
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
STUDY PROTOCOL article
Front. Med., 13 December 2022
Sec. Geriatric Medicine
Volume 9 - 2022 | https://doi.org/10.3389/fmed.2022.1071409
This article is part of the Research TopicMolecular and Physiological Aspects of Sarcopenia in the Older Person: Mechanisms, Diagnostics and TherapyView all 12 articles
Objective: Elderly individuals in long-term care facilities (LTCFs) have a higher prevalence of sarcopenia than those in the community. Exercise is the gold standard for preventing and treating sarcopenia. Regarding exercise, multicomponent exercises, including progressive resistance training (PRT), are beneficial. However, developing routine, structured exercise programs for the elderly in LTCFs is difficult because of a shortage of healthcare providers, particularly in rural regions. Exergame-based exercises can increase a player’s motivation and reduce staff time for an intervention. Nintendo Switch RingFit Adventure (RFA) is a novel exergame that combines resistance, aerobic, and balance exercises. In this study, we aim to investigate the clinical effectiveness of RFA on muscle and functional performance parameters among the elderly in LTCFs.
Methods: The EXPPLORE (using EXergame to Prevent and Postpone the LOss of muscle mass, muscle strength, and functional performance in Rural Elders) trial is a single-center randomized controlled trial involving elderly individuals (≥60 years) living in LTCFs in rural southern Taiwan. The participants will be equally randomized to the intervention group (exergame-based exercise plus standard care) or the control group (standard care alone). Both groups will receive standard care except that the intervention group will receive exergame-based exercises at the time previously scheduled for sedentary activities in the LTCFs. The exergame-based exercise will be performed using RFA in the sitting position with a specialized design, including arm fit skills and knee assist mode. Each session of the exercise lasts 30 mins and will be performed two times per week for 12 weeks. The primary outcomes will be the osteoporotic fracture index, appendicular skeletal muscle mass index, dominant handgrip strength, and gait speed. Meanwhile, the secondary outcomes will be the dexterity and agility, muscle strength and thickness, range of motion of the joints of the dominant upper extremity, Kihon checklist, Medical Outcomes Study 36-Item Short-Form Health Survey, and Brain Health Test.
Discussion: This trial will provide valuable knowledge on whether exergames using RFA can counteract physical decline and improve quality of life and cognition among the elderly in LTCFs.
Clinical trial registration: [www.ClinicalTrials.gov], identifier [NCT05360667].
Taiwan is now an aging society, and the population of elderly individuals aged ≥65 years constituted 15.95% of the total population in 2020. It is estimated that Taiwan will become a super-aged society as the number of individuals aged ≥65 years grow to be more than 20% of the total population by 2025 (1). Aging and inactivity are associated with declines in muscle mass, architecture, and strength (2, 3). The rate of muscle loss ranges from 1 to 2% per year for individuals more than 50 years old (4). Sarcopenia, defined as an age-related loss of skeletal muscle mass and a decline in muscle strength and physical performance (5), is thus emerging as an important issue in modern society. As reported by the Asian Working Group for Sarcopenia (AWGS), the prevalence of sarcopenia in community-dwelling older men and women in Taiwan was 9.3 and 4.1%, respectively (6). For mobility-impaired older adults, regular physical activity can prevent further disabilities and improve their overall health (7, 8), while physical inactivity is an important factor contributing to the development of sarcopenia (9). The prevalence of sarcopenia is much higher in individuals living in care facilities than those residing in the community, ranging between 17.7 and 73.3% in long-term nursing homes (10) and between 22 and 87.1% in daycare centers, because they are older and sicker and require more assistance with their activities of daily living (ADLs) after being admitted to care facilities (10–12).
The first-line strategies for preventing and treating sarcopenia focus on preserving skeletal muscle mass and maintaining muscle strength (13). A newly published network meta-analysis revealed that mixed exercises and physical activity with nutritional supplementation are the most effective interventions for sarcopenia (14). Resistance training (RT), particularly progressive RT (PRT) (15, 16), and multicomponent exercises have moderate- to high-quality evidence for their positive and significant effects on increasing muscle mass, muscle strength, and physical performance among elderly individuals with sarcopenia (17, 18). Moreover, some studies showed that low-intensity RT [≤50% 1 repetition maximum (RM)] is sufficient to induce strength gains (19, 20). However, the optimal exercise prescription, regarding intensity, type, frequency, duration, and progression, for preventing and treating sarcopenia among elderly individuals is still controversial (14, 17).
Taiwan is one of the fastest-aging countries in the world (21). The Taiwanese government established a long-term healthcare system in 2010, which was reformed into The Long-Term Care 2.0 Plan (LTC 2.0) in 2017 to guarantee suitable services in response to the fast-growing care needs of older individuals (21). The LTC 2.0 aims to provide aging-in-place values into practice by delivering integrated home- or community-based primary healthcare and preventive services (22). Based on the consensus of the AWGS in 2019, community-based care facilities are important places for integrated LTC services to prevent or delay disability, particularly for individuals who are physically inactive or at risk of sarcopenia (23). These settings are essential, particularly in rural regions in Taiwan, where the proportion of elderly individuals is higher than that in urban areas (24) and the healthcare resources are limited (25).
The principles of PRT and multicomponent exercise programs include regular, mass-practiced, mildly overwhelming engagement (26). To achieve these principles, the devotion of time, workforce, and money are critical. Staffing constraints and resource shortages have made it challenging to promote regular exercise programs in long-term care facilities (LTCFs) (27, 28). Exergames are defined as any type of video game that requires the movement of the player’s entire body, allowing real-time interaction (29). Exergames breakdown the barriers of repetitive and monotonous physical exercises since they contain attractive and multisensory game environments with an immersive environment in which the interaction occurs through whole-body movements (30). Moreover, the gamified approach and immersive scenarios motivate older individuals to acquire a greater commitment to the practice of physical and rehabilitative exercises (31). Therefore, playing exergames reduces staff time for intervention, encourages patients to perform relatively high-energy movements, and increases their motivation. Among community-dwelling older individuals with or without specific diseases (32), studies have proved the therapeutic application of exergames in improving lower limb strength (33), gait speed (34), balance (35), and cognitive function (34, 36). Few studies have evaluated the clinical effectiveness of exergames in LTCFs, and most outcomes of these studies pertained to health-related quality of life (HRQoL), cognition, and general functional status (37–39). Our team found that the handgrip strength (HGS) and walking speed of elderly individuals with sarcopenia living in care facilities improved significantly after 12 weeks of exergame-based progressive RT(40). However, it was a quasi-experimental study involving relatively few participants, and the platform to deliver exergames was difficult for older adults to use. Therefore, in this study, we will evaluate the feasibility and clinical application of a novel exergame-based multicomponent training program using Nintendo Switch® RingFit Adventure (RFA), which could deliver optimal exercise intensity for each player and perform fine-tuned upregulation and downregulation based on performance after each game, among elderly individuals living in rural care facilities.
This randomized controlled trial (RCT) compares an exergame-based multicomponent exercise training (exergame-based exercise) to the standard care in older users of LTCFs in rural regions. The trial design adheres to the Standard Protocol Items: Recommendations for Interventional Trials (SPIRIT) guidelines for RCT (41) and the Consolidation Standards of Reporting Trials guidelines (42). The flowchart of this study is shown in Figure 1. This study will be conducted according to the Declaration of Helsinki, was approved by the Institutional Review Board of a medical center in Taiwan (approval number: B-ER-111-058), and was registered at www.ClinicalTrials.gov (registration number: NCT05360667).
