- 1Second Medical Department, Korneuburg-Stockerau Hospital, Lower Austrian Centre for Rheumatology, Stockerau, Austria
- 2Medical Directorate, Hospital of St. John of God, Vienna, Austria
Objectives: Gout is generally managed in the primary health care sector. Compliance of primary care physicians with gout management recommendations has been shown to be insufficient in the past. The primary aims of this study were to assess primary care providers' knowledge regarding gout and to determine if their treatment decisions are influenced by recommendations. Facing considerable variations in postgraduate training options in Austria, we secondly looked for possible knowledge differences between urban and rural areas and eastern and western parts of Austria.
Methods: We conducted a survey among 343 primary care physicians in Austria, using a questionnaire consisting of 10 questions on acute, intercritical and general gout management. Gout treatment recommendations served as the therapeutic gold standard.
Results: Of the 343 physicians surveyed, 336 completed the questionnaire, leading to a very high return rate of 98%. 289 (86%) physicians were aware of the agreed-upon SUA target (<6 mg/dl). 323 (96.1%) reported change of therapy in case of missing this target. 112 (33.3%) physicians voted for long term ULT. No geographical differences in knowledge regarding gout or its management were revealed, except that colchicine was rated as being a safe medication significantly more often in rural areas (p = 0.035) and in western Austria (p = 0.014).
Conclusion: As opposed to former studies, gout knowledge among primary care physicians has improved - however, treatment patterns are still not fully concordant with gout recommendations. Our findings may help to better tailor future postgraduate training to improve primary care physicians' education in gout.
Introduction
Gout, with a prevalence of ~2%, is the leading cause of inflammatory arthritis within developed countries. Left untreated, gout has the potential to advance into a chronic stage, including joint destruction and associated problems (1). Globally, especially in countries with a high socio-demographic index, a growing prevalence can be observed (2). An association between gout and various internal diseases is generally acknowledged (3–6). Gout is an independent predictor of cardiovascular morbidity and mortality, although causal pathways have not yet been fully elucidated (7–9). Moreover, an extended therapeutic armamentarium with new urate-lowering therapies (ULT) has also elevated awareness about gout. Thus, a number of gout recommendations have been established by various rheumatologic societies (10–15). Gout is mainly managed in the primary care sector. Despite the multitude of recommendations available, the standard of gout management is not yet optimal and lags behind the research (16–18). Therefore, research, especially in primary care, is proposed (10).
The primary aims of the present study were to assess primary care physicians' knowledge regarding gout and their adherence to current treatment recommendations as the gold standard. Thus, therapeutic and general gout management was evaluated across Austria. As continuous advanced medical training is compulsory in Austria, approved postgraduate training is offered by the Austrian academy of physicians (Akademie der Ärzte), the educational branch of the Austrian medical association. According to the 2018 report of the Austrian academy of physicians, there is a regional variability in trainings offered. Trainings in internal medicine and rheumatology were offered in a considerable range from 720 (Vienna) to 98 (Burgenland)1. In relation to the number of primary care physicians per province, trainings offered per physician range from 0.54 (Upper Austria) to 0.95 (Vienna)2. Therefore, as a secondary aim, we also looked for differences in gout-related knowledge between urban and rural areas and between eastern and western parts of the country, respectively.
Materials and Methods
Participants
All physicians practicing in Austria are obliged to be members of the Austrian Medical Association (AMA) and are registered in an official list. This list served as the data source for the selection of the participants. Comparable to similar surveys, we aimed at a sample size of 5–10% of all Austrian primary care physicians. From January till March 2019, fourteen pharmaceutical representatives were instructed to randomly pick twenty-five physicians each from the AMA-list according to their catchment areas. They distributed the questionnaires directly to the physicians' offices, along with prepaid return envelopes. A financial incentive of €50 was offered for completing the questionnaire.
Questionnaire
We developed an anonymous, self-administered questionnaire, consisting of ten questions to assess clinical knowledge and beliefs and to investigate therapeutic patterns for acute and intercritical gout as well as general gout management (see Table 1). The questions were selected and adapted from a previous questionnaire of 17 questions, successfully tested and used in a survey among Austrian rheumatologists in 2013 (19). Again, the content of current gout treatment recommendations (EULAR recommendations, the evidence based S2e guidelines of the German Society of Rheumatology and the International 3e- as well as the Austrian 3e-recommendations for the management of gout) served as the gold standard (10, 12, 14, 15). These recommendations are concordant regarding questions 1–6, 9 and 10. Question 7 regarding the duration of ULT is addressed in the EULAR and International 3e- and Austrian 3e-recommendations. Question 8 is addressed only in the German S2e guideline.
