
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Med. , 24 April 2017
Sec. Pathology
Volume 4 - 2017 | https://doi.org/10.3389/fmed.2017.00043
 Chiara Saglietti1
Chiara Saglietti1 Marco Volante2
Marco Volante2 Stefano La Rosa1
Stefano La Rosa1 Igor Letovanec1
Igor Letovanec1 Marc Pusztaszeri3
Marc Pusztaszeri3 Gaia Gatti2
Gaia Gatti2 Massimo Bongiovanni1*
Massimo Bongiovanni1*
Primary pulmonary salivary gland-type tumors are rare neoplasms arising from the seromucinous submucosal glands of the lower respiratory tract (LRT), the most common of which are mucoepidermoid carcinoma (MEC) and adenoid cystic carcinoma. They are morphologically indistinguishable from their salivary gland counterpart and recognizing them is a challenge, especially on cytological specimens. We analyzed 15 cases of histologically proven primary salivary gland tumors of the LRT to identify cytomorphological features and define potential diagnostic clues that might assist cytopathologists in the preoperative diagnosis of these neoplasias. Three out of the four cases of adenoid cystic carcinomas showed the characteristic tridimensional cell clusters and hyaline globules, whereas the last one did not show malignant cells; only two cases of MEC presented the three characteristic cell types (i.e., squamous, intermediate, and mucin secreting) on cytology. Since these neoplasms are rare and do not have a completely specific set of cytological features, it is important for practicing cytopathologists to be aware of the possibility of encountering them, in specimens from patients with LRT masses, in order to render the correct diagnosis.
Primary salivary gland-type tumors (PSGT) arising from the seromucinous submucosal glands of the lower respiratory tract (LRT) (which includes trachea, bronchus and lung) account for <1% of central airway carcinomas (1). They are rare neoplasms morphologically indistinguishable from their salivary gland counterpart; therefore, recognizing them is a challenge, especially on cytology. Even though any type of salivary gland tumor that has been described in pathology textbooks can potentially arise in the LRT, published data show that the most commonly encountered primary salivary gland-type tumors in this anatomical site are malignant mucoepidermoid carcinoma (MEC), adenoid cystic carcinoma (AdCC), and epithelial-myoepithelial carcinoma (2–5). In fact, as opposed to the head and neck region, where the vast majority of salivary gland primaries are benign—with pleomorphic adenoma (PA) being the most common type—the contrary applies to LRT primaries (1).
Cytological examination of fine-needle aspiration (FNA), bronchial aspiration (BA) or brushing (BB), bronchoalveolar lavage (BAL), or even sputum has been shown to be a powerful tool for the diagnosis of lung cancer, particularly when it presents as an endobronchial growth. Moreover, in recent years, endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) has emerged as the standard of care for the diagnosis and staging of lung cancer and has been successfully implemented into daily clinical practice. EBUS-TBNA is minimally invasive, safe, cost-effective, and particularly useful in diagnosing centrally located lung lesions (6).
All the aforementioned cytological procedures are useful for collecting material for cytological examination, immunocytochemistry (ICC), fluorescent in situ hybridization (FISH), or molecular analyses, which may be relevant for diagnosis and targeted therapy. Moreover, in 30% of cases, cytological material is the only material available for pulmonary malignancies and proper classification of the lesions, often with subtyping, is fundamental for adequate patient management.
We describe 15 cases of histologically proven PSGT of the LRT; all but two were misdiagnosed on preoperative cytology. We have tried to identify cytomorphological features that could point to a correct cytological diagnosis. To the best of our knowledge, this is the largest cytological series of PSGT of the LRT ever published.
Nineteen cases of surgically resected PSGT originating from the trachea, main bronchi, and lung with corresponding preoperative cytology were identified by searching the databases of our institutions (Service of Clinical Pathology, Lausanne University Hospital; Department of Pathology, Geneva University Hospital; Section of Anatomic Pathology, San Luigi Hospital, Orbassano, Turin) over a period of 21 years (1995–2015). Cytological and histological specimens of each case were retrieved from the archives to be reviewed for adequacy. Three cases were excluded because slides were no longer available for revision, and one case was excluded because it originated from the larynx and not from the LRT. The database was also investigated to exclude the presence of primary salivary gland tumors that could have metastasized to the LRT.
The study cohort of the present work was thus composed of 15 cases. Clinical, radiological, and pathological reports for each patient were analyzed to collect pertinent information, including age, gender, alcohol and smoking history, presenting symptoms and signs, radiological findings, tumor size, and original preoperative cytological diagnosis.
All cytological smears were reviewed by an expert cytopathologist (Massimo Bongiovanni) to evaluate the presence of cytomorphological features that could have pointed to a correct preoperative diagnosis, namely: the presence of mucin and the three different neoplastic cellular components (mucin secreting, squamous, and intermediate) characteristic of MEC (3); organoid cell clusters, hyaline globules, cellular uniformity, and granular cytoplasm distinguishing AdCC (7). Particular attention was paid to look either cytologically or histologically for some of the newly described entities of salivary gland tumors, namely the mammary analog secretory carcinoma (MASC), the cribriform adenocarcinoma of the tongue, and minor salivary gland (CATS) that so far have never been described in the LRT (8).
A summary of all relevant clinical, radiological, and pathological data of the patients are presented in Table 1. Patients ranged in age from 16 to 87 years (mean 59.6 ± 18.6 years); there were nine males and six females. From histology, 11 cases were diagnosed as MEC (5 low grade and 6 high grade), and the remaining four cases were diagnosed as AdCC according to the histological criteria defined by the current WHO classification (3, 4).
The cytological slides that were revised included: 12 BA, 7 BB, 5 BAL, and 1 FNA. More than one type of cytological sample was available for 6 out of the 15 cases (Table 1). The smears were either alcohol-fixed, Papanicolaou (PAP) stained or air dried, May-Grünwald-Giemsa (MGG) stained. Neither FISH analysis nor molecular studies were originally performed.
