- 1Department of Social Medicine, College of Health Management, China Medical University, Shenyang, China
- 2Department of Humanities and Social Sciences, China Medical University, Shenyang, China
- 3Department of Public Health, Pennsylvania State University College of Medicine, Hershey, PA, United States
Background: Coronavirus Disease-19 (COVID-19), a rising global pandemic, has triggered psychological crises among the public. Panic, a severe symptom of mental disorders, is increasing in the public in China and it is urgent to provide research for intervention development.
Objectives: This study aimed to assess the prevalence of public panic in China during the earliest stage of the COVID-19 pandemic and to explore the associated psychological behavioral responses and public's risk perception of the pandemic.
Methods: A cross-sectional study using a web-based survey with convenience sampling was conducted with 2,484 participants nationally from February 11 to February 24, 2020 in China. A self-developed questionnaire was applied to assess the prevalence of public panic and its associated factors. Multivariable logistic regression analysis was applied to assess the risk and protective factors of public panic.
Results: There were 23.39% (581/2,484) of the participants who reported experiencing panic during the earliest stage of the COVID-19 pandemic. Taking temperature repeatedly, being nervous in a crowd, being suspicious of infection in the family, being worried about the future, and worries about high infectivity of the COVID-19, lack of effective therapies, and wide impact of the COVID-19 pandemic increased the odds of public panic. Whereas, avoiding gatherings during holidays was negatively associated with the odds of public panic.
Conclusions: Psycho-behavioral responses were closely associated with public panic during the earliest stage of the COVID-19 pandemic in China. Defusing excessive health-related worries, the guidance of appropriate self-protective behaviors, strengthening of health education in communities, and available treatment for mental disorders should be adopted to monitor the psychological responses and to guide the behaviors of the public.
Introduction
Coronavirus Disease-19 (COVID-19) has become an unprecedented enormous challenge facing mankind. It has not only affected human health and global development but has also caused social shutdowns and major economic damage. COVID-19 has not only caused a public health crisis, but it has also resulted in an information crisis (1–4). To slow the spread of COVID-19 in China, compulsory actions comprising the establishment of targeted hospitals, restrictions on traffic, community isolation, etc., have been taken (5). However, growing research has found that negative psychological responses, such as indifference, paranoia, sadness, fear, and anxiety, have increased during the COVID-19 pandemic (6–8). Mental health crises are also closely associated with the experience of public health emergencies (9–11). The decline in the public's mental wellbeing especially the high prevalence of psychological distress and panic has raised considerable concerns among medical fields, which will require urgent assessment and management (12–15).
The mental wellbeing of the public during the COVID-19 pandemic has highlighted multidimensional risk factors. Research on the behavioral immune system indicates that pandemics can induce extreme responses, such as persistent doubting and checking and excessive sensations about minor bodily ailments (16, 17). As the cognitive account of panic attacks presented, panic could result from a misinterpretation of external events, and interventions providing accurate and reliable information may be effective to prevent public panic (18–20). Additionally, the danger-laden schemas in mental disorders also suggest the appraisal of events as threatening because of the high-risk perception (21–23). In summary, panic can be triggered by physiological, psychological, and environmental factors during the unexpected suffering experiences.
Most people have paid attention to public health information about the pandemic and personal protection, adopting social distancing measures, regular hand washing and mask wearing, and canceling their social and travel plans. While public health measures are essential to fight against COVID-19, these measures have changed the public's sense of security, which have led to higher levels of stress, emotional disturbances, irrational anger, panic, impulsivity, anxiety, and depression among the public during the initial phase of the COVID-19 pandemic in China. Further, home confinement, being worried about family members exposed to COVID-19, the shortage of personal protective equipment, uncertainties of education or work progression, and the inaccuracy of the health information have exacerbated negative mental health (24–29). A stimulus-organism-response model proposed by a recent study indicates that information-avoidance behavior and perceived information overload are associated with sadness, anxiety, and cognitive dissonance during the COVID-19 pandemic (30–33). A variety of adverse conditions, such as public panic, are critical to be acknowledged and measured.
Additionally, behavioral changes are common during public health emergencies. For example, the social restrictions were consistently related to changes in behaviors, such as reduced physical activity, using hand sanitizer, panic buying and hoarding, and poor eating behaviors, during the COVID-19 pandemic (34–38). The Health Belief Model indicates that cognitive processing has a strong connection with the perception of risks and protective behaviors (39, 40). Furthermore, the integrative cognitive model of panic attacks and the neuroanatomical theory suggest that the cognition and apprehension of trigger stimulus are associated with panic (18, 23, 41, 42). Additionally, anxiety and cognitive risks are closely associated with protective behaviors (e.g., avoiding crowds, disinfecting the living environment) during the epidemic, especially during the early stage (43). Psycho-behavioral responses and panic share a close and significant relationship during the unexpected pandemic and accompany changes in daily life.
Various psychological responses could be correlated with public panic during the COVID-19 pandemic for personal protection, such as being nervous in a crowd, being worried about the future, being afraid of the recurrence of the COVID-19 pandemic, and being suspicious that infected people exist are around. Plenty of excessive protective behaviors may also significantly impact public panic, such as repeated temperature measurement and avoidance of gatherings during the holidays. Therefore, exploring the associations between the psycho-behavioral responses, the risk perception of the pandemic, and panic is crucial for the enhancement of public mental health during the COVID-19 pandemic.
Materials and Methods
Participants, Procedure, and Ethics Statement
From February 11 to 24, 2020, a cross-sectional survey was conducted in 2,484 participants using convenience sampling in mainland China. A link of the self-administrated questionnaire developed by the Environmental Health Institute at China Medical University was distributed via WeChat, one of the most popular social media platforms in China. The inclusion criteria of participants were as follows: at least 18 years of age; able to comprehend and complete the online questionnaire in Chinese independently; willing to participate in the study and; and able to provide signed informed consent. The exclusion criteria of the participants were as follows: having a history of the severe psychological disease (e.g., schizophrenia, bipolar disorder, mental disorders caused by epilepsy); having current psychological therapy; and having been diagnosed with diseases which limited the participation in this survey.
The validated questionnaire contained self-developed questions about panic, psycho-behavioral responses to the COVID-19 pandemic, and the risk perception of the COVID-19 pandemic. The questionnaire took about 20 min to complete. All of the procedures of this survey followed the Helsinki Declaration as revised in 1989 and the protocol authorized by the Ethics Committee of China Medical University (ID: 2020048).
Demographic Characteristics of the Participants
The gender (male, female), age, marital status (married, other), occupation (government worker/healthcare worker/employee of an enterprise/student/other [e.g., commercial personnel, soldier, teacher, etc.]), education (college and below, bachelor's degree, master's degree, or above), and monthly income (≤ 5,000 yuan [ ≤ US $725.19], 5,001–10,000 yuan [US $725.34–1,450.39], and >10,000 yuan [>US $1,450.39]) were collected as demographic characteristics.
