
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
REVIEW article
Front. Mater. , 03 July 2024
Sec. Biomaterials and Bio-Inspired Materials
Volume 11 - 2024 | https://doi.org/10.3389/fmats.2024.1420900
Parts of this article's content have been modified or rectified in:
Erratum: The current status and trends of oral bone regeneration materials: a bibliometric analysis from 1991 to 2023
 Ronglin Tu1,2†
Ronglin Tu1,2† Xiaoming Liu1,3†
Xiaoming Liu1,3† Lin Xu1,3†
Lin Xu1,3† Xuemin Yao1,3
Xuemin Yao1,3 Ran Zhang1,3
Ran Zhang1,3 Jiadi Li1,3
Jiadi Li1,3 Wenjun Zhang1,3
Wenjun Zhang1,3 Jinrong Liu1,3
Jinrong Liu1,3 Xiuping Wu1,3*
Xiuping Wu1,3* Bing Li1,3*
Bing Li1,3*Objectives: Due to the complexity and importance of oral bone structure, oral bone regeneration materials differ from those used in other parts of the body. To study the research trends and hotspots of oral bone regeneration materials, this paper conducts a bibliometric analysis of related papers from 1991 to 2023 (retrieved on 27 September 2023).
Materials and methods: Using bibliometric methods, two visualization metric software, Citespace and VOSviewer, were used to analyze 1217 papers in SCIE, including paper analysis, author analysis, country and institution analysis, keyword analysis, and cited literature analysis.
Results: ① The number of papers is generally increasing and gradually stabilizing; ② Buser D is the most influential author, while Jung, Ronald E has the highest number of papers and total citations; ③ The United States has the highest number of papers and citation frequency. The University of Bern and the University of Zurich in Switzerland are not only the institutions with the most papers, but also the institutions with the most collaborations with other institutions. ④ Many research directions have persisted for decades since their inception. The field of oral bone; regeneration materials is constantly developing and improving. In recent years, the research direction in this field may mainly focus on the role of blood cells and proteins in bone regeneration. ⑤ In recent years, the types of cited literature mainly include barrier membranes, alveolar ridge augmentation, bone graft materials, histological examination, and in vivo animal experimental models.
Conclusion: The United States and Switzerland have a significant influence in the field of oral bone regeneration materials. The research hotspot in recent years is mainly on tissue engineering materials. However, traditional materials still occupy a large proportion in clinical treatment or research. In addition, the combined use of new and old materials has gradually become one of the research hotspots in this field.
The oral bone structure, mainly composed of the upper and lower jawbones, includes the upper and lower alveolar bones. These bones play an important role in the oral maxillofacial structure, supporting the form and function of the oral cavity and face, and also forming a complex skeletal system. The maxilla is connected to the upper alveolar bone, and the mandible is connected to the lower alveolar bone, providing support and fixation for the teeth. The connection of the upper and lower jawbones also allows normal occlusion of the oral cavity. The anatomical structure of the oral maxillofacial area is very complex, and bone defects caused by trauma, tumors, and inflammation in these areas are extremely difficult to repair (Xia et al., 2021; Alavi et al., 2023). After severe diseases and injuries, their bone regeneration ability will weaken (Wagner et al., 2019). Therefore, alveolar bone deficiency caused by trauma, infection, deformity or systemic disease, jawbone defect repair has always been a focus of attention in the field of oral medicine (Gallego et al., 2010). There are many materials currently used for oral bone regeneration, but no material has been found that can completely replace the original healthy bones. Traditional bone defect repair methods include autologous bone grafting, allograft bone grafting, and artificial synthetic materials, but these methods have certain limitations. Due to the complexity and importance of oral bones, oral bone regeneration materials differ from bone regeneration materials in other parts (Tang et al., 2021; Wang et al., 2022; Zhang et al., 2022). At present, there are few bibliometric papers on the current status and trends of research on oral bone regeneration materials, and people’s understanding of the research trends and current status of oral bone regeneration materials is not clear enough. Therefore, in order to study the research trends and research hotspots of oral bone regeneration materials, this paper conducts a bibliometric analysis of related papers on oral bone regeneration materials from 1991 to 2023 (retrieved on 27 September 2023).
Bibliometrics is a scientific research method that quantitatively analyzes a large number of documents and their related data (such as authors, keywords, citations, etc.) to reveal the historical development process and future trends of a specific academic field. This method has a wide range of applications, including but not limited to scientific research evaluation, knowledge structure analysis, scientific cooperation network analysis, etc (Ge et al., 2022). The visualization tools CiteSpace and VOSviewer software were initially widely used in their origin map library and information science with good results. Therefore, they are increasingly used in different fields. These visualization tools can make full use of various data in publications for scientific mapping, making the process and results of bibliometric analysis clearer and easier to obtain (Pan et al., 2018). In the past few decades, researches and papers on oral bone regeneration materials have gradually increased. Traditional reviews can no longer fully understand the current status of research in this field. Therefore, this paper analyzes core papers on oral bone regeneration materials from 1991 to 2023 to understand the current status and trends of research in this field and provide effective reference materials for subsequent research. At the same time we will answer the following questions:
(1) Who are the authors, institutions, countries that have published research on oral bone regeneration materials? What is their relationship?
(2) What are the high-frequency keywords in the field of oral bone regeneration material research? What are the burst keywords?
(3) What are the hotspots and trends in research in the field of oral bone regeneration materials?
This study retrieved from the Web of Science database Web of Science Core Collection (WoSCC), and for the sake of precision, this study also selected SCIE as the index for retrieval. The system retrieved publications on oral bone regeneration materials from 1991 to 2023, with the retrieval time being 27 September 2023. The following search terms were used: (TS=(Bone Regeneration OR Osteoconduction)) AND TS=(“Material”) AND (TS=(Mandible OR Maxilla OR Mouth OR Stomatognathic System OR Alveolar Bone)). The literature retrieved was filtered through the WOS document type filter, with no language restrictions, A total of 1221 results were retrieved in this process. After the editorial material, note, and early access among them have been excluded, a total of 1,217 papers were finally included. These papers were from 66 countries, 1,364 institutions, and 5,322 authors, citing 28207 pieces of literature. The filtering process is shown in Figure 1.
We used CiteSpace (version 6.1.R6) and VOSviewer (version 1.6.19) software for bibliometric analysis. Research shows that VOSviewer and CiteSpace are the two most commonly used bibliometric tools at present. In addition, VOSviewer has advantages such as easy operation, beautiful pictures, and it is free. CiteSpace has some functions that other software does not have, such as detecting explosive citations of a certain paper in a certain year and presenting the dual map overlay of journals (Pan et al., 2018). From the WoS database, we obtained the annual publication quantity and annual citation times of publications on oral bone regeneration materials from 1991 to 2023. We used VOSviewer to calculate the top 11 most productive authors and the top 10 most productive institutions and countries, and constructed a clustering diagram of cited authors, institutions, and countries. By using the author, country, and institution statistics functions of VOSviewer, as well as the co-occurrence functions of collaboration networks among high-yield authors, countries, and institutions, we have compiled some information about the high-yield authors and countries in the field of oral bone regeneration, as well as their collaboration status. Then, we displayed the clustering results of keywords appearing more than 10 times through the VOSviewer’s keyword clustering function, where one node represents one keyword, and the larger the node, the more frequently the keyword appears (van Eck and Waltman, 2010). CiteSpace was used to create a time zone map of keywords, co-cited reference literature, and cluster visualization maps, and cluster analysis was conducted using the LLR algorithm (displaying cluster labels with log-likelihood ratio). In these maps, one node represents an object, different colors represent different years or clusters. In addition, CiteSpace was also used to create journal double overlay maps. This function presents the citation and cited situation of journals in different fields, thereby showing the contributions of all research fields to our research field. The size of the node reflects the number of times a keyword appears or is cited. The thicker and shorter the connection line, the closer the relationship between different nodes (Chen, 2017).
