- Department of Geriatrics, China National Clinical Research Center for Geriatric Medicine, Xuanwu Hospital, Capital Medical University, Beijing, China
Background: Physical function gradually decreases with age in older adults, affecting their independence and quality of life and leaving them prone to adverse outcomes. Despite the importance of assessing function for older adults, most studies have focused on disability and paid less attention to functional impairment. Thus, given the lack of valid and practical methods for evaluating functional impairment for older adults, we developed the function impairment screening tool (FIST) using the Delphi method.
Objective: This study aimed to evaluate the reliability and validity of the FIST in Chinese older adults.
Methods: A total of 489 participants aged 60 years or older, and who had completed the FIST were included. A subgroup of 50 participants completed the FIST a second time, 1 week after the first round, and the test–retest reliability was evaluated using the intraclass correlation coefficient (ICC). Reliability was tested using Cronbach's alpha. Validity was examined using exploratory factor analysis. Criterion-related validity was assessed using correlations between the FIST and the Barthel Index activities of daily living (ADL), Lawton, and Brody instrumental activities of daily living (LB-IADL).
Results: The Cronbach's alpha coefficient for the FIST was 0.930 (P < 0.001). The test–retest reliability was good, with an ICC of 0.928 (95% confidence interval [0.874, 0.960]). Exploratory factor analyses revealed one factor accounting for 60.14% of the scale's variance and the load values of every item were >0.4 (0.489–0.872). The correlation coefficient was 0.572 (P < 0.001) between the FIST score and ADL, and was 0.793 (P < 0.001) between the FIST score and IADL. The FIST score was positively correlated with walking speed (r = 0.475, P < 0.001) and grip strength (r = 0.307, P < 0.001), and negatively correlated with age (r = −0.588, P < 0.001) and Fried frailty phenotype (r = −0.594, P < 0.001).
Conclusion: The FIST is a reliable and valid instrument for assessing physical function impairment in older adults.
Introduction
Physical function gradually decreases with age in older adults, affecting their independence and quality of life, leaving older adults more vulnerable to adverse outcomes such as falls, hospitalization, and death (1–3). Declining function increases the cost of public healthcare systems and imposes the burden of additional care on families (4). In 2020, the Chinese population aged 60 or above was 264.02 million, accounting for 18.7% of the country's total population (5). Currently, China faces an enormous healthcare challenge. The World Health Organization (WHO) defined “healthy aging” as a process of maintaining functional ability to enable wellbeing in older age (6). The disease concept is increasingly being replaced by the concept of functional consequences in geriatric medicine (7). The original conceptual model on disability was proposed by Nagi. In his model, disability was defined as having problems in activities of daily life (ADL) (8). In 2001, WHO redefined disability by the International Classification of Functioning, Disability, and Health (ICF). Disability is an umbrella term, involving impairments, activity limitations, and participation restrictions (9). WHO developed Disability Assessment Schedule-3.6 for assessing disability which had very good psychometric properties (10). The frequently used tools for disability were Barthel Index (BI), Lawton and Brody instrumental activities of daily living (LB-IADL), and Katz Index (KI) (11). Physical function encompasses all body functions, activities, and participation (12). Physical function impairment is generally considered to occur earlier in the process of disability (13). Early identification and intervention are of great importance. Therefore, it is especially important to assess the functional status of older adults, as interventions for function impairment can prevent or delay the occurrence of disability and adverse events and promote healthy aging.
However, most previous studies have focused on disability (14–16), while paying less attention to the early stage of disability, that is, functional impairment. This may be attributable to the lack of valid tools to assess functional impairment in older adults. Though there were basic activities of daily living (BADL) and IADL for evaluating the performance in activities of daily living, but the BADL and IADL had low sensitivity for detecting mild function deficits. The advanced activities of daily living (AADL) can assess more complex functional performance, but some items of AADL were not suited to Chinese older adults; go to church, for example (17). We developed the function impairment screening tool (FIST) for Chinese older adults using the Delphi method (18, 19).
The FIST contains 16 items, divided into three domains: ability to perform activities of daily living, ability to engage in domestic life, and ability to engage in social activities (19). The FIST is a self-reported questionnaire, and it is low-cost and easy to use. Meanwhile, the FIST meets the definition of physical function, while avoiding the ceiling effect. However, there has been no formal psychometric evaluation of the FIST. This study aimed to evaluate the validity and reliability of the FIST in Chinese older adults.
Methods
Participants
Participants aged 60 years or older were recruited from the inpatient department at the Department of Geriatrics at Xuanwu Hospital, Capital Medical University. Exclusion criteria included a Mini-Mental State Exam (MMSE) score <23 (20) and a BI score <40. Based on the criteria, 500 older adults were enrolled in the study. The study was approved by the Ethics Committee of Xuanwu Hospital Capital Medical University, and was registered, number: ChiCTR1900028382. All participants agreed to be included in the study and provided their written informed consent before participation.
