
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Mater., 08 April 2024
Sec. Mechanics of Materials
Volume 11 - 2024 | https://doi.org/10.3389/fmats.2024.1363835
This article is part of the Research TopicCurrent Trends in Nickel-Titanium Instruments for Endodontic ApplicationsView all 5 articles
 Katia Greco1
Katia Greco1 Francesco Iacono2*
Francesco Iacono2* Francesco Montagna3
Francesco Montagna3 Carola Esposito Corcione3
Carola Esposito Corcione3 Gaetano Paolone1
Gaetano Paolone1 Enrico Gherlone1
Enrico Gherlone1 Giuseppe Cantatore1
Giuseppe Cantatore1Aim: The study aimed to evaluate the shaping characteristics of ProTaper Ultimate (Dentsply Sirona) and BlueShaper (Zarc4Endo) using microcomputed tomographic imaging technology (micro-CT).
Methods: Thirty mesial and distal canals of extracted second mandibular molars with similar anatomy were selected and scanned pre- and postoperatively by micro-CT scanning (SkyScan 1172, Bruker micro-CT) with a voxel size of 11 μm and shaped with two different procedures: ProTaper Ultimate (Group 1: n = 15) and BlueShaper (Group 2: n = 15) were used following the manufacturer’s recommendations up to final 30 apical size. Irrigation was ensured in all groups with 5.25% NaOCl and 10% EDTA during instrumentation. Canal transportation, the volume of removed dentin, and area of untreated surface were matched with preoperative values with Bruker CT Analyser (Bruker micro-CT). Data were statistically analyzed using Student’s t-test.
Results: No significant differences were observed between Group 1 and Group 2 in terms of canal transportation, volume of removed dentin, and untreated surfaces. A significant difference (p < 0.05) in the amount of untreated surfaces was found between the mesial and distal canals in both groups.
Conclusion: Shaping procedures with both ProTaper Ultimate and BlueShaper demonstrated similar canal enlargement volumes and similar canal transportation without evidence of significant preparation errors. Nevertheless, a high amount of untreated surface was reported for both systems, particularly in distal canals.
Shaping the root canal system represents a key moment in endodontic treatment, synergistic with cleansing and obturation phases. One of the most important objectives of instrumentation is the complete and centered incorporation of the original canals into the prepared shape (Arias and Peters, 2022). On one hand, the decontamination of the root canal system from bacteria, organic substrates, and shaping debris is crucial during the procedures; on the other hand, respect for the root canal anatomy is equally important to preserve the integrity of the tooth (Peters, 2004). One of the mechanical objectives of the instrumentation is to retain as much cervical and radicular dentin as possible so as not to weaken the root structure, thereby preventing root fractures (Arias and Peters, 2022). Manufacturers and researchers are constantly developing and investigating new nickel–titanium (NiTi) instruments to simplify canal preparation and prevent procedural errors. Alloys, design of cutting blades, tapers, helical angles, numbers of flutes, cross-sectional shapes, and tip outline are some of the major changes and evolutions in instrument design and characteristics (Shen and Haapasalo, 2008; Shen et al., 2013; Arias and Peters, 2022).
The nondestructive technique of microcomputed tomographic (micro-CT) scanning has been demonstrated to allow a complete description of the three-dimensional effects of the root canal preparation in terms of changes in the dentin volume, percentage of untreated canal surface, and degree of canal transportation (Peters et al., 2003; Gagliardi et al., 2015; Pedullà et al., 2016; Brasil et al., 2017; De-Deus et al., 2017; Drukteinis et al., 2019; Guedes et al., 2022; Generali et al., 2023; Yeniçeri Özata et al., 2023).
New systems have recently been introduced into the market. Amongst these, the ProTaper Ultimate system (Dentsply Sirona, Ballaigues, Switzerland) includes five instruments with variable tapers (https://www.dentsplysirona.com/en/service-contact/download-center/active-ifu-asset-detail-page.html/content/dam/master/product-procedure-brand-categories/endodontics/product-categories/full-solutions/protaper-ultimate-solution/ifu/END-IFU-PROTAPER-ULTIMATE-MANUAL-REUSABLE-STERILE-V00-WEB-ROW-Multilingual-2021-04.pdf) that are claimed to exhibit great flexibility and resistance to cyclic fatigue. The ProTaper Ultimate Slider alloy is manufactured in R-Phase alloy, while the other instruments are metallurgically similar to the gold heat-treated alloy (Martins et al., 2023).