Between 1991 and 2023, we collected a total of 1217 articles related to oral bone regeneration materials. Overall, both the annual number of publications and the annual number of citations showed an upward trend (Figure 2). These 33 years can be roughly divided into three stages. The first stage is from 1991 to 2012. Although the number of publications in some years during this period declined compared to the previous year, the overall trend was upward. In addition, the number of citations in this stage increased rapidly, indicating that the research field was gradually maturing. The second stage is from 2013 to 2018, during which the number of publications was relatively stable, which may indicate that a stable group of publications had formed in this field. The third stage is from 2019 to 2023. Notably, both the number of publications and citations increased significantly in 2019, with increases of 51.73% and 64.91% respectively compared to 2018. However, starting from 2020, the number of publications declined sharply. Some studies have shown that this phenomenon is to some extent due to the impact of the COVID-19 pandemic, especially in 2020, when many scientists, particularly female scientists who needed to take care of their families and children, saw a significant decline in their research output (Gao et al., 2021; Heo et al., 2022). Over these 3 years from 2020 to 2022, as the number of publications increased, the number of citations also reached its peak in 2022. This may indicate that research in this field is gradually maturing.
In this study, we analyzed the authors of papers related to oral bone regeneration materials. Among these authors, 11 authors published more than 12 papers, and their total citations and average citations are shown in Table 1. Among them, Jung, Ronald E has the highest number of publications and total citations, while Buser, Daniel has the highest average citations (about 75.78 times per publication). All these authors have a high frequency of average citations per paper, indicating that the quality of the articles on oral bone regeneration materials published by these high-volume authors is relatively high. We also conducted a cluster analysis of the cited authors in the field of oral bone regeneration materials from 1991 to 2023 (Figure 3). The results show that the cited authors were divided into 5 clusters. Since the research directions of the authors in each cluster are similar or highly related, we can see from the figure which high-output authors are in each field. Among them, Buser D is the most influential author. In addition, we also drew a collaboration network diagram of 77 authors who published more than 5 papers in the field of oral bone regeneration materials from 1991 to 2023 (Figure 4). The results show that most of these authors have a cooperative relationship, and they started to cooperate early.
In this study, we analyzed papers from 66 countries. As shown in Table 2, the United States has the highest number of publications and citations, with 239 papers and 9,349 citations respectively. Among the 66 countries with the most publications, 60 countries have cooperative relationships. The color of the lines connecting the nodes in the figure shows that these countries’ collaborations mainly concentrated around 2013 (Figure 5). Among them, the United States, Switzerland, Italy, Germany, and China are the five countries with the most collaborations with other countries. And we believe that collaboration between scientists from different countries can access more resources and innovative ideas, thereby promoting the development of a research field. For example, scientists from Beijing, China, and Zurich, Switzerland, used cone-beam computed tomography to assess the size changes in radiographs after tooth extraction using alveolar ridge preservation techniques or natural healing. In a study lasting half a year, patients were divided into two groups: one group was the test group using deproteinized bovine bone mineral (DBBM) with 10% collagen (DBBM-C) covered with a native bilayer collagen membrane (NBCM), and the other group was the self-healing control group. The results showed that the alveolar ridge preservation technique using DBBM-C covered with NBCM is an effective method that can reduce the radiographic loss of alveolar ridge size (Jung et al., 2018). In 2019, a collaborative study by scientists from Germany, the United States, and Spain showed that peri-implant inflammation often leads to buccal bone loss, providing new considerations for the clinical treatment of peri-implant inflammation (Monje et al., 2019). In addition, a collaborative study by scientists from the United States, China, and Japan showed that the composite scaffold of hydrogel/hydroxyapatite has the potential to maintain alveolar bone regeneration and promote soft tissue healing. Therefore, the future use of a hydrogel platform containing hydroxyapatite may become an effective method to promote the regeneration of bone tissue and soft tissue. These studies fully demonstrate the value of international scientific collaboration (Pan et al., 2020).
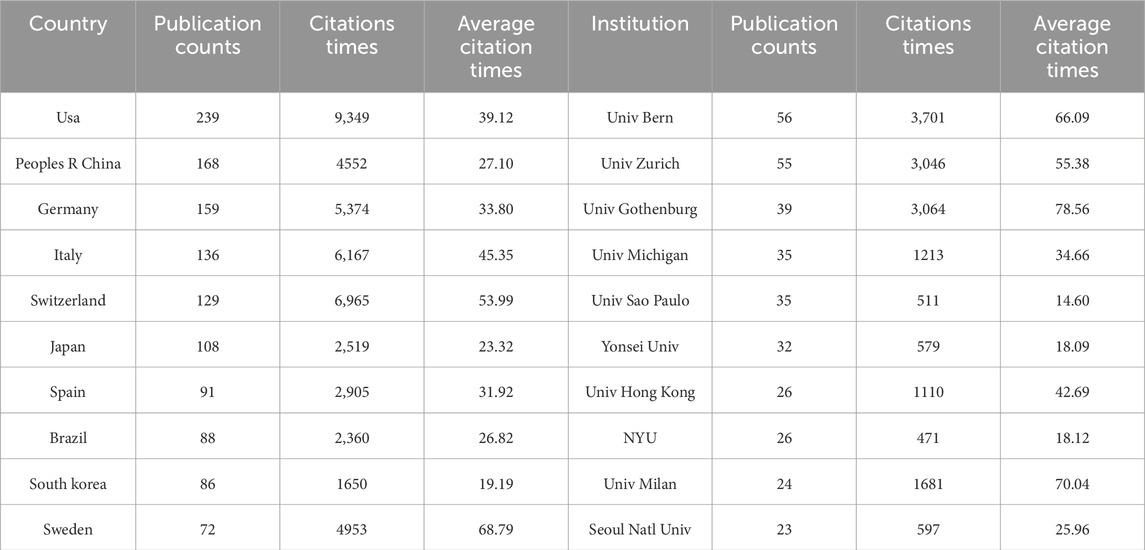
Table 2. Top 10 countries and institutions contributing the most to the field of dental bone regeneration materials.
In addition, we also analyzed 133 institutions that published more than five papers. As shown in Table 2, the University of Bern has the highest number of publications and citations, and its average number of citations is also among the top. The University of Gothenburg has the highest average number of citations per paper. Among these 133 institutions, 130 institutions have cooperative relationships, and these cooperative relationships almost all started a decade ago (Figure 6). Among them, the University of Bern and the University of Zurich in Switzerland are not only the institutions with the most publications but also the institutions with the most collaborations with other institutions. This may indicate that Switzerland is at the forefront in the field of oral bone regeneration materials research and has a huge influence.
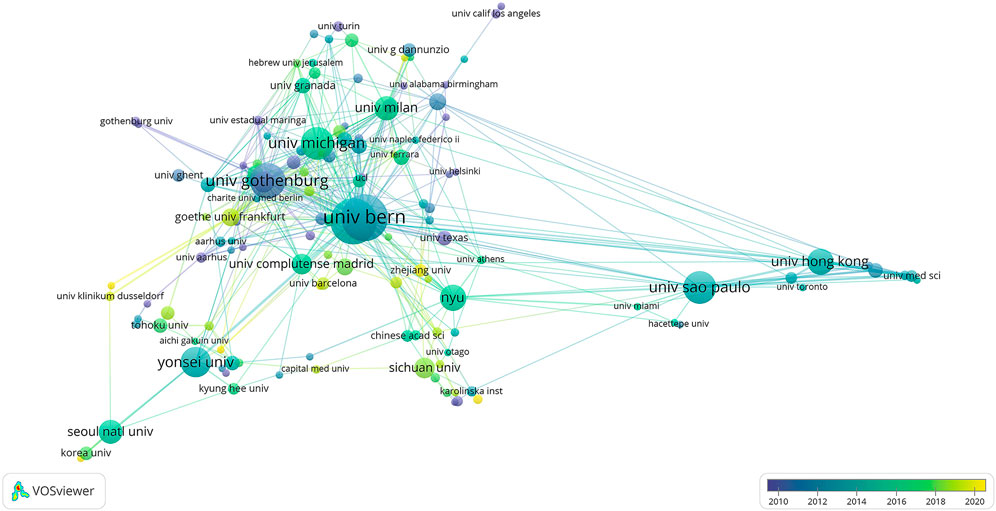
Figure 6. Network of institutions in the field of dental bone regeneration materials from 1991 to 2023.
