- Department of Orthopaedics, West China Hospital, Sichuan University, Chengdu, China
Background: Recently, there is an increasing interest in the therapeutic potential of platelet-rich plasma (PRP) for bone fracture treatment. Nevertheless, the effect of PRP for bone fracture treatment remains controversial and is still a matter of discussion. Therefore, we performed a systematic review to evaluate the efficacy and safety of PRP injection for treatment of bone fracture.
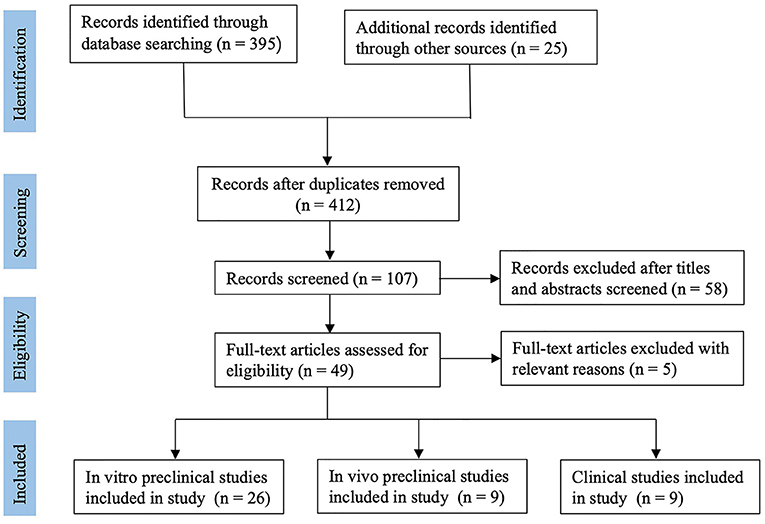
Methods: The main bibliographic databases, including Medline, PubMed, Embase, Web of Science, and the Cochrane library, were comprehensively searched for studies focusing on the application of platelet-rich plasma (PRP) on bone fracture treatment. All relevant articles were screened for eligibility and subdivided into the preclinical and clinical studies. Data were extracted and presented systematically.
Results: Finally, twenty-six in vitro preclinical studies (basic studies), nine in vivo preclinical studies (animal studies), and nine clinical studies, met the selection criteria, and were included in the present systematic review. Preclinical studies showed an overall positive effect of PRP on osteoblast-like cells in vitro and bone healing in animal models. The most used treatment for bone fracture in animal and clinical studies is fixation surgery combined with PRP injection. The clinical studies reported PRP shortened bony healing duration, and had no positive effect on improving the healing rate of closed fractures. However, the results of functional outcomes are controversial. Additionally, compared with control group, PRP would not increase the rate of postoperative wound infection.
Conclusion: The present systematic review confirmed the continuing interests of PRP as an additional treatment for bone fracture. Preclinical studies highlighted the potential value of PRP as promising therapy for bone fracture. However, the preclinical evidence did not translate into a similar result in the clinical studies. In addition, types of fractures and procedures of PRP preparation are heterogeneous in enrolled studies, which might result in controversial results. Meanwhile, characteristics of PRP, such as platelet concentration, the numbers of leukocytes, still need to be determined and further research is required.
Introduction
Bone tissue is a major part of the musculoskeletal system and provides the framework which supports the body and maintains its shape (1–3). Although bone tissue has the potential for spontaneous healing after injuries, the regenerative capacity of bone tissue is limited by many factors, such as age, type of fracture, genetic bone disorder (4–6). Additionally, up to 13% of tibial shaft fractures are associated with fracture non-union or delayed union, which are the most devastating complications of traumatic fractures (7–9). For elderly patients with lower limb fracture, the long period of bedridden time and immobilization increases the incidence of pulmonary infection, thrombosis, and bedsore, and as a consequence the risk of death (10, 11). Currently, the principle of clinical treatment for a fracture is reduction and fixation. Meanwhile, many clinical approaches, such as administration of bone morphogenetic proteins (12, 13), cell-based therapies (14, 15), platelet-rich plasma (16), or implantation of graft biomaterials (17), have been used either alone or in combination to enhance bone regeneration. Additionally, many previous studies demonstrated that low-intensity pulsed ultrasound (LIPUS) could also accelerate fracture healing and increase the rate of fracture healing (18, 19).
Deriving from centrifugation of peripheral blood, PRP can deliver a high concentration of autologous bioactive factors, including transforming growth factor-beta, platelet-derived growth factor, and interleukin, in a low cost and minimally invasive way (20). The bioactive factors released from PRP can take part in the process of neovascularization, tissue remodeling, and regulation of inflammation, which led to the idea of using PRP for tissue repair (21, 22). After further freeze-thawing and centrifugation steps, resulting in the lysis of platelets, PRP can turn into platelet lysate, which contains higher concentrations of growth factors (23). Additionally, PRP can combine with thrombin and calcium to form a coagulum, called platelet gel (24). Platelet-poor plasma is the residual plasma once the PRP is extracted, which still contains beneficial proteins, insulin-GF and a low number of platelets (25). In the last decade, as a fashionable treatment, PRP has shown sustained beneficial repair effects in clinical procedures involving various soft tissue, such as ligaments and tendons (20). Meanwhile, there is an increasing interest in the therapeutic potential of PRP for bone fracture treatment. Nevertheless, the effect of PRP for bone fracture treatment remains controversial and is still a matter of discussion. As there is no related systematic review published yet, we performed this systematic review to evaluate whether PRP injection improve outcome of bone fracture, in terms of bony union time, bone healing rate, functional scores, VSA scores, complication, and imaging.
Methods
Search Strategy
This systematic review was performed according to the Preferred Reporting Items for Systematic reviews and Meta-Analysis (PRISMA) guidelines (26). Two reviewers independently searched for potentially relevant published researches using electronic databases, including Medline, PubMed, Embase, Web of Science, and the Cochrane library from inception to March 2020. The search strategy for all electronic databases was built as follows: “(PRP OR platelet-rich plasma OR plasma rich in growth factors OR platelet derived growth factor OR autologous plasma OR autologous conditioned plasma) and (bone fracture OR fracture OR fractures OR osteoblast-like cells OR osteoblasts)”. The electronic database search was supplemented by a manual search of the reference lists of included articles. The titles and abstracts of the search results were initially evaluated, and then the full-text manuscript was reviewed. Disagreements were resolved by discussion, and a third author conducted an independent review if the agreement was not reached.
Eligibility Criteria
The inclusion criteria for all studies were as follows: (1) Original research. (2) Studies reporting the procedure of PRP preparation. (3) Studies written in English. Additional inclusion criteria for in vitro basic studies were as follows: (1) The domain had to be an osteoblast-like cell line. (2). Studies reporting the in vitro effect of PRP on osteoblast-like cells. Additional inclusion criteria for in vivo preclinical studies (animal studies) and clinical studies were as follows: (1) Prospective or retrospective controlled studies. (2) Studies involving the local application of PRP for bone fracture treatment. The exclusion criteria for all studies were as follows: (1) Duplicated publications. (2) Case reports, comment papers, and correspondence. (3) Reviews. (4) Studies involving stem cells or other biomaterial scaffolds. Furthermore, any disagreements were resolved by discussion and consensus with a third reviewer.
Data Extraction and Analysis
Two reviewers independently extracted data from each included study. The following data were extracted from in vitro preclinical studies: author, center, types of cells, effects of PRP on cells. The following data were extracted from in vivo preclinical studies: author, medical center, animal model, types of bone, treatment groups, PRP injection volume, the period of follow up, the procedure of PRP preparation, outcomes. The following data were extracted from clinical studies: author, medical center, study design, the number of patients, the average age of participants, types of bone, PRP injection volume, the period of follow-up, the procedure of PRP preparation, clinical outcomes. Due to the high heterogeneity of the included studies, a quantitative evaluation of the results was not performed. If there was a dispute between the two reviewers, it was settled through consultation with a third reviewer.
Assessment of Methodological Quality
Two reviewers independently evaluated the methodological quality of studies in this systematic review, according to the criteria in the Cochrane Collaboration for Systematic Reviews (27). The quality of the in vivo preclinical studies in this systematic review was assessed using the items of the Systematic Review Centre for Laboratory animal Experimentation (SYRCLE) risk of bias (RoB) tool (28). The quality of the clinical studies in this systematic review was assessed using the Cochrane RoB tool (29). Furthermore, any disagreements were resolved by discussion and consensus with a third reviewer.
Results
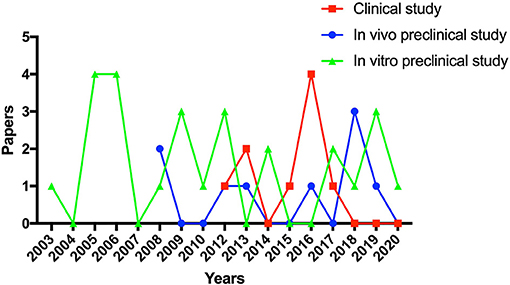
According to the search strategy, 412 relevant publications were screened. Finally, forty-four studies, including twenty-six in vitro preclinical studies (basic studies), nine in vivo preclinical studies (animal studies), and nine clinical studies, met the selection criteria and were enrolled in the present systematic review. The flow diagram of this systematic review is shown in Figure 1. The trend of preclinical and clinical studies published over time is reported in Figure 2. Details of all enrolled studies are summarized in the present systematic review, and the main results will be discussed separately for preclinical and clinical studies in this systematic review.
