- 1Department of Orthopedics, Taichung Veterans General Hospital, Taichung, Taiwan
- 2Department of Senior Services Industry Management, Minghsin University of Science and Technology, Hsinchu, Taiwan
- 3Department of Recreation and Sport Management, Shu-Te University, Kaohsiung, Taiwan
- 4Department of Orthopedics, Cishan Hospital, Ministry of Health and Welfare, Kaohsiung, Taiwan
- 5Department of Physical Medicine and Rehabilitation, Chung Shan Medical University Hospital, Taichung, Taiwan
- 6School of Medicine, Chung Shan Medical University, Taichung, Taiwan
- 7Department of Food Science and Technology, Hung Kuang University, Taichung, Taiwan
- 8Management Office for Health Data, China Medical University Hospital, Taichung, Taiwan
- 9Department of Allergy, Immunology and Rheumatology, Chung Shan Medical University Hospital, Taichung, Taiwan
- 10Institute of Medicine, College of Medicine, Chung Shan Medical University, Taichung, Taiwan
- 11Graduate Institute of Integrated Medicine, China Medical University, Taichung, Taiwan
Objective: To determine the trend of incidence rate of total knee arthroplasty (TKA), total hip arthroplasty (THA), and TKA or THA (major joint arthroplasty, MJA) among rheumatoid arthritis (RA) population and compared them with general population (GP) in Taiwan.
Methods: Incidence rates and trends of TKA, THA, and MJA were determined over a 14-year period (2000–2013) among RA patients and compared them with GP. RA of patients was diagnosed based on the ACR 1987 criteria and extracted from GP. Subanalyses of incidences of TKA, THA, and MJA by year, 10-year age group, and gender were further conducted for demographic analysis. Patient profiles were extracted from the National Health Insurance Research Database (NHIRD) for interrupted time-series analysis and cohort studies.
Results: Patients enrolled were 168,457 receiving TKA, 64,543 receiving THA, and 228,191 receiving MJA surgery. Incidences of TKA, THA, and MJA in RA patients were significantly lower by 49.0, 41.5, and 41.0% compared with concomitantly rises in GP by 131.0, 25.1, and 90.0% among the GP during the study period. The dominant age population for TKA, THA, and MJA were those aged 70–79 years in both GP and RA groups.
Conclusions: We found an opposing trend in incidence of TKA, THA, and MJA between RA patients and the GP. The possible influence of pharmacological treatment is implicated for the lower incidence rates of TKA, THA, and MJA surgeries among RA patients.
Introduction
Rheumatoid arthritis (RA) is one of the most prevalent chronic inflammatory diseases causing structural changes such as major joint deformity and soft tissue damage (1). RA affects 0.1–0.3% of Asians, and it has an incidence rate of 15.8 per 100,000 people in Taiwan (2, 3). Medications for RA are to improve function and prevent persistent major joint destructions. Conventional synthetic disease-modifying antirheumatic drugs (csDMARDs) and biological DMARDs (bDMARDs), applied as monotherapy or in combination with other anti-inflammatory drugs, had showed promising efficacy in preventing RA from progressing to late stages and improving functional outcome during since late 1980s (4). In Taiwan, lower healthcare utilization cost was offset with the increase medication cost in biologics such as csDMARDs and bDMARDs since 1990s (5).
Despite the effectiveness of pharmacological treatment, orthopedic procedures remain indispensable in managing severe RA. Among these procedures, total joint arthroplasty is the only available solution for non-reversible joint destruction of these patients. RA patients in Taiwan suffer 4.02 times greater risk, compared with non-RA patients, of undergoing major joint arthroplasty (MJA) surgeries, including total knee arthroplasty (TKA) and total hip arthroplasty (THA) (6). In the last three decades, 30–50% of RA patients have undergone orthopedic procedures. Specifically, up to 24% of patients with RA underwent MJA with substantial improvements of overall function and quality of life (7, 8).
In recent years, the fewer MJA in reducing joint erosion and chronic inflammatory progress is thought to be related to increased intensity and the introduction of more effective anti-rheumatic medications, like conventional and biological DMARDs (9–12). Pharmacological treatments are recommended as first line therapy for RA patients since MJA has greater complication risks and is a more expensive procedure (13). Whereas, among the general population (GP), the growing demand for MJA has made it the most common elective surgery (14). But few studies have compared incidences of MJA between RA patients and GP among Asian populations, including those in China and Taiwan.
Therefore, we aimed to determine population-based incidence rates of TKA, THA and MJA among a well-defined RA population and in GP of Taiwan, using the National Health Insurance Research Database (NHIRD) collected between 2000 and 2013.
Materials and Methods
Data Source
The Taiwan National Health Insurance Research Database (NHIRD) was first established in 1995. The health information it contained included outpatients, hospitalization, prescription, surgery and other medical services derived from the single payer health insurance program for the general population. In this study, we have chosen the Taiwan population-based hospitalization files to conduct our analyses. The identification numbers in the database were already encrypted before release to protect patients' privacy. Diagnosis of diseases was based on International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM). The Research Ethics Committee of China Medical University and Hospital in Taiwan approved our study [CMUH-104-REC2-115-(AR4)]. We disclaimed that there is no potentially identifiable images or data, animal, or human study involved in current study.
Study Population
We aimed to evaluate the annual incidence and the consecutive trend of TKA (ICD-9-OP: 81.54), THA (ICD-9-OP: 81.51) and MJA (defined as patient receiving TKA or THA) among GP and patients with RA (ICD-9-CM: 714.0) in Taiwan from 2000 to 2013. RA cohort was defined as: (1) Patients with newly diagnosed RA and with catastrophic illness card from 2000 to 2012 were identified as RA patients; (2) The date of the catastrophic illness card of RA applied was set up as the index date; (3) Patients were followed from the index date to TKA, THA, MJA (TKA or THA) diagnosis, death, withdrawn from NHIRD, or the end of the year 2013 which came first. Two study populations were enrolled: GP and RA cohorts. The GP cohort consisted of almost every hospitalized patient who had received surgery of TKA (ICD-9-OP: 81.54), THA (ICD-9-OP: 81.51), or MJA in the NHIRD database regardless of underlying diagnosis. Patients in the RA cohort were a subset of the GP cohort that underwent TKA, THA, or MJA surgery under the diagnosis of RA. The diagnosis of RA, defined by catastrophic illness card during the study period, was certified by rheumatologists according to the criteria of American College of Rheumatology in 1987 (ACR 1987) (15). Patients underwent TKA, THA, or MJA before the diagnosis of RA, having incomplete information like age or gender, or recorded on December 31, 2013 were excluded from the RA cohort.