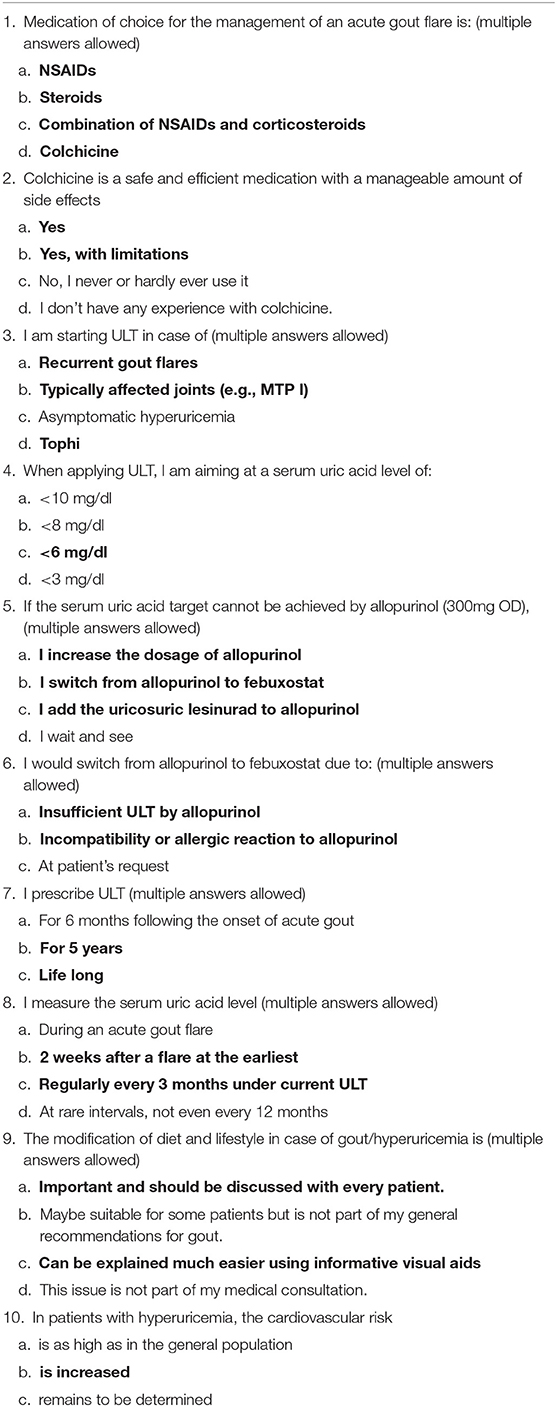
Table 1. Questionnaire, MTP I = metatarsophalangeal joint I, OD = once daily (correct answers are highlighted in bold).
The comprehensibility of the questionnaire was tested by interviews with two primary care physicians. The questionnaire was intentionally kept short and easy to complete in order to achieve a high return rate. Some of the questions had a multiple-choice response option. The questionnaire included a short explanation how to complete it. It was indicated to answer the questions according to the participants' knowledge of current national or international guidelines. All items with multiple answers allowed were indicated. Given several recommendations as gold standard, to gather the whole body of knowledge, the authors agreed to mark multiple-choice answers, as follows: full accordance if all answers were ticked in accordance with recommendations and as partial accordance if some answers conforming with recommendations were ticked. If both conforming and nonconforming answers were given, the answer was marked as partly conflicting and, if no concordance with recommendations at all was given, it was marked as fully conflicting. Concomitantly, basic demographic data for participants was collected, along with data on location and catchment area of physicians' practices in order to differentiate between urban and rural areas. Completion time for the questionnaire was tested beforehand on five primary care physicians and took <5 min. No patients were involved in the study and no patient data was obtained in the questionnaire. In accordance with the national legislation, written informed consent for participation was not required for this study. Because the study only involved voluntary participation and did not include any further intervention, a retrospective waiver of ethics approval was sufficient and has been obtained from the Lower Austrian Ethics committee.
Analysis
For initial analyses, descriptive statistics were used. For continuous variables, we calculated the mean as well as the standard deviation (SD). For categorical variables, proportions were calculated. We tested categorical data with the chi-square test. P-values < 0.05 were considered statistically significant. For unequal distributions, weighted contingency tables have been calculated.