Preclinical Studies
In Vitro Preclinical Studies
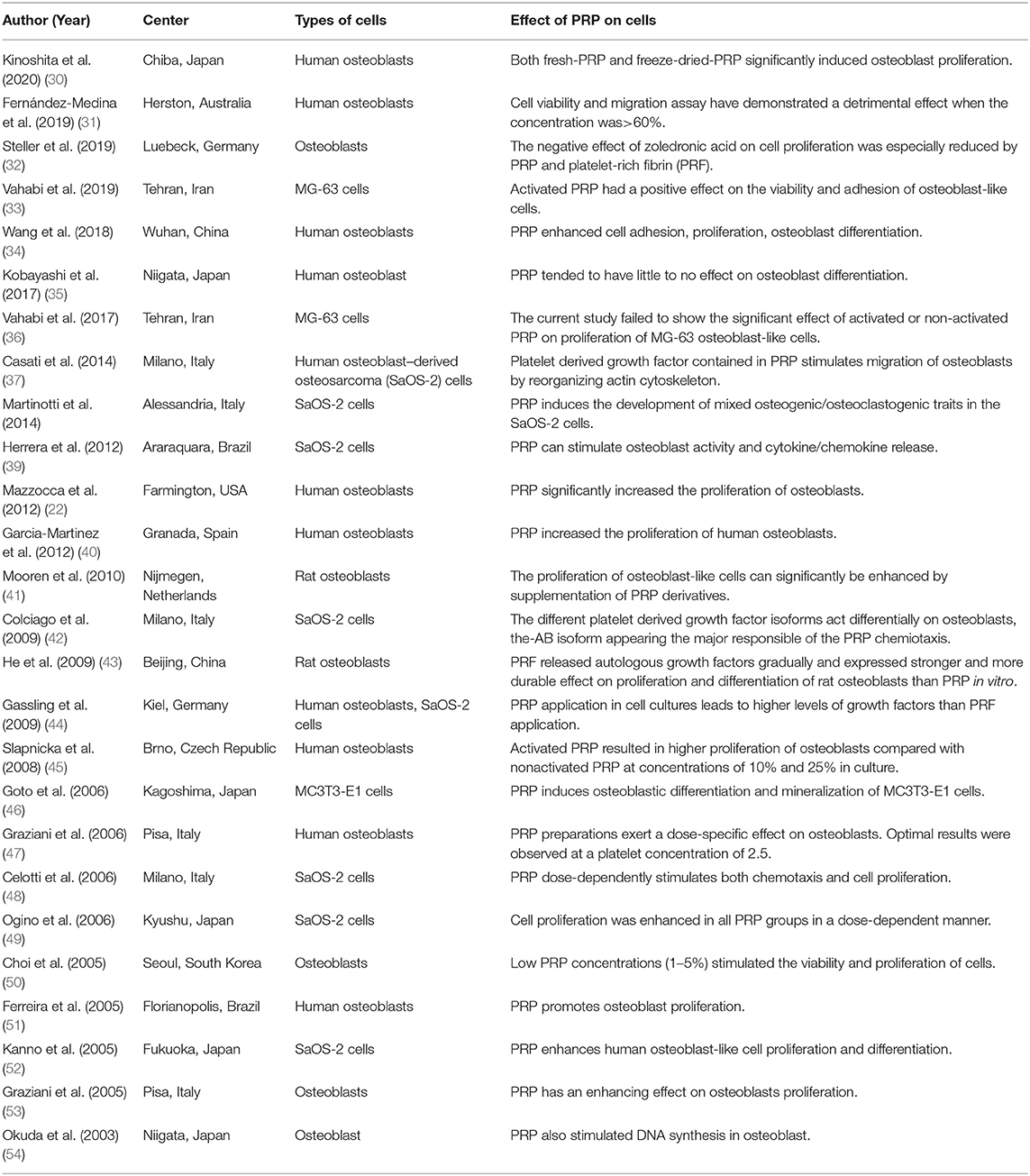
Twenty-six studies (22, 30–54) investigated the effect of PRP on osteoblast-like cells. The main details of in vitro studies are shown in Table 1. Among these studies, six studies were performed in Italy, six in Japan, two in Germany, two in Iran, two in China, two in Brazil, each one in Australia, Spain, USA, Netherlands, South Korea, and Czech Republic. Many kinds of osteoblast-like cells, including osteoblasts, MG-63 cells, SaOS-2 cells, MC3T3-E1 cells, were discussed in the present systematic review. Seventeen out of all enrolled in vitro preclinical studies reported that PRP enhanced the proliferation of osteoblast-like cells. Seven out of all enrolled studies focused on the effect of PRP on the differentiation, including six studies with positive outcomes, and one study with negative outcomes. Among all enrolled in vitro preclinical studies, four studies found that PRP improved the cell viability of osteoblast-like cells, four with positive outcomes in stimulating the migration of osteoblast-like cells, two with positive outcomes in enhancing the adhesion of osteoblast-like cells. Additionally, one study reported PRP application in osteoblast cultures leads to higher levels of platelet-derived growth factor (PDGF), insulin-like growth factor I (IGF1), and transforming growth factor (TGF) release than platelet-rich fibrin (44). One study reported that PRP application in osteoblast cultures leads to higher levels of TGF, PDGF, vascular endothelial growth factor (VEGF), hepatocyte Growth Factor (HGF), epidermal growth factor (EGF), and IGF1 release than cell medium with 5% or 15% fetal bovine serum (FBS) (22). Two out of all enrolled studies reported growth factor profile of PRP. Ogino et al. reported that the mean levels of TGF-β1, PDGF-AB, and IGF-I in PRP prepared by double-centrifugation were 0.190 ± 0.039, 0.271 6 ± 0.043, and 0.110 ± 0.039 ng/1500 × 103 platelets, respectively (49). Okuda et al. also found that the levels of PDGF-AB, and TGF-β1 were also concentrated up to 182.0 ng/ml and 140.9 ng/ml, respectively (54). Only two studies focused on mechanisms of the PRP effect. Casati et al. demonstrated that PDGF contained in PRP stimulates migration of osteoblasts by reorganizing actin cytoskeleton (37), while Kinoshita et al. found that PRP induced osteoblast proliferation via PDGF receptor-mediated signal transduction (30).
In Vivo Preclinical Studies
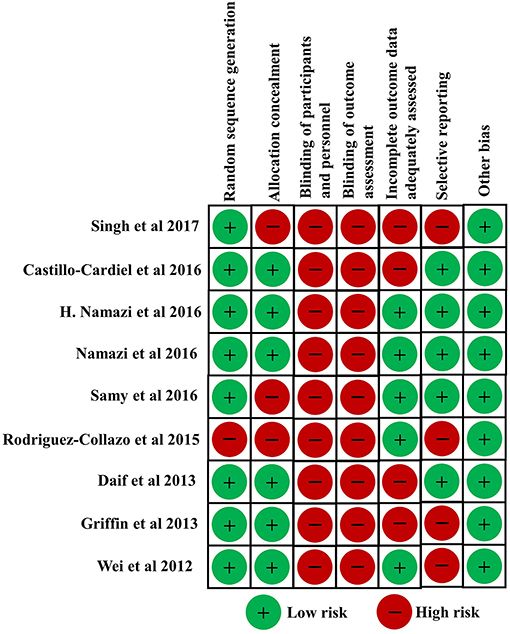
Nine in vivo preclinical studies (55–63) enrolled in this systematic review investigated the effect of PRP in the animal fracture model. The risk of bias of in vivo preclinical studies in this study was independently evaluated by two reviewers. All enrolled in vivo preclinical studies were considered to be of high quality. Risk of bias of all animal studies are shown in Figure 3. Among these studies, six studies carried out randomization. All enrolled animal studies reported a low risk of bias of baseline characteristics. Four studies conducted allocation concealment. Additionally, all enrolled animal studies reported a high risk of bias of random housing, blinding of researchers to intervention, and random outcome assessment. Eight studies reported a low risk of bias of free of selective outcome reporting. In addition, other obvious sources of bias in the animal studies were not detected.