Statistical Analyses
Demographic parameters and baseline comorbidities were included in our analysis. Age group, gender, occupation type, and the presence of baseline comorbidities were defined as categorical variable. The annual incidences of TKA, THA, and MJA by year, 10-year age group, and gender were calculated by the number of surgical events divided by total population person years (per 100,000 person years in GP and per 1,000 person years in patients with RA). The 95% confidence intervals for incidence were calculated by Fisher's exact test. Compared with the year 2000, differences in incidence rate (from 2001 to 2013) of all surgical types were evaluated by the Poisson regression model. We further verified the association between comorbidities and TKA, THA, and MJA by Cox model. Analyses were performed with the SAS 9.4 software (SAS Institute, Cary, NC, USA). Two-sided p-values < 0.05 were considered statistically significant.
Results
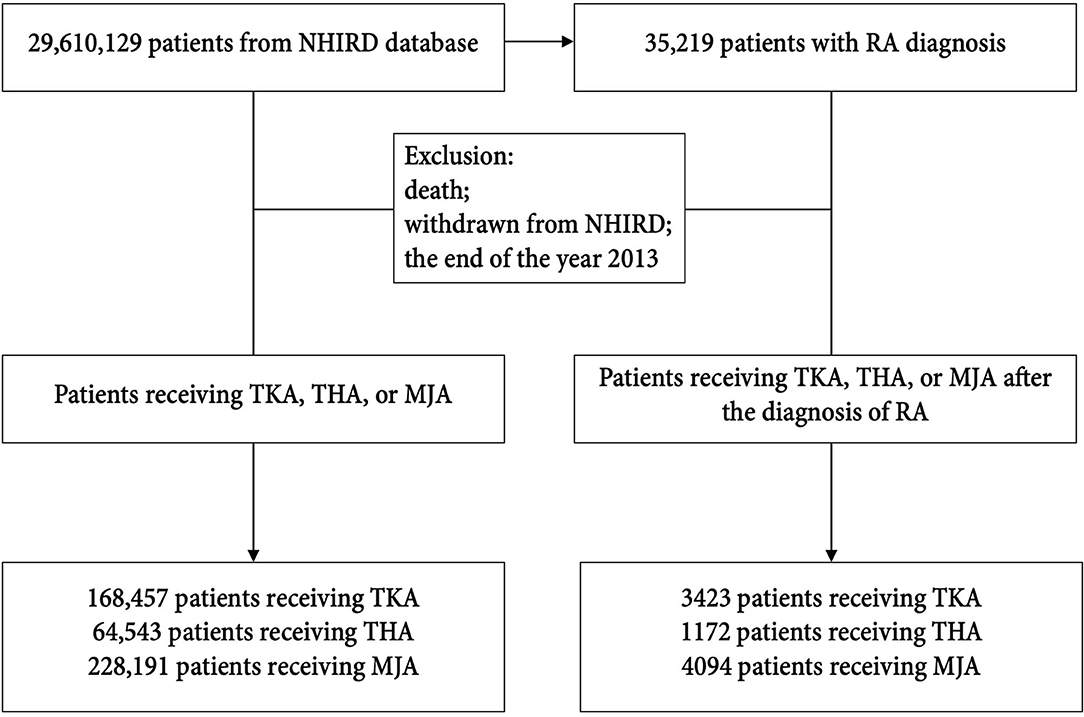
The NHIRD data base comprised of 29,610,129 registered patients (GP cohort), including 35,219 RA patients. After applying the study eligibility criteria, we enrolled 168,457 patients receiving TKA surgery, 64,543 patients receiving THA surgery, and 228,191 patients receiving MJA surgery during the study period (from 2000 to 2013) in the GP cohort. Among those patients, 3,423 (2.03%), 1,172 (1.81%), and 4,094 (1.79%) patients received respectively TKA, THA, and MJA under the diagnosis of RA (Figure 1).
General Population
Among the GP, comparing within years from 2000 to 2013, we found significant increments in their number of surgery and incidence rate (p for trend < 0.001): for TKA (N = 7,068–17,432 with incidence rate from 31.70 to 73.30 per 100,000 person years), THA (N = 4,160–5,583 with incidence rate from 16.64 to 23.39 per 100,000 person years), and MJA (N = 11,075–22,438 with incidence rate from 49.70 to 94.56 per 100,000 person years) (Figure 2). The ratio of incidence rate between 2013 and 2000 was 2.31 for TKA (95% CI 2.25–2.38), 1.25 for THA (95% CI 1.20–1.31), and 1.90 for MJA (95% CI 1.86–1.95). Patients aged between 70 and 79 years were the dominant population receiving TKA, THA, or MJA surgeries. Females generally received one to three times more TKA, THA and MJA surgeries than males over 60 years of age.
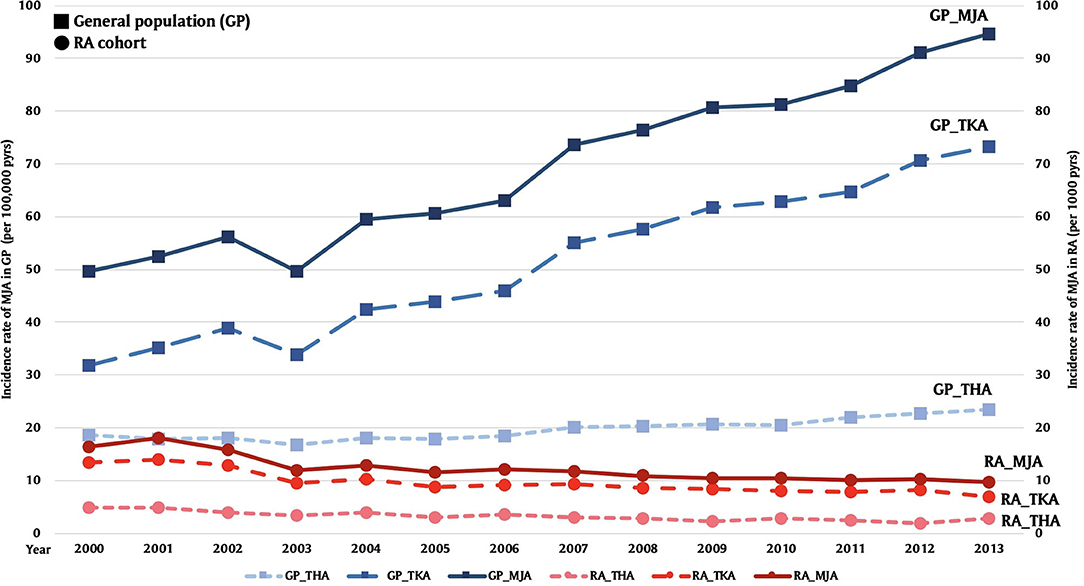
Figure 2. Comparison of incidence rates of total hip arthroplasty (THA), total knee arthroplasty (TKA), and major joint arthroplasty (MJA) between general hospitalization patients (GP) and rheumatoid arthritis (RA) patients from 2000 to 2013 [per 100,000 person years (pyrs) in GP and per 1,000 pyrs in RA patients].
