- Pulmonary Rehabilitation Department, Istituti Clinici Scientifici Maugeri, Istituto di Ricerca e Cura a Carattere Scientifico (IRCCS), Institute of Veruno, Novara, Italy
The management of bronchial secretions is one of the main problems encountered in a wide spectrum of medical conditions ranging from respiratory disorders, neuromuscular disorders and patients undergoing either thoracic or abdominal surgery. The purpose of this review is illustrate to the reader the different ACTs currently available and the related evidence present in literature. Alongside methods with a strong background behind as postural drainage, manual techniques or PEP systems, the current orientation is increasingly aimed at devices that can mobilize and / or remove secretions. Cough Assist, Vacuum Techniques, systems that modulate airflow have more and more scientific evidence. Different principles combination is a new field of investigation that goes toward an increasing of clinical complexity that will facing us.
Introduction
The management of bronchial secretions is one of the main problems encountered in a wide spectrum of medical conditions ranging from respiratory disorders (e.g., COPD, bronchiectasis, cystic fibrosis) to neuromuscular disorders (e.g., ALS) to patients undergoing either thoracic or abdominal surgery. The term airway clearance techniques (ACTs) refers to a variety of different strategies used to eliminate excess secretions. Their aim is to reduce airway obstruction caused by secretions occupying the airway lumen and so prevent respiratory tract infections, re-expand the collapsed areas of the lung, thus improving gas exchanges and decreasing the inflammatory response (1–4).
A wide range of treatments, techniques and devices are present in the scientific literature for managing bronchial encumbrance in respiratory physiotherapy; but their very multiplicity begs the question in daily clinical practice: “which of these treatments is it better to use to obtain the better result in my patient?.” Up to now, for all ACTs there is insufficient evidence to prove their efficacy and effectiveness in different clinical scenarios or to affirm the superiority of one technique over another (5–8). This absence of evidence, however, does not necessarily mean an absence of efficacy. Obviously, there is a need for more studies to increase the body of scientific evidence on this topic (9).
Looking at the issue from the other side, i.e., from the patient's perspective, rarely is just one single technique used for a given pathological condition. In addition, for many patients and/or categories of patients the goal might be to combine the best effect on clearance of the airways with the lowest possible incidence of side effects and of adverse events, such as exacerbation of the underlying pathophysiology (10). According to Lapin (11), the overall effectiveness of any technique is influenced by several factors closely related to the patient. Adherence to treatment is fundamental and it depends very much on the patient's satisfaction, motivation and perceived effectiveness. Therefore, it is essential always to take into account the patient's preferences, and base one's choices about which technique to use not only on the relief of symptoms, but also on the adaptability of the technique to the patient's lifestyle.
Underlying these numerous techniques, however, are a series of different physiological mechanisms used for “unblocking” the obstruction:
• Increase of expiratory flow
• Oscillation of the airflow
• Increase in lung volumes.
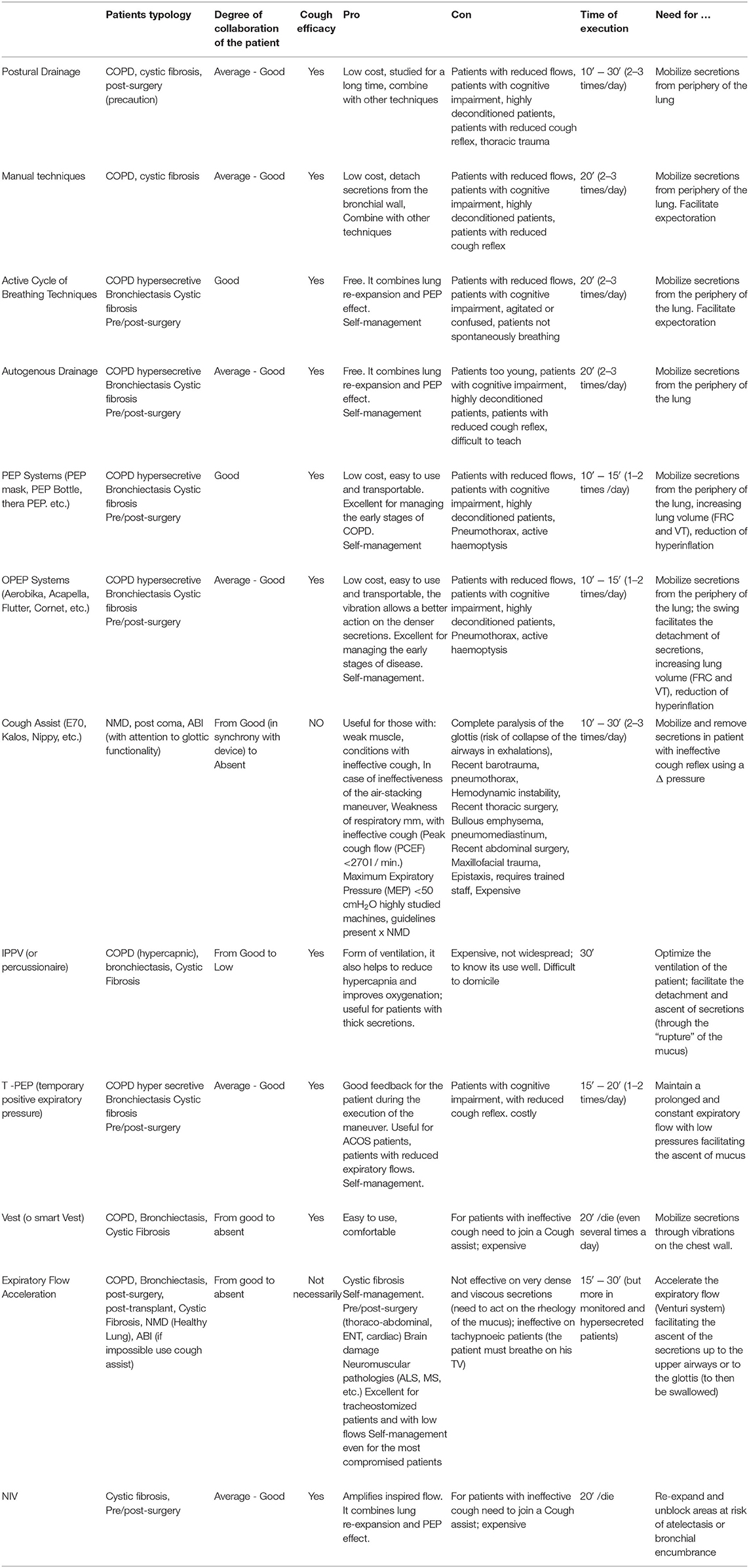
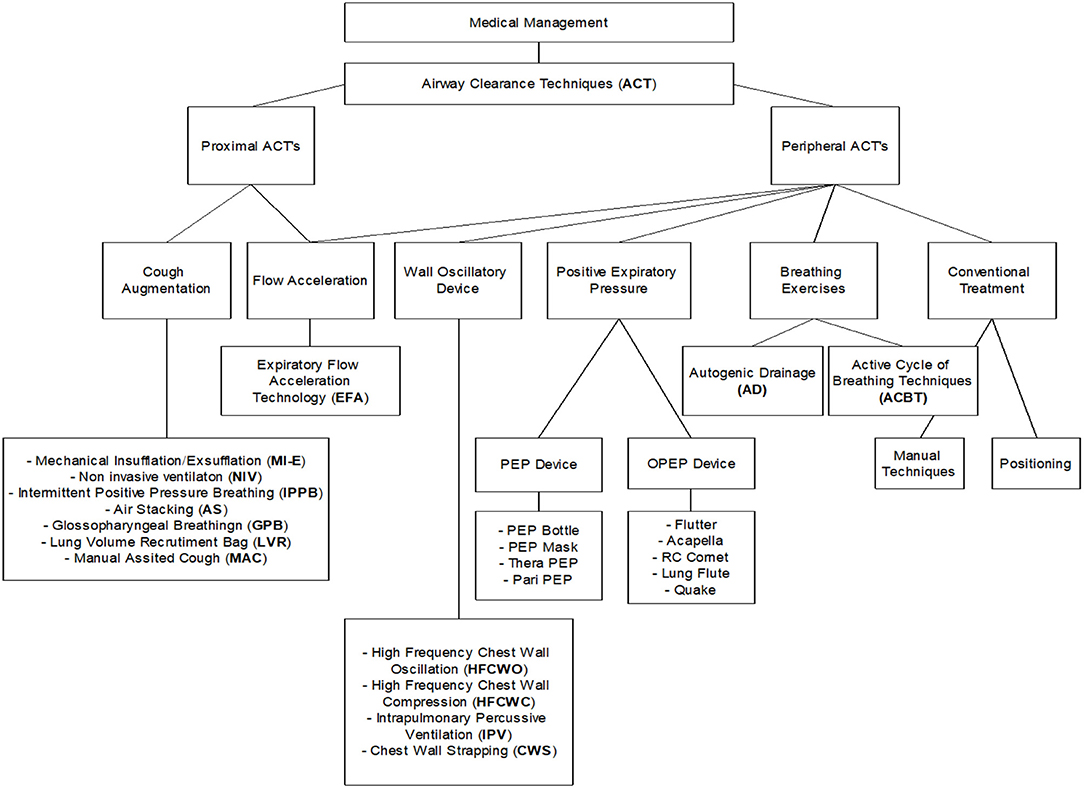
The aim of this review is to illustrate to the reader the different ACTs that are currently available (Table 1 and Figure 1). Although our paper is not a systematic review nor a meta-analysis, we hope it can help the reader gain a better understanding on how to proceed when choosing ACTs for their patients.
Description of Different Airway Clearance Techniques
Postural Drainage
Postural drainage (PD) was one of the first techniques used. Nelson (12) was the first to describe the use of precise postures based on the anatomy of the bronchial tree. This technique exploits the force of gravity in order to facilitate the sliding of the mucus from the periphery toward the central airways where, with coughing, forced expiration (FET) or bronchial aspiration, it can be removed.