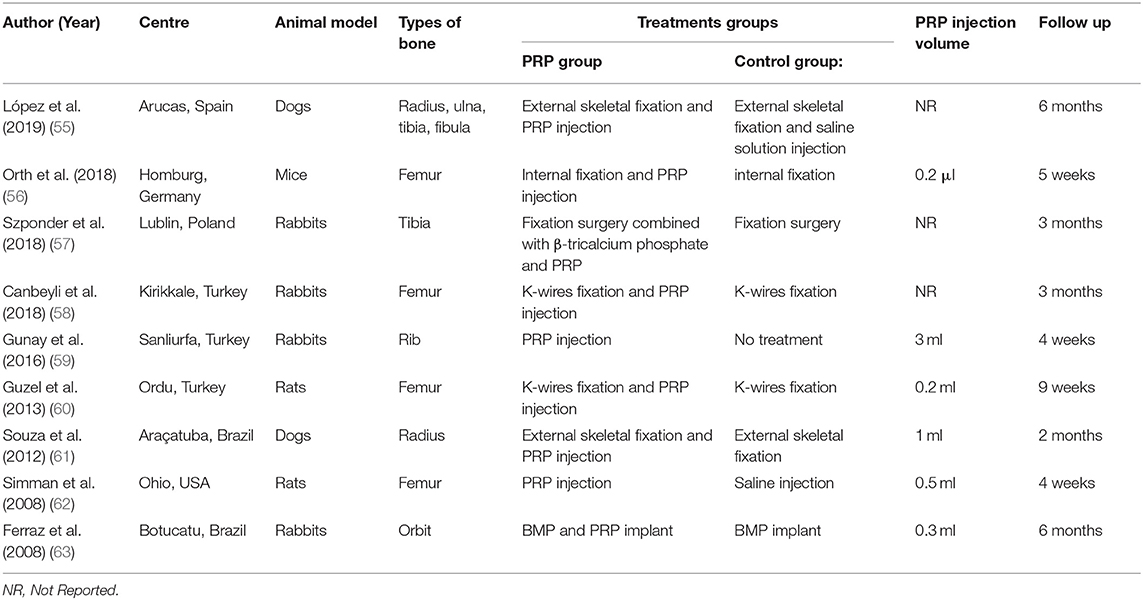
The main details of all these animal studies are shown in Table 2. Among these animal studies, three studies were performed in Turkey, two in Brazil, each one in Spain, Germany, Poland, and USA. The type of animal model varied among the studies. The most used animal is rabbit (44%), followed by rat (22%), dog (22%), and mice (11%). Additionally, femur fracture (44%) is the most commonly used fracture model in all enrolled animal studies.
The most used treatment for bone fracture in animal fracture models is fixation surgery combined with PRP injection (67%), followed by PRP injection alone (22%), and the local administration of PRP plus BMP (11%). Six animal studies reported the volume of PRP injection, ranging from 0.2μl to 3ml. The follow-up duration of all animal studies ranged from 1 to 6 months.
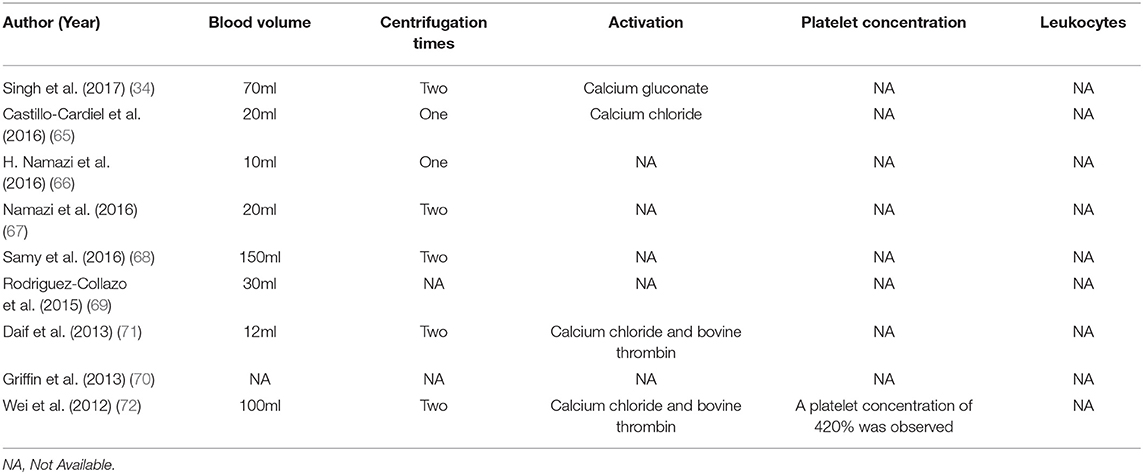
All enrolled animal studies reported the procedures of PRP preparation, which are shown in Table 3. The PRP in animal studies are isolated from the respective animal models. Seven studies reported the blood volume used for PRP preparation, ranging from 1ml to 20ml. The most used centrifugation technique for PRP preparation is double centrifugation technique (67%), followed by single centrifugation technique (33%). Four studies reported PRP activation is calcium chloride while the second most used PRP activation was the combination of calcium chloride and bovine thrombin followed by bovine thrombin, and calcium gluconate. Three studies reported the platelet concentration in PRP, ranging from 2- to 4- fold over peripheral blood. Additionally, only one study tested the number of leukocytes in PRP.
The main outcomes in vivo preclinical studies are shown in Table 3. Seven studies conducted a radiographic evaluation of the PRP group and Control group. Of these seven preclinical studies, five studies (71%) reported positive and two studies (29%) reported negative radiographic outcomes. Eight studies conducted a histopathological evaluation of the PRP group and Control group. Of these eight studies, seven (88%) studies reported positive and one studies (13%) reported negative histopathological outcomes. Additionally, only three studies performed biomechanical tests of the PRP group and Control group. Of these three studies, two studies (67%) reported positive and one study (33%) reported negative biomechanical outcomes.
Clinical Studies
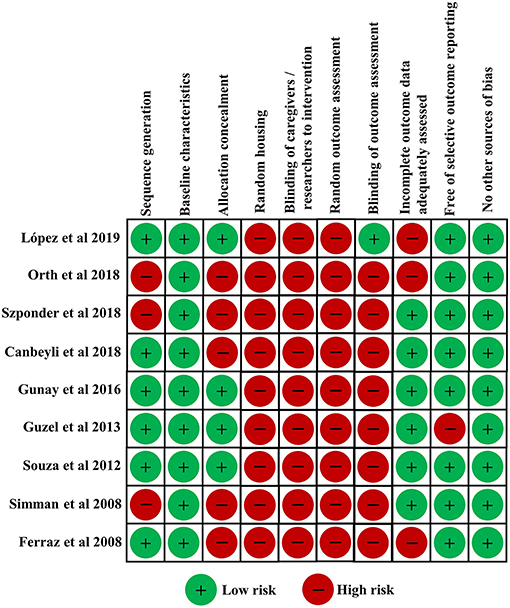
Nine clinical studies (64–72) in this systematic review investigated the clinical effect of PRP for bone fracture treatment. The risk of bias of clinical studies in this study was independently evaluated by two reviewers according to the criteria in the Cochrane Collaboration for Systematic Reviews. All enrolled clinical studies were considered to be of high quality. Risk of bias of all enrolled clinical studies are shown in Figure 4. Among these studies, eight studies carried out randomization. Six studies conducted allocation concealment. None of the studies reported blinding of participants and personnel, or described blinding of outcome assessment. Five studies reported a low risk of bias of incomplete outcome data. In addition, other obvious sources of bias in the trials were not detected.
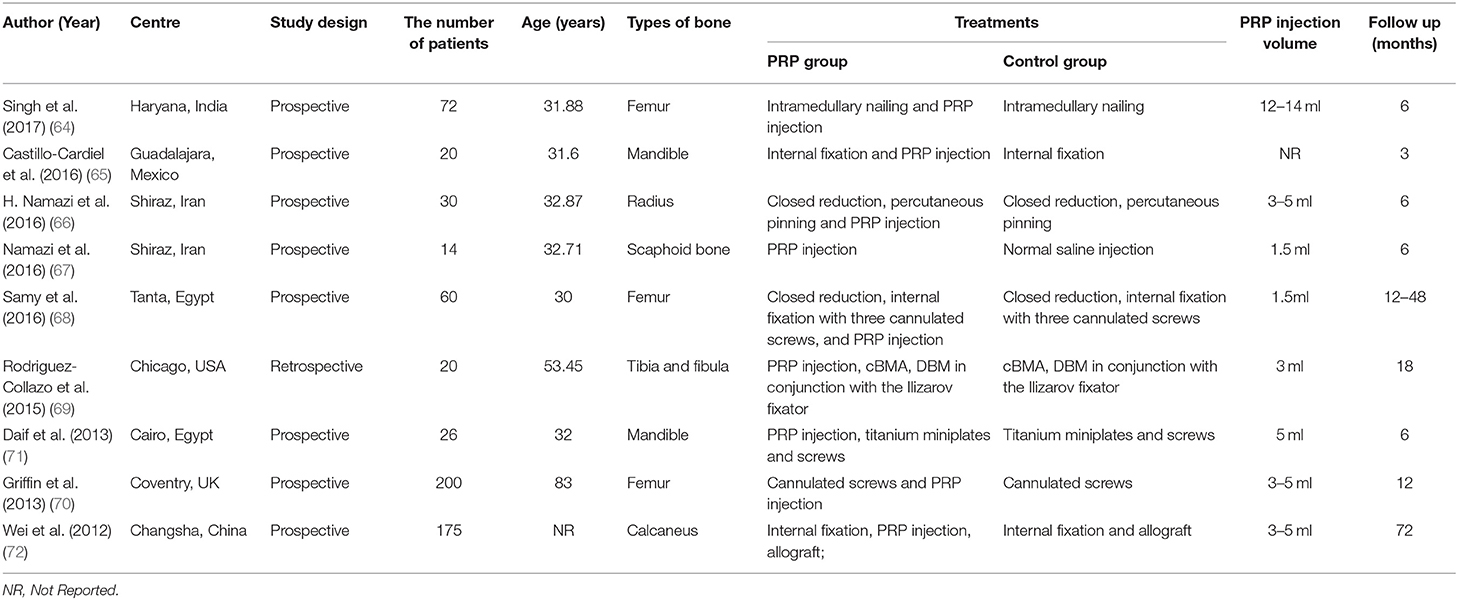
The demographic characteristics of clinical studies are shown in Table 4. Among all these enrolled studies, two studies were performed in Iran, two in Egypt, each one in USA, UK, Mexico, Indian, and China. The sample size of all these clinical studies ranged from 14 to 200. Eight studies reported the average age of patients, ranging from 30 to 83 years old. The most common fracture in these studies is femoral fracture (33%), followed by mandibular fracture (22%), radius fracture (11%), scaphoid fracture (11%), tibial and fibular fracture (11%), calcaneal fracture (11%). Only one study reported the smoking status of patients, and no significant differences of number of currently smoking patients were found between PRP group and control group (70). Among these clinical studies, eight studies applied local PRP injection combined with fixation surgeries in treatment for fracture patients, while only one study applied PRP injection alone as bone fracture treatment. Eight studies reported the volume of PRP injection, ranging from 1.5 to 14 ml. The follow-up period of all enrolled studies ranged from 3 to 72 months.
