- 1The First Dongguan Affiliated Hospital of Guangdong Medical University, Dongguan, China
- 2Peking University Clinical Research Institute, Peking University First Hospital, Beijing, China
- 3Shenzhen Longhua District Central Hospital, Shenzhen, China
- 4Department of Obstetrics and Gynecology, Peking University First Hospital, Beijing, China
Background: To address the worldwide dramatically increased Cesarean section (CS) rate in the past decades, WHO has recommended the CS rate should not be higher than 10–15%. Whether it is achievable remains unknown.
Methods: We collected the data of delivery from 2008 to 2017 in two typical regional hospitals in China: Longhua Hospital (national policies rigorously implemented) and Dongguan Hospital (national policies not rigorously implemented). We compared between the two hospitals the 10 years trend in annual rate of CS, standardized by age, education level, parity, and CS history, against the time of issuing relevant national, local, and hospital policies.
Results: In 10 years, 42,441 women in Longhua and 36,935 women in Dongguan have given birth. China's first national policy on CS reduction was issued in 2010 and the formal relaxation of one-child policy was issued in 2015–2016. In Longhua, the standardized annual CS rate was around 35% in 2008–2009, which declined sharply since 2010 down to 13.1% in 2016 (p < 0.001) and then leveled off. In contrast, in Dongguan, the rate stayed around 25% at the beginning, increased to 36% in 2011, decreased sharply to 27% in 2012, and leveled off until 2015 (p < 0.001), and then bounced back to 35% in 2017. The proportion of women with the history of CS increased significantly in the two hospitals (both roughly from 6% before 2010 to 20% after 2015). Analyses stratified by modified Robson classification showed that CS rates reduced in all risk classes of delivery women in Longhua but only in the Robson class 2 group in Dongguan. Major complications did not differ by hospital.
Conclusion: With vigorously implementing national policies at micro levels, the WHO-recommended CS rate could be achieved without increase in major complications.
Introduction
Although Cesarean sections (CSs) with medical indication can effectively reduce maternal and neonatal morbidity and mortality, overuse of CS is a threat to the health of the mother and the child (1, 2). WHO has recommended that the reasonable CS rate should not be higher than 10–15% of all deliveries (3, 4). In contrary to the recommendation, the worldwide CS rate has increased dramatically during the past 30 years and has led to global concerns (5, 6). This significant increase has been driven mainly by non-medically indicated CS in many countries (7).
In China, the overall annual CS rate increased from 29% in 2008 to 35% in 2014 (8) as one of the highest CS rates in the world (9). Concerning about the “alarming” CS rates, the Chinese government issued a variety of national policies, programs, and activities to reduce the CS rate nationwide (8). As a result, China became the only country where a reduction in CS rate has been achieved (6, 10, 11). The data from China's National Maternal Near Miss Surveillance System (NMNMSS) showed that hospital-based CS rate decreased from 45% in 2012 to 41% in 2016 (10). While we are proud of the big success as the first country in the world to have CS rate reduced at the country level, we have to admit that the CS rate (over 40% on an average) is still too high and far beyond the ideal rate of 10% as recommended by the WHO (4). Whether the WHO-recommended CS rate can be achieved in China and how it can be achieved remain largely unknown.
In addition to the national policies and activities that have been shown effective to reduce the national CS rate in China (8, 10, 12), the local government and hospital policies are also critical to make the national policies implemented and sustained. However, evidences on the relationship between the CS rate and the implementation of the national policies at hospital levels are lacking. Understanding this relationship would provide insights for the development of targeted intervention measures that will further bring down the high national CS rate in China.
China's one-child policy was first relaxed in November 2013 (10, 13) and then the two-child policy was implemented in October 2015 (13). How the policy relaxation would impact on the trend in overall CS rate in China bears critical importance but remains to be understood. On the one hand, the policy relaxation would accelerate the declining trend of CS rate among nulliparous women for they might not intend to have CS, so that they keep at lower risk for future births. On the other hand, multiparous women with higher age and previous uterine scar would have increased because of the previous one-child policy and high CS rate, they might be intended to choose CS for the birth (14).
Therefore, the current study aimed to understand, under the national CS reduction movement, the discrepant influences of the local policies and actions at hospital level on the CS rate, by comparing two typical regional hospitals in China for 10 years with against to the time of issuing national policies/clinical guidelines. Also, we explored how the relaxation of the one-child policy would impact the trend of CS rate in subgroups by parity and CS history in each hospital. The selected two hospitals (Shenzhen Longhua District Central Hospital, Longhua Hospital; The First Dongguan Affiliated Hospital of Guangdong Medical University, Dongguan Hospital) are located adjacent to each other but administratively belonged to different cities of Guangdong Province, which had significant difference in responses to the national policies and clinical guidelines on the reduction of CS rate. It would be helpful to analyze the effect of policy implementation on CS rate assuming the similar population characteristics in these two hospitals.
Materials and Methods
Setting and Study Population
This was a retrospective cohort study conducted in two hospitals in Guangdong Province of China: Longhua Hospital located in Shenzhen and Dongguan Hospital located in Dongguan, which is next to Shenzhen. The two hospitals are both tertiary hospitals and about 50 kms apart, though administratively belong to different cities. Shenzhen is one of the China's four first-tier cities, with an estimated population of 21 million, birth rate of 25‰, 2.7 medical staffs per thousand population, and gross domestic product per capita of $28,500. Dongguan is a third-tier city in China, with an estimated population of 8 million, birth rate of 22‰, 2.1 medical staffs per thousand population, and gross domestic product per capita of $14,100 (15).
We retrieved data from the hospital information systems for the obstetric records from January 1, 2008 to December 31, 2017. The study participants included women who aged ≥18 years, delivered at a gestational age of ≥28 weeks, and gave birth with a fetus of birth weight 1,000 g or higher. The study was approved by the institutional review boards of the two participating hospitals (IRB2020-135-01). Informed consent was not obtained as this was a retrospective study and the data came from the hospital's medical records.
Data Collection and Study Outcomes
The downloaded data were reviewed to ensure that the inclusion and exclusion criteria were met. Then, the database was de-identified and used for further analyses. Data abstracted included maternal age, gestational age, parity, history of CS, fetal position, delivery mode, and outcomes of delivery including neonatal death and maternal complications.