There are conflicting opinions in the literature about this technique. Several studies have investigated PD using radioactive aerosol to mark mucus and evaluate its clearance during PD, but none of them has ever confirmed the assumption that gravity alone can promote mucus displacement. In 2002, an article in Respiratory Care (Fink JB) stated that gravity is not a physiological mechanism for transporting mucus but is important for lung function, i.e., it has an effect on ventilation, perfusion and lymphatic drainage. Other authors such as Cecins (13) and Eaton (14) showed that PD is more effective than oscillatory positive expiratory pressure (OPEP) or Active Cycle of Breathing Techniques (ACBT) used alone in terms of the volume of secretions eliminated. However, several patients find this technique uncomfortable, as it increases the sense of dyspnoea (15). Fink (16) stated that “…PD has been shown to have little or no effect in diseases associated with low content of secretions, thus the signs indicating PD are largely limited to patients who have secretion production >30 ml per day….” Some authors, such as Bott (17), suggest that if severely affected patients find PD helpful during exacerbations, concomitant use of Intermittent Positive Pressure Breathing (IPPB) or Non-Invasive Ventilation (NIV) might help overcome the sense of increased dyspnoea with the additional benefits of PEP therapy for secretion management.
Manual Techniques
These are techniques that involve applying certain forces to the patient's chest using the hands. Among the best known and most used, we find:
• Percussion (or Clapping): a rhythmic succession of rapid and light strokes performed with cupped hands on the patient's chest wall. The technique is applied to the specific segment to be treated while the patient breathes at a tidal volume (therefore both during inspiration and during exhalation). Percussion strength should be based on patient feedback (it must not create discomfort). The frequency to use must be between 4.6 and 8.5 Hz (18).
• Vibration: the application, during the whole exhalation phase, of fine oscillatory movements combined with a compression of the chest wall. The force that the therapist uses must be enough to compress the rib cage and increase the expiratory flow but, at the same time, it must not create discomfort for the patient.
There is some evidence regarding the physiological effects of these manual techniques on the clearance of secretions. During these techniques, an intermittent positive pressure is applied on the chest wall; this pressure is then transmitted to the airways causing an oscillation of the airflow and an increase in expiratory flow (18), i.e., two of the three afore-mentioned physiological mechanisms that should help clear the airways. However, to date there is no strong evidence to support or reject the use of manual techniques compared to other clearance interventions (5, 19). Some studies show that a combination of PD and percussion or vibrations are equally useful to other unblocking techniques as clearance strategies (6), improving sputum production when used in addition to forced expiration (FET) and PD techniques (20). McCarren and Alison (18) made a comparison between the OPEP devices (Flutter and Acapella) and manual techniques and showed that, although the OPEP devices produced higher oscillation frequencies than vibrations and percussions, the vibrations produced higher expiratory flow rates. So long as there is no high-quality research giving us a definitive answer on the effectiveness of these interventions, it is necessary to depend on the patient's preference. It can therefore be said that manual techniques are useful in patients who prefer these techniques or who are unable to collaborate in the treatment (patients with neuromuscular weakness, with cognitive problems, unconscious, strongly sedated, too young, etc.) as they are manual techniques, administered by an operator (physiotherapist or caregiver). However, it is important to emphasize that the evidence suggests that patient adherence to treatment is greater if self-administered techniques are used (17).