Data Collection
Demographic characteristics and history of chronic diseases were collected for all participants by geriatricians or postgraduate students. All of the data gatherers were trained using standardized procedures on assessment a week before the study. ADL and IADL were assessed using the BI (21) and LB-IADL (22), respectively. Cognitive function was assessed via MMSE (20). We assessed frailty using the Fried frailty phenotype including weakness, slowness, exhaustion, inactivity, and weight loss (23). Weakness was assessed by measuring the dominant maximal grip strength according to standardized procedures. We used a hand dynamometer (EH101; Camry, Guangdong Province, China) to measure the grip strength. Participants sat in an upright position with the arm in adduction and the elbow flexed at 90 degrees (24). Two tests were carried out for the dominant hand, with a 1-min interval between two tests. We recorded the maximal grip strength of the two tests. Slowness was assessed by performing the 4-m walking test. A 4-m line was marked on the ground, and participants were asked to walk at their usual speed. Every participant was tested twice, and the shorter time was recorded (25). The cutoff values for grip strength and walking speed were derived from previous reports in Chinese older populations (26, 27). The total score of the Fried frailty phenotype is 5. Older adults with a score ≥ 3 were classified as “frail,” those with 0 were considered “robust,” and scores 1–2 indicated “prefrail.”
Function Impairment Screening Tool
The FIST is a self-report questionnaire for assessing physical function in older adults. The FIST contains 16 items, divided into three domains: ability to perform activities of daily living (including eating, washing, going to toilet, dressing, moving in and out of bed, and bathing), ability to engage in domestic life (including housekeeping, handling finances, handing medications, lifting 5 kg of weight, and up and down stairs), and ability to engage in social activities (including using transportation, shopping, walking for 250 m, using telephone, and physical exercise) (19). Each item has three levels—independence, partial dependence, and complete dependence—and is scored as 1, 0.5, and 0, respectively. The total score range for all 16 questions is 0 to 16; higher score indicates better physical function (19).
Statistical Analysis
The data were analyzed using SPSS version 19.0 (SPSS Inc., Chicago, IL, USA). The figures were drawn using GraphPad Prism version 7.0 software (GraphPad Software Inc., CA, USA). Quantitative variables were described as mean with standard deviation (±SD), and categorical variables were described as the number with percentages (%). The overall scale reliability was tested using Cronbach's alpha coefficient. Meanwhile, we also calculated item-to-total correlations (ITTC) the split-half coefficient, and the Guttman split-half coefficient. Internal Consistency Reliability and split-half testing measure reliability. The ITTC is a measure of the reliability of a multi-item scale and evaluates the correlation between an individual item and the total score without that item. An acceptable value should be >0.50 (28). Total score test–retest reliability was assessed by two-way random intraclass correlation coefficients (ICC) for absolute agreement. An indication of good reliability was values of ICC ≥ 0.7, and excellent reliability was indicated by ICC ≥ 0.9 (29). We also plotted the difference of scores between the test–retest measures using the Bland and Altman plot (30). The Bland and Altman plot is a graphical method to evaluate a bias and compare two measurements of the same variable. The construct validity was calculated by exploratory factor analysis (EFA). The EFA was run using the principal components analysis. The number of factors retained was based on the scree test (31, 32). An item was retained if its factor loading was >0.40. As the total score of FIST was non-normal distribution, the criteria validity of the FIST was measured using Spearman's correlation coefficient with the FIST and ADL, IADL scores. The absolute value of Spearman's correlation coefficient was used, for which <0.5, >0.7, and 0.5–0.7 mean weak correlation, strong correlation, and moderate correlation, respectively (33). Furthermore, we calculated the correlation between FIST score and age, physical performance, and physical frailty for exploring some related factors. All statistical tests were two-tailed, and a P of <0.05 was considered statistically significant.
We calculated sample size using subject-to-item ratios, allowing for a minimum of a 20:1 subject-to-item ratio (34). The minimum sample size was 320 subjects with a total of 16 items. The number of participants was greater than the number required (34, 35). We calculated the sample size of test–retest based on the COSMIN standards (36). We set an ICC value of 0.85 as a priori for the optimal target level of reliability. The minimal sample size was 35 and was calculated using two repeated measures with a confidence interval (CI) of 0.2. We evaluated the test–retest reliability with 50 older adults, which was greater than the above minimal sample size (37).
Results
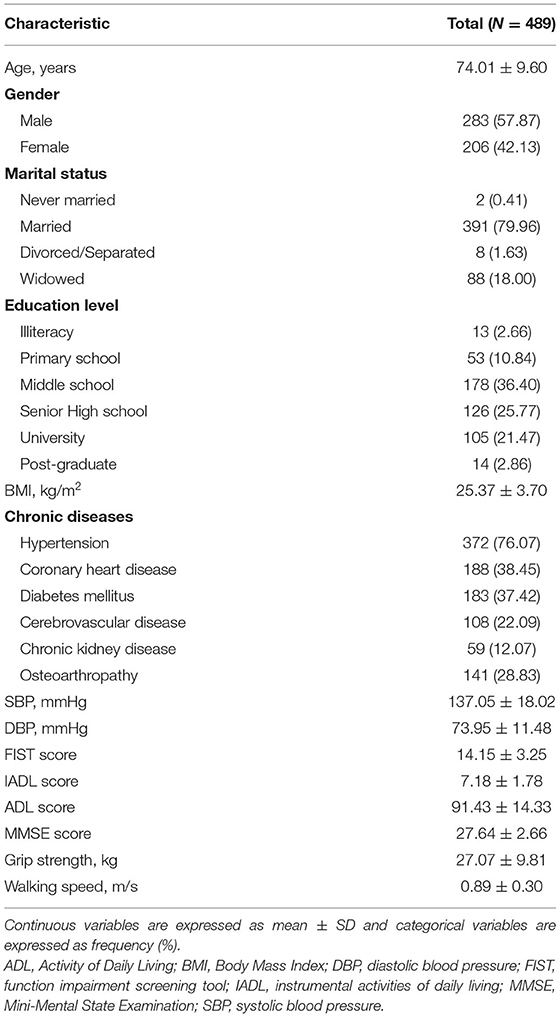
In total, 500 participants were enrolled from Jan 2020 to Mar 2021, 11 older adults declined to participate. A total of 489 older participants were included in the final analysis. The average age of participants was 74.01 (±9.60) years. Two hundred eighty-three (57.87%) of the participants were male. The mean FIST total score for all of the participants was 14.15 (±3.25). The mean ADL and IADL scores were 91.43 (±14.33) and 7.18 (±1.78), respectively. The mean values of grip strength and walking speed were 27.07 (±9.81) kg and 0.89 (±0.30) m/s, respectively. The demographic characteristics and chronic disease data of the participants are shown in Table 1.
