
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Med. , 26 July 2021
Sec. Geriatric Medicine
Volume 8 - 2021 | https://doi.org/10.3389/fmed.2021.693818
This article is part of the Research Topic Frailty: Risks and Management View all 13 articles
Background: Frailty is one of the most important global health challenges. We aimed to examine the associations between frequency of intellectual and social activities and frailty among community-dwelling older adults in China.
Methods: This is a prospective analysis of older adults (aged ≥60 years) who had intellectual and social activity data and were free of frailty from the national representative China Health and Retirement Longitudinal Study (CHARLS). The exposure was frequency of intellectual and social activities. Frailty was measured by the frailty index (FI) and defined as FI ≥ 0.25. Frailty incidents were followed up for 2 years. We estimated the relative risks (RRs) with 95% confidence intervals (CIs) using log-linear binominal regression adjusting for potential confounders.
Results: We documented 655 frailty cases over the past 2 years. Participants who had frequent intellectual activities had a lower frailty risk compared with participants who did not have intellectual activity (adjusted RR = 0.65, 95%CI = 0.47–0.90). The adjusted RRs were 0.51 (95%CI = 0.33–0.77) for participants who did not have a slip or a fall accident and 1.06 (95%CI = 0.65–1.75) for participants who had experienced slip and fall accidents (P = 0.01 for interaction). Having frequent social activities was not associated with a significant decrease in frailty risk compared with participants who did not have social activity (adjusted RR = 0.93, 95%CI = 0.78–1.12).
Conclusions: This observational study showed that having frequent intellectual activities was associated with a decreased frailty risk. The association was likely to be stronger in participants without a slip or a fall accident. Randomized controlled trials are needed to confirm this observational finding.
Frailty, as an extreme consequence of the normal aging process, is one of the most serious global health challenges (1). A recent systematic review and meta-analysis has reported that the pooled prevalence of frailty was 17.4% among community-dwelling older adults in low-income and middle-income countries (2). Frailty is an unstable status in which the physiological reserves are reduced, causing disorders in homeostatic systems (1, 3). This would lead to rapid deterioration in functional capacity across many physiological systems and, thus, significantly increased risks of adverse health outcomes, such as falls, disability, hospitalization, and death (1, 3). Therefore, the identification of and interventions to slow the progression of frailty are essential for healthcare systems in an aging society (4, 5).
Insights into the key risk factors of frailty would be very helpful in determining effective strategies for frailty prevention. Many cross-sectional and longitudinal studies have been conducted to explore factors associated with frailty (2, 6–22). The identified potential factors included sociodemographic factors (6–9), socioeconomic status (2, 7, 14, 15), physical and biological factors (20–22), and lifestyle and clinical factors (7, 11–14, 18, 19). Most of these risk factors could be modified by regular physical activities and adequate nutritional intake (23).
Several studies have shown that participation in social and intellectual activities could improve the cognitive reserve and reduce functional decline and disabilities (12, 23, 24). Social and intellectual activities, along with physical activities and nutritional intake, play an important role in frailty prevention (2, 12). The associations between social or intellectual activities and physical frailty have been investigated in many studies (25–32). For example, a 4-year cohort study in Japan found that social frailty was a significant risk factor that leads to physical frailty (25). Another study in Japan showed that social activities decreased the functional disability risks (32). Wang et al. conducted a cross-sectional study among seniors from Singapore (28). They found that participation in intellectual activities was likely to be associated with a lower frailty prevalence (28).
To date, prospective cohort evidence for the associations between intellectual and social activities and frailty is still lacking in China. In addition, the associations between the different frequencies of intellectual or social activity participation and frailty development also needed to be further investigated (3, 33–35). We therefore conducted this prospective study to evaluate the associations between the frequency of intellectual and social activities and frailty among Chinese community-dwelling older adults.
The analyses were performed based on the China Health and Retirement Longitudinal Study (CHARLS) (36). In brief, CHARLS is a biennial national study that collects a representative sample of Chinese residents using a multistage stratified probability proportionate to size technique. High-quality information of the included residents was collected. The details of the objectives and methods of CHARLS were published in a previous report (36). The survey in 2015–2016 and the follow-up survey in 2017–2018 were available for the analyses in this study. The CHARLS was approved by the Biomedical Ethics Review Committee of Peking University. Written informed consent was obtained from all participants. The ethical approval number of CHARLS is IRB00001052-11015.
For the current analysis, we restricted the participants to those aged 60 years or above. We also excluded participants without frailty information. For each participant, the intellectual and social performances were collected in 2015–2016. Each participant had a 2-year follow-up. The ascertainment of frailty was carried out in 2017–2018. The participants who did not respond to the 2018 survey were considered as lost to follow-up (see Figure 1). The data in this study were reported according to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guidelines (37).
