- 1Department of Hernia and Colorectal Surgery, The Second Hospital of Dalian Medical University, Dalian, China
- 2Department of Colorectal Surgery, The Hospital of Pyongyang Medical College, Pyongyang, Democratic People’s Republic of Korea
Purpose: Invasion of the pancreas and/or duodenum with/without neighboring organs by locally advanced right colon cancer (LARCC) is a very rare clinical phenomenon that is difficult to manage. The purpose of this review is to suggest the most reasonable surgical approach for primary right colon cancer invading neighboring organs such as the pancreas and/or duodenum.
Methods: An extensive systematic research was conducted in PubMed, Medline, Embase, Scopus, and the Cochrane Central Register of Controlled Trials (CENTRAL) using the MeSH terms and keywords. Data were extracted from the patients who underwent en bloc resection and local resection with right hemicolectomy (RHC), the analysis was performed with the survival rate as the outcome parameters.
Results: As a result of the analysis of 117 patient data with locally advanced colon cancer (LACC) (73 for males, 39 for females) aged 25–85 years old from 11 articles between 2008 and 2021, the survival rate of en bloc resection was 72% with invasion of the duodenum, 71.43% with invasion of the pancreas, 55.56% with simultaneous invasion of the duodenum and pancreas, and 57.9% with invasion of neighboring organs with/without invasion of duodenum and/or pancreas. These survival results were higher than with local resection of the affected organ plus RHC.
Conclusion: When the LARCC has invaded neighboring organs, particularly when duodenum or pancreas are invaded simultaneously or individually, en bloc resection is a reasonable option to increase patient survival after surgery.
Highlights
- Invasion of the pancreas and/or duodenum with/without neighboring organs by locally advanced right colon cancer (LARCC) is a very rare clinical phenomenon that is difficult to manage.
- A few studies have attempted to find the reasonable surgical approach to get high survival focusing on en bloc resection when the LARCC invaded neighboring organs.
- The en bloc resection is the gold standard surgical options for LARCC invading neighboring organs when there is no distant metastasis.
- This is important to raise awareness among clinicians and researchers to focus on en bloc resection, to improve patient survivals of LARCC with invading neighboring organs.
1. Introduction
The colorectal cancer is the third most common cancer in the world, accounting for more than a third of all cancer cases worldwide, and the mortality rate is usually high (1, 2).
In general, surgery is the first choice for colon cancer, and non-radical resection and blunt mobilization of the attached organs is associated with tumor recurrence and prognosis, particularly when the colon cancer invades neighboring organs, which is defined as “locally advanced colon cancer (LACC)” (3–6). The RCC also occasionally invades the pancreas and/or duodenum in the clinics, and this can cause troubles in the operation because these organs are attached due to an inflammatory or oncologic reaction (7–9).
When LACC invades the several neighboring organs with pancreas and/or duodenum, the first option to consider is performing the multi-organic or extended resection for the more achieving tumor negative margin of the resection (10–12).
Therefore, the en bloc resection is the gold standard surgical options for LACC invading neighboring organs when there is no distant metastasis. The goal of surgical resection of primary colon cancer is complete removal of the tumor, the major vascular pedicles, and the lymphatic drainage basin of the affected colonic segment, and the en bloc resection of contiguous structures is indicated if there is attachment or infiltration of the tumor into a potentially resectable organ or structure (13, 14).
An understanding of these issues may prove important to prolong survival, and surgical options for invading neighboring organs of RCC have been continuously explored over the past several decades (12, 15–23). Unfortunately, their outcomes have the limitations coming from the lack of study samples and designs, and despite of the perfect procedures in the operation, it is still remained unclear which operation is the best options for locally advanced RCC (LARCC) (8, 13, 17, 24–28).
The aim of this study is to provide comprehensive knowledge through the systematic review of fundamental literatures and to find a reasonable surgical approach for LARCC with invading neighboring organs.
2. Materials and methods
2.1. Research design and criteria
This systematic review was conducted in accordance with the preferred reporting items for systemic review and meta-analysis (PRISMA) statement. The electronic records provided a wealth of rich data and the large sample size required for this study, and the basic data were generated using the appropriate inclusion and exclusion criteria.
2.1.1. Inclusion criteria
The randomized controlled trials and non-randomized controlled trials of surgical treatment of LARCC with invasion of adjacent organs such as pancreas and/or duodenum were included in this study.
2.1.2. Exclusion criteria
Low quality studies (no detailed explanation pre-operation and surgical process) and studies with poor outcomes (no more than two outcome parameters) were excluded from this study.
2.1.3. Patient information
The adult patients (aged 25–85 years old) with LARCC invading neighboring organs without gender specification.
2.2. Systematic fundamental literature search
An extensive systematic search was conducted in PubMed, Medline, Embase, Scopus, and the Cochrane Central Register of Controlled Trials (CENTRAL) using the MeSH terms and keywords: (([All Fields] = (locally advanced*)) AND [All Fields] = (right*) AND [All Fields] = (colon* OR colonic*)) AND [All Fields] = (cancer* OR tumor* OR carcinoma*) AND [All Fields] = (invading* OR affecting*) AND ([All Fields] = (pancreas) OR [All Fields] = (duodenum) OR [All Fields] = (multivisceral*))) OR ((([All Fields] = (right*) AND [All Fields] = (hemicolectomy)) OR [All Fields] = (pancreatoduodenectomy)).