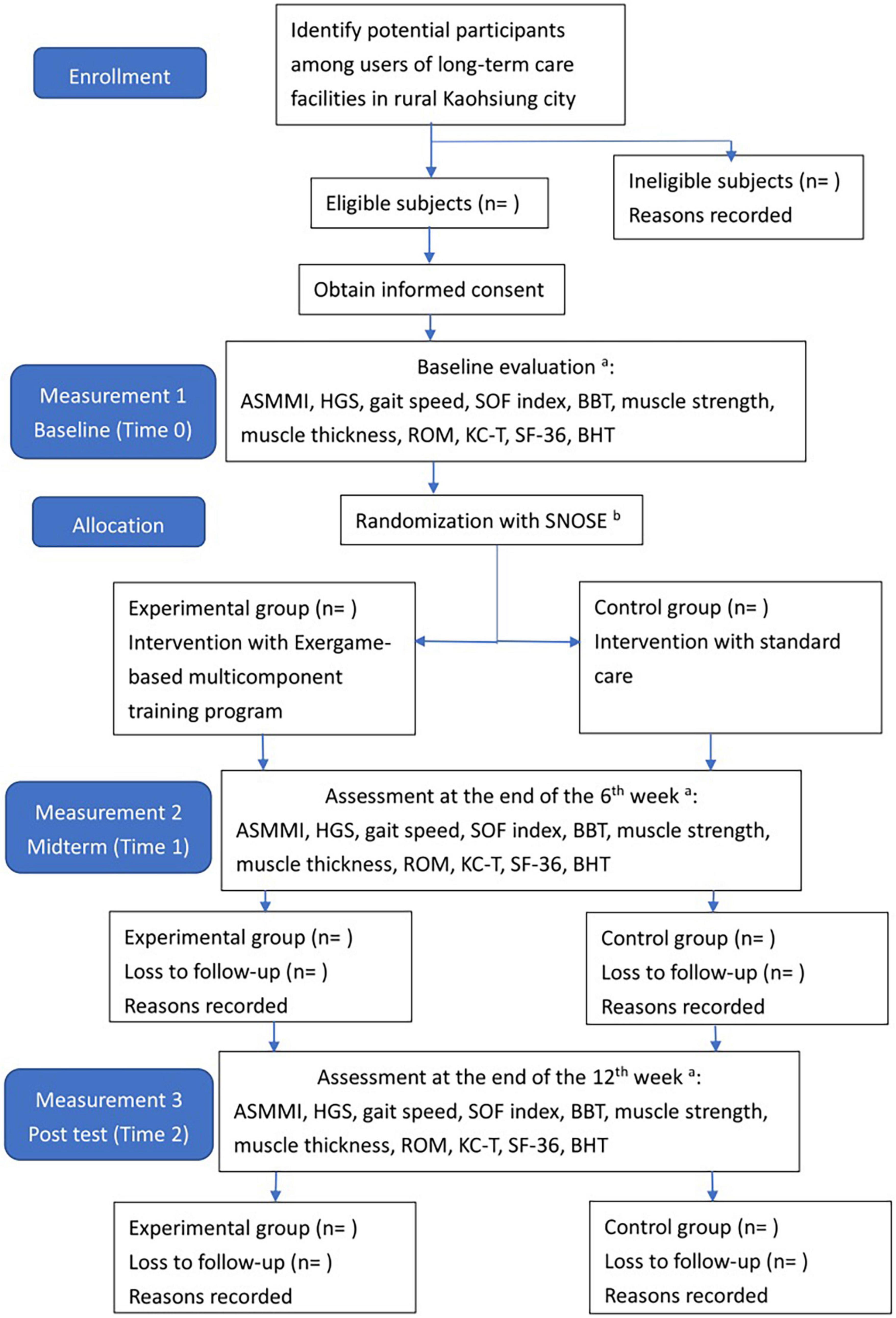
Figure 1. The flowchart of the participant inclusion and data collection process. aSee Table 1; bsequentially numbered, opaque, and sealed envelopes. ASMMI, appendicular skeletal muscle mass index; HGS, handgrip strength; SOF index, study of osteoporosis index; BBT, box and block test; ROM, range of motion; KC-T, Kihon checklist Taiwan version; SF-36, short form 36 questionnaire; BHT, brain health test.
All individuals, who participate regularly in LTCFs, including daycare centers and nursing homes, in rural regions of Kaohsiung City, southern Taiwan, will be eligible for study participation. The inclusion criteria are as follows: individuals (a) aged ≥60 years, (b) those living or participating in LTCFs for at least 1 month, (c) those who can understand and speak Chinese or Taiwanese, (d) those with sufficient cognitive capacity (judged by the researchers) to give informed consent and participate in the exergame-based exercise and data collection, and (e) those who can sit for more than 50 min for training and can complete the measurement of gait speed. (a) Individuals who have significant cardiopulmonary diseases, (b) those who regularly receive oxygen supplementation, (c) those who have uncontrollable hypertension, and (d) those who had a recent infection or fracture or were diagnosed with other diseases that might prohibit them from participating in exercises according to the guidelines of the American College of Sports Medicine will be excluded from this study (43). Participants in the intervention group will receive standard care with the exergame-based exercise for 12 weeks, whereas those in the control group will receive standard care routinely applied in LTCFs as usual. We will replace the scheduled sedentary activities in the LTCFs, such as singing, table games, and gardening, with the exergame-based exercise in the intervention group. Meanwhile, participants in the control group will perform the aforementioned sedentary activities in the LTCFs as usual. Therefore, the time for activities in the two groups will be the same. In addition to the exergame-based exercise and standard care, all participants will perform the usual traditional rehabilitation provided by therapists at the LTCFs.
We will use sequentially numbered, opaque, sealed envelopes containing a group assignment number created by a person who is not clinically involved and, therefore, could be blinded to this study. Participants who fulfilled the inclusion and exclusion criteria will be equally randomized to the intervention and control groups with an allocation ratio of 1:1.
The program consists of PRT and functional movement of the four extremities but mainly the upper limbs. We will use RFA to deliver the program. RFA is a Nintendo Switch®-based exergame. It requires one Nintendo Switch video game console, one Ring-Con (a Pilates ring that the user holds), one wireless controller Joy-Con (one should be placed on the Ring-Con and the other one should be affixed into a leg strap on the thigh of the player), and one display screen (Figure 2). The exergame-based exercise will be performed two times per week, at least 48 h apart from each training session, 50 min per session (10 min each for a warm-up and cool-down and 30 min for the main program), for 12 weeks, and will be supervised by a therapist.