The primary outcome was the annual CS rate standardized by age, education level, parity, and history of CS. Secondary outcomes included CS rate in subgroups separated by parity, history of CS, and Robson classification.
We modified the Robson classification into the following eight groups, as information on induction of labor was not available in the study: (1) nulliparous, single cephalic pregnancy, ≥37 weeks' gestation; (2) multiparous, single cephalic pregnancy, ≥37 weeks' gestation without a uterine scar; (3) multiparous, single cephalic pregnancy, ≥37 weeks' gestation with uterine scar(s); (4) nulliparous, single breech pregnancy; (5) multiparous, single breech pregnancy; (6) all multiple pregnancies, with/without previous uterine scar(s); (7) single pregnancy in other abnormal lie, with/without previous uterine scar(s); and (8) single cephalic pregnancy, ≤ 36 weeks' gestation (10, 16). We further merged the Robson groups 4 to 7 into one group, since these groups accounted for only 4.0% of all obstetric women and 13.9% of all CS cases.
Maternal complications were classified into mutually exclusive categories, including hysterorrhexis, hysterectomy, blood transfusion, and maternal deaths. Maternal death was defined as death from any cause during pregnancy or within 42 days of termination of pregnancy, except for accidental deaths. Neonatal death was defined as any neonatal deaths in the first 6 days after birth among stillbirths.
Statistical Analysis
We used Statistics Analysis System software (version 9.3, SAS Institute, Cary, NC, USA) for statistical analysis. All study variables were categorical and the differences between the two study hospitals were compared using the χ2 test. Using all women in the two study hospitals as the standard population, we calculated the weighted average annual CS rate standardized by age, education level, parity, CS history, and Robson classification over the 10 years based on the weights from combined population, to compare the trends between the two study hospitals. The CS rates were tested for changes over time using χ2 tests for trend. Crude odds ratio (cOR) and 95% CI were calculated for the association between year and the proportion of nulliparous women, with truncation analysis at year 2014. To understand the change in 10 years in composition of women in type of delivery by parity and CS history, we plotted the data annually. Similarly, we plotted the annual composition of CS cases by parity and CS history to understand the 10 years change, which indicated the change of each group's contribution to the overall CS rate. A p < 0.05 was considered to be statistically significant.
Role of the Funding Source
The funder of the study had no role in study design, data collection, statistical analysis, results interpretation, or writing of the manuscript. All authors had full access to all the data in the study and accept final responsibility to submit for publication.
Results
Differences in the Two Hospitals in Responses to the National Policies and Clinical Guidelines on Reduction of CS Rate
Against to each national policy and guideline, Table 1 listed the local policies and actions taken for the implementation. It clearly indicated that local health authorities and the director of obstetrics and gynecology department performed very differently in the two study hospitals. In Longhua, specific local policies, actions, and department rules were developed and taken to reinforce the national policies and guidelines recommendations. In Dongguan hospital, no specific local policies or department rules were taken except a research program that was initiated since 2012 to reduce CS rate among multiparous women with a scar uterus.
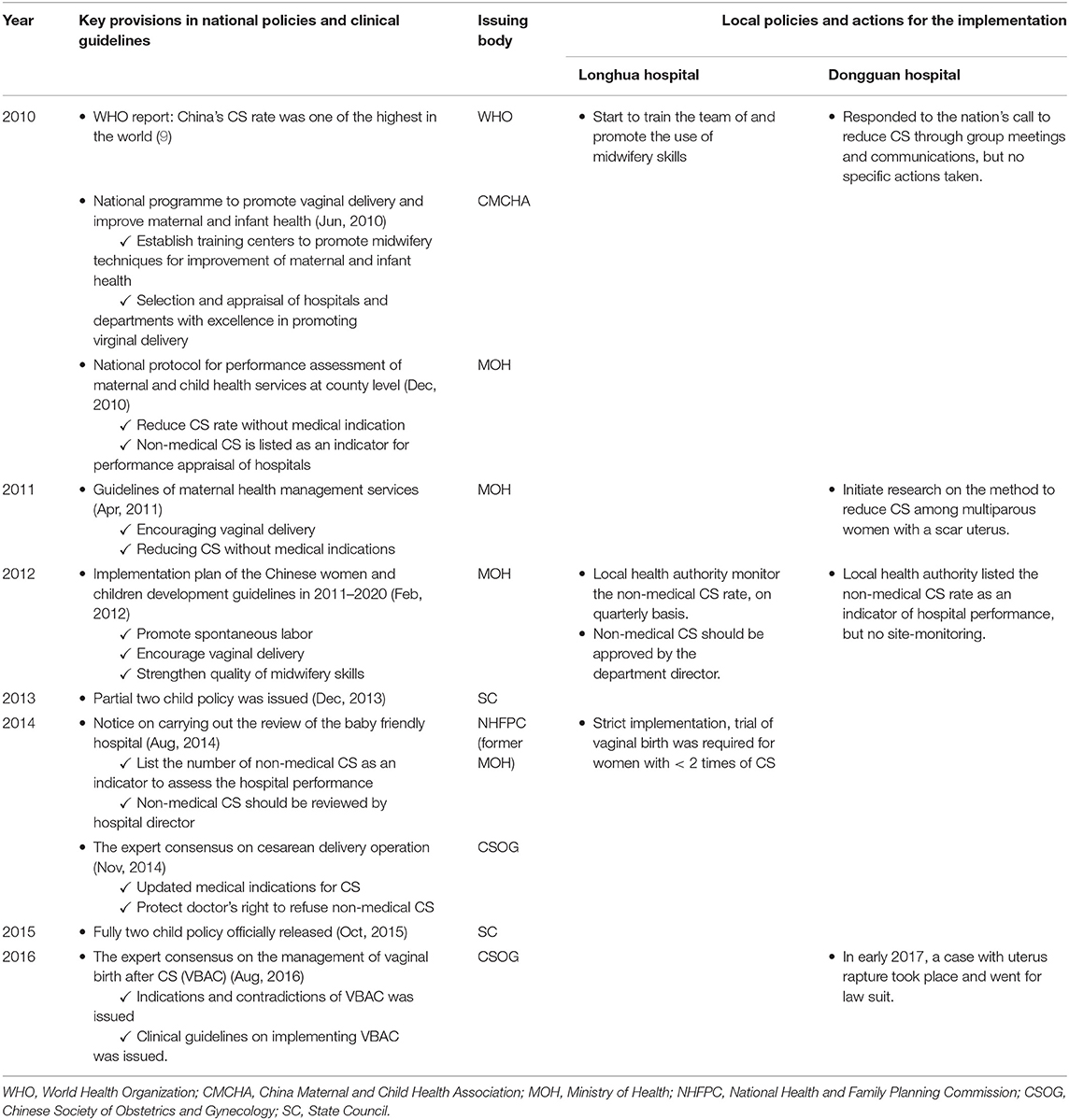
Table 1. The relevant national policies/clinical guidelines and local policies and actions for the implementation.
