
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CLINICAL TRIAL article
Front. Med. , 11 March 2022
Sec. Pulmonary Medicine
Volume 9 - 2022 | https://doi.org/10.3389/fmed.2022.807612
Background: Occupational exposure to pesticides has been associated with lung and cognitive function exacerbations. In the present study, we tested the effectiveness of breathing focused yoga intervention on alleviation of adverse respiratory and cognitive effects associated with chronic pesticide exposure in farmers.
Methods: We undertook a parallel, two-armed randomized controlled trial with blinded outcome assessors on a chronically pesticide-exposed farming population. The study was conducted at district Panipat, State Haryana located in the Northern part of India from November 2019 to August 2020. A total of 634 farmers were screened, and 140 farmers were randomized to breathing-focused yoga intervention (BFY, n = 70) and waitlist control arms (n = 65). BFY was delivered weekly in 45-min group sessions over 12 weeks followed by home-based practice. The primary outcome was the change in spirometry-based markers of pulmonary function from baseline expressed as raw values, Global Lung Initiative (GLI) percent predicted (pp), and GLI z-scores after 24 weeks of intervention. Secondary variables were Trail making tests (TMT A and B), Digit symbol substitution (DSST), and WHO Quality of life-BREF (WHOQOL-Bref). Analysis was by intention-to-treat. Mediation analysis was done considering oxidative stress markers as potential mediators.
Results: At the end of 6 months of intervention, the overall follow-up in the participants was 87.85% (n = 123); 90% (n = 63) in the control group, and 85.71% in the yoga group (n = 60). The mean age of the study cohort (n = 140) was 38.75 (SD = 7.50) years. Compared with the control group, at 24 weeks post-intervention, the BFY group had significantly improved status of the raw sand z scores markers of airway obstruction, after adjusting for confounders, FEV1, FVC, FEF25-75 [z score-adjusted mean differences (95% CI); 1.66 (1.10–2.21) 1.88 (1.21–2.55), and 6.85 (5.12–8.57), respectively. A fraction of FEF25-75 change (mediation percentage 23.95%) was explained by glutathione augmentation. There were also significant improvements in cognitive scores of DSST, TMT-A and TMT-B, and WHOQOL-Bref.
Conclusion: In conclusion, regular practice of BFY could improve the exacerbations in the markers of airway obstruction in chronically pesticide-exposed farmers and cognitive variables. A significant mediating effect of glutathione augmentation was also observed concerning the effect of the intervention on FEF25-75. These findings provide an important piece of beneficial evidence of the breathing-based yoga intervention that needs validation across different farming ethnicities.
Clinical Trial Registration:www.ClinicalTrials.gov, identifier: CTRI/2019/11/021989.
Pesticide use is an integral measure for agricultural sustainability, one of the primary objectives of the sustainable development goals (SDG-2) (1). However, the large-scale use of pesticides has surfaced as a double-edged sword associated with a varying range of detrimental health outcomes (2–15). Prevention of work-related respiratory disease constitutes the primary focus of the National Institute of Occupational Safety & Health (NIOSH) (16). Though the modifiability of occupational exposures through educational strategies has grabbed some clinical interest as a preventive measure for further exacerbations including chronic obstructive pulmonary disease (COPD), and chronic bronchitis (17). However, these interventions require changing the behavior of farmers which has been notified as a difficult outcome to achieve given the observation that many protective recommendations are never adopted by farmers (17).
Adverse respiratory consequences expressed as reductions in spirometric variables [forced expiratory volume in 1 s (FEV1), forced vital capacity (FVC), and their ratio percentage FEV/FVC%] are the most widely reported health concerns of chronic pesticide exposure (3–9). These manifestations are the established risk factors for fixed airway obstruction including chronic obstructive pulmonary disease (6). Several lines of evidence support the beneficial effects of yoga-based interventions on the respiratory system in various non-clinical and clinical settings exacerbations such as COPD and asthma (18–25). The improved efficiency of respiratory function associated with yoga practice has been attributed to various factors including enhanced ventilatory functions, increased forced vital capacity, FEV1, maximum breathing capacity and breath-holding time, maximal stretching of respiratory muscles, efficient use of diaphragmatic and abdominal muscle, blunting of excitatory pathways regulating respiratory systems, etc. (20, 22–25). Explicitly there is a particular indication of the limited effectiveness of the yoga-based intervention to its breathing-focused practices as compared to yoga postures against critical manifestations such as COPD (19). These respiratory exercises are relatively simple, low cost, and could be incorporated into the daily lives of farmers. However, there is no clinical trial report available addressing the effectiveness of these practices in pesticide-exposed farmers with adverse respiratory manifestations. Further, given the notion that the efficacy of yoga-based interventions depends on the fitness levels of the individuals (21), the generalisability of findings from different subject populations is limited.
Cognitive impairment is another major health exacerbation of chronic pesticide exposure. It is a risk factor for neurodegenerative diseases (13, 14) and could underline the reduced well-being of farmers directly linked to the sustainability of agriculture (26) and hence, calling for clinical attention. Several studies support role of yoga as an effective intervention to enhance cognitive function (Hedges' g = 0.33, standard error = 0.08, 95% CI = 0.18–0.48), with the strongest effects reported for attention and processing speed (g = 0.29, p < 0.001), followed by executive function (g = 0.27, p = 0.001) and memory (g = 0.18, p = 0.051) (27, 28). Importantly, these domains of cognition also intersect with pesticide exposure-induced cognitive decline, we thereby hypothesized that farmers with pesticide exposure will benefit cognitively through yoga-based interventions.
In view of the lack of available studies focused on the management of adverse chronic health effects in pesticide exposed farmers, we conducted a randomized clinical trial to test if 24 weeks of regular breathing-focused yoga practice could alleviate their adverse respiratory and cognitive manifestations against a wait-list control group.
Over recent years, there has been increased recognition of the importance of evaluating hypothesized mediating mechanisms in clinical trials (29). Oxidative stress is one of the unanimous pathological mechanisms underlying pesticide-induced toxicity of various pesticides (30–32), with lipid peroxidation and GSH depletion being the critical modulators of airway damage in obstructive lung diseases (33). Alleviation of imbalances in oxidative stress parameters has been one of the mechanistic insights obtained from yoga-based clinical research (34–36). Hence, the present trial also aimed to test the mediating role of the oxidative stress markers underlying the effectiveness of the breathing-focused yoga intervention on the respiratory and cognitive outcomes.
The study was a two-armed, randomized, parallel-group clinical trial with breathing-focused yoga intervention and the wait-list control groups with blinded outcome assessors (Figure 1). Details of the same have been appended in the study protocol (Supplementary Material). The trial was conducted at district Panipat, State Haryana located in the Northern part of India from November 2019 to August 2020. Farmers were invited to participate and were recruited during the meetings conducted by the village organizations. Only one member from each household was randomly selected to avoid any within-family clustering effects. After a detailed explanation of the study objectives and design, informed consent was obtained from willing individuals. The study was conducted following the CONSORT statement for non-pharmacological interventions and was approved by the Institutional ethics committee. The study was also registered with clinical trials of India registration number: CTRI/2019/11/021989.