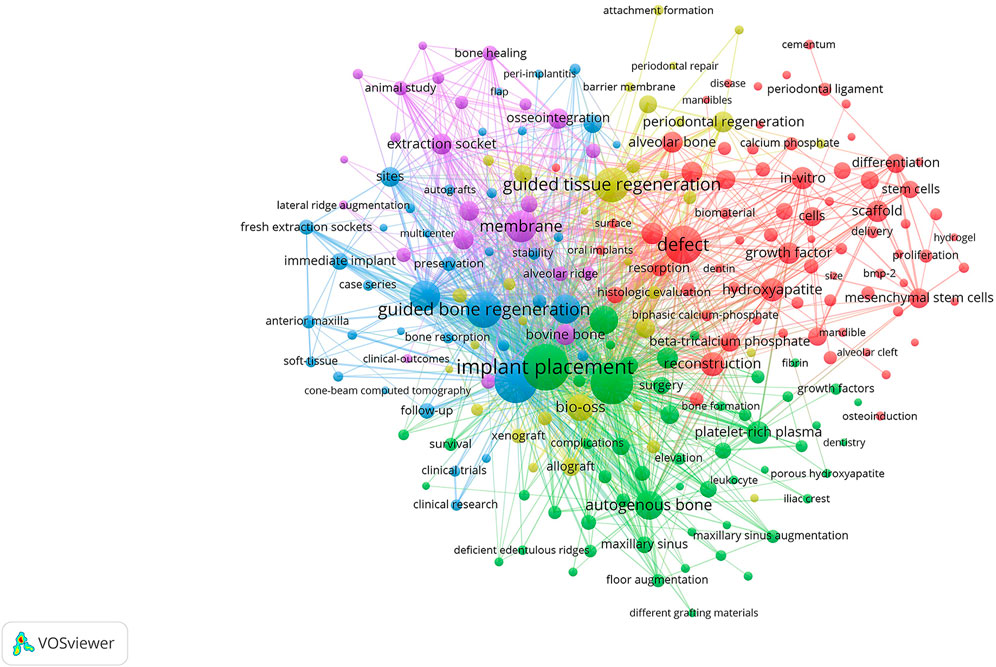
Figure 7. Cluster map of keywords in the field of oral bone regeneration materials from 1991 to 2023.
In this study, we analyzed keywords that appeared more than 10 times, totaling 264. After merging synonyms and removing meaningless words using VOSviewer, 220 keywords remained. We found that the keywords with the largest nodes, highest density, and highest frequency included “dental implant”, “guided bone regeneration”, “guided tissue regeneration”, “defect”, “autologous bone”, “implant placement”, etc., which are closely related to the theme of this study. After performing cluster analysis using VOSviewer, we found that these keywords can be divided into 5 natural clusters (Figure 7). The theme of the first cluster is “guided bone regeneration”, which includes keywords such as “guided bone regeneration”, “dental implant”, “tooth extraction”, etc. The theme of the second cluster is “implant placement”, which includes keywords such as “implant”, “bone graft”, “autologous bone”, etc. The theme of the third cluster is “defect”, with high-frequency keywords such as “hydroxyapatite”, “growth factors”, “alveolar ridge augmentation”, etc. The theme of the fourth cluster is “guided tissue regeneration”, with high-frequency keywords such as “allograft”, “BIO-OSS”, “freeze-dried allograft bone”, etc. The theme of the fifth cluster is “membrane”, including “barrier membrane”, “bovine bone”, etc. From the clustering results, there is less overlap between clusters 1 to 3, indicating that the research directions in these fields are clearly divided. Clusters 4 and 5 overlap more with other clusters, indicating more cross-research in these fields. These results provide us with a deep understanding of the research field of oral bone regeneration materials and reveal the research trends and hotspots in this field.
The keyword time zone map of CiteSpace is a unique analytical tool that incorporates the factor of time into keyword analysis. By analyzing “time slices”, we can observe the evolution of the research field. In the keyword time zone map, each node represents a keyword, and the size of the node reflects the frequency of the keyword. The more rings on a node, the more years the keyword appears, and rings of different colors represent different years. In addition, the lines represent the relationships between different nodes, and the thicker the line, the closer the relationship between the nodes (Chen, 2006). As shown in Figure 8, most high-frequency keywords have continued to appear since their emergence, and the connections between these keywords are quite close. This finding reveals that many research directions have continued for decades since their emergence, and also reflects that research in the field of oral bone regeneration materials is constantly developing and improving.
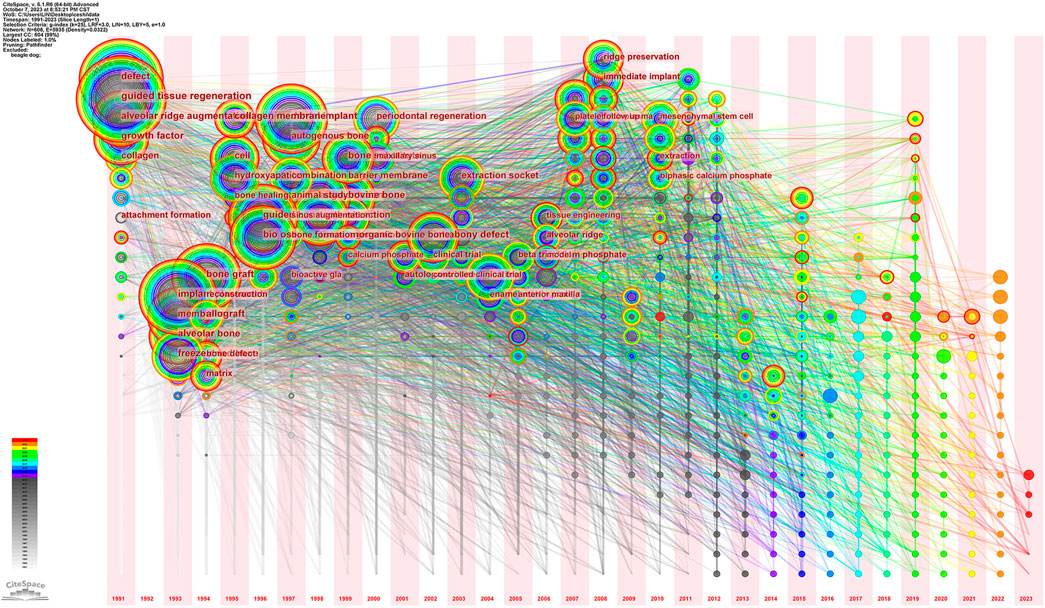
Figure 8. Time zone map of keywords in the field of dental bone regenerative materials from 1991 to 2023.
Burst word analysis is a method that extracts keywords with significant changes within a unit time by examining keyword frequency from a large number of subject words (Chen et al., 2014). In order to deeply understand the research hotspots and trends in the field of oral bone regeneration materials, and to some extent predict future development trends, we used the burst word analysis function of CiteSpace for in-depth analysis in this study. Figure 9 shows the 25 keywords with the highest burst strength in the field of oral bone regeneration materials from 1991 to 2023, these keywords are sorted according to the start time of the burst. Among them, “guided tissue regeneration” is the keyword with the largest burst strength, the earliest start time, and the longest duration. In addition, the three keywords “guided tissue regeneration”, “defects”, and “adhesion formation” appear almost every year. Notably, “alveolar ridge preservation”, “scaffold”, “platelet-rich fibrin”, “xenotransplantation”, “bone morphogenetic protein”, “platelet-rich plasma”, and “leukocytes” are the seven keywords with the highest burst strength that have burst in recent years and continue to this day. This may indicate that the research direction in this field in recent years may mainly focus on the role of blood cells and proteins in bone regeneration.
