
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Med. , 15 December 2022
Sec. Hematology
Volume 9 - 2022 | https://doi.org/10.3389/fmed.2022.1072427
This article is part of the Research Topic The Effect of COVID-19 on Hematological Disease Diagnosis, Management and Outcomes View all 12 articles
 Noha Mousaad Elemam1,2
Noha Mousaad Elemam1,2 Iman M. Talaat1,2*
Iman M. Talaat1,2* Fatehia A. Bayoumi1,3
Fatehia A. Bayoumi1,3 Dima Zein4
Dima Zein4 Ramy Georgy5
Ramy Georgy5 Abdalrahman Altamimi4
Abdalrahman Altamimi4 Noura Alkhayyal2,6
Noura Alkhayyal2,6 Alaa Habbal6
Alaa Habbal6 Feda Al Ali7
Feda Al Ali7 Alaa ElKhider7
Alaa ElKhider7 Abdallah Ahmed7
Abdallah Ahmed7 Salah Abusnana1,7
Salah Abusnana1,7 Riyad Bendardaf1,7*
Riyad Bendardaf1,7*Introduction: In this study, we aimed at exploring the morphologic and quantitative abnormalities in the peripheral blood counts of coronavirus disease 2019 (COVID-19) patients.
Methods: A cohort of 131 COVID-19 patients was recruited at University Hospital Sharjah (UHS), UAE. Their peripheral blood smears were examined for morphological evaluation. Also, their clinical laboratory investigations and radiological findings were retrieved from the medical records. Our cohort consisted of 63 males and 68 females with an age of 63.6 ± 18.6 years.
Results: The presence of atypical lymphocytes was observed in around 80% of the recruited COVID-19 patients. Further, monocytes with toxic cytoplasmic vacuoles were identified in 55% of the cases. Neutrophil-associated changes, including pseudo-Pelger-Huët, bands, and long nuclear endoplasm, were reported in around 25–35% of the patients. RBCs associated changes such as microcytic and hypochromic RBCs, as well as targetoid, dacrocytes, ovalocytes, echinocytes/burr cells, and schistocytes, were described. According to disease severity, RBCs chromicity was found to be significantly different between stable and critical patients. COVID-19 patients with CO-RADS 5 showed a similar change in RBCs as well as a decrease in the neutrophils with hypogranular cytoplasm.
Conclusion: Peripheral blood smear assessment in COVID-19 patients could provide information about the disease state and pulmonary involvement.
Coronavirus disease 2019 (COVID-19) remains a global pandemic, caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which affects multiple organs (1). In the United Arab Emirates (UAE), the first case of COVID-19 was identified on 29 January 2020 (2). The most common symptoms in COVID-19 patients include fever, fatigue, cough, and dyspnea (3). However, some cases could be asymptomatic carriers while others fall into mild, moderate, and severe categories. In critical COVID-19 patients, fatal acute respiratory distress syndrome (ARDS) occurs, leading to intensive care unit (ICU) admission (4, 5).
It was found that COVID-19 pathogenesis was associated with an activation of the immune system and subsequent immune dysregulation (6). A major clinical feature of COVID-19 was neutrophilia with concomitant lymphopenia, that were linked to the severity of the disease (7). Despite the known quantitative abnormalities in the peripheral blood, little is known about the morphologic changes in circulating blood cells in COVID-19 (8). Such changes could aid in the diagnosis of COVID-19 and management decisions in COVID-19 patients. The reported abnormalities in peripheral blood smears include a range of atypical lymphocytes, acquired Pelger-Huët anomaly, and fetus-shaped neutrophils (9). Furthermore, abnormal platelets and red blood cells (RBCs) morphology were also reported in peripheral blood of COVID-19 infected patients, thus inducing coagulopathies and malfunction of oxygen carrying capacity (10). In this study, we aim to explore the morphologic and quantitative abnormalities in the peripheral blood counts of COVID-19 patients recruited to a single center in the UAE.
This is a retrospective study conducted on 131 COVID-19 patients that were recruited at University Hospital Sharjah (UHS), UAE. Our cohort was composed of 63 males and 68 females, aged 63.6 ± 18.6 years (mean ± SD). The cases were diagnosed based on a positive nasopharyngeal swab result using reverse transcriptase-polymerase chain reaction (RT-PCR). Out of 270 patients that were admitted from July 2020 to July 2021, 131 COVID-19 patients were selected as they were not previously vaccinated for SARS-CoV-2. The study was approved by the Ethics and Research Committee of UHS (UHS-HERC-035-03052020).
Peripheral blood samples were collected from COVID-19 patients in EDTA sterile vacutainers, after which peripheral blood smears were prepared, and laboratory investigations were performed. These tests included complete and differential blood such as platelets, white blood cells (WBCs), neutrophils, lymphocytes, monocytes count, oxygen saturation and hemoglobin that were done using Sysmex XN 20 Hematology Analyzer (Sysmex, Germany). Also, prothrombin time (PT), international normalized ratio (INR), activated partial thromboplastin time (aPTT), and D-dimer were measured using STA Compact Max 3 (Stago, France). Moreover, lactate dehydrogenase (LDH) and C-reactive protein (CRP) were measured using Atellica® CH 930 Analyzer (Siemens Healthineers, Germany), while procalcitonin and ferritin were measured Atellica® IM 1300 Analyzer (Siemens Healthineers, Germany). All these tests are summarized in Table 1. Blood films were prepared and stained using the Leishman stain standard protocol. The smears were examined under the light microscope (Olympus BX43, Japan) by a hematopathologist for morphological evaluation, and images were captured using the digital camera (Olympus SC50, Japan). The evaluation was done blindly in terms of laboratory investigations.
