- 1Department of Internal Medicine, King Hussein Cancer Center, Amman, Jordan
- 2Department of Molecular and Cellular Biology, College of Osteopathic Medicine, Sam Houston State University, Conroe, TX, United States
- 3Department of Pathology and Laboratory Medicine, King Hussein Cancer Center, Amman, Jordan
- 4Department of Surgery, King Hussein Cancer Center, Amman, Jordan
- 5Independent Researcher, Amman, Jordan
- 6Human Research Protection Program Office, King Hussein Cancer Center, Amman, Jordan
The shortage of healthcare providers is well-documented in low-income countries (LIC) prior to COVID-19, due to various causes including the migration to developed countries, scarcity of supplies, poor healthcare infrastructure, limited ICU facilities, and lack of access to guidelines and protocols. One of the important hitches in LIC is the insufficient testing capacity that precluded accurate assessment of disease burden and subsequently resource allocations. Trying to adhere to the principles of bioethics including respect to others, beneficence, and justice should be applied on the ground in the particular setting of the LIC. Solutions should be tailored to the tangible needs and possibility of implementation in real life in the face of the “already” limited resources by making use of simple, yet plausible, measures. Implementing guidelines and frameworks that were set to work in the better-resourced nations is a call for futility. The adoption of novel solutions to overcome the unique challenges in the LIC is exigent. These include the use of automated screening algorithms and virtual video clinics. Moreover, integrating electronic intensive care unit (e-ICU) software may allow for remote monitoring of multiple patients simultaneously. Telemedicine could help in getting consultations worldwide. It can also enhance healthcare workers' knowledge and introduce new skills through teleconferences, e-workshops, and free webinars. Healthcare workers can be remotely trained to enhance their skills. Agencies, such as the WHO, should develop comprehensive programs to tackle different health issues in LIC in collaboration with major institutions and experts around the world.
Introduction
Coronaviruses (CoVs) are a family of positive single-stranded RNA (+ssRNA) viruses that belong to family Coronaviridae (1). Three out of seven human coronaviruses (HCoVs) cause severe respiratory diseases of high fatality rates (2, 3). The first is Severe Acute Respiratory Syndrome-CoV (SARS-CoV) that emerged in 2002 followed by Middle East Respiratory Syndrome-CoV (MERS-CoV) in 2012 (2). In December 2019, SARS-CoV-2 was identified as the third HCoV that causes acute respiratory distress syndrome (ARD) with viral pneumonia (3). This disease was later named COVID-19 (4). The first cases of SARS-CoV-2 infections originated in the city of Wuhan, China and soon the disease spread to 177 countries causing a global outbreak (4). Millions of COVID-19 cases and more than a million deaths have been reported worldwide. The World Health Organization (WHO) had declared a public health emergency and characterized COVID-19 as a global pandemic on March 11, 2020 (5). SARS-CoV-2 positive cases with varying disease severity have flooded hospitals and healthcare facilities. The number of cases and deaths varied per country depending on the protective measures and resources to deal with such a highly transmissible and infectious virus.
The main concern in COVID-19 pandemic is that the disease burden may exceed healthcare resources that are available for treating patients (6). Even in developed countries, there was a concern that healthcare systems would be overwhelmed if COVID-19 cases increase dramatically (6). For example, in USA, there were not enough N95 masks which necessitated the reuse of such single use masks (7, 8). In Italy, ventilators and ICU beds were made available only for critically ill patients during the peak of the disease (9, 10). South Korea faced a shortage in hospital beds which lead to many deaths (10, 11).
Healthcare systems in developing countries face major problems during this time and are unlikely to offer the care needed. The scarcity in healthcare resources, training, and low number of healthcare workers are the most important reasons (10). Developing countries lack the testing capacities and the technologies to trace the infected individuals. Moreover, the cost of the COVID-19 screening test in developing countries mostly exceeds the total sum that healthcare systems spend per individual. N95 masks are in short supply in many developing countries. According to the United Nations, there are only an average of 113 hospital beds per 100,000 in developing countries which is 80% lower than the number in developed countries (12). Moreover, developing countries have a scarcity of ICU beds (0.1–2.5 per 100,000) when compared to developed countries (5–30 beds per 100,000) (13).
The scarcity of healthcare resources, particularly in developing countries, may create ethical dilemmas. This may include the need to provide care and treatment for more severely ill patients while delaying treatment for others who are in a better condition (14). The need to take such decisions may cause some healthcare workers to experience moral injury or mental health problems (15). It becomes very challenging when such decisions have to be made at the expense of ethical values.
