- 1Department of Anaesthesiology, Faculty of Medicine, Universiti Malaya Medical Centre, Universiti Malaya, Kuala Lumpur, Malaysia
- 2Clinical School Johor Bahru, Jeffrey Cheah School of Medicine and Health Sciences, Monash University Malaysia, Subang Jaya, Malaysia
- 3Department of Social and Preventive Medicine, Faculty of Medicine, Universiti Malaya, Kuala Lumpur, Malaysia
- 4Faculty of Medicine and Health Sciences, Universiti Malaysia Sabah, Kota Kinabalu, Sabah, Malaysia
- 5Department of Anaesthesiology and Intensive Care, Hospital Kuala Lumpur, Kuala Lumpur, Malaysia
Background: Coronavirus disease 2019 (COVID-19) emerged with a wide range of clinical presentations; Malaysia was not spared from its impact. This study describes the clinical characteristics of COVID-19 patients admitted to intensive care unit, their clinical course, management, and hospital outcomes.
Methods: COVIDICU-MY is a retrospective analysis of COVID-19 patients from 19 intensive care units (ICU) across Malaysia from 1 March 2020 to 31 May 2020. We collected epidemiological history, demographics, clinical comorbidities, laboratory investigations, respiratory and hemodynamic values, management, length of stay and survival status. We compared these variables between survival and non-survival groups.
Results: A total of 170 critically ill patients were included, with 77% above 50 years of age [median age 60, IQR (51–66)] and 75.3% male. Hypertension, diabetes mellitus, hyperlipidemia, chronic cardiac disease, and chronic kidney disease were most common among patients. A high Simplified Acute Physiology Score (SAPS) II score [median 45, IQR (34–49)] and Sequential Organ Failure Assessment (SOFA) score [median 8, IQR (6–11)] were associated with mortality. Patients were profoundly hypoxic with a median lowest PaO2/FiO2 ratio of 150 (IQR 99–220) at admission. 91 patients (53.5%) required intubation on their first day of admission, out of which 38 died (73.1% of the hospital non-survivors). Our sample had more patients with moderate Acute Respiratory Distress Syndrome (ARDS), 58 patients (43.9%), compared to severe ARDS, 33 patients (25%); with both ARDS classification groups contributing to 25 patients (54.4%) and 11 patients (23.9%) of the non-survival group, respectively. Cumulative fluid balance over 24 h was higher in the non-survival group with significant differences on Day 3 (1,953 vs. 622 ml, p < 0.05) and Day 7 of ICU (3,485 vs. 830 ml, p < 0.05). Patients with high serum creatinine, urea, lactate dehydrogenase, aspartate aminotransferase and d-dimer, and low lymphocyte count throughout the stay also had a higher risk of mortality. The hospital mortality rate was 30.6% in our sample.
Conclusion: We report high mortality amongst critically ill patients in intensive care units in Malaysia, at 30.6%, during the March to May 2020 period. High admission SAPS II and SOFA, and severe hypoxemia and high cumulative fluid balance were associated with mortality. Higher creatinine, urea, lactate dehydrogenase, aspartate aminotransferase and d-dimer, and lymphopenia were observed in the non-survival group.
Introduction
Coronavirus Disease 2019 (COVID-19), caused by the novel beta coronavirus SARS-CoV-2, has a wide range of clinical presentations–from being asymptomatic to having a mild illness, pneumonia, severe pneumonia, Acute Respiratory Distress Syndrome (ARDS), sepsis and septic shock (1). In February 2020, the World Health Organization (WHO) declared COVID-19 as a pandemic, and by 19 December 2021, the WHO Situation Report documented a COVID-19 global infection of more than 273 million people with a mortality of more than 5.3 million with Southeast Asia contributing to 44 million cases and more than 700 thousand deaths (2). On 25 December 2021, the official website of the Ministry of Health Malaysia reported a cumulative case of 2,741,179 COVID-19 positive patients with 2,778 daily cases and 306 active intensive care unit (ICU) cases (3). Understanding the more severely ill COVID-19 patients is necessary given the wide range of clinical presentations and the high mortality. A retrospective cohort data suggested that as high as 35% of patients could fall into the severe group and 28% critical (4).
Based on the published summary by the Chinese Center for Disease Control and Prevention, mortality risk factors identified included cardiovascular disease (10.5% of the death population), diabetes (7.3%), chronic respiratory disease (6.3%), hypertension (6.0%), and cancer (5.6%) (5). Among the highest risk groups in this report was the elderly population aged 70–79 years old, with a documented case fatality rate of 8%. The critically ill subgroup population had also been identified as having a higher risk of mortality; 49% in the same report mentioned above (5). A more focused retrospective cohort study done in two hospitals hardest hit with COVID-19 in Wuhan, China showed that older age, high Sequential Organ Failure Assessment (SOFA) score, and d-dimer greater than 1 μg/ml would identify patients with poor prognosis at an early stage (4). Another retrospective observational study in a specific population of 52 ICU patients in another hospital in Wuhan showed 61% mortality rate, with median days to death from ICU admission of 7 days and a higher risk of dying in the elderly (>65 years old) with comorbidities and those who fulfill criteria for ARDS (6).