Assessment of Public Panic
A self-developed question was applied to measure the public panic among the public. Public panic was collected using a yes or no question: “I was panicked during the COVID-19 pandemic” with choices including “yes” or “no”.
Assessment of Psycho-Behavioral Responses
Behaviors in the past 2 weeks, such as “Taking temperature repeatedly”, “being nervous in a crowd”, “being suspicious of infection in the family”, “being worried about the future”, “being afraid of the recurrence of the COVID-19 pandemic”, “being constantly reminded of the COVID-19 pandemic by the surroundings”, “being suspicious that infected people are around”, and “avoiding gatherings during the holidays” comprised the collected psycho-behavioral responses. The psycho-behavioral responses were assessed by self-developed “yes” or “no” questions.
Assessment of Risk Perception of the COVID-19 Pandemic
The perception of risk during the COVID-19 pandemic was assessed with a multiple-choice question. The choices included worries about high infectivity of COVID-19; lack of effective therapies; the wide impact of the COVID-19 pandemic; lack of medical supplies and healthcare workers; sequelae after recovery from COVID-19; extensive announcements, rumors, and nervousness; extensive media coverage; and news of the pandemic on the internet.
Statistical Analyses
This study carried out the statistical analyses with SPSS version 23.0 statistical software for Windows (IBM Corporation). The relationship between public panic and other variables was explored with chi-square tests. The risk factors and preventive factors of public panic were explored with multivariable logistic regression analysis. Associations were considered significant when there was a two-tailed p < 0.05.
Results
Demographic Characteristics and Public Panic Distribution of the Public
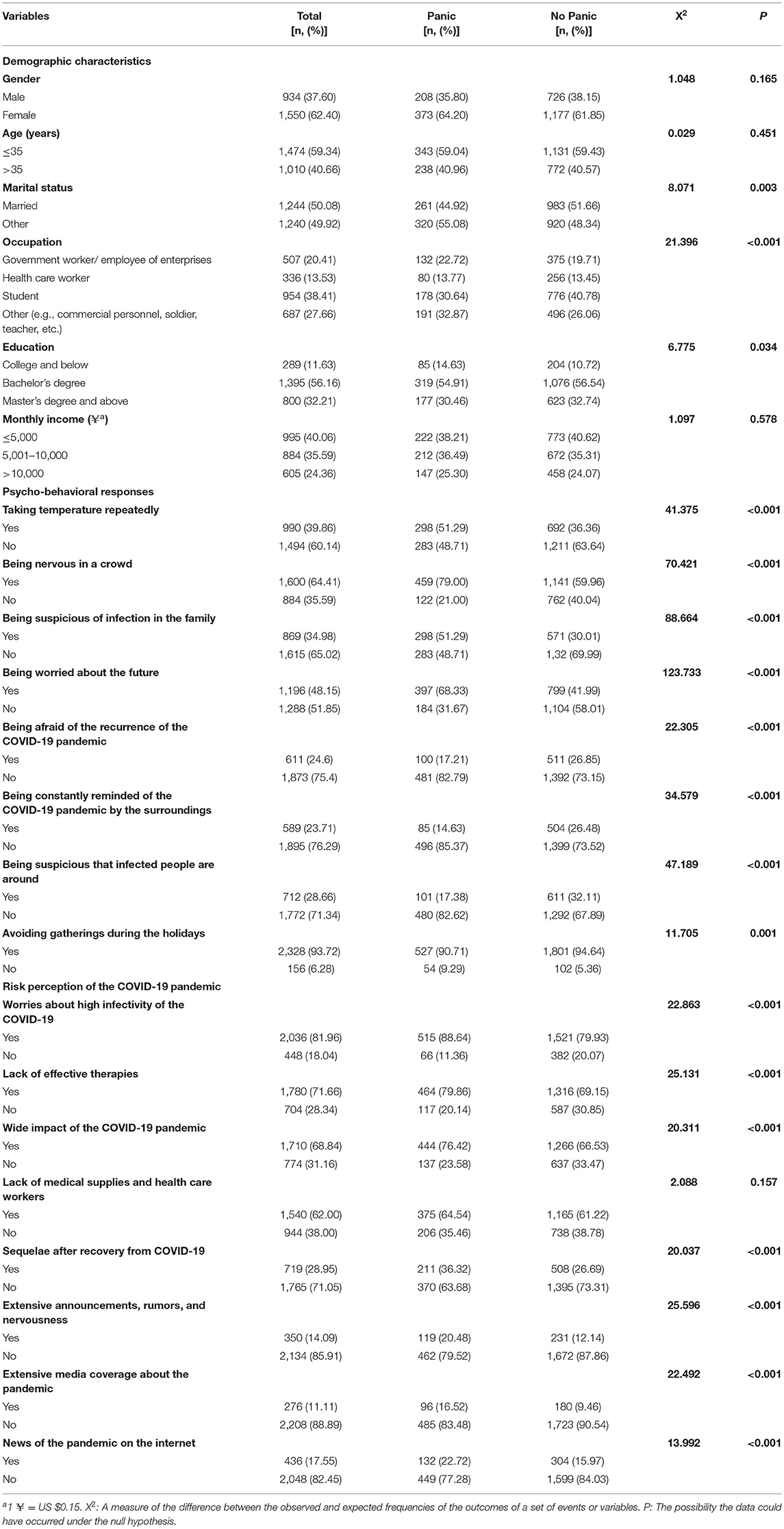
The prevalence of public panic during the earliest stage of the COVID-19 pandemic was 581/2,484 (23.39%). The results from the chi-square tests on public panic are shown in Table 1. The participants who were not married (1,240/2,484, 49.92%) had a higher prevalence of panic (p = 0.022). Differences in participants panic by education level (p = 0.034) and occupations (p < 0.001) were also significant.