Patients With RA
Of the 35,219 patients among RA cohort, 76.9% were women, and the mean age was 53.7 ± 13.8 of the RA cohort (Table 1). Most of the patients were office workers. Among RA patients, 1,421 (4.0%) had osteoarthrosis, 317 (0.9%) had Sjogren syndrome, 1,021 (2.9%) had gout, 211 (0.6%) had systemic lupus erythematous, 154 (0.4%) had ankylosing spondylitis. Patients of 70–79 years old were the dominant age group receiving TKA, THA, or MJA surgery. Regarding gender differences, females over age 60 years received more TKA, THA, and MJA than males. Females over 40 and 60 years-old also had higher incidences in receiving TKA and THA than males (Table 2). We further verified the association between comorbidities and TKA, THA, and MJA among RA cohort (Table 3). Sjogren syndrome (0.34, 95% CI 0.13–0.9) and osteoporosis (0.34, 95% CI 0.14–0.83) were less likely to receive TKA whilst coexisting with osteoarthrosis (2.59, 95% CI 2.23–3.01) increased the risk; ankylosing spondylitis (4.8, 95% CI 2.85–8.10) and osteoarthrosis (1.72, 95% CI 1.21–2.43) are associated with higher relative risk in receiving THA; osteoporosis (0.44, 95% CI 0.21–0.94) was less likely to receive MJA whilst osteoarthrosis (2.46, 95% CI 2.14–2.84) and ankylosing spondylitis (1.87, 95% CI 1.19–2.95) increased the risk. Obesity showed no impact to the relative risk for receiving surgeries. Comparing within years from 2000 to 2013, we found significant drop in numbers undergoing surgery numbers and incidence rate (p for trend < 0.001): for TKA (N = 176–270 with incidence rate from 13.42 to 6.85 per 1,000 person years), for THA (N = 65–113 with incidence rate from 4.79 to 2.80 per 1,000 person years), and for MJA (N = 210–347 with incidence rate from 16.36 to 9.65 per 1,000 person years) (Figure 2). Incidence rate ratios between year 2013 and 2000 were 0.51 for TKA (95% CI 0.42–0.62), 0.58 for THA (95% CI 0.43–0.79), and 0.59 for MJA (95% CI 0.5–0.7) (Table 4). Apparent decreasing incidence ratio of TKA, THA, and MJA of RA to GP cohort from 2000 to 2013 are demonstrated in Figure 3.

Table 1. Demographic characteristics and comorbidities of patients newly diagnosed rheumatoid arthritis (RA) in Taiwan from 2000 to 2013.
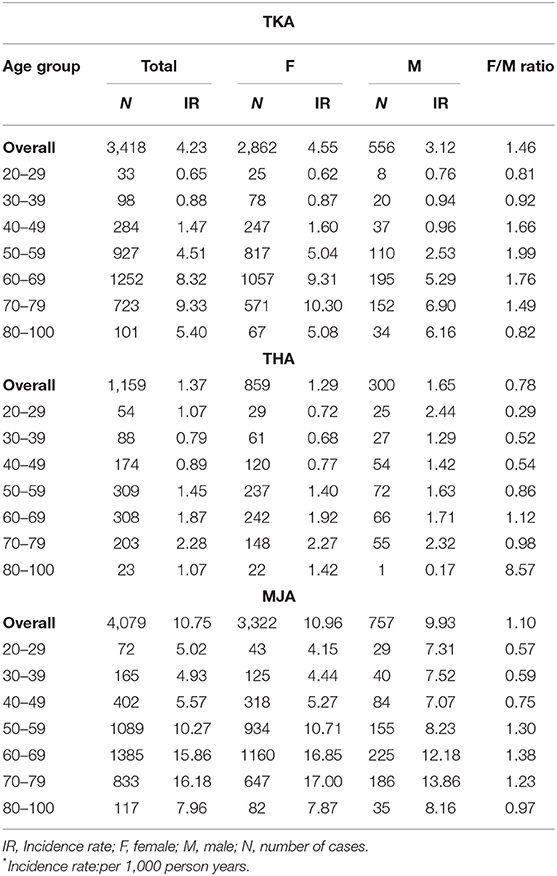
Table 2. Incidence rate and number of cases stratified by gender and age groups among rheumatoid arthritis (RA) patients from 2000 to 2013.
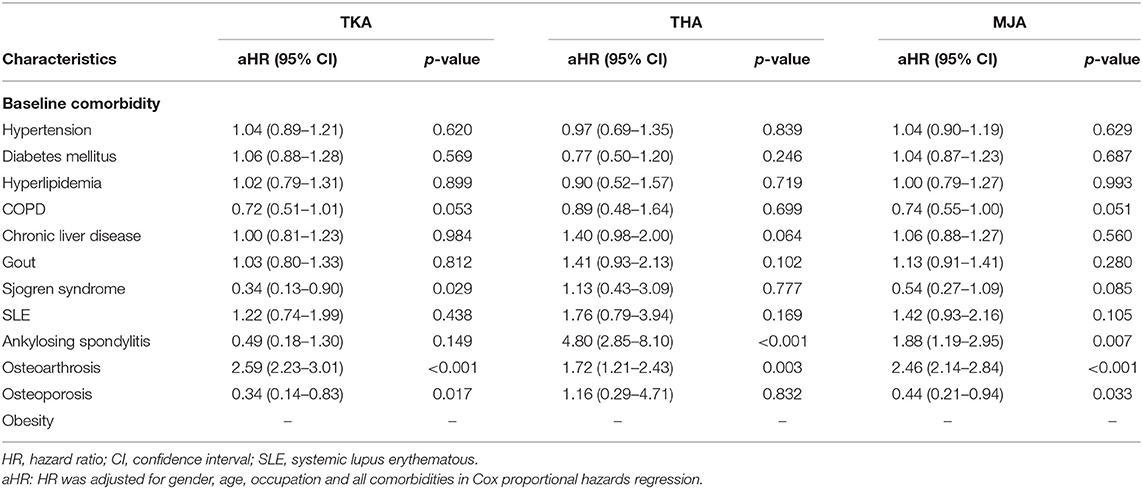
Table 3. Cox model measured hazard ratio and 95% confidence intervals of TKA, THA, or MJA associated with and without comorbidities among rheumatoid arthritis (RA) patients.
