- Department of Respiratory Medicine, Nagoya University Graduate School of Medicine, Nagoya, Japan
Because severe coronavirus disease 2019 (COVID-19) affects the respiratory system and develops into respiratory failure, patients with pre-existing chronic lung disorders, such as idiopathic pulmonary fibrosis (IPF), are thought to be at high risk of death. Patients with IPF often suffer from a lethal complication, acute exacerbation (AE), a significant part of which is assumed to be triggered by respiratory viral infection. However, whether mild to moderate COVID-19 can trigger AE in patients with IPF remains unknown. This is the case report of a 60-year-old man with a 4-year history of IPF who successfully recovered from moderate COVID-19 but subsequently developed more severe respiratory failure, which was considered to be a COVID-19-triggered acute exacerbation of idiopathic pulmonary fibrosis (AE-IPF). It is important to be aware of the risk of AE-IPF after COVID-19 and to properly manage this deadly complication of IPF. Recent literature reporting cases with chronic interstitial lung diseases which developed respiratory failure by complications with COVID-19 is also reviewed and discussed.
Introduction
Since its emergence in December 2019, more than five million patients have died of coronavirus disease 2019 (COVID-19) (1), which is caused by infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and manifests as acute respiratory failure in severe cases. Pre-existing chronic lung diseases have a significant impact on the clinical course and outcomes of patients with COVID-19 (2). Among those lung diseases, a significant increase in mortality due to COVID-19 has been reported in patients with idiopathic pulmonary fibrosis (IPF) (3). In particular, acute exacerbation (AE), a devastating complication of IPF (4), may be triggered by COVID-19 and can be one of the major causes of this elevated mortality. However, because severe COVID-19 and AE-IPF share many clinico-radiological features, it is not easy to distinguish these two diseases definitively, and there have been few reports clearly demonstrating the clinical course of AE-IPF induced by COVID-19.
We here present the clinical course of a case with pre-existing IPF presenting with COVID-19 that was successfully treated and recovered, but subsequently developed AE-IPF with severe and prolonged respiratory failure that was considered to be triggered by COVID-19. We believe it is important to understand the clinical course of this newly recognized trigger of AE-IPF in the era of the COVID-19 pandemic.
Case Presentation
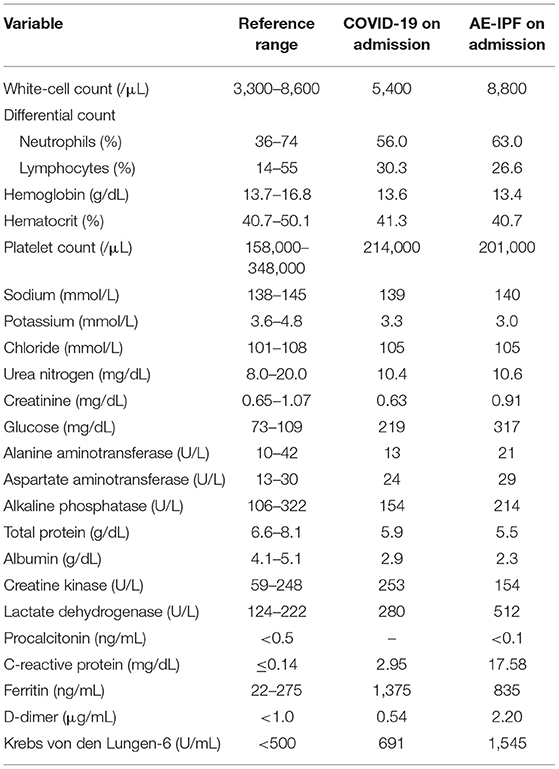
A 60-year-old Japanese man with a medical history of pulmonary tuberculosis, mild cerebral infarction, and type 2 diabetes mellitus presented at our hospital after 4 days of fever and pharyngeal discomfort. He had been diagnosed with IPF and treated with nintedanib for 4 years. He was not vaccinated against SARS-CoV-2. On presentation, he did not complain worsening dyspnea, cough, or sputum. On examination, his body temperature was 36.0°C, respiratory rate was 24/min, and oxygen saturation was 97% in room air, and he had not deteriorated since his last periodic visit. Compared to his baseline chest computed tomography (CT) (Figure 1A), that on admission demonstrated newly developed ground-glass opacities (GGOs) in the right middle