All enrolled clinical studies reported the procedures of PRP preparation, which are shown in clinical studies is shown in Table 5. Eight studies (89%) reported the blood volume used for PRP preparation, ranging from 10 to 150ml. Seven studies reported centrifugation times during the procedure of PRP preparation, including five studies with double centrifugation technique and two studies with single centrifugation technique. Four studies used PRP activation, including one study with calcium gluconate, one study with calcium chloride, and two studies with calcium chloride and bovine thrombin. Only one study investigated the platelet concentration in PRP, which is 420% over peripheral blood. Additionally, none study investigated the number of leukocytes in PRP.
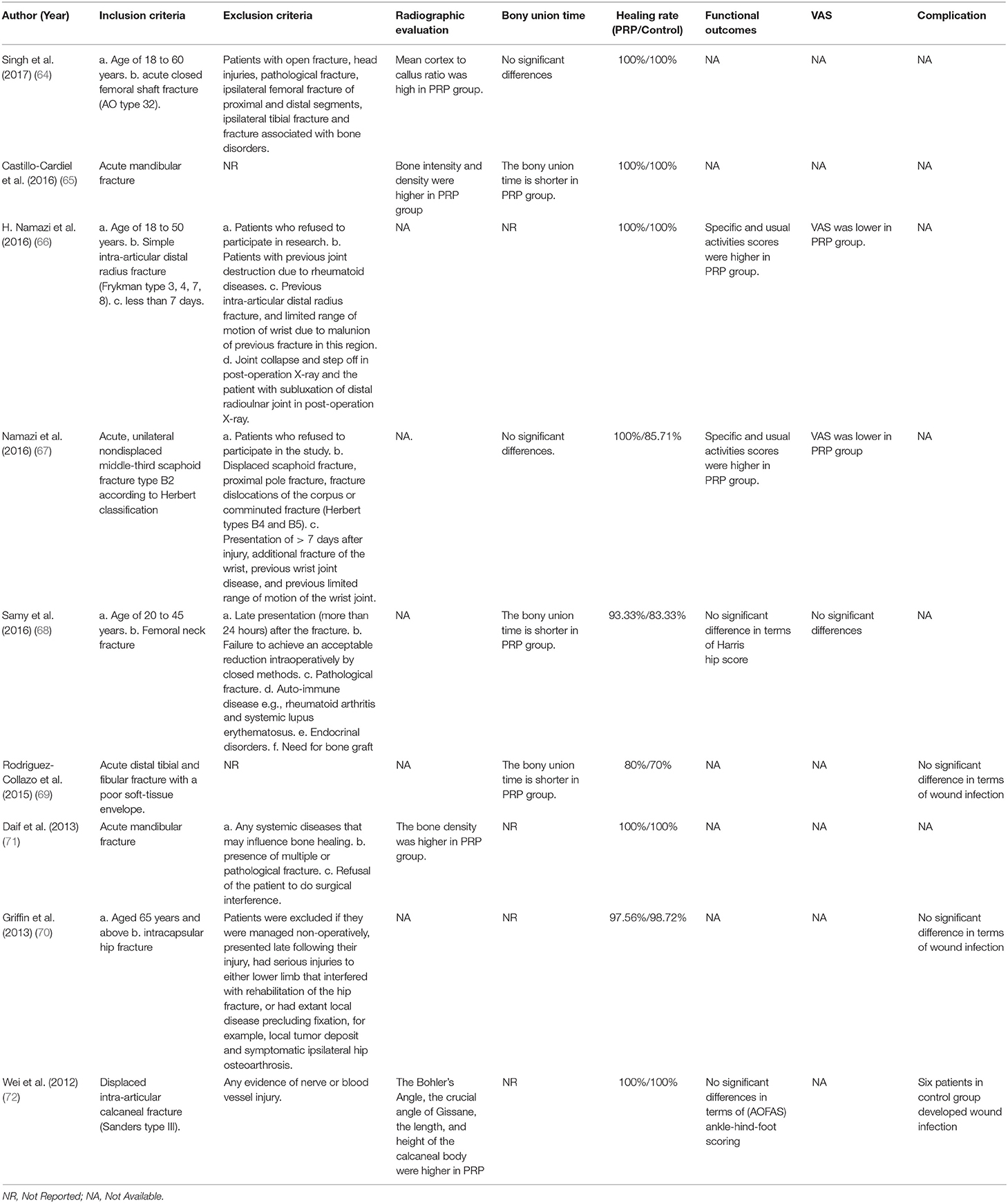
The inclusion criteria, exclusion criteria, and main outcomes of fracture patients in enrolled clinical studies are shown in Table 6. Among these studies, four studies performed a radiographic evaluation of fracture patients. Singh et al. found that the intraoperative application of PRP led to a higher mean cortex to callus ratio when dealing with diaphyseal femur fracture (64). Castillo-Cardiel et al. (65) and Daif et al. (71) reported the local administration of PRP increased the bone density of mandibular patients. Additionally, Wei et al. reported that intraoperative application of PRP led to superior results of Bohler's Angle, the crucial angle of Gissane, and length, width, and height of the calcaneal body regarding radiographic assessment at 24 months and 72 months postoperatively (72). Five studies reported the bony union time of fracture patients. Also, in this case, results were controversial. Three studies (60%) reported positive and two studies (40%) reported negative results in terms of bony union time. Eight studies investigated the bone healing rate of fracture patients at the final follow up. Among these studies, seven studies (88%) reported no significant difference between the PRP group and Control group. Only one study (13%) showed superior results in the PRP group (68). Only two studies reported the information on revision surgery. Samy et al. reported that revision surgery was done for non-union cases with femoral neck fracture (68). Rodriguez-Collazo et al. reported that of the two patients in the PRP group who experienced delayed union, only one revision was required due to consistent pain (69). Four studies reported functional outcomes. Two studies reported that specific and usual activities scores were higher in PRP group (66, 67). Samy et al. reported that no significant differences were observed in terms of Harris hip score between PRP group and control group when dealing with femoral neck fracture (68). Wei et al. reported that no significant differences were observed in terms of AOFAS scores between PRP group and control group when dealing with displaced intra-articular calcaneal fracture (72). Three studies evaluated VAS scores of fracture patients. Two studies found that VAS scores were significantly lower in PRP group (66, 67). While Samy et al. reported that no significant differences were observed in terms of VAS scores between PRP group and control group when dealing with femoral neck fracture (68).
Among these studies, only three studies reported postoperative wound infection, which is a type of fracture-related infection. Griffin et al. (70) and Rodriguez-Collazo et al. (69) reported no significant differences were found between the PRP group and Control group. Rodriguez-Collazo et al. reported that the two patients with wound infection were treated with oral antibiotics. Wei et al. (72) reported that the rate of postoperative wound infection in the allograft + PRP group was significantly lower than that of the allograft-only group when dealing with displaced intra-articular calcaneal fracture. Wei et al. reported that six cases of infection in the allograft were treated by sustained suction with negative pressure for a week, and the incision was closed using secondary suturing.
Discussion
As there was no related systematic review published yet, the goal of this overview was to systematically review all available preclinical and clinical studies concerning PRP for bone fracture treatment. The present review confirmed the continuing interest and debate about PRP as an additional treatment for bone fracture. All enrolled studies in this systematic review were published between 2003 and 2020. Among these studies, most of the enrolled studies are preclinical, and clinical researches account for only a small part. Additionally, we found that the most commonly used fracture model in vivo was femur fracture. In our opinion, current enrolled studies are representative of the tendency for application of PRP for bone fracture treatment.
