
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Med., 16 September 2020
Sec. Rheumatology
Volume 7 - 2020 | https://doi.org/10.3389/fmed.2020.524628
 Byeong-Gu Gang1
Byeong-Gu Gang1 Joon-Shik Shin1
Joon-Shik Shin1 Jinho Lee1
Jinho Lee1 Yoon Jae Lee2
Yoon Jae Lee2 Hyun-Woo Cho3
Hyun-Woo Cho3 Me-riong Kim2
Me-riong Kim2 Kyungwon Kang2
Kyungwon Kang2 Wonil Koh1
Wonil Koh1 Eun-Jung Kim4
Eun-Jung Kim4 Yeoncheol Park5
Yeoncheol Park5 Dongwoo Nam6
Dongwoo Nam6 In-Hyuk Ha2*
In-Hyuk Ha2*Objectives: The present study was undertaken to investigate the relationship between acupuncture therapy and surgery rate.
Design: Matched, retrospective cohort study.
Materials and Methods: From nationwide health insurance data (2002–2013 cohort data published by the National Health Insurance Service of Korea), patients with new cases of knee osteoarthritis that occurred between January 1, 2004 and December 31, 2010 were analyzed. Patients were divided into an acupuncture group (AG) and a control group (CG), based on records of acupuncture therapy. Propensity scores were calculated by using gender, age, income level, and Charlson comorbidity index (CCI), with the groups matched at a ratio of 1:3 (AG:CG). The final analysis period was 2 years after the first acupuncture therapy for AG and 2 years after initial diagnosis for CG; surgery rates were compared between the two groups. Stratified analyses were performed based on age, gender, and income level; sensitivity analyses were performed based on the frequency and duration of acupuncture therapy.
Results: Propensity score-matched AG and CG included 8,605 and 25,815 subjects, respectively. Post-matching surgery rates were 0.26 and 0.93% in AG and CG, respectively. For all age groups, AG showed a lower surgery rate than CG. In the analysis based on gender, the female group showed a significantly lower hazard ratio of 0.225. In analysis based on income level, the results of the entire group were significant, with the lower income group showing the lowest hazard ratio. In sensitivity analyses, AG tended to show a lower surgery rate than CG.
Conclusions: The present study demonstrated that acupuncture therapy is associated with a low rate of surgery for knee osteoarthritis. Additional studies are needed to support this conclusion.
Osteoarthritis is a degenerative disease associated with degeneration of the ligament and cartilage surrounding the joint; it exhibits gradual infiltration, loss of cartilage, structural change in the bone below the cartilage, and osteosclerosis, accompanied by bony spurs. Patients with knee osteoarthritis present with various symptoms, such as pain, muscle atrophy, stiffness, and limited range of motion (1). Pain is a major symptom associated with excessive joint use (2). According to the 2010 Global Burden Disease Study, the total social burden of hip and knee osteoarthritis was 11th in terms of years lived with disability and 38th in terms of disability-adjusted life years (3, 4).
Key treatment modalities recommended for patients with knee osteoarthritis in most international guidelines include patient education, exercise, and diet (5). When necessary, biomechanical methods involving a brace or insoles, or pharmacological approaches may be used, depending on the characteristics and preferences of individual patients (6, 7). Total knee replacement (TKR) is an effective treatment for patients with late-stage knee osteoarthritis (8), with an increasing number of TKR surgeries each year (9). However, even after surgery, ~20% of patients continue to experience persistent pain (10), in addition to persistent limitations in range of motion (11). Moreover, there have been reports of failed surgery involving sepsis, discontinuous extension, stiffness, femoral-tibial instability, patellar tracking, aseptic loosening, osteolysis, nearby fracture, and breakage of components (12).
Non-surgical treatments are typically administered to patients with early- and mid-stage knee osteoarthritis; among such methods, physical and acupuncture therapies are safe and effective (13). In particular, acupuncture therapy has a definitive effect on improving symptoms and movement (14, 15). In an overview of systematic reviews published in 2019, which examined the effects of acupuncture therapy on chronic knee pain due to osteoarthritis, acupuncture therapy was reported to demonstrate more total effective rate, short-term effective rate and less adverse reactions than western medicine of high quality outcomes (16).
Although the effects of acupuncture therapy on functional improvement and pain relief have been identified in cases of knee osteoarthritis, there have been no studies regarding the relationship between acupuncture therapy and knee surgery. Accordingly, the present study aimed to retrospectively review 2002–2013 Korean cohort data to investigate the relationship between acupuncture therapy and surgery rate for knee osteoarthritis.
The present study used 2002–2013 cohort data published in 2014 by the National Health Insurance Service of Korea. These data comprise random sampling of 1,025,340 people, representing ~2.2% of the total Korean population, for general research on the health status and health care utilization of all Koreans. The database included all medical claims filed from January 2002 to December 2010. In this study, diseases were classified according to the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM). For traditional Korean medicine (TKM), the Korean Standard Classification of Diseases (TKM), up to the end of 2009, was used. The present study was reviewed and approved by the Institutional Review Board of Jaseng Hospital of Korean Medicine (JASENG 2018-01-007).
Using the period from 2002 to 2003 as the wash-out period, the present study examined new cases of knee osteoarthritis that occurred between January 1, 2004 and December 31, 2010. M17* was selected as the diagnosis representing knee osteoarthritis, based on review of existing studies and consensus among the researchers (17–19). For TKM, J18*, J19*, and H13.13 were used for cases up to December 31, 2009, in accordance with the revised TKM diagnoses; cases from January 1, 2010 and beyond used the standard medical diagnoses. Patients with the main or sub diagnosis mentioned above were considered new patients with knee osteoarthritis for each department; cases involving cross-treatment were excluded. Among patients who were identified according to these conditions, those with no record of acupuncture therapy after the initial diagnosis were selected as members of the control group (CG). Of the patients with records of acupuncture therapy, patients who were determined to show clinical significance, as agreed upon by the researchers, were considered candidates for the acupuncture group (AG). Subsequently, AG was established for patients who received at least 2 rounds of acupuncture therapy within 6 weeks after the initial diagnosis of knee osteoarthritis (Figure 1).