and left upper lobes overlaying the pre-existing bilateral reticular abnormalities and honeycombing predominantly distributed in the subpleural area (Figure 1B). The real-time polymerase chain reaction (RT-PCR) test for SARS-CoV-2 performed on admission was positive. Blood test results are shown in Table 1. Based on a diagnosis of mild COVID-19, he was admitted to the hospital according to the governmental policy at that time and treatments for possible concomitant bacterial infection (ceftriaxone and azithromycin) were initiated. On day 6 of admission, dexamethasone and favipiravir were initiated because he had developed respiratory failure requiring 1 L/min of oxygen via a nasal cannula. His respiratory status gradually improved after the initiation of anti-COVID-19 treatment and supplemental oxygen was successfully withdrawn on day 16 of admission. After two negative salivary SARS-CoV-2 RT-PCR tests on consecutive days, he was ambulatory and discharged 22 days after admission. A chest CT scan taken just before discharge revealed that peripheral GGOs were mildly extended compared to the scan at admission (Figure 1C). Because his respiratory status was significantly improved, we considered this was due to delayed absorption of infiltrates.
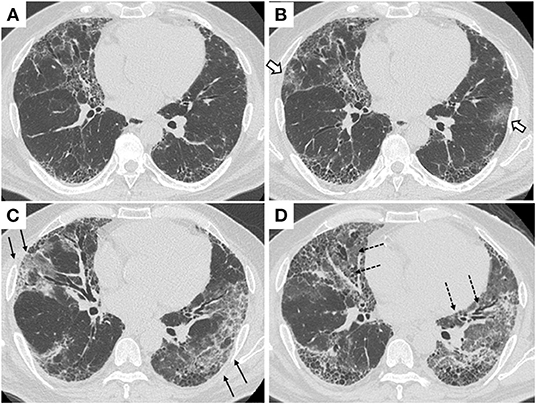
Figure 1. Chest CT scans. (A) On his last regular visit prior to the first admission. (B) On his first admission due to COVID-19. Open arrows indicate newly developed ground-glass opacities in the outer zones of both lungs. (C) On day 15 of his first admission, just before discharge. Arrows indicate ground-glass opacities were increased but limited to the outer zones of both lungs. (D) On his re-admission due to AE-IPF. Broken arrows indicate extensive ground-glass opacities spread to the inner zones of both lungs.
After discharge, the patient had a gradual worsening of dyspnea on exertion and re-visited our hospital 5 days later. On arrival at the emergency department, the patient was in respiratory distress with a respiratory rate of 30/min and an oxygen saturation of 95% on supplemental oxygen at a rate of 4 L/min using a face mask. Chest CT showed that bilateral diffuse ground-glass opacities extended to the inner zones (Figure 1D). The blood test showed remarkable elevations of lactate dehydrogenase (LDH) (512 U/L), C-reactive protein (CRP) (17.58mg/dL), and Krebs von den Lungen-6 (KL-6, a biomarker for fibrotic interstitial lung diseases (ILDs) (1,545 U/mL; Table 1). A salivary SARS-CoV-2 RT-PCR test on re-admission was negative. No significant bacterial pathogens were isolated from sputum cultures, and no physical signs suggestive of heart failure were observed. A diagnosis of AE-IPF was made based on the clinical and radiological findings. He was admitted to the ICU and given high-flow nasal cannula oxygen therapy. Steroid pulse therapy (methylprednisolone 500 mg twice daily, 3 consecutive days/week/cycle), tazobactam/piperacillin, and azithromycin were started (Figure 2). After 6 days of respiratory failure which required high-flow nasal cannula therapy, his respiratory status slowly improved with 2 cycles of steroid pulse therapy and subsequent methylprednisolone was gradually reduced and replaced with oral prednisolone. However, persistent hypoxia requiring supplementary oxygen continued on his discharge on the 33rd day of the second admission.