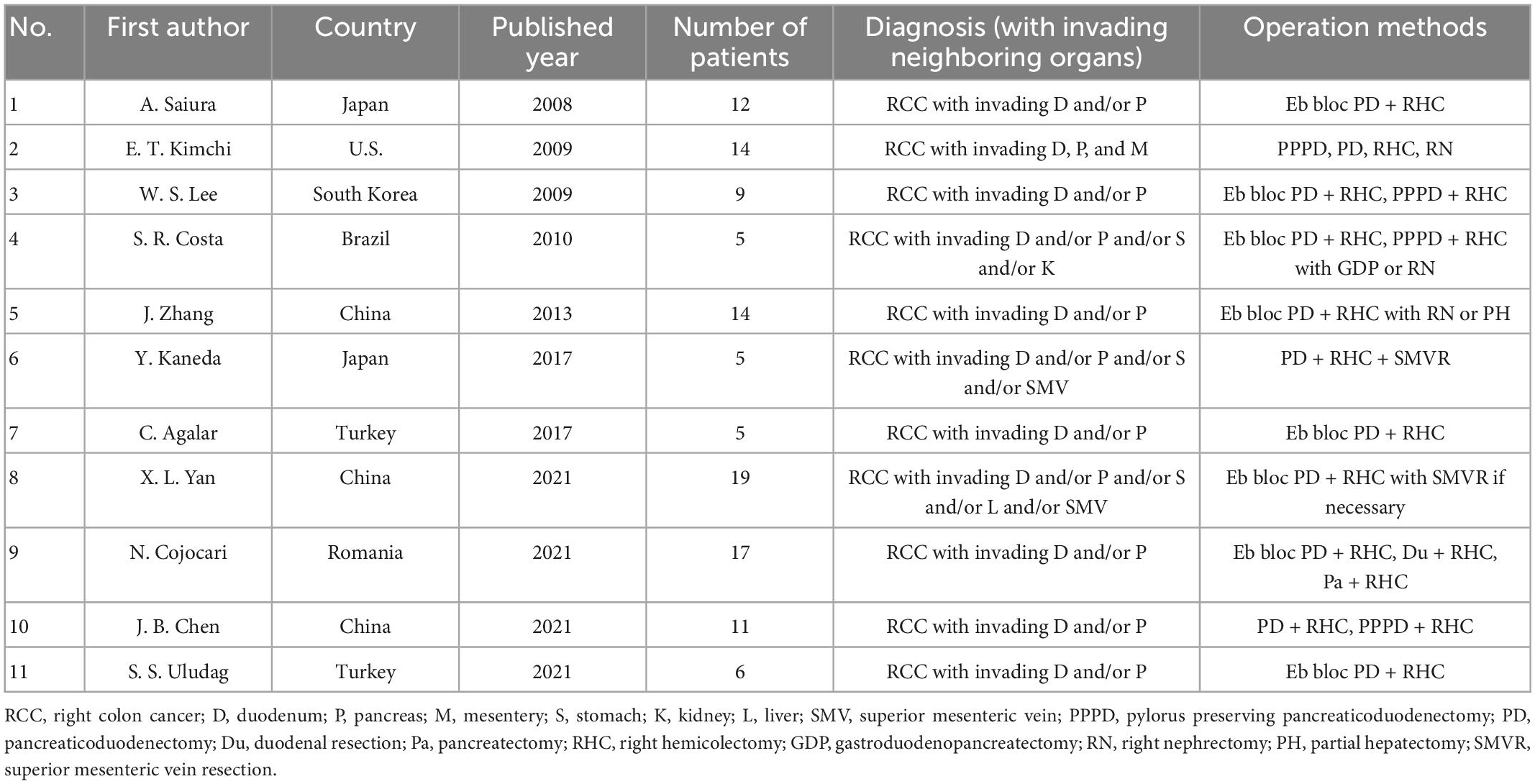
This study was conducted in April 2022 and the search process was performed manually. After collecting records, the three researchers consulted on the database and the very early pre-1950s studies and duplicates were first excluded, then the records were independently sourced according to the inclusion and exclusion criteria by researchers and finally merged into the core database (Figure 1).
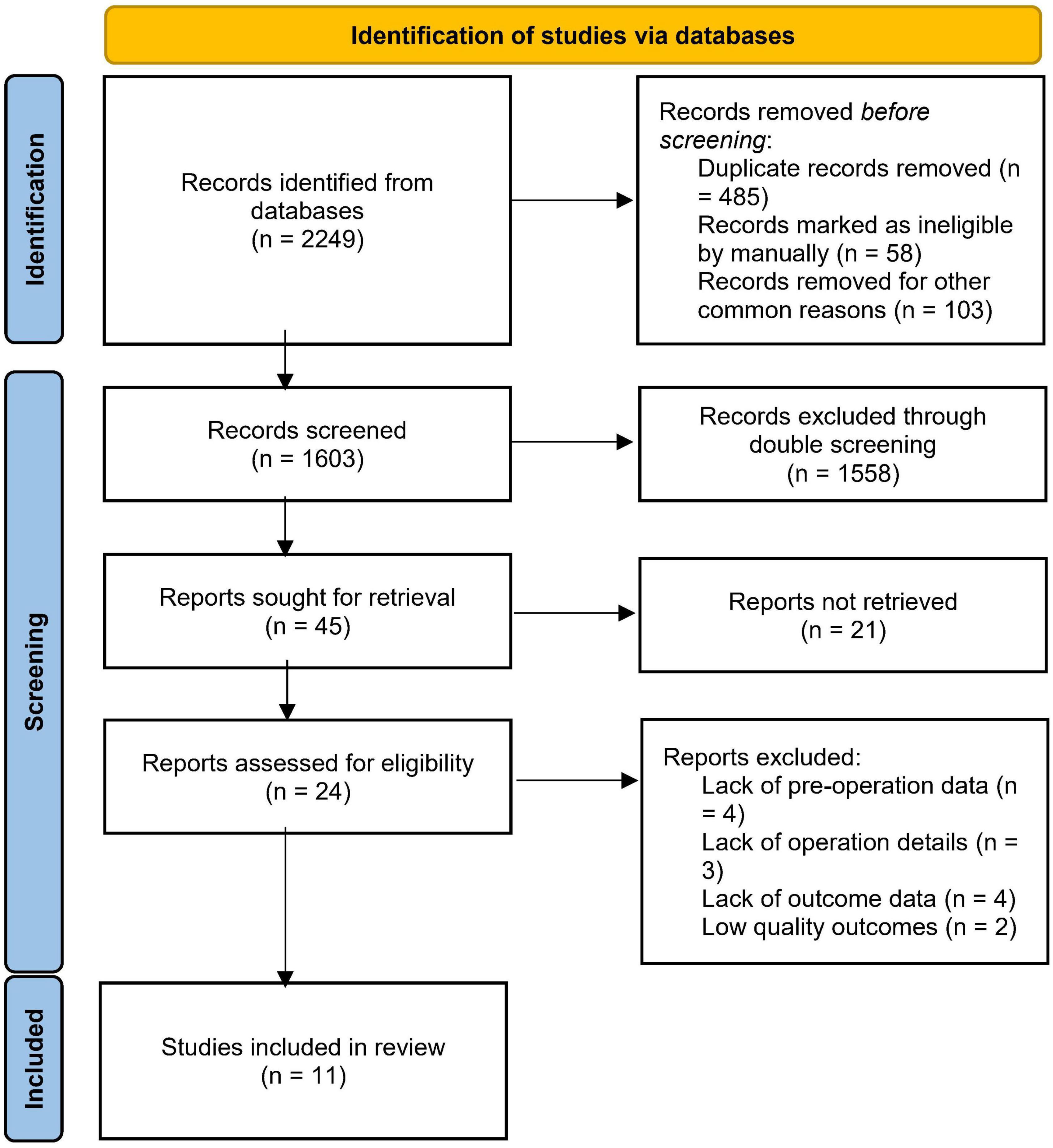
Figure 1. Preferred reporting items for systemic review and meta-analysis (PRISMA) flow chart for literature search.
2.3. Data extraction
The data was extracted based on the Cochrane Consumers and Communication Review Group’s data extraction template.