The BlueShaper system (Zarc4Endo, Gijón, Spain) consists of a total of eight instruments with variable tapers, BlueShaper shaping files (ZX, Z1, and Z2), and BlueShaper finishing files (Z3, Z4, Z5, Z6, and Z7), that are manufactured with two different alloys (pink and blue treatments) (https://zarc4endo.com/wp-content/uploads/2022/05/DFU-BlueShaper-ENG.pdf). These files are claimed to possess a martensitic phase that increases flexibility and resistance to fracture by cyclic fatigue (Rubio et al., 2022).
To the best of our knowledge, no information on the comparison of the shaping ability of these new instruments is currently available.
Therefore, the aim of this study was to evaluate the canal-shaping ability of ProTaper Ultimate and BlueShaper instruments using micro-CT imaging. The null hypothesis to be tested was that no difference exists in the shaping ability among these different instruments.
The sample size was determined a priori using G*Power. Cohen’s effect size was set as 0.8, the type error as 5%, the power test as 95%, and the number of groups as 2. Based on these parameters, a minimum sample size of 12 per group was established. Therefore, each group was composed of 15 canals.
Ten human permanent molars with completely formed apices, free of caries and cracks, extracted for periodontal or orthodontic reasons, with confluent mesial canals in the apical third and single distal canals (Vertucci Type configuration II), were selected on the basis of the curvature of the mesial root (10°–30°) according to Schneider’s technique (Schneider, 1971). Teeth were stored in distilled water at 4°C.
Teeth were slightly dried, mounted on a custom attachment, and prescanned in a relatively low isotropic resolution (10.98 μm) using a micro-CT scanner (SkyScan 1,172 Bruker microCT, Kontich, Belgium) at 70 kV and 141 μA. Scanning was performed through 180-degree rotation around the vertical axis. After the scan, the acquired projection images were reconstructed into cross-section slices (SkyScan NRecon 1.6.9.) and 3D volume rendering (Bruker CTVOX 3.3.1), and several morphological parameters of the mesial and distal canals (length, volume, and surface area) were obtained (Bruker CT Analyser 1.20.8.0).
The endodontic access cavities were prepared using high-speed diamond burs, and the pulp chambers were conservatively accessed. Preparation started at the central fossa of the occlusal surface and extended with smoothly convergent axial walls to the occlusal surface only as far as necessary to detect the canal orifices (Clark and Khademi, 2010; Silva et al., 2022). After their detection, a #10 K-file (Dentsply Maillefer) was inserted through the mesiobuccal, mesiolingual, and distal canals. A 25-mm, #10 stainless steel manual K-file (Dentsply Maillefer, Ballaigues, Swiss) was used to assess initial patency and to evaluate the working length (WL) that was established by subtracting 1 mm from the K-file tip visible at the apical foramen.
The teeth were then randomly divided into two groups, according to the shaping procedure.
Group 1 (n = 15) was instrumented with a ProTaper Ultimate Slider (016.002v), Shaper (020.004v) and then with finishing files up to size 30 (F1, 020.007v; F2, 025.008v; F3, 030.009v) (Figure 1A), following the manufacturer’s recommendations at 400 rpm and 4.0 Ncm. Upon removing any given file, canals were recapitulated with a #10 K-file.
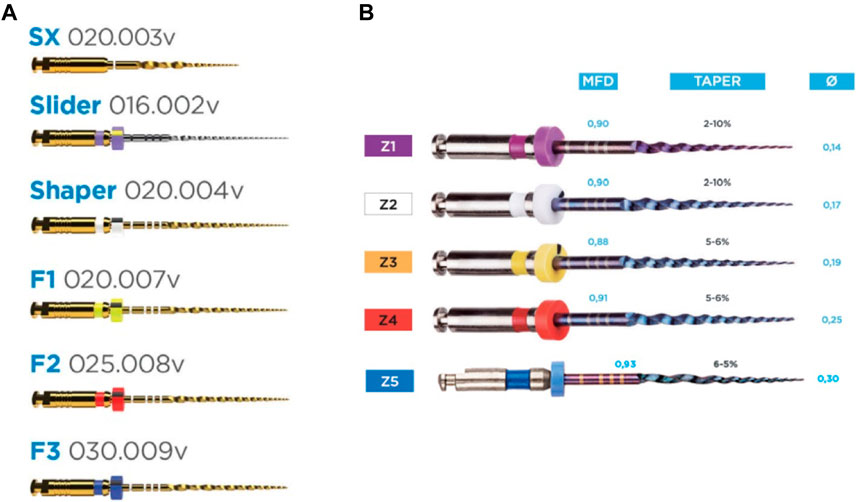
Figure 1. Web images reporting the investigated sequences, as proposed by manufacturers. Diameter and variable tapers are also reported. (A) ProTaper Ultimate and (B) BlueShaper.
