- 1Department of Ophthalmology, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences, Beijing, China
- 2Key Laboratory of Ocular Fundus Diseases, Chinese Academy of Medical Sciences, Peking Union Medical College, Beijing, China
- 3Department of Ophthalmology, Xi'an Fourth Hospital, Xi'an, China
- 4School of Medicine, University of New South Wales, Kensington, NSW, Australia
Purpose: To evaluate the effect of femtosecond laser-assisted in situ keratomileusis (FS-LASIK) on retinal fovea thickness, volume, and retinal nerve fibre layer (RNFL) thickness.
Methods: Thirty-seven eyes (37 patients) undergoing FS-LASIK were included in this prospective study. Optical coherence tomography (OCT) was performed 1 day before, 1 h and 1 day after FS-LASIK surgery.
Result: Eighteen male and nineteen females were enrolled. Mean patient age was 22.94 ± 4.22 years. One hour postoperatively, macula fovea thicknesses, macula fovea volume, macula parafovea thickness, macula parafovea volume, macula perifovea thickness, macula perifove volume, temporal RNFL thickness, and superior RNFL thickness measures showed significant decrease (t = 6.171, 6.032, and 9.837, 9.700, 2.532, 4.393, 4.926, 2.265; p = 0.000, 0.000, 0.000, 0.000, 0.016, 0.000, 0.000, and 0.011). Day 1 post-operation, macula fovea thicknesses, macula fovea volume, macula parafovea thickness, macula parafovea volume, and inferior RNFL thickness measures showed significant change compared to preoperative measures (t = 3.620, 3.220, 2.901, 2.910, 3.632; p = 0.001, 0.003, 0.006, 0.006, and 0.001).
Conclusion: Our data suggest there are alterations in retinal foveal and RNFL measurements by OCT 1 h and 1 day after FS-LASIK surgery.
Introduction
Laser-assisted in situ keratomileusis is a popular corneal refractive technique utilised to enhance visual acuity. Both traditional microkeratome and modern femtosecond laser laser-assisted in situ keratomileusis (FS-LASIK) involve the dissection of a superficial lamellar flap by suction to reveal the corneal stroma for remodelling. FS-LASIK creates a predictable homogeneously thick stromal flap, which is elevated by a suction ring. It leads to better refractive results in comparison to standard microkeratomes most likely due to more predictable and planar corneal flaps (1).
During the LASIK procedure, the intraocular pressure (IOP) is abruptly increased. Dramatic IOP change has been theorised to vitreous traction, thereby causing postoperative optic nerve and vitreoretinal complications. As such, glaucoma is also a contraindication (2, 3). It is evident from the literature that LASIK with mechanical microkeratome is not detrimental to retinal neve fibre layers of healthy individuals (4, 5). The evidence surrounding FS-LASIK and foveal and retinal thickness is conflicting and sparse. Some studies have demonstrated changes within the retina, following FS-LASIKS (6), whilst other have not (7), and there is uncertainty in the clinical significance of such change (8).
The objective of this study was to determine whether FS-LASIK induces changes in retinal foveal and RNFL measurements with optical coherence tomography (OCT) immediately post-procedure.
Materials and Methods
All patients underwent corneal pachymetry and topography preoperatively. Patients with contraindication to LASIKs were excluded. Contraindications include ocular disease, ocular surface disorder, glaucoma, corneal thickness <500 microns, and/or irregular corneal topography. The patients were also excluded from the study if their preoperative best-corrected visual acuity was <20/40 or if they had prior laser or intraocular surgery. Our prospective study recruited patients undergoing FS-LASIK by one surgeon (WZH).
All patients on examination had an intraocular pressure (IOP) <21 mmHg and normal optic disk. A normal optic disc was defined by a vertical cup-to-disk asymmetry <0.2, cup/disk ratio <0.6, and an intact neuro-retinal rim without peripapillary haemorrhages, notches, localised pallor, or nerve fibre layer defect.