The healing process of bone fracture is complex and involves a well-orchestrated series of biological events initiated by many growth factors in vivo (73–75). Deriving from peripheral blood, PRP can release considerable amounts of growth factors, such as fibroblast growth factor, platelet-derived growth factor, transforming growth factor, vascular endothelial growth factor, insulin-like growth factor, which can activate related intracellular and extracellular molecular-signaling pathways to enhance bone regeneration (76, 77). Theoretically, the rationale behind PRP use in bone fracture treatment is that PRP constitutes a high concentration of autologous growth factors that are critical to regulate the tissue healing process, which is quite similar in all kinds of tissues (78). The main intent of in vitro preclinical studies in present systematic review is to investigate the effect of PRP on osteoblast-like cells, and the analysis results have highlighted the positive effects an overall positive effect of PRP on osteoblast-like cells. Most of in vitro preclinical studies supported the role of PRP in the adhesion, migration, and proliferation of osteoblast-like cells. Additionally, some studies reported PRP stimulated osteoblast activity and cytokine/chemokine release. Besides some controversial results, most of in vitro preclinical studies in this systematic review induced osteoblastic differentiation. The platelet concentrations in PRP exert a dose-specific effect on osteoblasts. Meanwhile, cell viability and migration assay have demonstrated a detrimental effect at high platelet concentration (31). The positive effects of PRP on osteoblast-like cells provide convincing evidence for the clinical application of PRP as a potent tool to facilitate bone regeneration. Many kinds of cells, including osteoblasts, osteoclasts, and endothelial cells, take part in the different phases of the bone healing process (79–81). Previous studies are mainly about the effect of PRP on osteoblasts, but there are still few studies concerning the effect of PRP on osteoclasts. Vascularization is another important part of bone healing, the angiogenesis effect of PRP has been confirmed by many researches (82–84). However, there are still few studies reporting the angiogenesis effect of PRP in the bone healing process.
For the further clinical application of PRP, as an important part of preclinical research, animal research plays a vital role in effective prediction of PRP administration in vivo. Besides some controversial results, the systematic analysis of animal studies published up to now shows an overall positive effect of PRP in bone fracture treatment in terms of radiographic, histopathological, and biomechanical evaluation, which provide the theoretical basis for the clinical application of PRP in bone fracture. More than half of animal studies performed fixation surgery combined with intraoperative administration of PRP. Most of animal fracture models in this systematic review are small animals like mice, rats, and rabbits, which have advantages of low-cost, easy handling, and short period of bone healing. However, compared to large size animal models, small animals are less reliable in imitating bone structure and anatomy of humans (85). Interestingly, all the enrolled studies using the dog model showed positive results using PRP in bone fracture treatment. In contrast, the controversial results in animal studies mainly come from small animal studies.
The main aim of clinical studies was to investigate the effects of PRP in fracture patients. Most of the enrolled clinical studies performed intraoperative administration of PRP as an additional approach for bone fracture treatment. The systematic analysis of clinical studies shows an overall positive effect of PRP in radiographic evaluation. More than half of the clinical studies reported that PRP shortened bony healing duration. In our opinion, for fracture patients, especially in the elderly, shortening the bone healing time could shorten the bedridden time and immobilization and result in decreasing the incidence of pulmonary infection, thrombosis, and bedsore. Furthermore, the systematic analysis of clinical studies found PRP could not improve the healing rate, which might be associated with a high healing rate of closed fractures. However, the results of functional outcomes and VAS are controversial. Interestingly, all enrolled studies concerning wrist fractures showed that PRP could relieve pain and improve the functional outcomes in patients with wrist fractures. Previous studies found that PRP contains a high level of IL-1 receptor antagonist, which could inhibit IL-1 and result in decreasing the amount of substance P, a significant pain transmitter (86, 87). Also, the high level of hepatocyte growth factor (HGF) in PRP could also mediate the signal of NF-kb, resulting in decreasing the level of Cox-1, Cox-2, PGE2 (88). The incidence of postoperative complications is an important index to evaluate the clinical safety of PRP. Currently, no severe complications were reported in all enrolled studies.
All enrolled animal and clinical studies reported the procedure of PRP preparation. The most commonly used PRP activator in animal and clinical studies is calcium chloride. More than half of animal and clinical studies performed two centrifugation times in PRP preparation. Although the easy procedure of preparation and the promising results make PRP a potential therapeutic method to promote bone healing, the PRP preparation procedures of animal studies and clinical studies are heterogeneous. Many different methods of PRP preparation were reported in enrolled animal and clinical studies, leading to a difficult interpretation of PRP regenerative properties in the process of bone healing. Additionally, the effect of different centrifugation times and different activators on the osteogenic ability of PRP is still unclear. Additionally, leukocytes have many important roles in process of tissue healing, and their inclusion in PRP results in increased platelet concentrations (89–91). Generally, the levels of PDGF and TGF-β1 were higher in preparations that contain leukocytes compared to leukocyte-poor PRP (92). Leukocytes could not only secrete many growth factors, such as PDGF, VEGF, TGF-β1, and IGF, but also express many proteinases, including serine and metalloproteinases (93, 94). Consequently, leukocyte-rich PRP could attract other leukocytes, prevent infection, and enhance platelet production by megakaryocytes (95). However, some researchers found that leukocytes damaged surrounding tissues by excessive release of reactive oxygen species, which results in diminishing PRP efficacy in the process of tissue healing (89, 96). However, there are few studies focusing on the differences between leukocyte-rich PRP and leukocyte-poor PRP when dealing with bone fracture. In our opinion, further researches are still needed to investigate the role of leukocytes in PRP for the bone healing process.
There are several limitations to this systematic review. Firstly, due to the high heterogeneity of the enrolled animal and clinical studies in the present review, a meta-analysis of the main results was not performed. Secondly, there are many different protocols of PRP use in enrolled studies and lack of standardization in PRP preparation procedures. Long-term consensus on the standardization of PRP for bone fracture treatments still needs further large-scale trials. Additionally, the characteristics of PRP in enrolled studies, such as platelet concentration, the numbers of leukocytes, were not discussed in detail in the enrolled studies. Thirdly, PRP might also be a promising approach in the treatment of patients with a pathological fracture or periprosthetic fracture. However, all enrolled clinical studies in this systematic review were performed in the patients with traumatic fracture.
Conclusion
The present systematic review confirmed the continuing interests of PRP as an additional treatment for bone fracture. Preclinical studies highlighted the potential value of PRP as promising therapy for bone fracture. However, the preclinical evidence did not translate into a similar result in the clinical studies. PRP can shorten fracture healing time, but it cannot improve fracture healing rate in fracture patients. Meanwhile, characteristics of PRP, such as platelet concentration, the numbers of leukocytes, still need further researches. Although the present systematic review could not fully prove the role of PRP in bone healing, the easy procedure of preparation and the promising results make PRP a potential therapeutic method for bone fracture treatment.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Author Contributions
XD: conceptualization and supervision. FX and YZ: methodology, resources, and data extraction. RL: software. YZ and FX: validation. FX and RL: formal analysis. FX: investigation. YZ: writing—original draft preparation, writing—review, and editing. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by the National Natural Science Foundation of China (31870961, 81501879), the Sino-German Center for Research Promotion (GZ1219), the International Cooperation Project of the Science and Technology Department of Sichuan Province (Grant Nos. 2015HH0049 and 2017SZ0127) and the National Clinical Research Center for Geriatrics, West China Hospital, Sichuan University (Z2018A11).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Mester A, Apostu D, Ciobanu L, Piciu A, Lucaciu O, Campian RS, et al. The impact of proton pump inhibitors on bone regeneration and implant osseointegration. Drug Metab Rev. (2019) 51:330–339. doi: 10.1080/03602532.2019.1610767