Comparison of the Two Study Hospitals in Characteristics of Delivery Women
From 2008 to 2017, a total of 79,376 women gave birth in the two study hospitals; 42,441 in Longhua and 36,935 in Dongguan. The proportion of women aged over 35 years and the proportion of women in the modified Robson classification group 3–8 were comparable between the two hospitals. However, women in Longhua were more educated and likely to be nulliparous, and less likely to have CS, in comparison with women in Dongguan (Table 2).
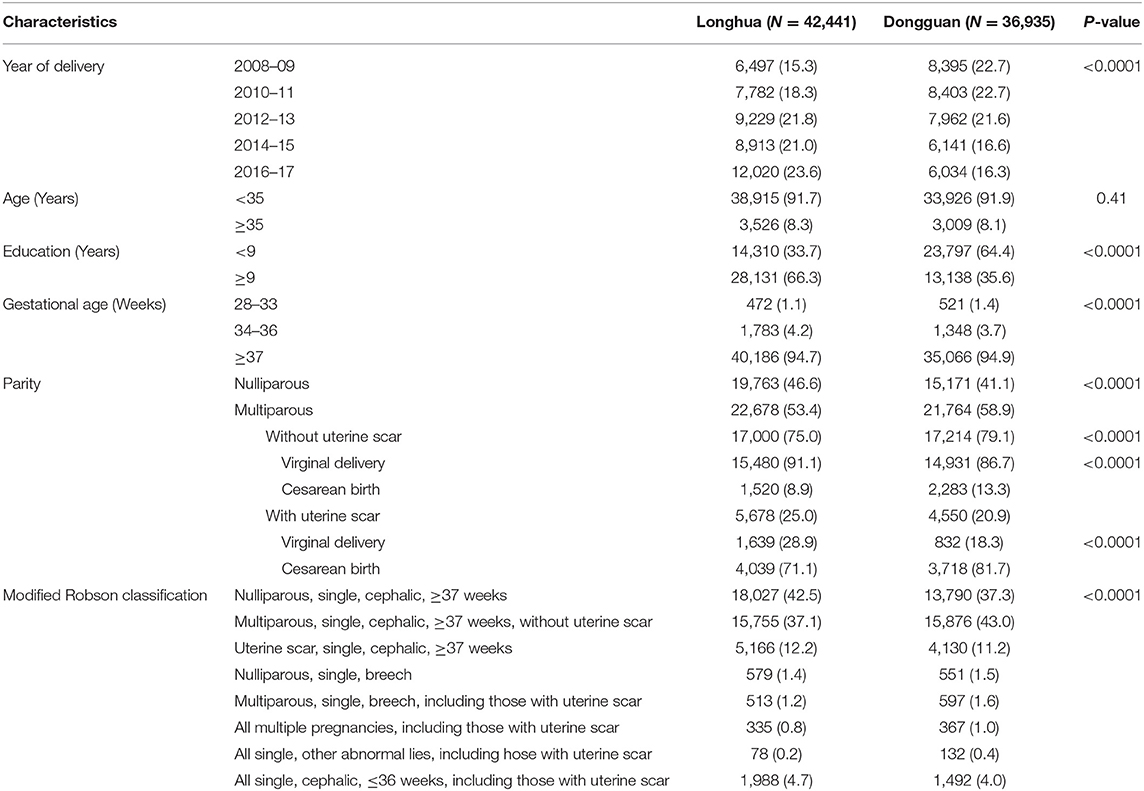
Table 2. Demographical and clinical characteristics of women delivering babies in 2008–2017 in two hospitals in Guangdong, China.
Trend in Composition of Delivery by Parity and History of CS
Although the number of deliveries increased in Longhua but decreased in Dongguan during the 10 years, the composition by parity were similar and showed the same temporal trend in the two hospitals. The proportion of nulliparous women decreased slowly from 2008 to 2014 (from 52.3 to 47.1% in Longhua, cOR 0.97, 95% CI: 0.96–0.98; and from 46.1 to 39.7% in Dongguan, cOR 0.95, 95% CI: 0.94—.97) but more quickly from 2015 to 2017 (from 43.7 to 35.2% in Longhua, cOR 0.84, 95% CI: 0.80–0.87; and from 37.5 to 33.4% in Dongguan, cOR 0.91, 95% CI: 0.87–0.96) (Figure 1). Among multiparous women, the proportion with CS history in both the hospitals increased with a similar magnitude, from 7.6 to 20.1% in Longhua and from 6.3 to 21.7% in Dongguan (Figure 1).
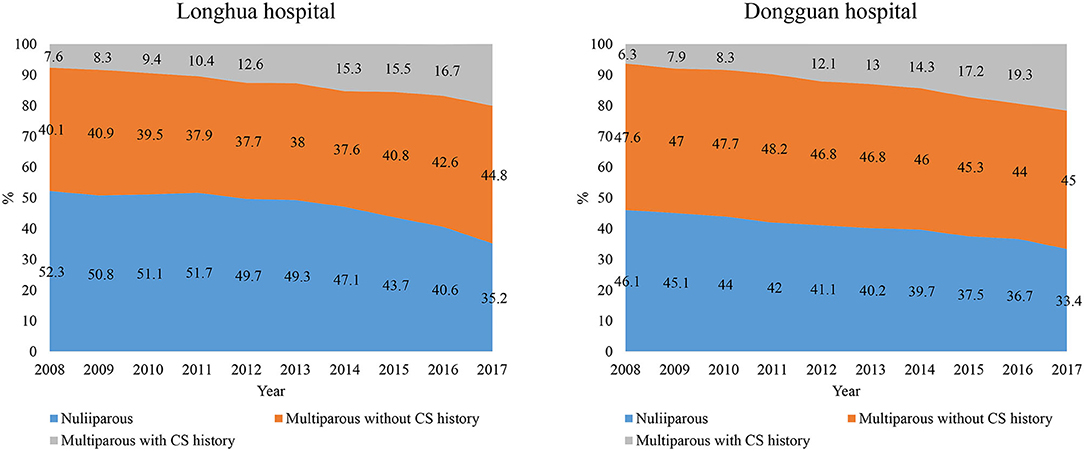
Figure 1. Trends in composition of women by parity and CS history in 10 years from 2008 to 2017 in two hospitals.