Results
Respondents
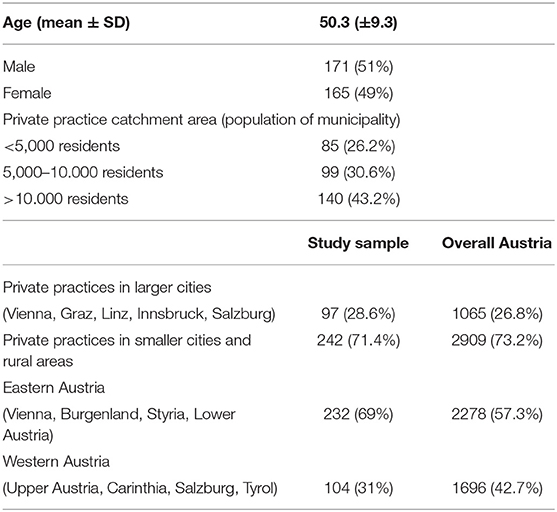
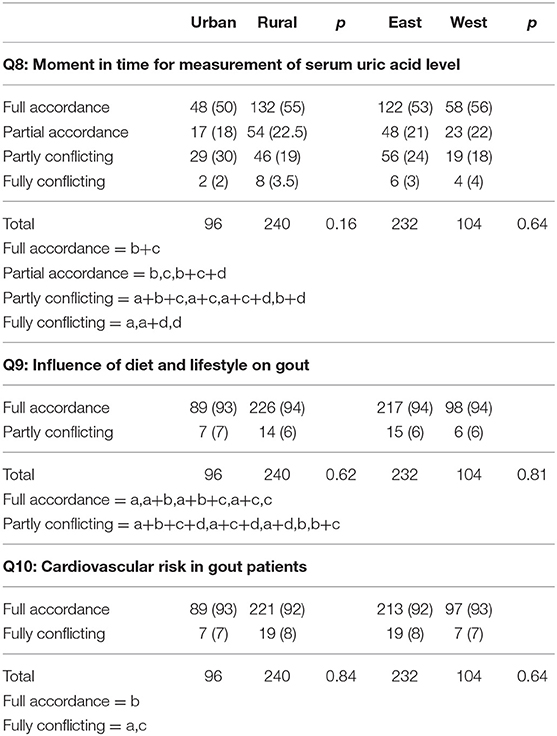
Out of 343 physicians approached, 339 responded. 336 questionnaires were complete which represents a return rate of 98%. We were able to gather participants from eight of nine Austrian provinces (for demographics and regional distribution of participating physicians see Table 2). The proportions of participants per province in our sample were similar to the proportions of overall primary care physicians per province in six of the comprised provinces. The rate of participating physicians in Upper Austria only reached 12% of the pursued rate whereas in Carinthia it exceeded the pursued rate 2.6 fold. The overall participation rate amounted to 8.5% (see Table 3).
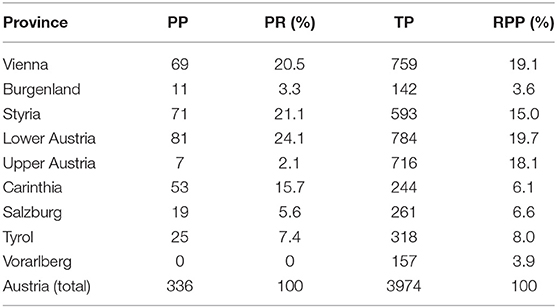
Table 3. Number of participating primary care physicians per province (PP), participation rate in relation to the sample size (PR), total number of primary care physicians per Austrian province (TP), relative number of primary care physicians per Austrian province (RPP).
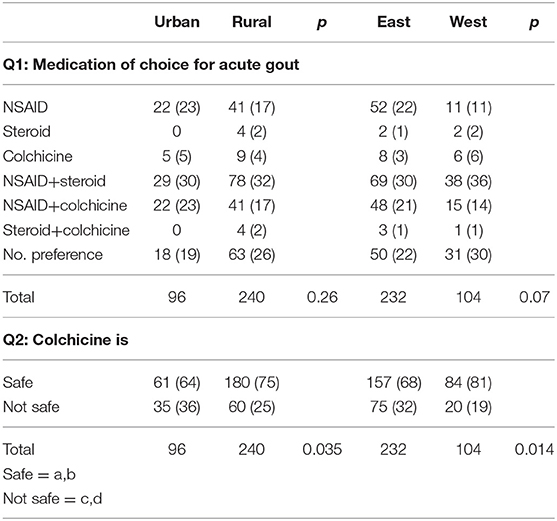
Management of Acute Gout Flares
For the management of acute gout flares, NSAIDs combined with corticosteroids are the medication of choice (107/31.8%), followed by NSAID monotherapy or combined with colchicine. 81 physicians (24.1%) ticked all available options, thereby giving no preference.
Colchicine is regarded as a safe medication by 241 (71.7%) physicians, with 61 (64%) in urban areas vs. 180 (75%) in rural areas, which is significantly different (p = 0.035). Likewise, 157 (68%) physicians in eastern Austria consider colchicine a safe medication vs. 84 (81%) in western Austria, which is also significantly different (p = 0.014) (see Table 4).