Reliability
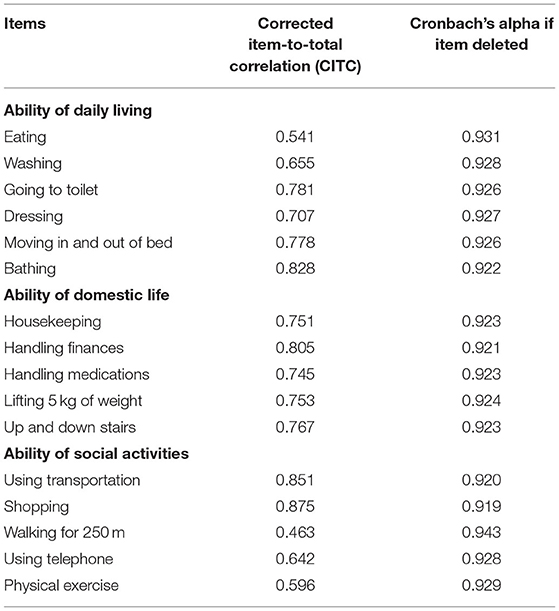
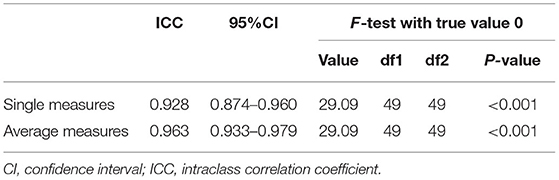
We calculated the internal consistency reliability using the Cronbach coefficients. The Cronbach's alpha coefficient of the FIST total score was 0.930 (Table 2), and the split-half coefficient and Guttman split-half coefficient were 0.924 and 0.881, respectively (Table 3). A subgroup of 50 participants completed the FIST a second time after 1 week. The two-way random ICC test–retest reliability was 0.928 (P < 0.001; Table 4). The mean change of FIST scores and its 95% CI between test and retest were presented in the Bland–Altman plot (Figure 1).
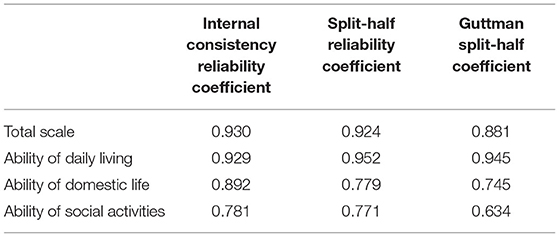
Table 3. Internal consistency reliability and split-half reliability of the FIST scale and each factor.
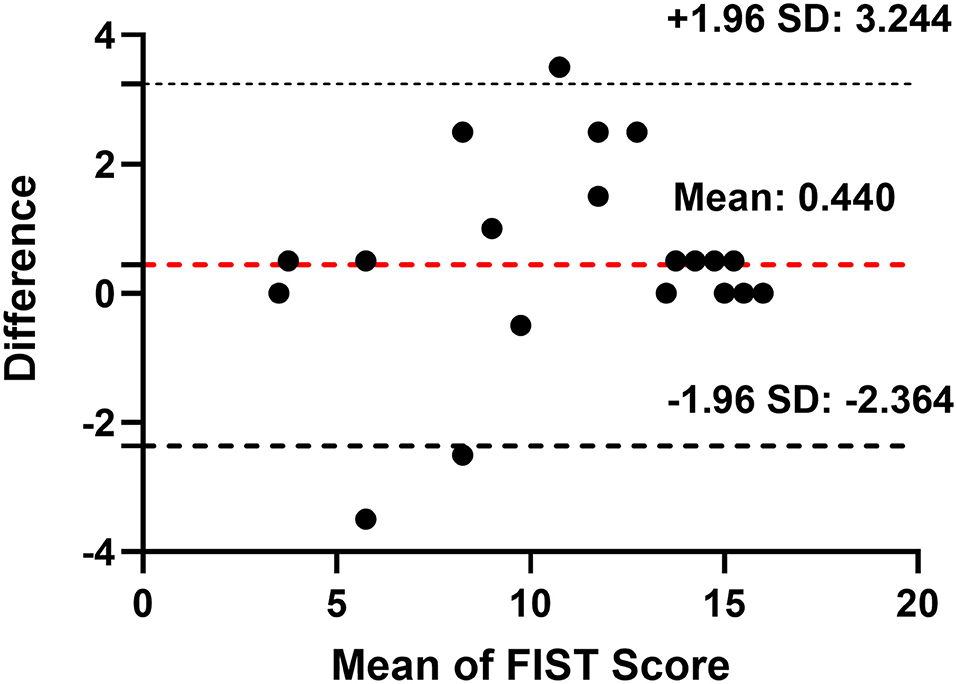
Figure 1. Bland-Altman plot: mean change of FIST scores between test and retest and its 95% confidence interval (CI). Red dotted lines indicate the mean change of FIST scores and black dotted lines indicate two standard deviations of the mean difference. SD, standard deviation.