Trends in CS Rates
Overall, 24.8% of women in the two hospitals had CS. The standardized CS rates in Longhua stayed around 35% at the beginning and started to decrease steadily and sharply from the year 2010 until the year 2016 (13.1%) and then leveled off (p for trend < 0.001). The standardized CS rate in Dongguan varied around 25% at the beginning, increased to 36% in 2011, decreased sharply to 27% in 2012 and leveled off until 2015 (p < 0.001), and then bounced back to 35% in 2017 (Figure 2). In fact, the CS rate declined significantly over the 10 years period in all subgroups by parity and history of CS in Longhua, while in Dongguan, the CS rate only declined from 2011 to 2015 and only in multiparous women (Table 3).
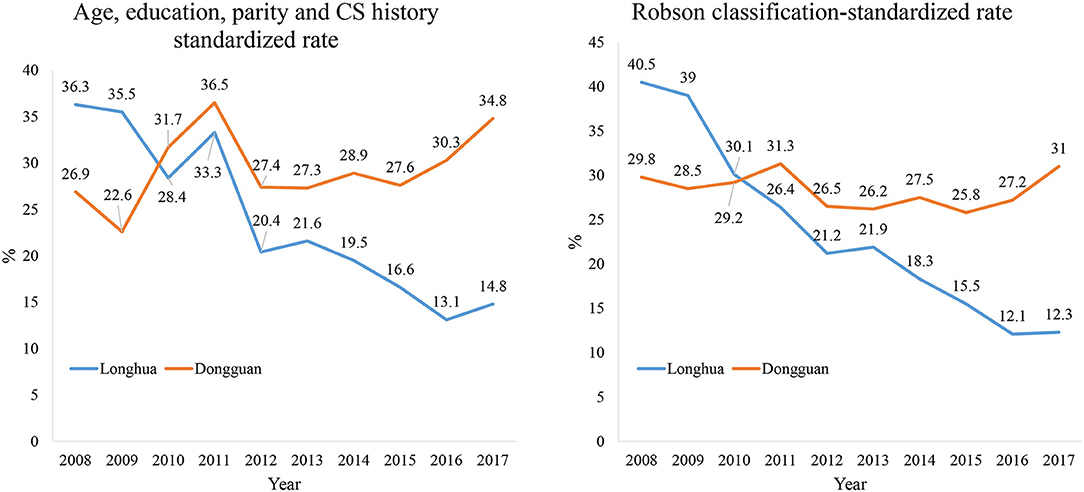
Figure 2. Comparison of two hospitals in CS rate standardized for composition of age, education level, parity, and history of CS (Left) and Robson classification (Right).

Table 3. CS rates (%) in each year in all women and by parity and history of CS in two study hospitals.
Figure 3 showed temporal trends of CS rates in each subgroup by modified Robson classification. Again, there was a significant decline of CS rate in all subgroups in Longhua Hospital, particularly in the Robson class 1 group (from 38.2 to 5.2%). However, the CS rate declined only among women in Robson class 2 and 3 groups in Dongguan, and it even increased in Robson class 4 to 8 groups.
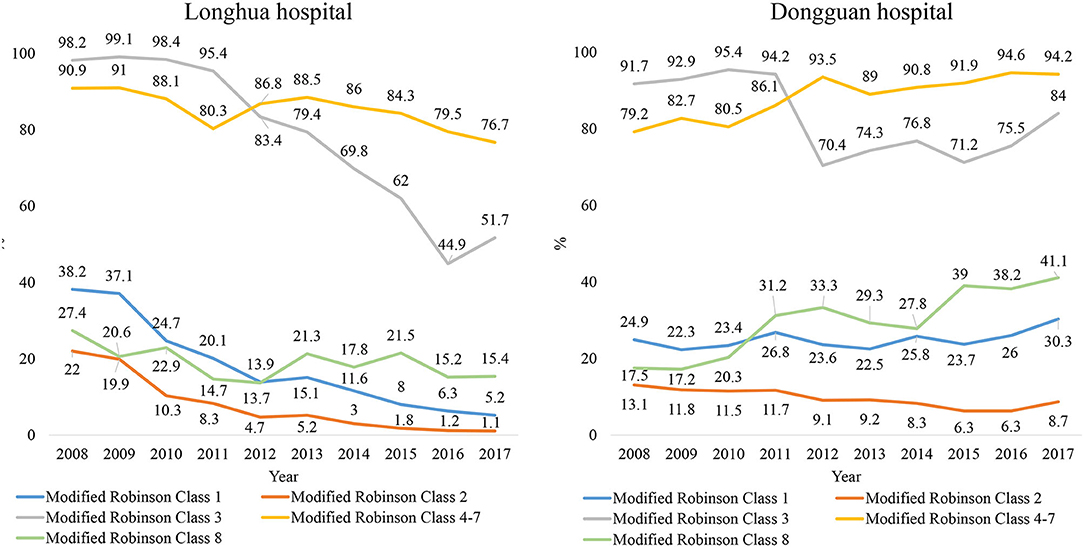
Figure 3. Comparison between Longhua and Dongguan hospitals on trends in CS rate in 10 years from 2008 to 2017, by Robson classification. Robson' class 1: Nulliparous, single, cephalic, ≥37 weeks; Robson's class 2: Multiparous, single, cephalic, ≥37 weeks, without uterine scar; Robson's class 3: Uterine scar, single, cephalic, ≥37 weeks; Robson's class 4–7 (Nulliparous, single, breech/multiparous, single, breech/all multiple pregnancies/all single other abnormal lies; Robson's class 8: All single, cephalic, ≤ 36 weeks.
