
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
BRIEF RESEARCH REPORT article
Front. Med., 21 February 2022
Sec. Infectious Diseases – Surveillance, Prevention and Treatment
Volume 9 - 2022 | https://doi.org/10.3389/fmed.2022.837411
This article is part of the Research TopicEmerging SARS-COV-2 Variants: Genomic Variations, Transmission, Pathogenesis, Clinical Impact and InterventionsView all 65 articles
Studies have discovered that wild-type SARS-CoV-2 infections are commonly linked to abnormalities in the hematological profiles of COVID-19 patients, one such abnormality being characterized by elevations in red blood cell distribution width (RDW). Whether this linkage reoccurs in delta variant SARS-CoV-2 infection remains unexamined. Here we compared baseline blood parameters in COVID-19 patients infected by wild type and its delta variant, respectively. Our results here point to that although the delta variant has shown increased virulence, transmissibility, and vaccine escape, it has a minimally negative impact on RDW values that were previously found prognostic for COVID-19 severity.
Twenty-one months into the coronavirus disease 2019 (COVID-19) pandemic, the world still faces the rolling waves of viral hits as public health systems have been continuously stressed by this devastating disease. According to the World Health Organization (WHO) epidemiological report, as of December 5, 2021, the confirmed cases of COVID-19 infections have exceeded 264 million, with a cumulative death toll of over 5 million (1). Insofar a dozen variants of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) have been identified, including the predominant delta variant and the upsurging omicron (1). In the latest coronavirus flare-ups, rapid spreading of SARS-CoV-2 in the form of delta variant has placed several cities in China under local lockdown, including Nanjing and Yangzhou in Jiangsu Province.
Red blood cell (RBC) distribution width (RDW) measures the heterogeneity of erythrocyte volumes, as abnormally elevated RDW values indicate anisocytosis of RBCs in circulation, being prognostic in a wide spectrum of human disorders (septic infection, cardiovascular diseases, cancers, etc.) and all-cause mortality (2). Recently, heightened RDW upon hospitalization was found in a close association with increased mortality for COVID-19 patients (3–5). Nevertheless, whether the RDW value upon hospital admission can predict the severity and mortality of delta variant SARS-CoV-2 infection remains unexplored.
We here report a total of 677 COVID-19 patients admitted at separate centers in China, where a cohort of 341 patients was hospitalized in Wuhan, Hubei Province during January-April 2020, and a cohort of 336 patients was hospitalized in Yangzhou, Jiangsu Province on August 2021 where the infections were identified to be caused by delta variant of SARS-CoV-2 (6). Clinical characteristics centered on RBC features were elaborated and compared between two cohorts of COVID-19 patients, to distinguish its delta variant from wild-type SARS-CoV-2 in their infection profiles. Details regarding the patient procedure, vaccination status, and statistical analysis can be found in Supplementary Material.
Between the two cohorts, no difference was shown in the median age, gender ratio, and major comorbidities (7). Table 1 lists the baseline hematological parameters for COVID-19 patients admitted during the outbreak at Wuhan. Anemia was common, reflected by low RBC counts, and hemoglobin and hematocrits levels in more than half of the patients. Other RBC indices, including mean corpuscular volume (MCV), mean corpuscular hemoglobin (MCH), and mean corpuscular hemoglobin concentration (MCHC) showed abnormality in a moderate to substantial portion of patients. Particularly, RDW displayed raised levels in more than half of COVID-19 patients, demonstrating the augmented distortion in RBC morphology. All RBC characters (except MCV) were prognostic indicators for COVID-19 severity but not mortality, as their differences between intensive care unit (ICU) and non-ICU patients were statistically significant while there was no noticeable difference in RDW between deceased and survived patients in the ICU. This stands in agreement with our own and others' previous findings (8–10).
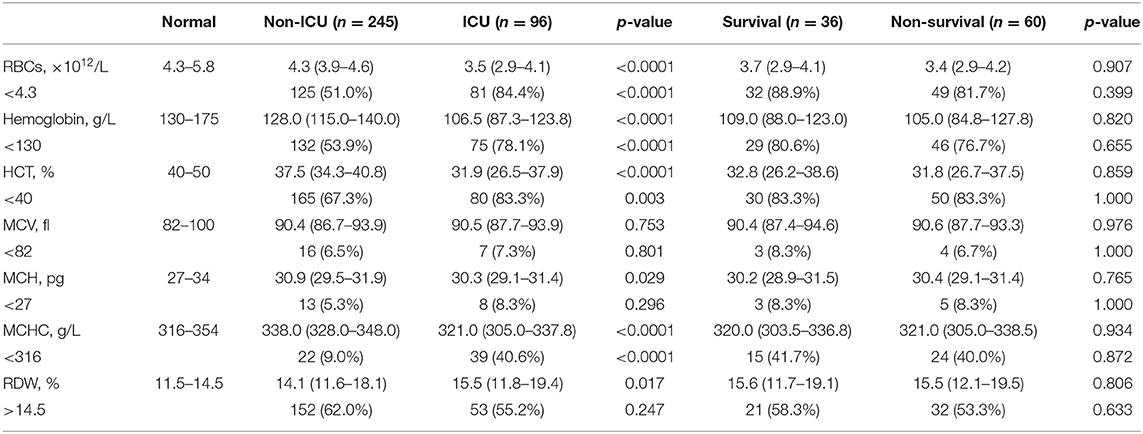
Table 1. Baseline hematological data were compared between non-ICU and ICU COVID-19 patients infected by wild-type SARS-CoV-2, and between survivors and non-survivors after transfer into ICU.