Tumors were all centrally located and ranged in size from 1.7 to 5.0 cm (mean 4.4 ± 1.2 cm). Only one AdCC and one MEC were somehow identified preoperatively: the AdCC was diagnosed as a salivary gland-type neoplasia and the MEC as a non-small cell lung carcinoma, consistent with MEC. Five preoperative cytological cases were originally reported as negative for malignant cells (33.3%) (1 AdCC and 4 MEC), and this diagnosis was confirmed after revision of the slides in four out of five cases. Revised cytological diagnosis of the fifth case was that of an adenocarcinoma (concerning the BA specimen only). Interestingly, one AdCC was misdiagnosed as a metastatic breast carcinoma (due to the previous history of ductal breast carcinoma in the patient). During revision of the slides, all three diagnostic cases of AdCC showed the characteristic tridimensional cell clusters and hyaline globules that permit the cytological diagnosis of this entity, whereas only two cases of MEC presented the three characteristic cell types (i.e., squamous, intermediate, and mucin secreting) on cytology.
Cytology has proven to be a powerful tool for the diagnosis of primary lung cancer. A summary of all published cases of PSGT of the LRT for which a cytological diagnosis is available in the literature is provided in Table 2. Exfoliative cytology, in particular bronchial brushing, aspiration, and washing, is especially useful for tumors with endobronchial growth. PSGT of the LRT, because of their origin from the submucosal bronchial glands, mainly present as endobronchial masses (1), and therefore, they are considered as accessible for cytological sampling and diagnosis. However, as previously reported by other authors, primary pulmonary AdCCs and MECs are usually covered by intact respiratory epithelium; therefore, FNA may be more effective than exfoliative cytology in diagnosis for some of such cases (9, 10). The results from our study confirm that when using exfoliative cytology only, a significant proportion of PSGT of the LRT cases (33%) do not yield diagnostic tumor cells.
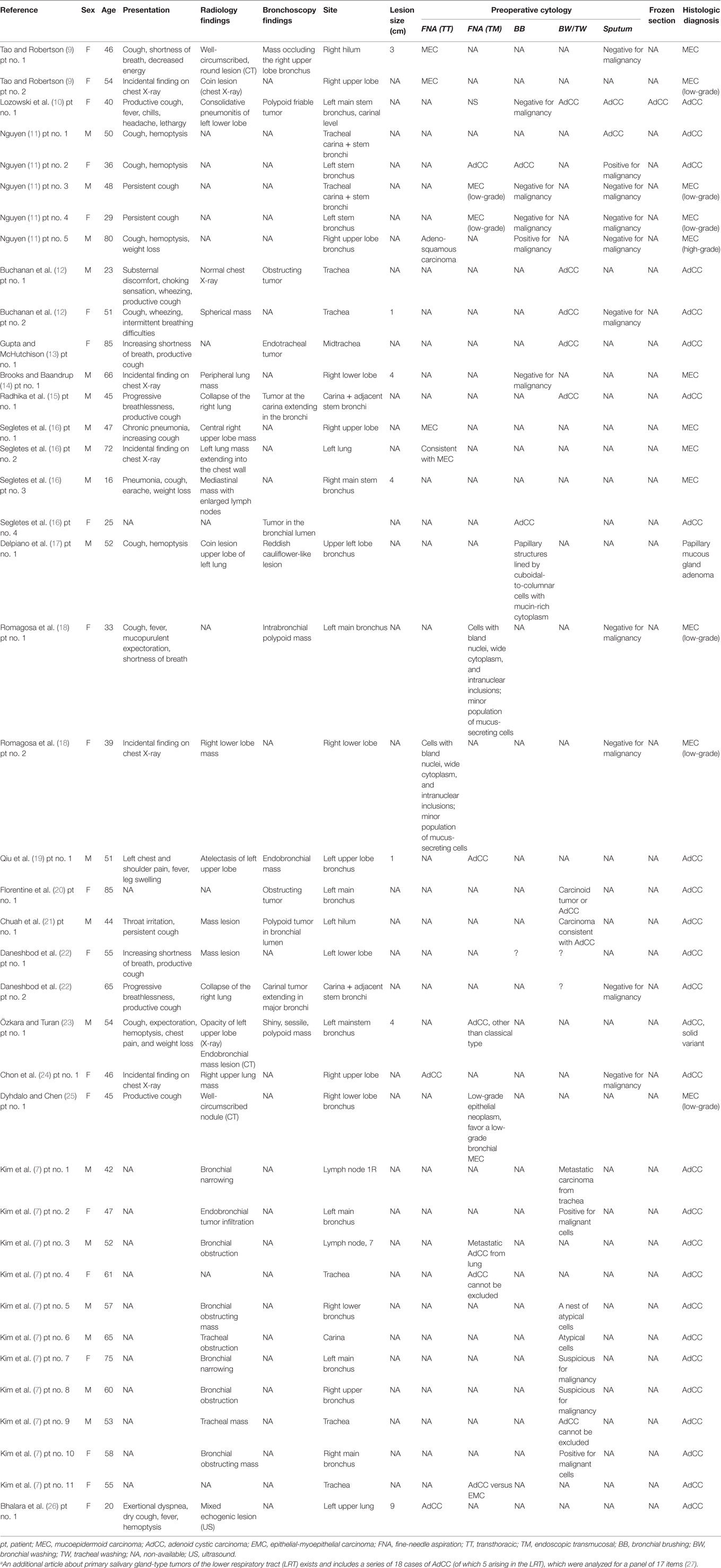
Table 2. Summary of all reported cases of primary salivary gland-type tumors of the lower respiratory tract for which cytological diagnosis is available in the literature.a
Mucoepidermoid carcinoma is the most common type of primary PSGT and it accounts for only 0.1–0.2% of all lung cancers (2, 28). In the majority of cases, it develops as an endobronchial lesion located in the central airways, namely trachea, carina, and main stem bronchi; less than 6% of patients present with a peripheral lung nodule (3, 28, 29). Prognosis of pulmonary MEC is significantly better than that of non-small cell lung cancer (NSCLC) and small cell lung cancer (SCLC). Five-year survival of these three entities is 88, 21 and <5%, respectively (30). When they are divided into high-grade and low-grade tumors, bronchial MEC show a 5-year survival of 31 and 80%, respectively (31). The cytological features of LRT MEC, which can be diagnosed by FNA, BB, BA, BW, and BAL, overlap those of their salivary gland counterpart. Three cell types should be identified from MEC histology: mucin-secreting, squamous, and intermediate cells, which can be organized in different architectural patterns (32). Low-grade tumors show cystic zones consisting of cytologically bland mucin-secreting cells and solid areas composed of squamous or intermediate cells. Mitoses and necrosis are rare. High-grade tumors mainly consist of atypical squamous and intermediate cells, accompanied by variable numbers of mucin-secreting cells; necrosis; and mitoses are frequent (Figures 1A,B) (3). On cytological specimens, various combinations of mucin-producing, squamous, and intermediate cells have been observed according to tumor grade, with the characteristic admixture of all three cell types being helpful for recognition of this entity (Figures 1C–F) (9, 14, 25): typical non-keratinized squamous cells show round nuclei and moderate cytoplasm; mucinous cells are variable in shape, have small uniform nuclei and prominent nucleoli, and may contain a single vacuole that displaces the nucleus; intermediate cells have well-defined homogeneous cytoplasm and small round nuclei with small nucleoli (25). Published cytological literature concerning primary pulmonary MEC shows that only Tao and Robertson and Brooks et al. have reported the presence of three distinct cell types (9, 14); all of the other authors described at best only two different cellular populations (Table 3) (11, 16, 18, 25). Other features encountered on MEC histology, such as the presence of intranuclear inclusions and clear cell change, have been occasionally described on cytology (18).