Respiratory Techniques
Active Cycle of Breathing Techniques
In 1979, Pryor et al. (21) described a clearance strategy characterized by the fact that it does not require the use of specific equipment, for which reason it is preferred by many patients. The strategy is called Active Cycle of Breathing Techniques (ACBTs) and consists of three distinct breathing cycles performed in sequence: Breath Control, Thoracic Expansion Exercises (TEE) and Forced Exhalation Technique (FET). Breath Control simply consists of breathing at tidal volume, using a diaphragmatic breathing pattern, at the patient's own frequency and respiratory volume. This allows recovery from fatigue, desaturation, signs of bronchospasm and possible dyspnoea that may have occurred during the most active components of the cycle (22). The TEE consist of three or four respiratory acts characterized by a slow, deep inhalation (larger volumes than the tidal volume) through the nose, with a pause of about 3 s at the end of inspiration, followed by a passive exhalation. This deep inhalation should facilitate the collateral ventilation, and then the flow of air through the intrabronchial channels of Martin, the bronchoalveolar channels of Lambert and the interalveolar pores of Kohn (23). In this way, the patient should be able to bring air behind the secretions and then expand those areas that are blocked. Finally, the patient has to perform the FET, which consists of a combination of one or two forced expirations, called “Huff” and a tidal volume respiratory act. This exercise is most effective when the length of the Huff and the contraction force of the expiratory muscles determines the maximum expiratory airflow, minimizing the collapsing the airways. Usually, ACBT is effective when applied in a vertical position, but in reality it can be combined with other devices and/or in other positions (13) or in conjunction with manual techniques (percussion or vibrations). A systematic review of Cochrane compared the clinical efficacy of ACBT with other clearance strategies, and concluded that there is not enough evidence to suggest that ACBT is superior to any other technique. One can consider it comparable to other techniques in terms of patient preference, lung function, sputum weight, oxygen saturation and number of lung exacerbations (24), and comparable in terms of lung function, exercise capacity and quality of life for a long-term use (25).
Autogenous Drainage
Another clearance strategy that requires no specific device or equipment is Autogenous Drainage (AD). Developed in the 60s in Belgium, AD is characterized by three phases: “Unstick,” “Collect,” and “Evacuate” (26). Each phase consists of a series of respiratory acts in which a certain lung volume is mobilized (the volume mobilized in the “Evacuate” phase will be greater than that in the “Collect” phase which in turn will be greater than that mobilized in the “Unstick” phase). The rationale behind this technique is that shear forces are generated, through the exhaled airflow to the various lung volumes, which should reduce the adhesion of the mucus, detach the secretions from the bronchial walls and transport them from the peripheral airways to the proximal ones (26). It is important to underline that this strategy, at a technical level, is very complex to perform and therefore it may be difficult for some patients. Several studies have compared the AD technique to other clearance methods. These include the study conducted by Pryor (25) which demonstrated its clinical equivalence, in terms of all measured results, including quality of life and lung function, with the other methods analyzed (AD, ACBT, PEP, Flutter and RC-Cornet).
PEP Mechanisms
In the late 1970s, the use of Positive Expiratory Pressure (PEP) as an airway clearance strategy, introduced in Denmark, became widespread. PEP therapy consists in exhaling against a flow or a resistance at the threshold in order to produce positive pressure in the airways throughout the expiratory phase. The rationale behind this therapy is that it promotes, during inspiration, the flow of air beyond the obstruction through the collateral channels, causing the accumulation of a greater volume of air behind the secretions. This should create a pressure gradient astride the obstruction, which would favor the movement of the secretions in a centripetal direction (27, 28). Furthermore, during exhalation, the positive pressure generated prevents premature collapse of the peripheral airways (29). The PEP therapy most used in clinical practice is the low-pressure type (also referred to as “low PEP”). It consists in maintaining a relatively low expiratory pressure in the mouth, between 10 and 20 cmH2O. Inspiration is required for a slightly larger volume of air than the tidal volume, with a pause at the end of inspiration (to allow the physiological mechanisms of Pendelluft flow, interdependence and collateral ventilation) and then a slightly active exhalation against resistance. A variant of PEP therapy, used much less frequently in clinical practice, is high-pressure PEP (“HiPEP”) (30). It is used especially in patients who have an airway instability during forced expiration. Pressures ranging from 40 to 120 cmH2O are used, thus allowing to perform a forced expiratory maneuver (FET). The application then of a PEP during a FET is to avoid the premature collapse of the airway during the maneuver, thus allowing the patient to exhale a volume greater than his/her usual forced vital capacity (FVC). There are many different devices on the market designed to provide PEP therapy. Some combine PEP with high frequency oscillations of the airflow, the therapy being defined in this case as Oscillatory PEP (OPEP). Among the OPEP devices we mention Flutter, Acapella, RC-Cornet, Lung Flute and the PEP Bottle. All these devices are characterized by breathing against intermittent expiratory resistance to induce oscillations of variable frequency (depending on the device or use), which are transmitted to the respiratory tract during the expiratory cycle. The PEP component encourages the flow of air behind the secretions, while the oscillation induces vibrations within the bronchial walls to move the secretions into the lumen, and the repeated accelerations of the expiratory flow facilitate the movement of the secretions from the peripheral airways to the central ones (31). Studies investigating this strategy are very contradictory. In several long-term studies conducted on patients with Cystic Fibrosis, PEP was found to be more effective with respect to PD and percussion (32), the OPEP device Flutter (33), and high-frequency chest-wall oscillation (HFCWO) (34). However, a Cochrane review (5) showed no significant differences between PEP and other ACTs in individual treatments or in treatments with a duration of <3 months, in terms of FEV1. A long-term study found no significant difference in outcome between ACBT, AD, PEP, Flutter and RC-Cornet (25). In a 2017 Cochrane review conducted by Lee et al. (35), nine studies were analyzed, involving a total of 213 patients with bronchiectasis. From the comparison between PEP therapy and other clearance techniques (ACBT, ELTGOL, AD, and PD), it was concluded that there are no significant differences between them in terms of health-related quality of life (HRQOL), dyspnoea, mucus expectoration or lung volumes.