Psycho-Behavioral Responses
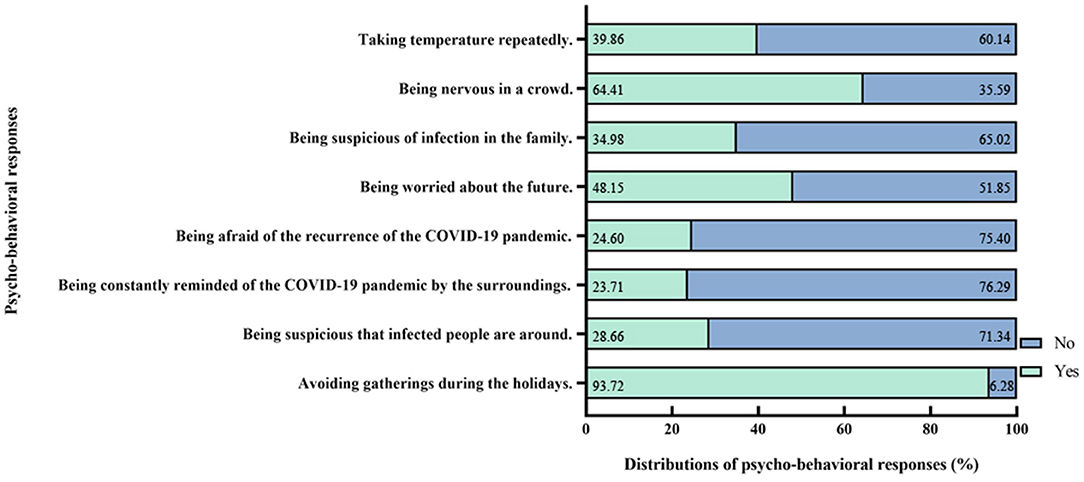
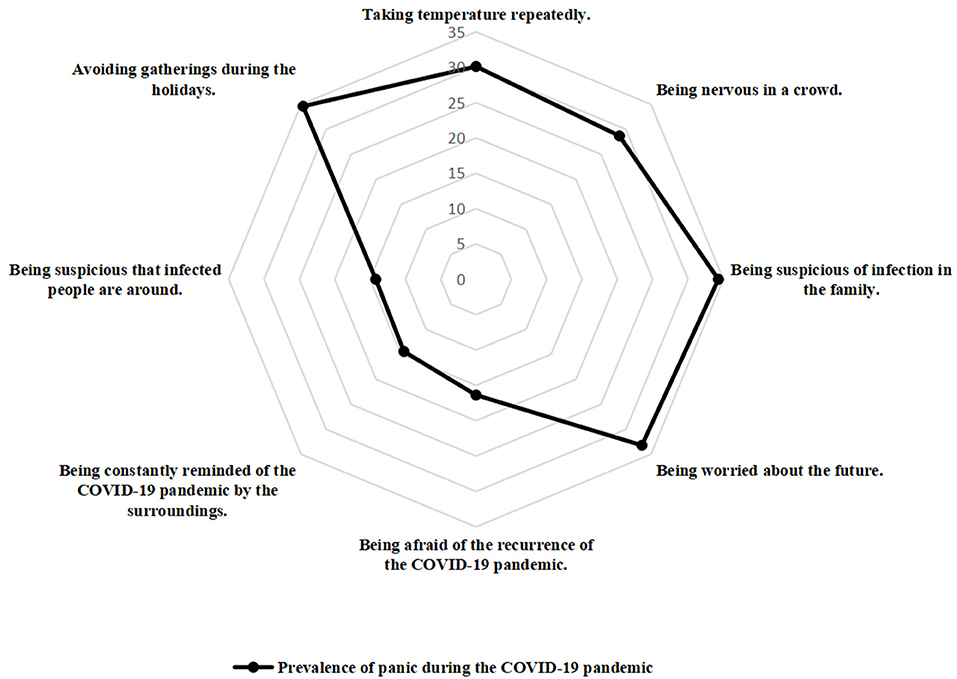
The psycho-behavioral responses and corresponding prevalence of public panic are also presented in Table 1; Figures 1, 2. Taking temperature repeatedly (990, 39.86%), being nervous in a crowd (1,600, 64.41%), being suspicious of infection in the family (869, 34.98%; p < 0.001), being worried about the future (1,196, 48.15%), being afraid of the recurrence of the COVID-19 pandemic (611, 24.60%), being constantly reminded of the COVID-19 pandemic by the surroundings (589, 23.71%), and being suspicious that infected people are around (712, 28.66%; p < 0.001), and avoiding gathering during the holidays (2,328, 93.72%; p = 0.001) were all significant factors of public panic.
Risk Perception of the COVID-19 Pandemic
Participates' risk perception of the COVID-19 pandemic and the corresponding prevalence of panic are shown in Table 1; Figures 3, 4. Worries of high infectivity of COVID-19 (2,036/2,484, 81.96%); lack of effective therapies (1,780, 71.66%); wide impact of the COVID-19 pandemic (1,710/2,484, 68.84%); sequelae after recovery from COVID-19 (719/2,484, 28.95%); extensive announcements, rumors, and nervousness (350, 14.09%; p < 0.001); extensive media coverage about the pandemic (276/2,484, 11.11%); and news of the pandemic on the internet (436/2,484, 17.55%; p < 0.001) were significantly associated with public panic.
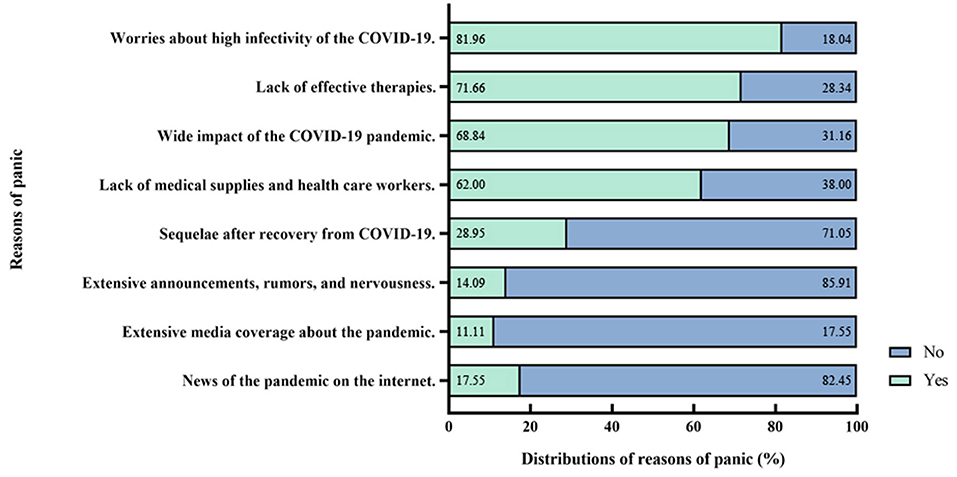
Figure 3. Risk perception of the Coronavirus Disease-2019 (COVID-19) pandemic and distributions of panic.