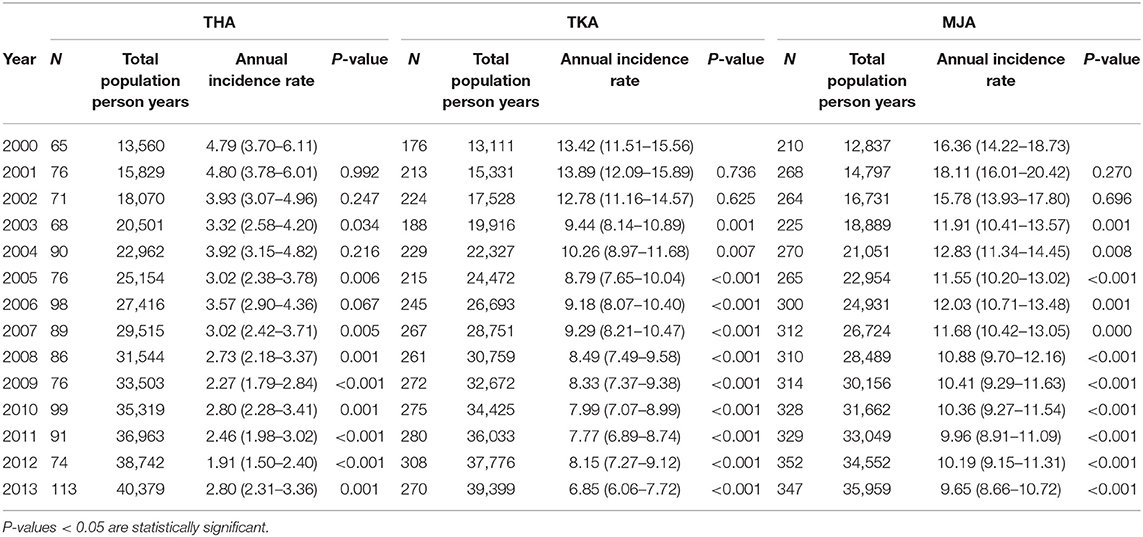
Table 4. Annual numbers and incidence rates [per 1,000 person years (pyrs)] compared to year 2,000 among patients with rheumatoid arthritis receiving total hip arthroplasty (THA), total knee arthroplasty (TKA), and major joint arthroplasty (MJA), respectively.
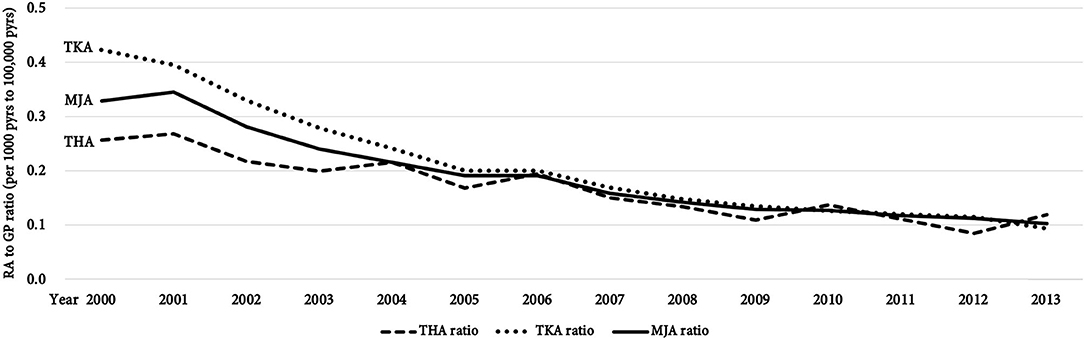
Figure 3. Incidence ratio of rheumatoid arthritis (RA) patients to general hospitalization patients (GP) from 2000 to 2013 [per 100,000 person years (pyrs) in GP and per 1,000 pyrs in RA patients], indicating the proportion of RA patients receiving total hip arthroplasty (THA), total knee arthroplasty (TKA), and major joint arthroplasty (MJA) among GP cohort.
Discussion
We found significantly lower incidence rates and numbers of TKA, THA, and MJA among the patients with RA, in contrast to a concomitantly rising trend in the general hospitalized population during the study period from 2000 to 2013. Opposing trend of incidence in total joint arthroplasty was also reported in several studies (11, 16, 17). However, comparison focusing on MJA among RA patients in Asian population has not been addressed. Our present study is the first population-based nationwide analysis based on the NHIRD records to reveal the opposing incidence trends over a period of 14 years in TKA, THA, and MJA between well-defined RA patients and general hospitalized population in Taiwan.
Our major results were the incidence of TKA, THA, and MJA among GP significantly increased by 131, 25.1, and 90% over 14 years, respectively (Figure 2). This rising trend is in line with previous epidemiology observations in Taiwan and worldwide (14, 18, 19). Noted that the decline of incidence in both TKA and THA in year 2003 we found could be attributed to the pandemic of severe acute respiratory syndrome (SARS) which prevented patients from undergoing TKA and THA (20). On the other hand, we found significant drops in the incidence rate of TKA, THA, and MJA among patients with RA by 49.0, 41.5, and 41.0%, respectively (Figure 2). According to the above findings, the proportion of RA patients receiving joint replacements among GP showed apparent decline trend by dividing incidence of GP by that of RA cohort (Figure 3). The falling trend is consistent with previous studies in both Europe (11, 12, 16, 17, 21–24) and the USA (9, 10, 25), whereas few reports have been published on Asian countries. These regional- and national-scale database studies provided enough power for the reliability of such findings. Comparison between reports related to incidence changes in joint arthroplasty surgery among RA patients is shown in Table 5. Since 1955, total joint arthroplasty surgeries (TJR), including total ankle, elbow, hip, shoulder, and knee showed a declining trend after the trajectory plateau of incidence (11, 12, 26). The difference in surgical incidences between our present study and the literature could be due to the heterogeneity of disease, alternative health insurance system, and intensity of treatment strategies. Females tended to receive more TKA and THA than males during the 4th−7th decades of their lives, a finding which is consistent with the age-specific incidence of RA as previously reported (27).