In March 2020, there was a sudden surge of adult intensive care unit COVID-19 admissions in Malaysia (7). The unprecedented COVID-19 outbreak poses significant challenges to intensive care practice for a middle-income country with limited intensive care capacity and resources like Malaysia. This study aimed to describe the clinical characteristics of COVID-19 patients admitted to the Malaysian ICUs, their clinical course, management and hospital outcomes.
Materials and methods
Study design and population
We conducted a retrospective analysis of data from 19 participating ICUs across Malaysia for a period of 2 months from 1 March 2020 to 31 May 2020. We included patients with confirmed positive COVID-19 reverse transcription polymerase chain reaction (RT-PCR) tests either before or after their ICU admissions.
Variables and outcomes
We collected data of socio-demography, admission characteristics including the severity scores, laboratory and radiographic investigations, management and clinical outcomes. The outcomes measured were duration of mechanical ventilation, tracheotomy, ICU length of stay and hospital length of stay. These variable and outcomes were then compared between the non-survived and survived groups.
Data extraction
We extracted data from paper and electronic resources available and documented in pre-designed case report forms (CRFs). The data for CRFs of each participating centre were collected by assigned clinicians who were experienced with intensive care practices.
There were three CRFs: the core CRF, the daily CRF, and the summary CRF. The core CRF consisted of baseline information on hospital and ICU admission i.e., epidemiological history, demographics, vital signs, comorbidities, admission date, hospital admission signs and symptoms, confirmatory pathogen testing, laboratory investigations and severity scores based on admission SAPS II and SOFA.
The daily CRF consisted of clinical observation data i.e., types of respiratory support, PaO2 values, need for prone positioning, worst hemodynamic values, and highest vasopressor dose. We also included data of fluids input, output and balance, renal replacement therapy and laboratory values.
The summary CRF included the discharge details–dead or alive status, length of ICU stay, oxygen and renal support required upon discharge, tracheostomy and length of hospital stay.
Ethics
We received ethics approval from the Medical Research Ethics Committee of Malaysian Ministry of Health (NMRR-20-1037-54772-IIR) and University of Malaya Medical Centre (202049-8484). Informed consent was waived as the study was observational and the data were de-identified.
Statistical analysis
Descriptive data are expressed as the median and interquartile range (IQR) for continuous data and numbers and percentages for categorical data. Associations between survival groups were examined using the Pearson’s chi-squared test or Fisher’s exact test for categorical data and the Wilcoxon rank-sum test for continuous data. A value of P < 0.05 is considered statistically significant. All analysis were performed with Stata version 17. Missing or unknown data were excluded from the analysis.
Results
Demographics and clinical characteristics
A total of 170 patients from 19 hospitals in Malaysia were included during the study period for analysis. A total of 52 patients died during hospitalization, and 118 were discharged. Majority of the patients were above 50 years old (77%) with a median age of 60 (IQR 51–66), and most patients were male (75.3%) (Table 1). A total of 137 (80.6%) patients were of Malay ethnicity, which represents the most of Malaysia’s population by ethnicity (8). This was followed by patients of Chinese ethnicity, 11.8%, and Indian, 3.5%, other Bumiputera, 1.2%, and foreigners, 2.9%. Most patients had close contact with a confirmed COVID-19 case (40%), a history of presence in large social gatherings (39.8%), and a history of traveling to an area with documented confirmed COVID-19 cases (34.7%). It is worth noting that there were cases with a history of presence in a healthcare facility (17.5%) and a history of laboratory handling of confirmed COVID-19 samples (11%).

Table 1. Demographics, epidemiological factors, comorbidities, clinical investigations, and symptoms within 24 h at presentation/Admission at the hospital of coronavirus disease 2019 (COVID-19) intensive care unit patients.
There were many comorbidities reported among our patients with the most common being hypertension (58.1%) and diabetes (44.1%). At hospital presentation, the median Body Mass Index (BMI) of all patients was 26.7 (IQR 24.8–30.5), median systolic blood pressure 134 mmHg (IQR 121–149), diastolic 75 mmHg (IQR 65–84), pulse rate 92 beats/min (IQR 82.5–105), respiratory rate 22 breaths/min (IQR 20–28) and temperature 37.4 degrees of Celsius (IQR 36.9–38.0). 70% of all patients received oxygen supplementation at admission, with the median oxygen saturation 97% (IQR 95–99). There was no difference between survivors and non-survivors for these co-morbidities and clinical parameters.