For COVID-19 patients admitted at Yangzhou, China in August 2021 (Table 2), the epidemiological investigation confirmed that their infections were due to the spreading of delta variant SARS-CoV-2 (6). Their hematological profiles were divided into groups of patients with no, partial (one-dose), and full (two-dose) vaccinations, and then unvaccinated delta variant COVID-19 patients in Yangzhou were compared to (unvaccinated) patients in Wuhan as well as the partially or fully vaccinated patients, respectively. Anemic conditions were ameliorated in delta variant SARS-CoV-2 infection, as RBC counts, hemoglobin, and hematocrit were substantially improved and the corresponding patient ratios with the abnormal values of the above parameters became significantly reduced. Other RBC indices showed a slight difference from those in COVID-19 patients in Wuhan. Notably, RDW exhibited markedly lowered values in delta variant infected patients at Yangzhou, where only a marginal portion (4.2%) of patients showed abnormally high values. Partial vaccination did not alleviate the anemia, but fully vaccinated patients demonstrated higher RBC counts and lower RDWs with significance, albeit the patient ratios with deranged hematological data showed no difference from those without vaccination.
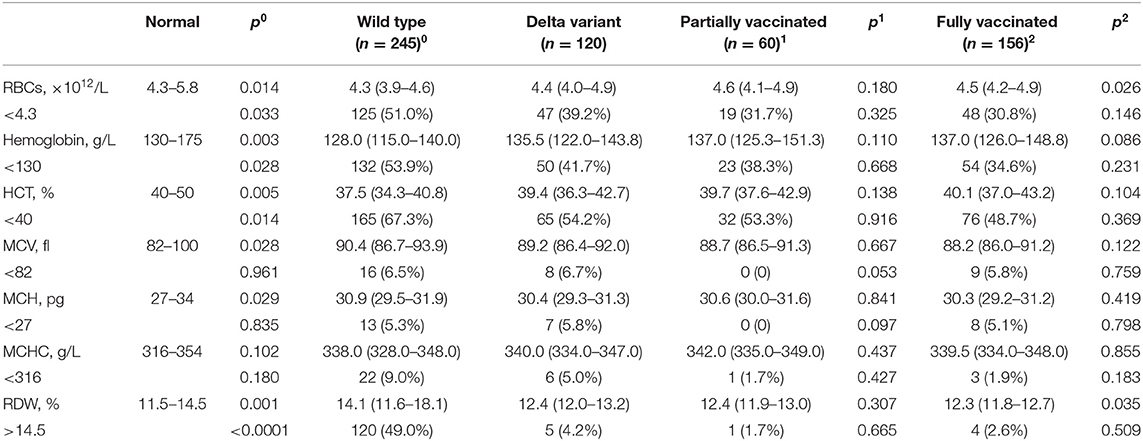
Table 2. Baseline hematological data were compared between unvaccinated COVID-19 patients infected by wild-type and delta variant SARS-CoV-2 (exhibited by p0 values) and between delta variant COVID-19 patients unvaccinated and partially vaccinated (exhibited by p1 values), and between delta variant COVID-19 patients unvaccinated and fully vaccinated patients (exhibited by p2 values).
This study is invalid to assess whether the deformed RBCs subject to COVID-19 infection were owing to the direct viral insults on erythrocytes or the indirect deterioration by triggered proinflammatory cytokines. Neither could our study validate if timely vaccinations protect patients from a blood infection. Of note, anemia in COVID-19 patients may partially result from iron deficiency in dietary supplements among Chinese adults, long before SARS-CoV-2 infection (11). Nevertheless, previous studies have revealed that elevated RDW in COVID-19 patients was related to the disease severity and mortality, especially in non-anemic patients (12). The result here suggested a lessened viremic effect of delta variant SARS-CoV-2 on RBCs, as the infected patients showed minimal alteration on RDW as an important index for COVID-19 hematological impact. Hence, unlike that in COVID-19 cases infected by wild-type SARS-CoV-2, RDW might not be a valid prognostic indicator of COVID-19 severity in delta variant SARS-CoV-2 infection, although this variant of concern still possesses increased virulence, transmissibility, and immune escape (13).