Urate Lowering Therapy
The question on the use of ULT, representing the management of intercritical recurrent gout, is answered correctly by less than a quarter of physicians (23% in rural areas, 18% in urban areas). 213 (63.4%) responses are at least partly in line with the applied current recommendations.
Concerning the serum uric acid (SUA) target, 289 (86%) answered correctly in accordance with the generally recommended SUA target of <6 mg/dl. There was no observable statistical difference between urban and rural areas nor between eastern and western Austria (p = 0.08).
The vast majority of physicians (323/96.1%) would actively change their therapeutic regime if the SUA target was not yet reached. Among these, 271 (80.7%) would switch medications from allopurinol to febuxostat. 12 (3.6%) would only increase the allopurinol dose. 2.4% would wait and see.
210 (62.5%) of physicians stated that they would switch from allopurinol to febuxostat if the former was no sufficient ULT or if patients would experience an allergy or incompatibility to allopurinol. 27 (8%) explicitly addressed an incompatibility or allergic reaction to allopurinol as the main reason for a switch.
A third of physicians chose long term ULT. Incorrect answers were obtained from 165 (49.1%) responders (see Table 5).
Measurement of Serum Uric Acid
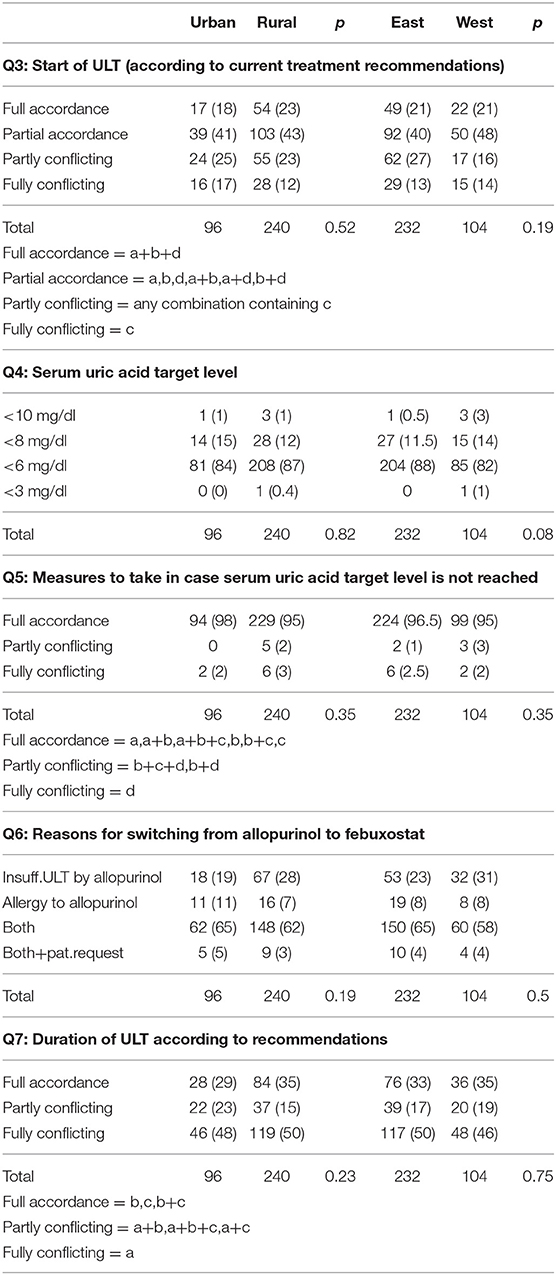
The correct moment in time for measurement of SUA was given by 53.6% of the responding physicians. Incorrect answers were obtained from only 3%.
Diet and Lifestyle
93.8% of physicians correctly acknowledged diet and lifestyle as important factors that have to be addressed in patients with gout. An elevated cardiovascular risk of gout patients was acknowledged by 92.3% (see Table 6).
Discussion
In a nationwide survey on knowledge and treatment practices for gout, we gathered data from primary care physicians and were able to achieve a return rate of 98%. Our sample represents 8.5% of the primary care physicians of Austria, a rate which is comparable to a similar survey in the US (20). Our study population represents the relative distribution of Austrian private practices with respect to urban and non-urban regions as well as the relative distribution for the majority of the Austrian provinces. As a limitation, two provinces are underrepresented whereas one is overrepresented. However, an additional weighted analysis of our data revealed no difference of results in comparison to the not weighted analysis.