Validity
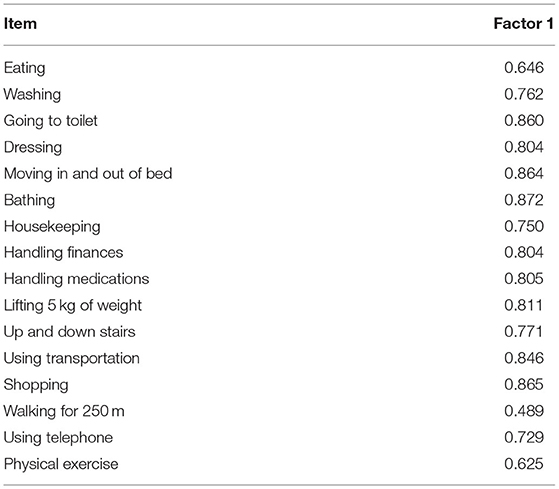
Exploratory factor analysis was used to calculate construct validity. The Kaiser–Meyer–Olkin (KMO) measure of sampling adequacy was 0.917, and the Bartlett's test of sphericity (BTS) was 7,904.477 (P < 0.001), which indicated that the data were suitable for factor analysis. Exploratory factor analyses revealed one factor accounting for 60.14% of the scale's variance, and the load values of every item were >0.4 (0.489–0.872; Table 5).
Criterion-related validity was assessed by Spearman's correlation between the FIST and ADL, IADL. The correlation coefficient was 0.572 (P < 0.001) between the FIST scores with ADL and 0.793 (P < 0.001) between the FIST scores and IADL (Figure 2). Based on the absolute value of Spearman's correlation coefficient, the FIST had a moderate correlation with ADL and a strong correlation with IADL.
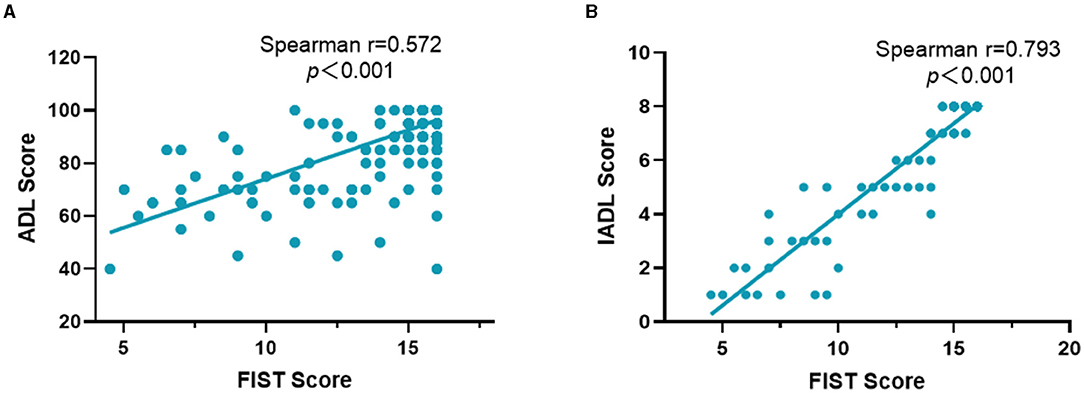
Figure 2. The Spearman's correlation between the FIST and ADL (A), IADL (B). ADL, the activities of daily living; FIST, function impairment screening tool; IADL, instrumental activities of daily living.
Figure 3 shows the correlation between the FIST score with age, physical performance, and physical frailty. The FIST score was positively correlated with walking speed (r = 0.475, P < 0.001) and grip strength (r = 0.307, P < 0.001) and negatively correlated with age (r = −0.588, P < 0.001) and the Fried frailty phenotype (r = −0.594, P < 0.001; Figure 3).
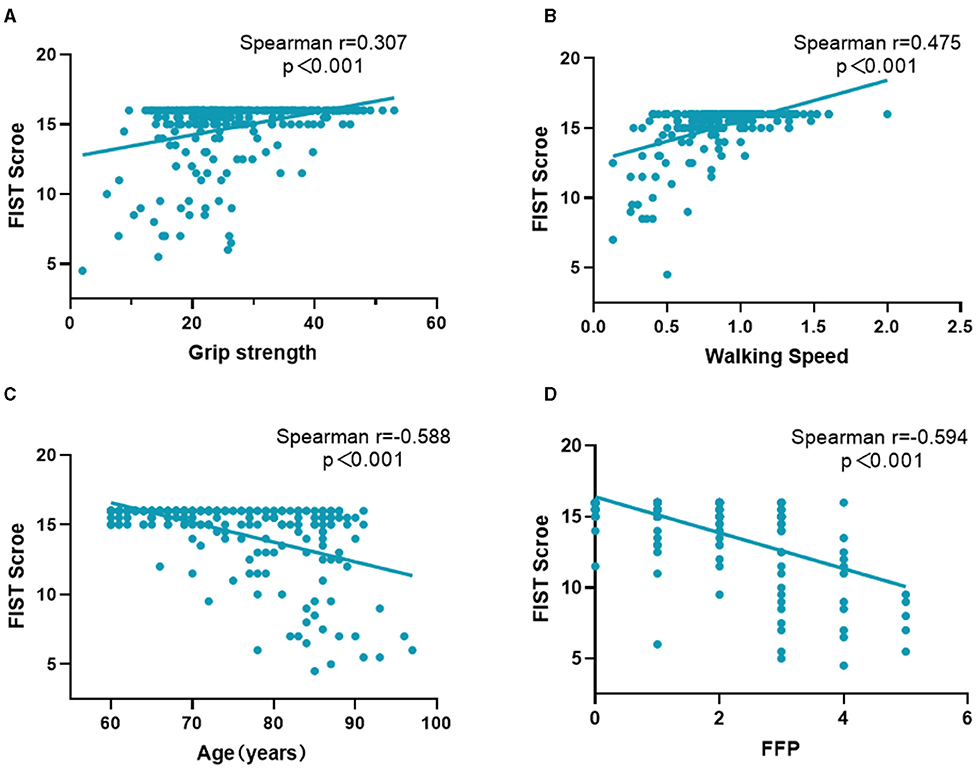
Figure 3. The Spearman's correlation between the FIST score and age, physical performance, physical frailty. (A) Describes the correlation between the FIST score and grip strength; (B) Describes the correlation between the FIST score and walking speed; (C) Describes the correlation between the FIST score and age; (D) Describes the correlation between the FIST score and the Fried frailty phenotype. FFP, the Fried frailty phenotype; FIST, function impairment screening tool.
