- 1Department of Internal Medicine, Western National Medical Center (IMSS), Guadalajara, Mexico
- 2Department of Public Health, University of Guadalajara, Guadalajara, Mexico
- 3Department of Urology, Western National Medical Center (IMSS), Guadalajara, Mexico
- 4Department of Radiology, Western National Medical Center (IMSS), Guadalajara, Mexico
- 5Department of Anesthesiology, Western National Medical Center (IMSS), Guadalajara, Mexico
- 6Department of Endocrinology, Western National Medical Center (IMSS), Guadalajara, Mexico
- 7Department of Infectious Diseases, Western National Medical Center (IMSS), Guadalajara, Mexico
- 8Department of Immunology, Western National Biomedical Center (IMSS), Guadalajara, Mexico
Background: Spontaneous pneumomediastinum (SPM) is an uncommon condition in COVID-19 patients. No information about outcome or risk factors is available at the time. The aim of this research is to report on the frequency and risk factors of spontaneous pneumomediastinum in COVID-19 patients.
Materials and Methods: An unmatched case-control study was carried out in a tertiary health-care facility for patients with COVID-19. Electronic files were reviewed to identify patients with confirmed COVID-19 infection by RT-PCR. Univariate analysis was used to describe demographic data. Mean differences were calculated using the Mann-Whitney test. Frequency and odds ratios were calculated by standard operations.
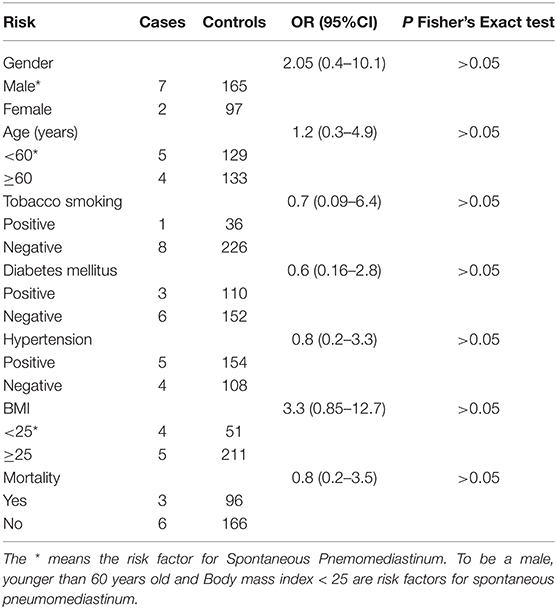
Results: A total of 271 patients were included in the study. Nine patients showed spontaneous pneumomediastinum and four of them presented associated spontaneous pneumothorax. The most common risk factors associated with poor outcomes in COVID-19 patients were not considered as risk factors for spontaneous pneumomediastinum development.
Conclusion: Spontaneous pneumomediastinum is an uncommon clinical feature in COVID-19 patients. More research is necessary to formulate statements regarding prevalence, risk factors, and outcome.
Introduction
Based on a report from the World Health Organization (WHO) from March 10, 2021, the number of confirmed COVID-19 cases worldwide were 117,332,262 and 2,605,356 deaths (1). Mexico is one of the counties with the highest number of cases. In the beginning of March, the number of confirmed cases was 2,130,477 with a total of 190,923 deaths (1). To date, the problem is of major concern for public health around the world.
Although a definitive diagnosis of COVID-19 infection is made by using a reverse transcription polymerase chain reaction (RT-PCR) assay (2), several authors reported on the role and utility of chest CT scan as a recommended tool for clinical practice for COVID-19 patients (3–5). In April 2020, the Dutch Radiological Society developed CO-RADS to assess the suspicion of pulmonary involvement of COVID-19. The scale is from 1 to 5, from very low to very high involvement (6). Nowadays, the CO-RADS scale is used widely in our medical facility as a complementary tool to measure the extent of compromised pulmonary parenchyma in COVID-19 patients.