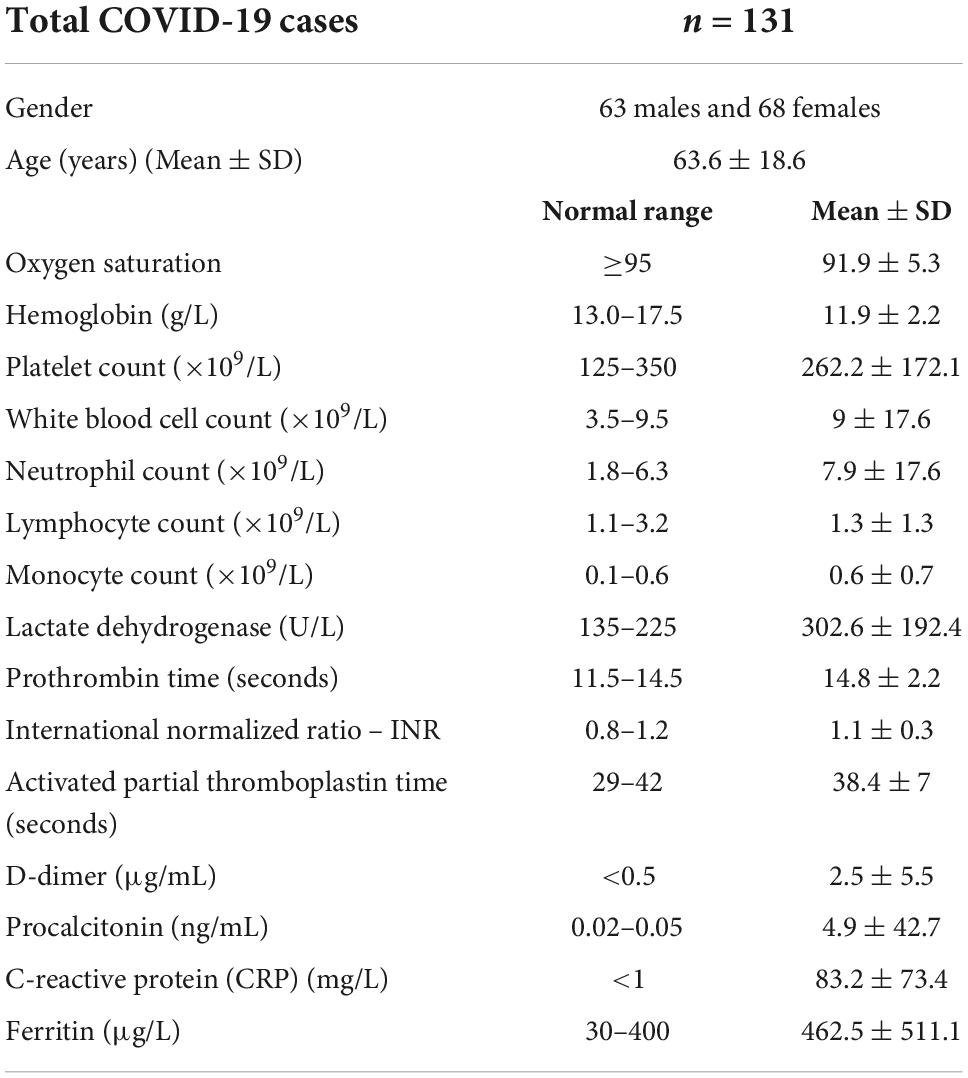
Table 1. Clinical and demographic of 131 coronavirus disease 2019 (COVID-19) patients recruited in this study.
Radiological evaluation was done using chest X-ray and high-resolution computed tomography (CT) scans, followed by an assessment using the COVID-19 Reporting and Data System (CO-RADS) as a standardized assessment of pulmonary involvement of COVID-19 (11). The CO-RADS classification is described in Table 2.
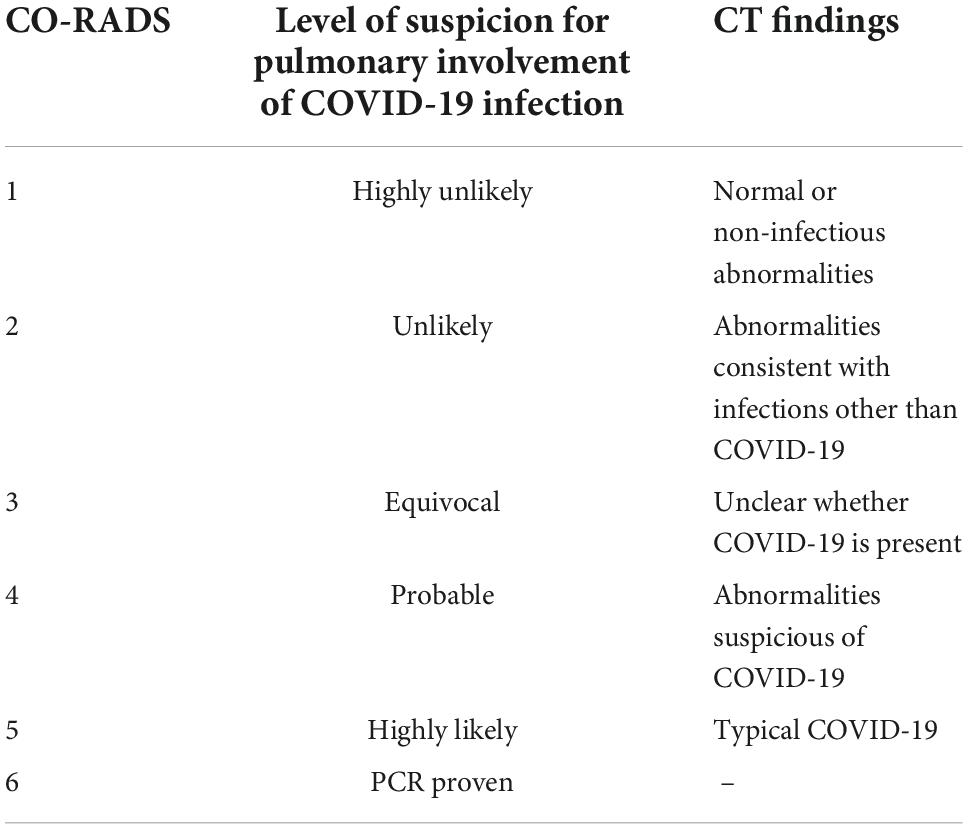
Table 2. COVID-19 Reporting and Data System (CO-RADS) interpretation with level of suspicion for pulmonary involvement of COVID-19 infection and its corresponding CT findings.
Values represent mean ± SD for the continuous variables, or percentage relative to the total number of patients in each group for the categorical variables. Statistical analysis was performed using GraphPad Prism 6 software (GraphPad Software, San Diego, CA, USA). Chi-square test was used for the comparison between the categorical variables. P-value < 0.05 was considered statistically significant.
Our cohort was composed of 131 patients that were proven to be COVID-19 positive by RT-PCR of the nasopharyngeal swabs. Their quantitative hematologic abnormalities were documented along with the microscopic examination of the peripheral smears to include various anomalies such as changes in WBCs, RBCs, and platelets.
The most common reported morphologic finding was the presence of atypical lymphocytes in around 80% of the COVID-19 patients (Figure 1A). This was followed by the presence of monocytes with toxic cytoplasmic vacuoles in 55% of the cases. As shown in Figure 1B, activated monocytes were observed showing prominent cytoplasmic vacuolization and few granules. Also, the nuclei were large, having fine chromatin with nuclear blebbing.