Several blood investigations showed clinically different levels in the non-survivors compared to survivors at hospital or ICU admissions. These were creatinine (111.5 vs. 90 μmol/L, P = 0.021) and lactate dehydrogenase (599.9 vs. 346 UL, P = 0.002).
The median SAPS II score on ICU admission for all patients was 29, and those that died had a significantly higher median SAPS II of 45 compared to the survival group’s score of 21.5 (P < 0.001). The median SOFA score for all patients was five and those that died had a significantly higher median SOFA score of eight compared to a SOFA score median of three for the survival group (P < 0.001).
Respiratory characteristics and support during first 24 h of ICU admission
In the first 24 h of ICU admission, 17 (10%) patients received oxygen via nasal prong while 49 patients received oxygen via different types of facemasks; 15 (30.6%) via Hudson facemask, 26 (53.1%) via non-rebreathing mask and 8 (16.3%) via Venturi mask (Table 2). A total of 91 patients had to be intubated in the first 24 h of ICU with a clinically significant number of them died while in the hospital, 38 (73.1% of the non-survival group) compared to 53 patients who survived (44.9% of the survival group); P = 0.256. The most common ventilation modes used for all patients were Synchronised Intermittent Mandatory Ventilation (SIMV) (63.5%) and Assist Control (AC) (16.5%). The median positive end-expiratory pressure, PEEP, that was used was 12 cmH2O (IQR 10–12.5).
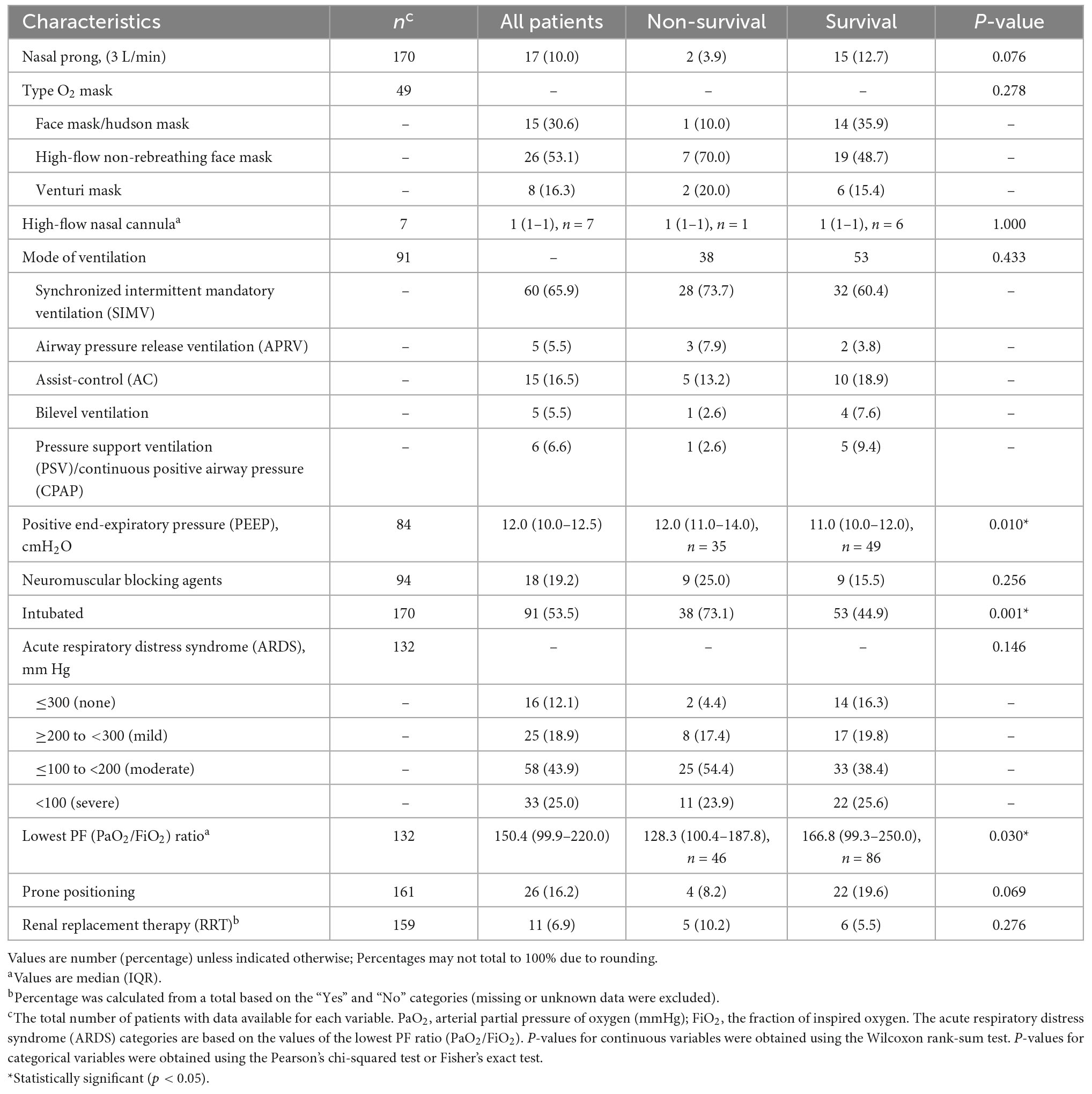
Table 2. Clinical and respiratory support characteristics during the first 24 h in the intensive care unit (ICU).