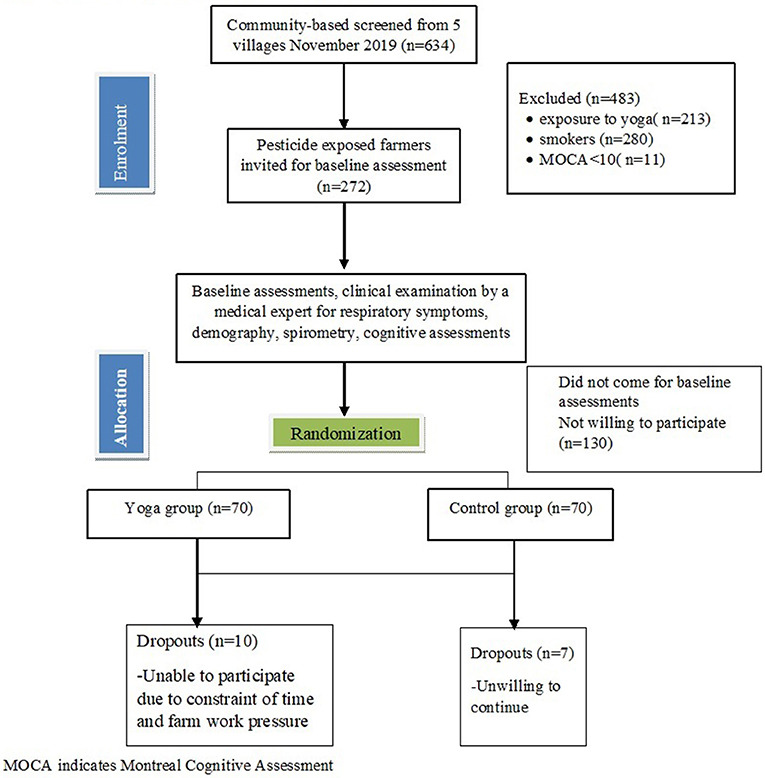
Figure 1. Trial consolidated standards of reporting trials profile. MOCA indicates Montreal Cognitive Assessment.
The participants were male farmers of the age group between 18 and 49 years, naïve to the practice of pranayama or other yoga-based practices, and with at least 6 months of self-reported spraying operations in the field. Farmers with prior exposure to yoga or any other mind-body medicine, symptoms of acute pesticide exposure/poisoning, smokers/ex-smokers, self-reported diagnosis of respiratory disease (such as COPD, asthma, bronchiectasis, pulmonary fibrosis, etc.), history of chronic or terminal disorders (such as active cancer, severe heart or cerebrovascular disease), or any limitations that could have led to difficulties in follow-up or assessments (such as mental illness or severe cognitive impairment, Montreal cognitive assessment, MoCA score <10) (37). were excluded from the study. For additional details see Supplementary Table 1.
An external statistician, not directly involved in the implementation of the BFY had randomized the participants during their baseline visit in a 1:1 ratio (n = 70, each arm) using a sequence randomizer. The allocation sequences were sealed and participants were informed about the further process immediately after their baseline assessment. Owing to the nature of the intervention, blinding was not possible, however, outcome measures were blinded for the randomization groups.
All the participants of the yoga group followed a breathing-focused yoga module for 24 weeks. For the initial 12 weeks, the instructions for the yoga practices were given by certified yoga teachers for 45 min for 6 days/week. Following the same, participants were advised to do daily home-based practice for the next 12 weeks; this was done to integrate the intervention into their daily routine settings. The farmers were not restricted from doing their routine farm work on fields and thereby were obligatorily physically active. The intervention included physical practices (loosening practices, breathing practices with body movements, asanas), relaxation techniques, pranayama, lectures regarding the importance of yoga, lifestyle changes through notional corrections, the importance of wearing personal protective equipment during pesticide spray. Since farmers were involved in physically-demanding routine activities and based on the indicative relevance of breathing-focused yoga interventions on pulmonary function under various settings, the intervention was drafted with special emphasis on breathing practices, relaxation techniques, and meditation (20, 28). Asansa (physical postures) (pavanamuktasana, sukhasana, gomukhasana, paschimotanasana, and vakrasana) were included only for preparatory requiremrnts for the practice of pranayama. Further, under pranayama, Bhastrika pranayama was included based on the associated beneficial outcomes on lung function as well as on cognitive improvement (20, 28). The pranayama session was drafted as a comprehensive respiratory exercise regime of 25 min, composed of fast practices Kapalabhati interspersed with Surya bedhana (20). Details of intervention are presented in Supplementary Table 2 of the Study Protocol.
For inactive control participants, we chose a wait-list design as we deemed it as an ethically appropriate alternative to provide needed care to the control pesticide-exposed group following the trial. Though the subjects in the wait-list group participated in no active intervention, while recruitment, they were instructed to continue their daily activities (without engaging in regular structured exercise) and were also given weekly once group lectures focused on the importance of wearing personal protective equipment during pesticide spray. All subjects received monthly phone calls to assess for any subjective changes in health. After the completion of the 24th week study, these participants received the same yoga-based intervention given to the intervention group post their data collection.
All outcome assessments were done at baseline and 6 months. Standard measures of spirometry included forced vital capacity (FVC), forced expiratory volume in one second (FEV1), the ratio of forced expiratory volume in 1 s to forced vital capacity (FEV1/FVC), forced expiratory flow between 25 and 75% of the FVC, FEF25–75 and peak expiratory flow rate (PEFR). The primary outcome was the adjusted mean difference in lung function variables analyzed as spirometric data from baseline to the 24th week. The data was presented as raw spirometric scores. Additionally, in order to meet the worldwide diagnostic standard, free of bias due to age, height, sex and ethnic groups, we used the Global Lung Function prediction equations to derive percent predicted values and standard deviation (z-) scores adjusted for sex, age, and height and ethnicity (38, 39). As specific reference ranges do not yet exist for South Asian population, the Caucasian equations (i.e., derived from white subjects of European origin) were used to derive the Global Lung Function Initiative (GLI) based scores. The secondary outcome variables were changes in cognitive functions scored through Digit Symbol Substitution Test (DSST) and Trail Making Tests part A and B (TMT-A and B); and psychological variables scored through perceived stress scale (PSS), and World Health Organization Quality of Life–BREF (WHOQOL-Bref). The neurocognitive tests/domains were selected based on the previous reports on neuropsychological outcomes in pesticide exposed farmers (13, 14). Mitigation of oxidative stress was hypothesized as the causal mediation mechanism for the breathing focused yoga and hence, the planned mediation analysis included oxidative stress markers; Malondialdehyde (MDA), Superoxide dismutase (SOD), and Glutathione (GSH).