Discussion
To evaluate the physical functional status in Chinese older adults, we developed the FIST using the Delphi method. The present study validated the new tool in Chinese older adults and showed that FIST was a reliable instrument to assess physical function impairment.
We previously developed a scale item pool based on a literature review and formed a preliminary scale through a two-round Delphi expert consultation (18). Next, the preliminary scale was used with older participants, and the FIST scale was developed using classical statistical methods (19). The FIST scale contains 16 items that belong to three domains of functional ability (ability to perform activities of daily living, ability to engage in domestic life, and ability to engage in social activities).
The instrument's reliability is the degree of measurement accuracy, and we evaluated the reliability of the FIST in three ways: internal consistency reliability, split-half reliability, and test–retest reliability. The internal consistency reliability and split-half reliability of the FIST were excellent. The Cronbach's alpha for the FIST was 0.930, and the split-half reliability was 0.924, meeting the recommended value range 0.70–0.95 (29, 38). These results were similar to those of other functional instruments. The internal consistency for the AADL overall scale was 0.80 in older adults in Brazil (17). The Cronbach's alpha coefficient of the Frenchay Activities Index was 0.83 in non-stroke older participants, 0.78 in pre-stroke participants, and 0.87 in post-stroke participants (39). Internal consistency reliabilities for the functional status questionnaire six subscales (basic ADL, intermediate ADL, mental health, work performance, social activity, quality of interaction) ranged from 0.64 to 0.82 in 1,153 outpatients (40). The test–retest reliability of the FIST scale was 0.928, which exceeded the recommendation (>0.75) (29, 41). The retest result was an ICC of 0.928, indicating that the FIST was stable. Thus, the FIST scale shows good reliability.
Exploratory factor analysis showed that FIST has good construct validity; the factor loading values of the 16 items were all >0.40, and the contribution rate of a common factor was 60.14%. In the exploratory factor analysis, according to the scree test, we retained one factor that variance contribution rate was 60.074% that was different from the three domains of the FIST. But the load values of each item were >0.4. No item was deleted according to the statistical analysis. As our participants were older inpatients, they had worse functional status than community-dwelling older adults. The FIST should be further refined in the future and verified in different populations, especially community-dwelling older adults. Meanwhile, we also evaluated the criterion validity. There is no gold standard for functional impairment, so we analyzed the correlation coefficients between the FIST and ADL, IADL, which showed that the FIST has a moderate correlation with ADL and a strong correlation with IADL.
A previous study showed that the Groningen activity restriction scale (GARS) and the modified Reintegration to Normal Living Index were reliable and valid tools for use in older adults both in hospital and community (42). GARS contained 11 ADL items and 7 IADL items (43). Compared with GARS, the FIST scale includes not only ADL and IADL items but also items regarding social activities.
With advancing age, physical function gradually deteriorates, age was a significant predictor of functional decline (44). Our results showed that the FIST score was negatively correlated with age. Frailty is a geriatric syndrome that increases vulnerability, and it is related to a series of adverse outcomes including falls, disability, and mortality (45, 46). Our results revealed that the FIST was negatively associated with frailty. However, the function impairment was different from frailty, although some items of FIST were similar to frailty. The FIST contains not only ability in daily living but also ability in domestic life and social activities.
Both muscle mass and muscle strength decreased gradually with aging, and strength declined faster than mass (47). Muscle strength and mobility ability are important components of physical performance. Walking speed is an objective measure of physical performance. Our study showed the FIST score was positively correlated with walking speed and grip strength. Several studies have reported that walking speed was associated with risks of functional dependence and disability (48–52). Furthermore, a 6-year follow-up study found that walking speed can predict the onset of functional dependence in rural older adults (48). Another study with 4.4 years follow-up found that Japanese community-dwelling older adults with faster walking speed had decreased risks of disability (adjusted hazard ratio [HR]: 0.87, 95% CI: 0.82–0.93) (49). Furthermore, slow walking speed increased the risk of future disability in frail (adjusted HR: 4.68, 95% CI: 2.72–8.05) and prefrail older adults (adjusted HR: 3.62, 95% CI: 2.19–5.96) (50). Muscle strength is also important to maintain physical function. Greater handgrip strength was associated with decreasing onset of ADL disability and IADL disability (51, 52). Thus, the FIST may reflect physical function. The diagnosis of sarcopenia, a progressive and generalized skeletal muscle disorder, includes the assessment of muscle strength, muscle mass, and physical performance (53, 54). Although the FIST score is positively correlated with muscle strength in the present study, the functional impairment is different from sarcopenia. If muscle strength is below the reference values, sarcopenia would be suspected, and the next diagnosis procedure would include the measurement of muscle mass (55).