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by Research Ethics Commissions in the First People's Hospital of Jiangxia District (FPHJD) in Wuhan City of Hubei Province, China, and in the Third People's Hospital of Yangzhou City (TPHYC), Jiangsu Province, China. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
JZ and ZT conceived the idea and designed the study. JZ, JH, SF, DD, and ZT contributed to the data acquisition, processing, and table preparation. XH and ZT contributed to the statistical analysis. All authors contributed to the manuscript writing and approved the manuscript submission.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
We thank the financial support from Jiangsu University.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2022.837411/full#supplementary-material
COVID-19, Coronavirus disease 2019; ICU, intensive care unit; MCH, mean corpuscular hemoglobin; MCHC, mean corpuscular hemoglobin concentration; MCV, mean corpuscular volume; RBC, Red blood cell; RDW, Red blood cell distribution width; SARS-CoV-2, Severe acute respiratory syndrome coronavirus 2.
1. World Health Organization. COVID-19 Weekly Epidemiological Update, Edition 69, 7 December (2021).
2. Salvagno GL, Sanchis-Gomar F, Picanza A, Lippi G. Red blood cell distribution width: a simple parameter with multiple clinical applications. Crit Rev Clin Lab Sci. (2015) 52:86–105. doi: 10.3109/10408363.2014.992064
3. Foy BH, Carlson JCT, Reinertsen E, Padros IVR, Pallares Lopez R, Palanques-Tost E, et al. Association of red blood cell distribution width with mortality risk in hospitalized adults with SARS-CoV-2 infection. JAMA Netw Open. (2020) 3:e2022058. doi: 10.1001/jamanetworkopen.2020.22058
4. Karampitsakos T, Akinosoglou K, Papaioannou O, Panou V, Koromilias A, Bakakos P, et al. Increased red cell distribution width is associated with disease severity in hospitalized adults with SARS-CoV-2 infection: an observational multicentric study. Front Med. (2020) 7:616292. doi: 10.3389/fmed.2020.616292
5. Banon T, Wortsman J, Ben Moshe S, Gazit S, Peretz A, Ben Tov A, et al. Evaluating red blood cell distribution width from community blood tests as a predictor of hospitalization and mortality in adults with SARS-CoV-2: a cohort study. Ann Med. (2021) 53:1410–8. doi: 10.1080/07853890.2021.1968484
6. Zhou L, Nie K, Zhao H, Zhao X, Ye B, Wang J, et al. Eleven COVID-19 outbreaks with local transmissions caused by the imported SARS-CoV-2 delta VOC—China, July–August, 2021. China CDC Weekly. (2021) 3:863. doi: 10.46234/ccdcw2021.213
7. Hu Z, Huang X, Zhang J, Fu S, Ding D, Tao Z. Differences in clinical characteristics between delta variant and wild-type SARS-CoV-2 infected patients. Front Med. (2022) 8:792135. doi: 10.3389/fmed.2021.792135
8. Tao Z, Xu J, Chen W, Yang Z, Xu X, Liu L, et al. Anemia is associated with severe illness in COVID-19: a retrospective cohort study. J Med Virol. (2021) 93:1478–88. doi: 10.1002/jmv.26444
9. Zhang J, Huang X, Ding D, Tao Z. Platelet-driven coagulopathy in COVID-19 patients: in comparison to seasonal influenza cases. Exp Hematol Oncol. (2021) 10:34. doi: 10.1186/s40164-021-00228-z
10. Zhang J, Huang X, Ding D, Zhang J, Xu L, Hu Z, et al. Comparative study of acute lung injury in COVID-19 and non-COVID-19 patients. Front Med. (2021) 8:666629. doi: 10.3389/fmed.2021.666629
11. Shi Z, Zhou M, Yuan B, Qi L, Dai Y, Luo Y, et al. Iron intake and body iron stores, anaemia and risk of hyperglycaemia among Chinese adults: the prospective jiangsu nutrition study (JIN). Public Health Nutr. (2010) 13:1319–27. doi: 10.1017/S1368980009991868
12. Sarkar S, Kannan S, Khanna P, Singh AK. Role of red blood cell distribution width, as a prognostic indicator in COVID-19: A systematic review and meta-analysis. Rev Med Virol. (2021) 6:e2264. doi: 10.1002/rmv.2264
Keywords: COVID-19, SARS-CoV-2, delta variant, red blood cell distribution width, vaccination
Citation: Zhang J, Hu J, Huang X, Fu S, Ding D and Tao Z (2022) Association Between Red Blood Cell Distribution Width and COVID-19 Severity in Delta Variant SARS-CoV-2 Infection. Front. Med. 9:837411. doi: 10.3389/fmed.2022.837411
Received: 16 December 2021; Accepted: 17 January 2022;
Published: 21 February 2022.
Edited by:
Pragya Dhruv Yadav, National Institute of Virology (ICMR), IndiaReviewed by:
Vijay Tripathi, Sam Higginbottom University of Agriculture, Technology and Sciences, IndiaCopyright © 2022 Zhang, Hu, Huang, Fu, Ding and Tao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhimin Tao, anN1dGFvQHVqcy5lZHUuY24=
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.