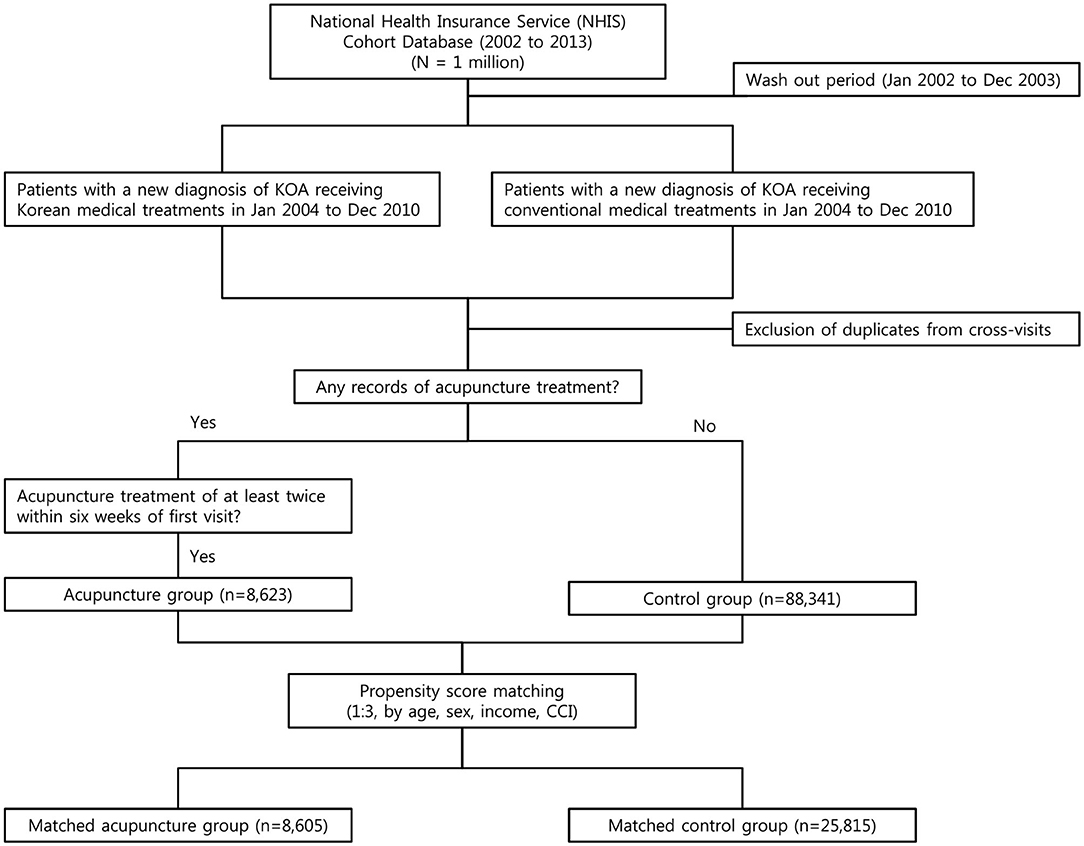
Figure 1. Flowchart of the study design. According to the propensity score matching (1:3, by age, sex, income, CCI), a total of 8,605 patients were included in the acupuncture group, and 25,815 patients were included in the control group.
Status of knee surgery was used as the factor for final analysis. For the definition of surgery, N0722* (diagnostic condition), N2072*, N2077*, N2712*, N2717*, N0691*, N0692*, N0694*, N0702* (diagnostic condition), N0707* (diagnostic condition), E7500 (diagnostic condition), N0821*, N0822*, N0826*, and N0827* were selected based on reviews of existing studies and consensus among the researchers (20, 21) The final analysis period was set to 2 years after the first acupuncture therapy for AG and 2 years after the initial diagnosis for CG. This was because the use of 2 years after the initial diagnosis for both groups may create a survival bias favorable to AG. Surgery rates that satisfied the aforementioned conditions were compared between the two groups.
To match the two groups, the present study used propensity score matching, generally used to eliminate confounding bias when comparing two non-randomized groups with different treatments. The present study calculated propensity scores based on gender, age, income level, and Charlson comorbidity index (CCI); considering the size of each group, the groups were matched at a ratio of 1:3 (AG:CG) (22). Data from subjects in each group who were not matched were discarded. Survival analysis was conducted for the surgery. Survival probability of acupuncture and control groups is presented as a Kaplan–Meier curve, and the difference between the two groups was tested using the log-rank test. Additionally, the number of patients at risk at each time point is presented. Cox proportional hazards regressions were used to estimate hazard ratios (HRs) and 95% confidence intervals (CI) for the relative risk of acquired incidence rate. The proportional hazards assumption was tested using Schoenfeld's global test. All analyses were performed using SAS statistical software (Version 9.3 for Windows; SAS Institute, Inc., Cary, NC, USA). Stratified analyses based on age, gender, and income level were performed to analyze the patterns by strata. Moreover, sensitivity analysis was performed to examine changes in results based on changes in the frequency and duration of acupuncture therapy specified in the study.
The numbers of unmatched subjects in AG and CG were 8,623 and 88,341, respectively. In the analysis by age, AG had the highest number of subjects (n = 3,035, 35.20%) in the 70–79 years' age group, while CG had the highest number of subjects (n = 23,616, 26.73%) in the 60–69 years' age group. With respect to gender, both groups had a higher percentage of females, with AG (n = 6,430, 74.57%) showing a higher percentage than CG (n = 53,188, 60.21%) (Table 1). The numbers of propensity score-matched subjects in the AG and CG groups were 8,605 and 25,815, respectively. For both AG and CG, the highest percentages of subjects belonged to the 70–79 years' age group, with 3,017 (35.06%) in AG and 9,000 (34.86%) in CG (Table 2). The median follow-up time of both groups was 730 days. The median duration of time to surgery was 144 days.