In this article, we will discuss the deleterious impacts of the COVID-19 pandemic on healthcare workers and availability of resources, particularly in countries with limited resources, and will provide possible solutions to cope with the current emergency.
Methodology
We did a literature search to identify challenges facing healthcare workers in countries with limited resources during COVID-19 pandemic. We discuss the number of physician per capita, the number of hospital beds, ICU and ventilators in limited settings, the allocation of limited budget to the healthcare system and its impact on other services and more prevalent health conditions. Finally, we provide insight into possible solutions that may help alleviate the stress and demand on healthcare system, resources, and personnel.
Challenges Faced by the Healthcare Systems in LIC
Healthcare Workers Shortage and Burnout
A disparity between different countries' response to COVID 19 pandemic is evident. According to the World Bank data (Table 1), high and high-intermediate income countries have a higher number of physicians and nurses per capita as compared to low and low-intermediate income countries. Shortage of physicians in countries with insufficient resources could be attributed to slow economic growth that leads to limited healthcare annual budget and exodus of physicians to work in higher income countries. A study conducted by Astor et al. investigated the factors that contributed to physician migration from developing to developed countries. The desire for increased income, greater access to enhanced technology, need for safer, more stable, and better future for the family were the main listed causes (24). Another study discussed the insufficient numbers of surgeons, obstetricians and anesthesiologists in low- and intermediate income countries which was in part due to lack of training and educational opportunities for surgeons and other healthcare workers (25–27). The shortage of healthcare workers and scarcity of resources in low- and intermediate- income countries have led to increased work hours and burnout of healthcare personnel in these countries and more severe economic deterioration.
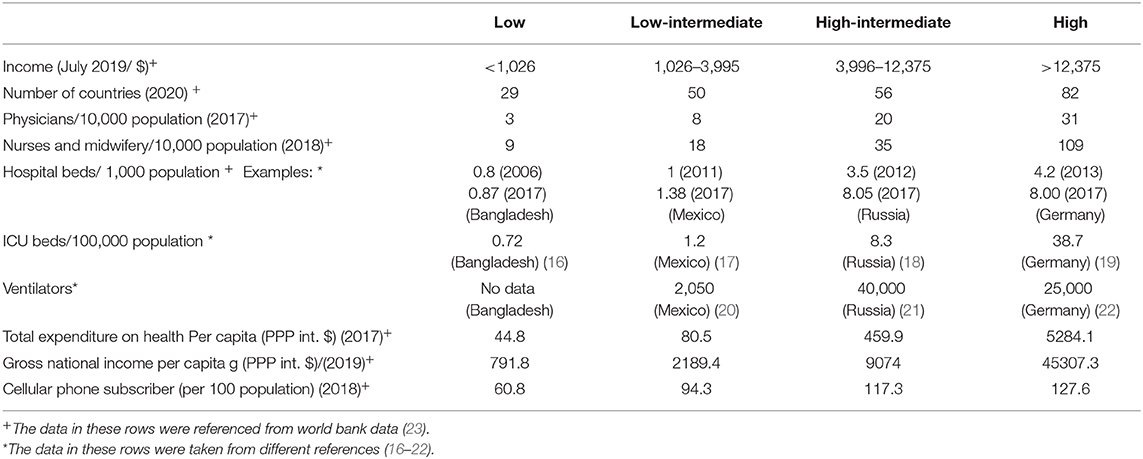
Table 1. The medical resources available in low income countries, low-intermediate, high-intermediate countries in comparison with high-income countries.
In the 2013–2016 Ebola outbreak, studies showed that stress and anxiety, due to tremendous pressure on healthcare workers, could lead to faster spread of the disease and the probability of healthcare workers quitting their job (28). This could result in a healthcare system collapse.
The healthcare systems worldwide are dealing with pandemic-related challenges and stressors that could eventually lead to healthcare workers' burnout (14). These include the fear of spreading infection to family members, and others, due to the close interaction with COVID-19 patients, increased workload, and requirement to provide care and treatment for all critically ill patients in the setting of inadequate PPE and other resources (14). This may require treatment of more severely ill patients while delaying treatment for others who are in a better condition; decisions which may cause some healthcare workers to experience moral injury or mental health problems. This may potentially progress to mental health problems such as depression, post-traumatic stress disorder, and even suicide (15). Furthermore, reduced social support, lack of self-care and family time, and lack of information about the COVID-19 transmission and disease prognosis are all factors that add up to the stressors that healthcare workers have to face (29). During the last SARS-CoV outbreak in Guangdong, China, there were reports of stress, anxiety, depression, and general psychological stress among health professionals (30). In addition, 21% of SARS cases were reported among healthcare providers (30).