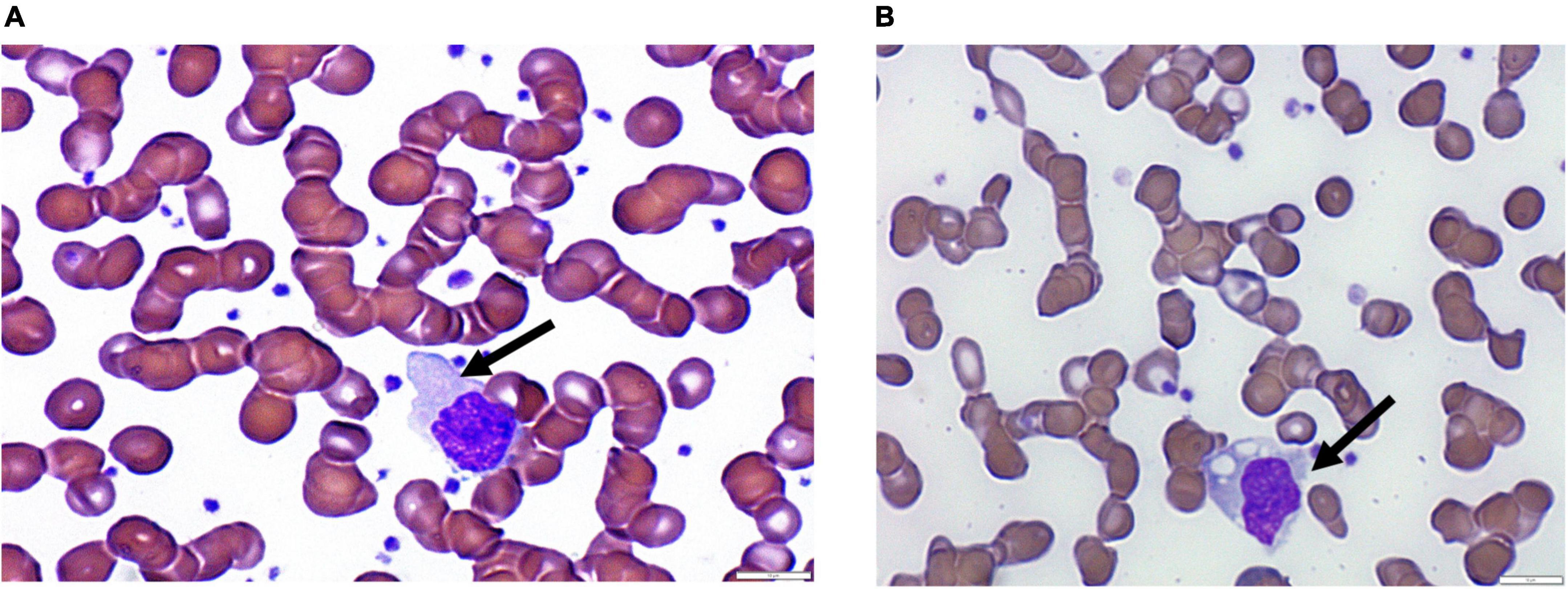
Figure 1. Images showing peripheral changes in lymphocytes and monocytes. (A) Atypical lymphocytes and (B) monocytes with vacuolated cytoplasm.
Neutrophil-associated changes, including pseudo-Pelger-Huët (Figure 2A), bands (Figure 2B), hypersegmented (Figure 2C), and long nuclear endoplasm (Figure 2D), were observed in some of the recruited COVID-19 patients. Such neutrophilic-associated changes were reported in around 25–35% of the patients, as shown in Table 3. Also, C-shaped, fetus-like nuclei were noted with aberrant nuclear projections (Figure 2E).
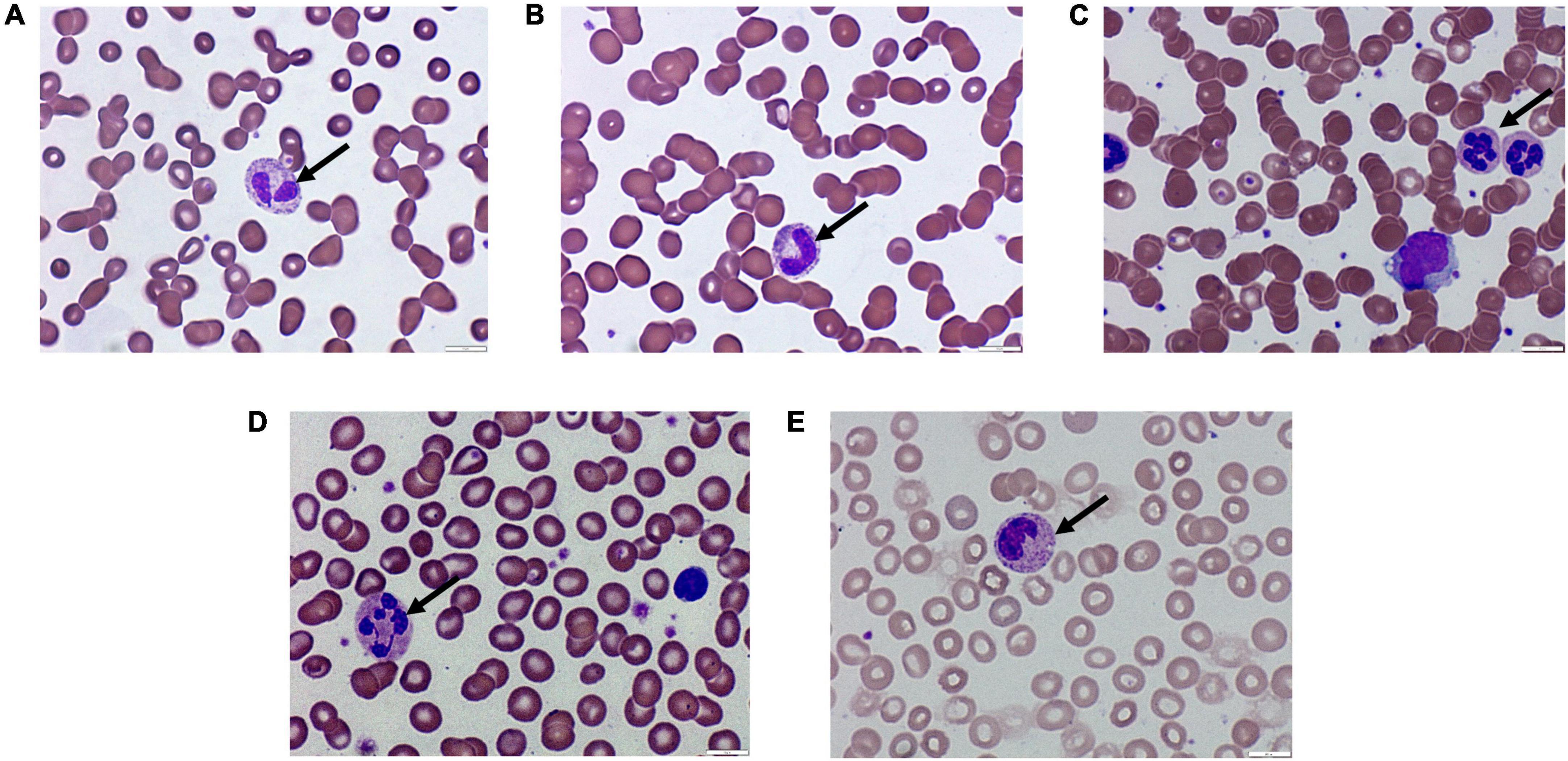
Figure 2. Images showing peripheral changes in neutrophils. (A) Pseudo-Pelger-Huët, (B) bands, (C) hypersegmented, (D) long nuclear cytoplasm, and (E) fetus-shaped nuclei in neutrophils.