All patients underwent FS-LASIK treatment using the VISX™ (Abbott Medical Optics Inc., Santa Clara, CA, USA) under topical anaesthesia. A corneal flap, 110-micron thick, was created by IFS IntraLase™ 150 HZ (Abbott Medical Optics Inc., Santa Ana, CA, USA). Suction during the creation of a flap lasted ~45 s. Retinal fovea thickness, volume, and retinal nerve fibre layer (RNFL) thickness were measured preoperatively, and postoperatively at 1 h and 1 day, following FS-LASIK surgery. OCT (Optovue Inc., Fremont, CA, USA) performed 360° circular scans with a diameter of 3.45 mm centred on the optic disk.
Only the right eyes of the participants were included to be observed.
Statistical Analysis
Volume and thickness of the inner retina (macula fovea, parafovea, and perifovea), and the thickness of the RNFL (superior, inferior, nasal, and temporal) were recorded pre- and postoperatively. The mean and standard deviation were calculated for both pre- and postoperative measurements. A paired t-test was utilised to determine any statistical difference between pre- and postoperative measurements. A p-value < 0.05 was considered statistically significant.
Result
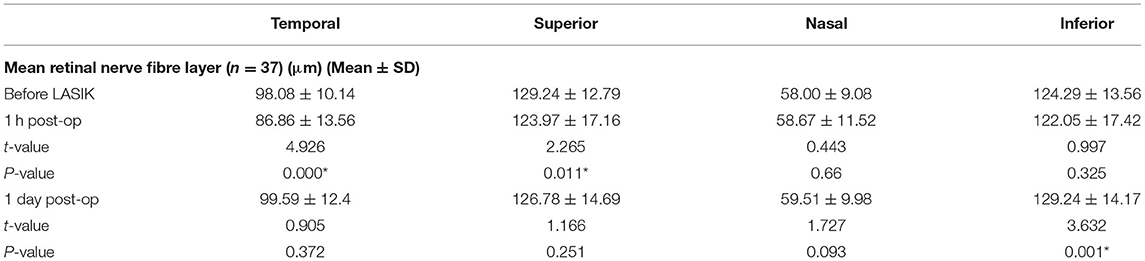
Eighteen males and nineteen females (n = 37) were enrolled in this study. Mean patient age was 22.94 ± 4.22 years. The thickness and volume of the macula declined significantly 1 h post operation (Table 1). By Day 1, post operation, five out of the six measures of the macula showed decreases compared to the preoperative values, but only four (fovea thickness and volume, parafovea thickness, and volume) of these were statistically significant (Table 1). All showed increases compared to immediate postoperatively.
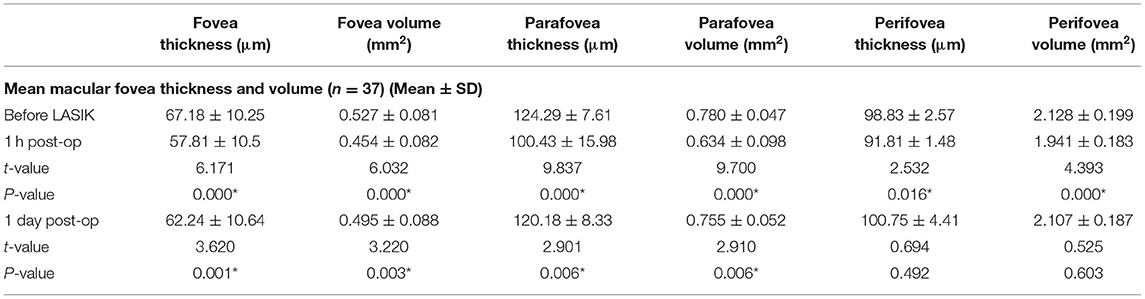
Table 1. Mean macular fovea thickness and volume before and after femtosecond laser laser-assisted in situ keratomileusis (FS-LASIK) surgery.
The mean RNFL decreased 1 h postoperatively in the temporal and superior RNFL (Table 2). At 1 day post-operation, the RNFL was only significantly increased in the inferior portion compared to the preoperative measures. All measurements of macula and RNFL thickness and volume increased between 1 h postoperatively and 1 day postoperatively.