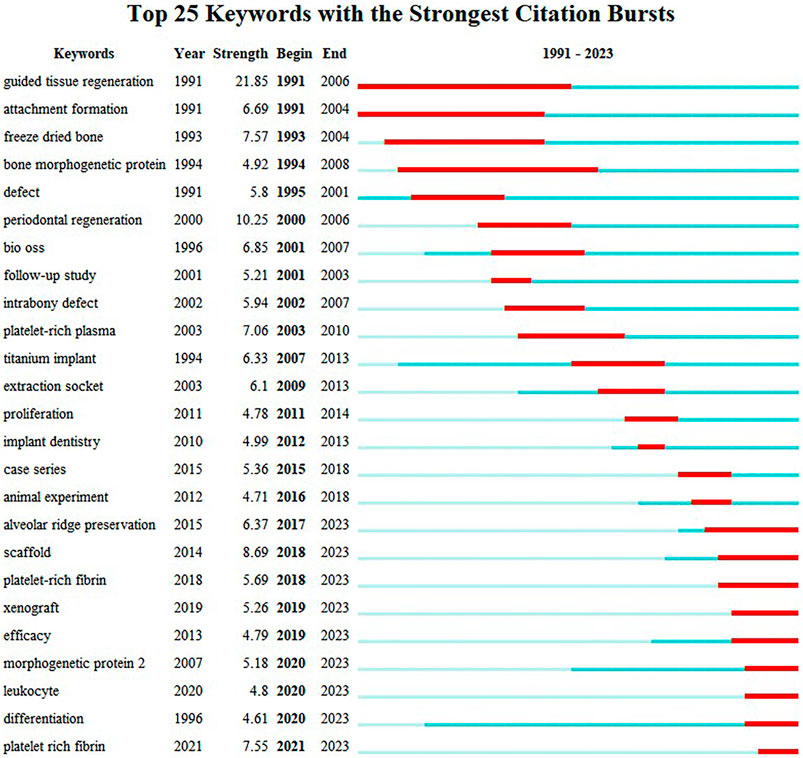
Figure 9. Top 25 breakout words in the field of dental bone regenerative materials from 1991 to 2023.
Cited literature forms the foundation of a field of study, and can thus be considered the knowledge base, while the citing literature is referred to as the knowledge Frontier. Figure 10 shows the dual-map overlay of journals in the field of oral bone regenerative materials (1991-2023). In this figure, we can see that the citing literature journals mainly involve the fields of dentistry and surgery. The cited literature journals mainly come from three fields: (Alavi et al., 2023): Dentistry and Surgery; (Xia et al., 2021); Molecular Biology, Genetics; (Wagner et al., 2019); Chemistry, Materials Science, Physics. The intersection and integration of these fields provide a rich knowledge base for the research of oral bone regenerative materials. This figure indicates that the main research in the field of oral bone regenerative materials is still concentrated in the field of dentistry and surgery. However, interdisciplinary research with molecular biology, genetics, as well as chemistry, materials science, physics and other fields is also increasing, which may indicate that future research in this field will be more in-depth and extensive.
The co-occurrence and clustering networks of the cited literature are shown in Figures 11A, B. In these figures, the larger the size of the node, the more times the literature is cited. The more rings a node has, the longer the literature has been cited. If a piece of literature is cited many times in a particular year, that year’s ring will be displayed in red. From left to right, the start time of citation is getting later and later. From the clustering diagram of cited literature, it can be seen that the main cited literature each year is distributed among articles of multiple categories. Most nodes of highly cited literature are almost entirely red, indicating that these pieces of literature are cited multiple times each year over several consecutive years. In recent years, the types of cited literature mainly include barrier membranes, alveolar ridge augmentation, bone graft materials, histological examinations, and live animal experimental models, etc.
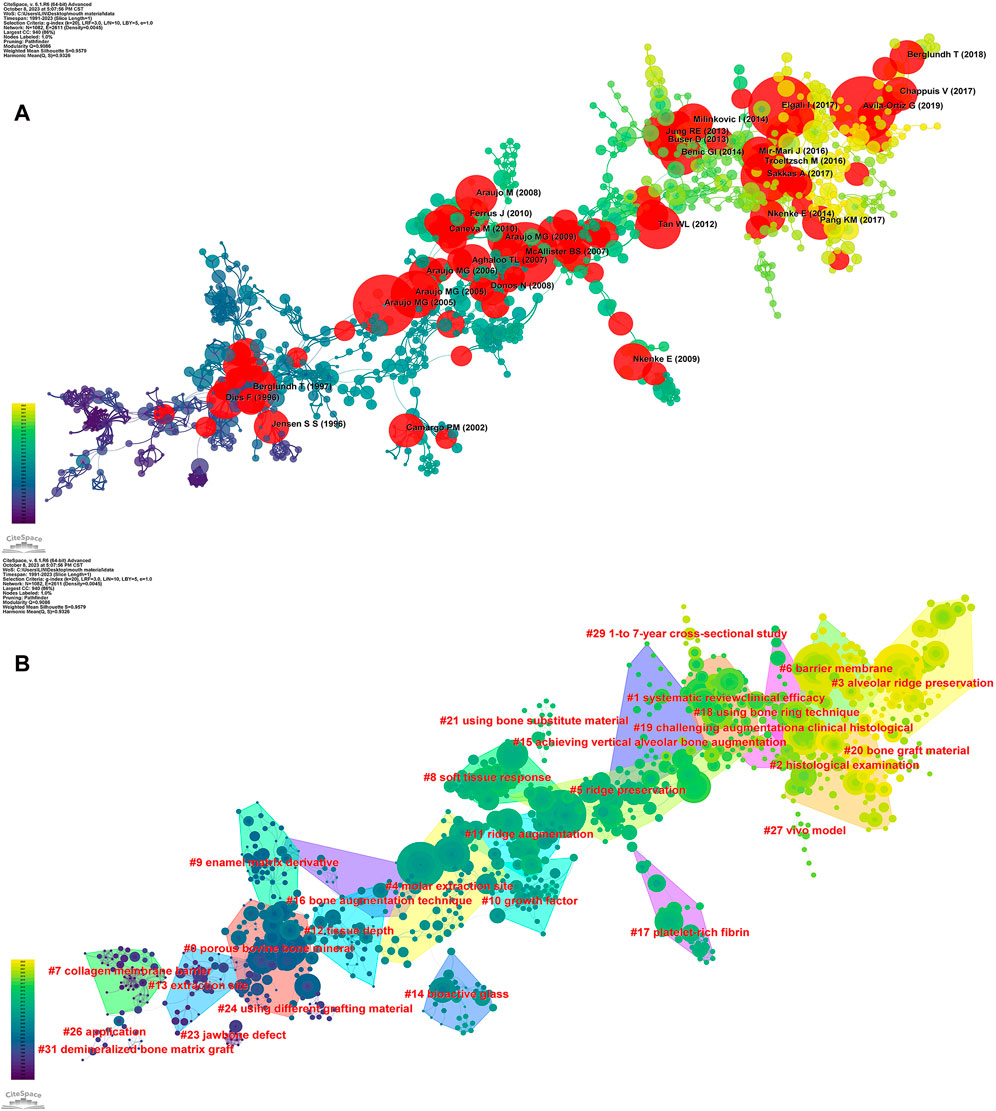
Figure 11. The field of dental bone regeneration materials 1991-2023 (A) literature co-citation co-occurrence map (B) literature co-citation cluster map.
Figure 12 shows the top 25 pieces of literature with the highest burst intensity. Among them, the literature with the highest intensity is a paper published by Gustavo Avila-Ortiz in the Journal of Clinical Periodontology in 2019, titled “Effect of alveolar ridge preservation interventions following tooth extraction: A systematic review and meta-analysis”. This article by Avila-Ortiz mainly compares the effects of different modes of Alveolar Ridge Preservation (ARP) and simple tooth extraction on relevant clinical, radiographic, and patient-centered outcomes (Avila-Ortiz et al., 2019). This study provides us with a deep understanding of the effects of post-extraction alveolar ridge preservation interventions.