Mechanical devices
Cough assist (or Mechanical Insufflator/Exsufflator)
The Mechanical Insufflator/Exsufflator (I/E) is a device that produces changes in the airflow inside the bronchial tree in such a way as to vicariate the cough (36, 37). It is used mainly in patients with neuromuscular pathologies or respiratory muscle deficiency, who have a hypo valid or ineffective cough. An ineffective cough causes retained secretions, chronic inflammation and infections, increased airway resistance, decreased lung compliance and respiratory failure (38). Even a single treatment would lead to a short-term reduction of dyspnoea, as demonstrated in patients with Duchenne Muscular Dystrophy (39). Several studies have analyzed the peak of cough (PCEF), and demonstrated with the use of mechanical I/E an increase in PCEF, and therefore an increase in the effectiveness of the cough, particularly in patients with neuromuscular diseases (40–42). Vianello et al. (43) in 2005 demonstrated its effectiveness in preventing intubation, while in 2009 Chatwin and Simonds (44) stated that its use decreases the treatment time in patients with neuromuscular disease (44). There are precise guidelines on the use of cough assist treatment in patients with NMD (45), while it has not been found to be very effective in patients with COPD (46).
Percussive Intrapulmonary Ventilation
Percussive Intrapulmonary Ventilation (IPV) is a device developed in 1979 by Forrest Bird. It consists of a high-pressure flow generator and a valve for stopping the flow. While the patient is breathing normally, the device provides the patient with high-frequency mini bursts of air (50–550 cycles per minute), thus creating an internal vibration (or percussion) in the lung. The vibration should promote clearance (47). The IPV device can also provide ventilatory support in patients with neuromuscular disease (48) and in patients with COPD (49). There are conflicting opinions, however, about IPV in the literature. Among the positive reports, IPV was found to improve the clearance of secretions in patients with Duchenne Muscular Dystrophy compared to conventional physiotherapy (FET and manually assisted cough) (50). And in 2006 Clini et al. (51) showed that the combination of conventional physiotherapy with IPV, compared to conventional physiotherapy alone, improved the PaO2/FiO2 ratio and maximum expiratory pressure (MEP) and reduced the incidence of pneumonia. Newhouse et al. (52) in 1998 compared the use of IPV, Flutter and PD with Percussion and HFCWC in patients with Cystic Fibrosis and found that they all had the same efficacy. Paneroni et al. (53) in 2011 compared IPV with conventional physiotherapy (combination of FET, PD, Percussion and Vibrations) and did not find any difference, except for a lower level of dyspnoea in patients treated with IPV. A systematic review conducted by Reychler et al. (54) investigated the effects of IPV use in patients with COPD and Cystic Fibrosis and concluded that the technique is not supported by strong enough evidence to recommend its use on a daily basis. However, it may offer some benefit during COPD exacerbations by improving gas exchange and possibly reducing hospitalization days.
High-Frequency Chest-Wall Oscillation (HFCWO)
High-frequency chest-wall oscillation (HFCWO) or high-frequency chest-wall compression (HFCWC) is a strategy for secretion clearance based on use of an inflatable vest connected to a compressor that can determine rapid inflation and deflation of the vest. This creates oscillations with a frequency of 5–25 Hz, which are transmitted through the chest wall to the entire bronchial tree. The oscillations should increase the interaction between the airflow and the mucus, increasing the cutting forces and thus decreasing the viscoelasticity of the secretions (55). Furthermore, according to Chang et al. (56), the oscillations should improve ciliary activity. There are conflicting studies on this strategy in the literature. The first studies carried out showed a significant increase in the expectoration of secretions compared to baseline and control, but no difference compared to other techniques (DP, Percussion and PEP) (57). Allan et al. (58) in 2003 reported that the potential benefits of HFCWO could be obtained in various clinical conditions (asthma, COPD, neuromuscular diseases, post-operative patients). However, more recent studies have suggested that this strategy eliminates a smaller amount of secretions than other unblocking techniques during an infectious exacerbation (59), and that it may even increase the frequency of exacerbations compared to PEP therapy (34). Nicolini et al. (60) compared a large variety of unblocking techniques, including HFCWO, to a control group that did not receive any type of intervention. All the techniques, including HFCWO, achieved better results in all outcomes than the control, but it was not possible to affirm the superiority of one technique over another.
Uniko - TPEP®
Uniko - TPEP® is a new generation temporary positive expiratory pressure (TPEP) device. At the beginning of the patient's expiratory phase, this device delivers a pulsed flow (about 42 Hz) contrary to the exhaled air resulting in a very low positive pressure of about 1 cmH2O. This pulsed flow stops before the end of the exhalation, so that the end of the expiratory phase is spontaneous, without any pressure support. The flow delivered is so slight that it does not create an excessive workload for the patient. The interruption of resistance at the end of expiration causes a pressure gradient, which can help reduce pressure within the airways thus improving the elasticity of the lung walls and consequently causing a reduction in excessive overdistention. The vibration generated by the pulsed flow is transmitted throughout the respiratory tract, where its effect is to detach the secretions from the internal walls of the lungs. The shape of the mouthpiece is such that the patient has to carry out an active non-forced exhalation. The resulting “open glottal exhalation,” in addition to prolonging the expiratory phase, produces an acceleration of the expiratory flow. This makes Uniko-TPEP® a very useful device for the drainage of secretions and reducing air-trapping. Although the device has been on the market for a relatively short time, there are already several studies published in the literature. D'Abrosca et al. (61) compared PEP therapy with TPEP therapy (delivered with the Uniko device). Physiological parameters of both groups improved significantly and in a similar way. A subgroup analysis suggested that TPEP could provide greater benefit to patients with emphysema or on oxygen therapy, while PEP therapy would be of more benefit for patients on mechanical ventilation. Nicolini et al. (62) compared intermittent positive pressure breathing (IPPB) with TPEP and showed that the two techniques both significantly improve dyspnoea, quality of life and lung function in patients with severe COPD, although IPPB would seem to be more effective. Again, Nicolini et al. (63) compared TPEP with OPEP, in patients with severe COPD, and found that both techniques are useful for the treatment of COPD but only TPEP reduces exacerbations. Other studies also show that patients with severe COPD treated with TPEP have a lower incidence of exacerbations, as TPEP improves respiratory function parameters, improving dyspnoea (64). A randomized multicentre trial (65) concluded that TPEP improves lung volumes and accelerates the improvement of bronchial dimensions in patients with lung disease and hypersecretion.