2.4. Data analysis
We divided LARCC cases into invasion of the duodenum alone, invasion of the pancreas alone, invasion of the duodenum and pancreas simultaneously, or invasion of the pancreas and/or duodenum with other adjacent organs. And the analysis was performed with the survival rate as the outcome parameter.
3. Results
3.1. The characteristics of included studies
Between 2008 and 2021, 11 studies involving 117 patients with LARCC invasion of neighboring organs were collected from the database search (Table 1). Among them, 73 patients (62.4%) were men and 39 patients (33.3%) were women, and the last 5 patients (4.3%) were unreported their gender information. All patients were ranged between 25 and 85 years old, and the primary tumors were located in the right colon, particularly in the hepatic flexion.
3.2. Comparison of classic pancreaticoduodenectomy and en bloc resection with right hemicolectomy when RCC invaded duodenum
Patient information, treatments, and outcome data are presented in Table 2. A total of 35 out of 117 patients were diagnosed RCC with invading duodenum, and two surgical methods including classic pylorus preserving pancreaticoduodenectomy (PPPD) and en bloc resection with right hemicolectomy (RHC) were performed. Of 10 patients who performed PPPD and local duodenal resection plus RHC, 5 patients died, including 2 of them with recurrences, while 5 patients are alive, of which 1 had recurrence. The survival rate was 50%. Of the 25 cases of en bloc resection, seven patients died from recurrence. The remaining 18 patients were alive and did not relapse. The survival rate was 72%.
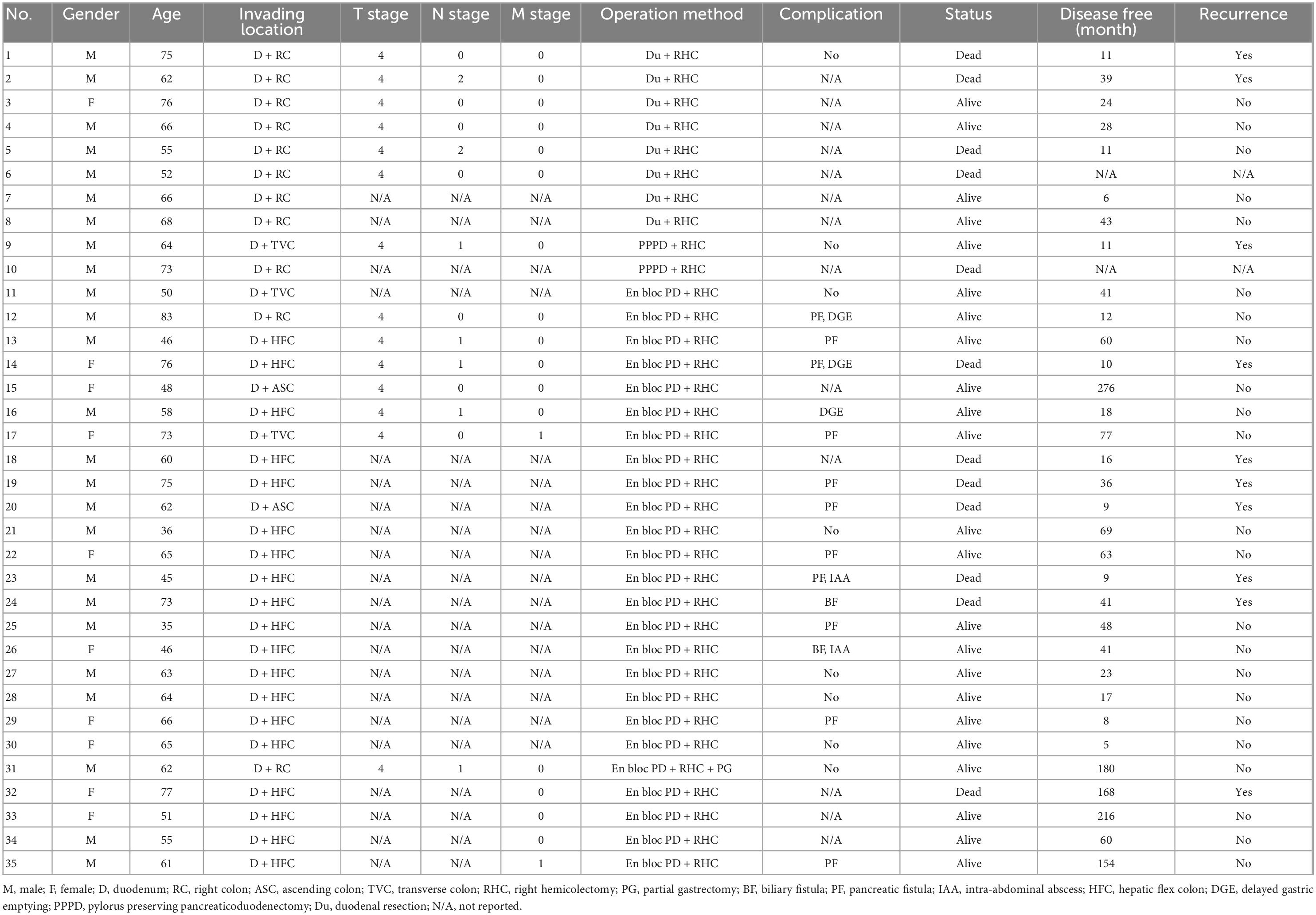
Table 2. The comparison of local pancreaticoduodenectomy and en bloc PD resection with RHC when right colon cancer (RCC) invaded duodenum.
3.3. Comparison of classic pancreaticoduodenectomy and en bloc resection with right hemicolectomy when RCC invaded pancreas
All information has been listed in Table 3. RCC with invading pancreas was diagnosed in 14 of 117 patients, and surgical approaches such as local pancreatectomy, classic PPPD, and en bloc resection with RHC were performed. Of seven patients who performed local pancreatectomy or PPPD, four patients died, including 3 of them with recurrences, while three patients were alive and none of them had recurrences. The survival rate was 42.86%. Of the seven cases that underwent en bloc resection, two patients died due to recurrence. The remaining five patients were still alive and had no relapse. The survival rate was 71.43%.