Radiological features such as spontaneous pneumothorax have been described in 1% of COVID-19 patients (7, 8). Spontaneous pneumomediastinum (SPM), unrelated to assisted ventilation, is another radiological feature reported in literature as a frequent complication and is related to a poor outcome (9). In general terms, SPM has a reported frequency in non-COVID-19 patients of 1 in 25,000 and is more common in children (10). To date, there is no reliable data on the frequency of SPM in COVID-19 patients, however, some clinical cases are available in international literature (11–15).
Based on the previous information, the aim of this work is to report on the frequency of spontaneous pneumomediastinum and the related risk factors in a tertiary health-care facility that was converted for the caring of COVID-19 patients.
Materials and Methods
An unmatched case-control study was carried out at the Western National Medical Center in a 2-month period (July and August 2020). This research was performed under permission from the ethics committee, Number 14 CEI 20190123/ COFEPRIS 17 CI 14 039 114. Electronic files from COVID-19 patients were reviewed (chest CT scans and laboratory results) that looked for clinical features related to spontaneous pneumomediastinum. Suspicious cases were reviewed by six physicians (including 2 radiologists) in order to validate the diagnosis. Selected files were reviewed in order to obtain anthropometric data, clinical features, inflammatory biomarkers, comorbidities, and outcomes. Inclusion criteria for cases and controls were complete electronic files (medical notes, laboratory results, and digital chest CT scan images) from both genders older than 18 years and COVID-19 diagnosis by RT-PCR. Selected patients were managed at the Western National Medical Center COVID-19 units by at least one of the authors of this report. A data analysis report used percentages, absolute frequencies, means, standard deviations, and a 95% confidence interval. Statistical significance was evaluated by means of the Mann-Whitney U-test (p < 0.05). The frequency and Odds Ratio (OR) were calculated using standard methods. All data were processed using Excel® (Microsoft, Redmond, WA, USA) Open Epi (Open-Source Epidemiologic Statistics for Public Health, Bill and Melinda Gates Foundation, Emory University, Atlanta, GA, USA) and EpiInfo version 7.2.4 (Centers for Disease Control and Prevention, Atlanta, GA, USA).
Results
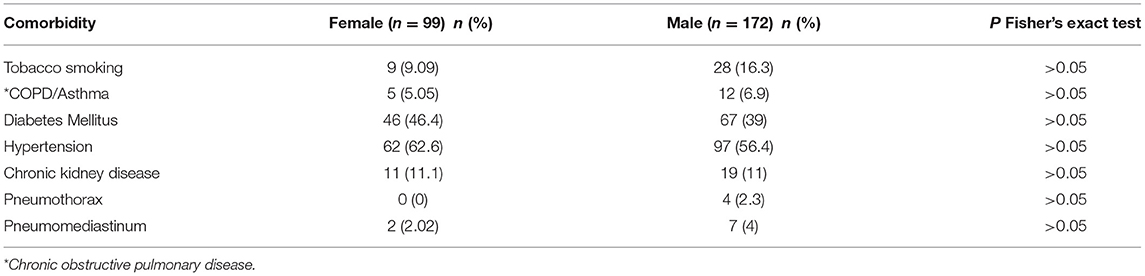
A total of 319 electronic files from COVID-19 patients confirmed by RT-PCR assay SARS-CoV-2 were reviewed. Those files without chest CT scans or complete laboratory reports were excluded (n = 48). The files included in the study were 271, including cases and controls. From the patient cohorts, 36.5% were women and 63.5% were males. Demographic data is shown in Table 1.
The percentage of deceased patients from the entire cohort was 36.5 (n = 99/271), corresponding to 23.9% for males and 12.6% for females. Comorbidities from the total sample were obtained from files. Details related to such are shown in Table 2.