Number of CS Attributed to Each Subgroup
Figure 4 showed the trends in composition of CS cases by parity and history of CS. In 2008, the composition of CS cases was comparable between the two study hospitals. For example, 55% in Longhua and 47% in Dongguan of CS cases were nulliparous women. Ten years later, the proportion of nulliparous women accounted for only 18% in Longhua but 32% in Dongguan. Analyses in Robson subgroups showed that the proportion for Robson class 1 and 2 groups decreased significantly, while that for other Robson subgroups all increased in Longhua. In Dongguan, the proportion for Robson subgroups showed a similar pattern as that in Longhua except that for Robson class 4–7 group, which remained unchanged (Supplementary Tables 1, 2).
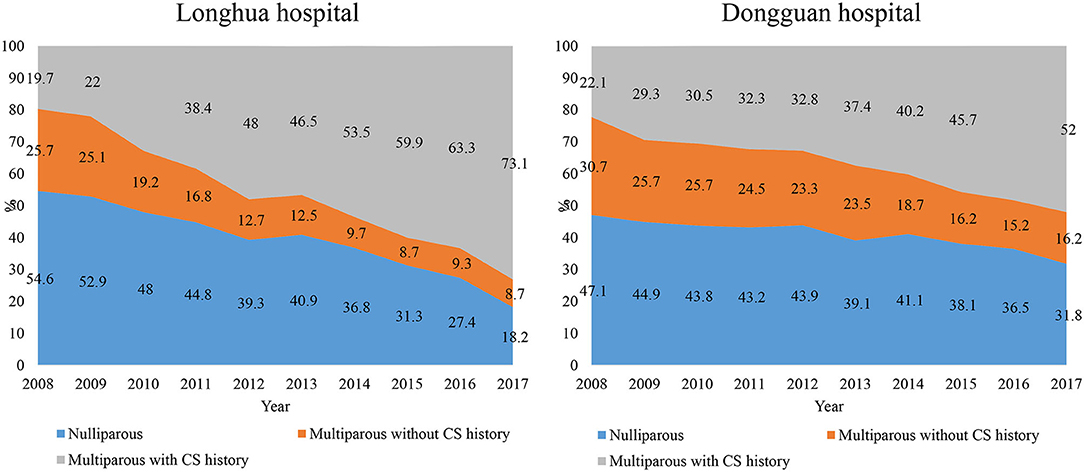
Figure 4. Trends in composition of CS by parity and history of CS in 10 years from 2008 to 2017 in two hospitals.
Reasons for No Trial of Vaginal Trial and Trial Failure
About 20% of women did not try vaginal birth in both the hospitals, but women in Dongguan were more likely due to the women's will (20.0 vs. 11.7%), while women in Longhua were more likely due to scarred uterus and severe complications (Table 4). For those women who tried in Dongguan were more likely to fail (6.7 vs. 2.8%). Among the reasons of the failure, women in Dongguan were twice likely to be called off by the women herself or families (32.2 vs. 14.7%), while women in Longhua were more likely due to abnormal stage of labor.
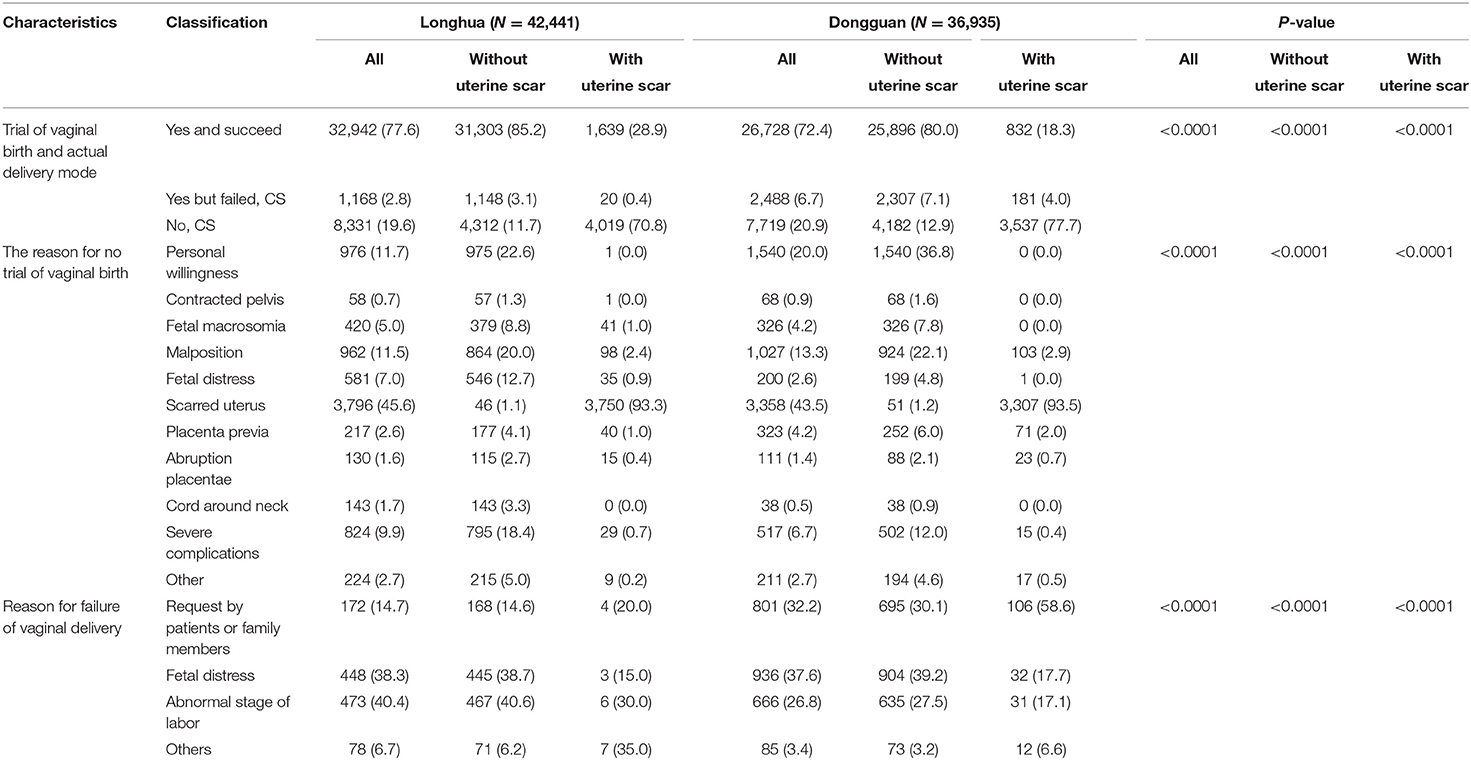
Table 4. Vaginal birth trial and reasons for no trial and trial failure in two hospitals in Guangdong, China.