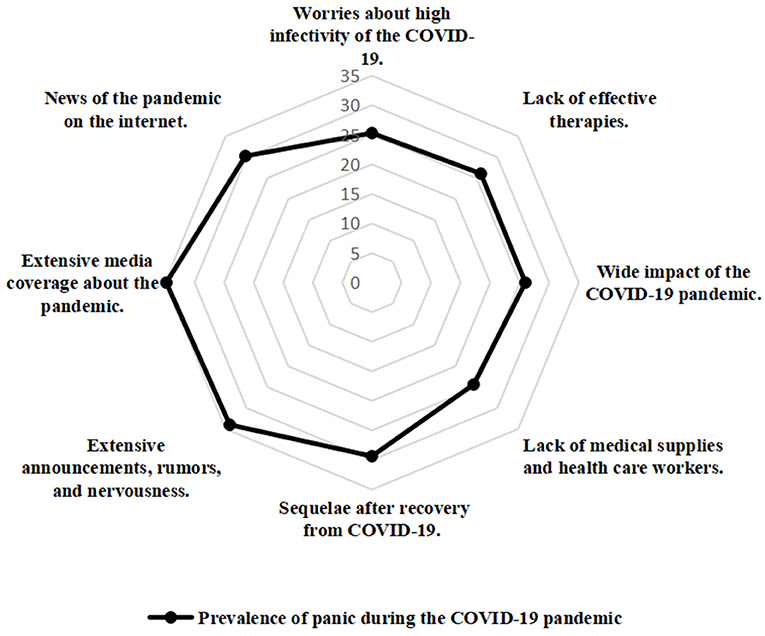
Figure 4. The radar map of the distribution of the public panic (risk perception of the Coronavirus Disease-2019 (COVID-19) pandemic).
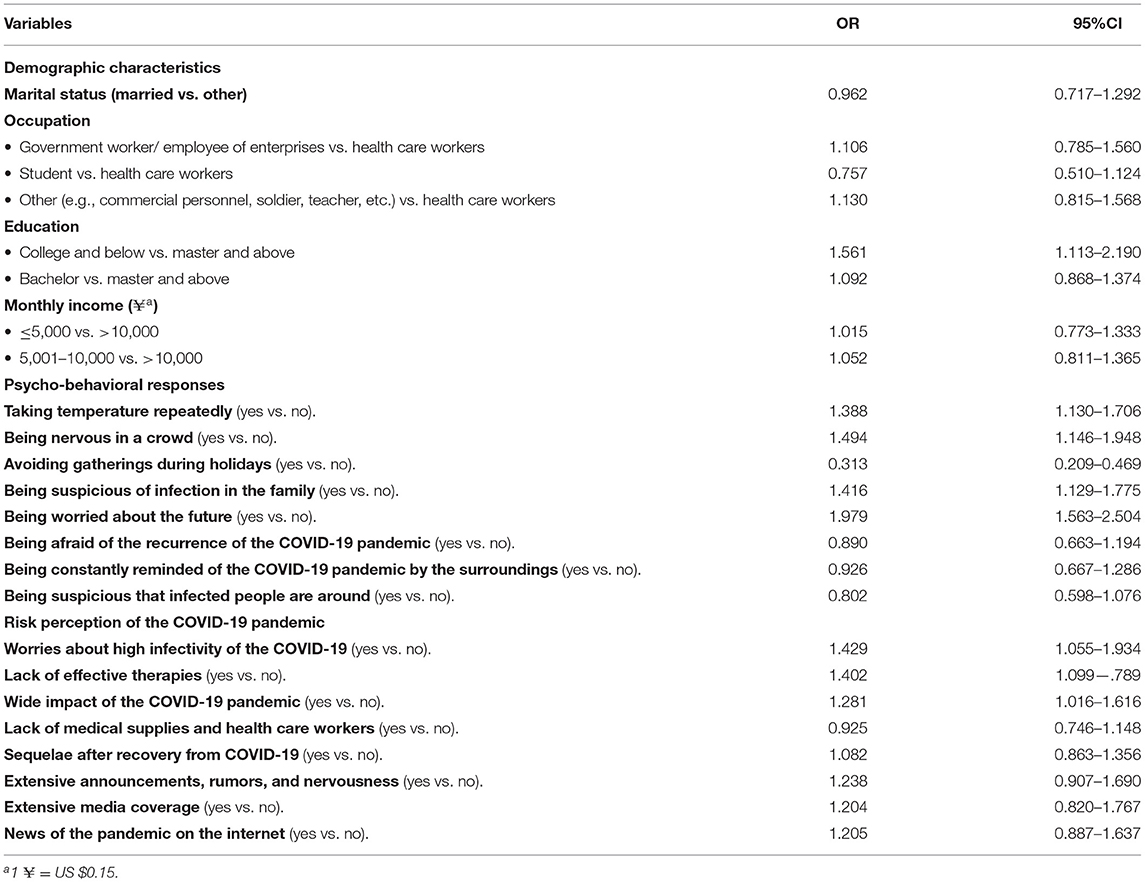
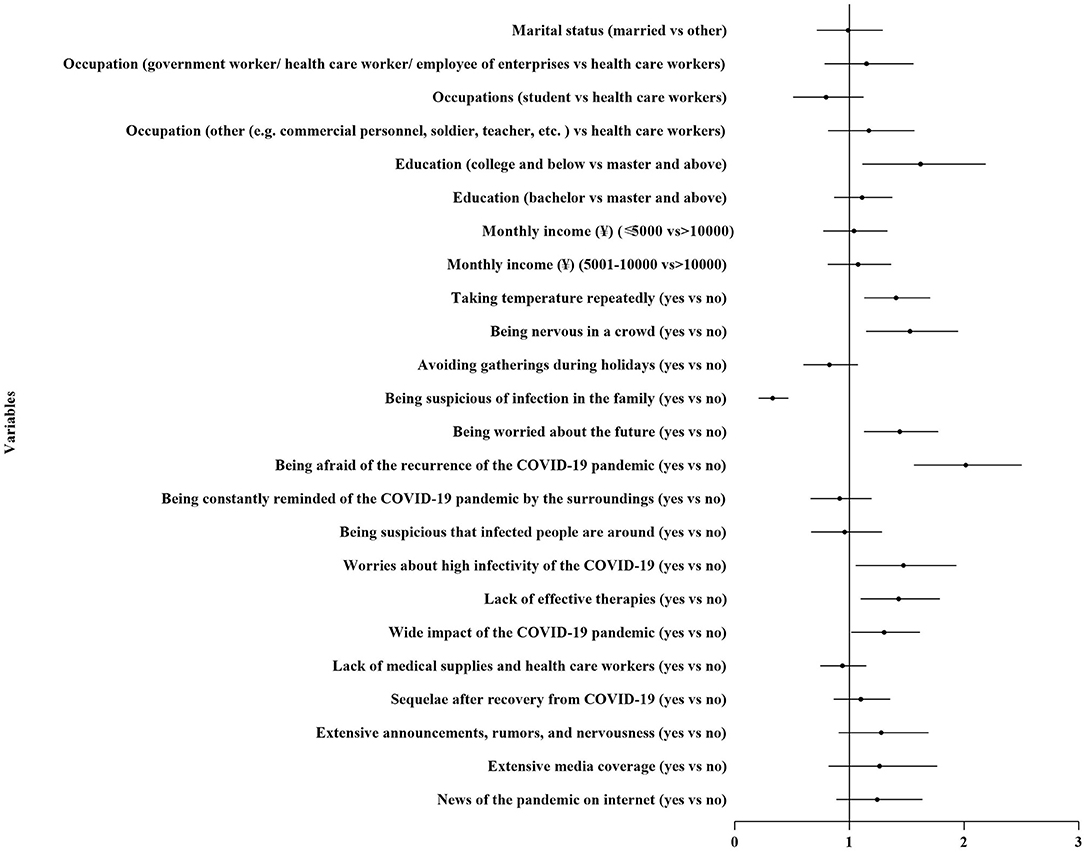
Risk Factors and Associated Factors of Public Panic During the COVID-19 Pandemic
The results from the multivariable logistic regression are presented in Table 2 and Figure 5. Psycho-behavioral responses, such as taking temperature repeatedly (odds ratio [OR] 1.388, 95% CI 1.130–1.706), being nervous in a crowd (OR 1.494, 95% CI 1.146–1.948), being suspicious of infection in the family (OR 1.416, 95% CI 1.128–1.775), and being worried about the future (OR 1.979, 95% CI 1.563–2.504) increased the chances of panic. Among those with worries about high infectivity of the COVID-19 (OR 1.429, 95% CI 1.055–1.934), lack of effective therapies (OR 1.402, 95% CI 1.099–1.789), and wide impact of the COVID-19 pandemic (OR 1.281, 95% CI 1.016–1.616) also increased the chances of panic. Inversely, avoiding gatherings during holidays (OR 0.313, 95% CI 0.209–0.469) decreased the chances of panic.