Out of 132 patients analyzed for ARDS, 25 had mild ARDS (18.9%), 58 had moderate ARDS (43.9%), and 33 had severe ARDS (25%). 25 patients in the moderate ARDS group and 11 patients in the severe ARDS group died, contributing to 54.4 and 23.9% of the non-survival group. The lowest PaO2/FiO2 (PF) ratio median value was 150 (IQR 99.6–220), with a significant difference between the non-survival group (median value 128.3) and the survival group (median value 166.8), P = 0.030.
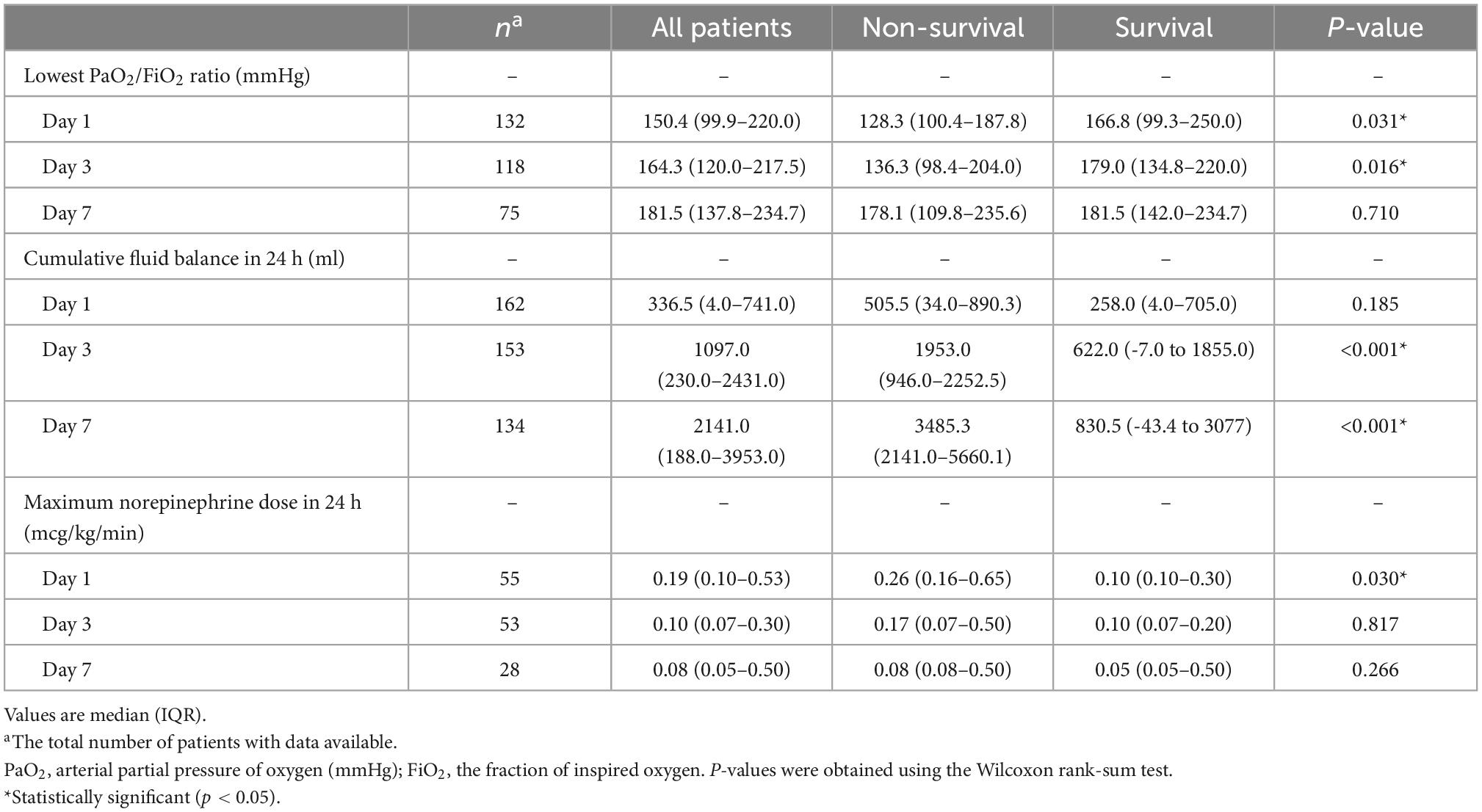
Lowest PaO2/FiO2 ratio, cumulative fluid balance and maximum norepinephrine dose for days 1, 3, and 7 of ICU
We analysed these clinical variables on days 1, 3, and 7 in the ICU, as shown in Table 3. The significant difference in median PF ratio between the non-survival group and survival group seen in the first 24 h (Day 1 of ICU) above was also seen on Day 3.