Baseline assessments of study outcome measures were performed before subjects were randomized. Assessments were repeated at the end of 6 months of intervention. The preliminary information was obtained from all study subjects which included questions on demographic data, and those related to pesticide exposure including detailed exposure information, names of the pesticides used, mode of application, period, dose, frequency of pesticide applications, and personal protective equipment repair status, duration used, etc.
A pulmonary function test was performed to assess pulmonary impairment in pesticide sprayers by using a spirometer (RMS Helios-702, India) following the standards of lung function testing of the American thoracic society/European respiratory Society (ATS/ERS) (40). Standard measures of spirometry included forced vital capacity (FVC), forced expiratory volume in 1 s (FEV1), the ratio of forced expiratory volume in 1 s to forced vital capacity (FEV1/FVC), forced expiratory flow between 25 and 75% of the FVC (FEF25–75%) and peak expiratory flow rate (PEFR). Participants were instructed to breathe, and three reproducible measurements each of FEV1, FVC, and maximal mid-expiratory flow were obtained. The highest values were documented and used for analysis. Other spirometric variables, including forced expiratory flow at 25–75% (FEF25–75) and peak expiratory flow (PEF), were obtained from the trial with the highest combined FEV1 and FVC. Using the Excel macro for GLI, reference values, the lower limit of normal (LLN), Z-scores, and percentiles for FEV1, FVC, and the FEV1/FVC ratio were calculated for each subject in the reference population available from www.lungfunction.org (41, 42). Height and weight at the time of spirometry were measured to the nearest 0.1 cm on a stadiometer and 0.1 kg on an electronic scale, respectively.
The Montreal Cognitive Assessment (MoCA) was used to evaluate the overall cognitive abilities of the participants (37). Cognitive function was assessed using the neuropsychological tests, DSST (43, 44) (for executive function, speed of processing, attention), and Trail Making Test A/B (TMT-A: speed of processing; TMT-B: executive function) (45–48). DSST is a component of the Wechsler Adult Intelligence Test with high test-retest reliability. This pen and pencil-based test has a considerable executive function component, evaluates psychomotor speed, attention, and executive function. The subject was given a key grid of numbers and matching symbols and a test section with numbers and empty boxes. The test consists of filling as many empty boxes as possible with a symbol matching each number. The score is the number of correct number-symbol matches achieved in 90 s. We used the DSST scores as a continuous variable. TMT measures scanning and visuomotor tracking, divided attention, and cognitive flexibility. Two raw scores (time needed to complete TMT A and TMT B) and three derived scores (TMT B-A, TMT B/A, and TMT (B-A)/A) were calculated for each participant. These tests were selected based on the previous reports on neuropsychological outcomes in pesticide-exposed farmers.
Stress perception was assessed using the perceived stress scale (PSS), a 10-item well-validated scale that gauges chronic stress on a 40-point scale (49). A total score ranging from 0 to 40 is computed by reverse scoring the four positively worded items and then summing all the scale items. Higher scores indicate greater levels of perceived stress. Though not as diagnostic criteria, PSS scores of 0–13, 14–26, and 27–40 points have been considered as indicators of low, moderate, and high perceived stress, respectively (50).
The quality of life (QOL) of the participants was assessed using the World Health Organization Quality of Life – BREF (WHOQOL-Bref) (51), a standardized comprehensive instrument comprising 26 items that elicits the perceived physical health, psychological health, social relations and environment—related QOL in an individual.
Oxidative stress markers, reduced glutathione (GSH) were estimated in the whole blood whereas, TBARS (Thiobarbituric acid reactive substances), and SOD (Superoxide dismutase) were analyzed from the hemolysate. TBARS concentration was expressed as serum malondialdehyde (MDA). The plasma and the buffy coat were removed from whole blood by centrifugation at 2,000 rpm for 10 min at 4°C. The red cells were washed thrice with normal saline and a hemolysate(s) was prepared as follows: MDA levels were measured with the method described by Ohkawa et al. (52). The plasma and the buffy coat were removed from whole blood by centrifugation at 2,000 rpm for 10 min at 4°C. The red cells were washed thrice with normal saline and a hemolysate(s) was prepared as follows: For the estimation, MDA hemolysate was prepared by mixing 1.9 ml of cold distilled water with 0.1 ml of packed cell volume (PCV) suspension. For estimation of SOD activity: The remaining red cells were haemolysed by approximately adding 1.5 volumes.
Given the lack of reported minimally clinically significant difference suggested for FEV1 defined for clinical trial endpoints for occupationally impaired lung function. The calculated sample size of n = 140 was based on the reported effect of on FEV1 [effect size of 0.54, (123/ml) improvement] 20 for 80% power and a 2-sided α = 0.05, with assumed attrition of 20% over 6 months. To meet the objective of recruiting 140 subjects, a rough sampling frame of 500 households was generated. The distribution of continuous variables was analyzed for normal distribution (using the Kolmogorov–Smirnov statistic) and for homogeneity of variance (Levene's test). Data for these variables are shown as means and standard deviation (SD). Covariates considered were age, educational level, BMI, cumulative exposure index (CEI), and serum achetylcholinesatse levels. Algorithms for calculation of CEI are Given in Supplementary Table 3. All statistical analyses were performed blinded to the randomization group and results are reported using intention-to-treat analysis. the 2012 Global Lung Function Initiative (GLI) reference equations were used and percent predicted and z-scores were calculated, using the open-source GLI R Macro. The GLI Z-score is a standardized measure of the positioning of an observed measurement in the distribution of the population from which the GLI reference values are derived and takes both between-subject and age- and height-related variability into account. LLN was defined as the lower fifth percentile in the distribution from which the GLI reference values are derived, as calculated by the GLI Excel macro. Airway obstruction was defined as FEV1/FVC less than the lower limit of normal as per the recommendations of The American Thoracic Society (ATS)/European Respiratory Society (ERS) (53). Linear regression was used to analyze study outcomes as adjusted mean differences (AMDs), additionally adjusted for their comparable value at baseline and other covariates Missing data were minimal. A P-value < 0.05 was considered to indicate significant differences between adjusted means.
We applied causal mediation method, to investigate if oxidative stress could be a causal pathway between intervention and the outcome. We fit mediation models to estimate the direct and indirect effects of the intervention assuming a mediating effect of the oxidative stress markers. Mediation analysis was performed using the methods described by Valeri and Vanderweele (54) to investigate direct and indirect effects of the BFY on study outcomes at 6 months. The PROCESS SPSS Macro version 2.13, model four was used to perform analysis by fitting a linear regression model to the outcomes with yoga yreatment and the mediators included were the covariates (described above), and then fitting a regression model to the mediator (linear or logistic depending on the mediator) including intervention as a covariate. In mediation analysis, effects can be broken down into separate paths: the c path between the treatment and outcome (without accounting for potential mediators), the a path between the intervention and the potential mediator; and the b path between the potential mediator and the outcome (Supplementary Figure 1). The mediating (indirect) pathway is calculated as the product of paths a and b (ab). Univariable linear regression models were fitted to the potential mediators MDA, GSH and SOD to test whether there was an association between the BFY and the mediators. Since a variable can only be a mediator of treatment if there is a significant effect (p < 0.05) of treatment on the mediator (path a), Following the sam, linear regression analyses were performed to examine the relationships between treatment allocation and change in each of the potential mediators, and between change in each of the potential mediators and the outcome posttreatment scores.