Discussion
Our study showed significant differences in preoperative and postoperative FS-LASIKs measurements of the macula and RNFL thickness as determined by OCT. Eight of ten measurements 1 h after FS-LASIKs were significantly different, whilst only five of ten measurements 1 day after FS-LASIKs were significantly different compared to preoperative measurements of the macula and RNFL. All measurements showed improvement between 1 and 1 day postoperatively. We hypothesise that our results are due to alterations in corneal architecture, thereby inducing artefactual OCT measurements.
There is conflicting evidence regarding measurements of macular edema and RNFL measurements by OCT in FS-LASIKs. Some studies have demonstrated changes within the macula and RNFL post FS-LASIKs (6, 8) and have attributed these effects to macular edema associated with IOP elevation during procedure. Elevation of IOP during LASIKs can be significant. In a previous study, intraoperative microkeratome LASIKs lead to IOP values of > 150 mmHg (9). Whilst FS-LASIKs leads to reduced IOP values during the suction, they lead to a greater period of maintenance of high IOP pressure, and there is uncertainty in comparative effect of FS-LASIKs on retinal measurements (10).
A range of microkeratome LASIK studies has demonstrated no detrimental effects on RNFL and macular thickness (3–5) and suggested that changes demonstrated via OCT are secondary to corneal aberrations, leading to artefactual measurements of the retina and fovea since there was no possibility that substantive decrease and the following increase of retina thickness can happen. The most likely cause of this phenomenon would be the reflectivity change, following the refractive procedure. Furthermore, larger studies with longer follow-up times have demonstrated that LASIKs is rarely associated with vitreoretinal pathology (11, 12).
Optical coherence tomography evaluates the reflectivity of posterior segment structures. Utilising these data, the RNFL thickness can consequently be calculated. FS-LASIK produces corneal spherical aberrations (13) and alters the refractive properties of the cornea. Consequently, this can interfere with OCT measurements, reducing reliability within the immediate postoperative period. These changes in refraction can be compensated for such as in scanning laser polarimetry (SLP) (14, 15). We should be aware of this measurement changes following the refractive procedure, since the myopia patients are the well-known potential high-risk group of glaucoma and retina disease in which OCT is one of the most important diagnostic tools.
Conclusion
In our study, FS-LASIKs induced alterations in the inner retina and RNFL measurements by OCT. This is unlikely to be actual structural changes but is associated with changes in refractive properties of the cornea.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author Contributions
All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
Funding
This work was supported by The Non-profit Central Research Institute Fund of Chinese Academy of Medical Sciences (2018PT32029).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Gil-Cazorla R, Teus MA, de Benito-Llopis L, Mikropoulos DG. Femtosecond laser vs. mechanical microkeratome for hyperopic laser in situ keratomileusis. Am J Ophthalmol. (2011) 152:16–21.e2. doi: 10.1016/j.ajo.2011.01.009
2. Lee AG, Kohnen T, Ebner R, Bennett JL, Miller NR, Carlow TJ, et al. Optic neuropathy associated with laser in situ keratomileusis. J Cataract Refract Surg. (2000) 26:1581–4. doi: 10.1016/S0886-3350(00)00688-X
3. Whitson JT, McCulley JP, Cavanagh HD, Song J, Bowman RW, Hertzog L. Effect of laser in situ keratomileusis on optic nerve head topography and retinal nerve fiber layer thickness. J Cataract Refract Surg. (2003) 29:2302–5. doi: 10.1016/S0886-3350(03)00466-8