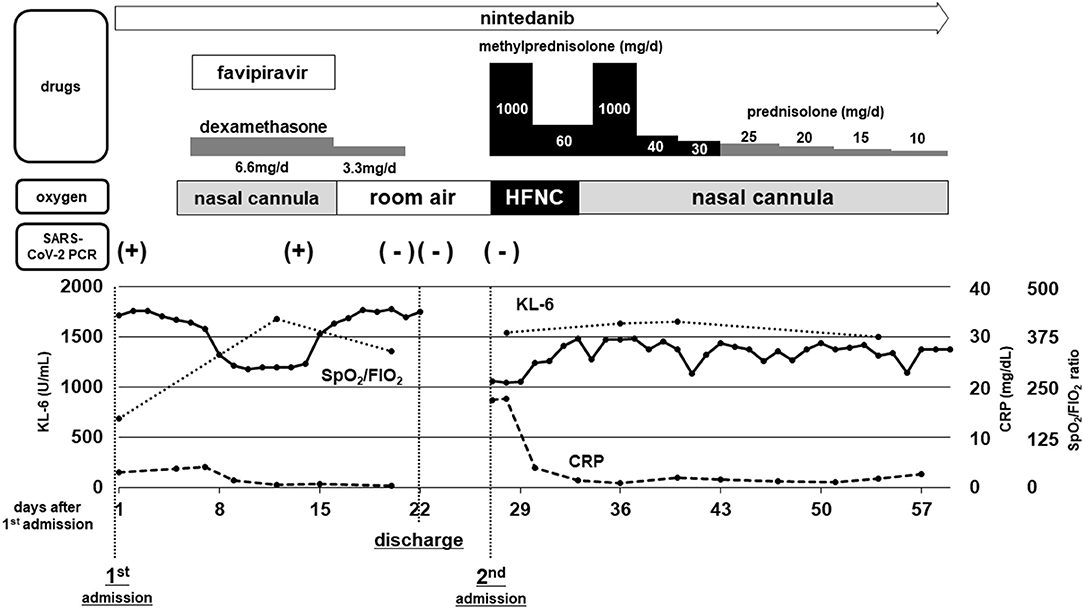
Figure 2. Schematic chart of clinical course and treatment. Therapeutic regimen and the dosages of drugs for COVID-19 and IPF/AE-IPF are shown at the top. The methods of oxygen supplementation required for the patient and the results of SARS-CoV-2 RT-PCR tests are shown in the middle. Changes in serum levels of C-reactive protein (CRP) and Krebs von den Lungen-6 (KL-6), along with the oxygenation index (ratio of SpO2/FIO2) are depicted in the bottom graph.
Discussion
Like patients with several other pre-existing medical conditions (5, 6), those with underlying lung comorbidities including chronic obstructive pulmonary disease, asthma, and ILDs have been shown to be at increased risk of severe disease and mortality due to COVID-19 (2). Previous studies have revealed that COVID-19 patients with pre-existing ILDs, especially fibrotic ILDs, are at very high risk of death (3, 7). Drake et al. assessed the relationship between pre-existing ILDs and mortality in patients with COVID-19 and showed that decreased lung function and a diagnosis of IPF (rather than other ILDs), both of which have also been reported as risk factors of developing acute exacerbation of pre-existing ILDs, were risk factors of death among ILD patients (3). Therefore, one of the reasons for a poor prognosis of COVID-19 in ILD patients is assumed to be acute exacerbation of interstitial lung disease (AE-ILD). In fact, a Japanese nationwide survey reported 12 suspected cases of AE-ILD associated with COVID-19 (8). However, this lethal complication is difficult to distinguish from severe COVID-19 on the basis of clinical manifestations.