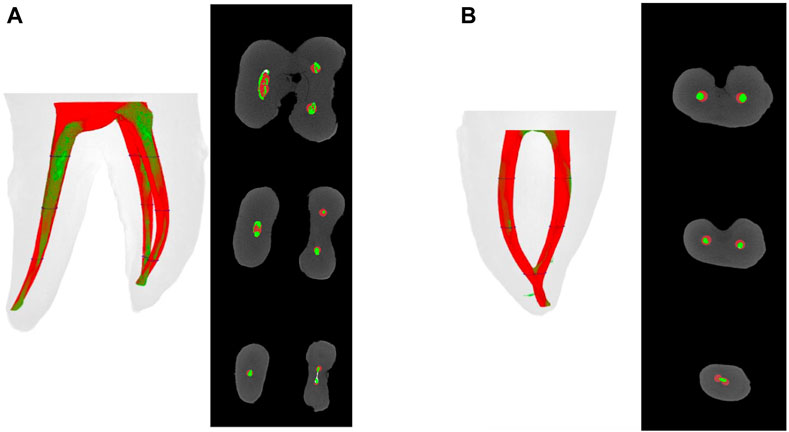
Figure 2. (A) Representative lateral and axial view of three-dimensional reconstructions of the internal anatomy of a second mandibular molar before (green) and after (red) canal preparation with BlueShaper instruments. (B) Frontal and axial views of the internal anatomy of a mesial root of a second mandibular molar before (green) and after (red) canal preparation with ProTaper Ultimate instruments. Images A and B report representative cross sections of the superimposed root canals before (green) and after (red) preparation at the coronal, middle, and apical thirds.
Group 2 (n = 15) was instrumented with a BlueShaper Z1 (014, variable taper 2%–10%), Z2 (017, variable taper 2%–10%), Z3 (019, variable taper 5%–6%), Z4 (025, variable taper 5%–6%), and Z5 (030, variable taper 5%–6%) (Figure 1B), following the manufacturer’s recommendations at 500 rpm and 4.0 Ncm. Upon removing any given file, canals were recapitulated with a #10 K-file.
Teeth were secured through ProTrain (Simit Dental Srl, Mantova, Italy) during the instrumentation procedures. A single trained operator completed all the shaping phases.
In all groups, each canal was irrigated with 5 mL of 5.25% NaOCl (Niclor 5 Ogna, Muggiò, Italy) and 3 mL of 10% EDTA (Tubuliclean Ogna, Muggiò, Italy) solutions during instrumentation.
When root canal instrumentation was completed, each canal was subjected to further irrigation with 1.0 mL of 5.25% NaOCl for 3 min, 0.5 mL 10% EDTA for 1 min, and 1.0 mL of NaOCL for 3 min.
Average canal transportations were calculated with Bruker CT Analyser, applying the technique developed by Gambill et al. (1996) and comparing the shifts of the centers in micrometers before and after the instrumentation for the apical, middle, and coronal thirds of the canals. In detail, Gambill et al. (1996) compared the shaping of 30 root canals by two nickel–titanium instrumentation techniques using micro-CT. The area of dentine removed at predetermined levels (2.0 mm, 3.0 mm, 4.5 mm, 6.0 mm, and 7.5 mm) from the apex was measured, and transportation and centering were recorded. Images constructed at these levels were compared with video images of equivalent physical sections created after the second scan. The volume of dentine removed in the apical 7.5 mm of the root canals of each tooth was calculated, and the different techniques were compared.
Rendered three-dimensional images were used to assess the preparations (Figure 2). The mean differences and standard deviations in the volume and surface area of the entire canal, as well as canal transportation of the apical, middle, and coronal thirds of the canals were calculated (Gambill et al., 1996).