Vacuum Technique
There is one device available that employs the vacuum technique to clear the airways: Free Aspire®. The device uses Expiratory Flow Accelerator (EFA®) technology, which accelerates the expiratory flow, promoting deep drainage and secretions removal in patients with or without ineffective cough, without applying any pressure in the airways. The secretions safely reach the upper airways where the patient can expel or ingest them in a physiological way through the mechanism of the mucociliary system.
The acceleration of expiratory flow is produced by a Venturi effect and the amount of flow acceleration is proportional to the expired airflow. The movement of air over the mucus layer develops a cutting force on the surface itself. When the shear force exceeds the surface tension in the mucous layer, the mucus begins to move in the direction of the airflow and secretions are “dragged” from peripheral to central areas. Bertelli et al. (66) described the clinical case of a 3-year-old girl with type-1 spinal muscular atrophy (SMA), and claimed that, in patients with ineffective cough and, hence, compromised secretions removal, Free Aspire is a safe and effective machine for the removal of bronchial secretions. Garuti et al. (67) described the use of Free Aspire in eight children with infantile cerebral palsy (a disease that, due to deformities of the ribcage, reduces cough and, given the patient's inability to collaborate, makes secretions management very problematic). They concluded that Free Aspire is safe and effective in reducing the impact of respiratory exacerbations in terms of visits to the pediatrician, days spent in hospital and days of antibiotic therapy. They also claimed that regular use of the device maintains these effects over time. Our group recently demonstrated the short-term efficacy of Free Aspire in tracheostomised patients; the device reduced the number of daily and deep aspirations in patients with bronchial dimensions from the first day of treatment (68). Likewise, Patrizio et al. (69), found a significant pre-post- improvement in arterial blood gases (ABG), and a significantly greater improvement with Free Aspire than Bubble PEP in PCEF, maximum inspiratory pressure (MIP), and the 6-min walk test (6MWT) post-treatment in patients with stable severe COPD.
Non-invasive Ventilation
NIV can be used to improve lung volume (PIP) associating the PEP effect during the expiratory phase. This option is used for patients who are not able to perform other ACTs without assistance, especially with severe/end-stage disease, inspiratory muscle weakness, severe hypoxia and dyspnoea. It can be useful adjuncts to other ACTs especially when people have difficulty expectorating (70–74).
Literature offers few studies demonstrating the effectiveness of this technique; most studies focus on cystic fibrosis patients and patients in acute settings.
It can certainly be considered a valid tool to assist traditional techniques.
Combined ACTs
In the last few years, new devices have begun to emerge that combine different techniques. The aim of these is to improve the clearance of excessive secretions in patients whose airway obstruction is driven by more than one mechanism. As an example, there is a device is now combining the vacuum with I/E techniques. It was designed to potentiate clearance by applying two different ACTs acting with different mechanisms; the principle is analogous to that of combining two different drugs in an inhalation device to treat asthma or COPD. Further research is needed (though to perform this adequately will not be easy) to investigate the effects of these new devices in different categories of patients.
COVID Patients
Clearance procedures should be administered only when considered strictly needed for the clinical improvement of the patient (75).
Assessment of mucus encumbrance or expectoration difficulties should be considered in all patient reporting pre-existing hyper-secretive condition, those after extubation or weaning from mechanicalventilation, those reporting phlegm or sticky mucus and productive cough. Early reports indicate that patients with COVID-19 do not show airway mucus hypersecretion, however, patients with specific comorbidities (e.g., COPD, cystic fibrosis, neuromuscular disease) might actually need respiratory support due to airway secretion retention or ineffective cough. In case of clinical signs for presence of airway secretion (by hearing, feeling, or chest x-ray), different techniques and devices can be applied to mobilization or evacuation (76). In hypersecretive patients, the use of continuous or temporary positive expiratory pressure device with or without oscillation (PEP, TPEP, OPEP), should be considered, alone or in combination with lung expansion strategies, to enhance lung volume recruitment, to better control the expiration flow and to facilitate peripheral and proximal mucus mobilization. Flow-dependent low resistance positive expiratory pressure (PEP) systems, with an antibacterial filter on expiration circuit, are more tolerated and should be preferred to high resistance and threshold-PEP, mostly in weaker or symptomatic patients
Since cough is one of the most annoying symptoms in COVID-19 lung involvement and can cause dyspnea or chest pain, forced expiratory flows (huffs) should be preferred to expectorate. Among ACTs, those that enable patient to auto-treatment should be preferred (77).
Conclusions
Based on the currently available ACTs, on the literature and on our experience, we have devised an algorithm to help in the decision-making as to what is the right ACT to use for each patient in our clinical practice.
We acknowledge that this schematic representation of the decision-tree for ATCs is somewhat arbitrary and reflects in many cases our own clinical judgement more than evidence-based data from the literature. Nevertheless, we propose it as a tool to help others confronted with the clinical problem of patients who require an ACT and the need to decide which one is best. We hope it may help in their decision-making and in building their clinical experience. Our goal, of course, is to improve the outcomes for our patients.
Author Contributions
SB drafted the paper. BB reviewed it and made important changes. All authors reviewed the literature and read the manuscript and made comments.
Funding
This work was supported by the Ricerca Corrente funding scheme of the Ministry of Health, Italy.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Fahy JV, Dickey BF. Airway mucus function and dysfunction. New Engl J Med. (2010) 363:2233–47. doi: 10.1056/NEJMra0910061
2. Randell SH, Boucher RC. Effective mucus clearance is essential for respiratory health. Am J Respir Cell Mol Biol. (2006) 35:20–8. doi: 10.1165/rcmb.2006-0082SF
3. Wanner A, Salathé M, O'Riordan TG. Mucociliary clearance in the airways. Am J Respir Crit Care Med. (1996) 154:1868–902. doi: 10.1164/ajrccm.154.6.8970383
4. Nici L, Donner C, Wouters E, Zuwallack R, Ambrosino N, Bourbeau J, et al. (2006) American Thoracic Society/European Respiratory Society statement on pulmonary rehabilitation. AMJ Respir Crit Care Med. 173:1390–413. doi: 10.1164/rccm.200508-1211ST
5. Elkins M, Jones A, van der Schans CP. Positive expiratory pressure physiotherapy for airway clearance in people with cystic fibrosis. Cochr Database Syst Rev. (2006) CD003147. doi: 10.1002/14651858.CD003147.pub3
6. Main E, Prasad A, Schans C. Conventional chest physiotherapy compared to other airway clearance techniques for cystic fibrosis. Cochr Database Syst Rev. (2005) 1:CD002011. doi: 10.1002/14651858.CD002011.pub2
7. Morrison L, Agnew J. Oscillating devices for airway clearance in people with cystic fibrosis. Cochr Database Syst Rev. (2009). doi: 10.1002/14651858.CD006842.pub2
8. Warnock L, Gates A, van der Schans CP. Chest physiotherapy compared to no chest physiotherapy for cystic fibrosis. Cochr Database Syst Rev. (2013). doi: 10.1002/14651858.CD001401.pub2
10. Hill K, Patman S, Brooks D. Effect of airway clearance techniques in patients experiencing an acute exacerbation of chronic obstructive pulmonary disease: a systematic review. Chron Respir Dis. (2010) 7:9–17. doi: 10.1177/1479972309348659
