- 1Department of Anesthesiology, Beijing Tsinghua Changgung Hospital, School of Clinical Medicine, Tsinghua University, Beijing, China
- 2Department of Anesthesiology, Peking University First Hospital, School of Clinical Medicine, Peking University, Beijing, China
- 3Department of Anesthesiology, West China Hospital, Sichuan University, Chengdu, China
- 4Department of Anesthesiology, The Third Affiliated Hospital of Guizhou Medical University, Guiyang, China
- 5Department of Anesthesiology, The Central Hospital of Yongzhou, School of Clinical Medicine, University of South China, Hengyang, China
- 6Department of Anesthesiology, Kaifeng People's Hospital, Kaifeng, China
- 7Department of Anesthesiology, Xiangdu District Hospital, Xingtai, China
Background: Little is known about the recent use of neuromuscular blocking agents (NMBAs) and monitoring in China. This paper presents the results of a nationwide survey conducted to obtain information regarding the current management of NMBAs in China.
Methods: A questionnaire was sent to Chinese anesthesiologists inviting them to participate in the study. The questionnaire was available through the wenjuanxing website, and the link was sent to 1,488 anesthesiologists using the Wechat mini app.
Results: The web-based survey consisted of 28 questions, and data were collected using an online tool. Between May 19, 2021 and June 16, 2021, 637 responses were collected (response rate = 42.8%). Only 10.2% of anesthesiologists reported using neuromuscular function monitors, and 6.59% of respondents reported that they had the relevant monitors in the operating room.
Conclusion: Although PORC is a potential safety issue, the frequency of using reversal agents and monitors remains extremely low in China. Surveys such as this are important to understand the use and application customs of NMBAs in China.
Introduction
Neuromuscular blocking agents (NMBAs) are commonly used by anesthesiologists during surgery (1). Post-operative residual curarization (PORC) is an important risk factor for anesthesia-related mortality. Even minor degrees of residual block are associated with a weakness of the upper airway muscles, airway obstruction, increased risk of aspiration, and unpleasant muscle weakness. Incomplete post-operative neuromuscular recovery can also cause prolonged recovery room stay, hypoxemia and airway obstruction, awareness during emergence from anesthesia, and increased post-operative pulmonary complications (2–4).
According to the results of a multicenter investigation in China in 2015, in a clinical series of 1,571 patients undergoing elective open or laparoscopic abdominal procedures at 32 hospitals, the incidence of PORC at the time of endotracheal extubation was 57.8% (5). Similar findings have been documented in previous studies conducted in several countries, including several developed countries. Although there are strong recommendations from guidelines and consensus statements, the residual effects of muscle relaxants and their complications have not received sufficient attention (6–12).
The aim of the survey was to evaluate the use and application of neuromuscular blocking agents and monitoring in China. An online questionnaire was designed to understand the use conventions of neuromuscular blockers.
Methods
A cross-sectional questionnaire was sent to anesthesiologists registered in the following: Luffy Anesthesia Channel, Primary Anesthesia Network, Chinese Society of Anesthesiology, and Chinese Association of Anesthesiologists. Participants were invited via Wechat to complete an online survey, and encouraged to forward the invitations to colleagues. The questionnaire consisted of 28 questions, 6 investigating demographics, and 22 regarding the perioperative management of NMBAs, neuromuscular function monitoring, and antagonists. The participants accessed a link to a website for online data collection (wjx.cn) using the WeChat mini app. Data collection remained open from May 19, 2021 to June 16, 2021.
Results
The questionnaire was sent to 1,488 anesthesiologists. During the study period, 637 responses were collected anonymously (response rate = 42.5%).