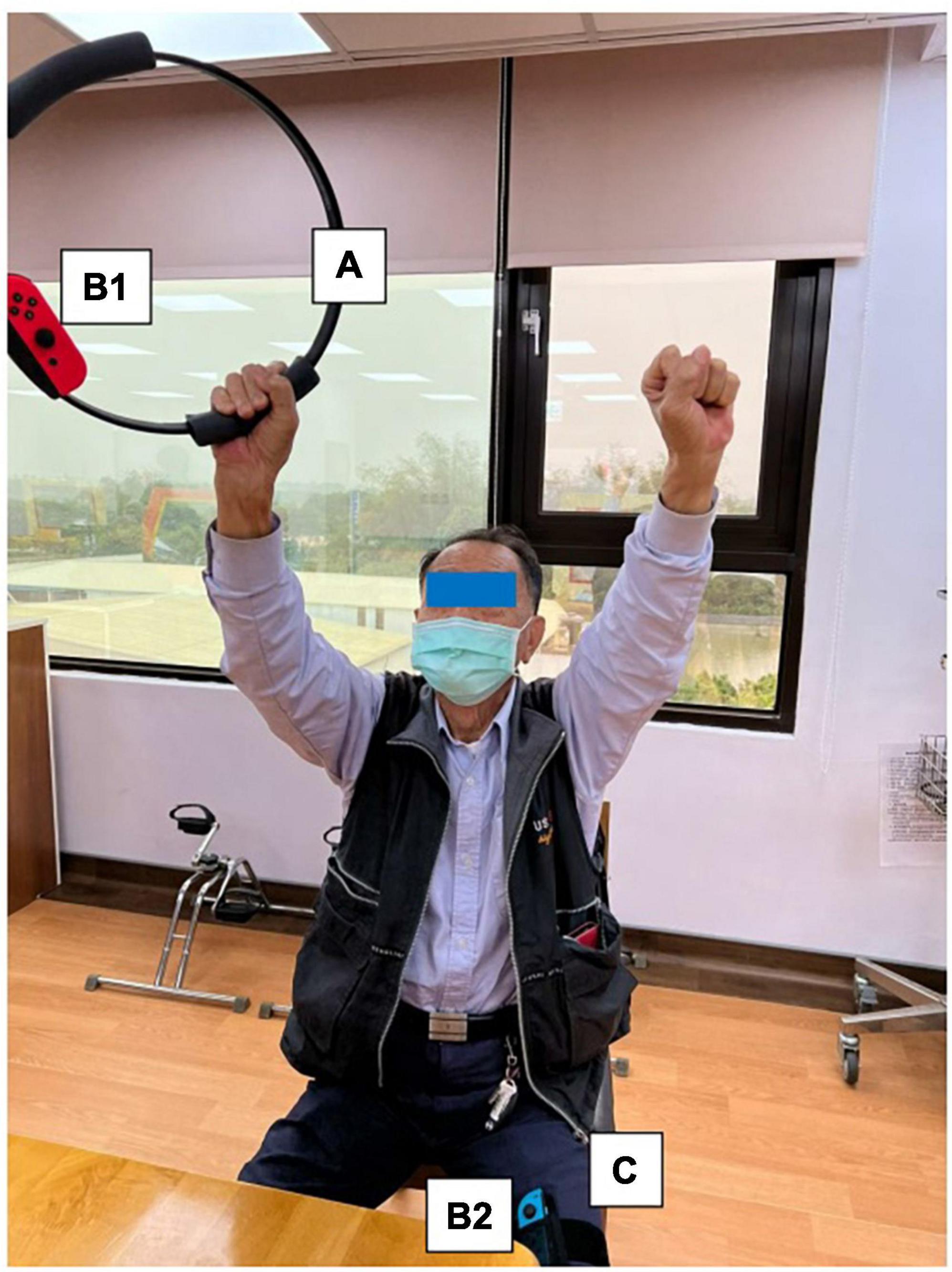
Figure 2. Components of Nintendo Switch. To play the RingFit Adventure, the player needs to use the Nintendo Switch, which includes the following devices: A. Ring-Con: A Pilates ring the user holds; B. Joy-Con: A wireless controller. One of the Joy-Con (B1) should be placed on the Ring-Con (A). The other Joy-Con (B2) should be affixed to a Leg Strap (C) on the thigh of the player.
RingFit Adventure is a fitness action role-playing game. The player advances the story while exercising as the movement of the player is linked to the main character on the screen. The movements of the player and battle actions are based on the performance of certain physical activities using the Ring-Con and leg strap (44). Ring-Con is a controller of the system with a built-in high-precision force and strain sensor that detects and digitizes the player’s movements, such as stretching and squeezing. Joy-Con is equipped with a motion infrared-ray camera and is used to monitor the heart rate of the player. RFA could estimate the optimal exercise intensity for each player and perform fine-tuned upregulation and downregulation based on this physiological feedback (45). Therefore, providing an appropriate amount of exercise for all generations, from children to the elderly, has become possible (46, 47).
Routinely, the player controls the character by jogging or squatting in the Adventure Mode. Each stage of the Adventure Mode consists of several battle scenes; in addition to aerobics training, the player must perform intensive RT and yoga exercises that exert stress on the muscles of the entire body to defeat the enemy and clear the stage. Players are rewarded based on the amount of exercise they perform and continue to advance while continuously improving their skills. Given that many individuals living in the LTCFs are becoming older and sicker and require more assistance with their ADLs, they have a higher potential risk of falls, and exergame-based exercise should be supervised to reduce unnecessary walking (40). Moreover, some individuals living in LTCFs use wheelchairs mainly for ambulation (28). Therefore, we will use the knee assist mode in RFA, which helps the player character jog and sprint when it is vital for level completion in the game. This means that traversal of the Adventure Mode is possible for players who only have reliable or pain-free use of their arms and trunk.
At the beginning of the game, we will enter the age, sex, and weight of each player, and they should stretch and squeeze the Ring-Con as hard as possible to measure their maximal intensity (this step could be considered the concept of 1 RM as in the traditional RT). Then, the Nintendo Switch sets the initial amount of exercise that must be performed in each stage and adjusts it progressively and automatically depending on the performance of the player. The ideal intensity of each session will set to be 13 (somewhat hard) on the Borg Rating of Perceived Exertion (RPE) scale (48). The higher the intensity, the more repetitions and the larger resistance of the Ring-Con to be stretched and squeezed. The supervisor could also adjust the intensity level manually based on the performance of the player; however, we will not adjust the intensity level manually in this study to ensure the consistency of the protocol. The Joy-Con on the Ring-Con could detect the heart rate of the player after the training session. RFA could provide a summary of the training results, such as exercising time, total calories burned, and total distance ran, after each training session. Warm-up and cool-down will last 10 min each for each training session. In addition to the data RFA records, we will measure the blood pressure, heart rate, heart rate reserve, and oxygen saturation using a pulse oximeter before and after each training session.
As for the skills required to complete the game, in addition to the regular stretching and squeezing that are mandatory for the character player to progress and earn rewards in the Adventure Mode, we have developed six fit skills that focus on training the upper extremities and trunk from the list provided by RFA, including overhead press, shoulder press, front press, bow pull, overhead arm spin, and triceps kickback. The player must choose three of the six aforementioned fit skills to defeat the monster in each beat mode. The flowchart of the exergame-based exercise and the corresponding trained muscle and joint movement is provided in Table 1.
The standard care in the control group will be applied as usual in our LTCFs, in the way of group activities, including calisthenics (that could be performed in the sitting position), horticultural therapy, and group static activities (e.g., tabletop games). The programs will be performed two times per week for approximately 30–60 min, depending on the activity, and will be led by a therapist.
Because of the design of the study and the nature of the interventions, blinding the staff and participants of the LTCFs is impossible. The assessors, measuring the outcomes, and the interpreter, analyzing the data, will be blinded in this study.
All participants will be subjected to three evaluations. The first evaluation is at baseline (Time 0), which is before randomization. The second and third evaluations will be performed at the end of the 6th (Time 1) and 12th (Time 2) weeks after the intervention, respectively (Table 2).
The primary outcomes chosen for this study are the criteria for the diagnosis of sarcopenia proposed by the AWGS, including appendicular skeletal muscle mass index (ASMMI), dominant HGS, and usual gait speed. Moreover, the Study of Osteoporotic Fractures Index (SOF index), which indicates the frailty status, is also one of the primary outcomes.
We will perform bioelectrical impedance analysis (BIA) to evaluate the participant’s appendicular skeletal muscle mass. Compared with other established methods for measuring body composition, including dual-energy X-ray absorptiometry, computed tomography, and magnetic resonance imaging, BIA has been widely used in clinical settings because it is relatively simple, quick, and non-invasive (49). BIA of the tetrapolar eight-point electrode type (InBody S10 for the supine measure, InBody Co., South Korea) will be used in this study given that some participants will be difficult to measure in the standing position. This BIA model enables multifrequency impedance measurement of the arms, trunk, and legs using eight electrodes positioned at each hand and foot. Impedance parameters are measured with alternating currents of 80 and 100 mA at frequencies of 1, 5, 50, 250, 500, and 1,000 kHz for InBody S10 (50). The participants will be placed in the lying position for approximately 10–15 min before the test so that body water may be dispersed evenly inside the body. The four extremities should be spread naturally to a 15° angle away from the trunk to ensure that the extremities do not touch the trunk part of the body (51). The device will be calibrated in the morning using a standard control circuit supplied by the manufacturer. The ASMMI is defined as the appendicular skeletal muscle mass (in kg) divided by the height squared (in m2) (52).
The HGS will be measured using a JAMAR dynamometer (J A Preston Corporation, New York, NY, USA) using all five notches. A JAMAR dynamometer is a hydraulic instrument that measures isometric strength in kilograms. It has been proven to have good reliability in various older populations (53). The measurement will be performed under a standard position, and the instrument should be freely held. Each participant will be instructed to sit straight with their upper arm in a neutral position and their elbow flexed at 90°C, their forearm in a neutral position, and their wrist at 0–30°C extension (54). The measurement should be performed three times, and the highest of the three measurements will be recorded. The participants will be allowed to rest for 1 min between measurements. The minimal clinically important difference (MCID), defined as the minimal amount of change required to distinguish a true performance change due to variability in performance or measurement error, is also measured in this study. No available studies on the MCID of the HGS in older adults so far, whereas, in healthy individuals, the MCID of the HGS is 2.44–2.69 kg (55).