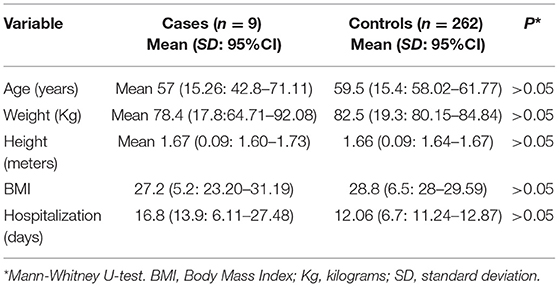
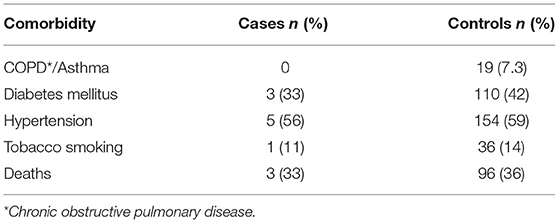
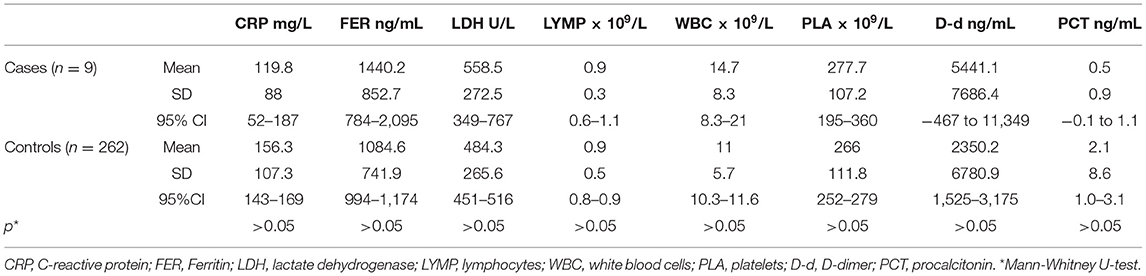
Based on the results, a total of 9 COVID-19 hospitalized patients developed spontaneous pneumomediastinum (3.3%), and 4 cases of spontaneous pneumothorax were detected (1.47%). All patients underwent a non-enhanced chest CT scan immediately after hospital admission, upon which SPM was identified by a COVID-19 physician team (Figures 1, 2). None of them received invasive mechanical ventilation at the time they were admitted. The principal characteristics of patients who developed SPM are described in Table 3. No significant differences were observed with regard to inflammatory biomarkers (p > 0.05). The main differences between non-spontaneous pneumomediastinum and SPM are shown in Tables 4, 5
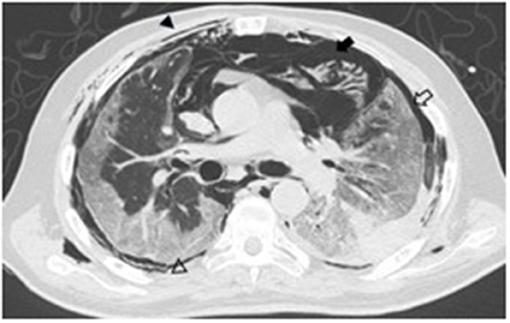
Figure 1. A 68-year-old male axial non-enhanced chest CT image showing subcutaneous emphysema (arrow heads), pneumomediastinum (black arrow), and pneumothorax (empty arrow).
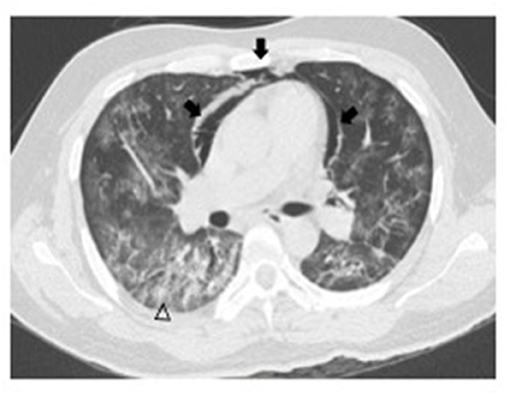
Figure 2. A 43-year-old male non-enhanced chest CT image showing pneumomediastinum (arrows) and ground glass opacity pattern over peripheral subpleural areas (arrowhead).