Discussion
Principal Findings
Our study found that the prevalence of public panic was 23.39% during the earliest stage of the COVID-19 pandemic in China. The prevalence of panic was higher than the prevalence before the pandemic (5.6–13.2%) (44–47). The pandemic has seriously threatened people's daily life and greatly disrupted the normal social order, resulting in tremendous changes in population health, and inducing the prevalence of public panic. It has been found in recent studies that the pandemic can trigger the negative emotions, such as sadness, worry and fear, and increase public's vulnerability to mental disorders, such as panic, social anxiety, depression, and post-traumatic stress disorder (48–52). During this vital period, the examination of public panic and the associated factors are indispensable, but also scarce.
Results from our study indicate that panic is significantly associated with psycho-behavioral responses. The psycho-behavioral responses, such as taking temperature repeatedly, being nervous in a crowd, being worried about the future, being afraid of the recurrence of the COVID-19 pandemic, being suspicious of infection in the family, and being worried about the future, were the key risk factors of public panic. Whereas, avoiding gatherings during holidays could decrease the possibility of public panic. The public has paid more attention to personal protection because of the severe impacts of COVID-19 in China. It is common for the public to adopt social distancing measures, mask wearing, frequent hand washing, and canceling social activities during the pandemics to reduce disease spread (53, 54). While the public health measures were necessary to prevent the spread of COVID-19, the impact on public behaviors and risk perception damaged mental wellbeing (55, 56). Previous research also reported that social distancing behaviors, a common response to avoid infection, were associated with negative psychological responses (57, 58). The rapid changes during the COVID-19 pandemic raised problems in social order and development of finance, resulting in risks threatening people's health, stable income, and living quality, triggering further public panic and other mental disorders.
The results of our survey were in agreement with the findings in recent studies that during the public health emergencies, the disruption of daily routine, the uncertainty of epidemic, the threats to wellbeing, and the wide range of disease-related information were the main factors associated with psychological distress including fear, anxiety, depression, and panic (59–61). Strengthening the understanding of psychological responses and their impact on mental health, reducing public panic, and effectively managing irrational responses have become prominent issues that need to be resolved globally in order to reduce the detrimental impacts of the pandemic on people's psychological health. Therefore, psychological interventions and guidance on behaviors during public health emergencies should be developed and popularized among the public to help them regulate negative psychological changes and to cope with the pandemic with appropriately rational behaviors.
In addition, the public panic was associated with risk perception of the COVID-19 pandemic. In this study, worries about the high infectivity of the COVID-19, worried about lack of effective therapies, and wide impact of the COVID-19 pandemic have increased the public's risk perception of the COVID-19 threat. Cognitive responses are associated with behavior coping and perception of the pandemic (62, 63). Perceptions of the pandemic, such as the mode of transmission, symptoms and therapies of the disease, proper self-protective behaviors, the importance of early detection, and treatment of mental disorders, should be enhanced among the public through official channels (64–66). Besides, the worries about potential risks of tough treatment experience, huge medical cost, long time of recovery, delay of study plan, or unemployment raised from infection of COVID-19 might be part of the influencing factors of panic.
In addition to the variables as above, the outcomes of the chi-square test also indicated that the prevalence of panic was also higher among the participants who were concerned about sequelae after recovery from COVID-19; extensive announcements, rumors, and nervousness; extensive media coverage; and news of the pandemic on the internet. The methods of acquisition of health information were also significantly associated with poor mental wellbeing and public's knowledge and attitude about the COVID-19 pandemic (11, 67, 68). While the various sources of pandemic-related information provide convenience for the public to access information in a timely manner, the accuracy and authenticity of the health information were hard to guarantee, resulting in a wide diversity of psychological-behavioral responses, or even triggering public panic (69, 70).
The general public is vulnerable to excessively high-risk perception and uncoordinated behavioral responses during a public health emergency (71, 72). Negative psychological impacts raised by inappropriate risk perception of the COVID-19 pandemic can seriously affect the public's normal life and mental health (9, 10, 32). Although people should protect their health, they should also adjust their risk perceptions and enhance their coping mechanisms during epidemics (73, 74). A recent study found that <50% of the public had sufficient and appropriate risk perception of the COVID-19 pandemic to ensure their wellbeing (75). Educational programs could resolve the misconceptions about the COVID-19 pandemic (76). It is vital for the public to perceive the pandemic within a controllable range with reliable sources of health information and to cope with pandemic-related stressors in healthy ways with available instructions from psychological professionals during public health emergencies.
Limitations
This study has several limitations. First, since the prevalence of panic is analyzed with a self-developed question, the generalizability of the outcomes is limited to other populations. Second, this survey was conducted during the earliest stage of the COVID-19 pandemic. Therefore, the collected data can only represent this special period, and the generalizability of the results to the other stages of the COVID-19 pandemic might be limited. Third, the results are limited by selection bias because the survey was conducted on the WeChat platform and the participants were only smartphone users. Finally, the results may be limited due to unmeasured confounders, such as gender-based violence and family violence.