The definition of AE-IPF proposed by the international working group is widely accepted currently (4). According to this, AE can be subcategorized into “triggered AE” which is followed by a known predisposing factor such as infection and invasive procedures, and “idiopathic AE” with no trigger identified. It has been suggested that respiratory viral infection triggers AE-ILD (9). While the exact mechanisms of AE development remain unknown, a systemic inflammatory insult with elevated cytokine levels is thought to be a central part of its pathogenesis. Similarly, SARS-CoV-2 infection also induces excessive host immune response, the so-called “cytokine storm” in severe cases. Therefore, although not yet proven statistically, it is suspected that COVID-19 may be one of the common triggers of AE in ILD patients in the current pandemic.
Typical severe COVID-19 exhibits sudden respiratory failure with newly developed bilateral lung opacities on chest CT, which are also common in AE-ILDs. Indeed, according to recent reports demonstrating cases of acute respiratory failure in patients with pre-existing chronic ILDs (10–12), it is hard, if not impossible, to distinguish severe COVID-19 from AE-ILDs triggered by COVID-19. In this case, we observed extension of peripheral dominant GGOs at the time of clinical recovery from COVID-19 (Figure 1C). We deemed them radiological findings of delayed recovery. A retrospective study suggested lung abnormalities on chest CT scans showed the greatest severity around 10 days and gradual resolution 2 weeks after the initial onset of symptoms (13). However, it is also possible that the extension of GGOs shown on chest CT taken at his initial discharge could be the radiological findings of undiagnosed AE-IPF. Indeed, peripheral dominant GGOs are one of the typical subtypes for the radiological feature of AE-IPF (14, 15).
As the pandemic of COVID-19 being prolonged, increasing number of cases with chronic ILDs who developed severe respiratory failure by complication with COVID-19 has been reported. We reviewed and summarized them in Table 2 (8, 11, 12, 16–19). The majority of the cases developed respiratory failure with newly-emerged GGOs simultaneously with the diagnosis of COVID-19, therefore treated with combination of antiviral and immunomodulation therapy against COVID-19. In these cases, it is hard to differentiate between “severe COVID-19 superimposed on pre-existing ILDs” and “AE of chronic ILDs triggered by SARS-CoV-2 