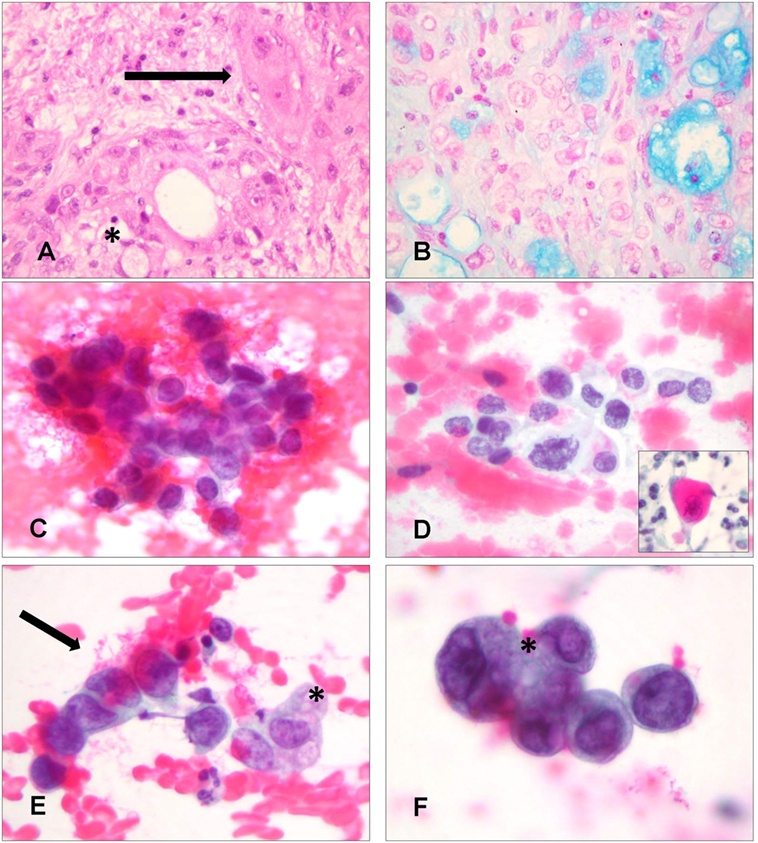
Figure 1. Histological and cytological aspects of primary mucoepidermoid carcinoma (MEC) of the lower respiratory tract. (A) Histologically, in case 9, diagnosed as a high-grade MEC, both squamous cells (arrow) and mucin-secreting cells (asterisk) are visible (Hematoxylin and Eosin, 400×). (B) Mucin-secreting cells are highlighted by Blue-Alcian stain. Small cystic spaces are also observed, even if these are more characteristic of low grade MEC (Blue-Alcian, 400×). (C) Cytologically, in the bronchial brushing of the same patient, atypical cells were recognized as intermediate cells after slide revision. These cells have a high nuclear/cytoplasmic ratio (Papanicolaou staining, 400×). (D) Squamous cells were also identified during revision of the slides, demonstrating atypical nuclei and more abundant cytoplasm. The inset shows cells with keratinizing cytoplasm (Papanicolaou staining, 400×). (E,F) Admixed intermediate cells (arrow) and mucin-secreting cells (asterisk); the abundance of mucin-secreting cells was the basis for diagnosis of adenocarcinoma on cytology (E) (Papanicolaou staining, 400×) (F) (Papanicolaou staining, 600×).