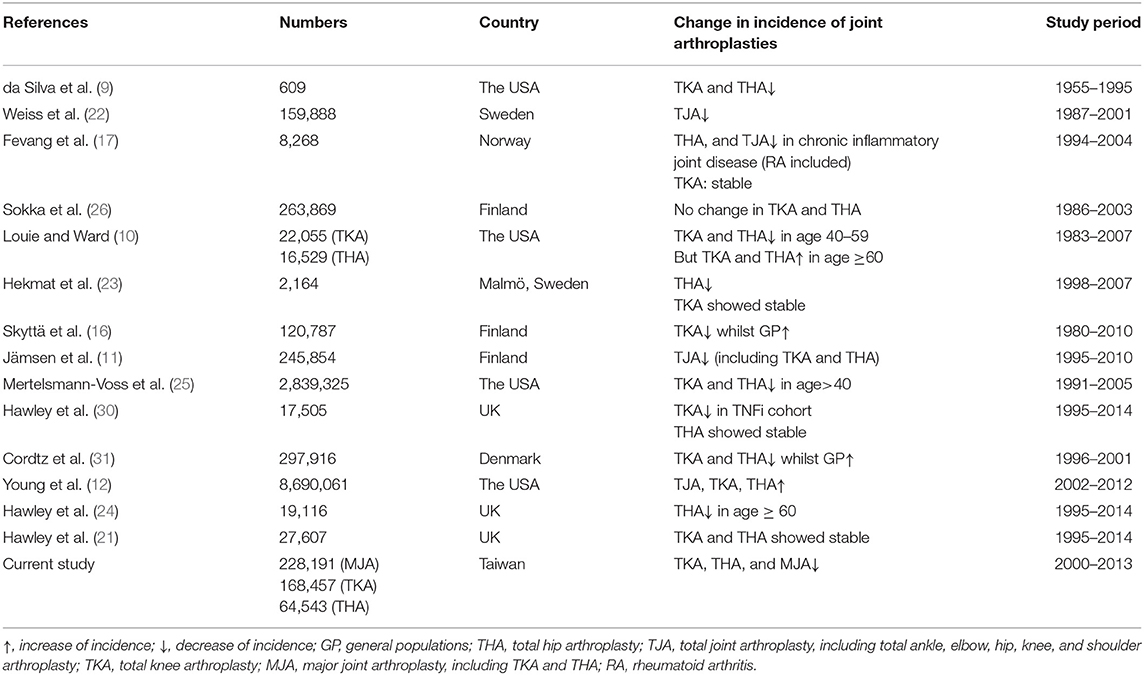
Table 5. Comparison of recent studies targeting incidences of joint arthroplasty surgeries among patients with rheumatoid arthritis.
RA in Taiwan has increased steadily in the last decade, with incidence rising from 14.2 to 15.2 per 100,000 people, and prevalence from 74.5 to 118.3 cases per 100,000 people (28). These patients have 4 times higher risk of undergoing TKA, THA, and MJA surgeries comparing with non-RA patients (6). Moreover, arthroplasty covered by Taiwan NHI program has also extended the indications and improved access for TKA and THA (18, 29). It is therefore reasonable to assume that demands for RA-related orthopedic procedures, including the need for MJA, might have increased with time along the escalated late-phase RA population. However, our current results showing a decline in demands of TKA, THA and MJA surgeries, are indirect support of the improving disease outcomes. Early observations from the Rochester Epidemiology Project showed that RA patients diagnosed after year 1985 were less likely to require total joint arthroplasty, matching the more frequent use of conventional DMARDs, especially methotrexate, hydroxychloroquine, and sulfasalazine (9, 11, 16). Introduction and aggressive prescriptions of biological DMARDs such as tumor necrosis factor inhibitor (TNFi) have lowered MJA rates since 2001 (23, 30, 31). In Taiwan, the more frequent use of DMARDs, especially after approving the prescription of adalimumab and etanercept in 2002, matched the concomitant drops in TKA, THA, and MJA surgeries in our RA patients (32–34).
Moreover, the fact that lower healthcare utilization cost was offset with the increase medication cost in biologics use may be alleviated by improvement in outcomes of RA in Taiwan since 1990s (5). Such constant occurrence is also linked with the improving long-term outcomes. Using the US Nationwide Inpatient Sample, significantly lower prevalence were found with total shoulder and elbow arthroplasty whereas prevalence of TKA and THA remained unchanged (12). In Finland, such constant occurrence of MJA was reported with RA patients, even before the emergence of biological DMARDs. At the same time an increase of MJA at 2–10-fold was found with the non-RA population (26). Similar occurrence of MJA was found in England from 1995 to 2004 (21). However, a relative 34% drop in incidence of TKA but not of THA was associated with the introduction of TNFi among a similar cohort (30). Supported by previous observations, the potential influence of modern pharmacological treatment strategies has been considered to be the plausible cause for the control of moderate to severe RA progression, and indirectly decreased or maintained the incidence of MJA surgery conducted worldwide. Moreover, patients seeking medical care toward milder cases, early detection of RA according to adjustment of criteria, and general improvement of RA disease may also contribute to such a decline (35, 36).
Meanwhile, the increasing trends of TKA, THA, and MJA in the GP could be explained by the rising number of symptomatic osteoarthrosis (OA) (96.9%) and avascular necrosis (46.9%), which were accountable for major contributors toward TKA and THA. RA was accountable for only 1–3% in TKA, and 0.5% in THA (29, 37). The rising elderly population and overweight individuals both increase demands for TKA with advanced OA. During the period from 2002 to 2010, the age group > 65 year-old accounted for 9–10.7% of the population, at an obesity rate of 17–18% (18, 29). Symptomatic OA is often caused by articular degeneration such as wearing and progressive loss of joint cartilage. Unlike OA, synovitis in RA often results from the destruction of joint cartilage, bone density loss, and periarticular osteopenia. Both destructive mechanisms end in irreversible joint deformity which requires arthroplasty. The current study shows patients with the combination of OA and RA have a 1.7–3.6 times higher risk to receive TKA, THA, and MJA. It has been reported that the risk of developing RA is higher in patients with symptomatic OA and OA-related surgery based on the similar expression of proinflammatory and anti-inflammatory cytokines. The synergistic effect of the disease may lead to higher demands of arthroplasties (38). However, these patients were included in the RA cohort according to our study design, and they underwent fewer TKA, THA, and MJA surgeries.