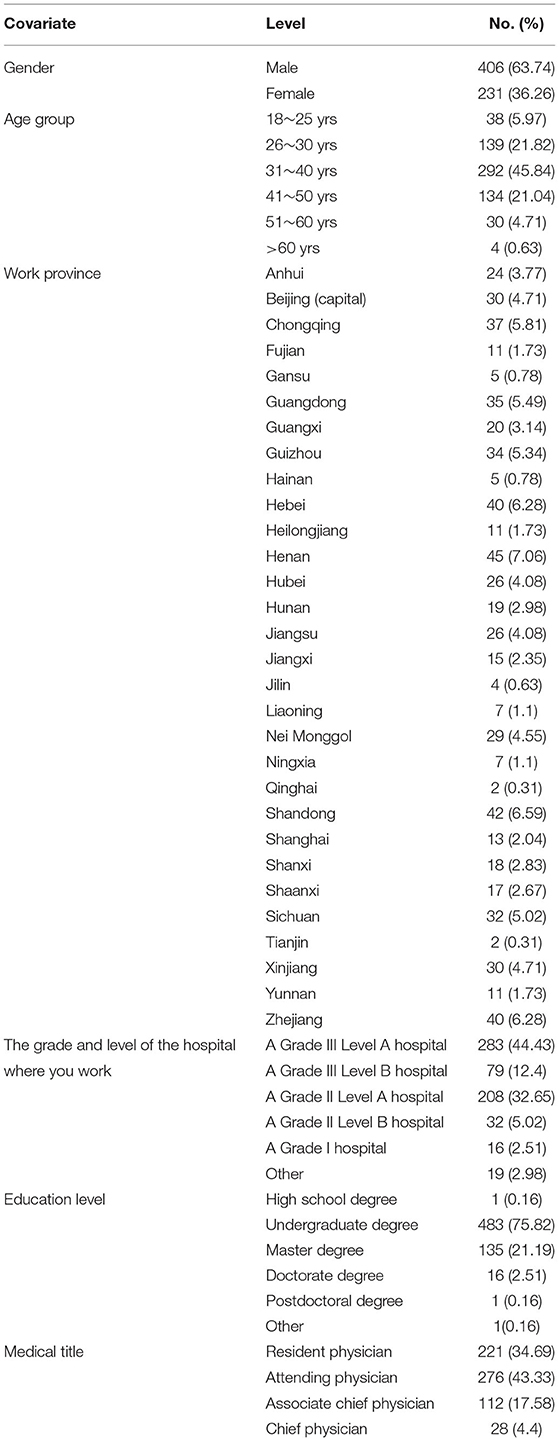
Regarding the rank of the responders, the questionnaires was answered by resident anesthesiologists (34.69%), attending anesthesiologists (43.33%), associate chief anesthesiologists (17.58%), and chief anesthesiologists (4.4%). Regarding the level of hospital, 44.43% of participants came from Grade III level A teaching hospitals (Table 1).
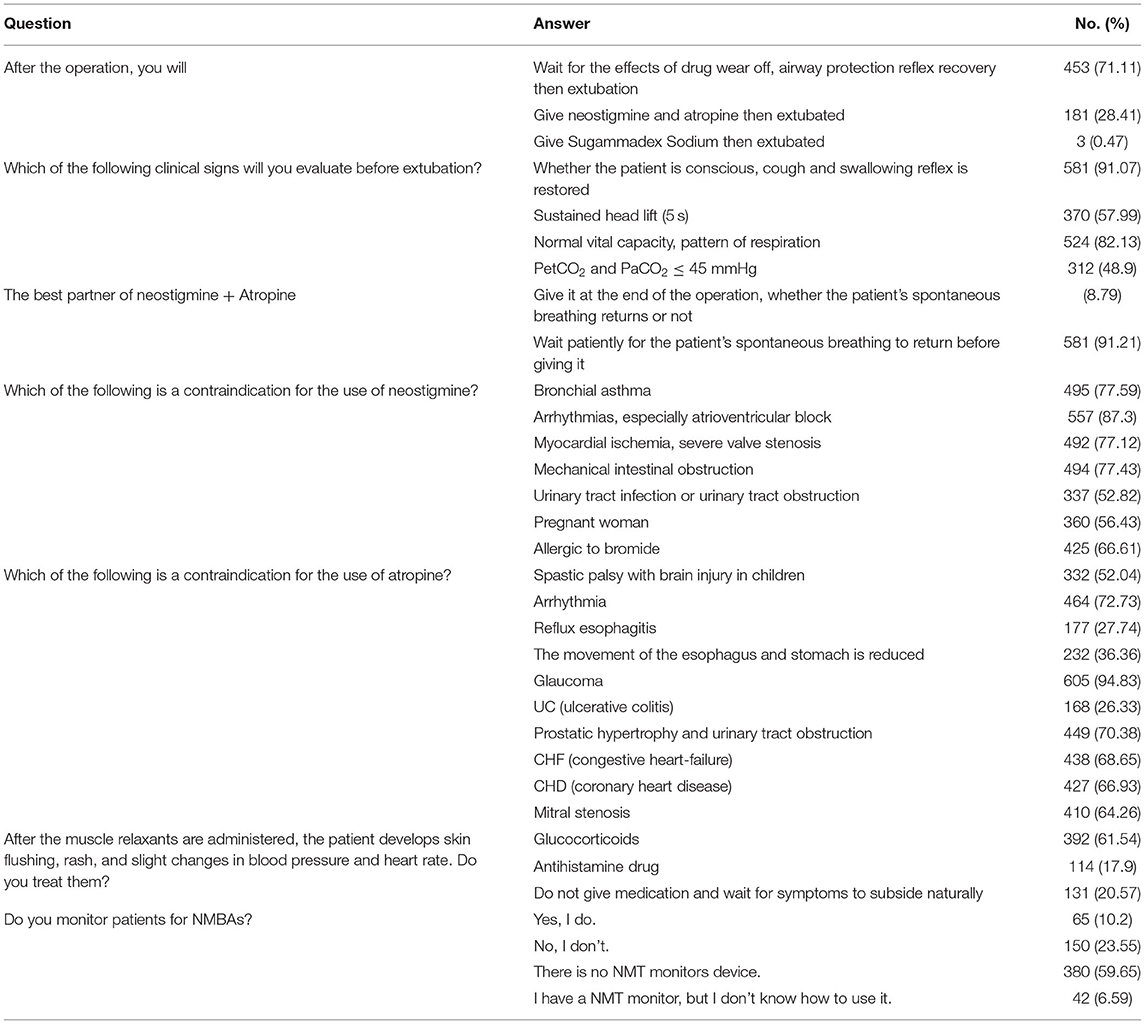
Cisatracurium (45.68%) and rocuronium (35.48%) were the most common neuromuscular blockers used during surgery (Table 2). Only 10.2% of anesthesiologists reported using neuromuscular function monitors, and 6.59% of respondents reported that they had such monitors in the operating room. A total of 71.11% of the respondents reported using only the post-operative clinical manifestation to evaluate if the patient had recovered from the muscle relaxant. Neuromuscular blockade reversal agents, such as sugammadex and neostigmine, were used in 0.47 and 28.41% of hospitals, respectively (Table 3).
Discussion
The aim of this study was to evaluate the use and application of neuromuscular blocking agents and monitoring in China.
Our survey showed that only 10.2% of Chinese anesthesiologists routinely monitored muscle relaxation, a rate that is very low compared to other countries. In another survey, 80.7% of Europeans and 90.6% of Americans used neuromuscular monitors (13). 71.11% of Chinese anesthesiologists in our study judged the recovery of muscle relaxation based solely on clinical manifestations. The ability of the patient to sustain their head in an elevated position for 5 s is the most commonly used test to assess the degree of residual muscle paralysis. However, such a test cannot be considered a reliable clinical test to detect significant degrees of residual neuromuscular block (14). A very recent seminal review article underlined the relevance of monitoring neuromuscular function when using NMBAs, both in anesthesia and intensive care unit, which should be an objective and quantitative NMFM, instead of a clinical, qualitative, and