There was significantly higher cumulative fluid balance among the non-survival group compared with the survival group on Day 3 (1,953 ml vs. 622 ml, P < 0.001) and on Day 7 (3,485 ml vs. 830 ml, P < 0.001). With regard to norepinephrine dose, there was a significant difference seen on Day 1 of ICU (non-survival 0.26 mcg/kg/min vs. survival 0.1 mcg.kg.min, P 0.03).
PaO2/FiO2 ratio for patients on prone position from day 1 to day 7
For a small number of patients put on prone positioning and had adequate PaO2 and FiO2 data, we compiled the changes in the PF ratio before and after the prone (Table 4). There was a significant difference before and after the prone position from Day 1 to Day 3. The PF ratios before prone were 88, 95, and 138 mmHg for Days 1, 2, and 3, respectively. After prone, the PF ratios for Days 1, 2, and 3 were significantly higher 173.2, 242, and 216 mmHg, respectively. From Day 4 to Day 7, the difference between before and after prone was no longer significant and there were also fewer patients with adequate PaO2 and FiO2 data for comparison.
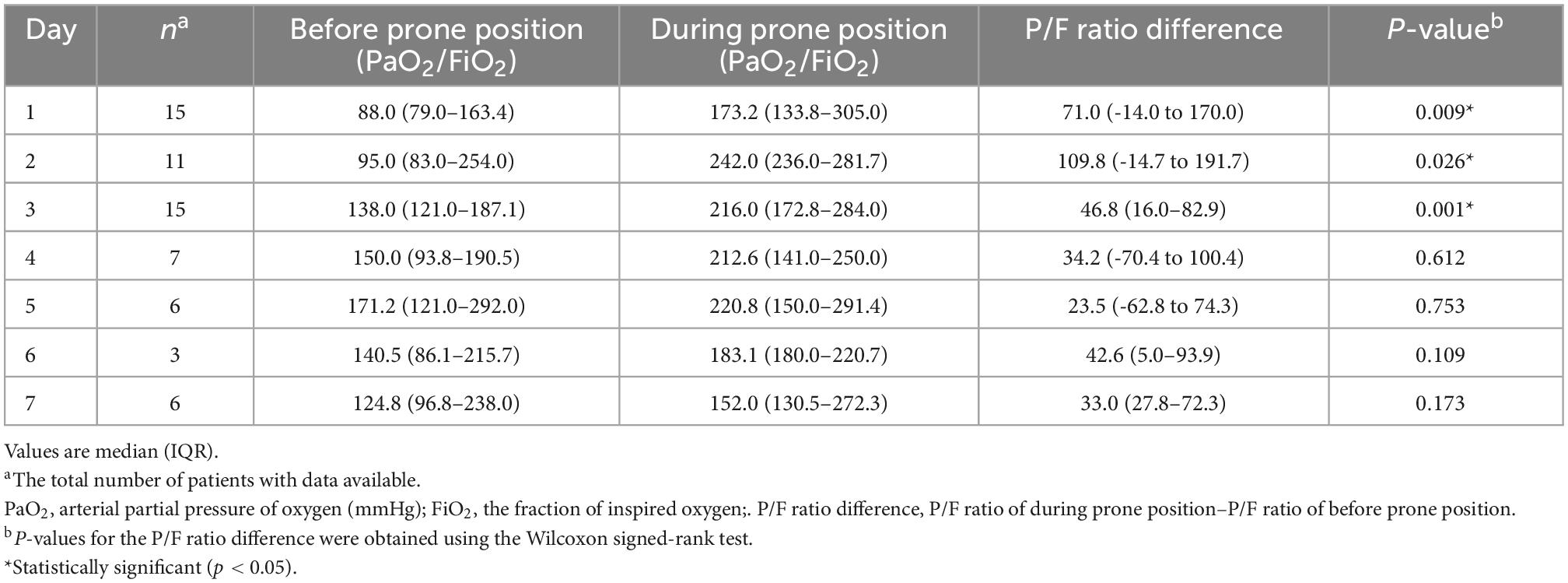
Table 4. PaO2/FiO2 ratio (mmHg) for coronavirus disease 2019 (COVID-19) intensive care unit patients on prone position in the intensive care unit (ICU) from days 1 to 7.