The flow of patients into the study is shown in Figure 1. During the months of November-January 2019–20, we had screened 634 farmers from five nearby villages of Panipat district state Haryana, India. Out of 634 farmers screened, only 280 fitted the eligibility criteria (Figure 1), of which only 140 completed the baseline assessments who were randomized into yoga and control groups. A total of 130 participants (92.85%) completed the post-intervention assessment.
The mean age of the study cohort (n = 140) was 38.75 (SD =7.50) years; and their mean BMI was 22.44 (SD = 1.37) kg/m2 (Table 1). Mean pesticide exposure among sprayers was found to be 5.71 (SD = 3.04) years. As compared with participants, non-participants were of lower age and had comparatively less exposure to pesticides (Supplementary Table 4). All the study subjects belonged to agricultural occupation with similar socioeconomic status (data not shown) with mean period of education as 3.54 (2.77) years. Aligining with the previous observations, farmers seemed to be exposed to combination of multiple pesticides, mostly organophosphates (see Supplementary Table 5) with mean serum cholinesterase levels of 5.37 (SD = 0.88) matching their exposure status (55). Table 1 also demonstrates the distribution of the spirometric variables following conversion to the GLI z-scores. Notably, the median z-score values were well-below zero [FEV1 = −3.39 (1.36); FVC = −3.07 (1.60); FEV1/FVC = −1.73 (1.76); FEF25–75 = −1.73 1.76, mean (SD)]. The median FEV1 z-score was less than −1.64, the lower limit of normal and the median FVC and FEF25–75 z-scores approached this mark. Almost the entire cohort had mild cognitive impairment (98.6%, MOCA scores 18–25). At baseline, the distribution of the demographic and study variables were found to be fairly even with the non-significant differences between the study groups (p > 0.05) (for details, see Table 1), except for DSST and TMT scores. However, the distribution of global cognition was balanced between the groups (MoCA, P = 0.225). The farmers were also exposed to a mixture of various pesticides, mostly organophosphate and a cumulative effect of pesticides, measured by activity of serum cholenesstase activity levels aligned with the range observed in previous populations with similar duration of pesticide exposure. Though almost the entire cohort exhibited potentially unsafe behavior with respect to the use personal protective equipments use with 72.85% reported none. There was also a significantly skewed distribution of PPE use between the study groups (Supplementary Table 6), however, the cumulative pesticide exposure index was equally distributed between the groups.
At the end of 6 months of intervention, the overall follow-up in the participants was 87.85% (n = 123); 90% (n = 63) in the control group, and 85.71% in the yoga group (n = 60). The adjusted means of the all spirometric variables and their z-scores are presented in Table 2. In the intention-to-treat analysis with the raw spirometric data on the 140 randomized patients, BFY group had a significantly improvement in FEV1 (L) [AMD, 1.02, 95% CI (0.75–1.38), p < 0.001)], FVC (L) [AMD, 1.14 95% CI (0.79–1.49), p < 0.001], FEF25–75 [AMD, 29.33 95% CI (22.46–36.20) p < 0.001], PEFR [AMD, 43.47 95% CI (35.33–51.60), p < 0.001] as compared to the controls, following adjustment for age, height, education level, cumulative pesticide exposure, and serum cholineestase levels. However, no significant between group difference was observed for FEV1/FVC% (Table 2). Analyses of z-scores which are independent of age, and height, gave similar results (FEV1 AMD = 1.66 (95% CI = 1.10–2.21), FVC AMD = 1.88 (95% CI = 1.21–2.55) FEV1/FVC GLI pp AMD = 3.19 (95%CI=−8.68–14.96), and FEF25–75 z-score AMD=6.85 (95% CI = 5.12–8.57) following adjustment for education level, cumulative pesticide exposure and serum cholinesterase levels.
In exploratory subgroup analyses, greater improvements in spirometric variables were noted in farmers with age>39 years as compared to those ≤39 years (data not shown).
The secondary variables were the cognitive and psychological variables. The post-intervention mean scores of DSST [AMD = 11.82 (95% CI, 8.90–14.75)], TMT-A [AMD = −24.60 (95% CI, −28.14 to −21.05)] and TMT-B [−41.99 (−49.72 to −34.25)] were significantly improved in the yoga group as compared to the control group (Table 2). The influence of BFY on the contrive outcomes was not confounded by age or education (Table 2). We could also observe significant improvement in WHO-BREF scores as compared to the control group [AMD = 26.89, (95% CI = 22.82–30.97)]. Concerning PSS, positive but non-significant changes in the adjusted means were observed between BFY and the control group (Table 2).
Concerning the proposed mediators of yoga intervention, MDA demonstrated a significant reduction in the yoga group as compared to the control group [(AMD = −63.72, 95% CI = −91.94– (−35.05)], whereas the anti-oxidative markers GSH and SOD indicated a comparative increase in the yoga group [AMD; GSH = 1.08, 95% CI = 0.79–1.37; AMD; SOD = 0.06, 95% CI = 0.010–0.11] as compared to the controls (Table 2). Hence, significant associations could be established between BFY and all the potential mediators using linear regression models (path a, Supplementary Figure 1). Therefore, further mediation models as presented in Table 3 were fitted to all the three (SOD, MDA, and GSH) variables.