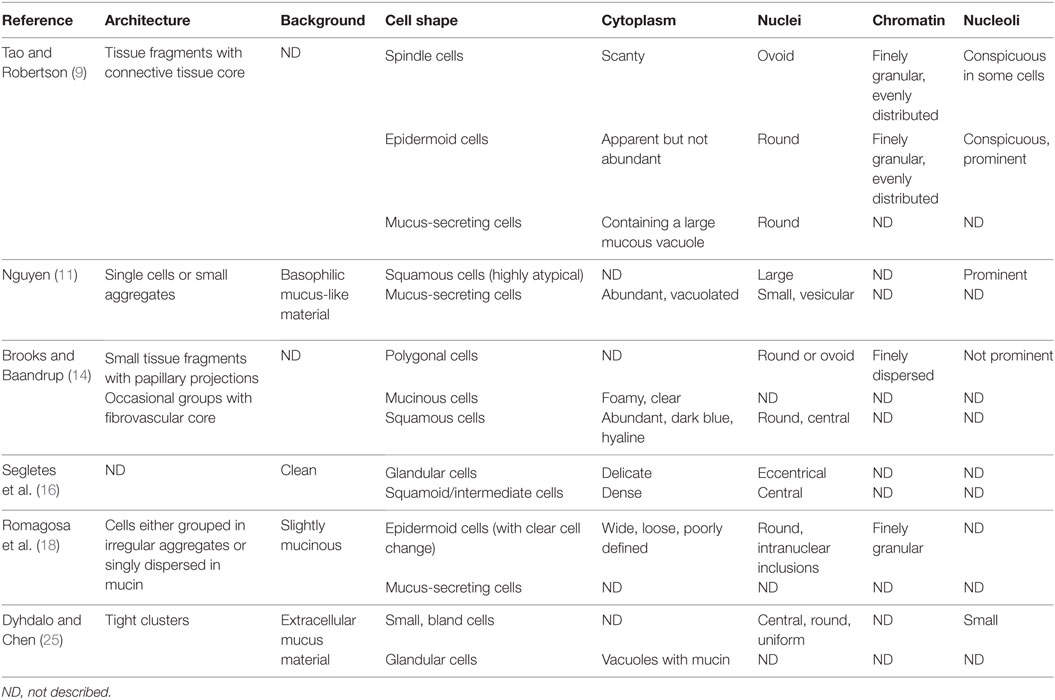
Table 3. Cytomorphological features of primary pulmonary mucoepidermoid carcinoma (MEC) reported in the literature.
Adenoid cystic carcinoma also generally arises as an endobronchial tumor in central airways (Figures 2A,B); only sporadically is it reported in a peripheral lung location (4). Primary pulmonary AdCC is composed of two main cell types, ductal and modified myoepithelial cells, and can present three main architectural patterns, in keeping with salivary AdCC: cribriform, tubular, and solid (1, 4). Cytological findings include cohesive clusters of repetitive medium-sized cells, with scant cytoplasm and uniform, small, hyperchromatic nuclei containing a finely granular, evenly distributed chromatin (Figures 2C–F). Tumor cells are often arranged around a central core of homogeneous myxoid material, or form three-dimensional, “ball-like” clusters (Table 4) (10–13, 15, 19–22, 24, 26, 33). All of these features that recapitulate the histopathology of AdCC are helpful in correctly orienting the cytological diagnosis of this neoplasm. Sometimes, isolated hyaline globules can be observed (7, 20, 24, 26); singly dispersed cells are present on some smears (11, 26). The basement membrane material, forming globules that have a light blue appearance on PAP stain and bright magenta on MGG stain, is the characteristic feature of AdCC; diagnostic difficulties arise when they are not present on cytological material, as the pattern could mimic carcinoid tumor, SCLC, NSCLC, and reserve cell hyperplasia (19).
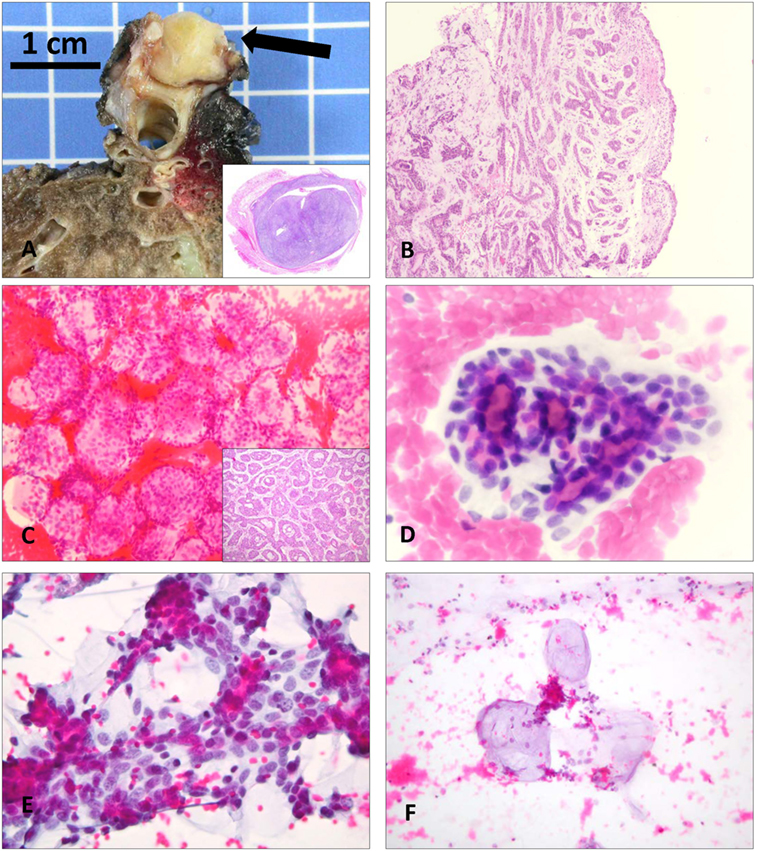
Figure 2. Macroscopic, histological, and cytological aspects of primary adenoid cystic carcinomas (AdCC) of the lower respiratory tract. (A) Macroscopic presentation of the 2.5-cm lesion in the distal carina of case 1. Inset shows the almost complete obliteration of the lumen of the bronchus (Hematoxylin and Eosin, scan of the slide). (B) Bronchial biopsy of case 4 demonstrates the typical cribriform and tubular pattern of AdCC (Hematoxylin and Eosin, 20×). (C) Ovoid structures constituted by monotonous cells surrounding a central lumen (“ball-like” clusters) that were considered as metastatic ductal breast carcinoma cells in case 2 (Papanicolaou staining, 200×). Inset shows the tubular architecture of the same case, exactly reflecting the cytological findings, which were correctly interpreted as primary AdCC on histology (Hematoxylin and Eosin, 20×). (D) Tubular structures comprised of repetitive medium-sized cells with scant cytoplasm and hyperchromatic nuclei containing a finely granular chromatin, containing a central core of homogeneous material. Note the inner layer of ductal cells and outer layer of myoepithelial cells (Papanicolaou staining, 400×). (E) The same cell types with scant pale-staining cytoplasm are arranged around hyaline globules in close proximity to each other (Papanicolaou staining, 400×). (F) Occasionally, the hyaline matrix is easily detected and is deprived of cells (Papanicolaou staining, 400×).