subjective assessment (15). Therefore, monitoring is recommended for patients receiving NMBAs, and it is the most objective and simple way to assess the recovery of muscle relaxation after surgery. There are many reasons for the low utilization rate of muscle relaxation monitoring. On the one hand, most anesthesiologists are overconfident in their patients' clinical performance. On the other hand, because of the cost of equipping muscle relaxation monitors with each operating room and the complexity of the monitoring method, monitoring is rarely performed, and indeed, many surgery rooms lack the requisite monitors. These results indicate that popularization of muscle relaxation monitors is very important; the Chinese Society of Anesthesiology, and the Chinese Association of Anesthesiologists should publish, promote, and provide education with relevant expert consensus and guidelines on these methods.
Our questionnaire reveals that 28.88% of the respondents reported using reversal agents to reverse neuromuscular blockade. Sugammadex and neostigmine were used in 0.47% and 28.41% of hospitals, respectively. This may be due to the fact that anesthesiologists in most Chinese hospitals prefer to judge muscle relaxant metabolism based on clinical symptoms and that most hospitals are not equipped with neuromuscular monitors. In a recent study, the rates of routine use of antagonists in Europe and the United States were only 18 and 34%, respectively, and quantitative monitors were available to fewer clinicians in the United States (22.7%) than in Europe (70.2%) (P < 0.0001) (13). In our survey, some anesthesiologists lacked an understanding of the contraindications of neostigmine and atropine, especially atropine, which reminds us to pay extra attention to these types of patients in clinical practice. Sugammadex is a modified gamma cyclodextrin that forms a complex with the non-depolarizing NMBAs rocuronium and vecuronium (16). However, because of its high price and lack of access in Chinese health insurance, only 0.47% of our questionnaire responders used it.