In order to calculate the Odds Ratio (OR), some independent variables (age and BMI) were adapted using a dichotomic approach that was used in the contingency tables. Age was considered as a risk factor if younger than 60-years old, and BMI was dichotomized in <25 and 25 or higher. Regarding gender, being male was considered as a risk factor. The ORs were calculated individually for each risk factor. Results obtained from the ORs are described in Table 6.
Discussion
The results obtained in the present study clearly show that SPM is not always a pathologic feature related to invasive mechanical ventilation in COVID-19 patients. Indeed, main risk factors for SPM such as young age, tobacco smoking, asthma, and gender (10) did not show a significant statistical association. Other risk factors which are associated with poor outcomes in COVID-19 patients like hypertension and obesity were not statistically related to SPM either (p > 0.05). International research reported a frequency of 1 in 25,000 (10), however, our results showed an increased frequency of SPM in COVID-19 patients (9 in 271). The difference between proportions is remarkable (p < 0.01).
Spontaneous pneumomediastinum in COVID-19 patients has been reported as single cases in international literature (11–14). Other authors had reported some case series of SPM. Eperjesiova et al. reported 20 cases of air leak in a cohort of 976 COVID-19 patients. Five cases were SPM and were unrelated to mechanical ventilation. Two patients developed spontaneous pneumothorax, and the rest (n = 13) were air leak cases that were associated with medical procedures (15). However, the manuscript does not describe the relationship between SPM and risk factors.
During the peak of the SARS-CoV-2 pandemics in Spain, Gorospe et al. reported four cases of SPM that were unrelated to mechanical ventilation. None of the patients had a previous history of tobacco consumption or predisposing risk factors. One patient died after an infection of Pseudomonas aeruginosa (8). No statistical analysis of risk factors was performed for the study.
Recently, Jones et al. reported an observational study in England that included 83 critically ill COVID-19 patients. The authors divided the group into barotrauma and non-barotrauma groups. The barotrauma group included a total of 8 patients. One hundred percent of them had subcutaneous emphysema, seven revealed pneumomediastinum, and four had pneumothorax (bilateral n = 2). The seven patients that developed pneumomediastinum received ventilatory support through CPAP or non-invasive mechanical ventilation (NIV). The study reported significant mean differences between some variables, and a 9.6% of barotrauma as a complication in the cohort of patients. They assumed that barotrauma in COVID-19 patients is related to longer management prior to critical care admission and the use of CPAP or NIV. However, the manuscript does not specify if the chest CT scans were performed before or after CPAP management, NIV, and invasive mechanical ventilation (16).
The inflammatory process induced by the SARS-CoV-2 infection in the respiratory tract is characterized by an increase in intrathoracic pressure. Differential pressure inside the pulmonary parenchyma is the main cause of alveolar rupture that causes air leak through interstitial and bronchovascular tissues including the pneumomediastinum (17). The abnormal increase in pressure in the mediastinum causes air to dissect in between the mediastinal structures. The effect of dissection, which is secondary to air leak, extends from the soft tissue structure in the anterior mediastinum up to the subcutaneous tissue over the upper abdomen and neck (10). Symptoms are characterized by retrosternal chest pain, neck pain and swelling, dyspnea, dysphagia, and facial swelling (18).
In general terms, our results reveal that SPM is an uncommon condition resulting from an inflammation of the respiratory tract in COVID-19 patients. No specific data on the incidence of SPM is available at the moment, however, based on the local number of cases, the frequency was calculated in 3.3% of hospitalized COVID-19 patients. It is important to mention that the development of SPM does not increase the risk of death, nor the length of hospital stay.