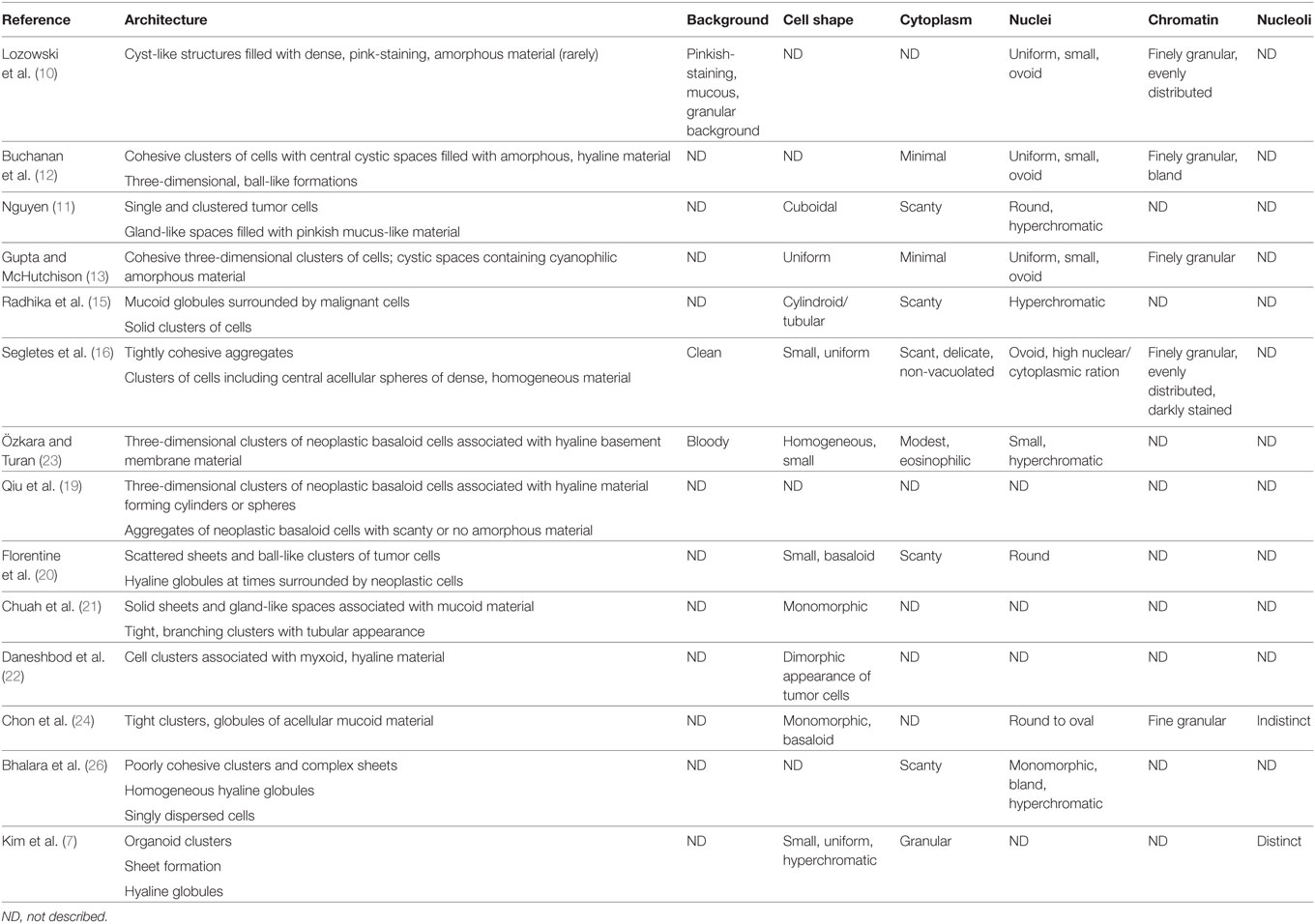
Table 4. Cytomorphological features of primary pulmonary adenoid cystic carcinoma (AdCC) reported in the literature.
Retrospectively, a correct preoperative diagnosis of all AdCC could have been rendered, because characteristic tridimensional clusters and hyaline globules were present on the smears; the hyaline globules were confused with a metastatic breast carcinoma in the original diagnosis of one case and considered suspicious for carcinoma, NOS, in the other. Considering MEC, only one additional case could have been identified. The cytological diagnosis of MEC was possible since all the three diagnostic cellular components were present with features of malignancy (i.e., squamous, glandular, and intermediate cells). When looking carefully at the smears, it was possible to identify aggregates of medium-sized cells that were bigger than basal and reserve bronchial cells. In the original cytological diagnosis, these intermediate cells were considered as suspicious for a carcinoma, NOS. Of note, in this case, an Alcian Blue staining was performed to identify glandular neoplastic cells, but only normal bronchial mucous cells were seen. Retrospective analysis revealed that the cells defined as “normal bronchial cells,” which stained positive for Blue-Alcian, were actually atypical. This allowed the retrospective diagnosis of MEC. In the remaining cases, the criteria for MEC were not fulfilled and only a poorly differentiated carcinoma could be diagnosed.
Immunocytochemistry is of limited value in diagnosing PSGT of the LRT. If these histological subsubtypes are not considered, only traditional markers of NSCLC subtyping are used. While epithelial cells of MEC and ductal cells of AdCC are positive for common epithelial markers (such as CK7 and CK 5/6) and p63 and p40 are expressed in all the intermediate and squamous cell component of MEC, myoepithelial cells of AdCC are usually positive for smooth muscle actin, vimentin, myosin, S-100, and for p63. Thus, CK7, CK5/6, p63, and p40 are potentially misleading markers as they are also part of the immunocyto-/histochemical panel used to classify lung carcinomas. Their positivity would lead to a diagnosis of primary lung squamous cell carcinoma, rather than pointing to the presence of a squamous cell component in MEC or to the myoepithelial differentiation typical of AdCC (34, 35).