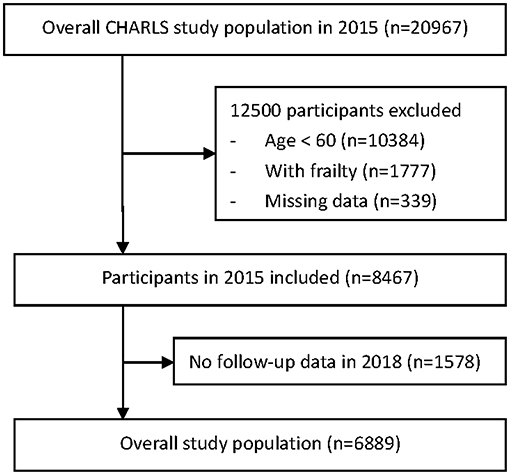
Figure 1. Flowchart of participant selection from the China Health and Retirement Longitudinal Study (CHARLS).
In the 2015–2016 CHARLS survey, participants were asked about their intellectual and social activities in the past month. Intellectual activities include playing Ma-jong, chess, cards; attending an educational or training course; investing in stock; and surfing the Internet. Social activities include interacting with friends; going to a sport, social, or other kinds of club; taking part in a community-related organization; and doing voluntary or charity work. The frequency of each activity was rated as follows: almost daily (score = 3), almost every week (score = 2), not regularly (score = 1), or never (score = 0). The total scores for intellectual and social activities ranged from 12 to 0 points and were categorized as ≥3, 1–2, and 0, where “≥3” referred to frequent participation, “1-2” referred to non-regular participation, and “0” referred to no participation in intellectual and social activities (30).
Frailty was measured by using a frailty index (FI). The construction of the FI was based on a standard procedure (38). The detailed method for the calculation of FI was reported in previous published studies (13, 17). In brief, a total of 39 deficit variables that were associated with FI in the CHARLS were selected, including 15 comorbidity variables, 5 disability variables, and 19 variables on activities of daily living. All of these 39 variables were scored from 0 to 1, where “0” indicated no deficit and “1” indicated the presence of a deficit. For each participant, FI was calculated by adding the scores of all the deficits and dividing by the total number of deficits. Frailty was defined as FI ≥ 0.25 (13, 16, 17, 39, 40).
The following information were obtained: sociodemographic factors, including age and sex; socioeconomic factors, including economic development regions (>$10,000, from $10,000 to >7,000, and ≤ $7,000) (41); lifestyle and health factors, including hours of actual sleep (≥6 h or <6 h), smoking (yes or no), and whether one had experienced slip and fall accidents (yes or no). The participants were deemed to have slip and fall accidents if they responded “yes” when asked “Have you fallen down?” The main comorbidities in medical history included cancer, diabetes mellitus, heart disease, hypertension, and stroke.
Baseline characteristics were compared among the different intellectual and social activity scores by using one-way analysis of variance (ANOVA) for continuous measures and using the Mantel–Haenszel test for proportion trends. The associations between intellectual and social activities and frailty were estimated as relative risks (RRs) with 95% confidence intervals (CIs) using log-linear binominal regression with a multivariable-adjusted model. In the multivariable-adjusted model 1, we adjusted for age and sex. To control potential confounding from socioeconomic status, we additionally adjusted for economic development regions in the multivariable-adjusted model 2. In the multivariable-adjusted model 3, we additionally controlled for lifestyle and health factors, such as sleep, smoking, and experiences of slip and fall accidents. Moreover, we finally introduced a model 4 to additionally adjust for the main comorbidities such as cancer, diabetes mellitus, heart disease, hypertension, and stroke. A multivariate logistic regression analysis was used in model 4. Odd ratios (ORs) with 95% CIs were reported.
Based on a review of previous literature (8, 16, 17), whether one had experienced slip and fall accidents was a potential effect modifier that may modify the associations between intellectual and social activities and frailty. Therefore, subgroup analysis was conducted based on whether the participants had experienced slip and fall accidents.
A number of sensitivity analyses were performed to examine the robustness of the associations between intellectual and social activities and frailty. Firstly, the impacts of lowering the cutoff value of FI were estimated, as FI ≥ 0.24 and FI ≥ 0.23. Secondly, only participants aged 65 years or older were included. Thirdly, we included only the participants without missing data. A p-value <0.05 was considered significant. All the analyses were performed using SAS, version 9.4 (SAS Institute, Cary, NC, USA).
This study included 6,889 participants. Table 1 presents the baseline characteristics according to the intellectual activity and social activity scores. Of the sample, 78.3% of the participants had an intellectual activity score of 0 and 62.4% had a social activity score of 0. Among the different intellectual activity scores, there were differences in the baseline characteristics such as age, sex, economic development region, actual sleep, smoking, cancer, diabetes, and heart disease. Among the different social activity scores, there were differences in the baseline characteristics such as age, sex, slip and fall accidents, smoking, diabetes, heart disease, and hypertension.