Table 3. Changes in the white blood cells (WBCs) count and morphological anomalies including lymphocytes, monocytes, and neutrophils.
Regarding platelet counts, the mean number was within the normal range in COVID-19 patients, which aligns with the coagulation parameters (PT, INR, and aPTT) that were almost in their normal ranges. Around half of the COVID-19 patients presented with normocytic RBCs along with anisocytosis and hyperchromicity (Table 4). Other common RBCs associated changes included erythrocytopenia and microcytic RBCs as well as targetoid, dacrocytes, ovalocytes, echinocytes/burr cells, and schistocytes (Figures 3A–E).
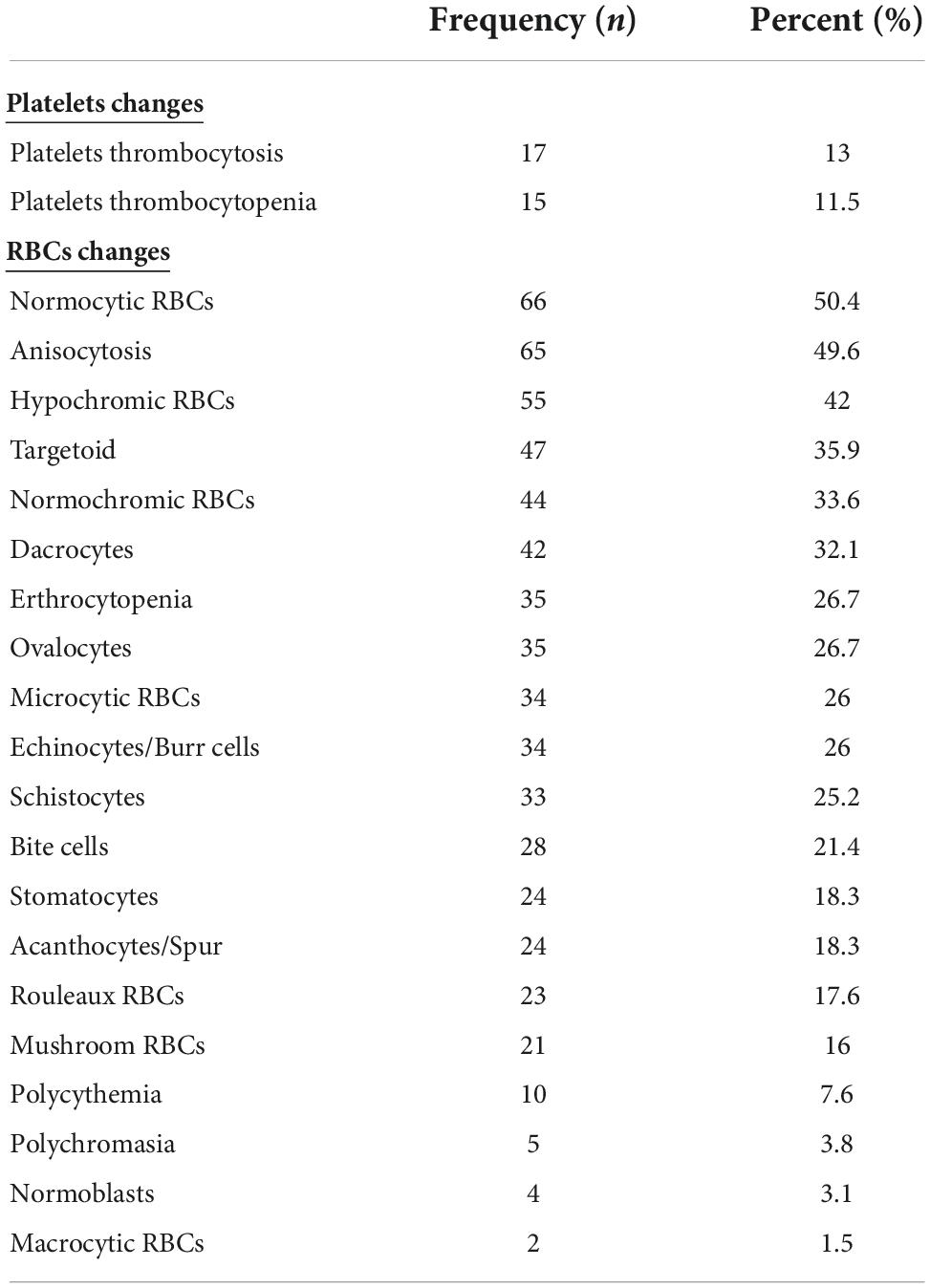
Table 4. Changes in the platelets and red blood cells (RBCs) count and their associated morphological anomalies.

Figure 3. Images showing peripheral changes in red blood cells (RBCs). (A) Normoblasts, (B) rouleaux, (C) acanthocytes, (D) mushroom-like, and (E) anisopoikilocytosis, ovalocytes, schistocytes, and targetoid cells.
The COVID-19 patients were classified into different groups according to their CO-RADS score. Almost 77% of the patients fell into the CO-RADS 5 category (Figure 4), indicating pulmonary involvement and a high probability of COVID-19 infection before confirmatory tests by qRT-PCR (Table 5).