Patients with osteoporosis in RA have lower risks for receiving TKA and MJA in current study. Osteoporosis in RA, caused by rapid remodeling of bone, is associated with joint instability and disease activity. Unlike postmenopausal osteoporosis, radius and hip joint bone were mainly affected whilst axial bone were relatively preserved in RA-related osteoporosis (39). However, patients undergoing elective MJA were lack of identification and treatment for osteoporosis (40). Actual fracture risk, disease activity, and glucocorticoid dosage should be well-evaluated for clinical practicing. We also found significant higher risk in RA patients receiving THA and MJA whilst coexist with ankylosing spondylitis (AS), since the hip joint was the most commonly effected peripheral joint of the inflammatory process (41). However, the co-existence of AS and RA is relatively uncommon. A proportion of these patients may have had seronegative RA/AS predominant phenotype which accounts for the significant differences in hip joint replacement data. On the other hand, primary Sjogren's arthritis are rarely damaging, whilst second hit of RA may be the leading cause in receiving MJA (42). SLE/RA overlap is not uncommon (43). However, it may be difficult to use the data with higher potential of anti-inflammatory agent control in this group (44). BMI data (including heights or weights) were not included in the NHIRD, thus, we replaced BMI with the diagnosis of Obesity (ICD-9-CM: 278 and A183). However, it is noted that obesity showed no impact on the relative risk in receiving TKA, THA, and MJA. This result should be cautiously interpreted since the small patient number may cause a relatively low impact on the regression model. Therefore, while rising number and incidence rate among GP provided greater operating capacity for TKA, THA, and MJA, an opposite trend of decline among RA patients indirectly supported the pharmacological potential on improving clinical status of the disease.
Below we describe the limitations and merits of our present study. First, the methodological limitations complicated our deduction for the impact of medication on RA patients that resulted in a drop of TKA, THA, and MJA, due to our retrospective design. The indications, the usage of different anti-RA drugs, and different disease severity of patients have probably confounded the results. Moreover, alternative health care systems were difficult to compare with each other. Second, RA incidences could have been underestimated. Since those with milder RA may have not applied for the catastrophic disease registry in the NHIRD. Moreover, the lag period between onset of RA symptoms and the diagnosis of the disease may require cautious interpretation for the time-specific cumulative incidence. The incidences TKA, THA, and MJA may have been miscalculated due to RA may not have been the primary indication for the surgery. However, the inflammatory process of RA contributed greatly to joint destruction, leading to inevitable joint arthroplasty surgeries. It is difficult to discriminate influences between comorbidities such as OA from RA due to high rates of incidence and prevalence in the elderly. The introduction of ACR 2010 criteria (36) may have altered incidence rates of surgery due to earlier diagnoses of RA. Longer term follow-up is needed for the evaluation of such bias due to RA and comorbidities were chronic diseases.
Our present interrupted time-series analysis has several advantages. We matched the incidence of TKA, THA, and MJA to clarify the possible impact of the opposite trend between GP and patients with RA from a well-collected national-wide population-based database. To specifically address the impact of anti-RA drugs on RA patients, the design with random control trials is difficult. Thus, we chose to study on a high credibility retrospective cohort based on a large-scale database. The national burden of RA can now be better handled based on what we found on incidence trends of MJA and the possible effectiveness of pharmacological treatments. MJA surgeries are highly utilized procedures with heavy load on the NHI resources in Taiwan. The increasing trend of MJA among the GP noted in our current study suggested the significant impact on health insurance expenditure in the future. However, the concomitant decreasing trend in MJA among RA patients allowed authority to focus the budget planning on effectiveness early aggressive treatment strategies, not MJA, among patients with RA.
Conclusion
We have demonstrated a substantial increase in incidences of TKA, THA, and MJA among the general population with a concomitant drop in RA patients during a 14-year period from 2000 to 2013 in Taiwan. Opposite trends for surgical incidences were provided for comparison across Asian populations. The potential influence of pharmacological treatment is a plausible cause for the lowered incidence of MJA surgeries, and the improvement in disease condition among RA patients. With cautious interpretation of our current findings, cost-effectiveness assessment of strategies for RA treatment could be conducted for reducing the financial burden of our national health insurance program.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Ethics Statement
The Research Ethics Committee of China Medical University and Hospital, Taiwan approved our study [CMUH-104-REC2-115-(AR4)].
Author's Note
At the time of submission, this is the first report to discuss the opposing incidence trends of the total knee arthroplasty, total hip arthroplasty, and major joint arthroplasty between well-defined patients with rheumatoid arthritis (RA) and general hospitalized population in Taiwan and Asia.
This report is interesting for the reason that despite the effectiveness of pharmacological treatment, orthopedic procedures still possess a crucial role in management of severe RA. However, increased intensity of more effective anti-rheumatic medications has been proposed to be associated with decreased incidence of procedures, specifically joint arthroplasty surgeries.
Overall, we believe that current findings of opposing trend of joint arthroplasty surgeries provide greater insights into epidemiology observation in effectiveness in pharmacological treatment of RA among Asian populations.
Patient and Public Involvement
All data were extracted from Taiwan National Health Insurance Research Database. Patients and the public were not involved.
Author Contributions
K-KT, M-CL, and JW had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. K-KT, M-CL, and JW: study concept and design, acquisition of data. M-CL: statistical analysis. K-KT, Y-HL, C-HL, and C-CL: drafting of the manuscript. JW: study supervision. All authors: interpretation of data and critical revision of the manuscript for important intellectual content.
Funding
This study was supported in part by Taiwan Ministry of Health and Welfare Clinical Trial Center (MOHW109-TDU-B-212-114004), MOST Clinical Trial Consortium for Stroke [MOST Clinical Trial Consortium for Stroke (MOST 109-2321-B-039-002)], Tseng-Lien Lin Foundation, Taichung, Taiwan.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Scott DL, Wolfe F, Huizinga TW. Rheumatoid arthritis. Lancet. (2010) 376:1094–108. doi: 10.1016/S0140-6736(10)60826-4
2. Alamanos Y, Drosos AA. Epidemiology of adult rheumatoid arthritis. Autoimmun Rev. (2005) 4:130–6. doi: 10.1016/j.autrev.2004.09.002
3. Chen H-H, Huang N, Chen Y-M, Chen T-J, Chou P, Lee Y-L, et al. Association between a history of periodontitis and the risk of rheumatoid arthritis: a nationwide, population-based, case–control study. Ann Rheum Dis. (2013) 72:1206–11. doi: 10.1136/annrheumdis-2012-201593
4. Sokka T, Möttönen T, Hannonen P. Disease-modifying anti-rheumatic drug use according to the 'sawtooth' treatment strategy improves the functional outcome in rheumatoid arthritis: results of a long-term follow-up study with review of the literature. Rheumatology. (2000) 39:34–42. doi: 10.1093/rheumatology/39.1.34
5. Chen D-Y, Yu F, Tuan L-W, Tang C-H. Comparison of healthcare utilization and costs between RA patients receiving biological and conventional synthetic DMARDs: a nationwide population-based cohort study in Taiwan. Front Pharmacol. (2019) 10:1214. doi: 10.3389/fphar.2019.01214
6. Lee Y-H, Ko P-Y, Kao S-L, Lin M-C, Cheng-Chung Wei J. Risk of total knee and hip arthroplasty in patients with rheumatoid arthritis: a 12-year retrospective cohort study of 65,898 patients. J Arthrop. (2020) 35:3517–23. doi: 10.1016/j.arth.2020.06.085
7. Singh JA, Saag KG, Bridges SL Jr, Akl EA, Bannuru RR, Sullivan MC, et al. 2015 American College of Rheumatology guideline for the treatment of rheumatoid arthritis. Arthritis Care Res. (2016) 68:1–25. doi: 10.1002/acr.22783
8. Massardo L, Gabriel SE, Crowson CS, O'Fallon WM, Matteson EL. A population based assessment of the use of orthopedic surgery in patients with rheumatoid arthritis. J Rheumatol. (2002) 29:52–6.