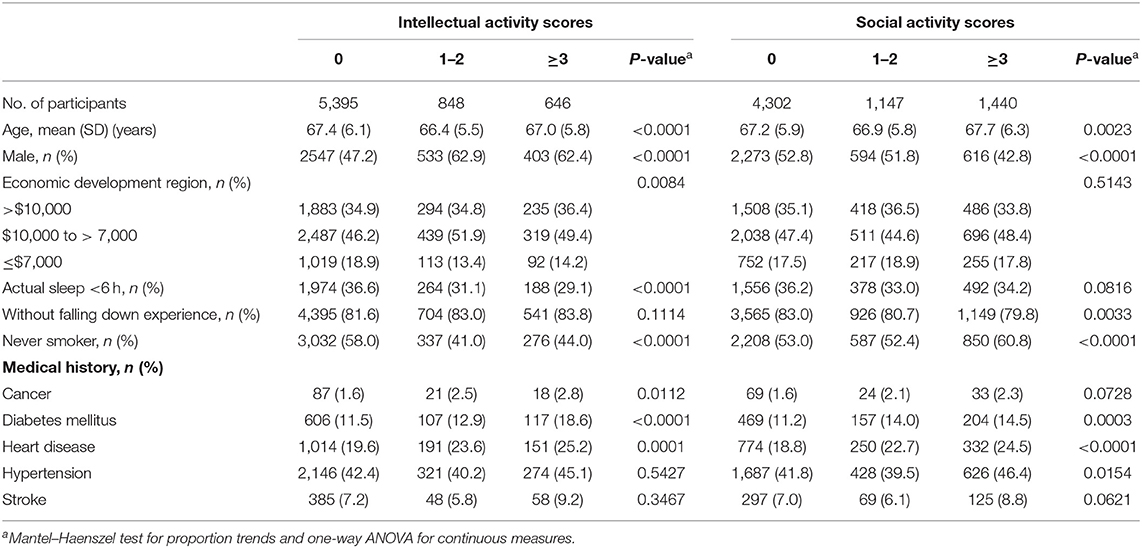
Table 1. Baseline characteristics according to the intellectual activity and social activity scores.
We observed 655 frailty cases over the past 2 years. In the fully adjusted model (model 3), participants with frequent intellectual activities (score ≥ 3) had a lower frailty risk compared with participants who did not have intellectual activity (scores = 0), with multivariable-adjusted RR of 0.65 (95%CI = 0.47–0.90). Participants who had non-regular intellectual activities (score = 1–2) had a lower frailty risk compared with participants who did not have intellectual activity, with multivariable-adjusted RR of 0.60 (95%CI = 0.44–0.80).
Results from the adjusted model (model 3) showed that participants who had non-regular social activities (score = 1–2) had a lower frailty risk compared with participants who had no social activity (score = 0), with multivariable-adjusted RR of 0.68 (95%CI = 0.54–0.86). However, having frequent social activities (score ≥ 3) was not associated with a decreased frailty risk compared with participants who had no social activity (score = 0), with multivariable-adjusted RR of 0.93 (95%CI = 0.78–1.12) (Table 2).
Subgroup analysis was conducted to detect whether having experienced slip and fall accidents was an interaction that modified the effect of intellectual activity on frailty. We found evidence of an interaction effect of “slip and fall accidents” when comparing participants who had frequent intellectual activities (score ≥ 3) to those who did not have intellectual activity (score = 0). Among the participants who did not have a slip or a fall accident, having frequent intellectual activities (score ≥ 3) was associated with a significant decrease in frailty risk compared with participants who did not have intellectual activity (score = 0). However, among the participants who had experienced slip and fall accidents, having frequent intellectual activities (score ≥ 3) was not associated with a decreased frailty risk compared with participants who had no intellectual activity (score = 0). The p-value for the “slip and fall accidents” interaction was 0.0103 (Table 3).
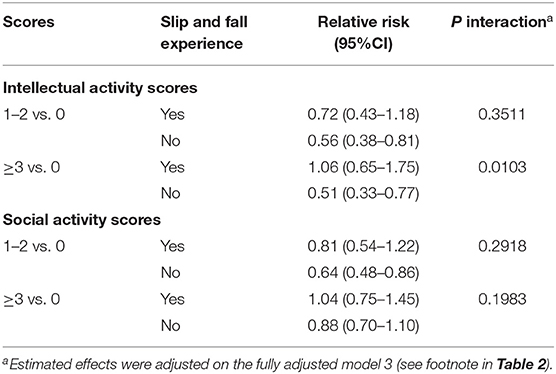
Table 3. Subgroup analyses of the intellectual activity and social activity scores and the risk of frailty.
In the sensitivity analyses, all the results were generally unchanged, indicating the robustness of the identified associations (Table 4).