In the overall analysis, AG and CG showed pre-matching surgery rates of 0.26 and 0.76% and post-matching surgery rates of 0.26 and 0.93%, respectively. AG and CG also showed HRs of 0.301 (0.197–0.461, 95% CI) and 0.273 (0.177–0.423, 95% CI), respectively (Table 3). The proportional hazards assumption was satisfied (Shoenfeld's global test, p = 0.307).
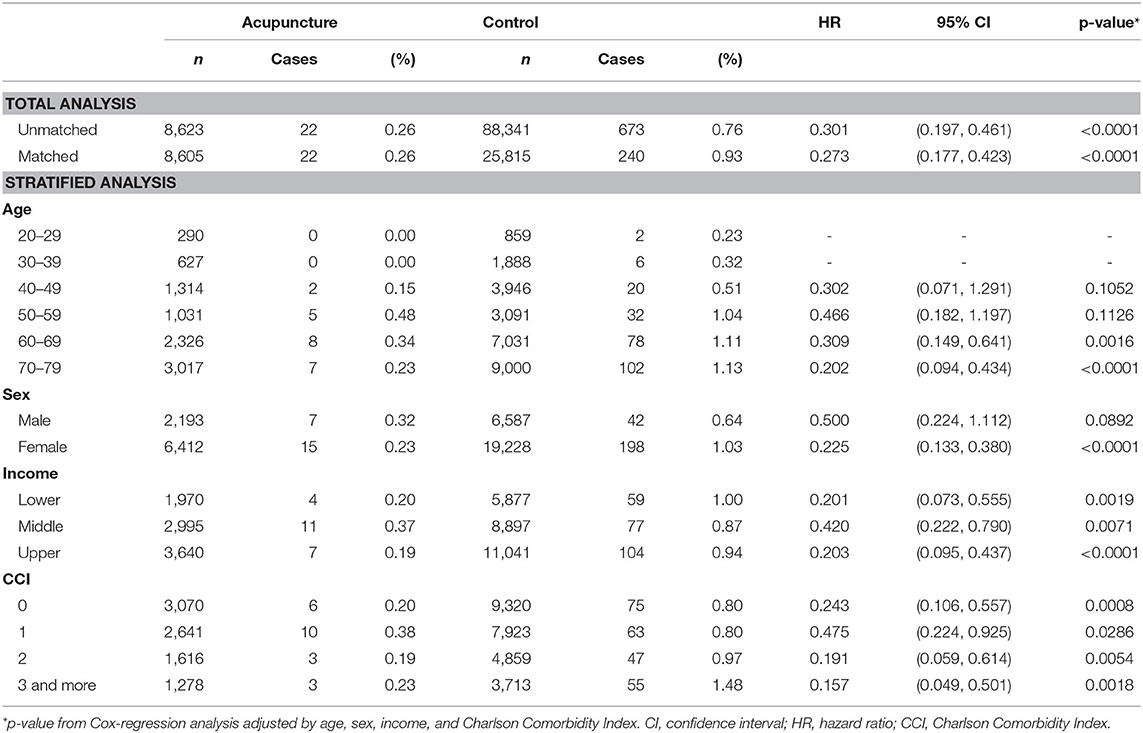
Table 3. Total and stratified analyses of the knee surgery rates in the acupuncture and control groups.
Stratified analyses were performed based on age, gender, and income level. In the analysis by age, the 70–79 years' age group showed the lowest HR of 0.202 (0.094–0.434, 95% CI). Among all ages, AG showed a lower surgery rate than CG, with an HR <1. However, the results were statistically significant only in the 60–79 years' age groups. In the 20–39 years' age groups, statistical comparisons could not be made because there were no cases that required surgery. In the 40–59 years' age group, HR was <1, but the results were not statistically significant. In the analysis by gender, males and females showed HRs of 0.5 (0.224–1.112, 95% CI) and 0.225 (0.133–0.380, 95% CI), respectively; the results were statistically significant only in females. In the analysis by income level, results for all groups were significant, but the lower income group showed the lowest HR, 0.201 (0.073–0.554, 95% CI) (Table 3, Figure 2).
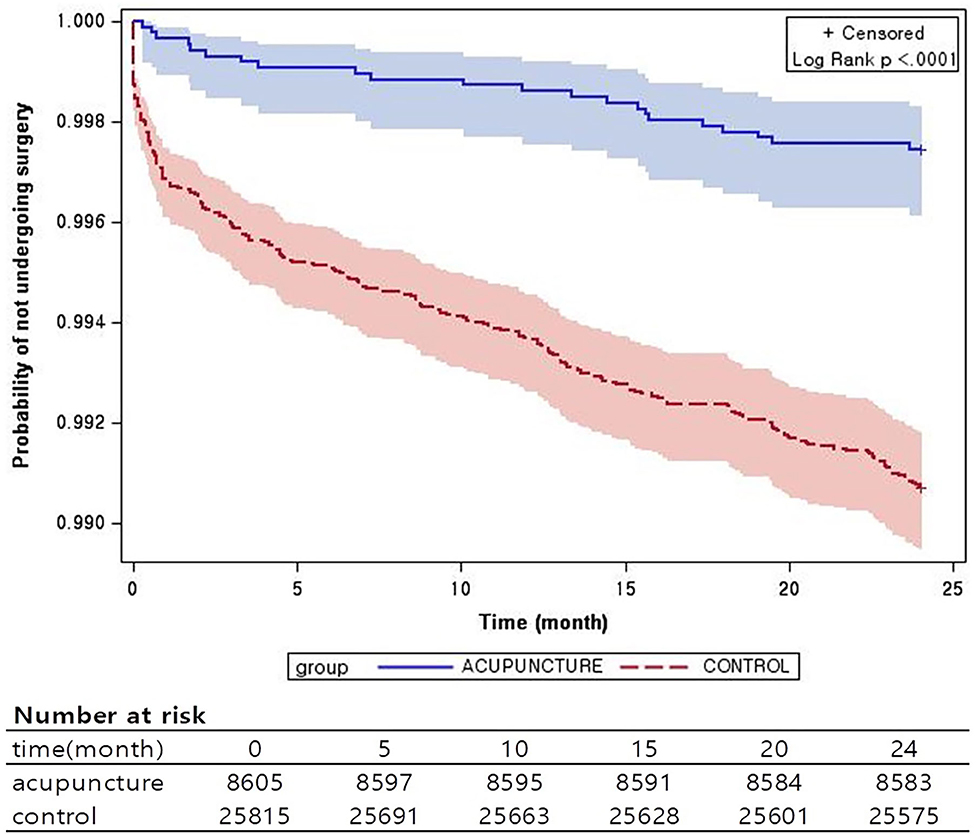
Figure 2. Kaplan–Meier survival estimates of knee surgery incidence. Probability of knee surgery with and without acupuncture treatment.