From the total number of cases of SPM (n = 9), two of them showed a bilateral pneumothorax. One of these patients required invasive mechanical ventilation and died 3 days later. The other patient recovered successfully. Another two patients with SPM required invasive mechanical ventilation after diagnosis and died 3 and 5 days later, respectively. The other 6 patients recovered without mechanical invasive ventilation and were discharged around 16 days after admission.
Conclusion
Development of SPM in COVID-19 patients is becoming an interesting topic nowadays. Information and data from international literature is still not enough to draw conclusions about specific causes, pathology, and outcome. More research and epidemiological data are necessary to make statements regarding this uncommon condition in patients affected by the novel SARS-CoV-2 virus.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by this research was performed under permission from the ethics committee, Number 14 CEI 20190123/ COFEPRIS 17 CI 14 039 114. Instituto Mexicano del Seguro Social (IMSS). Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author Contributions
All authors: participated directly in the care of COVID-19 patients. TR-A and ES-D: conceptualization, methodology, and writing-original draft preparation. ES-D: data analysis. TR-A, ES-D, JF-M, MA-P, IL-L, AC-N, and HC-G: investigation, formal analysis, validation, and sampling. TR-A, ES-D, JF-M, MA-P, IL-L, and HC-G: chest CT scan analysis. AC-N, TR-A, HC-G, and AB-C: writing-review and editing. AC-N, AB-C, and ES-D: project administration. All authors: have read and agreed to the published version of the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors greatly appreciate the efforts made by the healthcare personnel that worked tirelessly in saving several lives. Special thanks to our patients and their families. It was a pleasure to attend to them.
References
1. WHO Coronavirus Disease (COVID-19) Dashboard. World Health Organization. Available online at: https://covid19.who.int (accessed March 10, 2021).
2. Li Y, Yao L, Li J, Chen L, Song Y, Cai Z, et al. Stability issues of RT-PCR testing of SARS-CoV-2 for hospitalized patients clinically diagnosed with COVID-19. J Med Virol. (2020) 92:903–8. doi: 10.1002/jmv.25786
3. Li Y, Xia L. Coronavirus disease 2019 (COVID-19): role of chest CT in diagnosis and management. AJR Am J Roentgenol. (2020) 214:1280–6. doi: 10.2214/AJR.20.22954
4. Tenda ED, Yulianti M, Asaf MM, Yunus RE, Septiyanti W, Wulani V, et al. The importance of chest CT scan in COVID-19. Acta Med Indones. (2020) 52:68–73.
5. Bernheim A, Mei X, Huang M, Yang Y, Fayad ZA, Zhang N, et al. Chest CT findings in coronavirus disease-19 (COVID-19): relationship to duration of infection. Radiology. (2020) 295:200463. doi: 10.1148/radiol.2020200463
6. Prokop M, van Everdingen W, van Rees Vellinga T, Quarles van Ufford H, Stöger L, Beenen L, et al. CO-RADS: a categorical CT assessment scheme for patients suspected of having COVID-19-definition and evaluation. Radiology. (2020) 296:E97–104. doi: 10.1148/radiol.2020201473
7. Yang Q, Liu Q, Xu H, Lu H, Liu S, Li H. Imaging of coronavirus disease 2019: a Chinese expert consensus statement. Eur J Radiol. (2020) 127:109008. doi: 10.1016/j.ejrad.2020.109008