The pre- and post-shaping images were processed using Bruker CT Analyser 1.20.8.0 (Bruker microCT) to calculate quantitative parameters and construct 3-D models. Color rendering was obtained with Bruker CTVOX 3.3. The volume of removed dentin was calculated by subtracting the values for the treated canals from those recorded for the untreated counterparts. Superimposed images of the canals before and after preparation were analyzed to evaluate the percentage of the canal wall that was untreated. The analysis of touched and untouched surfaces consists of the following procedure. First, the before-and-after scans are registered in 3D. Then, we again made the binary datasets of the root canal space in the registered before-and-after datasets. We introduced a new step: making binary images of a thin boundary around the root canal only, not the whole root canal volume. We started this with the already-binarized “before” reference dataset. First, we thresholded the image dataset in custom processing (necessary even for binary images), then the following steps were used to create a 1-pixel-thick boundary exactly one pixel external to the original binary of the root canal (Bruker MicroCt, 2017). Data were statistically analyzed to determine the difference among groups by Student’s t-test. A p-value < .05 was regarded as significant.
No instruments fractured during the preparation of the canals. No major shaping errors and comparable canal shapes resulted during preparation procedures with either the BlueShaper or the ProTaper Ultimate instruments. Results of canal transportation, the volume of removed dentin, and untreated surfaces are summarized in Table 1. No significant differences were found between both instruments in terms of canal transportation (p > 0.05). No significant differences were observed between Group 1 and Group 2 in terms of volume of dentin removal after canal preparation, and no statistically significant differences were found between the groups in terms of untreated surface. A significant difference (p < 0.05) was found between untreated surfaces in the mesial and distal canals in both groups. Data are reported in Table 2.
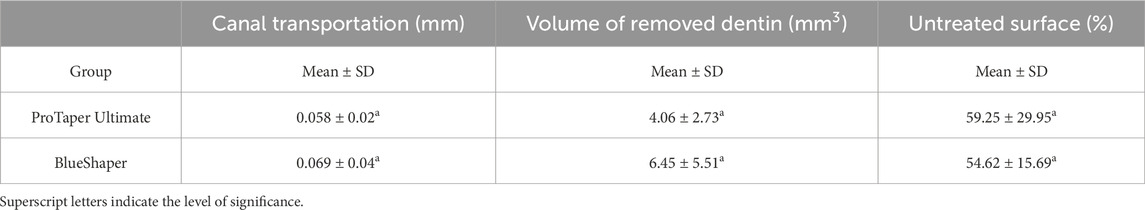
Table 1. Canal transportation (mm), the volume of the removed dentin (mm3), and the overall untreated surface (%) after instrumentation with ProTaper Ultimate and BlueShaper (mean ± SD).
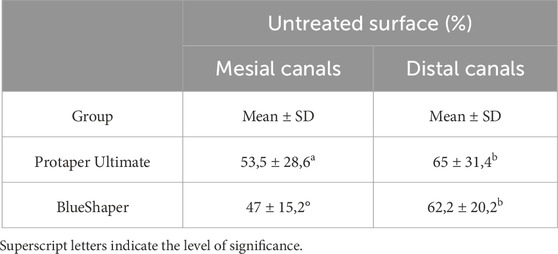
Table 2. Untreated mesial and distal canal surfaces (%) after instrumentation with ProTaper Ultimate and BlueShaper (mean ± SD).
Measurements of canal transportation made using micro-CT imaging have been increasingly used in endodontic research. This is a nondestructive, reproducible, and well-established method to assess the quality of the biomechanical shaping of new instruments and techniques engineered to facilitate the reduction of procedural errors (Hwang et al., 2014; Zhao et al., 2014; Pedullà et al., 2016; Yang et al., 2016; Brasil et al., 2017; Shah et al., 2017; Berutti et al., 2022). Freire et al. (2012) compared two methods of assessing apical transportation in curved canals after rotary instrumentation, namely, cross sections and micro-CT. In the case of micro-CT, they used the procedure suggested by Gambill et al. (1996), concluding that microCT can be considered superior to cross sections, especially in view of its ability to preserve specimens and provide results that are more closely related to clinical situations. Therefore, they recommend that micro-CT be preferred for assessing apical transportation in future experimental studies. Starting from these interesting results, we decided to follow the same procedure proposed by Gambill et al. (1996) and used by Freire et al. (2012).