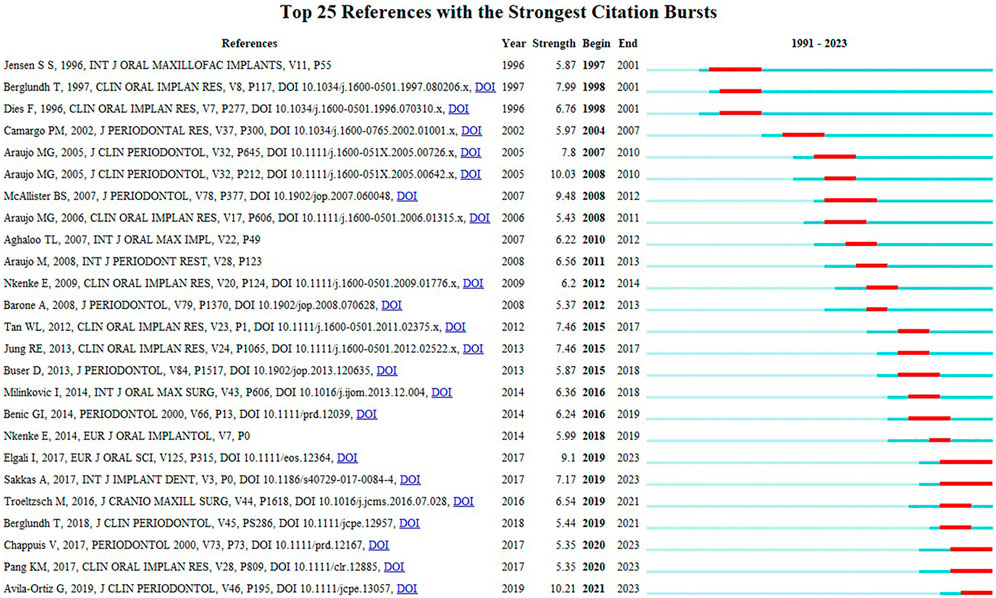
Figure 12. The top 25 most explosively cited articles in the field of oral bone regeneration materials from 1991 to 2023.
In recent years, the following literature has been explosively cited in the field of oral bone regeneration materials. In the article “Guided bone regeneration: materials and biological mechanisms revisited” published in 2017, Elgali I and others pointed out that whether or not there are implants, GBR membranes can promote tissue regeneration. This proves that in the process of tissue regeneration, the membrane itself plays an active role in promoting the regeneration process in the underlying defects, rather than just being a passive barrier (Elgali et al., 2017). In the same year, Sakkas, A and others mentioned in the article “Autogenous bone grafts in oral implantology—is it still a “gold standard”? A consecutive review of 279 patients with 456 clinical procedures” that clinical research results have proven the reliability and low comorbidity of autogenous bone grafting in anterior alveolar ridge reconstruction before implant placement, and the predictability of autogenous bone materials in alveolar ridge reconstruction before implant placement. Therefore, autogenous bone grafting is still the “gold standard” for alveolar ridge enhancement before oral implantation (Sakkas et al., 2017). Troeltzsch, M and others pointed out in the article “Clinical efficacy of grafting materials in alveolar ridge augmentation: A systematic review” published in 2017 that about 80% satisfactory defect filling can be achieved in peri-implant split defects using graft materials. However, in terms of vertical gain, although the use of isolation materials such as titanium mesh can significantly improve vertical gain, the possibility and severity of complications will also increase accordingly. Only when autogenous block grafts from extra-oral donor sites are used can block grafting significantly increase vertical gain compared to using granular materials alone (Troeltzsch et al., 2016). In 2018, Berglundh, T published “Peri-implant diseases and conditions: Consensus report of workgroup 4 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions” in the Journal of periodontology. The report proposed a classification of peri-implant diseases and conditions, discussed key issues such as peri-implant health characteristics, peri-implant mucositis, peri-implantitis, and soft tissue and hard tissue defects, and provided several suggestions for oral doctors in clinical treatment (Berglundh et al., 2018). In 2017, Chappuis, V and others published an article “Clinical relevance of dimensional bone and soft tissue alterations post-extraction in esthetic sites”, which summarized the degree of tissue changes at single extraction sites in the upper anterior teeth and identified relevant regulatory factors to help clinicians choose the most suitable treatment plan and achieve satisfactory cosmetic treatment results (Chappuis et al., 2017). The article “Comparable responses of osteoblast lineage cells to microstructured hydrophilic titanium–zirconium and microstructured hydrophilic titanium” by Lotz, E M et al. elaborates on the importance of hydrophilicity of bone implant materials to osteoblast lineage cells (Lotz et al., 2017).
In oral bone grafting, autogenous bone is considered the “gold standard” in oral implantation because it contains growth factors and osteoblasts that can promote bone regeneration, and it is the patient’s own bone tissue, so there is no rejection reaction. In the article “Autogenous bone grafts in oral implantology—is it still a “gold standard”? A consecutive review of 279 patients with 456 clinical procedures” published by Sakkas, A and others, 273 out of 279 patients successfully achieved the expected treatment goals, so autogenous bone grafting often has the best effect (Sakkas et al., 2017). However, autogenous bone grafting requires surgery to take bone from the patient’s body, which may cause additional pain and infection, and the amount of bone that can be taken is limited. Therefore, allogeneic bone with similar properties to autogenous bone is also a common option for bone grafting (Tang et al., 2021; Zhang et al., 2022). The study by Kloss, FR and others showed that freeze-dried cancellous allogeneic bone blocks have almost the same horizontal and vertical bone gain, bone remodeling rate, and use of autogenous bone in alveolar ridge augmentation (Kloss et al., 2018). Some studies have shown that decalcified freeze-dried allogeneic bone has growth factors that promote bone induction, can aggregate mesenchymal stem cells, and support osteoblast differentiation (Tresguerres et al., 2019). However, allogeneic bones have problems such as insufficient supply and immune rejection (Zhang et al., 2022). Although these problems can be alleviated to some extent by methods such as freezing, decalcification, and sterilization of allogeneic bones, these methods in turn reduce the performance of the graft in terms of bone induction, bone conduction, and mechanics (Tang et al., 2021). Compared with autogenous bones and allogeneic bones, xenogeneic bones have advantages such as wide sourcing, easy access, and similar structure to the patient’s excised bones when structural grafting (Sehn et al., 2015). Among xenogeneic bones, deproteinized bovine bone mineral (DBBM) has been widely used due to its superior performance and low price. The study by de Lange G L and others found that even if only DBBM is used, it can meet the needs of bone regeneration (de lange et al., 2014). Bio-Oss is currently one of the most commonly used xenogeneic bone materials. According to VOSviewer statistics, in the 1217 papers used in this study, Bio-Oss-related keywords appeared as many as 104 times. As early as 1999, Piattelli, M and others’ research showed that Bio-Oss seems to have high biocompatibility and osteoconductivity. It is slowly absorbed in the human body and can be successfully used as a bone substitute in maxillary sinus augmentation surgery (Sartori et al., 2003). But recent research shows that sometimes the use of Bio-Oss is unnecessary. Starch-Jensen, T and others studied that after performing Oral and Maxillofacial Surgery Functional Endoscopic Surgery (OMSFE), whether or not Bio-Oss is used, there is no significant difference in implant treatment results, and patient satisfaction is similar (Starch-Jensen et al., 2023).