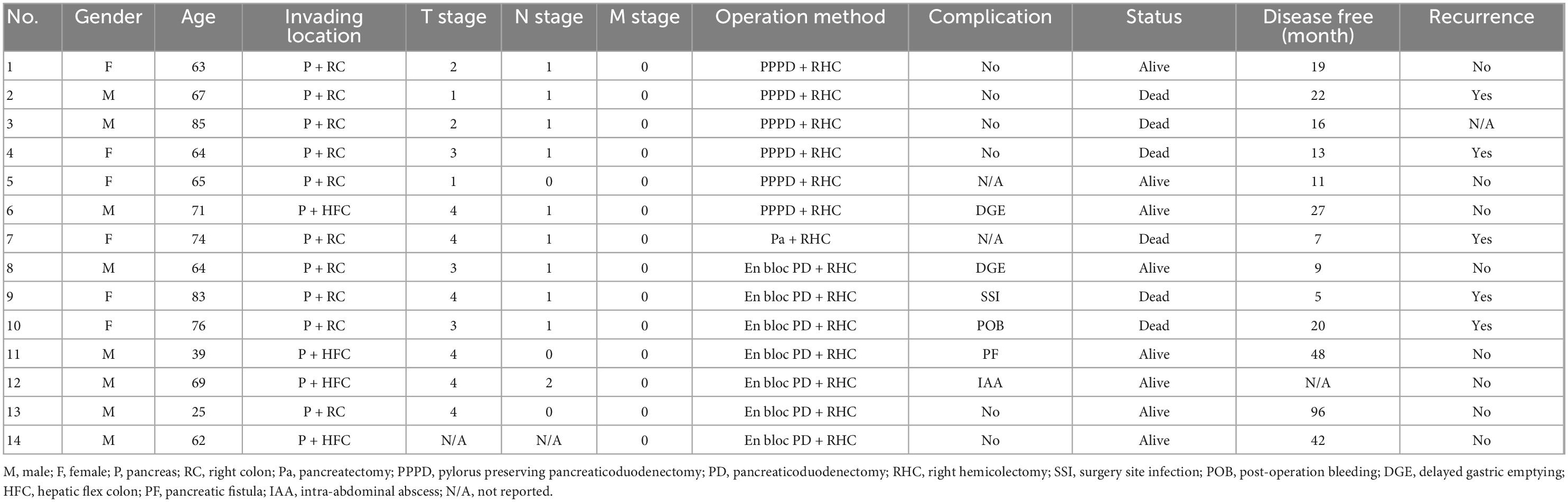
Table 3. The comparison of local pancreaticoduodenectomy and en bloc PD resection with RHC when right colon cancer (RCC) invaded pancreas.
3.4. Comparison of classic pancreaticoduodenectomy and en bloc resection with right hemicolectomy when RCC invaded duodenum and pancreas simultaneously
All patient, surgery and outcome information are presented in Table 4. Eighteen of 117 patients were diagnosed with RCC invading the duodenum and pancreas simultaneously and all underwent en bloc resection with RHC. A total of 18 patients who performed en bloc resection, 8 patients died, including 3 with recurrence and 5 without information of recurrence, and the remaining 10 patients are alive and all had no recurrences. The survival rate was 55.56%.
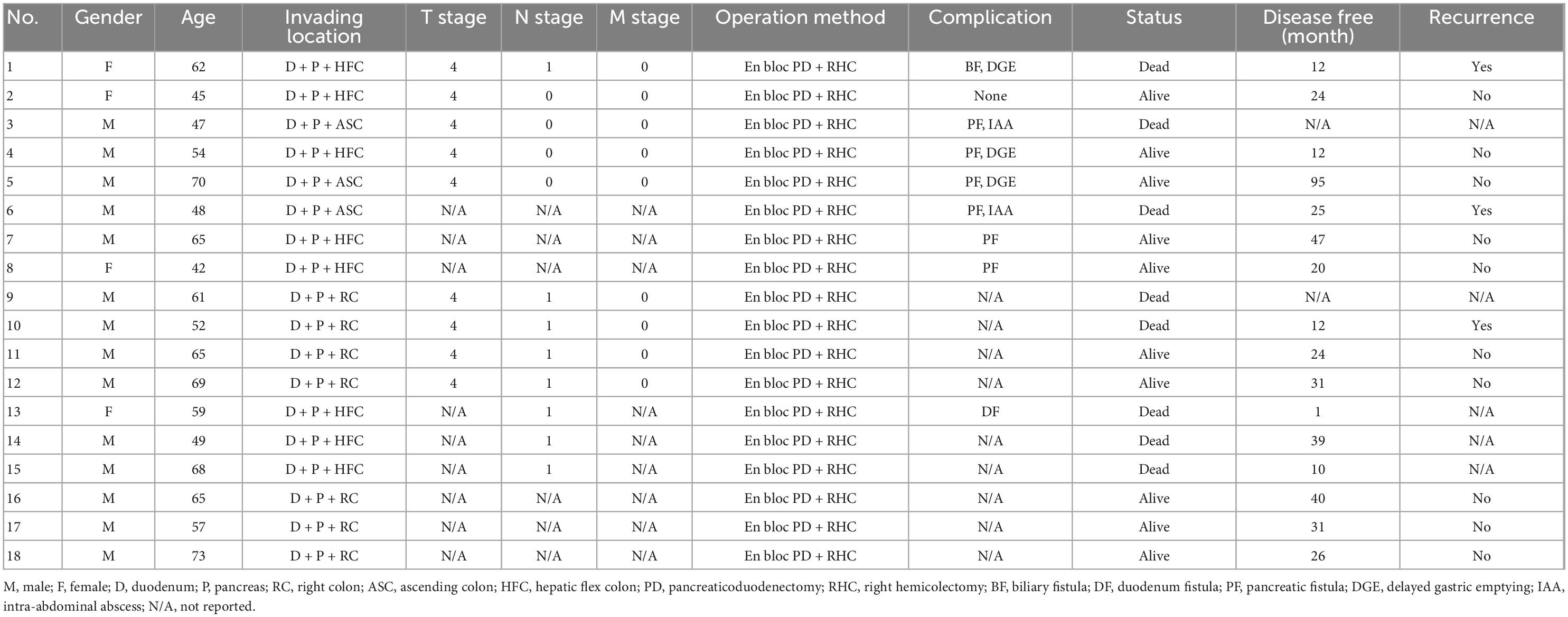
Table 4. The comparison of local pancreaticoduodenectomy and en bloc PD resection with RHC when right colon cancer (RCC) invaded pancreas and duodenum.
3.5. En bloc resection with right hemicolectomy when RCC invaded pancreas and/or duodenum with other neighboring organs
All patient, surgery and outcome information are presented in Table 5. RCC invading the pancreas and/or duodenum with other neighboring organs was diagnosed in 24 of 117 patients, and 19 of them underwent en bloc resection with RHC and 5 patients underwent PPPD with RHC. In addition, local resection of penetrating neighboring organs was performed in all cases. A total of 8 patients out of 19 patients with en bloc resection died, while two out of 5 patients with PPPD died. The survival rate of en bloc resection was is 57.9%.

Table 5. En bloc PD with RHC when right colon cancer (RCC) invaded pancreas and/or duodenum with other neighboring organs.