11. Lapin CD. Airway physiology, autogenic drainage, and active cycle of breathing. Respir Care. (2002) 47:778–85.
13. Cecins NM, Jenkins SC, Pengelley J, Ryan G. The active cycle of breathing techniques—to tip or not to tip?. Respir Med. (1999) 93:660–5. doi: 10.1016/S0954-6111(99)90107-5
14. Eaton T, Young P, Zeng I, Kolbe J. A randomized evaluation of the acute efficacy, acceptability and tolerability of flutter and active cycle of breathing with and without postural drainage in non-cystic fibrosis bronchiectasis. Chron Respir Dis. (2007) 4:23–30. doi: 10.1177/1479972306074481
15. Currie DC, Munro C, Gaskell D, Cole PJ. Practice, problems and compliance with postural drainage: a survey of chronic sputum producers. Br J Dis Chest. (1986) 80:249–53. doi: 10.1016/0007-0971(86)90060-4
17. Bott J, Blumenthal S, Buxton M, Ellum S, Falconer C, Garrod R, et al. Guidelines for the physiotherapy management of the adult, medical, spontaneously breathing patient. Thorax. (2009) 64 (Suppl. 1):i1–52. doi: 10.1136/thx.2008.110726
18. McCarren B, Alison JA, Herbert RD. Vibration and its effect on the respiratory system. Aust J Physiother. (2006) 52:39–43. doi: 10.1016/S0004-9514(06)70060-5
19. Lee AL, Burge A, Holland AE. Airway clearance techniques for bronchiectasis. Cochr Database Syst Rev. (2013) CD008351. doi: 10.1002/14651858.CD008351.pub2
20. Gallon A. Evaluation of chest percussion in the treatment of patients with copious sputum production. Respir Med. (1991) 85:45–51. doi: 10.1016/S0954-6111(06)80209-X
21. Pryor JA, Webber BA, Hodson ME, Batten JC. Evaluation of the forced expiration technique as an adjunct to postural drainage in treatment of cystic fibrosis. Br Med J. (1979) 2:417–8. doi: 10.1136/bmj.2.6187.417
22. Pryor JA, Webber BA, Hodson ME. Effect of chest physiotherapy on oxygen saturation in patients with cystic fibrosis. Thorax. (1990) 45:77. doi: 10.1136/thx.45.1.77
24. Mckoy NA, Saldanha IJ, Odelola OA, Robinson KA. Active cycle of breathing technique for cystic fibrosis. Cochr Database Syst Rev. (2012) (12). doi: 10.1002/14651858.CD007862.pub3
25. Pryor JA, Tannenbaum E, Scott SF, Burgess J, Cramer D, Gyi K, et al. Beyond postural drainage and percussion: Airway clearance in people with cystic fibrosis. J Cyst Fibrosis. (2010) 9:187–92. doi: 10.1016/j.jcf.2010.01.004
26. Heyningen V. Cystic fibrosis: horizons. Proceedings of the 9th International Congress, Brighton, England, June 9th-15th 1984. Edited by D. Lawson. Chichester: John Wiley. 1984. 446 pages. $15.00. ISBN 0 471 90439 2. Genet Res. (1984) 44:359–60. doi: 10.1017/S0016672300026598
27. Falk M, Kelstrup M, Andersen JB, Kinoshita T, Falk P, Støvring S, et al. Improving the ketchup bottle method with positive expiratory pressure, PEP, in cystic fibrosis. Eur J Respir Dis. (1984) 65:423–32.
28. Van der Schans CP, van der Mark TW, De Vries G, Piers DA, Beekhuis H, Dankert-Roelse JE, et al. Effect of positive expiratory pressure breathing in patients with cystic fibrosis. Thorax. (1991) 46:252–6. doi: 10.1136/thx.46.4.252
29. Darbee JC, Ohtake PJ, Grant BJ, Cerny FJ. Physiologic evidence for the efficacy of positive expiratory pressure as an airway clearance technique in patients with cystic fibrosis. Phys Ther. (2004) 84:524–37. doi: 10.1093/ptj/84.6.524
30. Oberwaldner B, Evans JC, Zach MS. Forced expirations against a variable resistance: a new chest physiotherapy method in cystic fibrosis. Pediatr Pulmonol. (1986) 2:358–67. doi: 10.1002/ppul.1950020608
31. App EM, Kieselmann R, Reinhardt D, Lindemann H, Dasgupta B, King M, et al. Sputum rheology changes in cystic fibrosis lung disease following two different types of physiotherapy: flutter vs autogenic drainage. Chest. (1998) 114:171–7. doi: 10.1378/chest.114.1.171
32. McIlwaine PM, Wong LT, Peacock D, Davidson AGF, of Paediatrics FD. Long-term comparative trial of conventional postural drainage and percussion versus positive expiratory pressure physiotherapy in the treatment of cystic fibrosis. J Pediatr. (1997) 131:570–4. doi: 10.1016/S0022-3476(97)70064-7
33. McIlwaine PM, Wong LT, Peacock D, Davidson AGF. Long-term comparative trial of positive expiratory pressure versus oscillating positive expiratory pressure (flutter) physiotherapy in the treatment of cystic fibrosis. J Pediatr. (2001) 138:845–50. doi: 10.1067/mpd.2001.114017
34. McIlwaine MP, Alarie N, Davidson GF, Lands LC, Ratjen F, Milner R, et al. Long-term multicentre randomised controlled study of high frequency chest wall oscillation versus positive expiratory pressure mask in cystic fibrosis. Thorax. (2013) 68:746–51. doi: 10.1136/thoraxjnl-2012-202915
35. Lee AL, Burge AT, Holland AE. Positive expiratory pressure therapy versus other airway clearance techniques for bronchiectasis. Cochr Libr. (2017) 9:CD011699. doi: 10.1002/14651858.CD011699.pub2
36. Fauroux B, Guillemot N, Aubertin G, Nathan N, Labit A, Clément A, et al. Physiologic benefits of mechanical insufflation-exsufflation in children with neuromuscular diseases. Chest. (2008) 133:161–8. doi: 10.1378/chest.07-1615
37. Morrow B, Zampoli M, van Aswegen H, Argent A. Mechanical insufflation-exsufflation for people with neuromuscular disorders. Cochr Database Syst Rev. (2013) CD010044. doi: 10.1002/14651858.CD010044.pub2