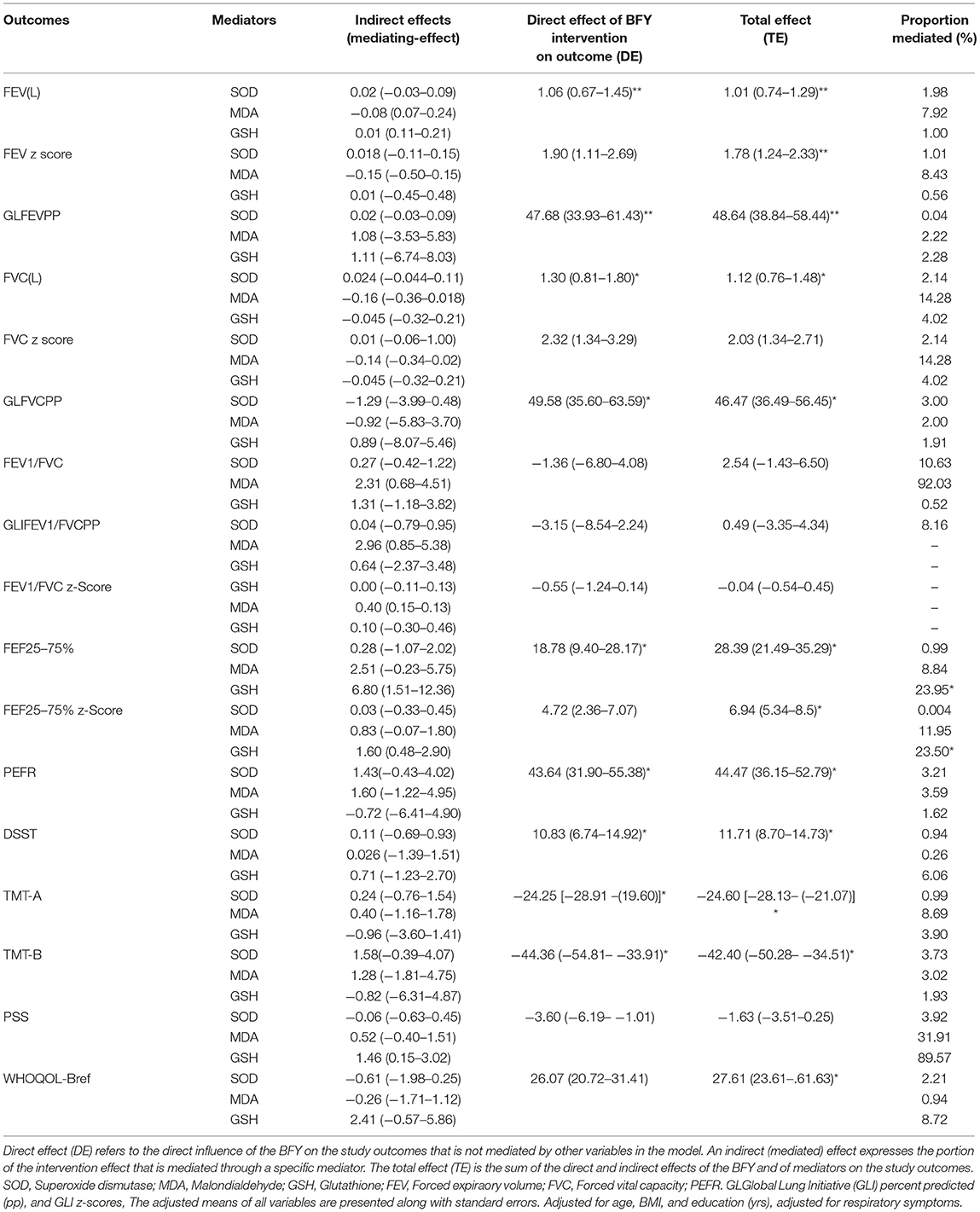
Table 3. Indirect, direct, and total effects of the mediation models on respiratory and cognitive outcomes at 6 months.
The indirect, direct and total effects of each of the models are given in Table 3. The mediation analyses indicated GSH as a mediator of the effect of BFY on FEF5-5. As observed in Table 3, a fraction of FEF25-75 change was partly explained by increases in GSH levels (mediation percentage 23.95%).
In this 24-weeks randomized controlled trial on chronically pesticide exposed farmers, BFY practice was significantly more observed to be more effective than the wait-list control condition in the alleviation of spirometry-based indices of airflow limitation, in particular FEV1, FVC, FEV25-75, and PEFR. The observed increment in FEV1 by 1.02L over 6 months in the BFY group seems relevant against an annual decline by 13.1 mL (95% CI, 19.1 to 7.1) (7) and a reduction by 140 ml observed over an average of 3.4 years of pesticide exposure (10). However, given the lack of specific reports on clinical interventions with spirometry-based pulmonary outcomes in pesticide-exposed populations, there remains an uncertainty in the clinical significance of the observed effect sizes. Nonetheless, the observed change of ~1 l in FEV1 is larger than the minimal clinically important difference of 100 ml suggested for pharmacological trials (56). Our observations accord with the previous reports of improvements in pulmonary function parameters with regular yoga practice, particularly breathing-focused practices (18–20). Additionally, there have been mixed findings as well-indicating that the effectiveness of yoga-based breathing interventions is influenced by the fitness levels of the subjects, with only marginal improvements in lung functions observed in the elderly (20) to moderate-but-clinically-significant improvements in COPD patients (18). This further explains the comparatively larger effect-sizes observed concerning FEV1 and FEV1 (Pred%) in the present pesticide-exposed cohort as compared to the meta-analyzed effect-sizes on patients with COPD [weighted mean difference (WMD) of 125 ml for FEV1(L)20 and 3.95% for FEV (Pred%)] (18). Pesticide exposure has been sought as a risk factor for obstructive pulmonary diseases marked by an early reduction in FEV1 (57). Our results justify the relevance of early intervention in pesticide-exposed populations for prevention of manifestations of irreversible lung function decline as in COPD (57). Mechanistically, we could establish a 24% mediating effect of glutathione increment underlying BFY induced improvements in FEF25-75, which is another primary spirometry-based marker of the airway in abundance in obstruction (4). Glutathione is the principal small molecular weight thiol of the antioxidant system abundant in the epithelial lining fluid of lungs and serves as a crucial protector of alveolar macrophages, pulmonary epithelial cells, and pulmonary endothelial cells from oxidative stresses (33). Its depletion and disturbed metabolism are key manifestations in pesticide exposed tissues under inflammatory settings of lung decline including chronic obstructive pulmonary disease (COPD). Our findings on GSH augmentation accord with prior reports on remarkably increased after yoga practice serum total glutathione (GSH) contents, activities of GSH-peroxidase, and GSH-transferase (58). The notion BFY could serve as a non-pharmacological substitute for GSH augmentation deserves attention since supplementation of GSH precursors has been considered as the best means of manipulating intracellular GSH biosynthesis to combat its depletion noted in varied inflammatory settings (59). For other spirometric parameters we failed to establish a significant mediating effect of alleviation of oxidative stress on BBY intervention. These findings indicate the need to explore other alternate markers, including inflammation. Altogether, the observed beneficial effects of BFY on FEV1 along with other spirometric markers of small airway obstruction (FEV25-75% and PEFR) deserve clinical attention to combat exacerbations of lung function decline in pesticide-exposed populations. These findings deserve clinical recognition given the observed poor status of precautionary practices in the farming population; most of the farmers (n = 102, 72.85%) were not using personal protective equipment. Moreover, when analyzed for airflow obstruction, 56.3% had airflow obstruction and ~70% of the farmers reported adverse respiratory symptoms.
Pesticides are known lipophilic neurotoxins and are reported to cross and disrupt the blood-brain barrier (60). Long-term exposure to these chemicals could lead to neuronal loss in specific brain regions and subsequent cognitive impairment (61). In line with previous reports on pesticide exposure and global cognitive function, the entire cohort of pesticide-exposed farmers had the manifestation of mild cognitive impairment (MOCA scores 18–25) (14, 33). In particular, the TMT-B scores of the study cohort were lower as compared to the normative population-based scores reported for the matched age and education status, indicative of their compromised executive control (61, 62). In this backdrop of cognitive decline, BBY intervention was found to have significant potential to mitigate neurocognitive decline through improvements in the TMT-B scores by 42 s, DSST by 11 s, and TMT-A by 25 s. Our results are in line with previous reports of yoga-based practices, However, no causal inference could be established for oxidative stress markers underlying the beneficial cognitive effects of the BFY. Inclusion of the objective mediators such as structural and functional brain changes could aid in unraveling the mediator influences.