Limitations
This study has several limitations. First, the participants were from a single-center general hospital in Beijing and did not provide a broad representation of all older adults in China. Further multi-center studies are warranted. Second, this is a cross-sectional study, and therefore the predictive validity of the FIST was not determined. Third, the assessment was conducted by several staff members, so measurement bias may have occurred; however, all the staff were trained using the same procedures to minimize the bias.
Conclusion
This study provided the validity and reliability evidence of the FIST. The results showed that the FIST is a reliable and valid instrument for assessing physical functional impairment in Chinese older adults. In addition, the assessment of function impairment in the early stage of disease could reduce the adverse outcome and improve the quality of life among older adults.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Ethics Committee of Xuanwu Hospital Capital Medical University. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
YuL and LM contributed to conception and design of the study. PL, YP, YiL, and LZ organized the database. YZ performed the statistical analysis and wrote the manuscript. All authors contributed to manuscript revision, read, and approved the submitted version.
Funding
This work was supported by National Key R&D Program of China (2018YFC2002101 and 2018YFC2002100) and Beijing Municipal Health Commission (Jing2019-2).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We wish to acknowledge Yu Song, Ou Zhao, Bixi Li, Yumeng Chen, Tong Ji, Shijie Li, and Yaru Zhou for their assistance in data collection. We acknowledge all the participants for their contributions.
References
1. Grande G, Vetrano DL, Fratiglioni L, Marseglia A, Vanacore N, Laukka EJ, et al. Disability trajectories and mortality in older adults with different cognitive and physical profiles. Aging Clin Exp Res. (2020) 32:1007–16. doi: 10.1007/s40520-019-01297-1
2. Vetrano DL, Rizzuto D, Calderón-Larrañaga A, Onder G, Welmer AK, Qiu C, et al. Walking speed drives the prognosis of older adults with cardiovascular and neuropsychiatric multimorbidity. Am J Med. (2019) 132:1207–15.e6. doi: 10.1016/j.amjmed.2019.05.005
3. Yang NP, Hsu NW, Lin CH, Chen HC, Tsao HM, Lo SS, et al. Relationship between muscle strength and fall episodes among the elderly: the Yilan study, Taiwan. BMC Geriatr. (2018) 18:90. doi: 10.1186/s12877-018-0779-2
4. Hu B, Li B, Wang J, Shi C. Home and community care for older people in urban China: receipt of services and sources of payment. Health Soc Care Community. (2020) 28:225–35. doi: 10.1111/hsc.12856
5. Communiqué of the Seventh National Population Census. National Bureau of Statistics of China (2021). Available online at: http://www.stats.gov.cn/english/PressRelease/202105/t20210510_1817190.html (accessed May 11, 2021).
6. Beard JR, Officer A, de Carvalho IA, Sadana R, Pot AM, Michel JP, et al. The World report on ageing and health: a policy framework for healthy ageing. Lancet. (2016) 387:2145–54. doi: 10.1016/S0140-6736(15)00516-4
7. Michel J-P, Graf C, Ma L, Ecarnot F. The end of the disease concept in geriatric medicine. Aging Med Healthc. (2020) 11:3–9. doi: 10.33879/AMH.2020.032-2002.006
8. Nagi SZ. Some conceptual issues in disability and rehabilitation. In: Sussman M, editor. Sociology and Rehabilitation. Washington, DC: American Sociological Association (1965). p. 110–3.
9. Towards a Common Language for Functioning Disability Health-ICF. Geneva: World Health Organization (2002). Available online at: https://www.who.int/classifications/icf/training/icfbeginnersguide.pdf (accessed March 28, 2021).