Exhausted Healthcare Systems and Limited Testing Capacity
LIC have long been challenged by the limited healthcare resources including the availability of ICU and mechanical ventilators, even before the pandemic. The high cost of mechanical ventilators, the need for proper training and education, and the unavailability of ventilator protocols are factors that contributed to the challenges facing healthcare systems in developing countries (31). Unfortunately, the militarization of healthcare in some of the LIC, particularly in areas of conflicts and wars, adds to the limitation. The ongoing wars in some of LICs have put these countries in a more compromised situation (32). Patients suffering from chronic diseases have also suffered from decreased follow up to their conditions with others not even getting diagnosed due to the overwhelming of the health sector. For example, Skeete et al. found that patients with hypertension have suffered worse outcomes (higher mortality and morbidity) during the ongoing pandemic (33).
In addition, the shortage of testing capacity in LIC has left most people untested, thus precluding the accurate estimation of disease burden (Figure 1). Consequently, low testing capacity has led to inadequate planning to maximize the use of the available healthcare resources (35–37). Without enough data, countries would not be able to estimate the disease burden leading to poor allocation of resources toward combating the pandemic. In Jordan, for example, the government opted for a complete and strict lockdown at the beginning of the pandemic. Then gradually these measures were loosened causing a delay in the first major wave till mid to late October. During this time the government was able to ramp up its testing capabilities and have testing be wildly available and immediately act when the number of COVID-19 cases started increasing in October (Figure 2).
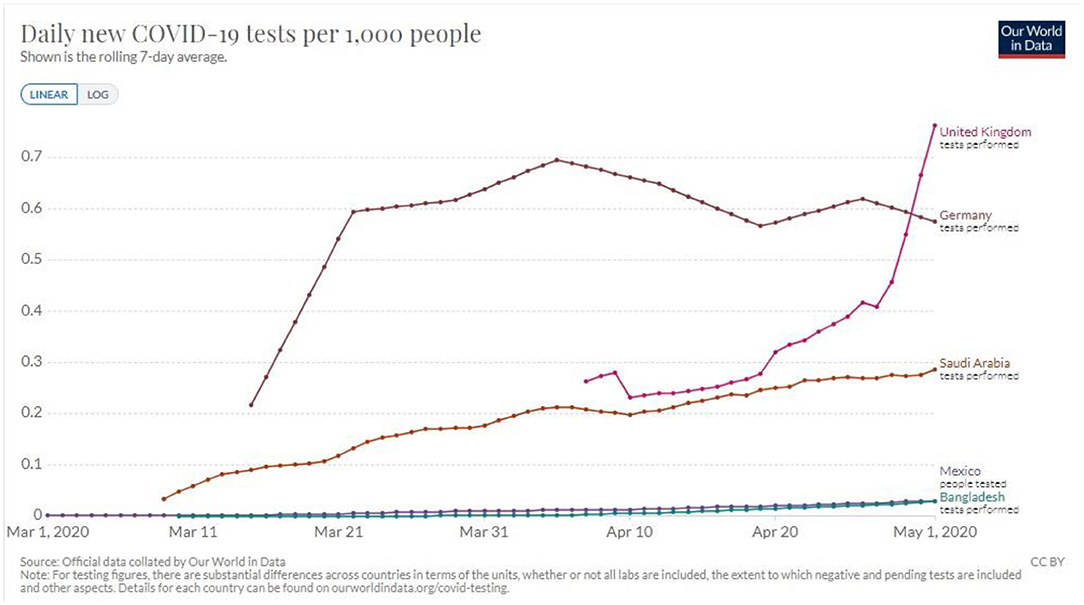
Figure 1. Testing capacity variations among countries of different incomes during the beginning of the pandemic (34).