The results of our survey revealed several interesting findings. Most importantly, we discovered that half of the anesthesiologists chose the sedation-analgesic-NMBAs induction order, but there were significant differences in administration speed and intubation time. Most of the responses (63.89%) indicated administering 1–2 times the ED95 when the laryngeal mask was placed. For obese patients with BMI ≥40.0 kg/m2, 68.13% of the responses indicated using the standard body weight (SBW) to calculate the dosage of inducible muscle relaxants. Patients undergoing laparoscopic surgery should reach a degree of deep muscle relaxation in order to prevent the abdominal pressure from being too high, to ensure good operation exposure. Studies have shown that NMBAs can improve these conditions. However, in our survey, the laparoscopic deep muscle relaxation technique was not widely used (34.85%), and when the surgeon could not close the upper abdomen during laparotomy, 45.05% of anesthesiologists chose to administer patient's normal saline while mis-informing the surgeons that muscle relaxants had been added; this may be due to concerns regarding delayed extubation or increased post-operative complications. In 2013, a French survey reported that the incidence of anaphylaxis during local or general anesthesia was ~1 in 100 (among the 1,816 cases), most of which were muscle relaxants (1,068 cases) (17). In our survey, after muscle relaxants were administered, if the patients developed skin flushing, rash, or slight changes in blood pressure and heart rate, more than half of the anesthesiologists chose intravenous glucocorticoids (61.54%).
The main limitation of our study is its small sample size; therefore, caution is warranted with regard to the generalization of the results. The nature of the questionnaire-based investigation includes a risk of data inaccuracy. Despite the small sample size, the findings would be helpful in understanding the current use of NMBAs, neuromuscular monitoring, and antagonists. Another limitation of the current survey is that no further questions were asked regarding monitoring methods and equipment for muscle relaxation. Finally, another limitation is that our survey did not enquire about serious adverse effects of muscle relaxants, including severe respiratory depression, malignant hyperthermia, and allergies.
Conclusions
Our survey shows that NMBAs and antagonists are often administered without appropriate guidance. Most anesthesiologists are overconfident regarding their clinical manifestations. Moreover, there is poor awareness of the importance of muscle relaxant antagonist administration and monitoring.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Ethics Statement
The study protocol was approved by the Beijing Tsinghua Changgung Hospital Ethics Committee (21368-6-01).
Author Contributions
HW helped with the conceptualization, questionnaire design and validation, data curation, and original draft of the manuscript. ZL helped with investigation, provision of research background materials, and preparation of the published work. RZ helped with supervision of the execution of this national survey. SH helped with designing of this study and statistical analysis process. LJC helped with supervision of the execution of this national survey and questionnaire validation. YS helped with the conceptualization and provision of research background materials. LNC helped with provision of research background materials, manage, and coordination of this survey. HZ helped with conceptualization and reviewing of the final version of manuscript. All authors contributed to the article and approved the submitted version.
Funding
Financial support for this study was provided, in part, by departmental funding.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
Authors thank to the Luffy Anesthesia Channel, Primary Anesthesia Network, the Chinese Society of Anesthesiology, and the Chinese Association of anesthesiologist.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2022.770105/full#supplementary-material
References
1. Utting JE. The era of relaxant anaesthesia. Br J Anaesth. (1992) 69:551–3. doi: 10.1093/bja/69.6.551