The participants will be instructed to walk at a normal speed on a 6-m-long corridor without a barrier, and the usual gait speed is calculated by measuring the time spent to reach the end of the corridor by a participant as suggested by the AWGS (52). The participants could walk with or without assistive devices during the measurement. The time will be initially recorded once the participants start walking and stop at the point when they reach a distance of 6 m. Gait speed should be measured two times, and the average of the two speeds will be recorded. The participants will be allowed to rest for 10 min between measurements. The MCID of gait speed across multiple patient groups is 0.10–0.20 m/s (56).
The SOF index consists of the following three components: (a) a weight loss of ≥5% during the preceding year (regardless of the intention to lose weight), (b) the inability to rise from a chair five times without using the arms, and (c) an answer of “no” to the question “Do you feel full of energy?” The participants will be identified to be frail if they have two or more of the aforementioned components; those with one disability are considered in pre-frailty status, and those with none of the aforementioned impairments are considered robust (57). The SOF index has been proven to be a valid tool to evaluate frailty, particularly for community-dwelling older adults in Taiwan (58).
The box and block test (BBT) can be used to measure the unilateral gross manual dexterity in various populations with high test–retest reliability and validity (59). The setup of the BBT consists of a wooden box divided into two compartments, with 100 wooden blocks inside one compartment. The participants will be instructed to transfer the wooden blocks one by one from one compartment to the other in the sitting position. The score is based on the number of blocks the participants transferred in 60 s. Most studies on the MCID of the BBT have involved patients with stroke, and the MCID was 5.5 cubes/min for the most affected side and 7.8 cubes/min for the least affected side (60).
We will use the microFET® 3 (Hoggan Health Industries, West Jordan, UT, USA) to measure the maximal voluntary isometric contraction (MVIC) of the biceps and triceps brachii of the dominant side. The microFET® 3 is an electronic handheld dynamometer that can detect 0–150 lb of force with high reliability and validity (61). The participants will be instructed to lie on the treatment table with their elbows forming a 90° angle to the horizontal such that the arm is perpendicular to the limb. The device will be placed on the ventral (for the biceps brachii) or dorsal (for the triceps brachii) side of the arm and aligned with the ulnar styloid. The participants will be encouraged to go against the force, which is exerted toward the device, with their maximum strength (62). The MVIC will be measured two times, and the average of the two measurements is recorded. The participants will be allowed to rest for 1 min between measurements.
A single-experienced operator, who is not involved in any further data analysis and is blinded to clinical symptoms, will use a portable LOGIQ e-ultrasound (General Electric Company, USA, 2010) equipped with a 5–12-MHz linear array transducer to measure the muscle thickness under sonography. Measurements should be performed by gently applying the transducer onto the skin that is coated by a thin layer of water-soluble gel. The transducer should be held orthogonal to the skin surface to ensure precise depth analyses and avoid transmission parallax error. All participants will undergo measurements in the afternoon. All measurements will be performed once on each side and recorded, respectively. The position used to measure each muscle is as follows:
The thickness of the brachial biceps will be obtained at two-third of the way between the acromion and the antecubital crease of the examined upper limb with the transducer placed perpendicular while exerting minimum pressure. The examined upper limb should be extended fully. The thickness is measured in the transverse plane (63).
The thickness of the brachial triceps will be obtained at the proximal one-third of the way between the acromion and the olecranon of the examined upper limb with the transducer placed perpendicular while exerting minimum pressure. The examined upper limb should be overhead and extended fully. The thickness is measured in the transverse plane (64).
The range of motions (ROMs) of the dominant upper extremity, including shoulder flexion, abduction, and external rotation; elbow flexion and extension; forearm supination and pronation; and wrist flexion and extension, will be measured. The ROMs will be measured using a goniometer under standard positions (65).
We will use the Kihon checklist-Taiwan (KC-T) to indicate the ADLs of the participants in this study. The KC-T is a self-reported questionnaire consisting of 25 items divided into seven subcategories: general independence, physical strength, nutrition, oral function, level of social activities outside the home, cognitive function, and risk of depression. Each item is rated as a pass (0) or fail (1); therefore, a higher total score indicates a lower level of function (66). The KC-T is used by the Ministry of Health and Welfare in Taiwan as an outcome indicator for community-based programs that delay and prevent disability (67), and its usability in practice in real-world settings in Taiwan has been proven (68).
We will use the Medical Outcomes Study 36-Item Short-Form Health Survey (SF-36) to indicate the HRQoL of the participants in this study. The SF-36 is a self-assessment validated generic health survey containing 36 items divided into eight subscales: physical functioning, role limitation due to physical problems, bodily pain, general health, vitality, social functioning, role limitation due to emotional problems, and mental health. The first four subscales represent the physical function, and the subsequent four subscales represent the mental function. Responses to each question will be transformed into a scale ranging from 0 to 100. The higher the scores, the better the HRQoL (69). All subscales have high levels of validity and reliability. The SF-36 has an acceptable internal consistency (Cronbach’s α value ranged from 0.74 to 0.95) among the Taiwanese population (70). We will record the scores of the entire questionnaire, physical function, and mental function in this study.
We will use the Brain Health Test (BHT)–brief cognitive test (BHT-Cog) to measure the cognitive level of the participants in this study. The BHT, developed by the Taiwan Dementia Society, is a simple dementia screening tool with high validity that can help primary care physicians identify patients with cognitive impairment among subjects with memory complaints or those at a high risk of dementia. It consists of risk factors and a brief cognitive test. The BHT-Cog includes orientation to time, immediate and delayed recall of five items, a categorical verbal fluency test (listing four-legged animals in 1 min), and the Clock Drawing Test (10:10) (71). The Ministry of Health and Welfare also uses the BHT in Taiwan as an outcome indicator for community-based programs that delay and prevent disability (67).
Since a high-quality study evaluating the effects of a similar intervention on muscle strength, physical activity, and function was unavailable when we wrote our protocol, we used previous results from one study using augmented reality (AR)-based exercise for one of our primary outcome measures (ASMMI) (72) for this power calculation. The effect size of a similar study for the AR-based intervention is high (0.71). Based on G*Power (version 3.1.9.2, for Windows), at least 18 observations in each group should be recruited by detecting a difference of 2 standard deviations (SD) of the ASMMI between the groups with a power of 80% and alpha of 5%, and the effect size is determined to be high (F-test family, 0.4) (73). To account for an expected dropout rate of 40%, given that most participants in the LTCFs have comorbidities, we decided to increase this number to a group size of 26. Thus, the aim will be to include at least 52 patients in the study.
We will use Statistical Package for the Social Sciences for Windows (version 19.0; Released 2010; IBM Corp., Armonk, NY, USA) for all statistical analyses. Continuous data are expressed as means with SDs, and categorical variables are presented as absolute numbers or percentages. The normality and homoscedasticity of the data will be checked before each analysis. For comparisons of demographic data between the experimental and control groups, the chi-square test, independent t-test, and Mann–Whitney U-test will be used as appropriate depending on the features of distributions of the data. As for the training effects on outcomes, a mixed analysis of variance, with time as a within-subject factor and intervention as a between-subject factor, will be performed. Post hoc analysis will be performed using the Bonferroni test. P-values < 0.05 will be used to indicate statistical significance. If both the data and the residuals are not normally distributed for ANOVA, we will use bootstrapping to get confidence intervals and use those to determine whether effects are statistically significant, rather than using p-values directly.