9. da Silva E, Doran MF, Crowson CS, O'Fallon WM, Matteson EL. Declining use of orthopedic surgery in patients with rheumatoid arthritis? Results of a long-term, population-based assessment. Arthritis Rheum. (2003) 49:216–20. doi: 10.1002/art.10998
10. Louie GH, Ward MM. Changes in the rates of joint surgery among patients with rheumatoid arthritis in California, 1983-2007. Ann Rheum Dis. (2010) 69:868–71. doi: 10.1136/ard.2009.112474
11. Jämsen E, Virta LJ, Hakala M, Kauppi MJ, Malmivaara A, Lehto MU. The decline in joint replacement surgery in rheumatoid arthritis is associated with a concomitant increase in the intensity of anti-rheumatic therapy: a nationwide register-based study from 1995 through 2010. Acta Orthop. (2013) 84:331–7. doi: 10.3109/17453674.2013.810519
12. Young BL, Watson SL, Perez JL, McGwin G, Singh JA, Ponce BA. Trends in joint replacement surgery in patients with rheumatoid arthritis. J Rheumatol. (2018) 45:158–64. doi: 10.3899/jrheum.170001
13. Cordtz RL, Zobbe K, Højgaard P, Kristensen LE, Overgaard S, Odgaard A, et al. Predictors of revision, prosthetic joint infection and mortality following total hip or total knee arthroplasty in patients with rheumatoid arthritis: a nationwide cohort study using Danish healthcare registers. Ann Rheum Dis. (2018) 77:281–8. doi: 10.1136/annrheumdis-2017-212339
14. Maradit Kremers H, Larson DR, Crowson CS, Kremers WK, Washington RE, Steiner CA, et al. Prevalence of total hip and knee replacement in the United States. J Bone Joint Surg Am. (2015) 97:1386–97. doi: 10.2106/JBJS.N.01141
15. Arnett FC, Edworthy SM, Bloch DA, McShane DJ, Fries JF, Cooper NS, et al. The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum. (1988) 31:315–24. doi: 10.1002/art.1780310302
16. Skyttä ET, Honkanen PB, Eskelinen A, Huhtala H, Remes V. Fewer and older patients with rheumatoid arthritis need total knee replacement. Scand J Rheumatol. (2012) 41:345–9. doi: 10.3109/03009742.2012.681061
17. Fevang BT, Lie SA, Havelin LI, Engesaeter LB, Furnes O. Reduction in orthopedic surgery among patients with chronic inflammatory joint disease in Norway, 1994-2004. Arthritis Rheum. (2007) 57:529–32. doi: 10.1002/art.22628
18. Kumar A, Tsai WC, Tan TS, Kung PT, Chiu LT, Ku MC. Temporal trends in primary and revision total knee and hip replacement in Taiwan. J Chin Med Assoc. (2015) 78:538–44. doi: 10.1016/j.jcma.2015.06.005
19. Sloan M, Premkumar A, Sheth NP. Projected volume of primary total joint arthroplasty in the U.S., 2014 to 2030. J Bone Joint Surg Am. (2018) 100:1455–60. doi: 10.2106/JBJS.17.01617
20. Boutis K, Stephens D, Lam K, Ungar WJ, Schuh S. The impact of SARS on a tertiary care pediatric emergency department. CMAJ. (2004) 171:1353–8. doi: 10.1503/cmaj.1031257
21. Hawley S, Edwards CJ, Arden NK, Delmestri A, Cooper C, Judge A, et al. Descriptive epidemiology of hip and knee replacement in rheumatoid arthritis: an analysis of UK electronic medical records. Semin Arthritis Rheum. (2020) 50:237–44. doi: 10.1016/j.semarthrit.2019.08.008
22. Weiss RJ, Stark A, Wick MC, Ehlin A, Palmblad K, Wretenberg P. Orthopaedic surgery of the lower limbs in 49,802 rheumatoid arthritis patients: results from the Swedish National Inpatient Registry during 1987 to 2001. Ann Rheum Dis. (2006) 65:335–41. doi: 10.1136/ard.2005.039420
23. Hekmat K, Jacobsson L, Nilsson J, Petersson IF, Robertsson O, Garellick G, et al. Decrease in the incidence of total hip arthroplasties in patients with rheumatoid arthritis–results from a well defined population in south Sweden. Arthritis Res Ther. (2011) 13:R67. doi: 10.1186/ar3328
24. Hawley S, Ali MS, Cordtz R, Dreyer L, Edwards CJ, Arden NK, et al. Impact of TNF inhibitor therapy on joint replacement rates in rheumatoid arthritis: a matched cohort analysis of BSRBR-RA UK registry data. Rheumatology. (2019) 58:1168–75. doi: 10.1093/rheumatology/key424
25. Mertelsmann-Voss C, Lyman S, Pan TJ, Goodman SM, Figgie MP, Mandl LA. US trends in rates of arthroplasty for inflammatory arthritis including rheumatoid arthritis, juvenile idiopathic arthritis, and spondyloarthritis. Arthritis Rheumatol. (2014) 66:1432–9. doi: 10.1002/art.38384
26. Sokka T, Kautiainen H, Hannonen P. Stable occurrence of knee and hip total joint replacement in Central Finland between 1986 and 2003: an indication of improved long-term outcomes of rheumatoid arthritis. Ann Rheum Dis. (2007) 66:341–4. doi: 10.1136/ard.2006.057067
27. James D, Young A, Kulinskaya E, Knight E, Thompson W, Ollier W, et al. Orthopaedic intervention in early rheumatoid arthritis. Occurrence and predictive factors in an inception cohort of 1064 patients followed for 5 years. Rheumatology. (2004) 43:369–76. doi: 10.1093/rheumatology/keh059
28. Kuo CF, Luo SF, See LC, Chou IJ, Chang HC, Yu KH. Rheumatoid arthritis prevalence, incidence, and mortality rates: a nationwide population study in Taiwan. Rheumatol Int. (2013) 33:355–60. doi: 10.1007/s00296-012-2411-7