38. Homnick DN. Mechanical insufflation-exsufflation for airway mucus clearance. Respir Care. (2007) 52:1296–307.
39. Cesareo A, LoMauro A, Santi M, Biffi E, D'Angelo MG, Aliverti A. Acute effects of mechanical insufflation-exsufflation on the breathing pattern in stable subjects with duchenne muscular dystrophy. Respir Care. (2018) 63:955–65. doi: 10.4187/respcare.05895
40. Bach JR. Mechanical insufflation/exsufflation: has it come of age? A commentary. Eur J Res. (2003) 21:385–6. doi: 10.1183/09031936.03.00098702
41. Mustfa N, Aiello M, Lyall RA, Nikoletou D, Olivieri D, Leigh PN, et al. Cough augmentation in amyotrophic lateral sclerosis. Neurology. (2003) 61:1285–7. doi: 10.1212/01.WNL.0000092018.56823.02
42. Sancho J, Servera E, Díaz J, Marín J. Efficacy of mechanical insufflation-exsufflation in medically stable patients with amyotrophic lateral sclerosis. Chest. (2004) 125:1400–5. doi: 10.1378/chest.125.4.1400
43. Vianello A, Corrado A, Arcaro G, Gallan F, Ori C, Minuzzo M, et al. Mechanical insufflation–exsufflation improves outcomes for neuromuscular disease patients with respiratory tract infections. Am J Phys Med Rehabil. (2005) 84:83–8. doi: 10.1097/01.PHM.0000151941.97266.96
44. Chatwin M, Simonds AK. The addition of mechanical insufflation/exsufflation shortens airway-clearance sessions in neuromuscular patients with chest infection. Respir Care. (2009) 54:1473–9.
45. Chatwin M, Toussaint M, Gonçalves MR, Sheers N, Mellies U, Gonzales-Bermejo J, et al. Airway clearance techniques in neuromuscular disorders: a state of the art review. Respir Med. (2018) 136:98–110. doi: 10.1016/j.rmed.2018.01.012
46. Sivasothy P, Brown L, Smith IE, Shneerson JM. Effect of manually assisted cough and mechanical insufflation on cough flow of normal subjects, patients with chronic obstructive pulmonary disease (COPD), and patients with respiratory muscle weakness. Thorax. (2001) 56:438–44. doi: 10.1136/thorax.56.6.438
47. Fink JB, Mahlmeister MJ. High-frequency oscillation of the airway and chest wall. Respir Care. (2002) 47:797–807.
48. Chatwin M, O'Driscoll D, Corfield D, Morrell M, Simonds A. Controlled trial of intrapulmonary percussion in adults and children with stable severe neuromuscular disease. Am J Crit Care Med. (2004) 169:A438.
49. Nava S, Barbarito N, Piaggi G, De Mattia E, Cirio S. Physiological response to intrapulmonary percussive ventilation in stable COPD patients. Respir Med. (2006) 100:1526–33. doi: 10.1016/j.rmed.2006.01.010
50. Toussaint M, De Win H, Steens M, Soudon P. Effect of intrapulmonary percussive ventilation on mucus clearance in duchenne muscular dystrophy patients: a preliminary report. Respir Care. (2003) 48:940–7.
51. Clini EM, Degli Antoni F, Vitacca M, Crisafulli E, Paneroni M, Chezzi-Silva S, et al. Intrapulmonary percussive ventilation in tracheostomized patients: a randomized controlled trial. Intens Care Med. (2006) 32:1994–2001. doi: 10.1007/s00134-006-0427-8
52. Newhouse PA, White F, Marks JH, Homnick DN. The intrapulmonary percussive ventilator and flutter device compared to standard chest physiotherapy in patients wit cystic fibrosis. Clin Pediatr. (1998) 37:427–32. doi: 10.1177/000992289803700705
53. Paneroni M, Clini E, Simonelli C, Bianchi L, Degli Antoni F, Vitacca M. Safety and efficacy of short-term intrapulmonary percussive ventilation in patients with bronchiectasis. Respir Care. (2011) 56:984–8. doi: 10.4187/respcare.01098
54. Reychler G, Debier E, Contal O, Audag N. Intrapulmonary percussive ventilation as an airway clearance technique in subjects with chronic obstructive airway diseases. Respir Care. (2018) 63:620–31. doi: 10.4187/respcare.05876
55. King M, Phillips DM, Gross D, Vartian V, Chang HK, Zidulka A. Enhanced tracheal mucus clearance with high frequency chest wall compression. Am Rev Respir Dis. (1983) 128:511–5. doi: 10.1164/arrd.1983.128.3.511
56. Chang HK, Weber ME, King M. Mucus transport by high-frequency nonsymmetrical oscillatory airflow. J Appl Physiol. (1988) 65:1203–9. doi: 10.1152/jappl.1988.65.3.1203
57. Braggion C, Cappelletti LM, Cornacchia M, Zanolla L, Mastella G. Short-term effects of three chest physiotherapy regimens in patients hospitalized for pulmonary exacerbations of cystic fibrosis: a cross-over randomized study. Pediatr Pulmonol. (1995) 19:16–22. doi: 10.1002/ppul.1950190104
58. Allan JS, Garrity JM, Donahue DM. The utility of high-frequency chest wall oscillation therapy in the post-operative management of thoracic surgical patient. Chest. (2003) 124:235. doi: 10.1378/chest.124.4_MeetingAbstracts.235S-b
59. Osman LP, Roughton M, Hodson ME, Pryor JA. Short-term comparative study of high frequency chest wall oscillation and European airway clearance techniques in patients with cystic fibrosis. Thorax. (2010) 65:196–200. doi: 10.1136/thx.2008.111492
60. Nicolini A, Cardini F, Landucci N, Lanata S, Ferrari-Bravo M, Barlascini C. Effectiveness of treatment with high-frequency chest wall oscillation in patients with bronchiectasis. BMC Pulmon Med. (2013) 13:21. doi: 10.1186/1471-2466-13-21