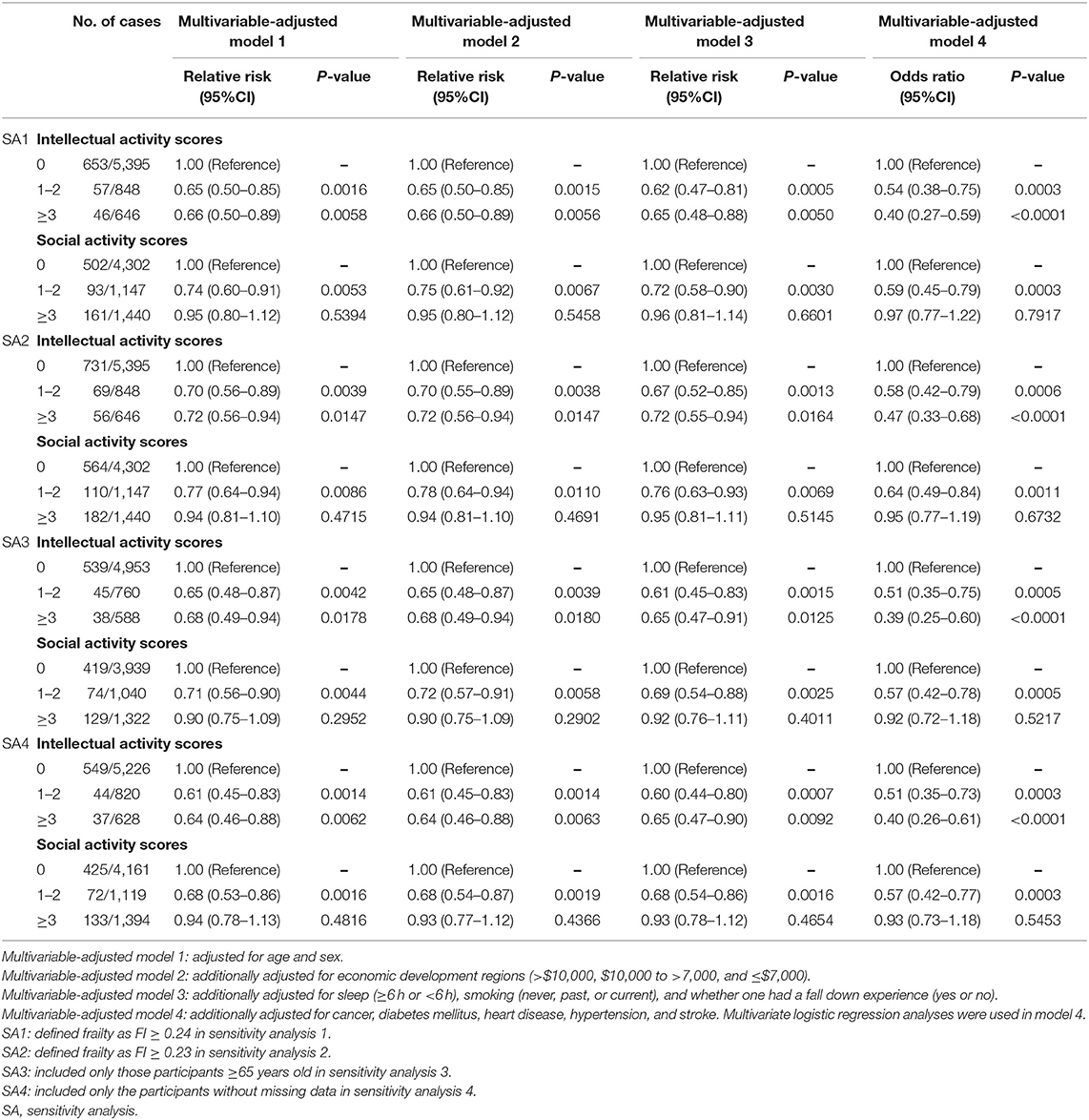
Table 4. Sensitivity analyses: risk of frailty according to the intellectual activity and social activity scores.
In this prospective analysis of 6,889 elderly Chinese participants, 655 frailty cases were identified over the 2-year follow-up. We found that having frequent intellectual activities was associated with a 35% lower risk of frailty. The association was likely to be stronger among participants who did not experience a slip or a fall accident, with a 49% lower risk of frailty. These associations showed robustness in a series of sensitivity analyses. On the contrary, having frequent social activities was not associated with a significant decrease in frailty risk compared with participants who did not have social activity.
Previous studies have shown that risk factors for the onset of frailty span across a broad range, including sociodemographic, socioeconomic, lifestyle-related, and biological and clinical aspects (2, 6–22). Feng et al. conducted a systematic review and meta-analysis to investigate protective factors that were associated with frailty among elderly people (7). A wider range of factors was identified, including psychological and social factors (7). Our study is in agreement with these previous findings.