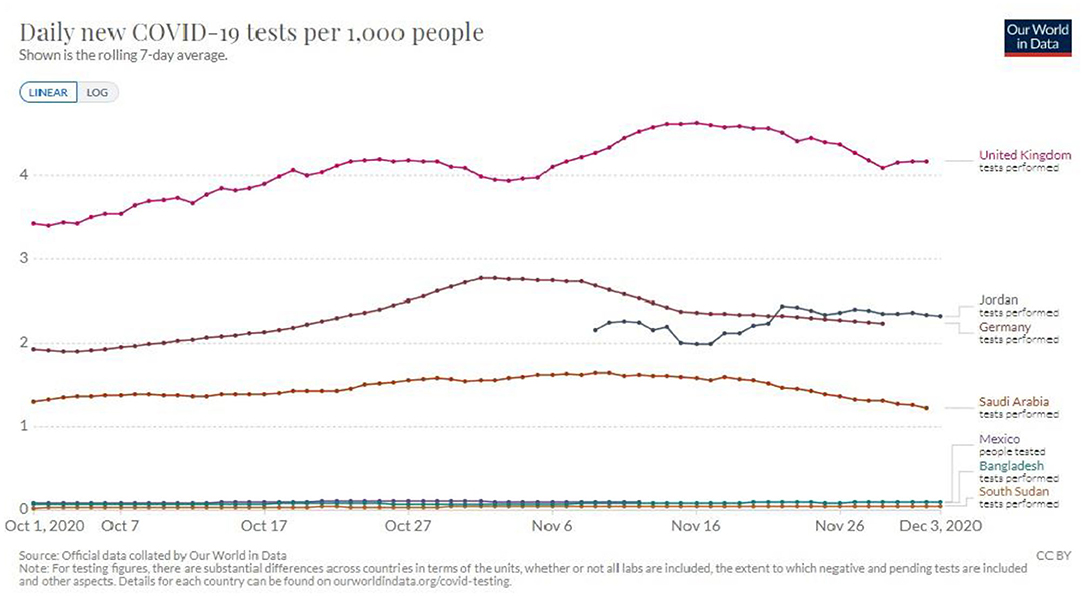
Figure 2. Testing capacity variations among countries of different incomes during the period of October–December, with a focus on Jordan's testing capacity in comparison to higher income countries (34).
The Scarcity of Personal Protective Equipment (PPE)
Disposable filtering face piece respirators (FFRs) including N95 respirator and surgical masks are designed for one-time use. LICs have always struggled with a deficient supply of Personal Protective Equipment (PPE). In view of the increased demand and shortage of supply, even with donations, stocks remained insufficient (35, 38, 39). Accordingly healthcare workers are wearing these masks for an extended period of time or they consider reusing them (40).
Humanitarian Aid Challenges
The withdrawal of humanitarian organizations‘ personnel, and travel constraints that interfere with international aids all add to the challenges that LICs have to face (35, 41, 42). During a crisis, the need for humanitarian aid spikes in LIC. This spike is normally dealt with by providing quick response, from logistical hubs, to supply the countries in need with the necessary provisions. However, during the lock downs and travel restrictions, aimed to suppress the spread of the virus, imposed by the countries that contain these hubs has left the countries dependent on aid in a dire need (43).
Suggested Solutions Tailored to the Actual Needs and Applicability to the LIC
Increasing Healthcare Systems' Work Force
Asking retired health care professionals to join the workforce to fight COVID-19, is an option adopted by some health authorities. Waiver of medical licensing fees and expediting the renewal of licenses for healthcare professionals, while providing extensions for the licenses that are expiring soon, could assist in promoting the accruing of this group of physicians. This might help in reducing the load on the practicing doctors. Retired healthcare workers are experienced, knowledgeable, and emotionally stable. However, asking retired healthcare professionals who are in their 60s and beyond to provide direct patient care could pose risk of infections for such individuals. We believe that it is better for this particular group of healthcare professionals to provide telemedicine or support services. Additinally, physicians who are specialized in other clinical areas may be trained to work in intensive care units. Medical assistants and nurses may be asked to help in patients' treatments under physicians' supervision.
Asking medical students of different institutions to help according to the level of seniority might also alleviate some of the workload. Medical students are usually young individuals who might be better suited to support the medical teams. We believe that these stratigies may increase the number of physicians at emergency care eventually leading to a reduced workload on individual physicions.
Social Support of the Healthcare Frontline Workers
In LIC, the extended families play a pivotal role in supporting working familiy members. However, practicing healthcare workers might be living away from their families. It is important that healthcare system leadership take measures to ensure that the healthcare workers are fully supported and cared for. Physicians who are placed on quarantine or are working over extended hours should be offered care for their children. Alternatively they could be asked to do office work for those who are in clinics and hospitals, and provide remote care and consultation for patients. Additional institutional policies that may help in alleviating healthcare workers stress and burnout may include paid time off and sick days in addition to coverage of expenses for employees with COVID-19-related illnesses.
Telemedicine
The application of telemedicine can be a sustainable solution to many of our challenges during the COVID 19 pandemic. According to the European commission, it can be defined as the provision of healthcare by using electronic information and communication technology to securely transmit information in text, sound, images and other forms to prevent, diagnose, or treat patients (44). Given the novelty of the COVID 19 virus, telemedicine can offer the community with a trusted medical opinion and avoid the chaos created by unreliable information on social media (45). It can help with the spread of experiences and medical knowledge form different parts of the world to reach remote areas and underserved communities by conducting frequent conferences and meetings between healthcare professionals and improving the response to this healthcare emergency (45). With the large increase in smartphone and internet users in developing countries, programs, and phone applications that allow for remote patient-doctor interaction are widely available (46). This can be very quickly utilized by training healthcare professionals to conduct online consults, as these applications don't require much training for use (46, 47).