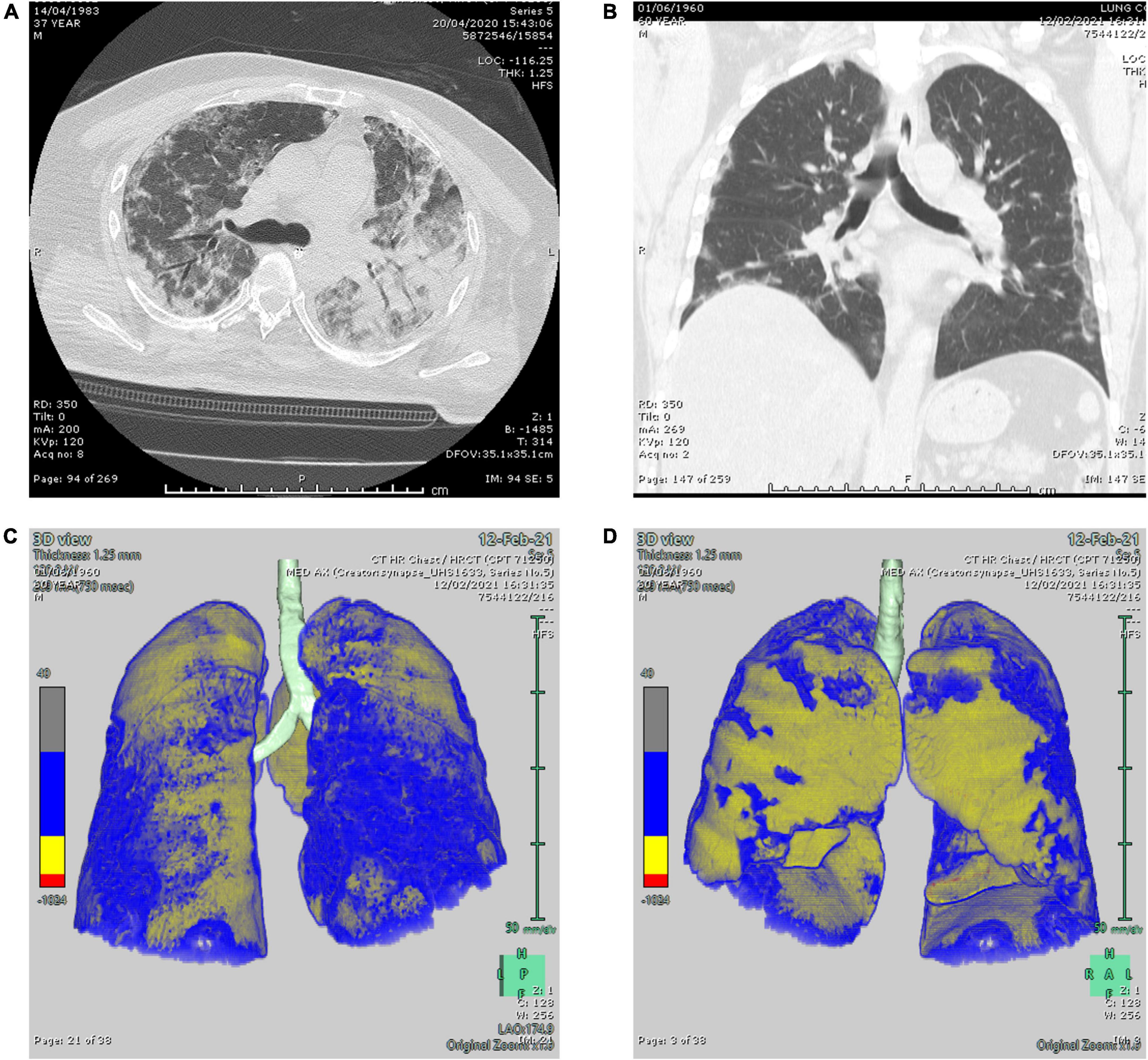
Figure 4. Two representative computed tomography (CT) lung window images. (A) Axial and (B) coronal lung window CT images showing bilateral scattered ground-glass attenuation opacities with an area of pneumonic consolidation at the left lower lobe (CO-RADS 5). (C,D) 3D reconstructed images of the lungs showing bilateral subpleural ground-glass attenuation opacities (CO-RADS 5) with 27.6% parenchymal high attenuation areas in both lungs (calculation performed on Fujifilm Synapse 4D PACS dedicated application).
In order to search for a relation between morphological changes in peripheral blood cells and disease severity, COVID-19 patients were classified into stable (patients not requiring ICU admission, n = 48) and critical (ICU admitted patients, n = 83) groups. No statistical significance was found between the two groups except for RBCs changes and platelets’ thrombocytosis (Table 6). There was a significant increase in the percentage of patients showing normocytic (p = 0.0301), normochromic (p = 0.0246), with a significant decrease in the patients’ microcytic (p = 0.0109), and hypochromic RBCs (p = 0.0158) in critical ICU-admitted patients. Furthermore, stable COVID-19 patients showed higher levels of platelets’ thrombocytosis compared to critical COVID-19 patients (p = 0.0209).
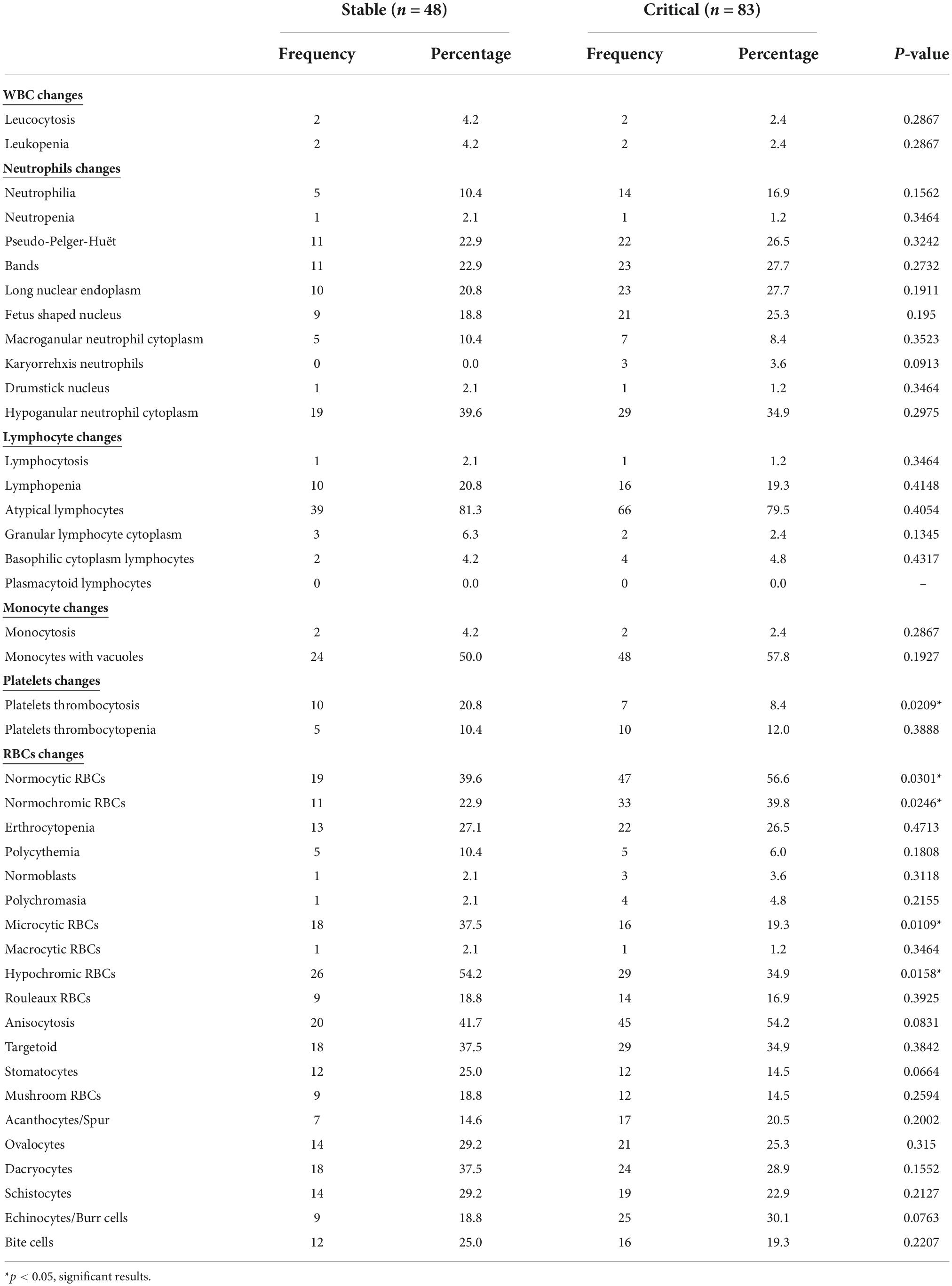
Table 6. Count and morphological changes in WBCs, platelets, and RBCs between stable and critical COVID-19 patient groups.