This study protocol describes the design of an RCT that evaluates the clinical effect of the exergame-based exercise delivered via RFA among older adults in LTCFs. Individuals around the world live longer nowadays, and many countries will become a super-aged society soon. Preventing and delaying the loss of intrinsic capacity and functional ability of older adults and helping them age successfully are crucial for us (74). Elderly individuals living in LTCFs are more prone to geriatric syndromes, such as frailty and sarcopenia, than those living in the community. Moreover, many LTCFs lack healthcare professionals, particularly those in rural regions. This project aims to study whether we can use exergame-based exercise as an alternative to previous manpower-consuming therapies in LTCFs. Given that the concepts of frailty and sarcopenia are multifactorial and their definitions vary, this study focuses on the parameters of muscle and functional performance.
This project is unique as the exergame-based exercise is delivered via RFA. Similar to other exergames, RFA uses a gamified approach and immersive scenarios to motivate the player by role-playing (31). It could provide both visual feedback from the screen and sensory feedback from the Ring-Con. Apart from other exergames, with its featured Ring-Con, RFA could be considered a multicomponent exercise, combining PRT and aerobic exercises for strength, balance, and muscle stretching. Studies have evaluated the effectiveness of PRT among community-dwelling older adults and proven that it is easily available at a low cost and effective in improving physical function and strength (10, 75). Therefore, we are looking forward to the clinical effectiveness in improving the muscle parameters after this study.
Another feature of using RFA to deliver exergames is that it could set up the initial amount of exercise that must be performed in each stage and adjust it progressively and automatically depending on the performance of the player. Therefore, the progression for the exercise prescription might be individualized, and it is time- and manpower-saving given that it could be modified by the machine. The ACSM suggests increasing intensity over time to maintain the intensity of the exercises at moderate levels (41–60% of 1 RM for resistance exercise and Borg RPE 12–14 for aerobic exercise) (76). Therefore, the study protocol sets the target intensity of the exergame-based exercise at Borg RPE 13 and leaves the weight intensity to Nintendo Switch itself. Although it is practical to do so in real-world settings, and it is safer for the elderly to perform PRT by squeezing or stretching the Ring-Con, one limitation is that we cannot confirm whether the weight intensity given by the Ring-Con is sufficient at moderate levels.
Given that many elderly individuals in LTCFs use a wheelchair for community ambulation because of poor muscle endurance even though they can walk for a short distance to complete gait measurements (40), the exergame-based exercise of this project focuses on training the upper extremities and trunk. By doing so, the participants could be trained in the sitting position to avoid the potential risk of falls. Therefore, most outcomes of this project, including the HGS, MVIC, sonographic thickness of the biceps and triceps brachii muscles, ROMs of the joints of the dominant upper extremity, and BBT, are measured to evaluate the training effects. A study has proven that aging can attenuate the hypertrophic response of muscle groups to RT (77). Contrary to the findings from healthy young adults, in whom neural factors account for a larger proportion of the initial strength increment and muscle hypertrophy becomes the dominant factor after the first 3–5 weeks (78), the effect of muscle training may entirely depend on the neuromuscular adaptation among older adults after an 8-week training course (79). Given the results from the classical studies by Moritani and deVries and considering that the project lasted only 3 months, we measured not only the MVIC but also the sonographic thickness to see whether some early morphological changes in the trained muscles could be detected earlier.
The primary outcomes in this protocol are the criteria to diagnose frailty and sarcopenia. Therefore, this project will measure the gait speed through the exergame-based exercise, which focuses on the upper extremities and trunk only. Walking is a complex movement that requires several functional tasks, such as ROMs, velocity, position, and trained muscles (80). The participants must balance in different positions, such as leaning forward, forward reaching, side shuffle, and lateral shifting, to use the RFA. Those movements might occur at the trunk/hips/knees, although the protocol does not allow the performance of PRT on the lower extremities. Granacher et al. demonstrated that the ability of older adults to rise from a chair, ambulate, and make turns improves after 9 weeks of core muscle strength training (81). Park et al. observed that walking speed increased after a sitting boxing program focusing on upper extremity stretching and strengthening for 6 weeks (82). Both studies have proven that strengthening programs can also induce adaptive processes, particularly in the neuromuscular system, thereby enhancing balance performance and functional mobility. Moreover, interlimb and intralimb segment coordination are important for bipedal human gait. Arm swing in the human gait cycle plays an active role in maintaining body posture. The gait speed increases when the amplitude of the arm and leg is increased (83). Given the aforementioned three main reasons, the exergame-based exercise in this study might increase gait speed.
By presenting with heterogeneity, one recent systematic review with the recruitment of 15 eligible RCTs found that exercise not only has a positive effect on physical outcomes but also improves QoL and ADLs in elderly individuals (84). Therefore, in addition to measuring the clinical effects of the exergame-based exercise on parameters of muscle and functional performance, this protocol also includes the QoL and ADL as secondary outcomes. The SF-36 is used to indicate the HRQoL because it is a validated self-assessment generic health survey with a reliable intraclass correlation coefficient (70). KC-T will be used to indicate the ADL since its usability in practice in real-world settings in Taiwan has been proven (68), and it is widely used in LTCFs. Moreover, both the SF-36 and Kihon checklist have Taiwanese versions, which are important when measuring the QoL and ADL because the values toward QoL and ADL vary from culture to culture.
No cutoff value of available cognitive measurements allows us to screen who is suitable for exergames. Most studies on exergames in the elderly recruited participants with sufficient cognition levels to understand the orders and procedures required in the game (36). Many older adults in LTCFs have some cognitive deficits, though the degree varies in Taiwan (68). Exergames have therapeutic effects on cognition among older adults (34, 36). Although the manner of play varies among exergames, there are some commonly shared concepts. Exergame environments provide an extra spatial feature. Players confront challenging tasks with visual and auditory stimuli, cues, and feedback. Immersion into a virtual environment also redirects the player’s experiences to improve attention restoration, reduce stress, and promote cognitive rehabilitation. Furthermore, exergames require players to make decisions during the game. Exergames delivered via RFA provide all aforementioned features, and we expect that the cognitive level of the elderly in LTCFs improves after the training.
Supervised exercise is safe for frail older adults (85). Only one well-trained assistant will be required to supervise the entire exergame-based exercise procedure in this project. Many participants can play the game simultaneously if the number of Nintendo Switch and RFA is sufficient, which is time- and manpower-consuming. However, this study protocol has some limitations. First, this study used the convenience sampling method because recruiting older adults who regularly participate in LTCFs publicly is difficult and impractical. This project might be less representative, even though the minimum estimated sample size can be met. The results of this study should be applied with caution and could only be generalizable to similar populations. Second, the exergame-based exercise and outcome measures only lasted 3 months. This duration might be insufficient to observe an increase in the muscle mass of older patients. However, given that an intervention period of more than 3 months might lead to a higher attrition rate of the participants, particularly for those in LTCFs with several comorbidities, we will also measure muscle morphology using sonography to detect any earlier change in muscle parameters, and we still suggest a 3-month protocol. Third, to our knowledge, this project is the first study to evaluate the effectiveness of using RFA among elderly individuals living in LTCFs. No established protocol for training with RFA could be followed. Although the entire exercise prescription is based on the guidelines for older adults by the ACSM, we cannot ensure that the protocol for the current exergame-based exercise is ideal. Fourth, individualized setting and progression of the exercises automatically are the features of using RFA to train elderly individuals. However, this project can only measure the exercise intensity by RPE. The investigators cannot confirm the exact resistance provided by the Ring-Con during each training session.
If the findings of this study show that the exergame-based exercise via RFA could improve the parameters of muscle and functional performance, the training method should be implemented as a treatment option for all older individuals living in LTCFs, particularly for those in rural regions with lesser healthcare resources. A successful exergame-based exercise would provide benefits beyond muscle strength, muscle mass, and ADLs of the elderly because it would also enhance the HRQoL or even help the elderly age gracefully. We expect that the protocol will be useful and practical to implement in real-world settings. With the positive results of this protocol, further larger studies could be conducted to examine whether the exergame-based exercise via RFA could be a treatment alternative to time- and manpower-consuming therapies currently applied in LTCFs.
Written informed consent was obtained from the individual for the publication of any potentially identifiable images or data included in this article.