Conclusions
The public in mainland China has suffered from the high prevalence of public panic during the earliest stage of the COVID-19 pandemic. The public panic stemmed from a variety of factors, such as excessive self-protective behaviors, such as taking temperature repeatedly, being nervous in a crowd, being suspicious of infection around; and inappropriate risk perception of the COVID-19 pandemic, such as worries about high infectivity of the COVID-19, lack of effective therapies and wide impact of the COVID-19 pandemic. Timely prevention and screenings of panic should be enhanced for the public to keep their mental status stable and healthy. This could be accomplished by managing health information, guiding appropriate self-protective behaviors, strengthening health education in communities, and promoting treatments of mental disorders.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by the Ethics Committee of China Medical University. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
WZ and CZ analyzed the data and drafted and revised the manuscript. KS revised the manuscript. CC, JF, SH, QP, and QC contributed to the acquisition and interpretation of data. XY was responsible for the conception and design and the revision of the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This study was conducted with the support from Research on Behaviors Rules and Emotions of the Public during the COVID-19 Epidemic, Public Behavior Research Project of Prevention and Control of COVID-19, and China Medical University (Grant Number: 121-1210120025).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
All of the authors are grateful to the participants.
References
1. Esakandari H, Nabi-Afjadi M, Fakkari-Afjadi J. Farahmandian, N, Miresmaeili SM, Bahreini E. A comprehensive review of COVID-19 characteristics. Biological Procedures Online. (2020) 22:19. doi: 10.1186/s12575-020-00128-2
2. Ceylan RF, Ozkan B, Mulazimogullari E. Historical evidence for economic effects of COVID-19. Eur J Health Econ. (2020) 21:817–23. doi: 10.1007/s10198-020-01206-8
3. Clarke L. An introduction to economic studies, health emergencies, and COVID-19. J Evid Based Med. (2020) 13:161–7. doi: 10.1111/jebm.12395
4. Nicola M, Alsafi Z, Sohrabi C, et al. The socio-economic implications of the coronavirus pandemic (COVID-19): A review. Int J Surg. (2020) 78:185–93. doi: 10.1016/j.ijsu.2020.04.018
5. Tian H, Liu Y, Li Y, et al. An investigation of transmission control measures during the first 50 days of the COVID-19 epidemic in China. Science (New York, NY). (2020) 368:638–42. doi: 10.1126/science.abb6105
6. Jakovljevic M, Bjedov S, Jaksic N, Jakovljevic I. COVID-19 pandemia and public and global mental health from the perspective of global health securit. Psychiatria Danubina. (2020) 32:6–14. doi: 10.24869/psyd.2020.6
7. Moccia L, Janiri L, Pepe M, et al. Affective temperament, attachment style, and the psychological impact of the COVID-19 outbreak: an early report on the Italian general population. Brain Behav Immun. (2020) 87:75–9. doi: 10.1016/j.bbi.2020.04.048
8. Nicomedes C, Avila R. An analysis on the panic during COVID-19 pandemic through an online form. J Affect Disord. (2020) 276:14–22. doi: 10.1016/j.jad.2020.06.046
9. Puspitasari IM, Yusuf L, Sinuraya RK, Abdulah R, Koyama H. Knowledge, attitude, and practice during the COVID-19 pandemic: a review. J Multidiscip Healthc. (2020) 13:727–33. doi: 10.2147/JMDH.S265527
10. Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. (2020) 17:1729. doi: 10.3390/ijerph17051729
11. Alrubaiee GG, Al-Qalah T, Al-Aawar M. Knowledge, attitudes, anxiety, and preventive behaviours towards COVID-19 among health care providers in Yemen: an online cross-sectional survey. BMC Public Health. (2020) 20:1541. doi: 10.1186/s12889-020-09644-y
12. Xiao H, Zhang Y, Kong D, Li S, Yang N. Social capital and sleep quality in individuals who self-isolated for 14 days during the coronavirus disease 2019 (COVID-19) outbreak in January 2020 in China. Med Sci Monit Int Med J Exp Clin Res. (2020) 26:e923921. doi: 10.12659/MSM.923921
13. Qiu J, Shen B, Zhao M, Wang Z, Xie B, Xu Y, et al. nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. General psychiatry. (2020) 33:e100213. doi: 10.1136/gpsych-2020-100213
14. Ran L, Wang W, Ai M, Kong Y, Chen J, Kuang L. Psychological resilience, depression, anxiety, and somatization symptoms in response to COVID-19: A study of the general population in China at the peak of its epidemic. Soc Sci Med. (2020) 262:113261. doi: 10.1016/j.socscimed.2020.113261
15. Tian F, Li H, Tian S, Yang J, Shao J, Tian C. Psychological symptoms of ordinary Chinese citizens based on SCL-90 during the level I emergency response to COVID-19. Psychiatry Res. (2020) 288:112992. doi: 10.1016/j.psychres.2020.112992
16. Taylor S. The Psychology of Pandemics: Preparing for the Next Global Outbreak of Infectious Disease. Newcastle upon Tyne, UK: Cambridge Scholars. (2019).
17. Taylor S, Asmundson GJG. Treatment of health anxiety. The Wiley Handbook of Obsessive Compulsive Disorders. Hoboken, NJ: Wiley. (2017) p. 977–89. doi: 10.1002/9781118890233.ch55
18. Clark DM, A. cognitive approach to panic. Behav Res Ther. (1986) 24:461–70. doi: 10.1016/0005-7967(86)90011-2
19. Clark DM. Cognitive therapy for panic disorder. In: Wolfe BE, Maser JD, editors. Treatment of panic disorder: A consensus development conference. Washington, DC: American Psychiatric Press. (1994) p. 121–32.
20. Rachman S. Psychological treatment of panic: Mechanisms. In: Wolfe BE, Maser JD, editors. Treatment of panic disorder: A consensus development conference. Washington, DC: American Psychiatric Press. (1994) p. 133–148.
21. Beck AT, Emery G, Greenberg RL. Anxiety disorders and phobias: A cognitive perspective. New York: Basic Books. (1985).