2. Tse JJ, Brunet SC, Salat P, Hazlewood GS, Barnabe C, Manske SL. Multi-modal imaging to assess the interaction between inflammation and bone damage progression in inflammatory arthritis. Front Med. (2020) 7:608. doi: 10.3389/fmed.2020.545097
3. Tay SH, Yeo JG, Leong JY, Albani S, Arkachaisri T. Juvenile spondyloarthritis: what more do we know about HLA-B27, enthesitis, and new bone formation? Front Med. (2021) 8:666772. doi: 10.3389/fmed.2021.666772
4. Freeman FE, Brennan MÁ, Browe DC, Renaud A, De Lima J, Kelly DJ, et al. A developmental engineering-based approach to bone repair: endochondral priming enhances vascularization and new bone formation in a critical size defect. Front Bioeng Biotechnol. (2020) 8:230. doi: 10.3389/fbioe.2020.00230
5. Pizzonia M, Casabella A, Natali M, Petrocchi L, Carmisciano L, Nencioni A, et al. Osteosarcopenia in very old age adults after hip fracture: a real-world therapeutic standpoint. Front Med. (2021) 8:612506. doi: 10.3389/fmed.2021.612506
6. Ayus JC, Fuentes N, Go AS, Achinger SG, Moritz ML, Nigwekar SU, et al. Chronicity of uncorrected hyponatremia and clinical outcomes in older patients undergoing hip fracture repair. Front Med. (2020) 7:263. doi: 10.3389/fmed.2020.00263
7. Audigé L, Griffin D, Bhandari M, Kellam J, Rüedi TP. Path analysis of factors for delayed healing and nonunion in 416 operatively treated tibial shaft fractures. Clin Orthop Relat Res. (2005) 438:221–32. doi: 10.1097/01.blo.0000163836.66906.74
8. Chen P-E, Chien C-W, Tung T-H. The relationship between fragility fractures and pain experience: a systematic review. Front Med. (2021) 8:705. doi: 10.3389/fmed.2021.609318
9. Kang DW, Wang S-M, Um YH, Na H-R, Kim N-Y, Han K, et al. Differential risk of incident fractures depending on intensity and frequency of physical activity according to cognitive status: a nationwide longitudinal study. Front Med. (2020) 7:921. doi: 10.3389/fmed.2020.572466
10. Colais P, Martino MD, Fusco D, Perucci CA, Davoli M. The effect of early surgery after hip fracture on 1-year mortality. BMC Geriatrics. (2015) 15:1–8. doi: 10.1186/s12877-015-0140-y
11. Levi Y, Punchik B, Zikrin E, Shacham D, Katz D, Makulin E, et al. Intensive inpatient vs. home-based rehabilitation after hip fracture in the elderly population, Front Med. (2020) 7:592693. doi: 10.3389/fmed.2020.592693
12. Nauth A, Giannoudis PV, Einhorn TA, Hankenson KD, Friedlaender GE, Li R, et al. Growth factors: beyond bone morphogenetic proteins. J Orthop Trauma. (2010) 24:543–6. doi: 10.1097/BOT.0b013e3181ec4833
13. Bharadwaz A, Jayasuriya AC. Osteogenic differentiation cues of the bone morphogenetic protein-9 (BMP-9) and its recent advances in bone tissue regeneration. Mater Sci Eng. (2021) 120:111748. doi: 10.1016/j.msec.2020.111748
14. Zuk PA, Zhu M, Mizuno H, Huang J, Futrell JW, Katz AJ, et al. Multilineage cells from human adipose tissue: implications for cell-based therapie. Tissue Eng. (2001) 7:211–28. doi: 10.1089/107632701300062859
15. Liu H, Li D, Zhang Y, Li M. Inflammation, mesenchymal stem cells and bone regeneration. Histochem. Cell Biol. (2018) 149:393–404. doi: 10.1007/s00418-018-1643-3
16. Alomari EB, Sultan K. Efficacy of injectable platelet-rich plasma in reducing alveolar bone resorption following rapid maxillary expansion: A cone-beam computed tomography assessment in a randomized split-mouth controlled trial. Angle Orthodontist. (2019) 89:705–12. doi: 10.2319/091018-661.1
17. Cheng A, Schwartz Z, Kahn A, Li X, Shao Z, Sun M, et al. Advances in porous scaffold design for bone and cartilage tissue engineering and regeneration. Tissue Eng B: Rev. (2018) 25:14–29. doi: 10.1089/ten.teb.2018.0119
18. Harrison A, Lin S, Pounder N, Mikuni-Takagaki Y. Mode & mechanism of low intensity pulsed ultrasound (LIPUS) in fracture repair. Ultrasonics. (2016) 70:45–52. doi: 10.1016/j.ultras.2016.03.016
19. Busse JW, Bhandari M, Einhorn TA, Schemitsch E, Heckman JD, Tornetta P, et al. Re-evaluation of low intensity pulsed ultrasound in treatment of tibial fractures (TRUST): randomized clinical trial. BMJ. (2016) 355:i5351. doi: 10.1136/bmj.i5351
20. Boesen AP, Hansen R, Boesen MI, Malliaras P, Langberg H. Effect of high-volume injection, platelet-rich plasma, and sham treatment in chronic midportion achilles tendinopathy: a randomized double-blinded prospective study. Am J Sports Med. (2017) 45:2034–43. doi: 10.1177/0363546517702862
21. Scott A, LaPrade RF, Harmon KG, Filardo G, Kon E, Della Villa S, et al. Platelet-rich plasma for patellar tendinopathy: a randomized controlled trial of leukocyte-rich PRP or leukocyte-poor PRP versus saline. Am J Sports Med. (2019) 47:1654–61. doi: 10.1177/0363546519837954
22. Mazzocca AD, McCarthy MBR, Chowaniec DM, Dugdale EM, Hansen D, Cote MP, et al. The positive effects of different platelet-rich plasma methods on human muscle, bone, tendon cells. Am J Sports Med. (2012) 40:1742–9. doi: 10.1177/0363546512452713
23. Hemeda H, Giebel B, Wagner W. Evaluation of human platelet lysate versus fetal bovine serum for culture of mesenchymal stromal cells. Cytotherapy. (2014) 16:170–80. doi: 10.1016/j.jcyt.2013.11.004
24. Mazzucco L, Balbo V, Cattana E, Borzini P. Platelet-rich plasma and platelet gel preparation using Plateltex®. Vox Sanguinis. (2008) 94:202–8. doi: 10.1111/j.1423-0410.2007.01027.x
25. Devereaux J, Nurgali K, Kiatos D, Sakkal S, Apostolopoulos V. Effects of platelet-rich plasma and platelet-poor plasma on human dermal fibroblasts. Maturitas. (2018) 117:34–44. doi: 10.1016/j.maturitas.2018.09.001
26. van Tulder MW, Assendelft WJ, Koes BW, Bouter LM. Method guidelines for systematic reviews in the Cochrane Collaboration Back Review Group for spinal disorders. Spine. (1997) 22:2323–30. doi: 10.1097/00007632-199710150-00001
27. Corbett MS, Higgins JP, Woolacott NF. Assessing baseline imbalance in randomised trials: implications for the Cochrane risk of bias tool. Res Synth Method. (2014) 5:79–85. doi: 10.1002/jrsm.1090
28. Hooijmans CR, Rovers MM, de Vries RBM, Leenaars M, Ritskes-Hoitinga M, Langendam MW, SYRCLE's risk of bias tool for animal studies. BMC Med Res Methodol. (2014) 14:43. doi: 10.1186/1471-2288-14-43
29. Higgins JPT, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. (2011) 343:d5928. doi: 10.1136/bmj.d5928
30. Kinoshita H, Orita S, Inage K, Fujimoto K, Shiga Y, Abe K, et al. Freeze-dried platelet-rich plasma induces osteoblast proliferation via platelet-derived growth factor receptor-mediated signal transduction. Asian Spine J. (2020) 14:1–8. doi: 10.31616/asj.2019.0048
31. Fernández-Medina T, Vaquette C, Ivanovski S. Systematic comparison of the effect of four clinical-grade platelet rich hemoderivatives on osteoblast behaviour. Int J Mol Sci. (2019) 20:6243. doi: 10.3390/ijms20246243
32. Steller D, Herbst N, Pries R, Juhl D, Hakim SG. Positive impact of Platelet-rich plasma and Platelet-rich fibrin on viability, migration and proliferation of osteoblasts and fibroblasts treated with zoledronic acid. Sci Report. (2019) 9:8310. doi: 10.1038/s41598-019-43798-z
33. Vahabi S, Yadegary Z, Karamshahi M. Evaluating the adhesion of human gingival fibroblasts and MG-63 osteoblast-like cells to activated PRP-coated membranes. Cell Tissue Bank. (2019) 20:339–49. doi: 10.1007/s10561-019-09772-9
34. Wang X, Zhang Y, Choukroun J, Ghanaati S, Miron RJ. Effects of an injectable platelet-rich fibrin on osteoblast behavior and bone tissue formation in comparison to platelet-rich plasma. Platelets. (2018) 29:48–55. doi: 10.1080/09537104.2017.1293807
35. Kobayashi E, Fujioka-Kobayashi M, Sculean A, Chappuis V, Buser D, Schaller B, et al. Effects of platelet rich plasma (PRP) on human gingival fibroblast, osteoblast and periodontal ligament cell behaviour. BMC Oral Health. (2017) 17:91. doi: 10.1186/s12903-017-0388-z
36. Vahabi S, Yadegari Z, Mohammad-Rahimi H. Comparison of the effect of activated or non-activated PRP in various concentrations on osteoblast and fibroblast cell line proliferation. Cell Tissue Bank. (2017) 18:347–53. doi: 10.1007/s10561-017-9640-7
37. Casati L, Celotti F, Negri-Cesi P, Sacchi MC, Castano P, Colciago A. Platelet derived growth factor (PDGF) contained in Platelet Rich Plasma (PRP) stimulates migration of osteoblasts by reorganizing actin cytoskeleton. Cell Adhes Migr. (2014) 8:595–602. doi: 10.4161/19336918.2014.972785
38. Simona M, Laura M, Valeria B, Mauro P, Marco M, Elia R, et al. Platelet-rich plasma induces mixed osteogenic/osteoclastogenic phenotype in osteosarcoma SaOS-2 cells: role of TGF-Beta, Curr Pharm Biotechnol. (2014) 15:120–6. doi: 10.2174/1389201015666140604121407
39. Herrera BS, Coimbra LS, Bastos AS, Teixeira SA, Steffens JP, Muscara MN, et al. Platelet-rich plasma stimulates cytokine expression and alkaline phosphatase activity in osteoblast-derived osteosarcoma cells. Arch Oral Biol. (2012) 57:1282–9. doi: 10.1016/j.archoralbio.2012.03.004
40. García-Martínez O, Reyes-Botella C, Díaz-Rodríguez L, De Luna-Bertos E, Ramos-Torrecillas J, Vallecillo-Capilla MF, et al. Effect of platelet-rich plasma on growth and antigenic profile of human osteoblasts and its clinical impact. J Oral Maxillofac Surg. (2012) 70:1558–64. doi: 10.1016/j.joms.2011.06.199
41. Mooren RECM, Hendriks EJ, van den Beucken JJJP, Merkx MAW, Meijer GJ, Jansen JA, et al. The effect of platelet-rich plasma in vitro on primary cells: rat osteoblast-like cells and human endothelial cells. Tissue Eng A. (2010) 16:3159–72. doi: 10.1089/ten.tea.2009.0832
42. Colciago A, Celotti F, Casati L, Giancola R, Castano SM, Antonini G, et al. In Vitro effects of PDGF isoforms (AA, BB, AB and CC) on migration and proliferation of SaOS-2 osteoblasts and on migration of human osteoblasts. Int J Biomed Sci. (2009) 5:380−9.