4. Discussion
Right colon cancer is usually treated with a RHC. This surgical treatment has solved many oncological and radical resection problems and is now widely used in clinical practice (29–31). However, if the RCC invades the duodenum and/or pancreas, or if it invades other neighboring organs simultaneously, the treatment is relatively difficult and the post-operative mortality rate is relatively high (8, 15, 28, 32–34). LACC in adjacent organs is a rare phenomenon, recently 5.2–23.6% of all colorectal cancers invade or attach to adjacent organs at this time of presentation (35). This problem had received the substantial interests of colorectal surgeons and they finally produced the significant operation procedure, the RHC with pancreatoduodenectomy which was defined as en bloc resection. This surgical method is considered to be quite difficult surgically in general, and there are relatively many complications including post-operative pancreas and/or gallbladder fistula, and post-operative patient management is relatively difficult and complex while the advantage of this en bloc resection is relatively radical and increases the survival rate of the patient after surgery (3, 15, 36).
The en bloc resection approach was first introduced in 1953 (37). At that time, the post-operative mortality and recurrence rate, and the incidence of post-operative complications were very high due to insufficient surgical equipment and inexperienced surgical technique, especially incomplete resection (38–41). With the development of numerous medical facilities, from laparotomy through laparoscopy to robotic surgery, and the rapid developing of medical science and technology have broken the difficulty of the en bloc resection, greatly increased the possibility of surgery, and lowered the incidence of post-operative complications (42–50). Currently, when RCC has invaded the duodenum and/or pancreas, this en bloc resection is the most reasonable surgical treatment option and several studies reported the long-term outcomes of this procedure (51–57).
In Saiura et al. (19) reported that pancreaticoduodenectomy for the advanced RCC invading the duodenum and/or pancreas was beneficial with a 5-year survival rate of 55%. In Costa et al. (58) reported that pancreatoduodenectomy plus RHC for LARCC could provide the long-term survival rates, while there were sample size limitations in five T4 patients. In Cojocari et al. (20) reported that four patients underwent RHC with duodenectomy and they had no recurrence at 11–39 months, and this surgical method could be a good choice for right-sided colon cancer invading neighboring organs.
In Curley et al. (51) reported the resection for cure of carcinoma of the colon directly invading the duodenum or pancreatic head, and the survival rate with en bloc resection is relatively high than local resection, especially in invading pancreatic head cases. They concluded long-term survival could be achieved by en bloc resection in patients with locally advanced carcinoma of the colon involving the duodenum or pancreatic head. In Sasson et al. (42) reported the en bloc resection for locally advanced pancreatic cancer. In their study, 13 of 116 patients required partial colectomy to completely remove the lesion because extensive involvement of the mesentery of the transverse and right colon resulted in significant shortening of the mesentery. However, they could not find any differences in outcomes for patients with locally advanced cancer requiring en bloc resection compared to patients with standard pancreatectomy, and only suggested that en bloc resection involving surrounding structures to completely remove all macroscopic disease in selected patients with locally advanced disease might be beneficial, particularly when combined with pre-operative chemoradiotherapy. The results like these can be found in papers published by other research groups (59–64).
In our study, the survival rate with en bloc resection was relatively higher than with RHC plus local duodenectomy, RHC plus local pancreatectomy, and RHC plus PPPD. This result was consistent with previous reports in several studies and it was because this operation could achieve the tumor clearance in patients with an adherent but not penetrating right colon carcinoma when RCC invades duodenum or pancreas alone or simultaneously (16, 18, 23, 65–67).
As we have already discussed, RCC is more advanced and the most commonly affected organs are the duodenum and pancreas. In some cases, however, abdominal organs such as the stomach, liver, gallbladder, and kidneys, etc., are affected singly or in combination, and there are also cases of invasion of the peritoneum and/or mesentery (68–71). In these cases, the partial excision of the affected organ and the RHC are performed simultaneously (16, 20, 23, 72). Unfortunately, in these cases there are many post-operative complications with a high rate of recurrence and a low survival rate. In combination with metastatic comorbidities, the prognosis is not so good (73, 74).
We also summarized that en bloc resection with RHC when RCC invaded pancreas and/or duodenum with other neighboring organs, and the survival rate was is 57.9%. This result still tells us that the mortality in these cases is relatively high and that the advanced study is needed to increase the patient’s survival.
This research has some shortcomings. It is a method of collecting English-only documents within the scope of collecting data, which does not guarantee the wide range of the research scope. It is revealed that en bloc resection is a very beneficial option only in terms of the surgical method without revealing the factors that have a great influence on the survival rate of post-operative patients, such as post-operative chemotherapy and lymph node-negative status, which were announced in some studies. In addition, the time interval in this study is relatively long, from 2008 to 2021. This may lead to a possible bias in the results of the study, but in practice, LARCC invading neighboring organs is very rare and there is insufficient data to avoid this bias by shortening the time interval. In this regard, we hope that readers will read the study results with caution. In the future, we plan to further supplement and deepen the related contents in future research.
5. Conclusion
This systematic review concludes that when LARCC has invaded neighboring organs, en bloc resection is a reasonable option to prolong patient survival after surgery.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
HR, XC, and HK: conceptualization. ZX, ZG, HJ, and BA: investigation. YX, YR, and WZ: data curation. HR, HK, and XC: writing—original draft preparation. ZX, ZG, HJ, YX, YR, and WZ: writing—review and editing. HR, XC, and BA: supervision and project administration. All authors have read and agreed to the submitted version of the manuscript.
Funding
This work was supported by the “1+X” program for the Clinical Competency Enhancement-Interdisciplinary Innovation Project, The Second Hospital of Dalian Medical University (2022JCXKYB01 and 2022JCXKYB20) and Dalian Medical Science Research Project (2012023 and 1912036).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Jiang X, Jiang Z, Jiang M, Sun Y. Berberine as a potential agent for the treatment of colorectal cancer. Front Med. (2022) 9:886996–886996. doi: 10.3389/fmed.2022.886996
2. Huynh C, Minkova S, Kim D, Stuart H, Hamilton T, et al. Current treatment strategies and patterns of recurrence in locally advanced colon cancer. J Clin Oncol. (2019) 37(suppl. 15):e15171–e15171. doi: 10.1200/JCO.2019.37.15_suppl.e15171
3. Ascierto PA, Marincola FM, Fox BA, Galon J. No time to die: the consensus immunoscore for predicting survival and response to chemotherapy of locally advanced colon cancer patients in a multicenter international study. Oncoimmunology. (2020) 9. 1826132 doi: 10.1080/2162402X.2020.1826132
4. Moutardier V, Turrini O, Lelong B, Hardwigsen J, Houvenaeghel G, Treut YPL, et al. Consecutive multiple organ resections for locally advanced colon cancer. Chirurgia Italy. (2020) 33:160–3. doi: 10.23736/S0394-9508.19.04981-7
5. Taylor WE, Donohue JH, Gunderson LL, Nelson H, Nagorney DM, Devine RM, et al. The Mayo Clinic experience with multimodality treatment of locally advanced or recurrent colon cancer. Ann Surg Oncol. (2002) 9:177–85. doi: 10.1007/BF02557371
6. Wang H, Cao FA, Gong HF, Zheng JM, Fu CG. Could tumor characteristics identified by colonoscopy predict the locally advanced rectal carcinoma? Chin Med J. (2010) 123:2353–7.