ProTaper Ultimate and BlueShaper files have been recently introduced to the market, and to the best of our knowledge, no information on their shaping ability is currently available. Both systems are made with thermally treated alloys, with the aim to increase flexibility over conventional NiTi alloy and positively affect canal transportation, especially in curved root canals. In the present study, no significant differences were observed between groups in terms of canal transportation, although ProTaper Ultimate exhibited less transportation in the cervical and middle sections of the root canals. This can probably be explained by considering the regressive taper of ProTaper Ultimate files in the coronal part of the finisher files (Ruddle et al., 2022, https://www.endoruddle.com/PTUltimate-Finishers), designed to create a more conservative coronal preparation. In fact, centering ability can be influenced by the design of the instrument (size, taper, flexibility, and the type of alloy) (Zhao et al., 2014). The present study confirms that the improved mechanical properties of new alloys due to the innovative fabrication processes and/or the thermomechanical treatments (Shen et al., 2013; Pirani et al., 2016; Iacono et al., 2017; Zupanc et al., 2018; Silva et al., 2023) could have important clinical relevance in minimizing the risk of procedural errors. However, it is not clear yet if enhanced instrument properties are directly translated to an improvement in clinical success (Arias and Peters, 2022). The tested systems have the characteristic of imparting a low taper to canals and are clinically indicated for shaping narrow and/or curved canals. It is known that canals should be prepared to a uniform and continuous taper (Schilder, 1974) with the aim of facilitating specific root-filling techniques rather than antimicrobial efficacy (Arias and Peters, 2022). Canals with reduced taper represent one of the major clinical indications for carrier-based obturation techniques or single cones with bioceramic sealers (Greco et al., 2014; American Association of Endodontists, 2016; Pirani et al., 2019).
Multirooted teeth with complex anatomy present a greater challenge to successful endodontic therapy than single-rooted teeth. In the present study, both the curved mesial and straight distal canals of second mandibular molars were taken into consideration. In fact, during daily endodontic procedures, clinicians generally use the same instruments and systems for different canal anatomies of the same tooth (Zhao et al., 2014). Moreover, as crown subsistence would result in a different pressure of the instruments against the outer aspect of the curve (Alovisi et al., 2018), the teeth were not decoronated in the present study, mimicking clinical conditions. Nevertheless, tooth selection was strictly standardized to obtain comparable anatomies of both mesial and distal canals with respect to geometric parameters (i.e., canal curvature and the initial canal volume) before instrumentation. Vertucci type II is the most common configuration of second mandibular molars (Pawar et al., 2017; Gomez et al., 2021) and, for this reason, it was investigated in the present study. Despite the apical confluence of the mesial canals, instrumentation was performed considering each canal separately, and preoperative and postinstrumentation scans were superimposed to evaluate the foramina transportation. Interestingly, no transportation or abnormal foramina enlargement was noted. Moreover, no differences were reported in terms of canal transportation between curved mesial and straight distal canals. This could be explained by the alloy flexibility of ProTaper Ultimate and BlueShaper to maintain the incorporation of the original canal into the prepared shape. However, none of the NiTi systems considered in this study could prepare the entire walls of the root canal space. Sousa-Neto et al. (2018) reported that several micro-CT assessments revealed a large percentage, ranging from 2.6% to 80%, of untreated canal walls after shaping procedures. Data from the present study confirm similar levels of unprepared root canal areas reported by Lopes et al. (2017), where the ProTaper Next and Twisted Files Adaptive were investigated.
In the present study, a significant difference was found between untreated surfaces in the mesial and distal canals in both groups. A high surface area of distal canals (>60%) was completely untreated by both the ProTaper Ultimate and the BlueShaper. The suboptimal mechanical preparation, especially in areas of anatomical challenges such as isthmuses, recesses, and flattened root canals, can retain bacteria and serve as a potential cause of persistent infection (Siqueira and Rôças, 2008; Siqueira et al., 2013).
This should increase the need for clinicians to adopt strategies to enhance antimicrobial efficacy, such as improving the performance of the irrigating solution and the physical action of ultrasonic activation and intracanal dressing to complement suboptimal mechanical action, and obtain optimal disinfection of the root canal space (Boutsioukis and Arias-Moliz, 2022).
The main strength of this study was that, to the best of our knowledge, no information comparing the shaping ability of both ProTaper Ultimate and BlueShaper is currently available. Nevertheless, further evaluations should be conducted in the presence of a larger number of samples.