43. He L, Lin Y, Hu X, Zhang Y, Wu H. A comparative study of platelet-rich fibrin (PRF) and platelet-rich plasma (PRP) on the effect of proliferation and differentiation of rat osteoblasts in vitro. Oral Surg Oral Med Oral Pathol Oral RadiolEndod. (2009) 108:707–13. doi: 10.1016/j.tripleo.2009.06.044
44. Gaßling VLW, Açil Y, Springer IN, Hubert N, Wiltfang J. Platelet-rich Plasma and Platelet-rich fibrin in human cell culture. Oral Surg Oral Med Oral Pathol Oral RadiolEndod. (2009) 108:48–55. doi: 10.1016/j.tripleo.2009.02.007
45. Slapnicka J, Fassmann A, Strasak L, Augustin P, Vanek J. Effects of activated and nonactivated platelet-rich plasma on proliferation of human osteoblasts in vitro. J Oral Maxillofac Surg. (2008) 66:297–301. doi: 10.1016/j.joms.2007.05.022
46. Goto H, Matsuyama T, Miyamoto M, Yonamine Y, Izumi Y. Platelet-rich plasma/osteoblasts complex induces bone formation via osteoblastic differentiation following subcutaneous transplantation. J Periodont Res. (2006) 41:455–62. doi: 10.1111/j.1600-0765.2006.00892.x
47. Graziani F, Ivanovski S, Cei S, Ducci F, Tonetti M, Gabriele M. The in vitro effect of different PRP concentrations on osteoblasts and fibroblasts. Clin Oral Implants Res. (2006) 17:212–9. doi: 10.1111/j.1600-0501.2005.01203.x
48. Celotti F, Colciago A, Negri-Cesi P, Pravettoni A, Zaninetti R, Sacchi MC. Effect of platelet-rich plasma on migration and proliferation of SaOS-2 osteoblasts: role of platelet-derived growth factor and transforming growth factor-β. Wound Repair Regen. (2006) 14:195–202. doi: 10.1111/j.1743-6109.2006.00110.x
49. Ogino Y, Ayukawa Y, Kukita T, Koyano K. The contribution of platelet-derived growth factor, transforming growth factor-β1, and insulin-like growth factor-I in platelet-rich plasma to the proliferation of osteoblast-like cells. Oral Surg Oral Med Oral Pathol Oral RadiolEndod. (2006) 101:724–9. doi: 10.1016/j.tripleo.2005.08.016
50. Choi BH, Zhu SJ, Kim BY, Huh JY, Lee SH, Jung JH. Effect of platelet-rich plasma (PRP) concentration on the viability and proliferation of alveolar bone cells: an in vitro study. Int J Oral Maxillofac Surg. (2005) 34:420–4. doi: 10.1016/j.ijom.2004.10.018
51. Ferreira CF, Carriel Gomes MC, Filho JS, Granjeiro JM, Oliveira Simões CM, Magini RdS. Platelet-rich plasma influence on human osteoblasts growth. Clin Oral Implants Res. (2005) 16:456–60. doi: 10.1111/j.1600-0501.2005.01145.x
52. Kanno T, Takahashi T, Tsujisawa T, Ariyoshi W, Nishihara T. Platelet-rich plasma enhances human osteoblast-like cell proliferation and differentiation. J Oral Maxillofac Surg. (2005) 63:362–9. doi: 10.1016/j.joms.2004.07.016
53. Graziani F, Cei S, Ducci F, Giuca MR, Donos N, Gabriele M. In vitro effects of different concentration of PRP on primary bone and gingival cell lines. Preliminary results. Minerva Stomatol. (2005) 54:15–22.
54. Okuda K, Kawase T, Momose M, Murata M, Saito Y, Suzuki H, Wolff LF, Yoshie H. Platelet-rich plasma contains high levels of platelet-derived growth factor and transforming growth factor-β and modulates the proliferation of periodontally related cells in vitro. J Periodontol. (2003) 74:849–57. doi: 10.1902/jop.2003.74.6.849
55. López S, Vilar JM, Sopena JJ, Damià E, Chicharro D, Carrillo JM, et al. Assessment of the efficacy of platelet-rich plasma in the treatment of traumatic canine fractures. Int J Mol Sci. (2019) 20:1075. doi: 10.3390/ijms20051075
56. Orth M, Shadmanov T, Scheuer C, Braun BJ, Fritz T, Holstein JH, et al. Marble-derived microcalcite improves bone healing in mice osteotomy. Biomed Mater. (2018) 14:025001. doi: 10.1088/1748-605X/aaee54
57. Szponder T, Wessely-Szponder J, Sobczyńska-Rak A, Zylińska B, Radzki RP, Polkowska I. Application of platelet-rich plasma and tricalcium phosphate in the treatment of comminuted fractures in animals. In Vivo. (2018) 32:1449–55. doi: 10.21873/invivo.11398
58. Canbeyli ID, Akgun RC, Sahin O, Terzi A, Tuncay IC. Platelet-rich plasma decreases fibroblastic activity and woven bone formation with no significant immunohistochemical effect on long-bone healing: An experimental animal study with radiological outcomes. J Orthop Surg. (2018) 26:2309499018802491. doi: 10.1177/2309499018802491
59. Gunay S, Candan H, Yilmaz R, Eser I, Aydogmus U. The efficacy of platelet-rich plasma in the treatment of rib fractures. Thorac cardiovasc Surg. (2017) 65:546–50. doi: 10.1055/s-0036-1582261
60. Guzel Y, Karalezli N, Bilge O, Kacira BK, Esen H, Karadag H, et al. The biomechanical and histological effects of platelet-rich plasma on fracture healing. Knee Surg, Sports Traumatol Arthrosc. (2015) 23:1378–83. doi: 10.1007/s00167-013-2734-2
61. Souza TFB, Andrade AL, Ferrreira GTNM, Sakamoto SS, Albuquerque VB, Bonfim SRM, et al. Healing and expression of growth factors (TGF-β and PDGF) in canine radial ostectomy gap containing platelet-rich plasma. Vet Comp Orthop Traumatol. (2012) 25:445–52. doi: 10.3415/VCOT-10-10-0146
62. Simman R, Hoffmann A, Bohinc RJ, Peterson WC, Russ AJ. Role of platelet-rich plasma in acceleration of bone fracture healing. Ann Plast Surg. (2008) 61:337–44. doi: 10.1097/SAP.0b013e318157a185
63. Ferraz FH, Schellini SA, Schellini RC, Pellizon CH, Hirai FE, Padovani CR. BMP implant associated with platelet-rich plasma in orbit fracture repair. Curr Eye Res. (2008) 33:293–301. doi: 10.1080/02713680801892020
64. Singh R, Rohilla R, Gawande J, Sehgal PK. To evaluate the role of platelet-rich plasma in healing of acute diaphyseal fractures of the femur. Chin J Traumatol. (2017) 20:39–44. doi: 10.1016/j.cjtee.2016.03.007
65. Castillo-Cardiel G, Medina-Quintana VM, Lomelí-Enríquez M, Medrano-Muñoz F, Guerrero-Velázquez C, Contreras-López CK, et al. Platelet-rich plasma and its effect in bone regeneration in mandibular fractures. Controlled clinical trial. Gac Med Mex. (2017) 153:421–6. doi: 10.24875/GMM.17002574
66. Namazi H, Mehbudi A. Investigating the effect of intra-articular PRP injection on pain and function improvement in patients with distal radius fracture. Orthop Traumatol Surg Res. (2016) 102:47–52. doi: 10.1016/j.otsr.2015.11.002
67. Namazi H, Kayedi T. Investigating the effect of intra-articular platelet-rich plasma injection on union: pain and function improvement in patients with scaphoid fracture. J Hand Microsurg. (2016) 8:140–4. doi: 10.1055/s-0036-1597088
68. Samy AM. The role of platelet rich plasma in management of fracture neck femur: new insights. Int Orthop. (2016) 40:1019–24. doi: 10.1007/s00264-015-2844-1
69. Rodriguez-Collazo ER, Urso ML. Combined use of the Ilizarov method, concentrated bone marrow aspirate (cBMA), and platelet-rich plasma (PRP) to expedite healing of bimalleolar fractures. Strateg Trauma Limb Reconstr. (2015) 10:161–6. doi: 10.1007/s11751-015-0239-x