7. Khalili M, Daniels L, Gleeson EM, Grandhi N, Thandoni A, Burg F, et al. Pancreaticoduodenectomy outcomes for locally advanced right colon cancers: a systematic review. Surgery. (2019) 166:223–9. doi: 10.1016/j.surg.2019.04.020
8. Yoshimi F, Asato Y, Kuroki Y, Shioyama Y, Hori M, Itabashi M, Amemiya R, Koizumi S, et al. Pancreatoduodenectomy for locally advanced or recurrent colon cancer: report of two cases. Surg Today. (1999) 29:906–10. doi: 10.1007/BF02482784
9. Yamanashi T, Nakamura T, Sato T, Naito M, Miura H, Tsutsui A, et al. Laparoscopic surgery for locally advanced T4 colon cancer: the long-term outcomes and prognostic factors. Surg Today. (2018) 48:534–44. doi: 10.1007/s00595-017-1621-8
10. Harada S, Iida T, Asai S, Nakamura K, Ishihara M, Iwasaki J, Itami A, Kyogoku T, et al. Successful en bloc resection of locally advanced pancreatic tail cancer with colonic perforation following neoadjuvant chemotherapy: a case report. Am J Case Rep. (2021) 22:e933226 doi: 10.12659/AJCR.933226
11. Tei M, Otsuka M, Suzuki Y, Akamatsu H. Initial experience of single-port laparoscopic multivisceral resection for locally advanced colon cancer. Surg Laparosc Endosc Percutan Tech. (2018) 28:108–12. doi: 10.1097/SLE.0000000000000508
12. Tei M, Otsuka M, Suzuki Y, Kishi K, Tanemura M, Akamatsu H. Safety and feasibility of single-port laparoscopic multivisceral resection for locally advanced left colon cancer. Oncol Lett. (2018) 15:10091–7. doi: 10.3892/ol.2018.8582
13. Paquette IM, Swenson BR, Kwaan MR, Mellgren AF, Madoff RD. Thirty-day outcomes in patients treated with en bloc colectomy and pancreatectomy for locally advanced carcinoma of the colon. J Gastrointest Surg. (2012) 16:581–6. doi: 10.1007/s11605-011-1691-7
14. Vorob’ev GI, Salamov KN, Zhuchenko AP, Shamsiev G Kh, Korniak BS. Locally-advanced cancer of the sigmoid colon. Voprosy onkologii. (1991) 37:864–9.
15. Uludag SS, Sanli AN, Akinci O, Tekcan SDE, Zengin AK, et al. Outcomes after combined right hemicolectomy and pancreaticoduodenectomy for locally advanced right-sided colon cancer: a case series. Signa vitae. (2021) 17:154–9.
16. Kaneda Y, Noda H, Endo Y, Kakizawa N, Ichida K, Watanabe F, et al. En bloc pancreaticoduodenectomy and right hemicolectomy for locally advanced right-sided colon cancer. World J Gastrointest Oncol. (2017) 9:372–8. doi: 10.4251/wjgo.v9.i9.372
17. Kimchi ET, Nikfarjam M, Gusani NJ, Avella DM, Staveley-‘Carroll KF. Combined pancreaticoduodenectomy and extended right hemicolectomy: outcomes and indications. HPB. (2009) 11:559–64. doi: 10.1111/j.1477-2574.2009.00087.x
18. Lee WS, Lee WY, Chun HK, Choi SH. En bloc resection for right colon cancer directly invading duodenum or pancreatic head. Yonsei Med J. (2009) 50:803–6. doi: 10.3349/ymj.2009.50.6.803
19. Saiura A, Yamamoto J, Ueno M, Koga R, Seki M, Kokudo N. Long-term survival in patients with locally advanced colon cancer after en bloc pancreaticoduodenectomy and colectomy. Dis Colon Rectum. (2008) 51:1548–51. doi: 10.1007/s10350-008-9318-0
20. Cojocari N, Crihana GV, Bacalbasa N, Balescu I, David L, et al. Right-sided colon cancer with invasion of the duodenum or pancreas: a glimpse into our experience. Exp Ther Med. (2021) 22:1378. doi: 10.3892/etm.2021.10813
21. Zhang J, Leng JH, Qian HG, Qiu H, Wu JH, Liu BN, et al. En bloc pancreaticoduodenectomy and right colectomy in the treatment of locally advanced colon cancer. Dis Colon Rectum. (2013) 56:874–80.
22. Yan XL, Wang K, Bao Q, Wang HW, Jin KM, Wang JY, et al. En bloc right hemicolectomy with pancreatoduodenectomy for right-sided colon cancer invading duodenum. BMC Surg. (2021) 21:302. doi: 10.1186/s12893-021-01286-0
23. Chen JB, Luo SC, Chen CC, Wu CC, Yen Y, Chang CH, et al. Colo-pancreaticoduodenectomy for locally advanced colon carcinoma-feasibility in patients presenting with acute abdomen. World J Emerg Surg. (2021) 16:7. doi: 10.1186/s13017-021-00351-6
24. Lehnert T, Methner M, Pollok A, Schaible A, Hinz U, Herfarth C. Multivisceral resection for locally advanced primary colon and rectal cancer - An analysis of prognostic factors in 201 patients. Ann Surg. (2002) 235:217–25. doi: 10.1097/00000658-200202000-00009
25. MacKay G, Molloy RG, O’Dwyer PJ. The outcome of patients with locally advanced primary and recurrent colon cancer. Br J Surg. (2005) 92:87–87.
26. Napolitano C, Valvano L, Salvati V, Barreca M. Laparoscopic en bloc resection of the right colon and VI hepatic segment for locally advanced colon cancer. Int J Colorectal Dis. (2006) 21:732–3. doi: 10.1007/s00384-006-0169-7
27. Sokmen S, Canda A, Terzi C, Sarioglu S, Obuz F, Oztop I, et al. Multivisceral resections in locally advanced colon carcinoma. Dis Colon Rectum. (2008) 51:735–6.