Within the limits of the present study, it can be concluded that ProTaper Ultimate and BlueShaper exhibited comparable maintenance of the original canal anatomy, supporting the use of both shaping techniques for the instrumentation of complex mandibular molars. Therefore, the null hypothesis was accepted.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
KG: writing–review and editing, writing–original draft, methodology, investigation, and conceptualization. FI: writing–review and editing and writing–original draft. FM: writing–review and editing, writing–original draft, validation, software, and investigation. CEC: writing–review and editing, writing–original draft, supervision, software, and methodology. GP: writing–review and editing, writing–original draft, visualization, and supervision. EG: writing–review and editing, writing–original draft, validation, project administration, and funding acquisition. GC: writing–review and editing, visualization, supervision, and conceptualization.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors, and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Alovisi, M., Pasqualini, D., Musso, E., Bobbio, E., Giuliano, C., Mancino, D., et al. (2018). Influence of contracted endodontic access on root canal geometry: an in vitro study. J. Endod. 44, 614–620. doi:10.1016/j.joen.2017.11.010
American Association of Endodontists, (2016) Colleagues for excellence. Canal preparation and obturation: an update view of the two pillars of nonsurgical endodontics, https://f3f142zs0k2w1kg84k5p9i1o-wpengine.netdna-ssl.com/specialty/wp-content/uploads/sites/2/2017/07/ecfefall2016canalpreparationandobturation.pdf
Arias, A., and Peters, O. A. (2022). Present status and future directions: canal shaping. Int. Endod. J. 55, 637–655. doi:10.1111/iej.13698
Berutti, E., Moccia, E., Lavino, S., Multari, S., Carpegna, G., Scotti, N., et al. (2022). Micro-computed tomography evaluation of minimally invasive shaping systems in mandibular first molars. J. Clin. Med. 11, 4607. doi:10.3390/jcm11154607
Boutsioukis, C., and Arias-Moliz, M. T. (2022). Present status and future directions - irrigants and irrigation methods. Int. Endod. J. 55, 588–612. doi:10.1111/iej.13739
Brasil, S. C., Marceliano-Alves, M. F., Marques, M. L., Grillo, J. P., Lacerda, M. F., Alves, F. R., et al. (2017). Canal transportation, unprepared areas, and dentin removal after preparation with BT-RaCe and ProTaper Next systems. J. Endod. 43, 1683–1687. doi:10.1016/j.joen.2017.04.012
Clark, D., and Khademi, J. (2010). Modern molar endodontic access and directed dentin conservation. Dent. Clin. N. Am. 54, 249–273. doi:10.1016/j.cden.2010.01.001
De-Deus, G., Silva, E. J., Vieira, V. T., Belladonna, F. G., Elias, C. N., Plotino, G., et al. (2017). Blue thermomechanical treatment optimizes fatigue resistance and flexibility of the reciproc files. J. Endod. 43, 462–466. doi:10.1016/j.joen.2016.10.039
Drukteinis, S., Peciuliene, V., Dummer, P. M. H., and Hupp, J. (2019). Shaping ability of BioRace, ProTaper NEXT and Genius nickel-titanium instruments in curved canals of mandibular molars: a MicroCT study. Int. Endod. J. 52, 86–93. doi:10.1111/iej.12961
Freire, L. G., Gavini, G., Cunha, R. S., and Santos, Md (2012). Assessing apical transportation in curved canals: comparison between cross-sections and micro-computed tomography. Braz Oral Res. 26, 222–227. doi:10.1590/s1806-83242012000300007
Gagliardi, J., Versiani, M. A., de Sousa-Neto, M. D., Plazas-Garzon, A., and Basrani, B. (2015). Evaluation of the shaping characteristics of ProTaper Gold, ProTaper NEXT, and ProTaper universal in curved canals. J. Endod. 41, 1718–1724. doi:10.1016/j.joen.2015.07.009
Gambill, J. M., Alder, M., and Rio, C. E. (1996). Comparison of nickel-titanium and stainless steel hand-file instrumentation using computed tomography. J. Endod. 22, 369–375. doi:10.1016/s0099-2399(96)80221-4