Psychological stress is a well-recognized health concern amongst farmers. Though we could find a trend for improvement in perceived stress in the BFY group, the difference between the groups was not statistically significant. Notably, there was a significant improvement in the quality of life in the BFY group as compared to the control group, which is a positive health marker indicative of improved capacity to function (63). and an important factor toward the attainment of sustainable agriculture (64).
This study is limited by the small sample size and use of prebronchodilator spirometry. The study was focused on early intervention in the high-risk farming population, the trial was of a short duration of 6 months, and hence, we did not include the outcome of COPD manifestation which would be required to get a more realistic insight into the preventive potential of BFY. We did not consider statistical power requirements for causal analyses which need extended validation in larger trials (29). The strength of this study lies in the fact that it is the first-ever trial that addressed the need for clinical attention to alleviate adverse health conditions in the chronically pesticide-exposed farmer population. The present trial was conducted in India which is predominantly a rural country with 67% of its population engaged in agricultural practice (65). In the Indian scenario, farmers mainly live in rural areas wherein government hospitals are the major health care setups with a preponderance of traditional health experts (66). However, originating in India as a comprehensive mind-body practice, yoga has become increasingly popular in the West as a holistic approach to health and well-being, the popularity and practice of yoga-based interventions are not restricted to the Indian subcontinent (67, 68). Over recent years, there has been a sharp rise in the spread of yoga-based interventions across the globe. Given the fact that ethnicity is an important factor in lung function, the trial findings need validation over different ethnic settings. Overall the study findings are useful for establishing preliminary evidence for future larger trials with longer follow-ups targeting the prevention of COPD in the high-risk population.
Enhanced respiratory surveillance has been stated as a need of the hour for pesticide-exposed farmers. Our findings indicate the scope of implementation of cost-effective breathing-focused interventions along with respiratory surveillance in pesticide exposed farmers. Given the multimodal influence of yoga on health, the effects of yoga may be broader when explored for other adverse health effects associated with pesticide exposure. Overall, the findings support the use of yoga-based interventions as a pragmatic strategy against exacerbations of respiratory and cognitive health decline in farming communities. In this 24-weeks randomized controlled trial on chronically pesticide exposed farmers, breathing focused yoga intervention was significantly more effective than the wait-list control condition in the alleviation of spirometry-based indices of airflow limitation, in particular FEV1, FEV25-75, and PEFR. The study also gave mechanistic insights into the understanding of the breathing-focused yoga intervention vis GSH augmentation for improvement for FEF5-5%. This could serve as a cost-effective substitute for GSH supplementation suggested for the management of airway inflammation.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The study was conducted in accordance with the CONSORT statement for non-pharmacological interventions and was approved by the Institutional Ethics Committee. The patients/participants provided their written informed consent to participate in this study.
VD: conceptualization, study design, and data analysis. VM: conceptualization, study design, data analysis, writing first draft of manuscript, and revision of manuscript. NM: conceptualization, study design, and revision of manuscript. US: data analysis. DS: revision of manuscript. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
USG is thankful to the Indian Council of Medical Research (ICMR) for providing Research associate fellowship (Sanction No. 45/02/2018-NAN/BMS).
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2022.807612/full#supplementary-material
1. Gil JDB, Reidsma P, Giller K, Todman L, Whitmore A, van Ittersum M. Sustainable development goal 2: improved targets and indicators for agriculture and food security. Ambio. (2019) 48:685–98. doi: 10.1007/s13280-018-1101-4
2. Nicolopoulou-Stamati P, Maipas S, Kotampasi C, Stamatis P, Hens L. Chemical pesticides and human health: the urgent need for a new concept in agriculture. Front Public Health. (2016) 4:148. doi: 10.3389/fpubh.2016.00148
3. Hu R, Huang X, Huang J, Li Y, Zhang C, Yin Y, et al. Long- and short-term health effects of pesticide exposure: a cohort study from China. PLoS ONE. (2015) 10:e0128766. doi: 10.1371/journal.pone.0128766
4. Hernández AF, Casado I, Pena G, Gil F, Villanueva E, Pla A. Low level of exposure to pesticides leads to lung dysfunction in occupationally exposed subjects. Inhal Toxicol. (2008) 20:839–49. doi: 10.1080/08958370801905524
5. de Jong K, Boezen HM, Kromhout H, Vermeulen R, Postma DS, Vonk JM. Association of occupational pesticide exposure with accelerated longitudinal decline in lung function. Am J Epidemiol. (2014) 179:1323–30. doi: 10.1093/aje/kwu053
6. Alif SM, Dharmage SC, Benke G, Dennekamp M, Burgess JA, Perret JL, et al. Occupational exposure to pesticides are associated with fixed airflow obstruction in middle-age. Thorax. (2017) 72:990–7. doi: 10.1136/thoraxjnl-2016-209665
7. Mamane A, Baldi I, Tessier JF, Raherison C, Bouvier G. Occupational exposure to pesticides and respiratory health. Eur Respir Rev. (2015) 24:306–19. doi: 10.1183/16000617.00006014
8. Ratanachina J, De Matteis S, Cullinan P, Burney P. Pesticide exposure and lung function: a systematic review and meta-analysis. Occup Med. (2020) 70:14–23. doi: 10.1093/occmed/kqz161
9. Fareed M, Pathak MK, Bihari V, Kamal R, Srivastava AK, Kesavachandran CN. Adverse respiratory health and hematological alterations among agricultural workers occupationally exposed to organophosphate pesticides: a cross-sectional study in North India. PLoS ONE. (2013) 8:e69755. doi: 10.1371/journal.pone.0069755
10. Negatu B, Kromhout H, Mekonnen Y, Vermeulen R. Occupational pesticide exposure and respiratory health: a large-scale cross-sectional study in three commercial farming systems in Ethiopia. Thorax. (2017) 72:498–9. doi: 10.1136/thoraxjnl-2016-208924
11. Aloizou AM, Siokas V, Vogiatzi C, Peristeri E, Docea AO, Petrakis D, et al. Pesticides, cognitive functions and dementia: a review. Toxicol Lett. (2020) 326:31–51. doi: 10.1016/j.toxlet.2020.03.005
12. Kamel F, Hoppin JA. Association of pesticide exposure with neurologic dysfunction and disease. Environ Health Perspect. (2004) 112:950–8. doi: 10.1289/ehp.7135
13. Muñoz-Quezada MT, Lucero BA, Iglesias VP, Muñoz MP, Cornejo CA, Achu E, et al. Chronic exposure to organophosphate (OP) pesticides and neuropsychological functioning in farm workers: a review. Int J Occup Environ Health. (2016) 22:68–79. doi: 10.1080/10773525.2015.1123848
14. Daghagh Yazd S, Wheeler SA, Zuo A. Key risk factors affecting farmers' mental health: a systematic review. Int J Environ Res Public Health. (2019) 16:4849. doi: 10.3390/ijerph16234849