22. Salkovskis PM. Panic disorder and agoraphobia. Comprehensive clinical psychology. Oxford, England: Pergamon/Elsevier Science. (1998) p. 399–437. doi: 10.1016/B0080-4270(73)00200-5
23. Casey LM, Oei TP, Newcombe PA. An integrated cognitive model of panic disorder: the role of positive and negative cognitions. Clin Psychol Rev. (2004) 24:529–55. doi: 10.1016/j.cpr.2004.01.005
24. Wu HL, Huang J, Zhang C, He Z, Ming WK. Facemask shortage and the novel coronavirus disease (COVID-19) outbreak: Reflections on public health measures. EClinicalMedicine. (2020) 21:100329. doi: 10.1016/j.eclinm.2020.100329
25. Leung CC, Lam TH, Cheng KK. Mass masking in the COVID-19 epidemic: people need guidance. Lancet (London, England). (2020) 395:945. doi: 10.1016/S0140-6736(20)30520-1
26. Wang S, Feng K, Zhang Y, Liu J, Wang W. Li, Y Antecedents of public mental health during the COVID-19 pandemic: mediation of pandemic-related knowledge and self-efficacy and moderation of risk level. Front Psychiatry. (2020) 11:567119. doi: 10.3389/fpsyt.2020.567119
27. Cohen J, Rodgers Y. Contributing factors to personal protective equipment shortages during the COVID-19 pandemic. Preventive medicine. (2020) 141:106263. doi: 10.1016/j.ypmed.2020.106263
28. Hossain MM, Tasnim S, Sultana A, et al. Epidemiology of mental health problems in COVID-19: a review. F1000Research. (2020) 9:636. doi: 10.12688/f1000research.24457.1
29. Javelot H, Weiner L. Panic and pandemic: Narrative review of the literature on the links and risks of panic disorder as a consequence of the SARS-CoV-2 pandemic. L'Encephale. (2020) 47:38–42. doi: 10.1016/j.encep.2020.08.001
30. Song S, Yao X. Wen N. What motivates Chinese consumers to avoid information about the COVID-19 pandemic?: The perspective of the stimulus-organism-response model. Inf Process Manag. (2021) 58:102407. doi: 10.1016/j.ipm.2020.102407
31. Song P, Karako T. COVID-19: Real-time dissemination of scientific information to fight a public health emergency of international concern. Biosci Trends. (2020) 14:1–2. doi: 10.5582/bst.2020.01056
32. Zhong B, Huang Y, Liu Q. Mental health toll from the coronavirus: Social media usage reveals Wuhan residents' depression and secondary trauma in the COVID-19 outbreak. Comput Human Behav. (2021) 114:106524. doi: 10.1016/j.chb.2020.106524
33. Depoux A, Martin S, Karafillakis E, Preet R, Wilder-Smith A, Larson H. The pandemic of social media panic travels faster than the COVID-19 outbreak. J Travel Med. (2020) 27:taaa031. doi: 10.1093/jtm/taaa031
34. Dunton GF, Wang SD, Do B, Courtney J. Early effects of the COVID-19 pandemic on physical activity locations and behaviors in adults living in the United States. Prev Med Rep. (2020) 20:101241. doi: 10.1016/j.pmedr.2020.101241
35. Cypryańska M, Nezlek JB. Anxiety as a mediator of relationships between perceptions of the threat of COVID-19 and coping behaviors during the onset of the pandemic in Poland. PLoS ONE. (2020) 15:e0241464. doi: 10.1371/journal.pone.0241464
36. Lins S, Aquino S. Development and initial psychometric properties of a panic buying scale during COVID-19 pandemic. Heliyon. (2020) 6:e04746. doi: 10.1016/j.heliyon.2020.e04746
37. Brown S, Opitz MC, Peebles AI, Sharpe H, Duffy F, Newman E, et al. qualitative exploration of the impact of COVID-19 on individuals with eating disorders in the UK. Appetite. (2021) 156:104977. doi: 10.1016/j.appet.2020.104977
38. Shorey S, Ang E, Yamina A, Tam C. Perceptions of public on the COVID-19 outbreak in Singapore: a qualitative content analysis. J Public Health (Oxford, England). (2020) 42:665–71. doi: 10.1093/pubmed/fdaa105
39. Becker MH, Haefner DP, Maiman LA. The health belief model in the prediction of dietary compliance: a field experiment. J Health Soc Behav. (1977) 18:348–66. doi: 10.2307/2955344
40. Trumbo CW, McComas KA. The function of credibility in information processing for risk perception. Risk Anal. (2003) 23:343–53. doi: 10.1111/1539-6924.00313
41. Fava L, Morton J. Causal modeling of panic disorder theories. Clin Psychol Rev. (2009) 29:623–37. doi: 10.1016/j.cpr.2009.08.002
42. Gorman JM, Kent JM, Sullivan GM, Coplan JD. Neuroanatomical hypothesis of panic disorder, revised. Am J Psychiatry. (2000) 157:493–505. doi: 10.1176/appi.ajp.157.4.493
43. Liao Q, Cowling BJ, Lam WW, Ng DM, Fielding R. Anxiety, worry and cognitive risk estimate in relation to protective behaviors during the 2009 influenza A/H1N1 pandemic in Hong Kong: ten cross-sectional surveys. BMC Infect Dis. (2014) 14:169. doi: 10.1186/1471-2334-14-169
44. Chen S, Wang C, Wu X. Research progress on panic disorder (in Chinese). J Dalian Med Uni. (2019) 41:366–73. doi: 10.11724/jdmu.2019.04.17
45. Zhong H, Yang J, Yang J, et al. The epidemiological investigation of anxiety disorders in Mosuo people in Ninglang area of Yunnan Province (in Chinese). J Clin Psychiatry. (2019) 29:28–31.
46. Li X. Epidemiological survey of panic disorder in Baoding (in Chinese). Chin J Public Health. (2008) 24:1366–9.
47. de Jonge P, Roest AM, Lim CC, et al. Cross-national epidemiology of panic disorder and panic attacks in the world mental health surveys. Depress Anxiety. (2016) 33:1155–77. doi: 10.1002/da.22572
48. Ozamiz-Etxebarria N, Dosil-Santamaria M, Picaza-Gorrochategui M, Idoiaga-Mondragon N. Stress, anxiety, and depression levels in the initial stage of the COVID-19 outbreak in a population sample in the northern Spain. Cad Saude Publica. (2020) 36:e00054020. doi: 10.1590/0102-311x00054020
49. Islam MS, Ferdous MZ, Potenza MN. Panic and generalized anxiety during the COVID-19 pandemic among Bangladeshi people: An online pilot survey early in the outbreak. J Affect Disord. (2020) 276:30–7. doi: 10.1016/j.jad.2020.06.049
50. Luo M, Guo L, Yu M, Jiang W. Wang H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public - A systematic review and meta-analysis. Psychiatry Res. (2020) 291:113190. doi: 10.1016/j.psychres.2020.113190
51. Choi E, Hui B, Wan E. Depression and Anxiety in Hong Kong during COVID-19. Int J Environ Res Public Health. (2020) 17:3740. doi: 10.3390/ijerph17103740
52. Sher L. The impact of the COVID-19 pandemic on suicide rates. QJM-Int J Med. (2020) 113:707–12. doi: 10.1093/qjmed/hcaa202