S-HT and Y-JT planned the project and developed the research design. S-HT and S-FS calculated the sample size. L-HC and K-LL were responsible for literature reviewing and evaluating the appropriate measurement tools. S-HT wrote the first draft. Y-JT, L-HC, and S-FS were responsible for the revisions of the manuscript. All authors read and approved the final manuscript version.
This study was funded by the Research and Development Grant of Ministry of Health and Welfare, Taiwan (ROC, grant number: MOHW-11150) and the Research and Development Grant of Ci-Shan Hospital (grant number: CHIS-111001). The funders had and will not have a role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
ASWG, Asian Working Group for Sarcopenia; ALDs, activities of daily living; RT, resistance training; PRT, progressive resistance training; RM, repetition maximum; LTC, long-term care; LTCFs, long-term care facilities; HRQoL, health-related quality of life; HGS, handgrip strength; ASMMI, appendicular skeletal muscle mass index; RFA, Nintendo Switch® RingFit Adventure; RCT, randomized controlled trial; Exergame-based exercise, exergame-based multicomponent exercise training via RFA; RPE, rate of perceived exertion; SOF index, Study of Osteoporotic Fractures Index; BIA, bioelectrical impedance analysis; MCID, minimal clinically important difference; BBT, Box and Block Test; MVIC, maximal voluntary isometric contraction; ROM, range of motion; KC-T, Kihon checklist-Taiwan; SF-36, Medical Outcomes Study 36-Item Short-Form Health Survey; BHT-Cog, Brain Health Test–brief cognitive test; AR, augmented reality.
1. Ministry of Health and Family Welfare. Ageing and Long-Term Care Statistics. New Delhi: Ministry of Health and Family Welfare (2021).
2. Evans W. Skeletal muscle loss: cachexia, sarcopenia, and inactivity. Am J Clin Nutr. (2010) 91:1123S–7S. doi: 10.3945/ajcn.2010.28608A
3. Seene T, Kaasik P, Riso E. Review on aging, unloading and reloading: changes in skeletal muscle quantity and quality. Arch Gerontol Geriatr. (2012) 54:374–80. doi: 10.1016/j.archger.2011.05.002
4. Marzetti E, Leeuwenburgh C. Skeletal muscle apoptosis, sarcopenia and frailty at old age. Exp Gerontol. (2006) 41:1234–8. doi: 10.1016/j.exger.2006.08.011
5. Cruz-Jentoft A, Baeyens J, Bauer J, Boirie Y, Cederholm T, Landi F, et al. Sarcopenia: European consensus on definition and diagnosis: report of the European Working Group on Sarcopenia in Older People. Age Ageing. (2010) 39:412–23. doi: 10.1093/ageing/afq034
6. Kuo Y, Wang T, Liu L, Lee W, Peng L, Chen L. Epidemiology of sarcopenia and factors associated with it among community-dwelling older adults in Taiwan. Am J Med Sci. (2019) 357:124–33. doi: 10.1016/j.amjms.2018.11.008
7. Cesari M, Vellas B, Hsu F, Newman A, Doss H, King A, et al. A physical activity intervention to treat the frailty syndrome in older persons—results from the LIFE-P study. J Gerontol A Biol Sci Med Sci. (2015) 70:216–22. doi: 10.1093/gerona/glu099
8. Thomas E, Battaglia G, Patti A, Brusa J, Leonardi V, Palma A, et al. Physical activity programs for balance and fall prevention in elderly: a systematic review. Medicine. (2019) 98:e16218.
9. Cruz-Jentoft A, Bahat G, Bauer J, Boirie Y, Bruyère O, Cederholm T, et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. (2019) 48:16–31.
10. Liu C, Latham N. Progressive resistance strength training for improving physical function in older adults. Cochrane Database Syst Rev. (2009) 2009:Cd002759.
11. Shiota A, Nakayama N, Saito Y, Maeda T, Maeda Y, Nakayama K. Prevalence and associated factors of malnutrition and sarcopenia in a daycare facility: a cross-sectional study. Healthcare. (2020) 8:576. doi: 10.3390/healthcare8040576
12. Chang C, Yeh Y, Chang H, Yi-Ju Tsai S, Wang J. Prevalence and risk factors of sarcopenia among older adults aged = 65 years admitted to daycare centers of Taiwan: using AWGS 2019 guidelines. Int J Environ Res Public Health. (2021) 18:8299. doi: 10.3390/ijerph18168299
13. Lo Y, Wahlqvist M, Huang Y, Chuang S, Wang C, Lee M. Medical costs of a low skeletal muscle mass are modulated by dietary diversity and physical activity in community-dwelling older Taiwanese: A longitudinal study. Int J Behav Nutr Phys Act. (2017) 14:31. doi: 10.1186/s12966-017-0487-x
14. Negm A, Lee J, Hamidian R, Jones C, Khadaroo R. Management of sarcopenia: a network meta-analysis of randomized controlled trials. J Am Med Dir Assoc. (2022) 23:707–14. doi: 10.1016/j.jamda.2022.01.057
15. Daly M, Vidt M, Eggebeen J, Simpson W, Miller M, Marsh A, et al. Upper extremity muscle volumes and functional strength after resistance training in older adults. J Aging Phys Act. (2013) 21:186–207. doi: 10.1123/japa.21.2.186
16. Papa E, Dong X, Hassan M. Resistance training for activity limitations in older adults with skeletal muscle function deficits: a systematic review. Clin Interv Aging. (2017) 12:955–61. doi: 10.2147/cia.S104674
17. Beckwée D, Delaere A, Aelbrecht S, Baert V, Beaudart C, Bruyere O, et al. Exercise interventions for the prevention and treatment of sarcopenia. a systematic umbrella review. J Nutr Health Aging. (2019) 23:494–502. doi: 10.1007/s12603-019-1196-8
18. Zhang Y, Zou L, Chen S, Bae J, Kim D, Liu X, et al. Effects and moderators of exercise on sarcopenic components in sarcopenic elderly: a systematic review and meta-analysis. Front Med. (2021) 8:649748. doi: 10.3389/fmed.2021.649748
19. Martins W, de Oliveira R, Carvalho R, de Oliveira Damasceno V, da Silva V, Silva M. Elastic resistance training to increase muscle strength in elderly: a systematic review with meta-analysis. Arch Gerontol Geriatr. (2013) 57:8–15. doi: 10.1016/j.archger.2013.03.002
20. Csapo R, Alegre L. Effects of resistance training with moderate vs heavy loads on muscle mass and strength in the elderly: a meta-analysis. Scand J Med Sci Sports. (2016) 26:995–1006. doi: 10.1111/sms.12536
21. Hsu H, Chen CF. LTC 2.0: the 2017 reform of home- and community-based long-term care in Taiwan. Health Policy. (2019) 123:912–6. doi: 10.1016/j.healthpol.2019.08.004
22. Liang C, Change Q, Hung Y, Chen C, Lin C, Wei Y, et al. Effects of a community care station program with structured exercise intervention on physical performance and balance in community-dwelling older adults: a prospective 2-year observational study. J Aging Phys Activity. (2017) 25:596–603. doi: 10.1123/japa.2015-0326
23. Chen L, Woo J, Assantachai P, Auyeung T, Chou M, Iijima K, et al. Asian Working Group for Sarcopenia: 2019 consensus update on sarcopenia diagnosis and treatment. J Am Med Dir Assoc. (2020) 21:300–(307.e2). doi: 10.1016/j.jamda.2019.12.012
24. Lin Y, Huang C. Aging in Taiwan: building a society for active aging and aging in place. Gerontologist. (2015) 56:176–83. doi: 10.1093/geront/gnv107
25. Yu T, Chung K, Wei C, Chien K, Hou Y. Do the preferences of healthcare provider selection vary among rural and urban patients with different income and cause different outcome? PLoS One. (2016) 11:e0152776. doi: 10.1371/journal.pone.0152776
26. Winstein C, Wolf S, Dromerick A, Lane C, Nelsen M, Lewthwaite R. Effect of a task-oriented rehabilitation program on upper extremity recovery following motor stroke: the ICARE randomized clinical trial. JAMA. (2016) 315:571–81. doi: 10.1001/jama.2016.0276
27. Benjamin K, Edwards N, Guitard P, Murray M, Caswell W, Perrier M. Factors that influence physical activity in long-term care: perspectives of residents, staff, and significant others. Can J Aging. (2011) 30:247–58. doi: 10.1017/S0714980811000080
28. Chen K, Li C, Huang H, Cheng Y. Feasible modalities and long-term effects of elastic band exercises in nursing home older adults in wheelchairs: a cluster randomized controlled trial. Int J Nurs Stud. (2016) 55:4–14. doi: 10.1016/j.ijnurstu.2015.11.004
29. Meekes W, Stanmore E. Motivational determinants of exergame participation for older people in assisted living facilities: mixed-methods study. J Med Internet Res. (2017) 19:e6841. doi: 10.2196/jmir.6841