The identification of essential modifiable risk and protective factors is very important for frailty prevention (1, 3, 42). Previously, the preventive strategies mainly focused on physical-related interventions, such as taking regular physical activities and providing adequate nutritional intake (4, 33, 43). Recently, loneliness and social isolation have been proven to have negative effects on health (10, 44, 45). More attention should be paid to the association between psychosocial factors and frailty development. In a 4-year cohort study, Makizako et al. found that social frailty leads to physical frailty in a relatively short period of time (25). Based on a 2-year cohort, the results from the study of Ye et al. showed that social participation was associated with a higher prefrail improvement (29). Kim et al. conducted a cross-sectional study to investigate the frequency of social activity participation and its association with the different levels of frailty (27). They found that social activities such as leisure and club activities at a frequency of once a week were associated with frailty prevention (27). The results of this study were in agreement with these previous findings, despite the differences in the setting population, the frailty index domains, and details in the social and intellectual activities included between this study and the previous studies. In addition, we found that non-regular participation in social activities has a positive impact on frailty prevention. However, having frequent social activities (such as an almost daily participation) was not associated with a decrease in frailty risk.
Understanding the associations between intellectual activity participation and frailty development was also important. In a cross-sectional study, Wang et al. found that engaging in intellectual activities in late-life was associated with a lower frailty prevalence, especially among female elderly people (28). To date, evidence from prospective cohort studies is still lacking for the impact of intellectual activities on frailty. The present study showed that participation in intellectual activity was associated with a significant decrease in frailty risk compared with non-participation in intellectual activity. Frailty often coexists with cognitive impairment (45, 46). Lack of intellectual activity increases the risks of cognitive impairment (30, 47, 48). In the future, strategies for frailty prevention should be more focused on improving participation in intellectual activities. In addition, intellectual training, when combined with physical training, could have a positive effect on preserving the function of physiological systems and, thus, slowing the progression of cognitive frailty (12, 48, 49), despite the underlying biological and psychological mechanisms still far from being understood (1, 48, 50).
Effective strategies are needed to prevent or slow the progression of frailty. To date, solid evidence, such as randomized controlled trials (RCTs), is still lacking to evaluate the effectiveness of intervention strategies on frailty development. Most of the previous studies were observational. They were mainly focused on physical activity and nutritional strategies, such as exercise and muscle training and sufficient protein intake (1, 4, 5, 51). Since the current observational evidence showed a significant association between participation in intellectual activities and decreased frailty risk, it is encouraged to include intellectual activities in the intervention strategies on frailty in the future. Individually tailored intellectual and social activity programs could be added into traditional frailty intervention strategies. Moreover, high-quality RCTs are also needed to examine the effectiveness of these intellectual activity programs on frailty prevention.
To our knowledge, this is the first prospective observational study investigating the associations between intellectual and social activities and frailty risks. We identified that having frequent intellectual activities is associated with decreased frailty risks whereas having frequent social activities is not compared with non-participation in intellectual and social activities. In addition, fall was a significant interaction for the effect of intellectual activity on frailty. The findings in this study would provide useful evidence for the management of and prevention strategies on frailty.
However, two potential limitations should be noted. Firstly, the current research was an observational cohort study. Despite potential confounders being adjusted in the log-linear binominal regression by multivariable-adjusted models, the results may still be biased by other potential important confounders, for example, nutrient intake, musculoskeletal function, and laboratory parameters such as serum uric acid levels (7). On the one hand, the analyses in this study were based on secondary data, so important factors such as nutrition and exercise were precluded. On the other hand, due to model limitation, the number of cases was too small to include enough adjusted variables in the adjusted model. In the future, RCTs are needed to determine the effect of the different levels of intellectual and social activities on frailty. Then, both the known and unknown confounders would be controlled in well-designed RCTs. Secondly, frailty should be detected reliably. Although multiple screening instruments for frailty have been developed and validated, to date, there is still a lack of the most effective instruments to detect frailty. There is also a lack of agreement between the different screening instruments. Nevertheless, in this study, multiple sensitivity analyses with different cutoff values of the FI were performed and the results were robust.
Overall, this prospective analysis study showed that having frequent intellectual activities was associated with a decreased risk of frailty, particularly in those participants who did not have slip and fall accidents. Non-regular participation in social activities was associated with a decreased risk of frailty compared with no social activity, whereas frequent social activity participation was not. These conclusions were based on observational evidences. In the future, more well-designed cohort studies and RCTs are still required to confirm our findings.
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found at: This analysis uses data or information from the Harmonized China Health and Retirement Longitudinal Study (CHARLS) dataset and Codebook, version C, which was developed by the Gateway to Global Aging Data (https://g2aging.org). The development of the Harmonized CHARLS was funded by the National Institute on Aging (grants R01 AG030153, RC2 AG036619, and R03 AG043052). Further inquiries can be directed to the corresponding authors. Data can also be obtained on request (eWFmYW5nQGNjbXUuZWR1LmNu; eHlndW9AY2NtdS5lZHUuY24=).
The studies involving human participants were reviewed and approved by Biomedical Ethics Review Committee of Peking University. The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
XG and YH contributed to conception of the study and drafted the manuscript. YH, XG, JD, and YL helped with acquisition, analysis, or interpretation of data. YH, XG, and JD critically revised the manuscript for important intellectual content. YH, XG, and YL performed statistical analysis. XG and YH provided administrative, technical, or material support, had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. All authors contributed to the article and approved the submitted version.