Another possible classification was to divide COVID-19 patients into those belonging to CO-RADS 5 group (n = 99) versus others (n = 30). There was an observed significant decrease in the neutrophils showing hypogranular cytoplasm in CO-RADS 5 group (p = 0.049). Also, there was a significant increase in the percentage of patients showing normocytic (p = 0.0431) and normochromic (p = 0.0135) RBCs in the CO-RADS 5 group. Further, there was a significant decrease in the percentage of patients showing ovalocytes in the CO-RADS 5 group (p = 0.0194, Table 7).
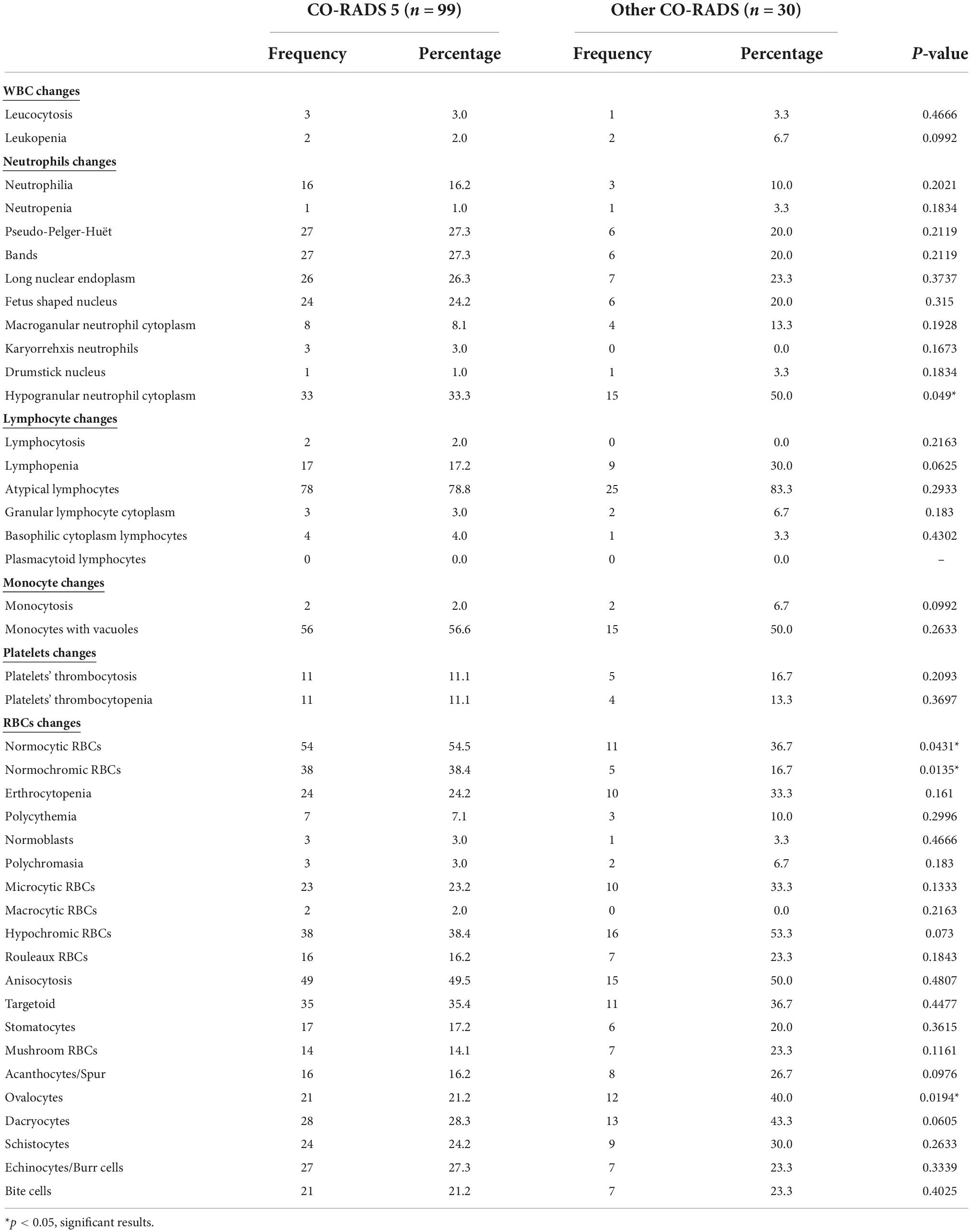
Table 7. Count and morphological changes in WBCs, platelets, and RBCs between COVID-19 patients with CO-RADS 5 and other CO-RADS.
Since gender plays a critical role in the COVID-19 pathogenesis (11, 12), it was interesting to explore if there is any difference in the peripheral blood anomalies between males (n = 63) and females (n = 68). There was a statistical significance in the chromicity of RBCs, where males showed a higher significant percentage of normochromic (p = 0.0093), with a concomitant decrease in the percentage of hypochromic RBCs (p = 0.0054, Table 8).