The results of sensitivity analyses based on frequency and duration of acupuncture therapy are also presented. In all analyses, AG tended to show a lower surgery rate than CG, with an HR <1 (Table 4).
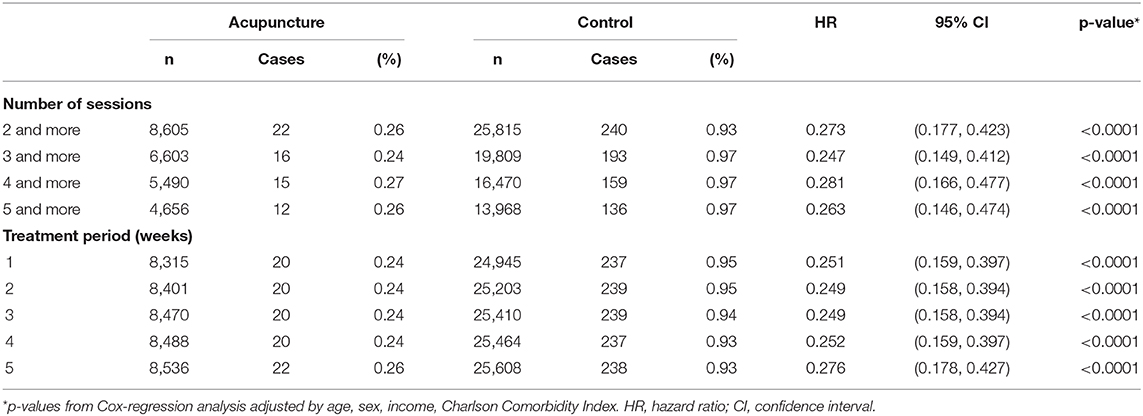
Table 4. Sensitivity analyses on knee surgery, according to the number of acupuncture sessions and the treatment period, in acupuncture and control groups.
The present study examined the association of acupuncture therapy with surgery rate in patients with knee osteoarthritis. In pre- and post-matching cohorts, AG showed a lower surgery rate than CG, with an HR <1. Analysis of surgery rates and HR values between the two groups showed that the results were significant in the age groups of 60–69 and 70–79 years, revealing appreciably lower HRs in older subjects. In the analysis by gender, females showed appreciably lower HRs. In sensitivity analyses based on frequency and duration of acupuncture therapy, the tendency of AG to have a lower surgery rate than CG was maintained, with HR <1.
In the pre-matching cohorts, primarily older age groups, females, and upper income level groups showed higher percentages; these patterns were maintained after matching. This may reflect differences in preferences based on age, gender, and income level with respect to TKM, including acupuncture therapy. In a study by Woo et al. that examined TKM preferences in the Korean population (23), acupuncture therapy was most well-known among users of TKM; most users of TKM, regardless of gender, age, education level, and TKM dependence, indicated that they had received acupuncture therapy, with preference for TKM especially high among the elderly. In addition, a 2006 study by Ock et al. (24) reported that preference for TKM was higher among females in Korea, with a large difference in utilization between males (69.3%) and females (80.3%). Such findings are supported by a 2008 study in Korea (25) and various foreign studies (26–28). In addition, a positive correlation was found between income level and use of CAM (29).
The number of subjects in the propensity score-matched groups tended to increase in age groups 50 years or older for both AG and CG, which may be because knee osteoarthritis is generally a degenerative joint disease (30). In both Tables 1, 2, the percentages of females were higher than those of males, which supported previous meta-analyses (31) which mentioned gender differences in the incidence rate of osteoarthritis, with a higher risk among females (32).
The major finding in the present study is that AG tended to show lower surgery rate than CG in the overall analysis and stratified analyses. However, because of no existing cases or small sample size (n), statistical significance could be found only in some groups.
The analysis results showed that pre- and post-matching surgery rates in CG increased from 0.76 to 0.93%, respectively, whereas HRs decreased from 0.301 to 0.273, respectively. This indicated that when the influences of other influencing factors of surgery rate were eliminated by propensity score matching, differences in surgery rate, in comparison with AG, were larger with statistically significant differences.