However, it should be noted that the applicability of autologous transplantation treatment is limited by the relatively high morbidity of donor sites and the shortage of available grafts, and allogeneic transplantation is also hindered by vascularization problems and host bone tissue integration (Moghadam et al., 2021). Traditional artificial materials, such as bioceramics, bioglasses, and metal materials, often have disadvantages such as low biocompatibility, susceptibility to corrosion, and insufficient mechanical strength (Tang et al., 2021). At this point, bone tissue obtained through bioengineering has become a direction to solve the problem. Bone morphogenetic protein (BMP) and platelet-rich plasma (PRP) are currently more commonly used biological tissue engineering materials (Ho-Shui-Ling et al., 2018). Bone morphogenetic protein has a significant impact on bone and cartilage growth, among which BMP-2 and BMP-7 have been proven to effectively treat bone defects (Sun et al., 2012). And BMP-6 and BMP-9 have also been proven to trigger the differentiation of mesenchymal stem cells (MSCs), to stimulate local bone regeneration of osteoblasts (Tong et al., 2019). Recent research shows that RGD and rhBMP-7 fixed on zirconia scaffolds can improve the biocompatibility and bone regeneration effect of zirconia scaffolds while possessing mechanical properties (Zang et al., 2023). BMP-2 is a burst word in the field of bone regeneration materials in recent years, which may indicate that BMP-2 is a hotspot in recent years. The research by Bilem, I and others shows that the synergy of RGD peptide and BMP-2 can significantly improve the level of bone regeneration (Bilem et al., 2016). Recombinant human bone morphogenetic protein-2 (rhBMP- 2) has been approved by the FDA for safe use in humans and is widely used. Some researchers pointed out that rhBMP-2 can promote wounds to heal faster and enhance the formation of new bones (Galarraga-Vinueza et al., 2023). This may be particularly beneficial for patients whose bone healing ability is impaired or who have limited donor sites. It is worth noting that a recently published article titled “Current Status of Recombinant Human Bone Morphogenetic Protein-2 (rhBMP-2) in Maxillofacial Surgery: Should It Be Continued?” mentioned that rhBMP-2 has high costs and safety issues, limited application conditions in maxillofacial trauma, and lacks ideal carriers and dosing regimens, so further research is needed to determine long-term safety, optimize dosage, and develop better carriers (On et al., 2023). PRP has evolved over many years to gradually derive platelet-rich fibrin (PRF) and concentrated growth factor (CGF). PRF is often used in periodontal disease treatment research, mainly treating periodontal intraosseous defects and gingival recession. Most studies show that PRF has good effects in soft tissue management and repair (Miron et al., 2017). The research by Shiezadeh, F and others shows that using PRF as an auxiliary grafting material can reduce the residual particles of allogeneic grafts and increase bone marrow formation, which may be a treatment option for treating atrophic posterior maxillary bones after treatment (Shiezadeh et al., 2023). The research by Lei, LH et al. shows that advanced platelet-rich fibrin (A-PRF) and CGF can stimulate the continuous stable release of total growth factors within 14 days, showing similar efficacy in periodontal bone regeneration, and can guide necrotic tissue regeneration in inflammatory bowel disease treatment (Lei et al., 2020). CGF is widely used in bone grafting surgery, but often encounters problems with too fast release of growth factors, resulting in slightly worse bone regeneration effects. The latest research shows that the application of RADA16 nanofiber scaffold hydrogel with CGF can become a new treatment strategy for treating alveolar bone loss and other problems requiring bone regeneration (Yang et al., 2023).
In recent years, the combination of various materials has become a trend. Researchers have successfully manufactured an biomimetic bilayer scaffold by combining a intrafibrillarly mineralized collagen (IMC) scaffold manufactured through a biomimetic self-assembly method and CGF. This scaffold effectively reconstructs natural periodontal tissue by recruiting host mesenchymal stem cells and activating the transforming growth factor β1/Smad3 signaling pathway, inserting periodontal ligament fibers into newly formed alveolar bone and dental bone. This method has great potential in recruiting and regulating host stem cells to promote the synergistic regeneration of hard/soft tissues (Yu et al., 2022). MXenes, composed of 2D transition metal carbides, nitrides, and carbonitrides, have high conductivity, hydrophilicity, excellent thermal stability, large interlayer spacing, easily adjustable structure, and high surface area. In the past, this material was often used for the development of high-performance electrode materials (Chaudhari et al., 2017). However, in recent years, researchers have combined 2D titanium carbide (MXene) nanosheets and ultralong hydroxyapatite nanowires (UHAPNWs) to make a UHAPNWs/MXene nanocomposite membrane. This composite membrane has a positive and significant effect on enhancing mechanical properties, biocompatibility, and osteoinductivity, and may become a new type of inorganic composite material for bone tissue regeneration in the future (Fu et al., 2021). Demineralized dentin matrix (DDM), as a bone conduction and bone induction material, has been successfully used in clinical applications such as sinus floor augmentation and alveolar ridge augmentation. However, the granular form of DDM makes it difficult to anchor in the bone defect area. Therefore, researchers have combined DDM and fibrin glue (FG) in a certain proportion to make a mixture. Experiments have shown that this mixture can exhibit stronger osteogenic activity and bone regeneration ability (Tian et al., 2022). A study in 2021 found that molybdenum ions are a multifunctional cell regulator that can be used in biomaterial design and bone tissue engineering. Researchers have manufactured a molybdenum-containing bioactive glass-ceramic scaffold through 3D printing. This scaffold can significantly promote osteoblast-guided bone formation and inhibit bone resorption caused by osteoclasts throughout the bone healing process, thereby enhancing bone regeneration (Bao et al., 2023). The current clinical bone regeneration treatment has limited ability to control bacteria and infections, which is not conducive to the formation of new bone. However, a recent study has synthesized a multifunctional scaffold that simulates the natural bone nanostructure by incorporating silver nanowires into the layered intrafiber mineralized collagen matrix (IMC/AgNW). This scaffold has excellent osteoinductive activity under both non-inflammatory and inflammatory conditions, showing great clinical potential (Zhang et al., 2024). In summary, the combination of multiple materials for oral bone regeneration has a larger application prospect. In addition, materials that were mainly used in the industry in the past have also shown great potential in the field of bioengineering.
The limitations of this study are as follows: ① In order to ensure the accuracy of the search, the “material” was accurately retrieved in the search, which may lead to the exclusion of some of the required literature. ② Although the SCIE data is large and relatively complete and relatively authoritative, it still cannot be excluded that some papers representing the field of oral bone regeneration materials were not included. ③ Researchers may have different views on the same analysis map.
This study uses Citespace and VOSviewer to conduct a bibliometric analysis of literature on oral bone regeneration materials from 1991 to 2023. By describing and visualizing the annual publications, countries, institutions, influential authors, keywords, and burst cited papers, we have understood the research hotspots, frontiers, and trends in this field, and have drawn the following conclusions: ① In recent years, the number of related research papers has reached a stable level and the research has entered a steady forward stage; ② From the perspective of the number of publications, author collaboration relationships, and citation frequency, Buser D is the most influential author in this field; The United States has the most publications and the closest cooperation with other countries; The University of Bern and the University of Zurich in Switzerland are not only the institutions with the most publications but also the institutions with the most cooperation with other institutions and the University of Bern is both the institution with the most output and the institution with the most citation frequency; ③ In recent years, research hotspots have mainly focused on tissue engineering materials, but traditional materials still occupy a large proportion in clinical treatment and research, still occupy a large proportion in clinical treatment and research. In addition, the combined use of new and old materials has gradually become one of the research hotspots in the field of oral bone regeneration materials.
RT: Conceptualization, Data curation, Formal Analysis, Writing–original draft, Writing–review and editing. XL: Investigation, Software, Writing–review and editing. LX: Data curation, Software, Writing–review and editing. XY: Supervision, Writing–review and editing. RZ: Supervision, Writing–review and editing. JaL: Validation, Writing–review and editing. WZ: Validation, Writing–review and editing. JnL: Validation, Writing–review and editing. XW: Funding acquisition, Resources, Writing–review and editing. BL: Funding acquisition, Resources, Writing–review and editing.