infection.” The present case showed the characteristic “two-peak” course (Figure 2) of respiratory failure in the initial COVID-19 phase, with successful recovery due to dexamethasone and favipiravir, and a negative RT-PCR test. The second peak with a more profound and persistent illness can be recognized as infection-triggered AE-IPF. We believe this case is noteworthy as it is important to understand, but not well-reported, the natural course of development of AE clearly triggered by COVID-19. A few reports also described the delayed onset of profound worsening of chronic ILDs after mild COVID-19 (20, 21).
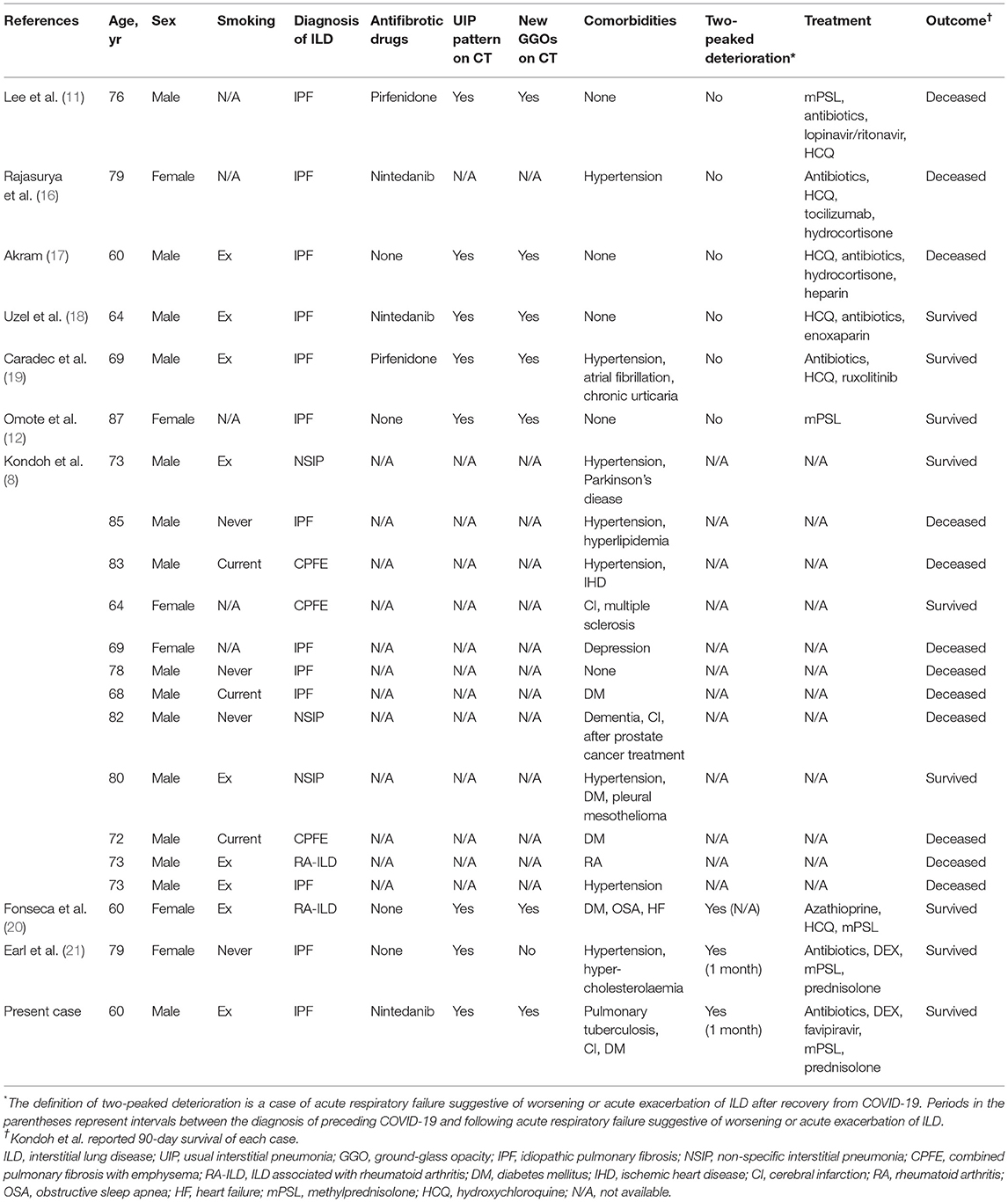
Table 2. Summary of reported cases with chronic ILDs who developed respiratory deterioration by complications with COVID-19.
The patient successfully recovered from the initial phase of acute respiratory failure due to treatment with the anti-viral agent favipiravir (22) and dexamethasone (23), which was the state-of-art treatment regimen at the time in Japan. Moreover, administration of the antifibrotic nintedanib was continued, though the secondary development of AE-IPF was not prevented. As none of vaccines were available at the time in Japan, the patient was not vaccinated against SARS-CoV-2. It is possible that optimal vaccination may reduce the occurrence of AE triggered by COVID-19 in patients with ILD. Future studies are warranted to develop the strategy for preventing and treating AE in IPF patients who developed COVID-19. The optimal duration of anti-viral/anti-inflammatory therapy and/or close monitoring for recovering COVID-19 cases with pre-existing ILD remains unknown. According to the previous reports, the intervals between known triggers and development of AE-IPF ranged between 3–41 days after bronchoalveolar lavage procedures (24) and 0–29 days after lung surgery (25). Considering the experience of the present case, we would emphasize the importance of careful monitoring of patients with IPF after recovery from COVID-19. When patients with pre-existing ILD experience worsening of respiratory failure in the recovery phase of COVID-19, we should consider the possibility of AE-ILD and initiate additional interventions such as corticosteroid pulse therapy.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
Written informed consent was waived by the Institutional Review Board, therefore not obtained from the individual. Oral consent was given for the publication of any identifiable information.