In the analysis based on age, the number of surgery cases among the 20–39 years aged AG group was zero. This may be because when AG patients were defined in the present study, disease codes corresponding to injuries were deemed unsuitable and excluded from patients with knee osteoarthritis. In AG, 50–59 years' age group showed the highest surgery rate, but the results were not statistically significant because the absolute number of patients was too small. The most noteworthy results were found in the 70–79 years' age group. In this age group, AG showed a relatively lower surgery rate than the other age groups (0.23%) and CG showed the highest surgery rate, while its HR was lowest (1.13%, 0.202, 0.094–0.434, 95% CI, p < 0.0001). This may be due to aforementioned preferences for TKM among the elderly. Moreover, older age groups tend to choose non-surgical treatment over surgery due to concerns regarding possible complications; thus, it is difficult to conclude that the findings in the present study solely reflected the effects of acupuncture therapy. A study by Belmar et al. (33) suggested that it may be more desirable to delay TKR in younger age groups, due to the possibility of re-operation, bone loosening, and pain due to over-use. Moreover, it might be better for older patients to delay or avoid surgery because there may be an increased risk of postoperative complications due to underlying diseases. Indeed, patients aged <50 years underwent surgery at a much lower rate than patients aged 60–69 years; patients aged ≥80 years underwent surgery at a lower rate than those aged 50–59 and 70–79 years.
In the analysis based on gender, AG showed a lower surgery rate than CG for both males and females. Surgery rates of females were statistically significant, with AG and CG showing 0.23% and 1.03%, respectively; the HR was 0.225 (0.133–0.380, 95% CI). This may be attributed to a greater number of female patients than male patients, as well as aforementioned gender differences in disease incidence. In the analysis based on income level, the results of the entire group were statistically significant.
To test the robustness of the analyses performed in the present study, sensitivity analyses based on frequency and duration of acupuncture therapy were performed. The results based on frequency and duration showed that surgery rate was higher in CG than in AG.
The noteworthy result in the analysis based on changes in frequency of acupuncture therapy was the difference between the ≥2 and ≥3 times groups. AG did not show a consistent tendency in surgery rate between the groups, whereas CG showed a noticeably higher surgery rate in the ≥3 times group than in the ≥2 times group; that rate was maintained as the frequency of acupuncture therapy increased. Moreover, the ≥3 times group showed the lowest HR, 0.247 (0.149–0.412, 95% CI). These results demonstrated that receiving acupuncture therapy ≥3 times within 6 weeks after the initial diagnosis was more closely associated with low surgery rates than receiving acupuncture therapy ≥2 times.
With respect to surgery rates based on duration of acupuncture therapy, AG showed a decrease in surgery rate from 0.26 to 0.24% when the duration decreased from 6 weeks to 1 week, while CG showed an increase from 0.93 to 0.95% for the same duration. Moreover, HRs showed a decreasing tendency. These results demonstrated that short-term intensive treatment after the initial diagnosis is associated with a low surgery rate.
The findings in the present study demonstrated that acupuncture therapy may be associated with a low surgery rate for knee osteoarthritis. As mentioned above, acupuncture therapy may show functional improvement and relieve pain in patients with knee osteoarthritis, which can reduce the need for surgery. Previous literature (34–37) mentioned that endogenous chemicals secreted during acupuncture therapy, such as enkephalin, dynorphin, and gamma aminobutyric acid, have a distinct effect on patients with chronic knee pain. However, the long-term pain control effect could not be verified; others have noted that the placebo effect may influence clinical outcomes (38). In other studies, compared with sham or no-treatment groups, acupuncture therapy did not show noticeable effects on functional recovery or pain relief in patients with chronic knee pain; thus, any clinical benefit may have been due to expectations by the patients. Indeed, patients who had positive expectations regarding acupuncture therapy showed better results than those who did not (39, 40). Consequently, the effect of acupuncture therapy on chronic knee pain remains controversial due to the limited number of studies and heterogeneity among studies (41–46). Moreover, currently suggested clinical guidelines have a contradictory view regarding the use of acupuncture therapy for knee osteoarthritis (6, 7, 47–49) Therefore, additional studies are needed to reaffirm the conclusions reached in the present study.
The present study used national cohort data, which had a large sample size that can represent the entire national population. Because the data were based on actual insurance claims, there is the advantage of no follow-up failure or loss, unlike other studies that require additional follow-up observations. While many studies have examined the association between acupuncture therapy and improvement in symptoms of knee osteoarthritis, there have been no studies regarding the correlation between acupuncture therapy and surgery rate for knee osteoarthritis. Moreover, the analyses in the present study were more significant due to additional sensitivity analyses regarding frequency and duration of acupuncture therapy.
The present study had some limitations. First, only surgery rate was used as the outcome for determining the association between acupuncture therapy and surgery. In doing so, the actual pre- and postoperative conditions of the patients could not be determined; thus, whether acupuncture therapy or surgery were helpful to patients could not be verified. Moreover, because new cases were defined relative to the date of initial diagnosis, there is a lack of information regarding whether the clinical conditions of the patients at the time required immediate surgery; whether the disease was in early stage; or what disease stage was present, based on radiologic findings. This suggests that the incidence of surgery may be influenced more by existing clinical conditions, compared with acupuncture therapy. Furthermore, the cohort data used in the present study did not consider items not covered under the Korean national health insurance system. Therefore, if the patient had received other treatments not covered by insurance, along with acupuncture therapy, the influence of such treatments could not be assessed. In addition, acupuncture therapy used in the present study was based on the curriculum used in traditional Korean medical colleges in Korea. Therefore, there may be differences with regard to acupuncture therapy used in other countries; differences may exist when applying these findings in other countries. Osteoarthritis is an age-related disease, but patients in their 20s and 30s were included in the analysis because the entire adult was subject to analysis. Although stratified analysis is presented by age, this limitation may weaken the meaning of the present results. Despite efforts to reduce selection bias through propensity matching, the entire health condition of the patient may not have been reflected because only the data in the claim data were checked. There may be concerns about the selection bias. Lastly, the number of patients in AG who underwent surgery was low; as a result, statistical significance could not be measured in some cases.