4. Dementyev DD, Kourenkov VV, Rodin AS, Fadeykina TL, Diaz Martines TE. Retinal nerve fiber layer changes after LASIK evaluated with optical coherence tomography. J Refract Surg. (2005) 21:S623–7. doi: 10.3928/1081-597X-20050902-13
5. Aristeidou AP, Labiris G, Paschalis EI, Foudoulakis NC, Koukoula SC, Kozobolis VP. Evaluation of the retinal nerve fiber layer measurements, after photorefractive keratectomy and laser in situ keratomileusis, using scanning laser polarimetry (GDX VCC). Graefe's archive for clinical and experimental ophthalmology = Albrecht von Graefes Archiv fur klinische und experimentelle. Ophthalmologie. (2010) 248:731–6. doi: 10.1007/s00417-009-1273-5
6. Zhang J, Zhou YH. Effect of suction on macular thickness and retinal nerve fiber layer thickness during LASIK used femtosecond laser and Moria M2 microkeratome. Int J Ophthalmol. (2015) 8:777–83. doi: 10.3980/j.issn.2222-3959.2015.04.24
7. Zhang J, Zhou Y, Zheng Y, Liu Q, Zhai C, Wang Y. Effect of suction on macular and retinal nerve fiber layer thickness during femtosecond lenticule extraction and femtosecond laser-assisted laser in situ keratomileusis. J Cataract Refract Surg. (2014) 40:1994–2001. doi: 10.1016/j.jcrs.2014.03.027
8. Zhao PF, Zhou YH, Zhang J, Wei WB. Analysis of macular and retinal nerve fiber layer thickness in children with refractory amblyopia after femtosecond laser-assisted laser in situ keratomileusis: a retrospective study. Chinese Med J. (2017) 130:2234–40. doi: 10.4103/0366-6999.213959
9. Bradley JC, McCartney DL, Craenen GA. Continuous intraocular pressure recordings during lamellar microkeratotomy of enucleated human eyes. J Cataract Refract Surg. (2007) 33:869–72. doi: 10.1016/j.jcrs.2007.02.017
10. Katsanos A, Arranz-Marquez E, Canones R, Lauzirika G, Rodriguez-Perez I, Teus MA. Retinal nerve fiber layer thickness after laser-assisted subepithelial keratomileusis and femtosecond LASIK: a prospective observational cohort study. Clin Ophthalmol. (2018) 12:1213–8. doi: 10.2147/OPTH.S168033
11. Arevalo JF, Ramirez E, Suarez E, Morales-Stopello J, Cortez R, Ramirez G, et al. Incidence of vitreoretinal pathologic conditions within 24 months after laser in situ keratomileusis. Ophthalmology. (2000) 107:258–62. doi: 10.1016/S0161-6420(99)00078-0
12. Ruiz-Moreno JM, Alio JL. Incidence of retinal disease following refractive surgery in 9,239 eyes. J Refract Surg. (2003) 19:534–47. doi: 10.3928/1081-597X-20030901-08
13. Zhang H, Wang Y, Li H. Corneal spherical aberration and corneal asphericity after small incision lenticule extraction and femtosecond laser-assisted LASIK. J Ophthalmol. (2017) 2017:4921090. doi: 10.1155/2017/4921090
14. Choplin NT, Schallhorn SC, Sinai M, Tanzer D, Tidwell JL, Zhou Q. Retinal nerve fiber layer measurements do not change after LASIK for high myopia as measured by scanning laser polarimetry with custom compensation. Ophthalmology. (2005) 112:92–7. doi: 10.1016/j.ophtha.2004.07.027
15. Halkiadakis I, Anglionto L, Ferensowicz M, Triebwasser RW, van Westenbrugge JA, Gimbel HV. Assessment of nerve fiber layer thickness before and after laser in situ keratomileusis using scanning laser polarimetry with variable corneal compensation. J Cataract Refract Surg. (2005) 31:1035–41. doi: 10.1016/j.jcrs.2004.12.045
Keywords: femtosecond laser-assisted in situ keratomileusis, macular thickness, retinal nerve fibre layer thickness, optical coherence tomography, myopia
Citation: Jiang Y, Wang Z, Li Y, Li Y and Lu TC (2021) Retinal Nerve Fibre Layer Thickness Change Following Femtosecond Laser-Assisted in situ Keratomileusis. Front. Med. 8:778666. doi: 10.3389/fmed.2021.778666
Received: 17 September 2021; Accepted: 19 October 2021;
Published: 29 November 2021.
Edited by:
Haijiang Lin, Harvard Medical School, United StatesCopyright © 2021 Jiang, Wang, Li, Li and Lu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhonghai Wang, d3pocHVtY2hAc2luYS5jb20=; Ying Li, bGl5aW5ncHVtY2hAMTI2LmNvbQ==; Yong Li, MzQ0ODEzOTk1QHFxLmNvbQ==
 Yang Jiang
Yang Jiang Zhonghai Wang1,2*
Zhonghai Wang1,2*