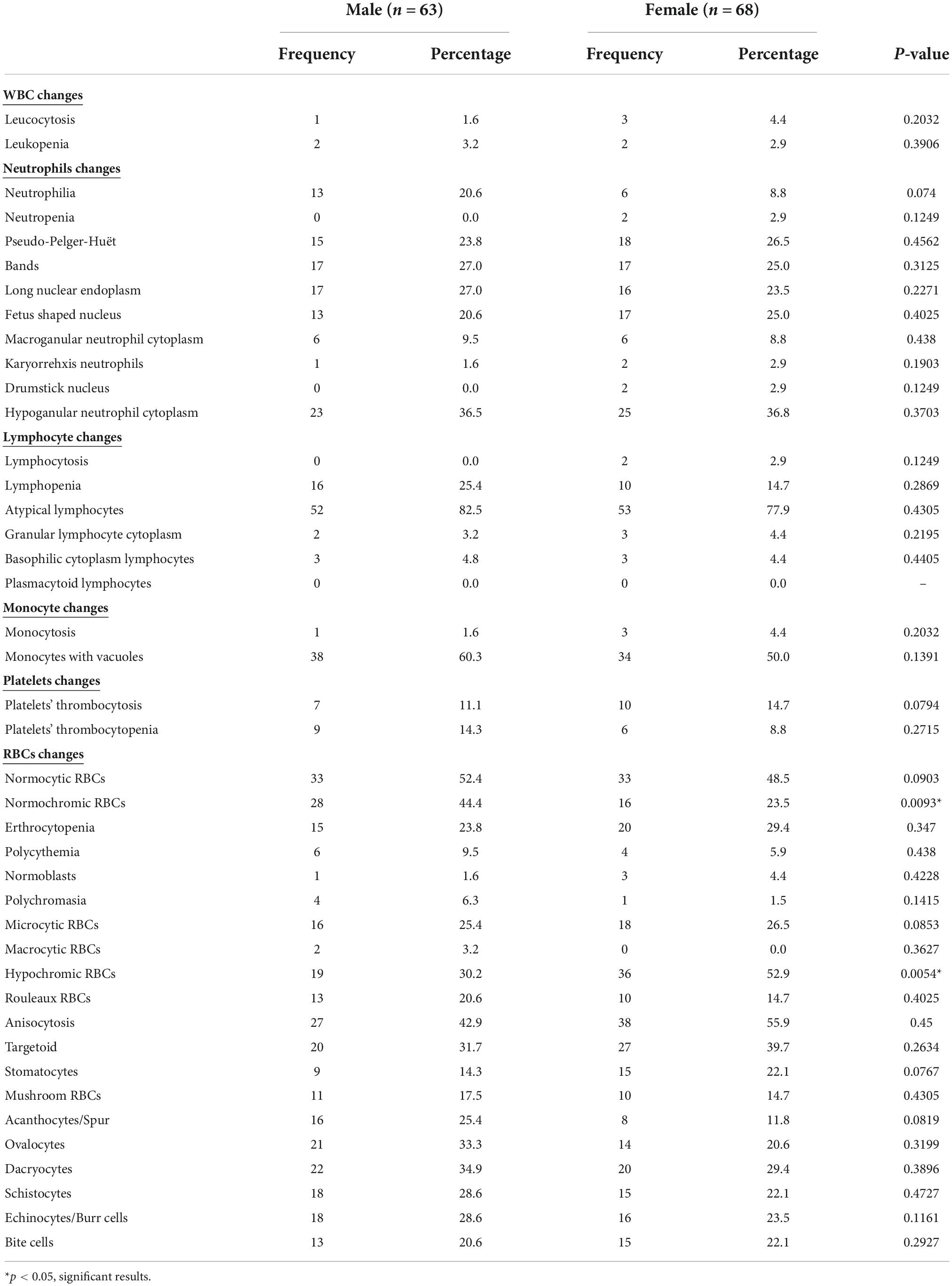
Table 8. Count and morphological changes in WBCs, platelets, and RBCs between male and female COVID-19 patients.
This study highlights the quantitative and morphological changes in the peripheral blood cells of COVID-19 patients. To our knowledge, this is the first study to report these changes in the UAE, which has taken extraordinary precautionary measures to restrict the spread of COVID-19 and guarantee the safety of citizens. Furthermore, this study explored if there is an association between disease severity and peripheral blood anomalies.
The most common morphological anomalies in our cohort were atypical lymphocytes, large monocytes with vacuoles, and hypogranular neutrophil cytoplasm of the peripheral blood smears. Despite the small number of reports on the peripheral morphological anomalies associated with COVID-19 infection, our findings go in line with a study by Zhang et al. where large monocytes with vacuoles were observed in peripheral smears of COVID-19 patients (13). In addition, our observed morphological anomalies were consistent with the findings by Zini et al. that reported various peripheral morphological blood changes, specifically in the neutrophils (14). Further, the presence of atypical lymphocytes was highly found to be similar to the previous reports (15–17). In addition, granulocytes and particularly neutrophils showed a pseudo-Pelger-Huët anomaly affecting 25% of the recruited COVID-19 patients, both stable and critical cases, unlike the observed findings by Ahnach et al. (18). Similarly, another type of neutrophil-associated anomaly was the presence of hypogranular cytoplasm in more than 30% of the patients (18).
Despite the advances in COVID-19 research, little information about the morphological changes in peripheral blood smears of infected individuals and their association with patients’ clinical outcomes is still unknown. Thus, we were interested in correlating the difference in these peripheral anomalies in ICU-admitted and stable COVID-19 patients. An increase in the percentage of patients showing neutrophilia, neutrophils with pseudo-Pelger-Huët, bands, long nuclear endoplasm, and fetus shaped nucleus, as well as large vacuolated monocytes, was recognized in the critical/ICU admitted group; however, such changes did not reach statistical significance. An increase in the percentage of aforementioned anomalies was also observed in COVID-19 patients with a CO-RADS score 5 compared to others. On the other hand, upon the classification of COVID-19 patients according to the severity of the disease or CO-RADS, there was a decrease in the number of patients showing hypogranular neutrophilic cytoplasm, which could be a sign of pulmonary deterioration. On the contrary, a study by Gabr et al. reported that the abundance of peripheral morphological abnormalities was significantly associated with unfavorable clinical outcomes in COVID-19 patients (17).
A plethora of abnormalities associated with RBCs was previously described in COVID-19 patients (19, 20). Morphological changes in COVID-19 patients were detected, along with a comparison between stable and critical cases. There was a significant decrease in the percentage of COVID-19 patients in the critical group with microcytic and hypochromic RBCs, along with a significant increase in the percentage of patients with normocytic and normochromic RBCs. A similar pattern was observed in the classification of COVID-19 according to CO-RADS. Additionally, there was a concomitant decrease in hemoglobin concentration in stable COVID-19 patients (11.4 ± 2.3) compared to critical (12.2 ± 2.0) cases. Hence, this could be attributed to other factors such as ferritin concentration or other underlying chronic diseases in such patients. Further, such findings suggest that anemia could be linked to inflammation, a known manifestation of COVID-19 infection. This was further confirmed with a higher percentage of female COVID-19 patients presenting hypochromic RBCs, which supports previous findings by Bergamaschi et al. (21).
To our knowledge, this is the first study in the UAE describing the morphological changes in the peripheral blood smears of COVID-19 patients and their association with disease severity. Peripheral blood smear assessment at the time of diagnosis in COVID-19 patients could provide information about the disease state and pulmonary involvement. One of the limitations of this study is the lack of information about the recruited patients’ mortality and the lack of peripheral smears of healthy controls for comparative investigation. Also, another limitation of this study is the lack of functional analysis of the aforementioned peripheral blood cells (including oxygen-carrying capacity of RBCs, ROS generation by leukocytes and immunoglobulin production by lymphocytes, phagocytosis capacity of macrophages/monocytes and leukocytes), that should be explored in future studies to further understand their role in the fight against SARS-CoV-2. Additionally, future studies could explore the association between antibody titers against SARS-CoV-2 proteins and hematological abnormalities that will aid in understanding the effect of infection and vaccinations on various blood cells.
The original contributions presented in this study are included in this article/supplementary material, further inquiries can be directed to the corresponding authors.