Between October 5 and October 26, an online virtual workshop, organized by the WHO, took place. In this workshop, medical health professionals from the Jordanian public health sector were given lectures on various topics pertinent to COVID-19 screening and patient management protocols. This online workshop facilitated the sharing of medical knowledge and protocols while at the same time setting the trend of online lecturing and data sharing. These methods were then implemented in various hospitals in the public sector, thus facilitating a better quality of health care while limiting the need for large gatherings (48).
Another major benefit is the provision of direct interaction between patients and healthcare professionals. This helps maintain follow-up on chronic diseases from a distance, which might be interrupted due to fear from acquiring the infection (45). Moreover, it can maximize the granted benefit from limited resources and physicians by enhancing the efficacy of critical care services and making it possible to expand ICUs with the same number of physicians by allowing off site intensivist to monitor patients in multiple locations simultaneously (49). Consultations from worldwide experts through many freely available applications on the readily available personal mobile phones can enhance healthcare workers knowledge and introduce new skills by teleconferences, e-workshops, and free webinars. Healthcare workers can be remotely trained to enhance their skills.
In King Hussein Cancer Center in Jordan various methods of limiting unnecessary exposure were implemented. Patients were contacted, by phone, by nurse coordinators from the center before scheduled appointments. In these phone calls, patients were asked if they suffered from any symptoms that would suggest a COVID-19 infection. They were also asked if they had been in contact with a confirmed COVID-19 case. Screening tests and vital signs were taken for patient with a high degree of suspicion before being admitted for scheduled procedures. Upgrades were also made to an existing call center to facilitate remote clinics (50).
Mobile Applications in Tracking Possible COVID-19 Patients
LIC have limited resources to allocate to testing a large number of people, so it is important to develop ways to maximize the efficiency of the testing process (Figures 1, 2). Mobile applications that use location to determine the proximity of a person to an affected individual can help in contact tracing, ultimately maximizing the efficiency of testing. These applications, if used by a large enough number of people, along with social distancing measures, could be sufficient in slowing the progress of the pandemic to a manageable rate. Similar measures have been deployed in Mainland China and South Korea with great success (51).
The Use of 3D Printing as a Possible Solution for Limited Equipment Due to Lack of Resources
The shortage in the medical supply chain has triggered us to search for bright solutions that can reshape our future response to persistent challenges. The technology of 3D printing is evolving and has a wide variety of applications. It has the ability to produce anything anywhere and can adapt complex manufacturing instruction in a short time and at a lower cost. During the current pandemic, it was used to manufacture PPE including facemasks, face shields, and goggles. Some universities used 3D printing to create diagnostic tools such as microscopes. In china, 3D printers were used to create quarantine booths (52). Moreover, 3D printing firms are volunteering their expertise and skills to respond to the current crises. Many 3D printing companies such as Stratasys, Carbon, and Shape ways are working rapidly to produce ventilator components, face masks, and medical test equipment. To globally materialize 3D printing service, they have shared free files for a 3D printed add-on hands-free door handles (52). These add-ons allows users to open most modern doors using their elbows to avoid touching door handles (hotspot for microbes) that are subjected to a lot of physical contact, especially in public places such as offices and hospitals (52).
Conclusion
This pandemic has presented a unique challenge to developed and developing countries alike. LIC countries have faced a harder toll due to preexisting challenges in their healthcare systems. Despite this there are many ways to utilize existing infrastructure to help combat the pandemic by utilizing retired healthcare workers, using telemedicine, or taking advantage of cheaper technologies (such as 3D printing) to decrease the burden of the pandemic. Raising public awareness remains of pivotal importance to decrease the pressure of the pandemic on the health care system. Public health measures known to limit viral spread are highly encouraged, these include hand hygiene, cough etiquette and social distancing; as they will reduce the need for limited supplies (10). We also believe that the WHO, as a global health oversight board, should develop comprehensive programs to tackle the different issue facing healthcare systems in LIC. Emergency health funding should be offered to enable health authorities in LIC to purchase appropriate consumables for healthcare workers.