70. Griffin XL, Achten J, Parsons N, Costa ML. Platelet-rich therapy in the treatment of patients with hip fractures: a single centre, parallel group, participant-blinded, randomised controlled trial. BMJ Open. (2013) 3:e002583. doi: 10.1136/bmjopen-2013-002583
71. Daif ET. Effect of autologous platelet-rich plasma on bone regeneration in mandibular fractures. Dental Traumatol. (2013) 29:399–403. doi: 10.1111/edt.12021
72. Wei LC, Lei GH, Sheng Py, Gao SG, Xu M, Jiang W, et al. Efficacy of platelet-rich plasma combined with allograft bone in the management of displaced intra-articular calcaneal fractures: A prospective cohort study. J Orthop Res. (2012) 30:1570–76. doi: 10.1002/jor.22118
73. Nakamura K, Kurokawa T, Kato T, Okazaki H, Mamada K, Hanada K, et al. Local application of basic fibroblast growth factor into the bone increases bone mass at the applied site in rabbits. Arch Orthop Trauma Surg. (1996) 115:344–6. doi: 10.1007/BF00420329
74. Hu K, Olsen BR. The roles of vascular endothelial growth factor in bone repair and regeneration. Bone. (2016) 91:30–8. doi: 10.1016/j.bone.2016.06.013
75. Lee SS, Kim JH, Jeong J, Kim SHL, Koh RH, Kim I, et al. Sequential growth factor releasing double cryogel system for enhanced bone regeneration. Biomater. (2020) 257:120223. doi: 10.1016/j.biomaterials.2020.120223
76. Hahn O, Kieb M, Jonitz-Heincke A, Bader R, Peters K, Tischer T. Dose-dependent effects of platelet-rich plasma powder on chondrocytes in vitro. Am J Sports Med. (2020) 48:1727–34. doi: 10.1177/0363546520911035
77. Talaat WM, Ghoneim MM, Salah O, Adly OA. Autologous bone marrow concentrates and concentrated growth factors accelerate bone regeneration after enucleation of mandibular pathologic lesions. J Craniofac Surg. (2018) 29:992–7. doi: 10.1097/SCS.0000000000004371
78. Filardo G, Kon E, Roffi A, Di Matteo B, Merli ML, Marcacci M. Platelet-rich plasma: why intra-articular? A systematic review of preclinical studies and clinical evidence on PRP for joint degeneration. Knee Surg Sports Traumatol Arthrosc. (2015) 23:2459–74. doi: 10.1007/s00167-013-2743-1
79. Veronesi F, Fini M, Sartori M, Parrilli A, Martini L, Tschon M. Pulsed electromagnetic fields and platelet rich plasma alone and combined for the treatment of wear-mediated periprosthetic osteolysis: an in vivo study. Acta Biomaterialia. (2018) 77:106–15. doi: 10.1016/j.actbio.2018.07.012
80. Majidinia M, Sadeghpour A, Yousefi B. The roles of signaling pathways in bone repair and regeneration. J Cell Physiol. (2018) 233:2937–48. doi: 10.1002/jcp.26042
81. Böhm A-M, Dirckx N, Tower RJ, Peredo N, Vanuytven S, Theunis K, et al. Activation of skeletal stem and progenitor cells for bone regeneration is driven by PDGFRβ signaling. Dev Cell. (2019) 51:236–54.e12. doi: 10.1016/j.devcel.2019.08.013
82. van der Bijl I, Vlig M, Middelkoop E, de Korte D. Allogeneic platelet-rich plasma (PRP) is superior to platelets or plasma alone in stimulating fibroblast proliferation and migration, angiogenesis, and chemotaxis as relevant processes for wound healing. Transfusion. (2019) 59:3492–500. doi: 10.1111/trf.15535
83. Noh K-C, Park S-H, Yang CJ, Lee GW, Kim MK, Kang Y-H. Involvement of synovial matrix degradation and angiogenesis in oxidative stress-exposed degenerative rotator cuff tears with osteoarthritis. J Shoulder Elbow Surg. (2018) 27:141–50. doi: 10.1016/j.jse.2017.08.007
84. Zhang L, Qiu H, Wang D, Miao H, Zhu Y, Guo Q, et al. Enhanced vascularization and biocompatibility of rat pancreatic decellularized scaffolds loaded with platelet-rich plasma. J Biomater Applic. (2020) 35:313–30. doi: 10.1177/0885328220933890
85. Moran CJ, Ramesh A, Brama PAJ, O'Byrne JM, O'Brien FJ, Levingstone TJ. The benefits and limitations of animal models for translational research in cartilage repair. J Exp Orthop. (2016) 3:1. doi: 10.1186/s40634-015-0037-x
86. Hauser J, Hsu B, Nader ND. Inflammatory processes in complex regional pain syndromes. Immunol Investig. (2013) 42:263–72. doi: 10.3109/08820139.2013.764317
87. Li W-w, Sabsovich I, Guo T-Z, Zhao R, Kingery WS, Clark JD. The role of enhanced cutaneous IL-1β signaling in a rat tibia fracture model of complex regional pain syndrome. PAIN®. (2009) 144:303–13. doi: 10.1016/j.pain.2009.04.033
88. Zhang J, Middleton KK, Fu FH, Im H-J, Wang JH. HGF mediates the anti-inflammatory effects of PRP on injured tendons. PLoS ONE. (2013) 8:e67303. doi: 10.1371/journal.pone.0067303
89. McCarrel TM, Minas T, Fortier LA. Optimization of leukocyte concentration in platelet-rich plasma for the treatment of tendinopathy. JBJS. (2012) 94:e143. doi: 10.2106/JBJS.L.00019
90. Davis VL, Abukabda AB, Radio NM, Witt-Enderby PA, Clafshenkel WP, Cairone JV, et al. Platelet-rich preparations to improve healing. part ii: platelet activation and enrichment, leukocyte inclusion, and other selection criteria. J Oral Implantol. (2014) 40:511–21. doi: 10.1563/AAID-JOI-D-12-00106
91. Pape H-C, Marcucio R, Humphrey C, Colnot C, Knobe M, Harvey EJ. Trauma-induced inflammation and fracture healing. J Orthop Trauma. (2010) 24:522–5. doi: 10.1097/BOT.0b013e3181ed1361
92. Zimmermann R, Arnold D, Strasser E, Ringwald J, Schlegel A, Wiltfang J, et al. Sample preparation technique and white cell content influence the detectable levels of growth factors in platelet concentrates. Vox Sanguinis. (2003) 85:283–9. doi: 10.1111/j.0042-9007.2003.00361.x
93. Barrientos S, Stojadinovic O, Golinko MS, Brem H, Tomic-Canic M. PERSPECTIVE ARTICLE: growth factors and cytokines in wound healing. Wound Repair Regen. (2008) 16:585–601. doi: 10.1111/j.1524-475X.2008.00410.x
94. Barrick A, Campbell EJ, Owen CA. Leukocyte proteinases in wound healing: roles in physiologic and pathologic processes. Wound Repair Regen. (1999) 7:410–22. doi: 10.1046/j.1524-475X.1999.00410.x
95. Dohan Ehrenfest DM, Rasmusson L, Albrektsson T. Classification of platelet concentrates: from pure platelet-rich plasma (P-PRP) to leucocyte- and platelet-rich fibrin (L-PRF). Trends Biotechnol. (2009) 27:158–67. doi: 10.1016/j.tibtech.2008.11.009
Keywords: platelet-rich plasma, platelet, fracture, osteoblasts, growth factors, systematic review
Citation: Zhang Y, Xing F, Luo R and Duan X (2021) Platelet-Rich Plasma for Bone Fracture Treatment: A Systematic Review of Current Evidence in Preclinical and Clinical Studies. Front. Med. 8:676033. doi: 10.3389/fmed.2021.676033
Received: 04 March 2021; Accepted: 06 July 2021;
Published: 03 August 2021.
Edited by:
Darius Widera, University of Reading, United KingdomReviewed by:
Gilberto Sammartino, University of Naples Federico II, ItalySiegmund Lang, University Medical Center Regensburg, Germany
Copyright © 2021 Zhang, Xing, Luo and Duan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xin Duan, ZHhiYWFsQGhvdG1haWwuY29t
†These authors have contributed equally to this work
 Yangming Zhang
Yangming Zhang Fei Xing
Fei Xing Rong Luo
Rong Luo Xin Duan
Xin Duan