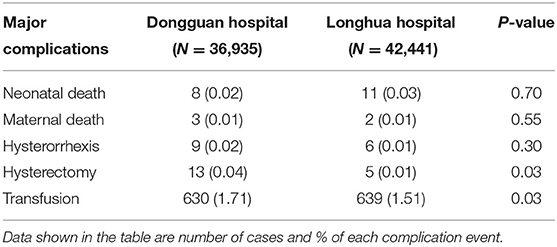
Comparison Between the Two Study Hospitals in Complications
The compatible data of complications showed that there were no differences in number of neonatal and maternal deaths and hysterorrhexis between the two study hospitals. The number of women who experienced hysterectomy and transfusion was slightly higher in Dongguan but with no clinical significance (Table 5).
Discussions
With tremendous efforts, China's national CS rate reduced significantly for about 5% from 2014 to 2016 (8, 10, 11). However, the average CS rate in China was still high, at around 40% (10). There were a lot of doubts that if the WHO's ideal goal of CS rate at 10–15% is achievable. It is particularly challenging for China, because its previous high CS rate and the relaxation of one-child policy would jointly lead to a significantly increased proportion of delivery women with a scar uterus.
Our study chose two typical regional hospitals in China. The CS rate standardized to age, education level, parity, and history of CS in Longhua hospital reduced sharply and steadily since 2010, when the first national policy was issued, from about 35% down to 13% in 2016, when the universal two-child policy was formally implemented. Although it leveled off then but remained well in the ideal range of the WHO-recommended goal. While the standardized rate in Dongguan hospital varied around 25% at the beginning, increased to 36% in 2011, decreased sharply to 27% in 2012, leveled off until 2015 (27.6%), and then bounced back to 35% in 2017. During the 10 years of observation, no difference was found in major maternal complications and neonatal deaths between the two study hospitals.
Under the same national policy, the performance of the two study hospitals governed by two different local health authorities varied significantly, in terms of taking actions to reduce CS rate. This variation matched well with the trend of standardized CS rate in the two hospitals. For example, the obstetric department director in Longhua hospital was personally very supportive to vaginal birth, and hence, immediately started to train the team and promote using midwifery techniques when the first national policy was issued. Empowering midwives to manage midwifery techniques by sequential training session is an effective intervention to reduce the CS rate (17, 18). Midwifery techniques were also recommended in “Implementation plan of the Chinese women and children development guidelines in 2011–2020,” which was issued by Ministry of Health (MOH) in 2012. The local health bureau of Shenzhen, which oversights Longhua hospital, not only put the non-medical CS rate as an indicator for hospital performance appraisal but also spot-checked the indication on quarterly basis. To comply with the local policy, the department director announced the rule that any non-medical CS must be approved before implementation. In contrast, the department director of Dongguan hospital responded to the call of the state to reduce CS through group meetings and communications, and took no more other administrative actions. The CS can increase the comorbidity risks for women and newborns when done without medical indication, and non-indicated CS accounted for the majority of cesarean deliveries (19, 20). Avoiding medically unnecessary CS operations is the effective method to control the high CS rate (20). The director was interested in the technical method to reduce CS among women with a scar uterus and the research program initiated since 2012. Since then, the CS rate also reduced in Dongguan, for about 5%. The local health authority also put the non-medical CS rate as an indicator for hospital appraisal but no site monitoring was carried out.
A detailed analysis supported that Longhua implemented the national and local policies more strictly and followed the clinical guidelines more precisely than Dongguan. For example, although women in both the hospitals had similar proportion (20%) of no-try vaginal birth, women in Dongguan were twice likely due to the women's will (20.0 vs. 11.7%), while women in Longhua were more likely due to scarred uterus and severe complications. For those women who tried in Dongguan were more likely to fail (6.7 vs. 2.8%). Among the reasons of the failure, women in Dongguan were twice likely to be called off by the women herself or families (32 vs. 15%), while women in Longhua were more likely due to abnormal stage of labor.
The women who gave birth in these two hospitals were comparable in terms of the proportion with Robson classification 3 and above and proportion with age over 35. Besides, the proportion of multiparous women with a scar uterus increased rapidly in both the hospitals and at the same pace, from about 7% in 2008 to 20% in 2017. These proportions are consistent with those found through NMNMSS (10). The repeat CS is clearly a new challenge for the reduction of CS rate in China. As shown in our study, the proportion of CS cases attributed to Robson class 3 (single, cephalic, ≥37 weeks of gestation with uterine scar) increased from 19 to 55% over the 10 years. To achieve the reduction in CS rate, vaginal birth after CS (VBAC) has been encouraged in the two hospitals since 2012, and the repeat CS rate dropped by half in Longhua and by about 6% in Dongguan. We estimated that about 6% absolute reduction in overall CS rate in Longhua and about 1% absolute reduction in Longhua was attributed to the dramatic reduction of the repeat CS. In comparison with the two hospitals, the weighted rate of VBAC in China was only 9.6% between 2012 and 2016 according to NMNMSS data (12). That will translate to only 2% reduction in the overall CS rate reduction. The low VBAC rate was believed due to concerning the risk of complications associated with VBAC. Our team previously reported a relatively high success rate of VBAC (84%) along with a low incidence of serious complications (0.3% uterine rupture) (21). VBAC was proved to be an accepted practice and contributed to reducing repeat CS in many countries (22, 23). We believe the expert consensus on implementing VBAC issued by the Chinese Society of Obstetrics and Gynecology in 2016 would help to promote VBAC to a larger scale in China (24). It will be interesting to keep looking on the trends in VBAC use at the country level after the expert consensus issued (25).