Author Contributions
MA-H: the conception of the idea. YA, HE, ME, MS, and AA-H: literature review. YA, HE, and AA-H: writing the first draft. ME, MS, AA-H, and MA-H: critical review. All authors: final approval. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Woo PC, Huang Y, Lau SK, Yuen KY. Coronavirus genomics and bioinformatics analysis. Viruses. (2010) 2:1804–20. doi: 10.3390/v2081803
2. Lim YX, Ng YL, Tam JP, Liu DX. Human coronaviruses: a review of virus-host interactions. Diseases. (2016) 4:26. doi: 10.3390/diseases4030026
3. Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. (2020) 382:727–33. doi: 10.1056/NEJMoa2001017
4. Inglesby TV. Public health measures and the reproduction number of SARS-CoV-2. JAMA. (2020) 323:2186–7. doi: 10.1001/jama.2020.7878
5. Cucinotta D, Vanelli M. WHO declares COVID-19 a pandemic. Acta Biomed. (2020) 91:157–60. doi: 10.23750/abm.v91i1.9397
6. Miller IF, Becker AD, Grenfell BT, Metcalf CJE. Disease and healthcare burden of COVID-19 in the United States. Nat Med. (2020) 26:1212–17. doi: 10.1038/s41591-020-0952-y
7. Grinshpun SA, Yermakov M, Khodoun M. Autoclave sterilization and ethanol treatment of re-used surgical masks and N95 respirators during COVID-19: impact on their performance and integrity. J Hosp Infect. (2020) 105:608–14. doi: 10.1016/j.jhin.2020.06.030
8. Tirupathi R, Bharathidasan K, Palabindala V, Salim SA, Al-Tawfiq JA. Comprehensive review of mask utility and challenges during the COVID-19 pandemic. Infez Med. (2020) 28(Suppl. 1):57–63.
9. Remuzzi A, Remuzzi G. COVID-19 and Italy: what next? Lancet. (2020) 395:1225–8. doi: 10.1016/S0140-6736(20)30627-9
10. Emanuel EJ, Persad G, Upshur R, Thome B, Parker M, Glickman A, et al. Fair allocation of scarce medical resources in the time of covid-19. N Engl J Med. (2020) 382:2049–55. doi: 10.1056/NEJMsb2005114
11. Kim SW, Lee KS, Kim K, Lee JJ, Kim JY, Daegu Medical Association. A brief telephone severity scoring system and therapeutic living centers solved acute hospital-bed shortage during the COVID-19 outbreak in Daegu, Korea. J Korean Med Sci. (2020) 35:e152. doi: 10.3346/jkms.2020.35.e152
12. Sun T, Wan W, Wu Z, Zhang J, Zhang L. Clinical outcomes and natural history of pediatric brainstem tumors: with 33 cases follow-ups. Neurosurg Rev. (2013) 36:311–9, discussion 319–20. doi: 10.1007/s10143-012-0428-8
13. Turner HC, Hao NV, Yacoub S, Hoang VMT, Clifton DA, Thwaites GE, et al. Achieving affordable critical care in low-income and middle-income countries. BMJ Glob Health. (2019) 4:e001675. doi: 10.1136/bmjgh-2019-001675
14. Bao Y, Sun Y, Meng S, Shi J, Lu L. 2019-nCoV epidemic: address mental health care to empower society. Lancet. (2020) 395:e37–8. doi: 10.1016/S0140-6736(20)30309-3
15. Greenberg N, Docherty M, Gnanapragasam S, Wessely S. Managing mental health challenges faced by healthcare workers during covid-19 pandemic. BMJ. (2020) 368:m1211. doi: 10.1136/bmj.m1211
16. Number of ICU beds insufficient to combat Covid-19 pandemic. Dhaka: Dhaka Tribune (21 March 2020). In reality, Hospitals in Bangladesh have only 1,169 ICU beds (432 govt, 737 private) in total against a population of 161,356,039 people.
17. Mexico's president in no hurry to confront virus outbreak. New York City, NY: AP News (March, 20 2020).
18. Available, online at website: http://government.ru/news/39218 (accessed December 8, 2020).
19. DIVI-Intensivregister Tagesreport 2020-05-19. Deutsche Interdisziplinäre Vereinigung für Intensiv- und Notfallmedizin e.V. 2020-05-19. (2020) Available online at: https://www.divi.de/divi-intensivregister-tagesreport-archiv/divi-intensivregister-tagesreport-2020-05-19/viewdocument/3654 (accessed December 8, 2020).
20. McDonald Brent; Tovar Miguel. As the Coronavirus Approaches, Mexico Looks the Other Way. New York City: The New York Times (March, 25 2020).