The studies involving human participants were reviewed and approved by the Ethics and Research Committee of University Hospital Sharjah in June 2020 (UHS-HERC-035-03052020). Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
NE and IT designed the study, analyzed, interpreted the results, and wrote the original draft. FB interpreted the slides of the peripheral blood smears. RG assessed the radiological imaging of the patients. DZ, AAl, NA, AH, FA, AE, AAh, and SA recruited and collected the data of the patients. RB designed the study. FB, RG, and RB reviewed the manuscript. All authors read and approved the final manuscript.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Borges do Nascimento I, O’Mathúna D, von Groote T, Abdulazeem H, Weerasekara I, Marusic A, et al. Coronavirus disease (COVID-19) pandemic: an overview of systematic reviews. BMC Infect Dis. (2021) 21:525. doi: 10.1186/s12879-021-06214-4
2. Al-Hosani F, Al-Mazrouei S, Al-Memari S, Al-Yafei Z, Paulo M, Koornneef EA. Review of COVID-19 mass testing in the United Arab Emirates. Front Public Health. (2021) 9:661134. doi: 10.3389/fpubh.2021.661134
3. Alimohamadi Y, Sepandi M, Taghdir M, Hosamirudsari H. Determine the Most common clinical symptoms in COVID-19 patients: a systematic review and meta-analysis. J Prev Med Hyg. (2020) 61:E304–12. doi: 10.15167/2421-4248/jpmh2020.61.3.1530
4. World Health Organization [WHO]. Coronavirus disease 2019 (Covid-19): situation Report, 51. Geneva: World Health Organization (2020).
5. McElvaney O, McEvoy N, McElvaney O, Carroll T, Murphy M, Dunlea D, et al. Characterization of the inflammatory response to severe COVID-19 illness. Am J Respir Crit Care Med. (2020) 202:812–21. doi: 10.1164/rccm.202005-1583OC
6. Tay M, Poh C, Rénia L, MacAry P, Ng L. The trinity of COVID-19: immunity, inflammation and intervention. Nat Rev Immunol. (2020) 20:363–74. doi: 10.1038/s41577-020-0311-8
7. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. (2020) 395:497–506. doi: 10.1016/S0140-6736(20)30183-5
8. Tan L, Wang Q, Zhang D, Ding J, Huang Q, Tang Y, et al. Lymphopenia predicts disease severity of COVID-19: a descriptive and predictive study. Signal Transduct Target Ther. (2020) 5:33. doi: 10.1038/s41392-020-0148-4
9. Nazarullah A, Liang C, Villarreal A, Higgins R, Mais D. Peripheral blood examination findings in sars-Cov-2 infection. Am J Clin Pathol. (2020) 154:319–29. doi: 10.1093/ajcp/aqaa108
10. Kubánková M, Hohberger B, Hoffmanns J, Fürst J, Herrmann M, Guck J, et al. Physical phenotype of blood cells is altered in COVID-19. Biophys J. (2021) 120:2838–47. doi: 10.1016/j.bpj.2021.05.025
11. Hachim I, Hachim M, Talaat I, López-Ozuna V, Saheb Sharif-Askari N, Al Heialy S, et al. The molecular basis of gender variations in mortality rates associated with the novel coronavirus (COVID-19) outbreak. Front Mol Biosci. (2021) 8:728409. doi: 10.3389/fmolb.2021.728409
12. Jin J, Bai P, He W, Wu F, Liu X, Han D, et al. Gender differences in patients with COVID-19: focus on severity and mortality. Front Public Health. (2020) 8:152. doi: 10.3389/fpubh.2020.00152
13. Zhang D, Guo R, Lei L, Liu H, Wang Y, Wang Y, et al. Frontline science: COVID-19 infection induces readily detectable morphologic and inflammation-related phenotypic changes in peripheral blood monocytes. J Leukoc Biol. (2021) 109:13–22. doi: 10.1002/JLB.4HI0720-470R
14. Zini G, Bellesi S, Ramundo F, d’Onofrio G. Morphological anomalies of circulating blood cells in COVID-19. Am J Hematol. (2020) 95:870–2. doi: 10.1002/ajh.25824
15. Gérard D, Henry S, Thomas B. Sars-Cov-2: a new aetiology for atypical lymphocytes. Br J Haematol. (2020) 189:845. doi: 10.1111/bjh.16730
16. Berber I, Cagasar O, Sarici A, Berber N, Aydogdu I, Ulutas O, et al. Peripheral blood smear findings of COVID-19 patients provide i?nformatio about the severity of the disease and the duration of hospital stay. Mediterr J Hematol Infect Dis. (2021) 13:e2021009. doi: 10.4084/MJHID.2021.009
17. Gabr H, Bastawy S, Abdel Aal A, Khalil N, Fateen M. Changes in peripheral blood cellular morphology as diagnostic markers for COVID-19 infection. Int J Lab Hematol. (2022) 44:454–60. doi: 10.1111/ijlh.13799
18. Ahnach M, Ousti F, Nejjari S, Houssaini M, Dini N. Peripheral blood smear findings in COVID-19. Turk J Haematol. (2020) 37:310–2. doi: 10.4274/tjh.galenos.2020.2020.0262
19. Berzuini A, Bianco C, Paccapelo C, Bertolini F, Gregato G, Cattaneo A, et al. Red cell-bound antibodies and transfusion requirements in hospitalized patients with COVID-19. Blood. (2020) 136:766–8. doi: 10.1182/blood.2020006695
20. Marchi G, Bozzini C, Bertolone L, Dima F, Busti F, Castagna A, et al. Red blood cell morphologic abnormalities in patients hospitalized for COVID-19. Front Physiol. (2022) 13:932013. doi: 10.3389/fphys.2022.932013
Keywords: CO-RADS, COVID-19, lymphocytes, neutrophils, peripheral smears, UAE
Citation: Elemam NM, Talaat IM, Bayoumi FA, Zein D, Georgy R, Altamimi A, Alkhayyal N, Habbal A, Al Ali F, ElKhider A, Ahmed A, Abusnana S and Bendardaf R (2022) Peripheral blood cell anomalies in COVID-19 patients in the United Arab Emirates: A single-centered study. Front. Med. 9:1072427. doi: 10.3389/fmed.2022.1072427
Received: 17 October 2022; Accepted: 24 November 2022;
Published: 15 December 2022.
Edited by:
Mohamed A. Yassin, Hamad Medical Corporation, QatarReviewed by:
Younes Zaid, Mohammed V University, MoroccoCopyright © 2022 Elemam, Talaat, Bayoumi, Zein, Georgy, Altamimi, Alkhayyal, Habbal, Al Ali, ElKhider, Ahmed, Abusnana and Bendardaf. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Iman M. Talaat, aXRhbGFhdEBzaGFyamFoLmFjLmFl; Riyad Bendardaf, cml5YWQuYmVuZGFyZGZAdWhzLmFl
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.