61. D'Abrosca F, Garabelli B, Savio G, Barison A, Appendini L, Oliveira LV, et al. Comparing airways clearance techniques in chronic obstructive pulmonary disease and bronchiectasis: positive expiratory pressure or temporary positive expiratory pressure? A retrospective study. Braz J Phys Ther. (2017) 21:15–23. doi: 10.1016/j.bjpt.2016.12.001
62. Nicolini A, Mollar E, Grecchi B, Landucci N. Comparison of intermittent positive pressure breathing and temporary positive expiratory pressure in patients with severe chronic obstructive pulmonary disease. Arch Bronconeumol. (2014) 50:18–24. doi: 10.1016/j.arbr.2013.12.008
63. Nicolini A, Mascardi V, Grecchi B, Ferrari-Bravo M, Banfi P, Barlascini C. Comparison of effectiveness of temporary positive expiratory pressure versus oscillatory positive expiratory pressure in severe COPD patients. Clin Respir J. (2018) 12:1274–82. doi: 10.1111/crj.12661
64. Mascardi V, Grecchi B, Barlascini C, Banfi P, Nicolini A. Effectiveness of temporary positive expiratory pressure (T-PEP) at home and at hospital in patients with severe chronic obstructive pulmonary disease. J Thorac Dis. (2016) 8:2895. doi: 10.21037/jtd.2016.10.69
65. Venturelli E, Crisafulli E, DeBiase A, Righi D, Berrighi D, Cavicchioli PP, et al. Efficacy of temporary positive expiratory pressure (TPEP) in patients with lung diseases and chronic mucus hypersecretion. The UNIKO® project: a multicentre randomized controlled trial. Clin Rehabil. (2013) 27:336–46. doi: 10.1177/0269215512458940
66. Bertelli L, Di Nardo G, Cazzato S, Ricci G, Pession A. Free-Aspire: a new device for the management of airways clearance in patient with ineffective cough. Pediatr Rep. (2017) 9:7270. doi: 10.4081/pr.2017.7270
67. Garuti G, Verucchi E, Fanelli I, Giovannini M, Winck JC, Lusuardi M. Management of bronchial secretions with Free Aspire in children with cerebral palsy: impact on clinical outcomes and healthcare resources. Ital J Pediatr. (2016) 42:7. doi: 10.1186/s13052-016-0216-0
68. Belli S, Cattaneo D, D'Abrosca F, Prince I, Savio G, Balbi B. A pilot study on the non-invasive management of tracheobronchial secretions in tracheostomised patients. Clin Respir J. (2019) 13:637–42. doi: 10.1111/crj.13074
69. Patrizio G, D'Andria M, D'Abrosca F, Cabiaglia A, Tanzi F, Garuti G, et al. Airway clearance with expiratory flow accelerator technology: effectiveness of the “free aspire” device in patients with severe COPD. Turk Thorac J. (2019) 20:209. doi: 10.5152/TurkThoracJ.2018.18053
70. Fauroux B, Boulé M, Lofaso F, Zérah F, Clément A, Harf A, et al. Chest physiotherapy in cystic fibrosis: improved tolerance with nasal pressure support ventilation. Pediatrics. (1999) 103:e32. doi: 10.1542/peds.103.3.e32
71. Flight WG, Shaw J, Johnson S, Webb AK, Jones AM, Bentley AM, et al. Long-term non-invasive ventilation in cystic fibrosis—Experience over two decades. J Cyst Fibrosis. (2012) 11:187–92. doi: 10.1016/j.jcf.2011.11.006
72. Holland AE, Denehy L, Ntoumenopoulos G, Naughton MT, Wilson JW. Non-invasive ventilation assists chest physiotherapy in adults with acute exacerbations of cystic fibrosis. Thorax. (2003) 58:880–4. doi: 10.1136/thorax.58.10.880
73. Moran F, Bradley JM, Piper AJ. Non-invasive ventilation for cystic fibrosis. Cochr Database Syst Rev. (2009) CD002769. doi: 10.1002/14651858.CD002769.pub3
74. Young AC, Wilson JW, Kotsimbos TC, Naughton MT. Randomised placebo controlled trial of non-invasive ventilation for hypercapnia in cystic fibrosis. Thorax. (2008) 63:72–7. doi: 10.1136/thx.2007.082602
75. Lazzeri M, Lanza A, Bellini R, Bellofiore A, Cecchetto S, Colombo A, et al. Respiratory physiotherapy in patients with COVID-19 infection in acute setting: a Position Paper of the Italian Association of Respiratory Physiotherapists (ARIR). Monaldi Arch Chest Dis. (2020) 90. doi: 10.4081/monaldi.2020.1285
76. Felten-Barentsz KM, van Oorsouw R, Klooster E, Koenders N, Driehuis F, Hulzebos EH, et al. Recommendations for hospital-based physical therapists managing patients with COVID-19. Phys Ther. (2020) 100:1444–57. doi: 10.1093/ptj/pzaa114
Keywords: airway clearance techniques, disability, rehabilitation, COPD, bronchiectasis, amyotrophic lateral sclerosis, positive pressure, negative pressure
Citation: Belli S, Prince I, Savio G, Paracchini E, Cattaneo D, Bianchi M, Masocco F, Bellanti MT and Balbi B (2021) Airway Clearance Techniques: The Right Choice for the Right Patient. Front. Med. 8:544826. doi: 10.3389/fmed.2021.544826
Received: 22 March 2020; Accepted: 14 January 2021;
Published: 04 February 2021.
Edited by:
Enrico M. Clini, University of Modena and Reggio Emilia, ItalyReviewed by:
Chieko Kurihara, National Institutes for Quantum and Radiological Science and Technology, JapanStefania Costi, University of Modena and Reggio Emilia, Italy
Copyright © 2021 Belli, Prince, Savio, Paracchini, Cattaneo, Bianchi, Masocco, Bellanti and Balbi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Stefano Belli, c3RlZmFuby5iZWxsaUBpY3NtYXVnZXJpLml0
 Stefano Belli
Stefano Belli Ilaria Prince
Ilaria Prince Bruno Balbi
Bruno Balbi