Author Contributions
YG and KS analyzed and interpreted the patient data and drafting the figures. YG, KS, JF, AS, NO, and YS edited the manuscript. All authors have read and approved the final manuscript.
Funding
This report was partly supported by funding from the Nitto Foundation.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. WHO COVID-19 Dashboard. Geneva: World Health Organization. Available online at: https://covid19.who.int/ (accessed Nov 11, 2021).
2. Lohia P, Sreeram K, Nguyen P, Choudhary A, Khicher S, Yarandi H, et al. Preexisting respiratory diseases and clinical outcomes in COVID-19: a multihospital cohort study on predominantly African American population. Respir Res. (2021) 22:37. doi: 10.1186/s12931-021-01647-6
3. Drake TM, Docherty AB, Harrison EM, Quint JK, Adamali H, Agnew S, et al. Outcome of hospitalization for COVID-19 in patients with interstitial lung disease. An international multicenter study. Am J Respir Crit Care Med. (2020) 202:1656–65. doi: 10.1164/rccm.202007-2794OC
4. Collard HR, Ryerson CJ, Corte TJ, Jenkins G, Kondoh Y, Lederer DJ, et al. Acute exacerbation of idiopathic pulmonary fibrosis. An International Working Group Report. Am J Respir Crit Care Med. (2016) 194:265–75. doi: 10.1164/rccm.201604-0801CI
5. Williamson EJ, Walker AJ, Bhaskaran K, Bacon S, Bates C, Morton CE, et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature. (2020) 584:430–6. doi: 10.1038/s41586-020-2521-4
6. Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. (2020) 395:1054–62. doi: 10.1016/S0140-6736(20)30566-3
7. Gallay L, Uzunhan Y, Borie R, Lazor R, Rigaud P, Marchand-Adam S, et al. Risk factors for mortality after COVID-19 in patients with preexisting interstitial lung disease. Am J Respir Crit Care Med. (2021) 203:245–9. doi: 10.1164/rccm.202007-2638LE
8. Kondoh Y, Kataoka K, Ando M, Awaya Y, Ichikado K, Kataoka M, et al. COVID-19 and acute exacerbation of interstitial lung disease. Respir Invest. (2021) 59:675–8. doi: 10.1016/j.resinv.2021.06.007
9. Wootton SC, Kim DS, Kondoh Y, Chen E, Lee JS, Song JW, et al. Viral infection in acute exacerbation of idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. (2011) 183:1698–702. doi: 10.1164/rccm.201010-1752OC
10. Kitayama T, Kitamura H, Hagiwara E, Higa K, Okabayashi H, Oda T, et al. COVID-19 pneumonia resembling an acute exacerbation of interstitial pneumonia. Int Med. (2020) 59:3207–11. doi: 10.2169/internalmedicine.5630-20
11. Lee YH, Kim CH, Lee J. Coronavirus disease 2019 pneumonia may present as an acute exacerbation of idiopathic pulmonary fibrosis. J Thorac Dis. (2020) 12:3902–4. doi: 10.21037/jtd-20-1658
12. Omote N, Kanemitsu Y, Inoue T, Yonezawa T, Ichihashi T, Shindo Y, et al. Successful treatment with high-dose steroids for acute exacerbation of idiopathic pulmonary fibrosis triggered by COVID-19. Intern Med. (2022) 61:233–6. doi: 10.2169/internalmedicine.8163-21
13. Pan F, Ye T, Sun P, Gui S, Liang B, Li L, et al. Time course of lung changes at chest CT during recovery from coronavirus disease 2019 (COVID-19). Radiology. (2020) 295:715–21. doi: 10.1148/radiol.2020200370
14. Akira M, Kozuka T, Yamamoto S, Sakatani M. Computed tomography findings in acute exacerbation of idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. (2008) 178:372–8. doi: 10.1164/rccm.200709-1365OC