Austrian primary care physicians are aware of current treatment recommendations for gout, to a greater extent than comparable surveys have shown (16, 20). While the pursued SUA target and the change of therapeutic regimes in case of not reaching it are well known, we observed deficits concerning the correct moment in time for SUA measurement, the correct start of ULT and its duration. In contrast to earlier investigations, the importance of addressing diet and lifestyle with gout patients is widely acknowledged (20). Despite regional variations in postgraduate training, no major differences in compliance with treatment recommendations between different regions of Austria could be observed.
Comparison With Former Surveys
Gout is largely managed by primary care physicians. It is therefore eminently important to ensure familiarity with rheumatologic recommendations for the management of gout. A few surveys on the compliance of clinicians' work with current guidelines have been conducted, using different designs and approaches - some among rheumatologists, others among primary care providers (16, 19–25). Our survey is—to our knowledge—the first one to compare urban and rural areas and different geographical regions, when assessing awareness of gout management recommendations and treatment patterns in the primary care setting. In contrast to similar studies in France and the US, we were able to achieve a considerably higher percentage of participating physicians. Also, the return rate in our survey was significantly higher (16, 26). This may have been positively influenced by two factors: personal delivery of questionnaires by traveling pharmaceutical staff on the one hand and offering a financial incentive for the completion of the questionnaire on the other. The latter had also been applied in one of the above-mentioned surveys (20). The inclusion of monetary incentives to partially compensate physicians for time spent completing a survey and also to show appreciation for their efforts is supported by the literature (26). The selection of participating physicians was representative, as their demographics perfectly match those of all Austrian primary care physicians (mean age 53.3 years, 48% female)3 (Table 2).
Management of Acute Gout
Regarding therapy for acute gout flares, NSAIDs in combination with corticosteroids are the preferred therapeutic strategy in Austria. This is in line with literature suggestions for gout. NSAIDs are also the preferred treatment for musculoskeletal pain among primary care physicians (27, 28). Colchicine is part of all recommendations for acute gout management as well as for the prophylaxis of recurrent flares. In the survey conducted among Austrian rheumatologists in 2013, only 17% of the responders considered colchicine as a safe medication (19). In the present survey, this percentage was higher and especially pronounced in rural areas, reaching statistical significance. Also, significantly more physicians in western Austria consider colchicine a safe medication as compared to eastern Austria. This observation is difficult to interpret, given the fact, that less postgraduate education is offered outside large cities and in western Austria1.
Management of Recurrent Gout
Apart from the correct answers regarding different indications for initiating ULT, more than one third of all participants also voted for starting ULT in the case of asymptomatic hyperuricemia, either per se or in combination with other indications (multiple answers allowed). Whether or not the participating primary care physicians were influenced by reports on positive effects of ULT in terms of internal comorbidities e.g., coronary artery disease, cannot be answered (29). Notably, we and others observed that the majority of rheumatologists comply with gout recommendations, not prescribing ULT in case of asymptomatic hyperuricemia (19, 22), whereas more than half of the interviewed specialists in internal medicine would treat asymptomatic hyperuricemia (22).
All gout therapy recommendations unanimously agree on the lifelong maintenance of the SUA target, once achieved. Knowledge about the SUA target <6 mg/dl in the treat to target approach in gout tends to be higher among the study participants than in former surveys (20, 22). Knowledge about possible risks of a SUA level below 3 mg/dl is as good (10). In summary, awareness of appropriate SUA target levels appears to be sufficient in the primary care sector. In case of not reaching the SUA target, the vast majority of physicians would modify their therapeutic strategy, which is also in line with the recommendations. Most physicians voted for a switch to febuxostat. Fewer would increase the allopurinol dose, which underscores earlier findings on allopurinol prescription practice (30–32).
Remarkably, we observed considerable differences in the prescription duration of ULT. Though the underlying recommendations agree upon the maintenance of a lifelong treatment, only a third of physicians voted for long term therapy. A possible explanation for the high percentage of answers favoring six months of ULT following an acute flare, could be confusion with the recommended duration of a flare prophylaxis. However, even in surveys among rheumatologists, long term maintenance of the SUA target once achieved, was identified as one of the main problems in gout management (25).
General Gout Management
Only half of the physicians responded correctly with respect to the moment in time for taking SUA measurement. For the treat to target approach in gout, measurement of uric acid is part of most recommendations, while no exact moment in time for taking SUA measurement is explicitly mentioned (10–15, 33, 34). As already pointed out by others, the clear definition of time intervals to measure SUA is mandatory but still lacking (11).
As opposed to the limited knowledge on diagnostic and therapeutic measures, a huge majority of physicians was well informed about the increased cardiovascular risk of patients with gout and about the necessity and benefits of addressing diet and lifestyle with gout patients (35). Knowledge of primary care providers on general aspects and the epidemiologic background of gout has considerably improved in recent years (20).