Knee replacement surgery is gradually becoming a more common treatment modality (8). This poses a significant economic burden in most health care systems, comprising $10.4 billion in the United States in 2008 (50). For this period, over 650,000 cases of TKR were performed in the US; between 2002 and 2005, a total of 103,601 cases of TKR were performed in Korea (51). However, after surgery, ~20% of the patients are known to suffer from persistent pain (52–54); some may require re-operation due to aseptic loosening, wear and tear of structures due to time and activities, and infection. Moreover, such adverse events may occur not only immediately after surgery, but at any time (55–58). Therefore, if an appropriate non-surgical treatment can be administered, postoperative pain and discomfort can be reduced, while reducing the economic burden associated with surgery within the overall health care system.
The findings in the present study demonstrated that intervention by acupuncture therapy is associated with a low surgery rate in Korean patients with knee osteoarthritis. With the growing elderly population, the number of patients with knee osteoarthritis and the associated social burden are expected to increase. Therefore, strategies that can help alleviate the social and economic burdens of surgery, including TKR, are important for public health care policy makers; the findings in the present study may be helpful in that regard.
The present study analyzed the NHIS-NSC database, licensed by the Korean NHIS. Data are available from Korean NHIS upon submission of an appropriate study design.
Due to the retrospective nature of this study, which utilized data with de-identified personal information, it was granted an exemption by the Institutional Review Board of Jaseng Hospital of Korean Medicine in Seoul, Korea (JASENG 2018-01-007). Informed consents process was waived by Institutional Review Board because the de-identified data was analyzed.
B-GG, YJL, M-rK, WK, and I-HH conceptualized and designed the study. J-SS, JL, KK, E-JK, YP, and DN acquired and analyzed the data. B-GG, YJL, KK, WK, and I-HH interpreted the results. B-GG, JL, YJL, M-rK, KK, and WK drafted the original article. J-SS, H-WC, E-JK, YP, DN, and I-HH critically revised the draft. All authors have read and approved of the final version.
This research was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (Grant No. HI17C0840).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
1. Igawa T, Katsuhira J. Biomechanical analysis of stair descent in patients with knee osteoarthritis. J Phys Ther Sci. (2014) 26:629–31. doi: 10.1589/jpts.26.629
2. Al-Johani AH, Kachanathu SJ, Hafez AR, Al-Ahaideb A, Algarni AD, Alroumi AM, et al. Comparative study of hamstring and quadriceps strengthening treatments in the management of knee osteoarthritis. J Phys Ther Sci. (2014) 26:817–20. doi: 10.1589/jpts.26.817
3. Murray CJ, Vos T, Lozano R, Naghavi M, Flaxman AD, Michaud C, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the global burden of disease study 2010. Lancet. (2012) 380:2197–223. doi: 10.1016/S0140-6736(12)61690-0
4. Vos T, Flaxman AD, Naghavi M, Lozano R, Michaud C, Ezzati M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the global burden of disease study 2010. Lancet. (2012) 380:2163–96. doi: 10.1016/S0140-6736(12)61729-2
5. Nelson AE, Allen KD, Golightly YM, Goode AP, Jordan JM. A systematic review of recommendations and guidelines for the management of osteoarthritis: the chronic osteoarthritis management initiative of the US bone and joint initiative. Semin Arthritis Rheum. (2014) 43:701–12. doi: 10.1016/j.semarthrit.2013.11.012
6. McAlindon TE, Bannuru RR, Sullivan M, Arden NK, Berenbaum F, Bierma-Zeinstra SM, et al. OARSI guidelines for the non-surgical management of knee osteoarthritis. Osteoarthr Cartilage. (2014) 22:363–88. doi: 10.1016/j.joca.2014.01.003
7. Fernandes L, Hagen KB, Bijlsma JW, Andreassen O, Christensen P, Conaghan PG, et al. EULAR recommendations for the non-pharmacological core management of hip and knee osteoarthritis. Ann Rheum Dis. (2013) 72:1125–35. doi: 10.1136/annrheumdis-2012-202745
8. Carr AJ, Robertsson O, Graves S, Price AJ, Arden NK, Judge A, et al. Knee replacement. Lancet. (2012) 379:1331–40. doi: 10.1016/S0140-6736(11)60752-6
9. Singh JA, Vessely MB, Harmsen WS, Schleck CD, Melton III LJ, Kurland RL, et al. A population-based study of trends in the use of total hip and total knee arthroplasty, 1969-2008. Mayo Clinic Proc. (2010) 85:898–904. doi: 10.4065/mcp.2010.0115
10. Beswick AD, Wylde V, Gooberman-Hill R, Blom A, Dieppe P. What proportion of patients report long-term pain after total hip or knee replacement for osteoarthritis? A systematic review of prospective studies in unselected patients. BMJ Open. (2012) 2:e000435. doi: 10.1136/bmjopen-2011-000435
11. Woolhead G, Donovan J, Dieppe P. Outcomes of total knee replacement: a qualitative study. Rheumatology. (2005) 44:1032–7. doi: 10.1093/rheumatology/keh674
12. Vince K. The problem total knee replacement: systematic, comprehensive and efficient evaluation. Bone Joint J. (2014) 96:105–11. doi: 10.1302/0301-620X.96B11.34531
13. Zhang Y, Bao F, Wang Y, Wu Z. Influence of acupuncture in treatment of knee osteoarthritis and cartilage repairing. Am J Transl Res. (2016) 8:3995–40002.