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This work is supported by Science and Technology Innovation Leader and Key Talent Team Project of Shanxi Province (202204051002034), Key Research and Development Plan of Shanxi Province (202102130501002), Scientific Research Project for Returned Overseas Professionals of Shanxi Province (2022-120), Key national science and technology cooperation project of Shanxi Provincial Department of Science and Technology (202204041101004) and Four“Batches” Innovation Project of Invigorating Medical through Science and Technology of Shanxi Province (2023XM013).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Alavi, S. E., Alavi, S. Z., Gholami, M., Sharma, A., Sharma, L. A., and Shahmabadi, H. E. (2023). Biocomposite-based strategies for dental bone regeneration. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 136 (5), 554–568. doi:10.1016/j.oooo.2023.04.015
Avila-Ortiz, G., Chambrone, L., and Vignoletti, F. (2019). Effect of alveolar ridge preservation interventions following tooth extraction: a systematic review and meta-analysis. J. Clin. Periodontology 46, 195–223. doi:10.1111/jcpe.13057
Bao, J., Fu, X., Wu, Y., Yang, S., Ren, X., Fang, X., et al. (2023). The healing capacity and osteogenesis pattern of demineralized dentin matrix (DDM)-fibrin glue (FG) compound. Sci. Rep. 13 (1), 13140. doi:10.1038/s41598-023-40258-7
Berglundh, T., Armitage, G., Araujo, M. G., Avila-Ortiz, G., Blanco, J., Camargo, P. M., et al. (2018). Peri-implant diseases and conditions: Consensus report of workgroup 4 of the 2017 World Workshop on the classification of periodontal and peri-implant diseases and conditions. J. Clin. Periodontology 45, S286-S291–S91. doi:10.1111/jcpe.12957
Bilem, I., Chevallier, P., Plawinski, L., Sone, E. D., Durrieu, M. C., and Laroche, G. (2016). RGD and BMP-2 mimetic peptide crosstalk enhances osteogenic commitment of human bone marrow stem cells. Acta Biomater. 36, 132–142. doi:10.1016/j.actbio.2016.03.032
Chappuis, V., Araujo, M. G., and Buser, D. (2017). Clinical relevance of dimensional bone and soft tissue alterations post-extraction in esthetic sites. Periodontology 73 (1), 73–83. doi:10.1111/prd.12167
Chaudhari, N. K., Jin, H., Kim, B., Baek, D. S., Joo, S. H., and Lee, K. (2017). MXene: an emerging two-dimensional material for future energy conversion and storage applications. J. Mater. Chem. A 5 (47), 24564–24579. doi:10.1039/c7ta09094c
Chen, C., Dubin, R., and Kim, M. C. (2014). Emerging trends and new developments in regenerative medicine: a scientometric update (2000 - 2014). Expert Opin. Biol. Ther. 14 (9), 1295–1317. doi:10.1517/14712598.2014.920813
Chen, C. M. (2006). CiteSpace II: detecting and visualizing emerging trends and transient patterns in scientific literature. J. Am. Soc. Inf. Sci. Technol. 57 (3), 359–377. doi:10.1002/asi.20317
Chen, C. M. (2017). Science mapping: a systematic review of the literature. J. Data Inf. Sci. 2 (2), 1–40. doi:10.1515/jdis-2017-0006
de lange, G. L., Overman, J. R., Farre-Guasch, E., Korstjens, C. M., Hartman, B., Langenbach, G. E. J., et al. (2014). A histomorphometric and micro-computed tomography study of bone regeneration in the maxillary sinus comparing biphasic calcium phosphate and deproteinized cancellous bovine bone in a human split-mouth model. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 117 (1), 8–22. doi:10.1016/j.oooo.2013.08.008
Elgali, I., Omar, O., Dahlin, C., and Thomsen, P. (2017). Guided bone regeneration: materials and biological mechanisms revisited. Eur. J. Oral Sci. 125 (5), 315–337. doi:10.1111/eos.12364
Fu, Y., Zhang, J., Lin, H., and Mo, A. (2021). 2D titanium carbide(MXene) nanosheets and 1D hydroxyapatite nanowires into free standing nanocomposite membrane: in vitro and in vivo evaluations for bone regeneration. Mater. Sci. Eng. C-Materials Biol. Appl. 118, 111367. doi:10.1016/j.msec.2020.111367
Galarraga-Vinueza, M. E., Barootchi, S., Nevins, M. L., Nevins, M., Miron, R. J., and Tavelli, L. (2023). Twenty-five years of recombinant human growth factors rhPDGF-BB and rhBMP-2 in oral hard and soft tissue regeneration. Periodontology 94, 483–509. doi:10.1111/prd.12522
Gallego, L., Junquera, L., Garcia, E., Garcia, V., Alvarez-Viejo, M., Costilla, S., et al. (2010). Repair of rat mandibular bone defects by alveolar osteoblasts in a novel plasma-derived albumin scaffold. Tissue Eng. Part A 16 (4), 1179–1187. doi:10.1089/ten.tea.2009.0517
Gao, J., Yin, Y., Myers, K. R., Lakhani, K. R., and Wang, D. (2021). Potentially long-lasting effects of the pandemic on scientists. Nat. Commun. 12 (1), 6188. doi:10.1038/s41467-021-26428-z
Ge, Y., Chao, T., Sun, J., Liu, W., Chen, Y., and Wang, C. (2022). Frontiers and hotspots evolution in psycho-cardiology: a bibliometric analysis from 2004 to 2022. Curr. Problems Cardiol. 47 (12), 101361. doi:10.1016/j.cpcardiol.2022.101361
Heo, S., Chan, A. Y., Diaz Peralta, P., Jin, L., Pereira Nunes, C. R., and Bell, M. L. (2022). Impacts of the COVID-19 pandemic on scientists’ productivity in science, technology, engineering, mathematics (STEM), and medicine fields. Humanit Soc. Sci. Commun. 9 (1), 434. doi:10.1057/s41599-022-01466-0
Ho-Shui-Ling, A., Bolander, J., Rustom, L. E., Johnson, A. W., Luyten, F. P., and Picart, C. (2018). Bone regeneration strategies: engineered scaffolds, bioactive molecules and stem cells current stage and future perspectives. Biomaterials 180, 143–162. doi:10.1016/j.biomaterials.2018.07.017
Jung, R. E., Sapata, V. M., Hammerle, C. H. F., Wu, H., Hu, X.-l., and Lin, Y. (2018). Combined use of xenogeneic bone substitute material covered with a native bilayer collagen membrane for alveolar ridge preservation: a randomized controlled clinical trial. Clin. Oral Implants Res. 29 (5), 522–529. doi:10.1111/clr.13149
Kloss, F. R., Offermanns, V., and Kloss-Brandstaetter, A. (2018). Comparison of allogeneic and autogenous bone grafts for augmentation of alveolar ridge defects-A 12-month retrospective radiographic evaluation. Clin. Oral Implants Res. 29 (11), 1163–1175. doi:10.1111/clr.13380
Lei, L., Yu, Y., Han, J., Shi, D., Sun, W., Zhang, D., et al. (2020). Quantification of growth factors in advanced platelet-rich fibrin and concentrated growth factors and their clinical efficacy as adjunctive to the GTR procedure in periodontal intrabony defects. J. Periodontology 91 (4), 462–472. doi:10.1002/jper.19-0290
Lotz, E. M., Olivares-Navarrete, R., Hyzy, S. L., Berner, S., Schwartz, Z., and Boyan, B. D. (2017). Comparable responses of osteoblast lineage cells to microstructured hydrophilic titanium-zirconium and microstructured hydrophilic titanium. Clin. Oral Implants Res. 28 (7), e51–e59. doi:10.1111/clr.12855
Miron, R. J., Zucchelli, G., Pikos, M. A., Salama, M., Lee, S., Guillemette, V., et al. (2017). Use of platelet-rich fibrin in regenerative dentistry: a systematic review. Clin. Oral Investig. 21 (6), 1913–1927. doi:10.1007/s00784-017-2133-z