15. Kim JY, Park S, Kim SK, Kim CS, Kim TH, et al. Correction: pesticide exposure and cognitive decline in a rural South Korean population. PLOS ONE. (2019) 14: e0216310. doi: 10.1371/journal.pone.0216310 eCollection 2019
16. Cummings KJ, Johns DO, Mazurek JM, Hearl FJ, Weissman DN. NIOSH's respiratory health division: 50 years of and service. Arch Environ Occup Health. (2019) 74:15–29. doi: 10.1080/19338244.2018.1532387
17. Afshari M, Karimi-Shahanjarini A, Khoshravesh S, Besharati F. Effectiveness of interventions to promote pesticide safety and reduce pesticide exposure in agricultural health studies: a systematic review. PLoS ONE. (2021) 16:e0245766. doi: 10.1371/journal.pone.0245766
18. Liu XC, Pan L, Hu Q, Dong WP, Yan JH, Dong L. Effects of yoga training in patients with chronic obstructive pulmonary disease: a systematic review and meta-analysis. J Thorac Dis. (2014) 6:795–802. doi: 10.3978/j.issn.2072-1439.2014.06.05
19. Cramer H, Haller H, Klose P, Ward L, Chung VC, Lauche R. The risks and benefits of yoga for patients with chronic obstructive pulmonary disease: a systematic review and meta-analysis. Clin Rehabil. (2019) 33:1847–62. doi: 10.1177/0269215519860551
20. Santaella DF, Devesa CR, Rojo MR, Amato MB, Drager LF, Casali KR, et al. Yoga respiratory training improves respiratory function and cardiac sympathovagal balance in elderly subjects: a randomised controlled trial. BMJ Open. (2011) 1:e000085. doi: 10.1136/bmjopen-2011-000085
21. Abel AN, Lloyd LK, Williams JS. The effects of regular yoga practice on pulmonary function in healthy individuals: a literature review. J Altern Complement Med. (2013) 19:185–90. doi: 10.1089/acm.2011.0516
22. Beutler E, Beltrami FG, Boutellier U, Spengler CM. Effect of regular yoga practice on respiratory regulation and exercise performance. PLoS ONE. (2016) 11:e0153159. doi: 10.1371/journal.pone.0153159
23. Makwana K, Khirwadkar N, Gupta HC. Effect of short term yoga practice on ventilatory function tests. Indian J Physiol Pharmacol. (1988) 32:202–8.
24. Mooventhan A, Khode V. Effect of Bhramari pranayama and OM chanting on pulmonary function in healthy individuals: a prospective randomized control trial. Int J Yoga. (2014) 7:104–10. doi: 10.4103/0973-6131.133875
25. Sodhi C Singh S Dandona PK A A study of the effect of yoga training on pulmonary functions in patients with bronchial asthma. Indian J Physiol Pharmacol. (2009) 53:169–74.
26. Menne B, Aragon de Leon E, Bekker M, Mirzikashvili N, Morton S, Shriwise A, et al. Health and well-being for all: an approach to accelerating progress to achieve the Sustainable Development Goals (SDGs) in countries in the WHO European region. Eur J Public Health. (2020) 30(Suppl_1):i3–9. doi: 10.1093/eurpub/ckaa026
27. Gothe NP, McAuley E. Yoga and cognition: a meta-analysis of chronic and acute effects. Psychosom Med. (2015) 77:784–97. doi: 10.1097/PSY.0000000000000218
28. Sharma VK M R S V, Subramanian SK, Bhavanani AB, Madanmohan, et al. Effect of fast and slow pranayama practice on cognitive functions in healthy volunteers. J Clin Diagn Res. (2014) 8:10–3. doi: 10.7860/JCDR/2014/7256.3668
29. Whittle R, Mansell G, Jellema P, van der Windt D. Applying causal mediation methods to clinical trial data: what can we learn about why our interventions (don't) work?. Eur J Pain. (2017) 21:614–22. doi: 10.1002/ejp.964
30. Lee KM, Park SY, Lee K, Oh SS, Ko SB. Pesticide metabolite and oxidative stress in male farmers exposed to pesticide. Ann Occup Environ Med. (2017) 29:5. doi: 10.1186/s40557-017-0162-3
31. Della Morte R, Villani GR, Di Martino E, Squillacioti C, De Marco L, Vuotto P, et al. Glutathione depletion induced in rat liver fractions by seven pesticides. Boll Soc Ital Biol Sper. (1994) 70:185–92.
32. Mecdad AA Ahmed MH ElHalwagy MEA Afify MMM A A study on oxidative stress biomarkers and immunomodulatory effects of pesticides in pesticide-sprayers. Egyptian J Forensic Sci. (2011) 1:93–8. doi: 10.1016/j.ejfs.2011.04.012
33. Drost EM, Skwarski KM, Sauleda J, Soler N, Roca J, Agusti A, et al. Oxidative stress and airway inflammation in severe exacerbations of COPD. Thorax. (2005) 60:293–300. doi: 10.1136/thx.2004.027946
34. Patil SG, Dhanakshirur GB, Aithala MR, Naregal G, Das KK. Effect of yoga on oxidative stress in elderly with grade-I hypertension: a randomized controlled study. J Clin Diagn Res. (2014) 8:BC04–7. doi: 10.7860/JCDR/2014/9498.4586
35. Pal R, Gupta N. Yogic practices on oxidative stress and of antioxidant level: a systematic review of randomized controlled trials. J Complement Integr Med. (2017) 16:20170079. doi: 10.1515/jcim-2017-0079
36. Gordon L, McGrowder DA, Pena YT, Cabrera E, Lawrence-Wright MB. Effect of yoga exercise therapy on oxidative stress indicators with end-stage renal disease on hemodialysis. Int J Yoga. (2013) 6:31–8. doi: 10.4103/0973-6131.105944
37. Nasreddine ZS, Phillips NA, Bédirian V, Charbonneau S, Whitehead V, Collin I. The montreal cognitive assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. (2005) 53:695–9. doi: 10.1111/j.1532-5415.2005.53221.x
38. Quanjer PH, Stanojevic S, Cole TJ, et al. Multi-ethnic reference values for spirometry for the 3–95-yr age range: the global lung function 2012 equations. Eur Respir J. (2012) 40:1324–43. doi: 10.1183/09031936.00080312
39. Devakumar D, Stocks J, Ayres JG, Kigby J, Yadav SK, Saville NM, et al. Effects of antenatal multiple micronutrient supplementation on lung function in mid-childhood: follow-up of a double-blind randomised controlled trial in Nepal. Eur Respir J. (2015) 45:1566–75. doi: 10.1183/09031936.00188914
40. American Thoracic Society – Standardization of spirometry 1995 update. Am J respire Crit Care Med. (1995) 152:1107–36. doi: 10.1164/ajrccm.152.3.7663792
41. Initiative GL. FR Macro (2012). Available online at: https://wwwers-educationorg/guidelines/global-lung-function-initiative/spirometry-tools/r-macroaspx
42. Hall GL Stanojevic S GLI Network Executive Members Members of the GLI Network Executive. The Global Lung Function Initiative (GLI) Network ERS Clinical Research Collaboration: how international collaboration can shape clinical practice. Eur Respir J. (2019) 53:1802277. doi: 10.1183/13993003.02277-2018
43. Matarazzo JD, Herman D. Base rate data for the WAIS-R: test-retest stability and VIQ-PIQ differences. J Clin Neuropsychol. (1984) 6: 351–66. doi: 10.1080/01688638408401227
44. Jaeger J. Digit symbol substitution test: the case for sensitivity over specificity in neuropsychological testing. J Clin Psychopharmacol. (2018) 38:513–9. doi: 10.1097/JCP.0000000000000941
45. Bowie CR, Harvey PD. Administration and interpretation of the trail making test. Nat. Protoc. (2006) 1:2277–81. doi: 10.1038/nprot.2006.390
46. Reitan R. Validity of the trail making test as an indicator of organic brain damage. Percept Mot Skills. (1958) 8:271–6. doi: 10.2466/pms.1958.8.3.271
47. Olivera-Souza RD, Moll J, Passman LJ, Cunha FC, Paes F, Adriano MV, et al. Trail making and cognitive set-shifting. Arq Neuropsiquiatr. (2000) 58(3B):826–9. doi: 10.1590/s0004-282x2000000500006
48. Strauss E, Sherman EMS, Spreen O. A compendium of neuropsychological tests: administration, norms, and commentary. Arch Clin Neuropsychol. (2006) 21:819–25. doi: 10.1016/j.acn.2006.09.002
49. Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. (1983) 24:385–96.