14. Plaster R, Vieira WB, Alencar FAD, Nakano EY, Liebano RE. Immediate effects of electroacupuncture and manual acupuncture on pain, mobility and muscle strength in patients with knee osteoarthritis: a randomised controlled trial. Acupunct Med. (2014) 32:236–41. doi: 10.1136/acupmed-2013-010489
15. Manyanga T, Froese M, Zarychanski R, Abou-Setta A, Friesen C, Tennenhouse M, et al. Pain management with acupuncture in osteoarthritis: a systematic review and meta-analysis. BMC Complement Altern Med. (2014) 14:312. doi: 10.1186/1472-6882-14-312
16. Li J, Li YX, Luo LJ, Ye J, Zhong DL, Xiao QW, et al. The effectiveness ans safety of acupuncture for knee osteoarthritis: an overview of systematic reviews. Medicine. (2019) 98:e16301. doi: 10.1097/MD.0000000000016301
17. Bergkvist D, Dahlberg LE, Neuman P, Englund M. Knee arthroscopies: who gets them, what does the radiologist report, and what does the surgeon find? An evaluation from southern Sweden. Acta Orthop. (2016) 87:12–6. doi: 10.3109/17453674.2015.1055179
18. Prieto-Alhambra D, Judge A, Javaid MK, Cooper C, Diez-Perez A, Arden NK, et al. Incidence and risk factors for clinically diagnosed knee, hip and hand osteoarthritis: influences of age, gender and osteoarthritis affecting other joints. Ann Rheum Dis. (2014) 73:1659–64. doi: 10.1136/annrheumdis-2013-203355
19. Hubertsson J, Petersson IF, Thorstensson CA, Englund M. Risk of sick leave and disability pension in working-age women and men with knee osteoarthritis. Ann Rheum Dis. (2013) 72:401–5. doi: 10.1136/annrheumdis-2012-201472
20. Buchbinder R, Richards B, Harris I. Knee osteoarthritis and role for surgical intervention: lessons learned from randomized clinical trials and population-based cohorts. Curr Opin Rheumatol. (2014) 26:138–44. doi: 10.1097/BOR.0000000000000022
21. Koh YG Jo SB Kwon OR Suh DS Lee SW Park SH . Mesenchymal stem cell injections improve symptoms of knee osteoarthritis. Arthroscopy. (2013) 29:748–55. doi: 10.1016/j.arthro.2012.11.017
22. Randolph JJ, Kristina F, Austin Kureethara M, Balloun JL. A step-byStep guide to propensity score matching in R. Pract Assess Res Evaluation. (2014) 19:18. doi: 10.7275/n3pv-tx27
23. Woo JM, Park EJ, Lee M, Ahn M, Kwon S, Koo KH. Changes in attitudes toward and patterns in traditional Korean medicine among the general population in South Korea: a comparison between 2008 and 2011. BMC Complement Altern Med. (2014) 14:436. doi: 10.1186/1472-6882-14-436
24. Ock SM, Choi JY, Cha YS, Lee J, Chun MS, Huh CH, et al. The use of complementary and alternative medicine in a general population in South Korea: results from a national survey in 2006. J Korean Med Sci. (2009) 24:1–6. doi: 10.3346/jkms.2009.24.1.1
25. Shin HK, Jeong SJ, Huang DS, Kang BK, Lee MS. Usage patterns and adverse experiences in traditional Korean medicine: results of a survey in South Korea. BMC Complement Altern Med. (2013) 13:340. doi: 10.1186/1472-6882-13-340
26. Upchurch DM, Chyu L. Use of complementary and alternative medicine among American women. Womens Health Issues. (2005) 15:5–13. doi: 10.1016/j.whi.2004.08.010
27. Upchurch DM, Chyu L, Greendale GA, Utts J, Bair YA, Zhang G, et al. Complementary and alternative medicine use among American women: findings from the National health interview survey, 2002. J Womens Health. (2007) 16:102–13. doi: 10.1089/jwh.2006.M074
28. Fugh-Berman A, Kronenberg F. Complementary and alternative medicine (CAM) in reproductive-age women: a review of randomized controlled trials. Reprod Toxicol. (2003) 17:137–52. doi: 10.1016/S0890-6238(02)00128-4
29. Metcalfe A, Williams J, McChesney J, Patten SB, Jetté N. Use of complementary and alternative medicine by those with a chronic disease and the general population-results of a national population based survey. BMC Complement Altern Med. (2010) 10:58. doi: 10.1186/1472-6882-10-58
30. Bonnet C, Walsh D. Osteoarthritis, angiogenesis and inflammation. Rheumatology. (2005) 44:7–16. doi: 10.1093/rheumatology/keh344
31. Srikanth VK, Fryer JL, Zhai G, Winzenberg TM, Hosmer D, Jones G. A meta-analysis of sex differences prevalence, incidence and severity of osteoarthritis. Osteoarthr Cartilage. (2005) 13:769–81. doi: 10.1016/j.joca.2005.04.014
32. Chaisson C, Zhang Y, McAlindon T, Hannan MT, Aliabadi P, Naimark A, et al. Radiographic hand osteoarthritis: incidence, patterns, and influence of pre-existing disease in a population based sample. J Rheumatol. (1997) 24:1337–43.