It has been shown that a more intense care of gout patients leads to a better outcome with significantly more patients achieving the SUA target experiencing significantly fewer gout attacks (36). That underscores the importance of thorough and comprehensive management of gout in the primary health care setting. Primary care physicians consent to the benefits of a close collaboration with rheumatologists, who are also assigned to deliver and improve ongoing rheumatologic training for the primary care sector (37).
A possible shortcoming of the study is that we did not ask for the individual amount of recent postgraduate training in gout. However, having given the situation in Austria, that postgraduate training is compulsory for all physicians, we chose to take the number of trainings per province, offered by the official agency (Österreichische Akademie der Ärzte) as a marker of available knowledge1. Moreover, a discrepancy between reported knowledge and treatment patterns in daily clinical practice cannot be ruled out (22). In order to create a compact questionnaire, we did neither ask for the inclusion of patient data nor for details concerning co-medications. However, this lean approach led to the highest response rate in a survey on gout so far.
Conclusion
In comparison to former findings, we observed a progress in knowledge regarding gout among primary care physicians. The participants show a high awareness of the pursued SUA target and tend to adjust their therapy when the SUA target is not achieved. The importance of addressing diet and lifestyle with gout patients as well as the increased cardiovascular risk of these patients is well known. However, there is still undeniable need for improvement regarding the issues of ULT and SUA measurement. Our findings may help to better tailor future postgraduate transfer of knowledge regarding gout for the primary care sector. A modified educational content could close the knowledge gaps revealed to improve the care of patients with gout.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author Contributions
JS: conception, design, acquisition of data and manuscript preparation. TS: statistical analysis and review of the manuscript.
Funding
This work was supported by Menarini Pharma GmbH Austria, who funded the printing of the questionnaires, delivery to the physicians, postal charges, the provision of monetary incentives for the participating physicians and the cost for linguistic review of the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors wish to thank Prof. Martina Mittlboeck from the Section for Clinical Biometrics of the Medical University of Vienna for her valuable statistical advice.
Abbreviations
SUA, serum uric acid; ULT, urate lowering therapy; NSAID, non steroidal antirheumatic drug.
Footnotes
1. ^Source: Österreichische Akademie der Ärzte GmbH: https://www.arztakademie.at/fileadmin/template/main/DFP_FBBerichte/2019_AErztlicher_Fortbildungsbericht.pdf (personal communication with the Austrian academy of physicians).
2. ^Source: Hauptverband der Österreichischen Sozialversicherungsträger, Austrian National Insurance, report on primary care physicians, 31.12.2015, page 8: https://www.sozialversicherung.at/cdscontent/load?contentid=10008.714996&version=1509372519
3. ^Source: Austrian Medical Association, report on physicians' statistics, 31.12.2018, https://www.aerztekammer.at/documents/261766/124736/OeAeK+Aerztestatistik_2018.pdf/a7504601-fae6-938d-368d-1dc224bb8118
References
1. Zhu Y, Pandya BJ, Choi HK. Prevalence of gout and hyperuricemia in the US general population: The National Health and Nutrition Examination Survey 2007-2008. Arthritis Rheum. (2011) 63:3136–41. doi: 10.1002/art.30520
2. Xia Y, Wu Q, Wang H, Zhang S, Jiang Y, Gong T, et al. Global, regional and national burden of gout, 1990–2017: a systematic analysis of the global burden of disease study. Rheumatology. (2019). doi: 10.1093/rheumatology/kez476. [Epub ahead of print].