53. Prem K, Liu Y, Russell TW, et al. The effect of control strategies to reduce social mixing on outcomes of the COVID-19 epidemic in Wuhan, China: a modelling study. The Lancet Public health. (2020) 5:e261–70. doi: 10.1016/S2468-2667(20)30073-6
54. Li Q, Chen T, Yang J, Cong G. Based on Computational Communication Paradigm: Simulation of Public Opinion Communication Process of Panic Buying During the COVID-19 Pandemic. Psychol Res Behav Manag. (2020) 13:1027–45. doi: 10.2147/PRBM.S280825
55. Ammar A, Brach M, Trabelsi K, et al. Effects of COVID-19 Home Confinement on Eating Behaviour and Physical Activity: Results of the ECLB-COVID19. Int Online Survey Nutrients. (2020) 12:1583. doi: 10.1159/000512852
56. Zachary Z, Brianna F, Brianna L, et al. Self-quarantine and weight gain related risk factors during the COVID-19 pandemic. Obes Res Clin Pract. (2020) 14:210–6. doi: 10.1016/j.orcp.2020.05.004
57. Williams L, Rasmussen S, Kleczkowski A, Maharaj S, Cairns N. Protection motivation theory and social distancing behaviour in response to a simulated infectious disease epidemic. Psychol Health Med. (2014) 20:832–7. doi: 10.1080/13548506.2015.1028946
58. Kleczkowski A, Maharaj S, Rasmussen S, Williams L, Cairns N. Spontaneous social distancing in response to a simulated epidemic: a virtual experiment. BMC Public Health. (2015) 15:973. doi: 10.1186/s12889-015-2336-7
59. Fenichel EP. Economic considerations for social distancing and behavioral based policies during an epidemic. J Health Econ. (2013) 32:440–51. doi: 10.1016/j.jhealeco.2013.01.002
60. Chew QH, Wei KC, Vasoo S, Chua HC, Sim K. Narrative synthesis of psychological and coping responses towards emerging infectious disease outbreaks in the general population: practical considerations for the COVID-19 pandemic. Singapore Med J. (2020) 61:350–6. doi: 10.11622/smedj.2020046
61. Xu T, Sattar U. Conceptualizing COVID-19 and public panic with the moderating role of media use and uncertainty in China: an empirical framework. Healthcare (Basel, Switzerland). (2020) 8:249. doi: 10.3390/healthcare8030249
62. Cai Z, Zheng S, Huang Y, et al. Emotional and cognitive responses and behavioral coping of chinese medical workers and general population during the pandemic of COVID-19. Int J Environ Res Public Health. (2020) 17:6198. doi: 10.3390/ijerph17176198
63. Doherty FV, Odeyemi OA, Adeola A, Amolegbe O, Ajagbe FE. Evaluation of knowledge, impacts and government intervention strategies during the COVID - 19 pandemic in Nigeria. Data in brief. (2020) 32:106177. doi: 10.1016/j.dib.2020.106177
64. Geldsetzer P. Use of rapid online surveys to assess people's perceptions during infectious disease outbreaks: a cross-sectional survey on COVID-19. J Med Internet Res. (2020) 22:e18790. doi: 10.2196/18790
65. Parikh PA, Shah BV, Phatak AG, Vadnerkar AC, Uttekar S, Thacker N, et al. COVID-19 pandemic: knowledge and perceptions of the public and healthcare professionals. Cureus. (2020) 12:e8144. doi: 10.7759/cureus.8144
66. Yin D, Gao Q, Zhu H, Li J. Public perception of urban companion animals during the COVID-19 outbreak in China. Health & place. (2020) s65:102399. doi: 10.1016/j.healthplace.2020.102399
67. Azlan AA, Hamzah MR, Sern TJ, Ayub SH, Mohamad E. Public knowledge, attitudes and practices towards COVID-19: A cross-sectional study in Malaysia. PLoS ONE. (2020) 15:e0233668. doi: 10.1371/journal.pone.0233668
68. Paul A, Sikdar D, Hossain MM, et al. Knowledge, attitudes, and practices toward the novel coronavirus among Bangladeshis: Implications for mitigation measures. PLoS ONE. (2020) 15:e0238492. doi: 10.1371/journal.pone.0238492
69. Gao Y, Sun F, Jiang W, et al. Beliefs towards the COVID-19 pandemic among patients with emotional disorders in China. General Psychiatry. (2020) 33:e100231. doi: 10.1136/gpsych-2020-100231
70. Motta Zanin G, Gentile E, Parisi A, Spasiano D. A. Preliminary evaluation of the public risk perception related to the COVID-19 health emergency in Italy. Int J Environ Res Public Health. (2020) 17:3024. doi: 10.3390/ijerph17093024
71. Poletti P, Ajelli M, Merler S. Risk perception and effectiveness of uncoordinated behavioral responses in an emerging epidemic. Math Biosci. (2013) 238:80–9. doi: 10.1016/j.mbs.2012.04.003
72. Shook E, Curtis A, Curtis J, Gibson G, Horst AV, Little V, et al. Assessing the geographic context of risk perception and behavioral response to potential Ebola exposure. Int J Environ Res Public Health. (2019) 16:831. doi: 10.3390/ijerph16050831
73. Raude J, MCColl K, Flamand C, Apostolidis T. Understanding health behaviour changes in response to outbreaks: Findings from a longitudinal study of a large epidemic of mosquito-borne disease. Soc Sci Med. (2019) 230:184–93. doi: 10.1016/j.socscimed.2019.04.009
74. Sahneh FD, Chowdhury FN. Scoglio, CM. On the existence of a threshold for preventive behavioral responses to suppress epidemic spreading. Sci Rep. (2012) 2:632. doi: 10.1038/srep00632
75. Chan E, Huang Z, Lo E, Hung K, Wong E, Wong S. Sociodemographic predictors of health risk perception, attitude and behavior practices associated with health-emergency disaster risk management for biological hazards: the case of COVID-19 pandemic in Hong Kong, SAR China. Int J Environ Res Public Health. (2020) 17:3869. doi: 10.3390/ijerph17113869
Keywords: panic, behavior, COVID-19, online survey, mental health
Citation: Zhang W, Zou C, Sznajder KK, Cui C, Fu J, He S, Peng Q, Chen Q and Yang X (2022) Panic, Psycho-Behavioral Responses, and Risk Perception in the Earliest Stage of the COVID-19 Pandemic in China. Front. Med. 9:766842. doi: 10.3389/fmed.2022.766842
Received: 30 August 2021; Accepted: 26 January 2022;
Published: 25 February 2022.
Edited by:
Bijaya Kumar Padhi, Post Graduate Institute of Medical Education and Research (PGIMER), IndiaReviewed by:
Tambone Vittoradolfo, Campus Bio-Medico University, ItalySusanta Kumar Ghosh, National Institute of Malaria Research (ICMR), India
Copyright © 2022 Zhang, Zou, Sznajder, Cui, Fu, He, Peng, Chen and Yang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiaoshi Yang, eHN5YW5nQGNtdS5lZHUuY24=
†These authors have contributed equally to this work and share first authorship
 Weiyu Zhang
Weiyu Zhang Changqing Zou
Changqing Zou Kristin K. Sznajder
Kristin K. Sznajder Can Cui
Can Cui Jiahui Fu1
Jiahui Fu1 Shan He
Shan He Qinqi Peng
Qinqi Peng Qiongli Chen
Qiongli Chen Xiaoshi Yang
Xiaoshi Yang