33. Belmar CJ, Barth P, Lonner JH, Lotke PA. Total knee arthroplasty in patients 90 years of age and older. J Arthroplasty. (1999) 14:911–4. doi: 10.1016/S0883-5403(99)90002-5
34. Pomeranz B, Berman B. Scientific basis of acupuncture. in Basics of Acupuncture. Berlin, Heidelberg: Springer (2003). p. 7–86. doi: 10.1007/978-3-642-18988-3_2
35. Cho W. Acupuncture and Moxibustion as an Evidence-based Therapy for Cancer. William C-S. editor. New York, NY: Springer Science & Business Media (2012). doi: 10.1007/978-94-007-4833-0
36. Xia Y, Ding G, Wu G-C. Current Research in Acupuncture. New York, NY: Springer Science & Business Media. (2012). doi: 10.1007/978-1-4614-3357-6
37. Ren Z. World Century Compendium To TCM-Volume 6: Introduction To Acupuncture And Moxibustion. Hackensack, NJ: World Scientific (2013). doi: 10.1142/u004-vol6
38. Hinman RS, McCrory P, Pirotta M, Relf I, Forbes A, Crossley KM, et al. Acupuncture for chronic knee pain: a randomized clinical trial. JAMA. (2014) 312:1313–22. doi: 10.1001/jama.2014.12660
39. Lin X, Huang K, Zhu G, Huang Z, Qin A, Fan S. The effects of acupuncture on chronic knee pain 346 due to osteoarthritis: a meta-analysis. J Bone Joint Surg Am. (2016) 98:1578–85. doi: 10.2106/JBJS.15.00620
40. Chen LX, Mao JJ, Fernandes S, Galantino ML, Guo W, LaRiccia P, et al. Integrating acupuncture with exercise-based physical therapy for knee osteoarthritis: a randomized controlled trial. J Clin Rheumatol. (2013) 19:308. doi: 10.1097/RHU.0b013e3182a21848
41. White A, Foster NE, Cummings M, Barlas P. Acupuncture treatment for chronic knee pain: a systematic review. Rheumatology. (2007) 46:384–90. doi: 10.1093/rheumatology/kel413
42. Manheimer E, Linde K, Lao L, Bouter LM, Berman BM. Meta-analysis: acupuncture for osteoarthritis of the knee. Ann Int Med. (2007) 146:868–77. doi: 10.7326/0003-4819-146-12-200706190-00008
43. Cao L, Zhang XL, Gao YS, Jiang Y. Needle acupuncture for osteoarthritis of the knee. A systematic review and updated meta-analysis. Saudi Med J. (2012) 33:526–32.
44. Ezzo J, Hadhazy V, Birch S, Lao L, Kaplan G, Hochberg M, et al. Acupuncture for osteoarthritis of the knee: a systematic review. Arthritis Rheum. (2001) 44:819–25. doi: 10.1002/1529-0131(200104)44:4 <819::AID-ANR138>3.0.CO;2-P
45. Kwon Y, Pittler M, Ernst E. Acupuncture for peripheral joint osteoarthritis: a systematic review and meta-analysis. Rheumatology. (2006) 45:1331–7. doi: 10.1093/rheumatology/kel207
46. Hopton A, MacPherson H. Acupuncture for chronic pain: is acupuncture more than an effective placebo? A systematic review of pooled data from meta-analyses. Pain Pract. (2010) 10:94–102. doi: 10.1111/j.1533-2500.2009.00337.x
47. Hochberg MC, Altman RD, April KT, Benkhalti M, Guyatt G, McGowan J, et al. American college of rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care Res. (2012) 64:465–74. doi: 10.1002/acr.21596
48. Jevsevar DS. Treatment of osteoarthritis of the knee: evidence-based guideline. J Am Acad Orthop Surg. (2013) 21:571–6. doi: 10.5435/00124635-201309020-00008
49. Hawker GA, Badley EM, Croxford R, Coyte PC, Glazier RH, Guan J, et al. A population-based nested case-control study of the costs of hip and knee replacement surgery. Med Care. (2009) 47:732–41. doi: 10.1097/MLR.0b013e3181934553
50. Kolasinski SL, Neogi T, Hochberg MC, Oatis C, Guyatt G, Block J, et al. 2019 American college of rheumatology/arthritis foundation guideline for the management of osteoarthritis of the hand, hip, and knee. Arthritis Rheumatol. (2020). 72:220–33. doi: 10.1002/art.41142
51. Kim H-A, Kim S, Seo Y, Choi HJ, Seong SC, Song YW, et al. The epidemiology of total knee replacement in South Korea: national registry data. Rheumatology. (2008) 47:88–91. doi: 10.1093/rheumatology/kem308
52. Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KD. Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res. (2010) 468:57–63. doi: 10.1007/s11999-009-1119-9
53. Brander VA, Stulberg SD, Adams AD, Harden RN, Bruehl S, Stanos SP, et al. Ranawat award paper: predicting total knee replacement pain: a prospective, observational study. Clin Orthop Relat Res. (2003) 416:27–36. doi: 10.1097/01.blo.0000092983.12414.e9
54. Hawker G, Wright J, Coyte P, Paul J, Dittus R, Croxford R, et al. Health-related quality of life after knee replacement: results of the knee replacement patient outcomes research team study. J Bone Joint Surg Am. (1998) 80:163–73. doi: 10.2106/00004623-199802000-00003
55. Knutson K, Robertsson O. Swedish knee arthroplasty register. Acta Orthop. (2010) 81:5–7. doi: 10.3109/17453671003667267
56. Graves S, Davidson D, de Steiger R, Ryan P, Griffith EC, McDermott BF, et al. Australian Orthopaedic Association National Joint Replacement Registry. Annual Report. Adelaide, SA: AOA (2010).
57. Roberts V, Esler C, Harper W. A 15-year follow-up study of 4606 primary total knee replacements. J Bone Joint Surg Br. (2007) 89:1452–6. doi: 10.1302/0301-620X.89B11.19783
Keywords: knee osteoarthritis, knee surgery, acupuncture, National Health Insurance Service-National Sample Cohort (NHIS-NSC), respective cohort study
Citation: Gang B-G, Shin J-S, Lee J, Lee YJ, Cho H-W, Kim M-r, Kang K, Koh W, Kim E-J, Park Y, Nam D and Ha I-H (2020) Association Between Acupuncture and Knee Surgery for Osteoarthritis: A Korean, Nationwide, Matched, Retrospective Cohort Study. Front. Med. 7:524628. doi: 10.3389/fmed.2020.524628
Received: 08 January 2020; Accepted: 13 August 2020;
Published: 16 September 2020.
Edited by:
Peter Mandl, Medical University of Vienna, AustriaReviewed by:
Deng-Ho Yang, Taichung Armed Forces General Hospital, TaiwanCopyright © 2020 Gang, Shin, Lee, Lee, Cho, Kim, Kang, Koh, Kim, Park, Nam and Ha. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: In-Hyuk Ha, aGFuaWhhdGFAZ21haWwuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.