21. The Ventilator Problem. (2020). Available online at website: https://meduza.io/en/feature/2020/03/21/the-ventilator-problem (accessed December 8, 2020).
22. There Aren't Enough Ventilators to Cope With the Coronavirus. (2020). Available online at website: https://www.nytimes.com/2020/03/18/business/coronavirus-ventilator-shortage.html (accessed December 8, 2020).
23. World Bank Open Data. (2020). Available online at website: https://data.worldbank.org/) (accessed December 8, 2020).
24. Astor A, Akhtar T, Matallana MA, Muthuswamy V, Olowu FA, Tallo V, et al. Physician migration: views from professionals in Colombia, Nigeria, India, Pakistan and the Philippines. Soc Sci Med. (2005) 61:2492–500. doi: 10.1016/j.socscimed.2005.05.003
25. Hoyler M, Finlayson SR, McClain CD, Meara JG, Hagander L. Shortage of doctors, shortage of data: a review of the global surgery, obstetrics, and anesthesia workforce literature. World J Surg. (2014) 38:269–80. doi: 10.1007/s00268-013-2324-y
26. Mullan F, Frehywot S. Non-physician clinicians in 47 sub-Saharan African countries. Lancet. (2007) 370:2158–63. doi: 10.1016/S0140-6736(07)60785-5
27. Mullan F, Frehywot S, Omaswa F, Buch E, Chen C, Greysen SR, et al. Medical schools in sub-Saharan Africa. Lancet. (2011) 377:1113–21. doi: 10.1016/S0140-6736(10)61961-7
28. Shultz JM, Cooper JL, Baingana F, Oquendo MA, Espinel Z, Althouse BM, et al. The role of fear-related behaviors in the 2013-2016 west Africa Ebola virus disease outbreak. Curr Psychiatry Rep. (2016) 18:104. doi: 10.1007/s11920-016-0741-y
29. Petzold MB, Plag J, Ströhle A. Umgang mit psychischer belastung bei gesundheitsfachkräften im rahmen der covid-19-pandemie [dealing with psychological distress by healthcare professionals during the COVID-19 pandemia]. Nervenarzt. (2020) 91:417–21. doi: 10.1007/s00115-020-00905-0
30. Wu P, Fang Y, Guan Z, Fan B, Kong J, Yao Z, et al. The psychological impact of the SARS epidemic on hospital employees in China: exposure, risk perception, and altruistic acceptance of risk. Can J Psychiatry. (2009) 54:302–11. doi: 10.1177/070674370905400504
31. Krishnamoorthy V, Vavilala MS, Mock CN. The need for ventilators in the developing world: an opportunity to improve care and save lives. J Glob Health. (2014) 4:010303. doi: 10.7189/jogh.04.010303
32. Schmidinger M, Linzmayer L, Becherer A, Fazeny-Doemer B, Fakhrai N, Prayer D, et al. Psychometric- and quality-of-life assessment in long-term glioblastoma survivors. J Neurooncol. (2003) 63:55–61. doi: 10.1023/A:1023740303162
33. Skeete J, Connell K, Ordunez P, DiPette DJ. Approaches to the management of hypertension in resource-limited settings: strategies to overcome the hypertension crisis in the post-COVID Era. Integr Blood Press Control. (2020) 13:125–33. doi: 10.2147/IBPC.S261031
34. Roser M, Ritchie H, Ortiz-Ospina E, Hasell J. “Coronavirus Pandemic (COVID-19)”. (2020) Retrieved from: https://ourworldindata.org/coronavirus-testing (accessed December 02, 2020).
35. The new humanitarian. Zimbabwe's Triple Threat: Coronavirus fs, and an Economy in Meltdown. (2020). Available online at: https://www.thenewhumanitarian.org/news/2020/04/09/zimbabwe-coronavirus-food-economy (accessed May 30, 2020).
36. Arab news. Gaza Runs Out of Coronavirus Tests; Palestinian Health Officials Say. (2020). Available online at: https://www.arabnews.com/node/1655501/middle-east (accessed May 30, 2020).