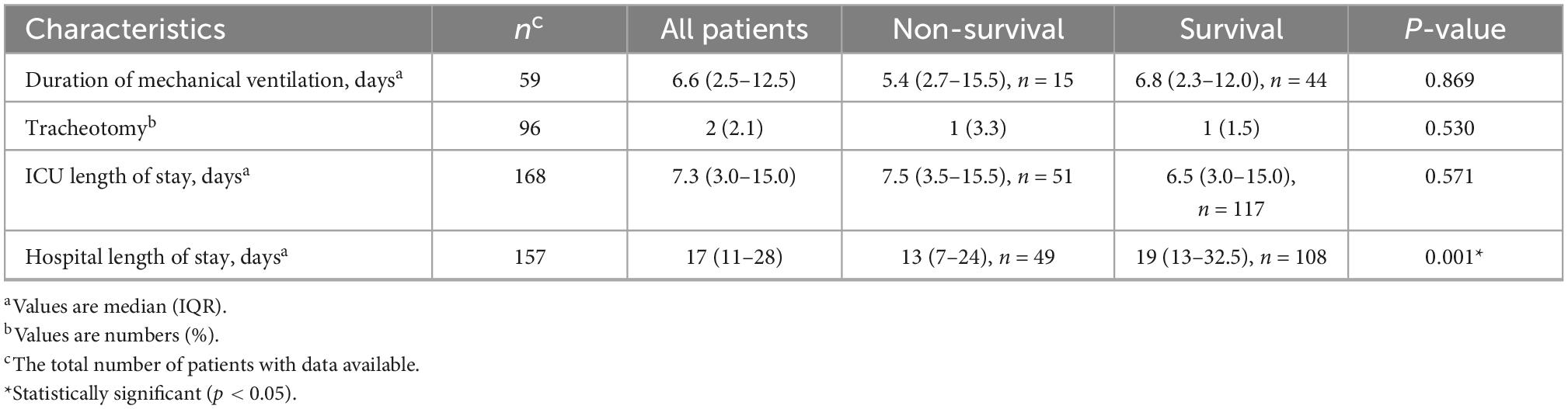
Clinical outcomes
There was no difference in the duration of mechanical ventilation between the survival group (median 6.8 days, IQR 2.7–15.5) and the non-survival group (median 5.4 days, IQR 2.7–15.5); P = 0.869 (Table 5). There was also no difference in the length of ICU stay; the survival group had a median ICU stay of 7.5 days (IQR 3.5–15.5) and the non-survival group 6.5 days (IQR 3.0–15.0); P = 0.571. However, there was a significant difference in the hospital length of stay between the groups, survival group had a median of hospital stay 19 days (IQR 13–32.5) and non-survival group 13 days (IQR 7–24), P = 0.001.
Supplementary results
Lymphocyte counts were generally low for both groups at admission and generally improved over time for survivors, but for non-survivors continued to dip and, toward the end, soared to a much higher level (Supplementary Figure 1). As per Table 1, we found that there were significant differences in some markers, and we tracked them over 14 days; ferritin, lactate dehydrogenase (LDH), d-dimer, creatinine, urea, and amino aspartate (AST) were generally higher in non-survival throughout 14 days in ICU. However, we only found significant differences between the groups for up to Day 2 for procalcitonin and AST, up to Day 4 for 165 d-dimer and LDH, and as long as Day 12 for urea and creatinine.
Discussion
Key findings
We analyzed data of 170 critically ill patients with confirmed COVID-19 infection admitted to ICUs during the first wave of COVID-19 outbreak between March and May 2020. A total of 52 (30.6%) of the critically ill patients died, and 118 (69%) were discharged.
Our analysis reveals that the non-survival group had higher SAPS II and SOFA scores on ICU admission, lower PF ratio on Days 1 and 3 of ICU, and higher cumulative balance on Days 3 and 7 of ICU. Patients in the non-survival group were also observed to have significantly higher ferritin, lactate dehydrogenase (LDH), d-dimer, creatinine, urea, and amino aspartate (AST) levels throughout their ICU stay.
Strengths of the study
This was the first and only study on a multi-centre COVID-19 ICU patients in Malaysia. Its main strength lies on the valuable record of clinical characteristics of critically ill COVID-19 patients in a low–and middle-income (LMIC) country, and how the intensive care practice in such setting managed the ever-challenging early wave of COVID-19.