Generali, L., Checchi, V., Borghi, A., La Rosa, G. R. M., Conte, G., Zavattini, A., et al. (2023). Shaping ability of Procodile and R6 Reziflow nickel-titanium reciprocating instruments in curved mesial root canals of mandibular molars: a MicroCT study. Microsc. Res. Tech. 86, 1345–1352. doi:10.1002/jemt.24326
Greco, K., and Cantatore, G. (2014). A critical approach to the root canal obturation techniques. G. Ital. Endod. 28, 48–78. doi:10.1016/j.gien.2014.09.002
Guedes, I. G., Rodrigues, R. C. V., Marceliano-Alves, M. F., Alves, F. R. F., Rôças, I. N., and Siqueira, J. F. (2022). Shaping ability of new reciprocating or rotary instruments with two cross-sectional designs: an ex vivo study. Int. Endod. J. 55, 1385–1393. doi:10.1111/iej.13834
Hwang, Y. H., Bae, K. S., Baek, S. H., Kum, K. Y., Lee, W., Shon, W. J., et al. (2014). Shaping ability of the conventional nickel-titanium and reciprocating nickel-titanium file systems: a comparative study using micro-computed tomography. J. Endod. 40, 1186–1189. doi:10.1016/j.joen.2013.12.032
Iacono, F., Pirani, C., Generali, L., Bolelli, G., Sassatelli, P., Lusvarghi, L., et al. (2017). Structural analysis of HyFlex EDM instruments. Int. Endod. J. 50, 303–313. doi:10.1111/iej.12620
Lopes, R. M. V., Marins, F. C., Belladonna, F. G., Souza, E. M., De-Deus, G., Lopes, R. T., et al. (2018). Untouched canal areas and debris accumulation after root canal preparation with rotary and adaptive systems. Aust. Endod. J. 44, 260–266. doi:10.1111/aej.12237
Martins, J. N. R., Silva, EJNL, Marques, D., Ajuz, N., Rito Pereira, M., Pereira da Costa, R., et al. (2023). Characterization of the file-specific heat-treated ProTaper Ultimate rotary system. Int. Endod. J. 56, 530–542. doi:10.1111/iej.13880
microCT, B. (2017) MicroCT 3D registration after tooth root canal procedures: removed volume, drill debris and touched/untouched surfaces, Method note MN110. Available at: https://www.foa.unesp.br/Home/pesquisa/escritoriodeapoioapesquisa/mn110_endodontic-root-canal-analysis-debris-and-untouched-surfaces.pdf.
Pawar, A. M., Pawar, M., Kfir, A., Singh, S., Salve, P., Thakur, B., et al. (2017). Root canal morphology and variations in mandibular second molar teeth of an Indian population: an in vivo cone-beam computed tomography analysis. Clin. Oral Investig. 21, 2801–2809. doi:10.1007/s00784-017-2082-6
Pedullà, E., Plotino, G., Grande, N. M., Avarotti, G., Gambarini, G., Rapisarda, E., et al. (2016). Shaping ability of two nickel-titanium instruments activated by continuous rotation or adaptive motion: a micro-computed tomography study. Clin. Oral Investig. 20, 2227–2233. doi:10.1007/s00784-016-1732-4
Peters, O. A. (2004). Current challenges and concepts in the preparation of root canal systems: a review. J. Endod. 30, 559–567. doi:10.1097/01.don.0000129039.59003.9d
Peters, O. A., Peters, C. I., Schönenberger, K., and Barbakow, F. (2003). ProTaper rotary root canal preparation: effects of canal anatomy on final shape analysed by micro CT. Int. Endod. J. 36, 86–92. doi:10.1046/j.1365-2591.2003.00626.x
Pirani, C., Iacono, F., Generali, L., Sassatelli, P., Nucci, C., Lusvarghi, L., et al. (2016). HyFlex EDM: superficial features, metallurgical analysis and fatigue resistance of innovative electro discharge machined NiTi rotary instruments. Int. Endod. J. 49, 483–493. doi:10.1111/iej.12470
Pirani, C., Zamparini, F., Peters, O. A., Iacono, F., Gatto, M. R., Generali, L., et al. (2019). The fate of root canals obturated with Thermafil: 10-year data for patients treated in a master's program. Clin. Oral Investig. 23, 3367–3377. doi:10.1007/s00784-018-2756-8
Rubio, J., Zarzosa, J. I., Aranda, S., Casino, A., and Pallarés, A. (2022). A comparative study of cyclic fatigue of 6 endodontic systems. An in vitro study. J. Clin. Exp. Dent. 14, e560–e565. doi:10.4317/jced.59747
Ruddle, C. J., Machtou, P., and West, J. D. (2022) Deep shape in endodontics. Significance, rationale and benefit, dentistry today. Available at: https://www.endoruddle.com/tc2pdfs/249/DeepShape_Jan2022.pdf.