50. Wiriyakijja P, Porter S, Fedele S, Hodgson T, McMillan R, Shephard M, et al. Validation of the HADS and PSS-10 and a cross-sectional study of psychological status in patients with recurrent aphthous stomatitis. J. Oral Pathol Med. (2020) 49:260–70. doi: 10.1111/jop.12991
51. Skevington SM, Lotfy M, O'Connell KA. WHOQOL Group. The world health organization's WHOQOL-BREF quality of life assessment: psychometric properties and results of the international field trial. A report from the WHOQOL group. Qual Life Res. (2004) 13:299–310. doi: 10.1023/B:QURE.0000018486.91360.00
52. Ohkawa H, Ohishi N, Yagi K. Assay for lipid peroxides in animal tissues by thiobarbituric acid reaction. Anal Chem. (1979) 95:351–8. doi: 10.1016/0003-2697(79)90738-3
53. Quanjer PH, Pretto JJ, Brazzale DJ, Boros PW. Grading the severity of airways obstruction: new wine in new bottles. Eur Respir J. (2014) 43:505–12. doi: 10.1183/09031936.00086313
54. Valeri L, Vanderweele TJ. Mediation analysis allowing for exposure-mediator interactions and causal interpretation: theoretical assumptions and implementation with SAS and SPSS macros. Psychol Methods. (2013) 18:137–50. doi: 10.1037/a0031034
55. Dhalla AS, Sharma S. Assessment of serum cholinesterase in rural punjabi sprayers exposed to a mixture of pesticides. Toxicol Int. (2013) 20:154–9. doi: 10.4103/0971-6580.117258
56. McGlothlin AE, Lewis RJ. Minimal clinically important difference: defining what really matters to patients. JAMA. (2014) 1:1342–3. doi: 10.1001/jama.2014.13128
57. Pourhassan B Meysamie A Alizadeh S Habibian A Beigzadeh Z. Risk of obstructive pulmonary diseases and occupational exposure to pesticides: a systematic review and meta-analysis. Public Health. (2019) 174:31–41. doi: 10.1016/j.puhe.2019.05.024
58. Lim SA, Cheong KJ. Regular yoga practice improves antioxidant status, immune function, and stress hormone releases in young healthy people: a randomized, double-blind, controlled pilot study. J Altern Complement Med. (2015) 21:530–8. doi: 10.1089/acm.2014.0044
59. Rahman I, MacNee W. Lung glutathione and oxidative stress: implications in cigarette smoke-induced airway disease. Am J Physiol. (1999) 277:L1067–88. doi: 10.1152/ajplung.1999.277.6.L1067
60. Richardson JR, Fitsanakis V, Westerink RHS, Kanthasamy AG. Neurotoxicity of pesticides. Acta Neuropathol. (2019) 138:343–62. doi: 10.1007/s00401-019-02033-9
61. Arbuthnott K, Frank J. Trail making test, part B as a measure of executive control: validation using a set-switching paradigm. J Clin Exp Neuropsychol. (2000) 22:518–28. doi: 10.1076/1380-3395(200008)22:4;1-0;FT518
62. Tombaugh TN. Trail making test A and B: normative data stratified by age and education. archives of clinical neuropsychology. Arch Clin Neuropsychol. (2004) 19:203–14. doi: 10.1016/S0887-6177(03)00039-8
63. Wojewódzka-Wiewiórska A, Kłoczko-Gajewska A, Sulewski P. Between the social and economic dimensions of sustainability rural areas—in search of farmers' quality of life. Sustainability. (2020) 12:148. doi: 10.3390/su12010148
64. Gladis MM, Gosch EA, Dishuk NM, Crits-Christoph P. Quality of life: expanding the scope of clinical significance. J Consult Clin Psychol. (1999) 67:320–31. doi: 10.1037//0022-006x.67.3.320
65. Suryatapa D, Annalakshmi C, Tapan KP. Organic farming in India: a vision towards a healthy nation. Food Qual Safet. (2020) 4:69–76.
66. Bawaskar PH, Bawaskar PH, Bawakar HS. India– science small progress in health care, decline in rural service. Lancet. (2015) 386:2389. doi: 10.1016/S0140-6736(15)01189-7
67. Fitogram: yoga-markt in Deutschland (2016). Avaialble online at: https://www.fitogram.pro/blog/yoga-markt-in-deutschland-2016/. (accessed September 21, 2018).
Keywords: farmers, pesticide exposure, breathing-focused yoga intervention, respiratory decline, cognitive decline
Citation: Dhansoia V, Majumdar V, Manjunath NK, Singh Gaharwar U and Singh D (2022) Breathing-Focused Yoga Intervention on Respiratory Decline in Chronically Pesticide-Exposed Farmers: A Randomized Controlled Trial. Front. Med. 9:807612. doi: 10.3389/fmed.2022.807612
Received: 02 November 2021; Accepted: 07 February 2022;
Published: 11 March 2022.
Edited by:
Hsiao-Chi Chuang, Taipei Medical University, TaiwanReviewed by:
Irma Ruslina Defi, Dr. Hasan Sadikin General Hospital, IndonesiaCopyright © 2022 Dhansoia, Majumdar, Manjunath, Singh Gaharwar and Singh. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Vijaya Majumdar, bWFqdW1kYXIudmlqYXlhQGdtYWlsLmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.