Limitations of the study
The biggest limitation of this study is its incomplete data acquisition. There were many constraints that led to this. These include the lack of electronic medical record facilities in most hospitals and the overwhelming burden of COVID-19 to the nationwide ICU healthcare teams during the period of March to May 2020. We also acknowledge that while we collected data from multiple ICUs across the country, the small sample in our study may limit the generalizability of the results.
Comparison with previous studies
Our sample’s ICU mortality rate of 30.6% reflected the high risk of mortality in the critically ill patients in Malaysia, with a study on all adult COVID-19 hospital admissions in 18 designated centres at about the same period only showing a case fatality rate of 1.2% (8). Comparatively, in the European countries, a study by the REVA network group reported 31% mortality (9) among the critically ill while a study in Wuhan reported 61.5% mortality (6). On another note, our finding of a median SOFA score of eight on Day 1 of ICU in the non-survival group was comparatively higher than other reported mortality-associated SOFA scores, namely a median of 4.5 that was reported by Wang et al. (10) in Wuhan and a median score of six by Yang et al. (6).
Our 53.5% rate of intubation and mechanical ventilation on the first day of ICU admission was comparable to the study in Wuhan by Wang et al. (10) at 47% and Yang et al. (6) at 42%. The REVA network group reported that 63% of patients required intubation in their first 24 h of ICU admission, and 80% required intubation during their ICU stay (9). On the other hand, in Lombardy, Italy, the rate of ICU intubation was 88% (11).
Our hypoxemia findings in the non-survival group were consistent with observations made in other COVID-19 ICU cohorts (12). With regard to ARDS, our findings that 54.4% of the non-survivors had moderate ARDS and 23.9% severe ARDS reflect a higher mortality rate for ARDS compared to Bellani et al. (13) in the LUNG SAFE study, in which the mortality rate was close to 50%.
Our biochemistry findings, on the other hand, are also consistent with the observations by Zhou et al. (4) and Yang et al. (6) in Wuhan, who reported lymphopenia coupled with raised inflammatory markers, increased liver transaminases, and serum creatinine in the severely diseased group.
Significance of study findings
Our findings demonstrate comparable clinical characteristics and outcomes in our low–and middle-income country setting. The similar patterns of ICU severity scores, respiratory and biochemistry presentations, and the clinical outcomes seen in our population importantly add to the body of knowledge surrounding the global impact and response to the COVID-19 pandemic.
Conclusion
In conclusion, we reported high mortality among critically ill patients in multi-intensive care units in Malaysia during the first wave of COVID-19 between March and May 2020. Most patients were above 50 years old with a prevalence of comorbidities. Higher SAPS II and SOFA scores on ICU admission, severe hypoxemia and higher cumulative fluid balance were associated with mortality in our sample. We also found the non-survivors to have significantly higher ferritin, lactate dehydrogenase (LDH), d-dimer, creatinine, urea, and amino aspartate (AST) levels throughout their ICU stay.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
This study was approved by the Medical Research Ethics Committee of the Malaysian Ministry of Health (NMRR-20-1037-54772-IIR) and the University of Malaya Medical Centre (202049-8484). Informed consent was waived as the study was observational and the data were deidentified.
Author contributions
NY: full access to all the data in the study, takes responsibility for the integrity of the data, the accuracy of the data analysis, and critical revision of the manuscript for important intellectual content. NY and RA: study concept and design and acquisition of data. JM, NA, MA, and RA: analysis and interpretation of data. NA and JM: drafting of the manuscript. JM: statistical analysis. SD and NY: obtained funding. SD and AI: administrative, technical, or material support. All authors contributed to the article and approved the submitted version.
Funding
This study was funded by the Malaysian Society of Intensive Care.
Acknowledgments
We acknowledge and immensely thank the following site investigators who coordinated the data collection: Lee Chew Kiok, Nor Haliza Zainol Abidin (Hospital Sungai Buloh), Ismail Tan, Kee Pei Wei, Lavitha Vyveganathan, Louisa Chan, SD (Hospital Kuala Lumpur), Laila Kamaliah Kamalul Bahrin (Hospital Selayang), NY, RA, Mohd Shahnaz Hasan (Universiti Malaya Medical Centre), Siti Zuraidah Abdul Karim (Hospital Kajang), Suneta Sulaiman (Institut Jantung Negara), Dr. Tam Wei Yaw (Hospital Tuanku Fauziah), Asmah Zainudin, Ahmad Shaltut Othman (Hospital Sultanah Bahiyah), Foong Kit Weng (Hospital Raja Perempuan Bainun), Anita Alias, Tan Kok Wang, Angelina Lim Chia Chia (Hospital Tuanku Jaafar), Nahla Irtiza Ismail, Siti Zuraida Ismail, Nour Suriani Husin (Hospital Melaka), Azmin Huda Abdul Rahim, Mahazir Kassim (Hospital Sultanah Aminah), Muhammad Zihni Abdullah (Hospital Tengku Ampuan Afzan), Mohd Ridhwan Mohd Noor (Hospital Sultanah Zahirah), Noryani Mohd Samat (Hospital Kuala Krai), Mohd Nazri Ali, Wan Nasrudin Wan Ismail (Hospital Raja Perempuan Zainab), James Joseph (Hospital Miri), Wan Daud Wan Kadir (Hospital Umum Sarawak), and Abdul Jabbar Bin Ismail, Fong Kean Khang, and Khoo Tien Meng (Hospital Queen Elizabeth).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. World Health Organization. Clinical Management of Severe Acute Respiratory Infection (SARI) when COVID-19 271 Disease is Suspected: Interim Guidance. Geneva: World Health Organization (2020). doi: 10.15557/PiMR.2020.0003