Schilder, H. (1974). Cleaning and shaping the root canal. Dent. Clin. N. Am. 18, 269–296. doi:10.1016/s0011-8532(22)00677-2
Schneider, S. W. (1971). A comparison of canal preparations in straight and curved root canals. Oral Surg. Oral Med. Oral Pathol. 32, 271–275. doi:10.1016/0030-4220(71)90230-1
Shah, D. Y., Wadekar, S. I., Dadpe, A. M., Jadhav, G. R., Choudhary, L. J., and Kalra, D. D. (2017). Canal transportation and centering ability of protaper and self-adjusting file system in long oval canals: an ex-vivo cone-beam computed tomography analysis. J. Conserv. Dent. 20, 105–109. doi:10.4103/0972-0707.212234
Shen, Y., and Haapasalo, M. (2008). Three-dimensional analysis of cutting behavior of nickel-titanium rotary instruments by microcomputed tomography. J. Endod. 34, 606–610. doi:10.1016/j.joen.2008.02.025
Shen, Y., Zhou, H. M., Zheng, Y. F., Peng, B., and Haapasalo, M. (2013). Current challenges and concepts of the thermomechanical treatment of nickel-titanium instruments. J. Endod. 39, 163–172. doi:10.1016/j.joen.2012.11.005
Silva, EJNL, Ajuz, N. C., Martins, J. N. R., Antunes, B. R., Lima, C. O., Vieira, V. T. L., et al. (2023). Multimethod analysis of three rotary instruments produced by electric discharge machining technology. Int. Endod. J. 56, 775–785. doi:10.1111/iej.13915
Silva, EJNL, Pinto, K. P., Ferreira, C. M., Belladonna, F. G., De-Deus, G., Dummer, P. M. H., et al. (2020). Current status on minimal access cavity preparations: a critical analysis and a proposal for a universal nomenclature. Int. Endod. J. 53, 1618–1635. doi:10.1111/iej.13391
Siqueira, J. F., Alves, F. R., Versiani, M. A., Rôças, I. N., Almeida, B. M., Neves, M. A., et al. (2013). Correlative bacteriologic and micro-computed tomographic analysis of mandibular molar mesial canals prepared by self-adjusting file, reciproc, and twisted file systems. J. Endod. 39, 1044–1050. doi:10.1016/j.joen.2013.04.034
Siqueira, J. F., and Rôças, I. N. (2008). Clinical implications and microbiology of bacterial persistence after treatment procedures. J. Endod. 34, 1291–1301.e3. doi:10.1016/j.joen.2008.07.028
Sousa-Neto, M. D., Silva-Sousa, Y. C., Mazzi-Chaves, J. F., Carvalho, K. K. T., Barbosa, A. F. S., Versiani, M. A., et al. (2018). Root canal preparation using micro-computed tomography analysis: a literature review. Braz Oral Res. 18, e66. doi:10.1590/1807-3107bor-2018.vol32.0066
Yang, Y., Shen, Y., Ma, J., Cao, Y., and Haapasalo, M. (2016). A micro-computed tomographic assessment of the influence of operator’s experience on the quality of waveone instrumentation. J. Endod. 42, 1258–1262. doi:10.1016/j.joen.2016.04.020
Yeniçeri Özata, M., Falakaloğlu, S., Keleş, A., Adıgüzel, Ö., and Gündoğar, M. (2023). Evaluation of shaping ability of different glide path instruments: a micro-computed tomography study. BMC Oral Health 23, 780. doi:10.1186/s12903-023-03529-3
Zhao, D., Shen, Y., Peng, B., and Haapasalo, M. (2014). Root canal preparation of mandibular molars with 3 nickel-titanium rotary instruments: a micro-computed tomographic study. J. Endod. 40, 1860–1864. doi:10.1016/j.joen.2014.06.023
Keywords: NiTi, shaping ability, thermally treated NiTi, endodontics, micro-CT
Citation: Greco K, Iacono F, Montagna F, Esposito Corcione C, Paolone G, Gherlone E and Cantatore G (2024) Shaping ability of ProTaper Ultimate and BlueShaper in mandibular molars: a micro-CT evaluation. Front. Mater. 11:1363835. doi: 10.3389/fmats.2024.1363835
Received: 31 December 2023; Accepted: 29 February 2024;
Published: 08 April 2024.
Edited by:
Giusy Rita Maria La Rosa, Università degli Studi di Catania, ItalyReviewed by:
Luca Testarelli, Sapienza University of Rome, ItalyCopyright © 2024 Greco, Iacono, Montagna, Esposito Corcione, Paolone, Gherlone and Cantatore. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Francesco Iacono, ZnJhbmNlc2NvLmlhY29ub0Bob3RtYWlsLml0
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.