30. Adcock M, Thalmann M, Schättin A, Gennaro F, De Bruin E. A pilot study of an in-home multicomponent exergame training for older adults: feasibility, usability and pre-post evaluation. Front Aging Neurosci. (2019) 11:304. doi: 10.3389/fnagi.2019.00304
31. Jahouh M, González-Bernal J, González-Santos J, Fernández-Lázaro D, Soto-Cámara R, Mielgo-Ayuso J. Impact of an intervention with Wii video games on the autonomy of activities of daily living and psychological–cognitive components in the institutionalized elderly. Int J Environ Res Public Health. (2021) 18:1570. doi: 10.3390/ijerph18041570
32. Ismail N, Hashim H, Ahmad Yusof H. Physical activity and exergames among older adults: a scoping review. Games Health J. (2022) 11:1–17. doi: 10.1089/g4h.2021.0104
33. Willaert J, De Vries A, Tavernier J, Van Dieen J, Jonkers I, Verschueren S. Does a novel exergame challenge balance and activate muscles more than existing off-the-shelf exergames? J Neuroeng Rehabil. (2020) 17:6. doi: 10.1186/s12984-019-0628-3
34. Liao Y, Chen I, Lin Y, Chen Y, Hsu W. Effects of virtual reality-based physical and cognitive training on executive function and dual-task gait performance in older adults with mild cognitive impairment: a randomized control trial. Front Aging Neurosci. (2019) 11:162. doi: 10.3389/fnagi.2019.00162
35. Afridi A, Rathore F, Nazir S. Wii fit for balance training in elderly: a systematic review. J Coll Physicians Surg Pak. (2021) 30:559–66. doi: 10.29271/jp.2021.05.559
36. Yen H, Chiu H. Virtual reality exergames for improving older adults’ cognition and depression: a systematic review and meta-analysis of randomized control trials. J Am Med Dir Assoc. (2021) 22:995–1002. doi: 10.1016/j.jamda.2021.03.009
37. Gunst M, De Meyere I, Willems H, Schoenmakers B. Effect of exergaming on wellbeing of residents in a nursing home: a single blinded intervention study. Aging Clin Exp Res. (2022) 34:151–7. doi: 10.1007/s40520-021-01903-1
38. Chao Y, Scherer Y, Montgomery C, Lucke K, Wu Y. Exergames-based intervention for assisted living residents: a pilot study. J Gerontol Nurs. (2014) 40:36–43. doi: 10.3928/00989134-20140407-04
39. Chu C, Biss R, Cooper L, Quan A, Matulis H. Exergaming platform for older adults residing in long-term care homes: user-centered design, development, and usability study. JMIR Serious Games. (2021) 9:e22370. doi: 10.2196/22370
40. Chen G, Lin C, Huang H, Wu Y, Su H, Sun S, et al. Using virtual reality-based rehabilitation in sarcopenic older adults in rural health care facilities-a quasi-experimental study. J Aging Phys Activity. (2021) 29:866–77. doi: 10.1123/japa.2020-0222
41. Chan A, Tetzlaff J, Gøtzsche P, Altman D, Mann H, Berlin J, et al. SPIRIT 2013 explanation and elaboration: guidance for protocols of clinical trials. BMJ. (2013) 346:e7586. doi: 10.1136/bmj.e7586
42. Schulz K, Altman D, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. BMJ. (2010) 340:c332. doi: 10.1136/bmj.c332
43. Garber C, Blissmer B, Deschenes M, Franklin B, Lamonte M, Lee I, et al. American College of Sports Medicine position stand. quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. (2011) 43:1334–59. doi: 10.1249/MSS.0b013e318213fefb
44. Koivisto J, Hamari J. The rise of motivational information systems: a review of gamification research. Int J Inf Manage. (2019) 45:191–210. doi: 10.1016/j.ijinfomgt.2018.10.013
45. Lu C, Hassan L, Buruk O, Nummenmaa T, Peltonen J. “Switch” Up Your Exercise: An Empirical Analysis of Online User Discussion of the Ring Fit Adventure Exergame. Proceedings of the 5th International GamiFIN Conference. Liverpool (2021).
46. Comeras-Chueca C, Villalba-Heredia L, Pérez-Llera M, Lozano-Berges G, Marín-Puyalto J, Vicente-Rodríguez G, et al. Assessment of active video games’ energy expenditure in children with overweight and obesity and differences by gender. Int J Environ Res Public Health. (2020) 17:6714. doi: 10.3390/ijerph17186714
47. Sato T, Shimizu K, Shiko Y, Kawasaki Y, Orita S, Inage K, et al. Effects of nintendo ring fit adventure exergame on pain and psychological factors in patients with chronic low back pain. Games Health J. (2021) 10:158–64. doi: 10.1089/g4h.2020.0180
49. Heymsfield S, Adamek M, Gonzalez M, Jia G, Thomas D. Assessing skeletal muscle mass: Historical overview and state of the art. J Cachexia Sarcopenia Muscle. (2014) 5:9–18. doi: 10.1007/s13539-014-0130-5
50. Buckinx F, Reginster J, Dardenne N, Croisiser J, Kaux J, Beaudart C, et al. Concordance between muscle mass assessed by bioelectrical impedance analysis and by dual energy X-ray absorptiometry: a cross-sectional study. BMC Musculoskeletal Disord. (2015) 16:60. doi: 10.1186/s12891-015-0510-9
51. Choi H, Ko C, Chang Y, Kim G, Choi K, Kim C. Development and validation of bioimpedance prediction equations for fat-free mass in unilateral male amputees. PeerJ. (2021) 9:e10970. doi: 10.7717/peerj.10970
52. Chen L, Liu L, Woo J, Assantachai P, Auyeung T, Bahyah K, et al. Sarcopenia in Asia: consensus report of the Asian working group for sarcopenia. J Am Med Dir Assoc. (2014) 15:95–101. doi: 10.1016/j.jamda.2013.11.025
53. Vermeulen J, Neyens J, Spreeuwenberg M, van Rossum E, Hewson D, de Witte L. Measuring grip strength in older adults: comparing the grip-ball with the Jamar dynamometer. J Geriatr Phys Ther. (2015) 38:148–53. doi: 10.1519/jpt.0000000000000034
54. Trampisch U, Franke J, Jedamzik N, Hinrichs T, Platen P. Optimal jamar dynamometer handle position to assess maximal isometric hand grip strength in epidemiological studies. J Hand Surg. (2012) 37:2368–73. doi: 10.1016/j.jhsa.2012.08.014
55. Bobos P, Nazari G, Lu Z, MacDermid J. Measurement properties of the hand grip strength assessment: A systematic review with meta-analysis. Arch Phys Med Rehabil. (2020) 101:553–65. doi: 10.1016/j.apmr.2019.10.183
56. Bohannon R, Glenney S. Minimal clinically important difference for change in comfortable gait speed of adults with pathology: a systematic review. J Eval Clin Pract. (2014) 20:295–300. doi: 10.1111/jep.12158
57. Ensrud K, Ewing S, Cawthon P, Fink H, Taylor B, Cauley J, et al. A comparison of frailty indexes for the prediction of falls, disability, fractures, and mortality in older men. J Am Geriatr Soc. (2009) 57:492–8. doi: 10.1111/j.1532-5415.2009.02137.x
58. Hu B, Hsiao-Wei Y, Chiu T, Li-Ling L, Chen Y. The validity of the study of osteoporotic fractures (sof) index for assessing community-based older adults in Taiwan. Innov Aging. (2018) 2(Suppl 1):1015–1015. doi: 10.1093/geroni/igy031.3746
59. Desrosiers J, Bravo G, Hebert R, Dutil E, Mercier L. Validation of the box and block test as a measure of dexterity of elderly people: reliability, validity, and norms studies. Arch Phys Med Rehabil. (1994) 75:751–5. doi: 10.1016/0003-9993(94)90130-9
60. Chen H, Chen C, Hsueh I, Huang S, Hsieh C. Test-retest reproducibility and smallest real difference of 5 hand function tests in patients with stroke. Neurorehabil Neural Repair. (2009) 23:435–40. doi: 10.1177/1545968308331146
61. Buckinx F, Croisier J, Reginster J, Dardenne N, Beaudart C, Slomian J, et al. Reliability of muscle strength measures obtained with a hand-held dynamometer in an elderly population. Clin Physiol Funct Imaging. (2017) 37:332–40. doi: 10.1111/cpf.12300
62. Stark T, Walker B, Phillips J, Fejer R, Beck R. Hand-held dynamometry correlation with the gold standard isokinetic dynamometry: a systematic review. PM R. (2011) 3:472–9. doi: 10.1016/j.pmrj.2010.10.025
63. Sanz-Paris A, González-Fernandez M, Hueso-Del Río L, Ferrer-Lahuerta E, Monge-Vazquez A, Losfablos-Callau F, et al. Muscle thickness and echogenicity measured by ultrasound could detect local sarcopenia and malnutrition in older patients hospitalized for hip fracture. Nutrients. (2021) 13:2401. doi: 10.3390/nu13072401
64. De Toni L, Petre G, Garolla A, De Santis I, Valente U, Foresta C, et al. Prognostic value of ultrasound stratigraphy in long-term weight loss: results from a nutritional counseling program. Obesity Facts. (2019) 12:606–17. doi: 10.1159/000502119