Besides these more common entities, other rarer PSGT of the LRT include acinic cell carcinoma, PA with its malignant counterpart carcinoma ex PA, myoepithelioma and myoepithelial carcinoma, mucous gland adenoma, and oncocytoma (1, 33, 36, 37). No cytological description of such lesions in the LRT has been reported. Recently, a case of a primary pulmonary mucin-rich variant of salivary duct carcinoma with preoperative cytology was published: BAL revealed cytologic atypia, and the right upper lobe bronchial brushing was positive for carcinoma. However, ICC was not performed due to the paucity of diagnostic material and a conclusive diagnosis was not reached on cytological material (38). MASC, a rare salivary gland tumor first described in 2010, has never been described as a primary lung neoplasm (39). While reviewing the cytological and histological slides for our study, we paid particular attention to the identification of features that could point to a diagnosis of MASC, which we did not observe. No features resembling acinic cell carcinomas, that could have warranted (on cytological as well as on histological material) an immunocytochemical analysis for mammaglobin or FISH/molecular analysis for ETV6-NTRK3 translocation or ETV6 break, were seen (40, 41). ETV6-NTRK3 translocation or ETV6 breaks are present in up to 80 and 99% of MASC cases, respectively, and are quite specific for this entity (8).
In recent years, in addition to this molecular feature characteristic of MASC, other diagnostic molecular signatures have been described for salivary gland tumors, even the ones developing in the LRT, and some with a high prevalence and discrete specificity (8, 34, 35, 42). With respect to MEC, specific translocations involving the CRTC1 gene and MAML2 or CRTC3 and MAML2 have been described, with frequencies up to 80 and 6% respectively (8, 43, 44). AdCC is characterized by a specific translocation, namely MYB/NFIB, present in up 90% of cases (8, 45). This translocation results in MYB protein overexpression that can be detected using IHC (46, 47). This test can be particularly useful to confirm the diagnosis of AdCC, especially when combined with c-KIT (CD117) positivity, and can be applied on cytological smears. However, immunohistochemical staining for CD117 cannot be used alone in differential diagnosis of salivary gland neoplasms, because AdCC, PA, polymorphous low-grade adenocarcinoma, and monomorphic adenoma have all been found to be positive, to differing degrees, for CD117. The use of a panel of immunomarkers including MYB, CD117, and the zinc finger protein PLAG1 (PA gene 1), quite specific for PA, is more judicious and very effective (46–48). A search for the EGFR mutations was performed on the resected specimens of only one of our AdCC cases, which gave a negative result. Usually these tumors do not have EGFR mutations (49), although one case of AdCC with EGFR mutations has recently been reported (50). In our series (MEC and AdCC), molecular techniques could have been applied on cytological material in the case of diagnostic doubt, in order to detect these specific molecular alterations. However, apart the search for the EGFR mutation that has been done for therapeutic reasons, no molecular test was originally performed, not even for more recent cases. This supports the hypothesis that a diagnosis of primary PSGT was not considered.
An awareness of the possibility of encountering primary PSGT in the cytological specimens of patients investigated for LRT masses is fundamental to establishing a correct diagnosis. This is particularly relevant for AdCC, as all cases reported in literature showed characteristic cytological features that could have allowed a correct preoperatory diagnosis. As far as MEC is concerned, its preoperative diagnosis is more difficult, as the three different cellular components (i.e., squamous, intermediate, and mucin-secreting cells) were not always reported to be present on cytology specimens. In cases that raise suspicion of AdCC or MEC, additional immunohistochemical (MYB, c-kit) or molecular techniques (e.g., FISH) could be applied to cytological smears to refine the diagnosis.
The study protocol was approved by the regional ethical commission on research and human beings (CER-VD, 2016-00224). Informed consent was not necessary according to the art. 34 of the Federal Act on Research involving Human Beings (Human Research Act, HRA); data concerning study participants were anonymized.
MB conceived the idea of the project. MB, MV, GG, and MP contributed to identification of cases and data curation. CS and MB prepared the manuscript. MV, SLR, IL, MP, and MB reviewed the manuscript. All authors edited the manuscript before its submission.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
1. Falk N, Weissferdt A, Kalhor N, Moran CA. Primary pulmonary salivary gland-type tumors: a review and update. Adv Anat Pathol (2016) 23:13–23. doi: 10.1097/PAP.0000000000000099
2. Colby T, Koss M, Travis WD. Tumors of salivary gland type. In: Rosai J, editor. AFIP Atlas of Tumor Pathology. Tumors of the Salivary Glands. 3rd Series. (Vol. 13), Washington, DC: American Registry of Pathology (1995). p. 65–89.
3. Ishikawa Y, Alvarez-Fernandez E, Aubry MC, Dacic S, Nicholson AG. Salivary gland-type tumours. Mucoepidermoid carcinoma. In: Travis WD, Brambilla E, Burke AP, Marx A, Nicholson AG, editors. WHO Classification of Tumours of Lung, Pleura, Thymus and Heart. Lyon: IARC Press (2015). p. 99–100.
4. Ishikawa Y, Dacic S, Nicholson AG. Salivary gland-type tumours. Adenoid cystic carcinoma. In: Travis WD, Brambilla E, Burke AP, Marx A, Nicholson AG, editors. WHO Classification of Tumours of Lung, Pleura, Thymus and Heart. Lyon: IARC Press (2015). p. 101–2.
5. Ishikawa Y, Dacic S, Husain AN, Nicholson AG. Salivary gland-type tumours. Epithelial-myoepithelial carcinoma. In: Travis WD, Brambilla E, Burke AP, Marx A, Nicholson AG, editors. WHO Classification of Tumours of Lung, Pleura, Thymus and Heart. Lyon: IARC Press (2015). p. 103–4.
6. VanderLaan PA, Wang HH, Majid A, Folch E. Endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA): an overview and update for the cytopathologist. Cancer Cytopathol (2014) 122:561–76. doi:10.1002/cncy.21431
7. Kim S, Chu J, Kim H, Han J. Comprehensive cytomorphologic analysis of pulmonary adenoid cystic carcinoma: comparison to small cell carcinoma and non-pulmonary adenoid cystic carcinoma. J Pathol Transl Med (2015) 49:511–9. doi:10.4132/jptm.2015.09.07
8. Simpson RHW, Skálová A, Di Palma S, Leivo I. Recent advances in the diagnostic pathology of salivary carcinomas. Virchows Arch (2014) 465:371–84. doi:10.1007/s00428-014-1639-x
9. Tao LC, Robertson DI. Cytologic diagnosis of bronchial mucoepidermoid carcinoma by fine needle aspiration biopsy. Acta Cytol (1978) 22:221–4.