29. Lin FH, Chen HC, Lin C, Chiu YL, Lee HS, Chang H, et al. The increase in total knee replacement surgery in Taiwan: a 15-year retrospective study. Medicine. (2018) 97:e11749. doi: 10.1097/MD.0000000000011749
30. Hawley S, Cordtz R, Dreyer L, Edwards CJ, Arden NK, Delmestri A, et al. Association between NICE guidance on biologic therapies with rates of hip and knee replacement among rheumatoid arthritis patients in England and Wales: an interrupted time-series analysis. Semin Arthritis Rheum. (2018) 47:605–10. doi: 10.1016/j.semarthrit.2017.09.006
31. Cordtz RL, Hawley S, Prieto-Alhambra D, Højgaard P, Zobbe K, Overgaard S, et al. Incidence of hip and knee replacement in patients with rheumatoid arthritis following the introduction of biological DMARDs: an interrupted time-series analysis using nationwide Danish healthcare registers. Ann Rheum Dis. (2018) 77:684–9. doi: 10.1136/annrheumdis-2017-212424
32. Lee CY, Tai CJ, Tsai YF, Kuan YH, Lee CH, Huang KH. Prescribing trend of antirheumatic drugs in taiwan and risk of cardiovascular disease in patients with rheumatoid arthritis: a nationwide cohort study. Biomed Res Int. (2019) 2019:7987529. doi: 10.1155/2019/7987529
33. Lang HC, Lee HC, Lee SS, Lin HY, Chiu YM. The impact of introducing biologics to patients with rheumatoid arthritis in Taiwan: a population-based trend study. Int J Rheum Dis. (2016) 19:1112–8. doi: 10.1111/1756-185X.12813
34. Liao TL, Lin CH, Chen YM, Chang CL, Chen HH, Chen DY. Different risk of tuberculosis and efficacy of isoniazid prophylaxis in rheumatoid arthritis patients with biologic therapy: a nationwide retrospective cohort study in Taiwan. PLoS ONE. (2016) 11:e0153217. doi: 10.1371/journal.pone.0153217
35. Sokka T, Kautiainen H, Häkkinen A, Hannonen P. Radiographic progression is getting milder in patients with early rheumatoid arthritis. Results of 3 cohorts over 5 years. J Rheumatol. (2004) 31:1073–82.
36. Aletaha D, Neogi T, Silman AJ, Funovits J, Felson DT, Bingham CO 3rd, et al. 2010 Rheumatoid arthritis classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Arthritis Rheum. (2010) 62:2569–81. doi: 10.1002/art.27584
37. Lai YS, Wei HW, Cheng CK. Incidence of hip replacement among national health insurance enrollees in Taiwan. J Orthop Surg Res. (2008) 3:42. doi: 10.1186/1749-799X-3-42
38. Lu MC, Liu KC, Lai NS, Koo M. Higher incidence of rheumatoid arthritis in patients with symptomatic osteoarthritis or osteoarthritis-related surgery: a nationwide, population-based, case-control study in Taiwan. BMJ Open. (2015) 5:e008513. doi: 10.1136/bmjopen-2015-008513
39. Bogoch ER, Moran EL. Bone abnormalities in the surgical treatment of patients with rheumatoid arthritis. Clin Orthop Relat Res. (1999) 366:8–21. doi: 10.1097/00003086-199909000-00003
40. Bernatz JT, Brooks AE, Squire MW, Illgen RI 2nd, Binkley NC, Anderson PA. Osteoporosis is common and undertreated prior to total joint arthroplasty. J Arthroplasty. (2019) 34:1347–53. doi: 10.1016/j.arth.2019.03.044
41. Tang WM, Chiu KY. Primary total hip arthroplasty in patients with ankylosing spondylitis. J Arthrop. (2000) 15:52–8. doi: 10.1016/S0883-5403(00)91155-0
42. Carsons SE, Vivino FB, Parke A, Carteron N, Sankar V, Brasington R, et al. Treatment guidelines for rheumatologic manifestations of Sjögren's syndrome: use of biologic agents, management of fatigue, and inflammatory musculoskeletal pain. Arthritis Care Res. (2017) 69:517–27. doi: 10.1002/acr.22968
43. Panush RS, Edwards NL, Longley S, Webster E. ‘Rhupus’ syndrome. Arch Intern Med. (1988) 148:1633–6. doi: 10.1001/archinte.1988.00380070117028
Keywords: rheumatoid arthritis, total knee arthroplasty, total hip arthroplasty, population-based, pharmacological influences, big data and analytics
Citation: Tung K-K, Lee Y-H, Lin C-C, Lee C-H, Lin M-C and Wei J-C (2021) Opposing Trends in Total Knee and Hip Arthroplasties for Patients With Rheumatoid Arthritis vs. the General Population—A 14-Year Retrospective Study in Taiwan. Front. Med. 8:640275. doi: 10.3389/fmed.2021.640275
Received: 11 December 2020; Accepted: 24 March 2021;
Published: 20 April 2021.
Edited by:
Xenofon Baraliakos, Rheumazentrum Ruhrgebiet, GermanyReviewed by:
Deng-Ho Yang, Taichung Armed Forces General Hospital, TaiwanArti Mahto, King's College Hospital NHS Foundation Trust, United Kingdom
Copyright © 2021 Tung, Lee, Lin, Lee, Lin and Wei. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: James Cheng-Chung Wei, amNjd2VpJiN4MDAwNDA7Z21haWwuY29t
†These authors have contributed equally to this work and share first authorship
 Kuan-Kai Tung
Kuan-Kai Tung Yung-Heng Lee
Yung-Heng Lee Chuan-Chao Lin
Chuan-Chao Lin Cheng-Hung Lee1,7
Cheng-Hung Lee1,7 Mei-Chen Lin
Mei-Chen Lin James Cheng-Chung Wei
James Cheng-Chung Wei