8. Gorospe L, Ayala-Carbonero A, Ureña-Vacas A, Fra Fernández S, Muñoz-Molina GM, Arrieta P, et al. Spontaneous pneumomediastinum in patients with COVID-19: a case series of four patients. Arch Bronconeumol. (2020) 56:754–6. doi: 10.1016/j.arbres.2020.06.008
9. Chu CM, Leung YY, Hui JY, Hung IF, Chan VL, Leung WS, et al. Spontaneous pneumomediastinum in patients with severe acute respiratory syndrome. Eur Respir J. (2004) 23:802–4. doi: 10.1183/09031936.04.00096404
10. Kouritas VK, Papagiannopoulos K, Lazaridis G, Baka S, Mpoukovinas I, Karavasilis V, et al. Pneumomediastinum. J Thorac Dis. (2015) 7(Suppl. 1):S44–9. doi: 10.3978/j.issn.2072-1439.2015.01.11
11. Quincho-Lopez A, Quincho-Lopez DL, Hurtado-Medina FD. Case report: pneumothorax and pneumomediastinum as uncommon complications of COVID-19 pneumonia-literature review. Am J Trop Med Hyg. (2020) 103:1170–6. doi: 10.4269/ajtmh.20-0815
12. Kolani S, Houari N, Haloua M, Alaoui Lamrani Y, Boubbou M, Serraj M, et al. Spontaneous pneumomediastinum occurring in the SARS-COV-2 infection. IDCases. (2020) 21:e00806. doi: 10.1016/j.idcr.2020.e00806
13. Janssen J, Kamps MJA, Joosten TMB, Barten DG. Spontaneous pneumomediastinum in a male adult with COVID-19 pneumonia. Am J Emerg Med. (2020) 40: 228.e3–e5. doi: 10.1016/j.ajem.2020.07.066
14. Sun R, Liu H, Wang X. Mediastinal emphysema, giant bulla, and pneumothorax developed during the course of COVID-19 pneumonia. Korean J Radiol. (2020) 21:541–4. doi: 10.3348/kjr.2020.0180
15. Eperjesiova B, Hart E, Shokr M, Sinha P, Ferguson GT, Eperjesiova B, Hart E, Shokr M, Sinha P, Ferguson GT. Spontaneous pneumomediastinum/pneumothorax in patients with COVID-19. Cureus. (2020) 12:e8996. doi: 10.7759/cureus.8996
16. Jones E, Gould A, Pillay TD, Khorasanee R, Sykes R, Bazo-Alvarez JC, et al. Subcutaneous emphysema, pneumomediastinum, and pneumothorax in critically ill patients with coronavirus disease 2019: a retrospective cohort study. Crit Care Explorations. (2020) 2:e0210. doi: 10.1097/CCE.0000000000000210
17. Varela-Patiño M, Torres-Blanco B. Pneumomediastinum and subcutaneous emphysema in relation with SARS-CoV-2 pandemic. Med Gem Fam. (2020) 9:162–4. doi: 10.24038/mgyf.2020.026
Keywords: spontaneous pneumomediastinum, spontaneous pneumothorax, SARS-CoV-2, complications, risk factors, case-control study
Citation: Rodriguez-Arciniega TG, Sierra-Diaz E, Flores-Martinez JA, Alvizo-Perez ME, Lopez-Leal IN, Corona-Nakamura AL, Castellanos-Garcia HE and Bravo-Cuellar A (2021) Frequency and Risk Factors for Spontaneous Pneumomediastinum in COVID-19 Patients. Front. Med. 8:662358. doi: 10.3389/fmed.2021.662358
Received: 01 February 2021; Accepted: 12 March 2021;
Published: 09 April 2021.
Edited by:
Atefeh Abedini, Shahid Beheshti University of Medical Sciences, IranReviewed by:
Mohammad Varahram, National Research Institute of Tuberculosis and Lung Diseases (NRITLD), IranYoshihiko Raita, Massachusetts General Hospital and Harvard Medical School, United States
Copyright © 2021 Rodriguez-Arciniega, Sierra-Diaz, Flores-Martinez, Alvizo-Perez, Lopez-Leal, Corona-Nakamura, Castellanos-Garcia and Bravo-Cuellar. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Erick Sierra-Diaz, erksland@hotmail.com
 Tania Guadalupe Rodriguez-Arciniega1
Tania Guadalupe Rodriguez-Arciniega1 Erick Sierra-Diaz
Erick Sierra-Diaz Alejandro Bravo-Cuellar
Alejandro Bravo-Cuellar