10. Lozowski MS, Mishriki Y, Solitare GB. Cytopathologic features of adenoid cystic carcinoma. Case report and literature review. Acta Cytol (1983) 27:317–22.
12. Buchanan AJ, Fauck R, Gupta RK. Cytologic diagnosis of adenoid cystic carcinoma in tracheal wash specimens. Diagn Cytopathol (1988) 4:130–2. doi:10.1002/dc.2840040210
13. Gupta RK, McHutchison AG. Cytologic findings of adenoid cystic carcinoma in a tracheal wash specimen. Diagn Cytopathol (1992) 8:196–7. doi:10.1002/dc.2840080222
14. Brooks B, Baandrup U. Peripheral low-grade mucoepidermoid carcinoma of the lung – needle aspiration cytodiagnosis and histology. Cytopathology (1992) 3:259–65. doi:10.1111/j.1365-2303.1992.tb00516.x
15. Radhika S, Dey P, Rajwanshi A, Guleria R, Bhusnurmath B. Adenoid cystic carcinoma in a bronchial washing. A case report. Acta Cytol (1993) 37:97–9.
16. Segletes LA, Steffee CH, Geisinger KR. Cytology of primary pulmonary mucoepidermoid and adenoid cystic carcinoma. A report of four cases. Acta Cytol (1999) 43:1091–7. doi:10.1159/000331358
17. Delpiano C, Claren R, Sironi M, Cenacchi G, Spinelli M. Cytological appearance of papillary mucous gland adenoma of the left lobar bronchus with histological confirmation. Cytopathology (2000) 11:193–6. doi:10.1046/j.1365-2303.2000.00243.x
18. Romagosa C, Morente V, Ramirez JF, Esteve R, Alos L, Cardesa A, et al. Intranuclear inclusions in fine needle aspirates of bronchial low grade mucoepidermoid carcinoma with clear cell change: a report of two cases. Acta Cytol (2002) 46:57–60. doi:10.1159/000326717
19. Qiu S, Nampoothiri MM, Zaharopoulos P, Logrono R. Primary pulmonary adenoid cystic carcinoma: report of a case diagnosed by fine-needle aspiration cytology. Diagn Cytopathol (2004) 30:51–6. doi:10.1002/dc.10422
20. Florentine BD, Fink T, Avidan S, Braslavski D, Raza A, Cobb CJ. Extra-salivary gland presentations of adenoid cystic carcinoma: a report of three cases. Diagn Cytopathol (2006) 34:491–4. doi:10.1002/dc.20500
21. Chuah KL, Lim KH, Koh MS, Tan HW, Yap WM. Diagnosis of adenoid cystic carcinoma of the lung by bronchial brushing: a case report. Acta Cytol (2007) 51:563–6. doi:10.1159/000325795
22. Daneshbod Y, Modjtahedi E, Atefi S, Bedayat GR, Daneshbod K. Exfoliative cytologic findings of primary pulmonary adenoid cystic carcinom: a report of 2 cases with a review of the cytologic features. Acta Cytol (2007) 51:558–62. doi:10.1159/000325794
23. Özkara SK, Turan G. Fine needle aspiration cytopathology of primary solid adenoid cystic carcinoma of the lung. Acta Cytol (2009) 53:707–10. doi:10.1159/000325416
24. Chon SH, Park YW, Oh YH, Shinn SH. Primary peripheral pulmonary adenoid cystic carcinoma: report of a case diagnosed by fine needle aspiration cytology. Diagn Cytopathol (2011) 39:283–7. doi:10.1002/dc.21409
25. Dyhdalo KS, Chen L. Endobronchial ultrasound-guided fine-needle aspiration cytology of bronchial low-grade mucoepidermoid carcinoma: rapid on-site evaluation of cytopathologic findings. Diagn Cytopathol (2013) 41:1096–9. doi:10.1002/dc.22928
26. Bhalara RV, Gamit MJ, Popat M, Gandhi SH, Dhruva GA. Cytomorphology of primary adenoid cystic carcinoma of the lung: an exceedingly rare case. Ann Pathol Lab Med (2015) 2:511–9.
27. Hara H, Oyama T, Suda K. New criteria for cytologic diagnosis of adenoid cystic carcinoma. Acta Cytol (2005) 49:43–50. doi:10.1159/000326094
28. Molina JR, Aubry MC, Lewis JE, Wampfler JA, Williams BA, Midthun DE, et al. Primary salivary gland-type lung cancer: spectrum of clinical presentation, histopathologic and prognostic factors. Cancer (2007) 110:2253–9. doi:10.1002/cncr.23048
29. Zhu F, Liu Z, Hou Y, He D, Ge X, Bai C, et al. Primary salivary gland-type lung cancer: clinicopathological analysis of 88 cases from China. J Thorac Oncol (2013) 8:1578–84. doi:10.1097/JTO.0b013e3182a7d272
30. Fischer B, Arcaro A. Current status of clinical trials for small cell lung cancer. Rev Recent Clin Trials (2008) 3:40–61. doi:10.2174/157488708783330503
31. Vadasz P, Egervary M. Mucoepidermoid bronchial tumors: a review of 34 operated cases. Eur J Cardiothorac Surg (2000) 17(5):566–9. doi:10.1016/S1010-7940(00)00386-9
32. Liu X, Adams AL. Mucoepidermoid carcinoma of the bronchus: a review. Arch Pathol Lab Med (2007) 131:1400–4. doi:10.1043/1543-2165(2007)131[1400:MCOTBA]2.0.CO;2
33. Cwierzyk TA, Glasberg SS, Virshup MA, Cranmer JC. Pulmonary oncocytoma. Report of a case with cytologic, histologic and electron microscopic study. Acta Cytol (1985) 29:620–3.