This work was supported by a Social Science Program General Project Grant (SM202110025003) from Beijing Municipal Education Commission. The funder had no role in the design and conduct of the study, collection, management, analysis, and interpretation of the data, preparation, review, or approval of the manuscript, and the decision to submit the manuscript for publication.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Dent E, Martin FC, Bergman H, Woo J, Romero-Ortuno R, Walston JD. Management of frailty: opportunities, challenges, and future directions. Lancet. (2019) 394:1376–86. doi: 10.1016/S0140-6736(19)31785-4
2. Siriwardhana DD, Hardoon S, Rait G, Weerasinghe MC, Walters KR. Prevalence of frailty and prefrailty among community-dwelling older adults in low-income and middle-income countries: a systematic review and meta-analysis. BMJ Open. (2018) 8:e018195. doi: 10.1136/bmjopen-2017-018195
3. Hoogendijk EO, Afilalo J, Ensrud KE, Kowal P, Onder G, Fried LP. Frailty: implications for clinical practice and public health. Lancet. (2019) 394:1365–75. doi: 10.1016/S0140-6736(19)31786-6
4. Walston J, Buta B, Xue QL. Frailty screening and interventions: considerations for clinical practice. Clin Geriatr Med. (2018) 34:25–38. doi: 10.1016/j.cger.2017.09.004
5. Woolford SJ, Sohan O, Dennison EM, Cooper C, Patel HP. Approaches to the diagnosis and prevention of frailty. Aging Clin Exp Res. (2020) 32:1629–37. doi: 10.1007/s40520-020-01559-3
6. Fhon JRS, Rodrigues RAP, Santos JLF, Diniz MA, Santos EBD, Almeida VC, et al. Factors associated with frailty in older adults: a longitudinal study. Rev Saude Publica. (2018) 52:74. doi: 10.11606/S1518-8787.2018052000497
7. Feng Z, Lugtenberg M, Franse C, Fang X, Hu S, Jin C, et al. Risk factors and protective factors associated with incident or increase of frailty among community-dwelling older adults: A systematic review of longitudinal studies. PLoS ONE. (2017) 12:e0178383. doi: 10.1371/journal.pone.0178383
8. Kendhapedi KK, Devasenapathy N. Prevalence and factors associated with frailty among community-dwelling older people in rural Thanjavur district of South India: a cross-sectional study. BMJ Open. (2019) 9:e032904. doi: 10.1136/bmjopen-2019-032904
9. Ntanasi E, Yannakoulia M, Mourtzi N, Vlachos GS, Kosmidis MH, Anastasiou CA, et al. Prevalence and risk factors of frailty in a community-dwelling population: the HELIAD Study. J Aging Health. (2020) 32:14–24. doi: 10.1177/0898264318801735
10. Sha S, Xu Y, Chen L. Loneliness as a risk factor for frailty transition among older Chinese people. BMC Geriatr. (2020) 20:300. doi: 10.1186/s12877-020-01714-5
11. Miettinen M, Tiihonen M, Hartikainen S, Nykänen I. Prevalence and risk factors of frailty among home care clients. BMC Geriatr. (2017) 17:266. doi: 10.1186/s12877-017-0660-8
12. Cheong CY, Nyunt MSZ, Gao Q, Gwee X, Choo RWM, Yap KB, et al. Risk factors of progression to frailty: findings from the Singapore longitudinal ageing study. J Nutr Health Aging. (2020) 24:98–106. doi: 10.1007/s12603-019-1277-8
13. Yin JH, Zeng YB, Zhou Z, Fang Y. [Study on the status of frailty and related determinants among the elderly in China]. Zhonghua Liu Xing Bing Xue Za Zhi. (2018) 39:1244–8. doi: 10.3760/cma.j.issn.0254-6450.2018.09.019
14. Yang F, Chen QW. Evaluation of frailty and influencing factors in old people in hospital institution: Evidence for a phenotype of frailty. Medicine (Baltimore). (2018) 97:e9634. doi: 10.1097/MD.0000000000009634
15. Lian Y, Yang L, Gao M, Jia CX. Relationship of frailty markers and socioeconomic status to incidence of depressive symptoms in a community cohort. J Am Med Dir Assoc. (2021) 22:570–6.e1. doi: 10.1016/j.jamda.2020.08.026
16. Kojima G, Kendrick D, Skelton DA, Morris RW, Gawler S, Iliffe S. Frailty predicts short-term incidence of future falls among British community-dwelling older people: a prospective cohort study nested within a randomised controlled trial. BMC Geriatr. (2015) 15:155. doi: 10.1186/s12877-015-0152-7
17. Wang X, Chen Z, Li Z, Chen B, Qi Y, Li G, et al. Association between frailty and risk of fall among diabetic patients. Endocr Connect. (2020) 9:1057–64. doi: 10.1530/EC-20-0405
18. Ng TP, Feng L, Nyunt MS, Larbi A, Yap KB. Frailty in older persons: multisystem risk factors and the Frailty Risk Index (FRI). J Am Med Dir Assoc. (2014) 15:635–42. doi: 10.1016/j.jamda.2014.03.008
19. Lorenzo-López L, Maseda A, de Labra C, Regueiro-Folgueira L, Rodríguez-Villamil JL, Millán-Calenti JC. Nutritional determinants of frailty in older adults: A systematic review. BMC Geriatr. (2017) 17:108. doi: 10.1186/s12877-017-0496-2