Besides the efforts on the reduction of repeat CS, Longhua also made a lot to reduce CS among nulliparous women as well as multiparous women without the history of CS. We found various reasons for these high CS rate in China, and for the variations among the hospitals, and sometimes even in the same cities. In different hospitals, one can find different populations, which explain the differences; these cannot be explained by the modified Robson classification. The reasons underling CS decision-making are complex, involving pregnant women, their families, health-care providers (fear of the obstetricians from possible lawsuits), and contextual factors. A systematic review reported that women preferred CS due to perceived consequences of vaginal delivery or fear of pain during labor (26, 27). In our study, personal willingness was the leading cause for CS except for scarred uterus, and more than one quarter of CS were required by patients or family members after trying vaginal birth. Health education that aimed to increase knowledge on the advantages of vaginal birth should be strengthened through an intensive publicity campaign. The proportion of women with over 9 years of education was significantly higher in Longhua; this may also explain why CS rate reduction in all subgroups in Longhua was more apparent, comparing with its counterpart.
The impact of full relaxation of the one-child policy in China was generally negative and increased the CS rate in all women in Dongguan after 2015. In Longhua, the CS rate also increased in multiparous women with a scar uterus, leveled off in multiparous women without a scar uterus, and kept decreasing in nulliparous women. Again, it should represent the differences in the two hospitals in implementing the national policy on CS reduction, but it might also reflect the increase of women with older age for the second delivery due to the relaxation of one-child policy. A recent report of national database also indicated the same trend after universal two-child policy was issued in 2015 (10).
Our study has several limitations. First, the study included only two hospitals and should not represent all hospitals in China. In particular, both Shenzhen and Dongguan are economically developed cities, and many of the study participants in these two hospitals were immigrants. However, we believe that the successful experiences from Longhua should be applicable to other hospitals in mainland China, if the actions and local policies that were taken by Longhua hospital and the Shenzhen health authority for strict implementation of the national policies and clinical guidelines/consensus could be replicated. Considering the geography and population size, it may still require a long time to achieve the WHO's goal nationwide in China. How the policies are implemented elsewhere in China is unknown. Whether the Longhua experiences are generalizable to other hospitals in other part of the world remain to be proved, though it does not hurt the comparability between the participants from the two hospitals. Second, since we were unable to separate women who had spontaneous labor from those who had CS before labor or delivered after induction, we used the modified Robson classification for our analysis. Because these groups account only small proportion of all delivery women, it should not affect our study results significantly. Finally, the participants came from different hospitals and there were significant differences in certain demographic and clinical characteristics, leading to the inevitable confounding bias. To control these important potential confounding biases, we compared the trend of CS rate over 10 years in the two hospitals by standardizing the CS rate with age, education level, parity, CS history, and Robson classification.
Conclusions
Our study demonstrated that the ideal goal recommended by the WHO for CS reduction is achievable in China, without increase in major maternal complications and neonatal deaths. The execution ability of local governments and hospitals, and the obstetric department director in particular in implementing the national policies and clinical guidelines played a critical role for the success. These important and valuable national policies should be persistently promoted and supervised around the country, including midwifery techniques training and non-medical CS approval (obligatory documented second opinion before any operation except for obvious emergencies).
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by the Institutional Review Boards of The First Dongguan Affiliated Hospital of Guangdong Medical University. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author Contributions
Y-JJ, H-BW, Y-XL, Y-FW, and HY contributed to the development of the study protocol and took responsibility for the accuracy of the data analysis. Y-JJ, H-BW, and Y-XL were the principal investigators and managed the protocol. Y-JJ, H-BW, ZB, D-JL, KM, JY, Y-XL, Y-FW, and HY were involved in the initial draft of the manuscript. H-BW was responsible for data management and statistical analysis. All authors had full access to all of the data in the study, critically revised the manuscript for important intellectual content, and gave approval for final manuscript.
Funding
The study was funded by Guangdong Provincial Science and Technology Plan (2017A020214007) and Dongguan Technology Development Society (201950715032188).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We wish to thank the project staffs for their efforts in the study. We also wish to thank the subjects for theirparticipation.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2021.774487/full#supplementary-material
Abbreviations
CS, cesarean sections; WHO, World Health Organization; VBAC, vaginal birth after CS; cOR, crude odds ratio; CMCHA, China Maternal and Child Health Association; MOH, Ministry of Health; NHFPC, National Health and Family Planning Commission; CSOG, Chinese Society of Obstetrics and Gynecology; SC, State Council; NMNMSS, National Maternal Near Miss Surveillance System.