2. Grosse-Sundrup M, Henneman JP, Sandberg WS, Bateman BT, Uribe JV, Nguyen NT, et al. Intermediate acting non-depolarizing neuromuscular blocking agents and risk of post-operative respiratory complications: prospective propensity score matched cohort study. BMJ. (2012) 345:e6329. doi: 10.1136/bmj.e6329
3. Bronsert MR, Henderson WG, Monk TG, Richman JS, Nguyen JD, Sum-Ping JT, et al. Intermediate-acting nondepolarizing neuromuscular blocking agents and risk of postoperative 30-day morbidity and mortality, and long-term survival. Anesth Analg. (2017) 124:1476. doi: 10.1213/ANE.0000000000001848
4. Kirmeier E, Eriksson LI, Lewald H, Jonsson Fagerlund M, Hoeft A, Hollmann M, et al. Post-anaesthesia pulmonary complications after use of muscle relaxants (POPULAR): a multicentre, prospective observational study. Lancet Respir Med. (2019) 7:129–40. doi: 10.1016/S2213-2600(18)30294-7
5. Yu B, Ouyang B, Ge S, Luo Y, Li J, Ni D, et al. Incidence of postoperative residual neuromuscular blockade after general anesthesia: a prospective, multicenter, anesthetist-blind, observational study. Curr Med Res Opin. (2016) 32:1–9. doi: 10.1185/03007995.2015.1103213
6. Söderström CM, Eskildsen KZ, Gätke MR, Staehr-Rye AK, Objective neuromuscular monitoring of neuromuscular blockade in Denmark: an online-based survey of current practice. Acta Anaesthesiol Scand. (2017) 61:619–26. doi: 10.1111/aas.12907
7. Pongrácz A, Nemes R, Breazu C, Asztalos L, Mitre I, Tassonyi E, et al. International survey of neuromuscular monitoring in two European countries: a questionnaire study among Hungarian and Romanian anaesthesiologists. Rom J Anaesth Intensive Care. (2019) 26:45–51. doi: 10.2478/rjaic-2019-0007
8. Fink H, Fink H, Geldner G, Fuchs-Buder T, Hofmockel R, Blobner M. [Muscle relaxants in Germany 2005: a comparison of application customs in hospitals and private practices]. Anaesthesist. (2006) 55:668–78. doi: 10.1007/s00101-006-1015-6
9. Cammu GV, Klewais LR, Vandeput DM, Foubert LA. Neuromuscular monitoring, reversal and postoperative residual neuromuscular block: an intradepartmental survey over the years. Anaesth Intensive Care. (2020) 48:73–5. doi: 10.1177/0310057X19897655
10. Nauheimer D, Fink H, Fuchs-Buder T, Geldner G, Hofmockel R, Ulm K, et al. Muscle relaxant use for tracheal intubation in pediatric anaesthesia: a survey of clinical practice in Germany. Paediatr Anaesth. (2009) 19:225–31. doi: 10.1111/j.1460-9592.2008.02803.x
11. Bouderka MA, Nsiri A, Bouhouri A, Bouaggad A, Alharrar R, Hamoudi D. [Moroccan survey about neuromuscular relaxant blocking drugs use and reversal management]. Ann Fr Anesth Reanim. (2014) 33:21–5. doi: 10.1016/j.annfar.2013.06.018
12. Locks Gde F, Cavalcanti IL, Duarte NM, da Cunha RM, de Almeida MC. Use of neuromuscular blockers in Brazil. Braz J Anesthesiol. (2015) 65:319–25. doi: 10.1016/j.bjane.2015.03.001
13. Naguib M, Kopman AF, Lien CA, Hunter JM, Lopez A, Brull SJ. A survey of current management of neuromuscular block in the United States and Europe. Anesth Analg. (2010) 111:110–9. doi: 10.1213/ANE.0b013e3181c07428
14. Naguib M, Brull SJ, Kopman AF, Hunter JM, Fülesdi B, Arkes HR, et al. Consensus statement on perioperative use of neuromuscular monitoring. Anesth Analg. (2018) 127:71–80. doi: 10.1213/ANE.0000000000002670
15. Naguib M, Brull SJ, Hunter JM, Kopman AF, Fülesdi B, Johnson KB, et al. Anesthesiologists' overconfidence in their perceived knowledge of neuromuscular monitoring and its relevance to all aspects of medical practice: an international survey. Anesth Analg. (2019) 128:1118–26. doi: 10.1213/ANE.0000000000003714
Keywords: NMBAs, neuromuscular monitoring, residual neuromuscular block, survey, reversal
Citation: Wu H, Lin Z, Zhou R, Huang S, Chen L, Su Y, Cheng L and Zhang H (2022) Neuromuscular Blocking Agents and Monitoring in China: A Cross-Sectional Survey of Current Management. Front. Med. 9:770105. doi: 10.3389/fmed.2022.770105
Received: 03 September 2021; Accepted: 31 March 2022;
Published: 27 April 2022.
Edited by:
Ahmet Eroglu, Karadeniz Technical University, TurkeyReviewed by:
Francesco Forfori, University of Pisa, ItalyCopyright © 2022 Wu, Lin, Zhou, Huang, Chen, Su, Cheng and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Huan Zhang, d2h0YTAxOTU2QGJ0Y2guZWR1LmNu
 HaoTian Wu
HaoTian Wu ZengMao Lin2
ZengMao Lin2 RuiHao Zhou
RuiHao Zhou