3. Singh JA, Cleveland JD. Gout is associated with a higher risk of chronic renal disease in older adults: a retrospective cohort study of U.S Medicare population. BMC Nephrol. (2019) 20:93. doi: 10.1186/s12882-019-1274-5
4. Bhole V, Choi JW, Kim SW, de Vera M, Choi H. Serum uric acid levels and the risk of type 2 diabetes: a prospective study. Am J Med. (2010) 123:957–61. doi: 10.1016/j.amjmed.2010.03.027
5. Kuo CF, Yu KH, See LX, Chou IJ, Ko YS, Chang HC, et al. Risk of myocardial infarction among patients with gout. A nationwide population-based study. Rheumatology. (2013) 52:111–7. doi: 10.1093/rheumatology/kes169
6. Kim SY, Guevara JP, Kim KM, Choi HK, Heitjan DF, Albert DA. Hyperuricemia and risk of stroke: a systematic review and meta-analysis. Arthritis Rheum. (2009) 61:885–92. doi: 10.1002/art.24612
7. Perez-Ruiz F, Richette P, Stack A, Karra Gurunath R, Garcia de Yebenes MJ, Carmona L. Failure to reach uric acid target of <0.36 mmol/l in hyperuricemia of gout is associated with elevated total and cardiovascular mortality. RMD Open. (2019) 5:e001015. doi: 10.1136/rmdopen-2019-001015
8. Disveld IJM, Zoakman S, Jansen TLTA, Rongen GA, Kienhorst LBE, Janssens HJEM, et al. Crystal-proven gout patients have an increased mortality due to cardiovascular diseases, cancer, and infectious diseases especially when having tophi and/or high serum urid acid level: a prospective cohort study. Clinical Rheumatol. (2019) 38:1385–91. doi: 10.1007/s10067-019-04520-6
9. Perez-Ruiz F, Martinez-Indart L, Carmona L, Herrero-Beites AM, Pijoan JI, Krishnan E. Tophaceous gout and high level of hyperuricemia are both associated with increased risk of mortality in patients with gout. Ann Rheum Dis. (2014) 73:177–82. doi: 10.1136/annrheumdis-2012-202421
10. Richette P, Doherty M, Pascual E, Barskova V, Becce F, Castaneda-Sanabria J, et al. 2016 updated EULAR evidence-based recommendations for the management of gout. Ann Rheum Dis. (2017) 76:29–42. doi: 10.1136/annrheumdis-2016-209707
11. Kiltz U, Smolen J, Bardin J, Cohen Solal A, Dalbeth N, Doherty M, et al. Treat-to-Target (T2T) recommendations for gout. Ann Rheum Dis. (2017) 76:632–8. doi: 10.1136/annrheumdis-2016-209467
12. Kiltz U, Alten R, Fleck M, Krüger K, Manger B, Müller-Ladner U, et al. Full version of the S2e guidelines on gouty arthritis: Evidence-based guidelines of the German Society of Rheumatology (DGRh). Z Rheumatol. (2016) 75 Suppl 2:11–60. doi: 10.1007/s00393-016-0147-6
13. Jordan JM, Cameron JS, Snaith M, Zhang W, Doherty M, Seckl J, et al. British Society for Rheumatology and British Health Professionals in Rheumatology guideline for the management of gout. Rheumatology. (2007) 46:1372–4. doi: 10.1093/rheumatology/kem056a
14. Sivera F, Andrés M, Carmona L, Kydd AS, Moi J, Seth R, et al. Multinational evidence-based recommendations for the diagnosis and management of gout: integrating systematic literature review and expert opinion of a broad panel of rheumatologists in the 3e initiative. Ann Rheum Dis. (2014) 73:328–35. doi: 10.1136/annrheumdis-2013-203325
15. Sautner J, Gruber J, Herold M, Zwerina J, Leeb BF. Austrian 3e-recommendations for diagnosis and management of gout 2013. Wien Klin Wochenschr. (2014) 126:79–89. doi: 10.1007/s00508-013-0469-1
16. Goossens J, Lancrenon S, Lanz S, Ea HK, Lambert C, Guggenbuhl P, et al. GOSPEL 3: Management of gout by primary-care physicians and office-based rheumatologists in France in the early 21st century – comparison with 2006 EULAR recommendations. Joint Bone Spine. (2017) 84:447–53. doi: 10.1016/j.jbspin.2017.04.002
17. Keenan RT. Limitations of the current standards of care for treating gout and crystal deposition in the primary care setting: a review. Clin Ther. (2017) 39:430-441. doi: 10.1016/j.clinthera.2016.12.011
18. Pascual E, Sivera F. Why is gout so poorly managed? Ann Rheum Dis. (2007) 66:1269–7. doi: 10.1136/ard.2007.078469
19. Sautner J. Diagnosis and management of gout in Austria. Survey of current practice considering the EULAR recommendations. Z Rheumatol. (2014) 73:836–42. doi: 10.1007/s00393-014-1371-6
20. Harrold LR, Mazor KM, Negron A, Ogarek J, Firneno C, Yood RA. Primary care providers' knowledge, beliefs and treatment practices for gout: results of a physician questionnaire. Rheumatology. (2013) 52:1623–9. doi: 10.1093/rheumatology/ket158