2. World Health Organization. COVID-19 Weekly Epidemiological Update. Geneva: World Health Organization (2020).
3. Ministry of Health Malaysia. Situasi Terkini COVID-19 di Malaysia sehingga 31 Disember 2021. Putrajaya: Ministry of Health Malaysia (2021).
4. Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z. Clinical course and risk factors for mortality of adult 275 inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. (2020) 395:1054–62. doi: 10.1016/S0140-6736(20)30566-3
5. Wu Z, Mcgoogan J. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72,314 cases from the Chinese Center for Disease Control and Prevention. JAMA. (2020) 323:1239–81. doi: 10.1001/jama.2020.2648
6. Yang X, Yu Y, Xu J, Shu H, Liu H, Wu Y. Clinical course and outcomes of critically ill patients with 281 SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. (2020) 8:475–81. doi: 10.1016/S2213-2600(20)30079-5
7. Abdullah N. Situasi semasa jangkitan penyakit Coronavirus 2019 (COVID-19) di Malaysia. Malaysia: Ministry of Health (2020).
8. Sim B, Chidambaram S, Wong X, Pathmanathan M, Peariasamy K, Hor C. Clinical characteristics and risk factors for severe COVID-19 infections in Malaysia: A nationwide observational study. Lancet Region Health-West Pac. (2020) 4:100055. doi: 10.1016/j.lanwpc.2020.100055
9. COVID-ICU Group on behalf of the REVA Network and the COVID-ICU Investigators. Clinical characteristics and day-90 outcomes of 4244 critically ill adults with COVID-19: a prospective cohort study. Intens Care Med. (2021) 47:60–73. doi: 10.1007/s00134-020-06294-x
10. Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. (2020) 323:1061–70. doi: 10.1001/jama.2020.1585
11. Grasselli G, Greco M, Zanella A, Albano G, Antonelli M, Bellani G. Risk factors associated with mortality among patients with COVID-19 in intensive care units in Lombardy, Italy. JAMA Intern Med. (2020) 180:1345–55.
12. Thomson R, Hunter J, Dutton J, Schneider J, Khosravi M, Casement A. Clinical characteristics and outcomes of critically ill patients with COVID-19 admitted to an intensive care unit in London: a prospective observational cohort study. PLoS One. (2020) 15:e243710. doi: 10.1371/journal.pone.0243710
Keywords: COVID-19, critically ill, intubation, acute respiratory distress syndrome, mortality, prone
Citation: Ab Rahman NI, Yunos NM, Atan R, Mariapun J, Ab Rahman MA‘I, Ismail AJ and Deva SR (2023) Clinical characteristics and outcomes of critically ill coronavirus disease 2019 patients in Malaysia during the first wave: A multi-center observational study (COVIDICU-MY). Front. Med. 9:1086288. doi: 10.3389/fmed.2022.1086288
Received: 01 November 2022; Accepted: 19 December 2022;
Published: 09 January 2023.
Edited by:
Luigi Pisani, Mahidol Oxford Tropical Medicine Research Unit (MORU), ThailandReviewed by:
Tanveer Rehman, Regional Medical Research Center (ICMR), IndiaRasha Shemies, Mansoura University, Egypt
Copyright © 2023 Ab Rahman, Yunos, Atan, Mariapun, Ab Rahman, Ismail and Deva. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nor’azim Mohd Yunos,  bm9yYXppbUB1bW1jLmVkdW15
bm9yYXppbUB1bW1jLmVkdW15
 Noor Iftitah Ab Rahman
Noor Iftitah Ab Rahman Nor’azim Mohd Yunos
Nor’azim Mohd Yunos Rafidah Atan
Rafidah Atan Jeevitha Mariapun
Jeevitha Mariapun Mohd Ali‘Imran Ab Rahman3
Mohd Ali‘Imran Ab Rahman3 Abdul Jabbar Ismail
Abdul Jabbar Ismail