20. Woods NF, LaCroix AZ, Gray SL, Aragaki A, Cochrane BB, Brunner RL, et al. Frailty: emergence and consequences in women aged 65 and older in the Women's Health Initiative Observational Study. J Am Geriatr Soc. (2005) 53:1321–30. doi: 10.1111/j.1532-5415.2005.53405.x
21. Semba RD, Bartali B, Zhou J, Blaum C, Ko CW, Fried LP. Low serum micronutrient concentrations predict frailty among older women living in the community. J Gerontol A Biol Sci Med Sci. (2006) 61:594–9. doi: 10.1093/gerona/61.6.594
22. Cawthon PM, Ensrud KE, Laughlin GA, Cauley JA, Dam TT, Barrett-Connor E, et al. Sex hormones and frailty in older men: the osteoporotic fractures in men (MrOS) study. J Clin Endocrinol Metab. (2009) 94:3806–15. doi: 10.1210/jc.2009-0417
23. McPhee JS, French DP, Jackson D, Nazroo J, Pendleton N, Degens H. Physical activity in older age: perspectives for healthy ageing and frailty. Biogerontology. (2016) 17:567–80. doi: 10.1007/s10522-016-9641-0
24. Gobbens RJ, Luijkx KG, Wijnen-Sponselee MT, Schols JM. Towards an integral conceptual model of frailty. J Nutr Health Aging. (2010) 14:175–81. doi: 10.1007/s12603-010-0045-6
25. Makizako H, Shimada H, Doi T, Tsutsumimoto K, Hotta R, Nakakubo S, et al. Social frailty leads to the development of physical frailty among physically non-frail adults: a four-year follow-up longitudinal cohort study. Int J Environ Res Public Health. (2018) 15:490. doi: 10.3390/ijerph15030490
26. Nagai K, Tamaki K, Kusunoki H, Wada Y, Tsuji S, Itoh M, et al. Physical frailty predicts the development of social frailty: a prospective cohort study. BMC Geriatr. (2020) 20:403. doi: 10.1186/s12877-020-01814-2
27. Kim A, Yi E, Kim J, Kim M. A study on the influence of social leisure activities on the progression to the stage of frailty in Korean seniors. Int J Environ Res Public Health. (2020) 17:8909. doi: 10.3390/ijerph17238909
28. Wang X, Lu Y, Li C, Larbi A, Feng L, Shen Q, et al. Associations of lifestyle activities and a heathy diet with frailty in old age: a community-based study in Singapore. Aging (Albany NY). (2020) 12:288–308. doi: 10.18632/aging.102615
29. Ye B, Chen H, Huang L, Ruan Y, Qi S, Guo Y, et al. Changes in frailty among community-dwelling Chinese older adults and its predictors: evidence from a two-year longitudinal study. BMC Geriatr. (2020) 20:130. doi: 10.1186/s12877-020-01530-x
30. Li H, Li C, Wang A, Qi Y, Feng W, Hou C, et al. Associations between social and intellectual activities with cognitive trajectories in Chinese middle-aged and older adults: a nationally representative cohort study. Alzheimers Res Ther. (2020) 12:115. doi: 10.1186/s13195-020-00691-6
31. Gao M, Sa Z, Li Y, Zhang W, Tian D, Zhang S, et al. Does social participation reduce the risk of functional disability among older adults in China? A survival analysis using the 2005–2011 waves of the CLHLS data. BMC Geriatr. (2018) 18:224. doi: 10.1186/s12877-018-0903-3
32. Kanamori S, Kai Y, Aida J, Kondo K, Kawachi I, Hirai H, et al. Social participation and the prevention of functional disability in older Japanese: the JAGES cohort study. PLoS ONE. (2014) 9:e99638. doi: 10.1371/journal.pone.0099638
33. Gómez-Gómez ME, Zapico SC. Frailty, cognitive decline, neurodegenerative diseases and nutrition interventions. Int J Mol Sci. (2019) 20:2842. doi: 10.3390/ijms20112842
34. Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. Lancet. (2013) 381:752–62. doi: 10.1016/S0140-6736(12)62167-9
35. Fabrício DM, Chagas MHN, Diniz BS. Frailty and cognitive decline. Transl Res. (2020) 221:58–64. doi: 10.1016/j.trsl.2020.01.002
36. Zhao Y, Hu Y, Smith JP, Strauss J, Yang G. Cohort profile: the China Health and Retirement Longitudinal Study (CHARLS). Int J Epidemiol. (2014) 43:61–8. doi: 10.1093/ije/dys203
37. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS Med. (2007) 4:e296. doi: 10.1371/journal.pmed.0040296
38. Searle SD, Mitnitski A, Gahbauer EA, Gill TM, Rockwood K. A standard procedure for creating a frailty index. BMC Geriatr. (2008) 8:24. doi: 10.1186/1471-2318-8-24
39. Song X, Mitnitski A, Rockwood K. Prevalence and 10-year outcomes of frailty in older adults in relation to deficit accumulation. J Am Geriatr Soc. (2010) 58:681–7. doi: 10.1111/j.1532-5415.2010.02764.x
40. Kehler DS, Ferguson T, Stammers AN, Bohm C, Arora RC, Duhamel TA, et al. Prevalence of frailty in Canadians 18–79 years old in the Canadian Health Measures Survey. BMC Geriatr. (2017) 17:28. doi: 10.1186/s12877-017-0423-6
41. National currency per U.S. dollar, end of period. Principal global indicators (PGI) database. Washington: International Monetary Fund, 2018. Available online at: http://www.principalglobalindicators.org/regular.aspx?key=60942001 (accessed March 31, 2021).