21. Roddy E, Packham J, Obrenovic K, Rivett A, Ledingham JM. Management of gout by UK rheumatologists: a British Society for Rheumatology national audit. Rheumatology. (2018) 57:826–30. doi: 10.1093/rheumatology/kex521
22. Doherty M, Bardin T, Pascual E. International survey on the diagnosis and management of gout. Ann Rheum Dis. (2007) 66:1685–6. doi: 10.1136/ard.2007.071530
23. Pal B, Foxall M, Dysart T, Carey F, Whittaker M. How is gout managed in primary care? A review of current practice and proposed guidelines. Clin Rheumatol. (2000) 19:21–5. doi: 10.1007/2100670050005
24. Jeyaruban A, Soden M, Larkins S. General practitioners' perspectives on the management of gout: A qualitative study. Postgrad Med. (2016) 92:603–07. doi: 10.1136/postgradmedj-2015-133920
25. Roddy E, Zhang W, Doherty M. Concordance of the management of chronic gout in a UK primary-care population with the EULAR gout recommendations. Ann Rheum Dis. (2007) 66:1311–5. doi: 10.1136/ard.2007.070755
26. Thorpe C, Ryan B, McLean SL, Burt A, Stewart M, Brown JB, et al. How to obtain excellent response rates when surveying physicians. Fam Pract. (2009) 26:65–8. doi: 10.1093/fampra/cmn097
27. Engel B, Just J, Bleckwenn M, Weckbecker K. Treatment options for gout. Dtsch Arztebl Int. (2017) 114:215–22. doi: 10.3238/arztebl.2017.0215
28. Babatunde OO, Jordan JL, van der Windt DA, Hill JC, Foster NE, Protheroe J. Effective treatment options for musculoskeletal pain in primary care: A systematic overview of current evidence. PLoS ONE. (2017) 12:e0178621. doi: 10.1371/journal.pone.0178621
29. Yen FS, Hsu CC, Li HL, Wie JC, Hwu CM. Urate-lowering therapy may prevent the development of coronary artery disease in patients with gout. Front Med. (2020) 7:63. doi: 10.3389/fmed.2020-00063
30. Coburn BW, Bendlin KA, Syles H, Meza J, Russell CL, Mikuls TR. Allopurinol medication adherence as a mediator of optimal outcomes in gout management. J Clin Rheumatol. (2017) 23:317–23. doi: 10.1097/RHU.0000000000000561
31. Rashid N, Coburn BW, Wu YL, Cheetham TC, Curtis JR, Saag KG, et al. Modifiable factors associated with allopurinol adherence and outcomes among patients with gout in an integrated healthcare system. J Rheumatol. (2015) 42:504–12. doi: 10.3899/jrheum.140588
32. Clarson LE, Hider SL, Belcher J, Roddy E, Mallen CD. Factors influencing allopurinol initiation in primary care. Ann Fam Med. (2017) 15:557–60. doi: 10.1370/afm.2137
33. Qaseem A, Harris RP, Forciea MA. Clinical guidelines committee of the american college of physicians. Management of acute and recurrent gout: a clinical practice guideline from the American College of physicians. Ann Intern Med. (2017) 166:58–68. doi: 10.7326/M16-0570
34. Richette P, Doherty M, Pascual E, Barskova V, Becce F, Castaneda J, et al. 2018 updated European League Against Rheumatism evidence-based recommendations for the diagnosis of gout. Ann Rheum Dis. (2020) 79:31–8. doi: 10.1136/annrheumdis-2019-215315
35. Sautner J, Eichbauer-Sturm G, Gruber J, Puchner R, Spellitz P, Strehblow C, et al. Austrian nutrition and lifestyle recommendations for gout and hyperuricemia. Z Rheumatol. (2015) 74:631–6. doi: 10.1997/s00393-015-1580-7
36. Doherty M, Jenkins W, Richardson H, Sarmanova A, Abhishek A, Ashton D, et al. Efficacy and cost-effectiveness of nurse-led care involving education and engagement of patients and a treat-to-target urate-lowering strategy versus usual care for gout: A randomised controlled trial. Lancet. (2018) 392:1403–12. doi: 10.1016/S0140-6736(18)32158-5
Keywords: primary health care, compliance, gout management recommendations, gout knowledge questionnaire, treatment patterns, gout flare, serum uric acid target, urate lowering therapy (ULT)
Citation: Sautner J and Sautner T (2020) Compliance of Primary Care Providers With Gout Treatment Recommendations—Lessons to Learn: Results of a Nationwide Survey. Front. Med. 7:244. doi: 10.3389/fmed.2020.00244
Received: 18 March 2020; Accepted: 07 May 2020;
Published: 02 June 2020.
Edited by:
Peter Mandl, Medical University of Vienna, AustriaReviewed by:
Filipa Farinha, University College London, United KingdomWarren Fong, Singapore General Hospital, Singapore
Copyright © 2020 Sautner and Sautner. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Judith Sautner, anVkaXRoLnNhdXRuZXI5MEBnbWFpbC5jb20=
 Judith Sautner
Judith Sautner Thomas Sautner
Thomas Sautner