65. Norkin C, White D. Measurement of Joint Motion: A Guide to Goniometry. Philadelphia, PA: F.A. Davis (2009).
66. Satake S, Senda K, Hong Y, Miura H, Endo H, Sakurai T, et al. Validity of the kihon checklist for assessing frailty status. Geriatr Gerontol Int. (2016) 16:709–15. doi: 10.1111/ggi.12543
67. Tsay S, Chen S, Lu S, Liu L. [The policy and practice of preventive care for the elderly]. Hu Li Za Zhi. (2018) 65:13–9. doi: 10.6224/jn.201804_65(2)0.03
68. Mao H, Tsai A, Chang L, Tsai I. Multi-component cognitive intervention for older adults with mixed cognitive levels: implementation and preliminary effectiveness in real-world settings. BMC Geriatrics. (2021) 21:543. doi: 10.1186/s12877-021-02489-z
69. Chang C, Huang C, Chang Y, Tai C, Lin J, Wang J. Cross-validation of the Taiwan version of the moorehead-ardelt quality of life questionnaire II with WHOQOL and SF-36. Obesity Surg. (2010) 20:1568–74. doi: 10.1007/s11695-009-9813-y
70. Tseng H, Lu J, Gandek B. Cultural issues in using the SF-36 Health Survey in Asia: results from Taiwan. Health Qual Life Outcomes. (2003) 1:72. doi: 10.1186/1477-7525-1-72
71. Tsai P, Liu J, Lin K, Chang C, Pai M, Wang W, et al. Development and validation of a dementia screening tool for primary care in Taiwan: brain health test. PLoS One. (2018) 13:e0196214. doi: 10.1371/journal.pone.0196214
72. Jeon S, Kim J. Effects of augmented-reality-based exercise on muscle parameters, physical performance, and exercise self-efficacy for older adults. Int J Environ Res Public Health. (2020) 17:3260. doi: 10.3390/ijerph17093260
73. Faul F, Erdfelder E, Lang A, Buchner A. G* Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. (2007) 39:175–91.
74. Michel J, Leonardi M, Martin M, Prina M. WHO’s report for the decade of healthy ageing 2021–30 sets the stage for globally comparable data on healthy ageing. Lancet Healthy Longevity. (2021) 2:e121–2. doi: 10.1016/S2666-7568(21)00002-7
75. Bårdstu H, Andersen V, Fimland M, Aasdahl L, Raastad T, Cumming K, et al. Effectiveness of a resistance training program on physical function, muscle strength, and body composition in community-dwelling older adults receiving home care: a cluster-randomized controlled trial. Eur Rev Aging Phys Act. (2020) 17:11. doi: 10.1186/s11556-020-00243-9
76. McDermott A, Mernitz H. Exercise and older patients: prescribing guidelines. Am Family Phys. (2006) 74:437–44.
77. Brook M, Wilkinson D, Phillips B, Perez-Schindler J, Philp A, Smith K, et al. Skeletal muscle homeostasis and plasticity in youth and ageing: impact of nutrition and exercise. Acta Physiol. (2016) 216:15–41. doi: 10.1111/apha.12532
78. Moritani T, deVries H. Neural factors versus hypertrophy in the time course of muscle strength gain. Am J Phys Med. (1979) 58:115–30.
79. Moritani T, Devries H. Potential for gross muscle hypertrophy in older men. J Gerontol. (1980) 35:672–82. doi: 10.1093/geronj/35.5.672
80. Eng J. Strength Training in Individuals with Stroke. Physiother Can. (2004) 56:189–201. doi: 10.2310/6640.2004.00025
81. Granacher U, Lacroix A, Muehlbauer T, Roettger K, Gollhofer A. Effects of core instability strength training on trunk muscle strength, spinal mobility, dynamic balance and functional mobility in older adults. Gerontology. (2013) 59:105–13. doi: 10.1159/000343152
82. Park J, Gong J, Yim J. Effects of a sitting boxing program on upper limb function, balance, gait, and quality of  life in stroke patients. NeuroRehabilitation. (2017) 40:77–86. doi: 10.3233/NRE-161392
83. Bovonsunthonchai S, Hiengkaew V, Vachalathiti R, Vongsirinavarat M, Tretriluxana J. Effect of speed on the upper and contralateral lower limb coordination during gait in individuals with stroke. Kaohsiung J Med Sci. (2012) 28:667–72. doi: 10.1016/j.kjms.2012.04.036
84. Campbell E, Petermann-Rocha F, Welsh P, Celis-Morales C, Pell J, Ho F, et al. The effect of exercise on quality of life and activities of daily life in frail older adults: a systematic review of randomised control trials. Exp Gerontol. (2021) 147:111287. doi: 10.1016/j.exger.2021.111287
85. De Labra C, Guimaraes-Pinheiro C, Maseda A, Lorenzo T, Millán-Calenti J. Effects of physical exercise interventions in frail older adults: a systematic review of randomized controlled trials Physical functioning, physical health and activity. BMC Geriatrics. (2015) 15:154. doi: 10.1186/s12877-015-0155-4
Keywords: exergame, sarcopenia, frailty, long term care, multicomponent training, RingFit Adventure
Citation: Tuan S-H, Chang L-H, Sun S-F, Lin K-L and Tsai Y-J (2022) Using exergame-based exercise to prevent and postpone the loss of muscle mass, muscle strength, cognition, and functional performance among elders in rural long-term care facilities: A protocol for a randomized controlled trial. Front. Med. 9:1071409. doi: 10.3389/fmed.2022.1071409
Received: 16 October 2022; Accepted: 21 November 2022;
Published: 13 December 2022.
Edited by:
Marios Kyriazis, National Gerontology Centre, CyprusReviewed by:
Yolanda Castellote Caballero, University of Jaén, SpainCopyright © 2022 Tuan, Chang, Sun, Lin and Tsai. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yi-Ju Tsai, eWp0c2FpbmNrdUBnbWFpbC5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.