42. Hamilton W, Round J. Identifying frailty in primary care. BMJ. (2017) 358:j4478. doi: 10.1136/bmj.j4478
43. Nascimento CM, Ingles M, Salvador-Pascual A, Cominetti MR, Gomez-Cabrera MC, Viña J. Sarcopenia, frailty and their prevention by exercise. Free Radic Biol Med. (2019) 132:42–9. doi: 10.1016/j.freeradbiomed.2018.08.035
44. Monin J, Doyle M, Levy B, Schulz R, Fried T, Kershaw T. Spousal associations between frailty and depressive symptoms: longitudinal findings from the cardiovascular health study. J Am Geriatr Soc. (2016) 64:824–30. doi: 10.1111/jgs.14023
45. Zhào H, Wei W, Liu Y, Gao J, Huang Y. Cognitive frailty among elderly Chinese patients with cerebral small vessel disease: a structural MRI study. Front Med. (2020) 7:397. doi: 10.3389/fmed.2020.00397
46. Panza F, Lozupone M, Solfrizzi V, Sardone R, Dibello V, Di Lena L, et al. Different cognitive frailty models and health- and cognitive-related outcomes in older age: from epidemiology to prevention. J Alzheimers Dis. (2018) 62:993–1012. doi: 10.3233/JAD-170963
47. Lam LC, Ong PA, Dikot Y, Sofiatin Y, Wang H, Zhao M, et al. Intellectual and physical activities, but not social activities, are associated with better global cognition: a multi-site evaluation of the cognition and lifestyle activity study for seniors in Asia (CLASSA). Age Ageing. (2015) 44:835–40. doi: 10.1093/ageing/afv099
48. Aartsen MJ, Smits CH, van Tilburg T, Knipscheer KC, Deeg DJ. Activity in older adults: cause or consequence of cognitive functioning? A longitudinal study on everyday activities and cognitive performance in older adults. J Gerontol B Psychol Sci Soc Sci. (2002) 57:P153–62. doi: 10.1093/geronb/57.2.P153
49. Kirk-Sanchez NJ, McGough EL. Physical exercise and cognitive performance in the elderly: current perspectives. Clin Interv Aging. (2014) 9:51–62. doi: 10.2147/CIA.S39506
50. Karssemeijer EGA, Aaronson JA, Bossers WJ, Smits T, Olde Rikkert MGM, Kessels RPC. Positive effects of combined cognitive and physical exercise training on cognitive function in older adults with mild cognitive impairment or dementia: A meta-analysis. Ageing Res Rev. (2017) 40:75–83. doi: 10.1016/j.arr.2017.09.003
Keywords: frailty, intellectual activity, social activity, prospective cohort study, CHARLS
Citation: Huang Y, Guo X, Du J and Liu Y (2021) Associations Between Intellectual and Social Activities With Frailty Among Community-Dwelling Older Adults in China: A Prospective Cohort Study. Front. Med. 8:693818. doi: 10.3389/fmed.2021.693818
Received: 12 April 2021; Accepted: 25 June 2021;
Published: 26 July 2021.
Edited by:
Grazia Daniela Femminella, University of Naples Federico II, ItalyReviewed by:
Fabrizia Lattanzio, National Institute of Science and Health for Aging (INRCA-IRCCS), ItalyCopyright © 2021 Huang, Guo, Du and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yafang Huang, eWFmYW5nQGNjbXUuZWR1LmNu; Xiangyu Guo, eHlndW9AY2NtdS5lZHUuY24=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.