28. Hung HY, Yeh CY, Changchien CR, Chen JS, Fan CW, Tang R, et al. Surgical resection of locally advanced primary transverse colon cancer-not a worse outcome in stage II tumor. Int J Colorectal Dis. (2011) 26:859–65. doi: 10.1007/s00384-011-1146-3
29. Cirocchi R, Partelli S, Castellani E, Renzi C, Parisi A, Noya G, et al. Right hemicolectomy plus pancreaticoduodenectomy vs partial duodenectomy in treatment of locally advanced right colon cancer invading pancreas and/or only duodenum. Surg Oncol. (2014) 23:92–8.
30. Govindarajan A, Kiss A, Rabeneck L, Smith AJ, Hodgson D, Law CH. Impact of surgeon and hospital factors on the surgical treatment of locally advanced colon cancer: a population-based study. Ann Surg Oncol. (2008) 15:90.
31. Guidolin K, Ng D, Chadi S, Quereshy FA. Post-operative outcomes in patients with locally advanced colon cancer: a comparison of operative approach. Surg Endosc. (2022) 36:4580–4587.
32. Chow Z, Gan T, Chen Q, Huang B, Schoenberg N, Dignan M, et al. Nonadherence to standard of care for locally advanced colon cancer as a contributory factor for high mortality rates in kentucky. J Am Coll Surg. (2020) 230:428–39. doi: 10.1016/j.jamcollsurg.2019.12.041
33. Esposito L, Allaix ME, Galosi B, Cinti L, Arezzo A, Ammirati CA, Morino M, et al. Should be a locally advanced colon cancer still considered a contraindication to laparoscopic resection? Surg Endosc. (2022) 36:3039–48.
34. Pittam MR, Thornton H, Ellis H. Survival after extended resection for locally advanced carcinomas of the colon and rectum. Ann R Coll Surg Engl. (1984) 66:81–4.
35. Loutfy A, Vasani S. Locally advanced colon cancer resulting in en bloc right hemicolectomy and pancreaticoduodenectomy: case report and review of literature. J Surg Case Rep. (2018) 2018: rjy100. doi: 10.1093/jscr/rjy100
36. Goffredo P, Zhou P, Ginader T, Hrabe J, Gribovskaja-Rupp I, Kapadia M, et al. Positive circumferential resection margins following locally advanced colon cancer surgery: risk factors and survival impact. J Surg Oncol. (2020) 121:538–46. doi: 10.1002/jso.25801
37. Van Prohaska J, Govostis MC, Wasick M. Multiple organ resection for advanced carcinoma of the colon and rectum. Surg Gynecol Obstet. (1953) 97:177–82.
38. Halligan EJ, Perkel LL, Catlaw JK, Troast L. Surgical lesions of the right half of the colon and their treatment. Am J Proctol. (1951) 2:200–8.
39. Delannoy E, Gautier P, Devambez J, Toison G. [Extended right hemicolectomy for cancer of the right colon]. Lille Chir. (1954) 9:243–5.
40. Calmenson M, Black BM. Surgical management of carcinoma of the right portion of the colon with secondary involvement of the duodenum, including duodenocolic fistula; data on eight cases. Surgery. (1947) 21:476–81.
41. Welti H. [Duodenocolic fistula in a patient with cancer of the right colic flexure]. Arch Mal Appar Dig Mal Nutr. (1952) 41:689–91.
42. Sasson AR, Hoffman JP, Ross EA, Kagan SA, Pingpank JF, Eisenberg BL. En bloc resection for locally advanced cancer of the pancreas: is it worthwhile? J Gastrointest Surg. (2002) 6:147–57. doi: 10.1016/s1091-255x(01)00063-4
43. Hameed I, Aggarwal P, Weiser MR. Robotic Extended Right Hemicolectomy with Complete Mesocolic Excision and D3 Lymph Node Dissection. Ann Surg Oncol. (2019) 26:3990–1. doi: 10.1245/s10434-019-07692-2
44. Liao SF, Chen HC, Chen TC, Liang JT. Robotic multivisceral en bloc resection with reconstruction and multidisciplinary treatment of T4 sigmoid colon cancer - a video vignette. Colorectal Dis. (2021) 23:3047–8. doi: 10.1111/codi.15894
45. Sun Y, Yang HJ, Zhang ZC, Zhou YD, Li P, Zeng QS, Liu SX, Zhang XP, et al. Fascial space priority approach for laparoscopic en bloc extended right hemicolectomy with pancreaticoduodenectomy for locally advanced colon cancer. Tech Coloproctol. (2021) 25:1085–7. doi: 10.1007/s10151-021-02426-7
46. Mukai T, Nagasaki T, Akiyoshi T, Fukunaga Y, Yamaguchi T, Konishi T, et al. Laparoscopic multivisceral resection for locally advanced colon cancer: a single-center analysis of short- and long-term outcomes. Surg Today. (2020) 50:1024–31. doi: 10.1007/s00595-020-01986-9
47. Wasmann KA, Klaver CE, Bilt JD, Dieren SV, Nagtegaal ID, Punt CJ, et al. Laparoscopic surgery facilitates administration of adjuvant chemotherapy in locally advanced colon cancer: propensity score analyses. Cancer Manag Res. (2019) 11:7141–57. doi: 10.2147/CMAR.S205906
48. Podda M, Pisanu A, Morello A, Segalini E, Jayant K, Gallo G, et al. Laparoscopic versus open colectomy for locally advanced T4 colonic cancer: meta-analysis of clinical and oncological outcomes. Br J Surg. (2022) 109:319–31.
49. Huynh C, Minkova S, Kim D, Stuart H, Hamilton TD. Laparoscopic versus open resection in patients with locally advanced colon cancer. Surgery. (2021) 170:1610–5.
50. Tay PWL, Xiao JL, Lim WH, Wong NW, Chong CSC Laparoscopic versus open surgery for locally advanced colon cancer: a retrospective cohort study. Br J Surg. (2021) 108.
51. Curley SA, Evans DB, Ames FC. Resection for cure of carcinoma of the colon directly invading the duodenum or pancreatic head. J Am Coll Surg. (1994) 179:587–92.
52. Harrison LE, Merchant N, Cohen AM, Brennan MF. Pancreaticoduodenectomy for nonperiampullary primary tumors. Am J Surg. (1997) 174:393–5. doi: 10.1016/s0002-9610(97)00121-9
53. Koea JB, Conlon K, Paty PB, Guillem JG, Cohen AM. Pancreatic or duodenal resection or both for advanced carcinoma of the right colon: is it justified? Dis Colon Rectum. (2000) 43:460–5.
54. Kapoor S, Das B, Pal S, Sahni P, Chattopadhyay TK. En bloc resection of right-sided colonic adenocarcinoma with adjacent organ invasion. Int J Colorectal Dis. (2006) 21:265–8.
55. Song XM, Wang L, Zhan WH, Wang JP, He YL, Lian L, Cai GF, Zhou HF, Huang BY, Lan P. Right hemicolectomy combined with pancreatico- duodenectomy for the treatment of colon carcinoma invading the duodenum or pancreas. Chin Med J. (2006) 119:1740–3.