37. Stupp R, Mason WP, van den Bent MJ, Weller M, Fisher B, Taphoorn MJ, et al. Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med. (2005) 352:987–96. doi: 10.1056/NEJMoa043330
38. Steinbach J, Blaicher HP, Herrlinger U, Wick W, Nägele T, Meyermann R, et al. Surviving glioblastoma for more than 5 years: the patient's perspective. Neurology. (2006) 66:239–42. doi: 10.1212/01.wnl.0000194221.89948.a0
39. Gately L, McLachlan SA, Dowling A, Philip J. Life beyond a diagnosis of glioblastoma: a systematic review of the literature. J Cancer Surviv. (2017) 11:447–52. doi: 10.1007/s11764-017-0602-7
40. Strategies for Optimizing the Supply of N95 Respirators. Atlanta: Centers for Disease Control and Prevention. (2020). Available online at: https://www.cdc.gov/coronavirus/2019-ncov/hcp/respirators-strategy/index.html
41. Giovagnoli AR, Silvani A, Colombo E, Boiardi A. Facets and determinants of quality of life in patients with recurrent high grade glioma. J Neurol Neurosurg Psychiatry. (2005) 76:562–8. doi: 10.1136/jnnp.2004.036186
42. United Nations Development Programme. Available online at: http://hdr.undp.org/en/composite/HDI (accessed May 17, 2020).
43. Cook ADB, Chen CZ. Establishing Humanitarian Lanes During COVID-19. East Asia Forum. Canberra: Australian National University. (2020) Available online at: https://www.eastasiaforum.org/2020/06/30/establishing-humanitarian-lanes-during-covid-19/ (accessed December 16, 2020).
44. Chakrabarti I, Cockburn M, Cozen W, Wang YP, Preston-Martin S. A population-based description of glioblastoma multiforme in Los Angeles County, 1974–1999. Cancer. (2005) 104:2798–806. doi: 10.1002/cncr.21539
45. Noreen K, Umar M, Sabir AA. Opportunities and development of telemedicine in response to COVID-19: experience from public sector medical university. Biomed. (2020) 36:1–4.
46. Lewis T, Synowiec C, Lagomarsino G, Schweitzer J. E-health in low- and middle-income countries: findings from the center for health market innovations. Bull World Health Organ. (2012) 90:332–40. doi: 10.2471/BLT.11.099820
47. Reeves JJ, Hollandsworth HM, Torriani FJ, Taplitz R, Abeles S, Tai-Seale M, et al. Rapid response to COVID-19: health informatics support for outbreak management in an academic health system. J Am Med Inform Assoc. (2020) 27:853–9. doi: 10.1093/jamia/ocaa037
48. WHO Launches COVID-19 Clinical Management Online Training,. (2020). Available online at: http://www.emro.who.int/jor/jordan-news/who-launches-covid-19-clinical-management-online-training.html (accessed December 8, 2020).
49. Breslow MJ. ICU telemedicine. Organization and communication. Crit Care Clin. (2000) 16:707–22, x–xi. doi: 10.1016/S0749-0704(05)70142-1
50. Al-Tabba' A, Al-Hussaini M, Mansour R, Sultan H, Abdel-Razeq H, Mansour A. Ethical considerations for treating cancer patients during the SARS-CoV-2 virus crisis: to treat or not to treat? A literature review and perspective from a cancer center in low-middle income country. Front Med. (2020) 7:561168. doi: 10.3389/fmed.2020.561168
51. Ferretti L, Wymant C, Kendall M, Zhao L, Nurtay A, Abeler-Dörner L, et al. Quantifying SARS-CoV-2 transmission suggests epidemic control with digital contact tracing. Science. (2020) 368:eabb6936. doi: 10.1126/science.abb6936
Keywords: COVID-19, resources, low-income countries, challenges, solutions
Citation: Alhalaseh YN, Elshabrawy HA, Erashdi M, Shahait M, Abu-Humdan AM and Al-Hussaini M (2021) Allocation of the “Already” Limited Medical Resources Amid the COVID-19 Pandemic, an Iterative Ethical Encounter Including Suggested Solutions From a Real Life Encounter. Front. Med. 7:616277. doi: 10.3389/fmed.2020.616277
Received: 11 October 2020; Accepted: 11 December 2020;
Published: 14 January 2021.
Edited by:
Hilde Stevens, Université Libre de Bruxelles, BelgiumReviewed by:
Domenico Criscuolo, Italian Society of Pharmaceutical Medicine, ItalyFrits Lekkerkerker, Consultant, Amsterdam, Netherlands
Copyright © 2021 Alhalaseh, Elshabrawy, Erashdi, Shahait, Abu-Humdan and Al-Hussaini. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Maysa Al-Hussaini, bWh1c3NhaW5pQGtoY2Muam8=
 Yazan Nedal Alhalaseh
Yazan Nedal Alhalaseh Hatem A. Elshabrawy
Hatem A. Elshabrawy Madiha Erashdi
Madiha Erashdi Mohammed Shahait4
Mohammed Shahait4 Abdulrahman Mohammad Abu-Humdan
Abdulrahman Mohammad Abu-Humdan Maysa Al-Hussaini
Maysa Al-Hussaini