34. Roden AC, Garcia JJ, Wehrs RN, Colby TV, Khoor A, Leslie KO, et al. Histopathologic, immunophenotypic and cytogenetic features of pulmonary mucoepidermoid carcinoma. Mod Pathol (2014) 27:1479–88. doi:10.1038/modpathol.2014.72
35. Huo Z, Wu H, Li J, Li S, Wu S, Liu Y, et al. Primary pulmonary mucoepidermoid carcinoma: histopathological and moleculargenetic studies of 26 cases. PLoS One (2015) 10:e0143169. doi:10.1371/journal.pone.0143169
36. Nicholson AG, Beasley MB, Travis WD. Mucous gland adenoma. In: Travis WD, Brambilla E, Burke AP, Marx A, Nicholson AG, editors. WHO Classification of Tumours of the Lung, Pleura, Thymus and Heart. Lyon: IARC Press (2015). 115 p.
37. Alvarez-Fernandez E, Dacic S, Ishikawa Y, Nicholson AG. Salivary gland-type tumours. Pleomorphic adenoma. In: Travis WD, Brambilla E, Burke AP, Marx A, Nicholson AG, editors. WHO Classification of Tumours of the Lung, Pleura, Thymus and Heart. Lyon: IARC Press (2015). 105 p.
38. Fishbein GA, Grimes BS, Xian RR, Lee JM, Barjaktarevic I, Xu H. Primary salivary duct carcinoma of the lung, mucin-rich variant. Hum Pathol (2016) 47:150–6. doi:10.1016/j.humpath.2015.09.011
39. Sethi R, Kozin E, Remenschneider A, Meier J, VanderLaan P, Faquin WC, et al. Mammary analogue secretory carcinoma: update on a new diagnosis of salivary gland malignancy. Laryngoscope (2014) 124:188–95. doi:10.1002/lary.24254
40. Bishop JA, Yonescu R, Batista D, Begum S, Eisele DW, Westra WH. Utility of mammaglobin immunohistochemistry as a proxy marker for the ETV6-NTRK3 translocation in the diagnosis of salivary mammary analogue secretory carcinoma. Hum Pathol (2013) 44:1982–8. doi:10.1016/j.humpath.2013.03.017
41. Skálová A, Vanecek T, Sima R, Laco J, Weinreb I, Perez-Ordonez B, et al. Mammary analogue secretory carcinoma of salivary glands, containing the ETV6-NTRK3 fusion gene: a hitherto undescribed salivary gland tumor entity. Am J Surg Pathol (2010) 34:599–608. doi:10.1097/PAS.0b013e3181d9efcc
42. Roden AC, Greipp PT, Knutson DL, Kloft-Nelson SM, Jenkins SM, Marks RS, et al. Histopathologic and cytogenetic features of pulmonary adenoid cystic carcinoma. J Thorac Oncol (2015) 10(11):1570–5. doi:10.1097/JTO.0000000000000656
43. Tonon G, Modi S, Wu L, Kubo A, Coxon AB, Komiya T, et al. t(11;19)(q21;p13) translocation in mucoepidermoid carcinoma creates a novel fusion product that disrupts a Notch signaling pathway. Nat Genet (2003) 33:208–13. doi:10.1038/ng1083
44. Nakayama T, Miyabe S, Okabe M, Sakuma H, Ijichi K, Hasegawa Y, et al. Clinicopathological significance of the CRTC3-MAML2 fusion transcript in mucoepidermoid carcinoma. Mod Pathol (2009) 22:1575–81. doi:10.1038/modpathol.2009.126
45. Brill LB II, Kanner WA, Fehr A, Andren Y, Moskaluk CA, Loning T, et al. Analysis of MYB expression and MYB-NFIB gene fusions in adenoid cystic carcinoma and other salivary neoplasms. Mod Pathol (2011) 24:1169–76. doi:10.1038/modpathol.2011.86
46. Pusztaszeri MP, Faquin WC. Update in salivary gland cytopathology: recent molecular advances and diagnostic applications. Semin Diagn Pathol (2015) 32:264–74. doi:10.1053/j.semdp.2014.12.008
47. Pusztaszeri MP, Sadow PM, Ushiku A, Bordignon P, McKee TA, Faquin WC. MYB immunostaining is a useful ancillary test for distinguishing adenoid cystic carcinoma from pleomorphic adenoma in fine-needle aspiration biopsy specimens. Cancer Cytopathol (2014) 122:257–65. doi:10.1002/cncy.21381
48. Foo WC, Jo VY, Krane JF. Usefulness of translocation-associated immunohistochemical stains in the fine-needle aspiration diagnosis of salivary gland neoplasms. Cancer Cytopathol (2016) 124:397–405. doi:10.1002/cncy.21693
49. Macarenco RS, Uphoff TS, Gilmer HF, Jenkins RB, Thibodeau SN, Lewis JE, et al. Salivary gland-type lung carcinoma: an EGFR immunohistochemical, molecular genetic, and mutational analysis study. Mod Pathol (2008) 21:1168–75. doi:10.1038/modpathol.2008.113
Keywords: cytology, lung, salivary gland-type tumors, mucoepidermoid carcinoma, adenoid cystic carcinoma
Citation: Saglietti C, Volante M, La Rosa S, Letovanec I, Pusztaszeri M, Gatti G and Bongiovanni M (2017) Cytology of Primary Salivary Gland-Type Tumors of the Lower Respiratory Tract: Report of 15 Cases and Review of the Literature. Front. Med. 4:43. doi: 10.3389/fmed.2017.00043
Received: 02 February 2017; Accepted: 05 April 2017;
Published: 24 April 2017
Edited by:
Luca Di Tommaso, Humanitas Research Hospital, ItalyReviewed by:
Fernando Schmitt, Porto University, PortugalCopyright: © 2017 Saglietti, Volante, La Rosa, Letovanec, Pusztaszeri, Gatti and Bongiovanni. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Massimo Bongiovanni, bWFzc2ltby5ib25naW92YW5uaUBjaHV2LmNo
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.