56. Fuks D, Pessaux P, Tuech JJ, Mauvais F, Bréhant O, Dumont F, Chatelain D, Yzet T, Joly JP, Lefebure B, Deshpande S, Arnaud JP, Verhaeghe P, Regimbeau JM. Management of patients with carcinoma of the right colon invading the duodenum or pancreatic head. Int J Colorectal Dis. (2008) 23:477–81.
57. Lianwen Y, Jianping Z, Guoshun S, Dongcai L, Jiapeng Z. Surgical treatment for right colon cancer directly invading the duodenum. Am surg. (2009) 75:385–8.
58. Costa SRP, Henriques AC, Horta SHC, Waisberg J, Speranzini MB. En-bloc pancreatoduodenectomy and right hemicolectomy for treating locally advanced right colon cancer (T4): a series of five patients. Arq Gastroenterol. (2009) 46:151–3. doi: 10.1590/s0004-28032009000200014
59. Arredondo J, Baixauli J, Pastor C, Chopitea A, Sola JJ, González I, et al. Mid-term oncologic outcome of a novel approach for locally advanced colon cancer with neoadjuvant chemotherapy and surgery. Clin Trans Oncol. (2017) 19:379–85. doi: 10.1007/s12094-016-1539-4
60. Arredondo J, Pastor C, Baixauli J, Rodríguez J, González I, Vigil C, et al. Preliminary outcome of a treatment strategy based on perioperative chemotherapy and surgery in patients with locally advanced colon cancer. Colorectal Dis. (2013) 15:552–7.
61. Arredondo J, Pastor E, Sim V, Beltrán M, Castañón C, Magdaleno MC, et al. Neoadjuvant chemotherapy in locally advanced colon cancer: a systematic review. Tech Coloproctol. (2020) 24:1001–15.
62. Cheong CK, Nistala KRY, Ng CH, Syn N, Chang HSY, Sundar R, Yang SY, Chong CS. Neoadjuvant therapy in locally advanced colon cancer: a metaanalysis and systematic review. J Gastrointest Oncol. (2020) 11:847.
63. De Gooyer JM, Verstegen MG, Lam-Boer J, Radema SA, Verhoeven RHA, Verhoef C, Schreinemakers JMJ, De Wilt JHW, et al. Neoadjuvant chemotherapy for locally advanced t4 colon cancer: a nationwide propensity-score matched cohort analysis. Digestive Surg. (2020) 37:292–301.
64. Group Foxtrot Collaborative. Feasibility of preoperative chemotherapy for locally advanced, operable colon cancer: the pilot phase of a randomised controlled trial. Lancet Oncol. (2012) 13:1152–60. doi: 10.1016/S1470-2045(12)70348-0
65. Bhandari RS, Lakhey PJ, Mishra PR. En bloc pancreaticodudenectomy with colectomy for locally advanced right sided colon cancer. J Nepal Med Assoc. (2015) 53:301–3.
66. Taflampas P, Moran BJ. Extraperitoneal resection of the right colon for locally advanced colon cancer. Colorectal Dis. (2013) 15:E56–9. doi: 10.1111/codi.12031
67. Biyani DK, Speake D, Siriwardena A, Watson AJM. Management of duodenal involvement in locally advanced colonic carcinoma. Colorectal Dis. (2007) 9:178–81.
68. Zwanenburg ES, Wisselink DD, Klaver CEL, Brandt ARM, Bremers AJA, Burger JWA, van Grevenstein WMU, Hemmer PHJ, de Hingh IHJT, Kok NFM, Wiezer MJ, et al. Adhesion formation after surgery for locally advanced colonic cancer in the COLOPEC trial. Br J Surg. (2022) 109:315–8. doi: 10.1093/bjs/znab467
69. Jain V, Sharma D, Simeunovic K, Gavrancic T, Jubbal S, Ramasamy V, et al. Colon cancer with gastric invasion resulting in gastric outlet obstruction: an uncommon presentation of locally advanced colorectal cancer that was successfully treated with surgical resection. Am J Gastroenterol. (2014) 109:S411–411.
70. Zhao YZ, Han GS, Wang JX. En bloc pancreaticoduodenectomy and colectomy for locally advanced right-sided colon cancer - a video vignette. Colorectal Dis. (2015) 17:828–9. doi: 10.1111/codi.13043
71. Luna P, Ramirez-Ramirez M, Rodriguez-Ramirez S, Gutierrez M, Cravioto A, Martinez H, et al. Justify aggressive multivisceral resection for primary locally advanced colon cancer? Ann Surg Oncol. (2008) 15:87–87.
72. Ağalar C, Canda AE, Unek T, Sokmen S. En bloc pancreaticoduodenectomy for locally advanced right colon cancers. Int J Surg Oncol. (2017) 2017:5179686.
73. Schiele S, Arndt TT, Martin B, Miller S, Bauer S, Banner BM, Brendel EM, Schenkirsch G, Anthuber M, Huss R, Märkl B, Müller G, et al. Deep learning prediction of metastasis in locally advanced colon cancer using binary histologic tumor images. Cancers. (2021) 13:2074. doi: 10.3390/cancers13092074
Keywords: advanced colon cancer, en bloc resection, pancreaticoduodenectomy, hemicolectomy, multivisceral resection
Citation: Ri H, Kang H, Xu Z, Gong Z, Jo H, Amadou BH, Xu Y, Ren Y, Zhu W and Chen X (2023) Surgical treatment of locally advanced right colon cancer invading neighboring organs. Front. Med. 9:1044163. doi: 10.3389/fmed.2022.1044163
Received: 14 September 2022; Accepted: 29 December 2022;
Published: 13 January 2023.
Edited by:
Enis Kostallari, Mayo Clinic, United StatesReviewed by:
Marcello Giuseppe Spampinato, Ospedale Vito Fazzi, ItalyBo Feng, Shanghai Jiao Tong University, China
Copyright © 2023 Ri, Kang, Xu, Gong, Jo, Amadou, Xu, Ren, Zhu and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xin Chen,  Y2hlbnhpbmNqekBnbWFpbC5jb20=
Y2hlbnhpbmNqekBnbWFpbC5jb20=
†These authors have contributed equally to this work and share first authorship
‡ORCID: HyokJu Ri, orcid.org/0000-0002-5172-7029; HaoNan Kang, orcid.org/0000-0003-3893-3749; Yang Xu, orcid.org/0000-0002-6923-8274; Xin Chen, orcid.org/0000-0001-8122-4396
 HyokJu Ri
HyokJu Ri HaoNan Kang
HaoNan Kang ZhaoHui Xu1
ZhaoHui Xu1 HyonSu Jo
HyonSu Jo Xin Chen
Xin Chen