10. Federici S, Meloni F, Mancini A, Lauriola M, Olivetti Belardinelli M. World Health Organisation Disability Assessment Schedule II: contribution to the Italian validation. Disabil Rehabil. (2009) 31:553–64. doi: 10.1080/09638280802240498
11. Yang M, Ding X, Dong B. The measurement of disability in the elderly: a systematic review of self-reported questionnaires. J Am Med Dir Assoc. (2014) 15:150.e1–9. doi: 10.1016/j.jamda.2013.10.004
12. Linden M. Definition and assessment of disability in mental disorders under the perspective of the International Classification of Functioning Disability and Health (ICF). Behav Sci Law. (2017) 35:124–34. doi: 10.1002/bsl.2283
13. Martin LG, Schoeni RF, Andreski PM. Trends in health of older adults in the United States: past, present, future. Demography. (2010) 47(Suppl):S17–S40. doi: 10.1353/dem.2010.0003
14. Hou C, Ma Y, Yang X, Tao L, Zheng D, Liu X, et al. Disability transitions and health expectancies among elderly people aged 65 years and over in China: a Nationwide Longitudinal Study. Aging Dis. (2019) 10:1246–57. doi: 10.14336/AD.2019.0121
15. Liu Z, Han L, Wang X, Feng Q, Gill TM. Disability prior to death among the oldest-old in China. J Gerontol Ser A Biol Sci Med Sci. (2018) 73:1701–7. doi: 10.1093/gerona/gly010
16. Zhang H, Wang ZH, Wang LM, Qi SG, Li ZX. Study on activities of daily living disability in community-dwelling older adults in China. Zhonghua Liu Xing Bing Xue Za Zhi. (2019) 40:266–71. doi: 10.3760/cma.j.issn.0254-6450.2019.03.003
17. Dias EN, da Silva JV, Pais-Ribeiro JL, Martins T. Validation of the advanced activities of daily living scale. Geriatr Nurs. (2019) 40:7–12. doi: 10.1016/j.gerinurse.2018.05.008
18. Zhang Y, Yang M, Wu F, Wang Q, Ni X, Wang P, et al. Development of preliminary version of function impairment screening tool for the elderly using Delphi method. Chin J Mult Organ Dis Elder. (2021) 20:86–91. doi: 10.11915/j.issn.1671-5403.2021.02.019
19. Zhang Y, Tang Z, Yang M, Wu F, Wang Q, Ni X, et al. Development of the formal version of function impairment screening tool. Chin J Mult Organ Dis Elder. (2021) 20:265–9. doi: 10.11915/j.issn.1671-5403.2021.04.055
20. Li H, Jia J, Yang Z. Mini-mental state examination in elderly Chinese: a population-based normative study. J Alzheimers Dis. (2016) 53:487–96. doi: 10.3233/JAD-160119
21. Mahoney FI, Barthel DW. FUNCTIONAL EVALUATION: THE BARTHEL INDEX. Md State Med J. (1965) 14:61–5. doi: 10.1037/t02366-000
22. Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. (1969) 9:179–86. doi: 10.1093/geront/9.3_Part_1.179
23. Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol Ser A Biol Sci Med Sci. (2001) 56:M146–M56. doi: 10.1093/gerona/56.3.M146
24. Bertrand AM, Fournier K, Wick Brasey MG, Kaiser ML, Frischknecht R, Diserens K. Reliability of maximal grip strength measurements and grip strength recovery following a stroke. J Hand Ther. (2015) 28:356–62; quiz 63. doi: 10.1016/j.jht.2015.04.004
25. Muñoz-Mendoza CL, Cabañero-Martínez MJ, Millán-Calenti JC, Cabrero-García J, López-Sánchez R, Maseda-Rodríguez A. Reliability of 4-m and 6-m walking speed tests in elderly people with cognitive impairment. Arch Gerontol Geriatr. (2011) 52:e67–e70. doi: 10.1016/j.archger.2010.06.020
26. Wu C, Smit E, Xue QL, Odden MC. Prevalence and correlates of frailty among community-dwelling Chinese older adults: the China health and retirement longitudinal study. J Gerontol Ser A Biol Sci Med Sci. (2017) 73:102–8. doi: 10.1093/gerona/glx098
27. Ma L, Zhang L, Sun F, Li Y, Tang Z. Cognitive function in Prefrail and frail community-dwelling older adults in China. BMC Geriatr. (2019) 19:53. doi: 10.1186/s12877-019-1056-8
28. Hajjar STE. STATISTICAL ANALYSIS: INTERNAL-CONSISTENCY RELIABILITY AND CONSTRUCT VALIDITY. Int J Quant Qual Res Methods. (2018) 6:27–38.
29. Terwee CB, Bot SD, de Boer MR, van der Windt DA, Knol DL, Dekker J, et al. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol. (2007) 60:34–42. doi: 10.1016/j.jclinepi.2006.03.012
30. de Vet HC, Terwee CB, Knol DL, Bouter LM. When to use agreement versus reliability measures. J Clin Epidemiol. (2006) 59:1033–9. doi: 10.1016/j.jclinepi.2005.10.015
31. Ledesma RD, Valero-Mora P, Macbeth G. The scree test and the number of factors: a dynamic graphics approach. Span J Psychol. (2015) 18:E11. doi: 10.1017/sjp.2015.13
32. Cattell RB. The scree test for the number of factors. Multivariate Behav Res. (1966) 1:245–76. doi: 10.1207/s15327906mbr0102_10
33. Mukaka MM. Statistics corner: a guide to appropriate use of correlation coefficient in medical research. Malawi Med J. (2012) 24:69–71.
34. Anthoine E, Moret L, Regnault A, Sebille V, Hardouin JB. Sample size used to validate a scale: a review of publications on newly-developed patient reported outcomes measures. Health Qual Life Outcomes. (2014) 12:176. doi: 10.1186/s12955-014-0176-2
35. Leentjens AF, Dujardin K, Pontone GM, Starkstein SE, Weintraub D, Martinez-Martin P. The Parkinson Anxiety Scale (PAS): development and validation of a new anxiety scale. Mov Disord. (2014) 29:1035–43. doi: 10.1002/mds.25919
36. Mokkink LB, Terwee CB, Patrick DL, Alonso J, Stratford PW, Knol DL, et al. The COSMIN checklist for assessing the methodological quality of studies on measurement properties of health status measurement instruments: an international Delphi study. Qual Life Res. (2010) 19:539–49. doi: 10.1007/s11136-010-9606-8
37. de Menezes KKP, Avelino PR, Faria-Fortini I, Basílio ML, Nascimento LR, Teixeira-Salmela LF. Test-retest reliability of the ABILOCO questionnaire in individuals with stroke. PM R. (2019) 11:843–8. doi: 10.1002/pmrj.12008
39. Schuling J, de Haan R, Limburg M, Groenier KH. The Frenchay activities index. Assessment of functional status in stroke patients. Stroke. (1993) 24:1173–7. doi: 10.1161/01.STR.24.8.1173
40. Jette AM, Davies AR, Cleary PD, Calkins DR, Rubenstein LV, Fink A, et al. The Functional Status Questionnaire: reliability and validity when used in primary care. J Gen Intern Med. (1986) 1:143–9. doi: 10.1007/BF02602324
41. Long WM. Questionnaire Statistical Analysis Practice: SPSS Operation and Application. Chongqing: Chongqing University Press (2010).