Moghadam, E. T., Yazdanian, M., Alam, M., Tebyanian, H., Tafazoli, A., Tahmasebi, E., et al. (2021). Current natural bioactive materials in bone and tooth regeneration in dentistry: a comprehensive overview. J. Mater. Res. Technology-Jmr&T 13, 2078–2114. doi:10.1016/j.jmrt.2021.05.089
Monje, A., Pons, R., Lnsua, A., Nart, J., Wang, H.-L., and Schwarz, F. (2019). Morphology and severity of peri-implantitis bone defects. Clin. Implant Dent. Relat. Res. 21 (4), 635–643. doi:10.1111/cid.12791
On, S.-W., Park, S.-Y., Yi, S.-M., Park, I.-Y., Byun, S.-H., and Yang, B.-E. (2023). Current status of recombinant human bone morphogenetic protein-2 (rhBMP-2) in maxillofacial surgery: should it Be continued? Bioengineering-Basel 10 (9), 1005. doi:10.3390/bioengineering10091005
Pan, X., Yan, E., Cui, M., and Hua, W. (2018). Examining the usage, citation, and diffusion patterns of bibliometric mapping software: a comparative study of three tools. J. Inf. 12 (2), 481–493. doi:10.1016/j.joi.2018.03.005
Pan, Y., Zhao, Y., Kuang, R., Liu, H., Sun, D., Mao, T., et al. (2020). Injectable hydrogel-loaded nano-hydroxyapatite that improves bone regeneration and alveolar ridge promotion. Mater. Sci. Eng. C-Materials Biol. Appl. 116, 111158. doi:10.1016/j.msec.2020.111158
Sakkas, A., Wilde, F., Heufelder, M., Winter, K., and Schramm, A. (2017). Autogenous bone grafts in oral implantology-is it still a “gold standard”? A consecutive review of 279 patients with 456 clinical procedures. Int. J. Implant Dent. 3, 23. doi:10.1186/s40729-017-0084-4
Sartori, S., Silvestri, M., Forni, F., Cornaglia, A. I., Tesei, P., and Cattaneo, V. (2003). Ten-year follow-up in a maxillary sinus augmentation using anorganic bovine bone (Bio-Oss). A case report with histomorphometric evaluation. Clin. Oral Implants Res. 14 (3), 369–372. doi:10.1034/j.1600-0501.2003.140316.x
Sehn, F. P., Dias, R. R., Santos, T. S., Silva, E. R., Salata, L. A., Chaushu, G., et al. (2015). Fresh-frozen allografts combined with bovine bone mineral enhance bone formation in sinus augmentation. J. Biomaterials Appl. 29 (7), 1003–1013. doi:10.1177/0885328214552709
Shiezadeh, F., Taher, M., Shooshtari, Z., Arab, H., and Shafieian, R. (2023). Using platelet-rich fibrin in combination with allograft bone particles can induce bone formation in maxillary sinus augmentation. J. Oral Maxillofac. Surg. 81 (7), 904–912. doi:10.1016/j.joms.2023.03.015
Starch-Jensen, T., Bruun, N. H., and Spin-Neto, R. (2023). Outcomes following osteotome-mediated sinus floor elevation with Bio-Oss Collagen or no grafting material: a one-year single-blind randomized controlled trial. Int. J. Oral Maxillofac. Surg. 52 (9), 988–997. doi:10.1016/j.ijom.2022.12.009
Sun, P., Wang, J., Zheng, Y., Fan, Y., and Gu, Z. (2012). BMP2/7 heterodimer is a stronger inducer of bone regeneration in peri-implant bone defects model than BMP2 or BMP7 homodimer. Dent. Mater. J. 31 (2), 239–248. doi:10.4012/dmj.2011-191
Tang, G., Liu, Z., Liu, Y., Yu, J., Wang, X., Tan, Z., et al. (2021). Recent trends in the development of bone regenerative biomaterials. Front. Cell Dev. Biol. 9, 665813. doi:10.3389/fcell.2021.665813
Tian, B., Li, X., Zhang, J., Zhang, M., Gan, D., Deng, D., et al. (2022). A 3D-printed molybdenum-containing scaffold exerts dual pro-osteogenic and anti-osteoclastogenic effects to facilitate alveolar bone repair. Int. J. Oral Sci. 14 (1), 45. doi:10.1038/s41368-022-00195-z
Tong, Z., Guo, J., Glen, R. C., Morrell, N. W., and Li, W. (2019). A bone morphogenetic protein (BMP)-derived peptide based on the type I receptor-binding site modifies cell-type dependent BMP signalling. Sci. Rep. 9, 13446. doi:10.1038/s41598-019-49758-x
Tresguerres, F. G. F., Cortes, A. R. G., Vallejo, G. H., Cabrejos-Azama, J., Tamimi, F., and Torres, J. (2019). Clinical and radiographic outcomes of allogeneic block grafts for maxillary lateral ridge augmentation: a randomized clinical trial. Clin. Implant Dent. Relat. Res. 21 (5), 1087–1098. doi:10.1111/cid.12834
Troeltzsch, M., Troeltzsch, M., Kauffmann, P., Gruber, R., Brockmeyer, P., Moser, N., et al. (2016). Clinical efficacy of grafting materials in alveolar ridge augmentation: A systematic review. J. Cranio-Maxillofacial Surg. 44 (10), 1618–1629. doi:10.1016/j.jcms.2016.07.028
van Eck, N. J., and Waltman, L. (2010). Software survey: VOSviewer, a computer program for bibliometric mapping. Scientometrics 84 (2), 523–538. doi:10.1007/s11192-009-0146-3
Wagner, J. M., Reinkemeier, F., Wallner, C., Dadras, M., Huber, J., Schmidt, S. V., et al. (2019). Adipose-Derived stromal cells are capable of restoring bone regeneration after post-traumatic osteomyelitis and modulate B-cell response. Stem Cells Transl. Med. 8 (10), 1084–1091. doi:10.1002/sctm.18-0266
Wang, B., Feng, C., Liu, Y., Mi, F., and Dong, J. (2022). Recent advances in biofunctional guided bone regeneration materials for repairing defective alveolar and maxillofacial bone: a review. Jpn. Dent. Sci. Rev. 58, 233–248. doi:10.1016/j.jdsr.2022.07.002
Xia, D., Yang, F., Zheng, Y., Liu, Y., and Zhou, Y. (2021). Research status of biodegradable metals designed for oral and maxillofacial applications: a review. Bioact. Mater. 6 (11), 4186–4208. doi:10.1016/j.bioactmat.2021.01.011
Yang, R., Chen, J., Wang, D., Xu, Y., and Ou, G. (2023). Self-assembling peptide RADA16 nanofiber scaffold hydrogel-wrapped concentrated growth factors in osteogenesis of MC3T3. J. Funct. Biomaterials 14 (5), 260. doi:10.3390/jfb14050260
Yu, M., Luo, D., Qiao, J., Guo, J., He, D., Jin, S., et al. (2022). A hierarchical bilayer architecture for complex tissue regeneration. Bioact. Mater. 10, 93–106. doi:10.1016/j.bioactmat.2021.08.024
Zang, S., Xiao, C., He, M., Chen, B., Liu, B., Yi, S., et al. (2023). RGD and rhBMP-7 immobilized on zirconia scaffold with interweaved human dental pulp stem cells for promoting bone regeneration. Mater. Des. 232, 112052. doi:10.1016/j.matdes.2023.112052
Zhang, X., Li, Q., Wang, Z., Zhou, W., Zhang, L., Liu, Y., et al. (2022). Bone regeneration materials and their application over 20 years: a bibliometric study and systematic review. Front. Bioeng. Biotechnol. 10, 921092. doi:10.3389/fbioe.2022.921092
Keywords: bone regeneration, bibliometric analysis, materials, mandible, maxilla, alveolar
Citation: Tu R, Liu X, Xu L, Yao X, Zhang R, Li J, Zhang W, Liu J, Wu X and Li B (2024) The current status and trends of oral bone regeneration materials: a bibliometric analysis from 1991 to 2023. Front. Mater. 11:1420900. doi: 10.3389/fmats.2024.1420900
Received: 21 April 2024; Accepted: 17 June 2024;
Published: 03 July 2024.
Edited by:
Gabriella Epasto, University of Messina, ItalyReviewed by:
Weimin Lin, Sichuan University, ChinaCopyright © 2024 Tu, Liu, Xu, Yao, Zhang, Li, Zhang, Liu, Wu and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiuping Wu, Nzd3eHBAMTYzLmNvbQ==; Bing Li, bGliaW5nMTk3NXZpcEAxNjMuY29t
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.