References
1. Blustein J, Liu J. Time to consider the risks of caesarean delivery for long term child health. BMJ. (2015) 350:h2410. doi: 10.1136/bmj.h2410
2. Belizan JM, Minckas N, McClure EM, Saleem S, Moore JL, Goudar SS, et al. An approach to identify a minimum and rational proportion of caesarean sections in resource-poor settings: a global network study. Lancet Glob Health. (2018) 6:e894–901. doi: 10.1016/S2214-109X(18)30241-9
3. Althabe F, Belizan JM. Caesarean section: the paradox. Lancet. (2006) 368:1472–3. doi: 10.1016/S0140-6736(06)69616-5
4. Betran AP, Torloni MR, Zhang JJ, Gulmezoglu AM, WHO Working Group on Caesarean Section. WHO Statement on Caesarean Section Rates. BJOG. (2016) 123:667–70. doi: 10.1111/1471-0528.13526
5. Boerma T, Ronsmans C, Melesse DY, Barros AJD, Barros FC, Juan L, et al. Global epidemiology of use of and disparities in caesarean sections. Lancet. (2018) 392:1341–8. doi: 10.1016/S0140-6736(18)31928-7
6. Vogel JP, Betran AP, Vindevoghel N, Souza JP, Torloni MR, Zhang J, et al. Use of the Robson classification to assess caesarean section trends in 21 countries: a secondary analysis of two WHO multicountry surveys. Lancet Glob Health. (2015) 3:e260–70. doi: 10.1016/S2214-109X(15)70094-X
7. The L. Stemming the global caesarean section epidemic. Lancet. (2018) 392:1279. doi: 10.1016/S0140-6736(18)32394-8
8. Li HT, Luo S, Trasande L, Hellerstein S, Kang C, Li JX, et al. Geographic variations and temporal trends in cesarean delivery rates in China, 2008-2014. JAMA. (2017) 317:69–76. doi: 10.1001/jama.2016.18663
9. Lumbiganon P, Laopaiboon M, Gulmezoglu AM, Souza JP, Taneepanichskul S, Ruyan P, et al. Method of delivery and pregnancy outcomes in Asia: the WHO global survey on maternal and perinatal health 2007-08. Lancet. (2010) 375:490–9. doi: 10.1016/S0140-6736(09)61870-5
10. Liang J, Mu Y, Li X, Tang W, Wang Y, Liu Z, et al. Relaxation of the one child policy and trends in caesarean section rates and birth outcomes in China between 2012 and 2016: observational study of nearly seven million health facility births. BMJ. (2018) 360:k817 doi: 10.1136/bmj.k817
11. Liu X, Lynch CD, Cheng WW, Landon MB. Lowering the high rate of caesarean delivery in China: an experience from Shanghai. BJOG. (2016) 123:1620–8. doi: 10.1111/1471-0528.14057
12. Mu Y, Li X, Zhu J, Liu Z, Li M, Deng K, et al. Prior caesarean section and likelihood of vaginal birth, 2012-2016, China. Bull World Health Organ. (2018) 96:548–57. doi: 10.2471/BLT.17.206433
13. Zeng Y, Hesketh T. The effects of China's universal two-child policy. Lancet. (2016) 388:1930–8. doi: 10.1016/S0140-6736(16)31405-2
14. Kang L, Ye S, Jing K, Fan Y, Chen Q, Zhang N, et al. A segmented logistic regression approach to evaluating change in Caesarean section rate with reform of birth planning policy in two regions in China from 2012 to 2016. Risk Manag Healthc Policy. (2020) 13:245–53. doi: 10.2147/RMHP.S230923
16. Robson M, Hartigan L, Murphy M. Methods of achieving and maintaining an appropriate caesarean section rate. Best Pract Res Clin Obstet Gynaecol. (2013) 27:297–308. doi: 10.1016/j.bpobgyn.2012.09.004
17. Sandall J, Hatem M, Devane D, Soltani H, Gates S. Discussions of findings from a Cochrane review of midwife-led versus other models of care for childbearing women: continuity, normality and safety. Midwifery. (2009) 25:8–13. doi: 10.1016/j.midw.2008.12.002
18. Zahumensky J, Psenkova P, Dolezal P, Otapkova P, Papcun P, Ferianec V, et al. Impact of implementing a multifaceted intervention to reduce rates of cesarean section: A quality-improvement study. Int J Gynaecol Obstet. (2020) 151:244–8. doi: 10.1002/ijgo.13345
19. Zahroh RI, Disney G, Betran AP, Bohren MA. Trends and sociodemographic inequalities in the use of caesarean section in Indonesia, 1987-2017. BMJ Glob Health. (2020) 5:3844. doi: 10.1136/bmjgh-2020-003844
20. Song C, Xu Y, Ding Y, Zhang Y, Liu N, Li L, et al. The rates and medical necessity of cesarean delivery in China, 2012-2019: an inspiration from Jiangsu. BMC Med. (2021) 19:14. doi: 10.1186/s12916-020-01890-6
21. Li YX, Bai Z, Long DJ, Wang HB, Wu YF, Reilly KH, et al. Predicting the success of vaginal birth after caesarean delivery: a retrospective cohort study in China. BMJ Open. (2019) 9:e027807. doi: 10.1136/bmjopen-2018-027807
22. Smith GC, Pell JP, Cameron AD, Dobbie R. Risk of perinatal death associated with labor after previous cesarean delivery in uncomplicated term pregnancies. JAMA. (2002) 287:2684–90. doi: 10.1001/jama.287.20.2684
23. Richardson BS, Czikk MJ, daSilva O, Natale R. The impact of labor at term on measures of neonatal outcome. Am J Obstet Gynecol. (2005) 192:219–26. doi: 10.1016/j.ajog.2004.06.034
24. Obstetrics Subgroup Chinese Society of Obstetrics Gynocology Association. CM. [Consensus of management of vaginal birth after cesarean (2016)]. Zhonghua Fu Chan Ke Za Zhi. (2016) 51:561–4. doi: 10.3760/cma.j.issn.0529-567X.2016.08.001
25. Chen Y, Wang C, Shang H, Yang K, Norris SL. Clinical practice guidelines in China. BMJ. (2018) 360:j5158. doi: 10.1136/bmj.j5158
26. Long Q, Kingdon C, Yang F, Renecle MD, Jahanfar S, Bohren MA, et al. Prevalence of and reasons for women's, family members', and health professionals' preferences for cesarean section in China: A mixed-methods systematic review. PLoS Med. (2018) 15:e1002672. doi: 10.1371/journal.pmed.1002672
Keywords: health policy, policy implementation, China, cesarean section rate, one-child policy
Citation: Ji Y-J, Wang H-B, Bai Z, Long D-J, Ma K, Yan J, Li Y-X, Wu Y-F and Yang H (2021) Achieving WHO's Goal for Reducing Cesarean Section Rate in a Chinese Hospital. Front. Med. 8:774487. doi: 10.3389/fmed.2021.774487
Received: 12 September 2021; Accepted: 15 October 2021;
Published: 22 November 2021.
Edited by:
Andrea Tinelli, Moscow Institute of Physics and Technology, RussiaReviewed by:
Liping Feng, Duke University, United StatesQihui Chen, China Agricultural University, China
Michael Stark, New European Surgical Academy (NESA), Germany
Martina Licchelli, Ospedale I. Veris Delli Ponti, Italy
Copyright © 2021 Ji, Wang, Bai, Long, Ma, Yan, Li, Wu and Yang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yun-Xiu Li, bHl4aG9uZ2ZhQDE2My5jb20=; Yang-Feng Wu, d3V5ZkBiam11LmVkdS5jbg==; Huixia Yang, eWFuZ2h1aXhpYUBiam11LmVkdS5jbg==
†These authors share first authorship
 Yan-Jie Ji1†
Yan-Jie Ji1† Hai-Bo Wang
Hai-Bo Wang Yang-Feng Wu
Yang-Feng Wu Huixia Yang
Huixia Yang