJMoa044113
16. Juhn YJ, Kita H, Yawn BP, Boyce TG, Yoo KH, McGree ME, et al. Increased risk of serious pneumococcal disease in patients with asthma. J Allergy Clin Immunol. (2008) 122:719–23. doi: 10.1016/j.jaci.2008.07.029
17. Klemets P, Lyytikainen O, Ruutu P, Ollgren J, Kaijalainen T, Leinonen M, et al. Risk of invasive pneumococcal infections among working age adults with asthma. Thorax. (2010) 65:698–702. doi: 10.1136/thx.2009.132670
18. Almirall J, Serra-Prat M, Bolíbar I, Balasso V. Risk factors for community-acquired pneumonia in adults: a systematic review of observational studies. Respiration. (2017) 94:299–311. doi: 10.1159/000479089
19. Lu TC, Shen TC, Lin CL, Yen CC, Wu HS. Risk factors of empyema and their impacts on the prognosis in Taiwan. J Intern Med Taiwan. (2020) 31:276–83. doi: 10.6314/JIMT.202008_31(4).08
20. Lu HY, Liao KM. Risk of empyema in patients with COPD. Int J Chron Obstruct Pulmon Dis. (2018) 13:317–24. doi: 10.2147/COPD.S149835
21. Dusemund F, Chronis J, Baty F, Albrich WC, Brutsche MH. The outcome of community-acquired pneumonia in patients with chronic lung disease: a case-control study. Swiss Med Wkly. (2014) 144:w14013. doi: 10.4414/smw.2014.14013
22. Elemraid MA, Thomas MF, Blain AP, Rushton SP, Spencer DA, Gennery AR, et al. Risk factors for the development of pleural empyema in children. Pediatr Pulmonol. (2015) 50:721–6. doi: 10.1002/ppul.23041
23. Hsing AW, Ioannidis JP. Nationwide population science: lessons from the Taiwan national health insurance research database. JAMA Intern Med. (2015) 175:1527–9. doi: 10.1001/jamainternmed.2015.3540
Keywords: empyema, asthma, pneumonia, cohort study, retrospective study
Citation: Liao W-C, Lin C-L, Shen T-C, Tu C-Y, Hsia T-C and Hsu W-H (2022) Risk of Pleural Empyema in Adult Patients With Asthma: A Nationwide Retrospective Cohort Study. Front. Med. 9:851573. doi: 10.3389/fmed.2022.851573
Received: 10 January 2022; Accepted: 14 March 2022;
Published: 04 April 2022.
Edited by:
Laurent Pierre Nicod, University of Lausanne, SwitzerlandReviewed by:
Kuang-Ming Liao, Chi Mei Medical Center, TaiwanChin Kook Rhee, The Catholic University of Korea, South Korea
Copyright © 2022 Liao, Lin, Shen, Tu, Hsia and Hsu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Te-Chun Shen, Y2hlc3RzaGVuQGdtYWlsLmNvbQ==
 Wei-Chih Liao
Wei-Chih Liao Cheng-Li Lin
Cheng-Li Lin Te-Chun Shen
Te-Chun Shen Chih-Yen Tu1,2
Chih-Yen Tu1,2 Wu-Huei Hsu
Wu-Huei Hsu