15. Sakamoto K, Taniguchi H, Kondoh Y, Ono K, Hasegawa Y, Kitaichi M. Acute exacerbation of idiopathic pulmonary fibrosis as the initial presentation of the disease. Eur Respir Rev. (2009) 18:129–32. doi: 10.1183/09059180.00000409
16. Rajasurya V, Gunasekaran K, Damarla V, Kolluru A. A fatal case of coronavirus disease 2019 (COVID-19) in a patient with idiopathic pulmonary fibrosis. Cureus. (2020) 12:e8432. doi: 10.7759/cureus.8432
17. Akram A. Overwhelming COVID-19 sepsis in a patient with idiopathic pulmonary fibrosis. Cureus. (2020) 12:e9320. doi: 10.7759/cureus.9320
18. Uzel FI, Iliaz S, Karataş F, Çaglayan B. COVID-19 pneumonia and idiopathic pulmonary fibrosis: a novel combination. Turk Thorac J. (2020) 21:451–3. doi: 10.5152/TurkThoracJ.2020.20123
19. Caradec E, Mouren D, Zrounba M, Azoulay LD, Blandin C, Ivanoff S, et al. COVID-19 in a patient with idiopathic pulmonary fibrosis successfully treated with Ruxolitinib. Respir Med Res. (2021) 79:100799–100799. doi: 10.1016/j.resmer.2020.100799
20. Fonseca M, Summer R, Roman J. Acute exacerbation of interstitial lung disease as a sequela of COVID-19 pneumonia. Am J Med Sci. (2021) 361:126–9. doi: 10.1016/j.amjms.2020.08.017
21. Earl N, Schoeneberg D, Davidson PD. Severe progression of idiopathic pulmonary fibrosis post-COVID-19 infection. BMJ Case Rep. (2021) 14:e244472. doi: 10.1136/bcr-2021-244472
22. Doi Y, Hibino M, Hase R, Yamamoto M, Kasamatsu Y, Hirose M, et al. A prospective, randomized, open-label trial of early versus late favipiravir therapy in hospitalized patients with COVID-19. Antimicrob Agents Chemother. (2020) 64:e01897–20. doi: 10.1128/AAC.01897-20
23. The RECOVERY and Collaborative Group. Dexamethasone in hospitalized patients with Covid-19. NEJM. (2020) 384:693–704. doi: 10.1056/NEJMoa2021436
24. Sakamoto K, Taniguchi H, Kondoh Y, Wakai K, Kimura T, Kataoka K, et al. Acute exacerbation of IPF following diagnostic bronchoalveolar lavage procedures. Respir Med. (2012) 106:436–42. doi: 10.1016/j.rmed.2011.11.006
Keywords: COVID-19, acute exacerbation, idiopathic pulmonary fibrosis, high resolution CT scan, viral infection
Citation: Goto Y, Sakamoto K, Fukihara J, Suzuki A, Omote N, Ando A, Shindo Y and Hashimoto N (2022) COVID-19-Triggered Acute Exacerbation of IPF, an Underdiagnosed Clinical Entity With Two-Peaked Respiratory Failure: A Case Report and Literature Review. Front. Med. 9:815924. doi: 10.3389/fmed.2022.815924
Received: 16 November 2021; Accepted: 03 January 2022;
Published: 03 February 2022.
Edited by:
Sevket Ozkaya, Bahçeşehir University, TurkeyReviewed by:
Mengmeng Zhao, Tongji University, ChinaAurelien Justet, Centre Hospitalier Universitaire de Caen, France
Nalan Ogan, Ufuk University, Turkey
Takuma Isshiki, Toho University, Japan
Copyright © 2022 Goto, Sakamoto, Fukihara, Suzuki, Omote, Ando, Shindo and Hashimoto. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Koji Sakamoto, c2FrYWtvamlAbWVkLm5hZ295YS11LmFjLmpw
†These authors have contributed equally to this work
 Yosuke Goto†
Yosuke Goto† Koji Sakamoto
Koji Sakamoto Atsushi Suzuki
Atsushi Suzuki Yuichiro Shindo
Yuichiro Shindo