42. Wales K, Lannin NA, Clemson L, Cameron ID. Measuring functional ability in hospitalized older adults: a validation study. Disabil Rehabil. (2018) 40:1972–8. doi: 10.1080/09638288.2017.1323021
43. Suurmeijer TP, Doeglas DM, Moum T, Briancon S, Krol B, Sanderman R, et al. The Groningen Activity Restriction Scale for measuring disability: its utility in international comparisons. Am J Public Health. (1994) 84:1270–3. doi: 10.2105/AJPH.84.8.1270
44. Payette H, Gueye NR, Gaudreau P, Morais JA, Shatenstein B, Gray-Donald K. Trajectories of physical function decline and psychological functioning: the Quebec longitudinal study on nutrition and successful aging (NuAge). J Gerontol Ser B Psychol Sci Soc Sci. (2011) 66(Suppl. 1):i82–i90. doi: 10.1093/geronb/gbq085
45. Brummel NE, Bell SP, Girard TD, Pandharipande PP, Jackson JC, Morandi A, et al. Frailty and subsequent disability and mortality among patients with critical illness. Am J Respir Crit Care Med. (2017) 196:64–72. doi: 10.1164/rccm.201605-0939OC
46. Fhon JR, Rodrigues RA, Neira WF, Huayta VM, Robazzi ML. Fall and its association with the frailty syndrome in the elderly: systematic review with meta-analysis. Rev Esc Enferm USP. (2016) 50:1005–13. doi: 10.1590/s0080-623420160000700018
47. Goodpaster BH, Park SW, Harris TB, Kritchevsky SB, Nevitt M, Schwartz AV, et al. The loss of skeletal muscle strength, mass, and quality in older adults: the health, aging and body composition study. J Gerontol Ser A Biol Sci Med Sci. (2006) 61:1059–64. doi: 10.1093/gerona/61.10.1059
48. Shinkai S, Watanabe S, Kumagai S, Fujiwara Y, Amano H, Yoshida H, et al. Walking speed as a good predictor for the onset of functional dependence in a Japanese rural community population. Age Ageing. (2000) 29:441–6. doi: 10.1093/ageing/29.5.441
49. Abe T, Kitamura A, Taniguchi Y, Amano H, Seino S, Yokoyama Y, et al. Pathway from gait speed to incidence of disability and mortality in older adults: a mediating role of physical activity. Maturitas. (2019) 123:32–6. doi: 10.1016/j.maturitas.2019.02.002
50. Shimada H, Makizako H, Doi T, Tsutsumimoto K, Suzuki T. Incidence of disability in frail older persons with or without slow walking speed. J Am Med Dir Assoc. (2015) 16:690–6. doi: 10.1016/j.jamda.2015.03.019
51. McGrath R, Robinson-Lane SG, Peterson MD, Bailey RR, Vincent BM. Muscle strength and functional limitations: preserving function in older Mexican Americans. J Am Med Dir Assoc. (2018) 19:391–8. doi: 10.1016/j.jamda.2017.12.011
52. Germain CM, Vasquez E, Batsis JA, McQuoid DR. Sex, race and age differences in muscle strength and limitations in community dwelling older adults: data from the Health and Retirement Survey (HRS). Arch Gerontol Geriatr. (2016) 65:98–103. doi: 10.1016/j.archger.2016.03.007
53. Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, et al. Sarcopenia: European consensus on definition and diagnosis: report of the European Working Group on Sarcopenia in Older People. Age Ageing. (2010) 39:412–23. doi: 10.1093/ageing/afq034
54. Chen LK, Liu LK, Woo J, Assantachai P, Auyeung TW, Bahyah KS, et al. Sarcopenia in Asia: consensus report of the Asian Working Group for Sarcopenia. J Am Med Dir Assoc. (2014) 15:95–101. doi: 10.1016/j.jamda.2013.11.025
Keywords: functional impairment, reliability, validity, screen, older adults
Citation: Zhang Y, Liu P, Pan Y, Li Y, Zhang L, Li Y and Ma L (2021) Reliability and Validity of the Function Impairment Screening Tool in Chinese Older Adults. Front. Med. 8:720607. doi: 10.3389/fmed.2021.720607
Received: 04 June 2021; Accepted: 16 September 2021;
Published: 13 October 2021.
Edited by:
Jinhui Wu, Sichuan University, ChinaReviewed by:
Fatih Özden, Mugla University, TurkeyLi Mo, Sichuan University, China
Cuili Wang, Peking University, China
Copyright © 2021 Zhang, Liu, Pan, Li, Zhang, Li and Ma. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yun Li, bGl5X3h3QHNpbmEuY29t; Lina Ma, bWFsaW5hMDg4M0AxMjYuY29t
 Yaxin Zhang
Yaxin Zhang Pan Liu
Pan Liu Yiming Pan
Yiming Pan Li Zhang
Li Zhang Lina Ma
Lina Ma