
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Mater. , 09 June 2023
Sec. Biomaterials and Bio-Inspired Materials
Volume 10 - 2023 | https://doi.org/10.3389/fmats.2023.1177468
Background: Guidewire fracture and dislodgment are very rare but can cause serious complications.
Method: A case was reported where part of the guidewire was blocked to the posterior tibial. We attempted to remove it using a Solitaire AB Neurovascular Remodeling Device.
Result: A Solitaire AB Neurovascular Remodeling Device was successfully used to remove the fracture and dislodgment of a guidewire. There were no complications during the removal of the guidewire.
Conclusion: A Solitaire AB can be used to remove a fractured guidewire, which is a simple and effective method to reduce complications. The Solitaire stent gradually crimped and tightened to form a dense inverted conical meshwork, similar to the “trans embolic protection device.” We can use minimally invasive methods to remove a broken and displaced guidewire within the vascular lumen.
With the introduction and widespread use of vascular intervention, the application of catheter-directed thrombolysis to treat peripheral vascular disease has increased. The infusion catheter fully contacts the target lesions and perfuses the therapeutic drugs. This method can effectively and safely treat the disease (Shammas et al., 2008). However, if a guidewire catheter is fractured and dislodged during the operation, many serious complications may occur, such as displacement embolism, bleeding, and vascular dissection (Orief et al., 2011). In particular cases, these complications may be life-threatening. Here we report a case in which a guidewire was fractured and dislodged, and we used the Solitaire AB stent to remove it from the posterior tibial.
A 52-year-old male patient was admitted to our department from the outpatient clinic on 24 November 2020. The patient had the symptom of 2 years of lameness with numbness between the lower extremities. Two years ago, the patient had intermittent claudication of both lower extremities without obvious inducement. In the beginning, the patient felt swelling pain in both lower limbs when walking for 500 m. The claudication distance gradually decreased, and he could only walk about 50 m when he was seen. Three weeks earlier, the patient developed pain in the right fourth toe on the right foot, which became more obvious at night and was accompanied by ulceration. The skin around the ulceration gradually turned gangrenous. The patient was admitted to the outpatient clinic of our department for further treatment. In the course of the disease, the patient had no chills and fever, chest tightness, asthma, nausea and vomiting, no abdominal distension and abdominal pain, no diet and sleep, no urine, normal stool, no significant recent weight loss, and no abnormal mental state. The patient had an 11-year history of diabetes and underwent hemodialysis for chronic kidney disease 7 years ago. In 2017, he underwent coronary artery bypass grafting for acute myocardial infarction.
After admission, we gave the patient a physical examination. The skin of the bilateral groin area was intact, the femoral arteries on both sides were accessible but weak, the pulsations of the bilateral popliteal arteries and dorsal foot arteries were not palpable, and the skin temperature, color, and feeling of the left lower extremity were acceptable. The right calf had low skin temperature, cyanosis, hypersensitivity, and poor peripheral blood supply, and the fourth toe was black and ulcerated. There was no obvious exudation around. The ABI of both lower limbs was not detected. Color Doppler ultrasound of the right lower limb on 17 November 2020 indicated arteriosclerosis of the right lower limb with multiple hard plaque formations (conforming to changes in arteriosclerosis obliterans), and the diameter of the posterior tibial artery on the right side became narrow. The deep vein of the right lower limb was not seen as abnormal. The angiography of both lower extremities in the local hospital showed extensive atherosclerotic plaques in the bilateral femoral arteries with stenosis, obvious stenosis of the upper end of the right femoral artery, occlusion of the lower end of the bilateral femoral arteries, and obvious collateral circulation.
The study was approved by the ethics committee of our hospital (KY20201124-11). After admission, relevant laboratory examinations were completed on the day. The results of the laboratory examination are as follows: neutrophils 79.40%, hemoglobin 93 g/L, glutamyl transpeptidase 268.00 U/L, alkaline phosphatase 222.00 U/L, urea 19.25 mmol/L, creatinine 498.00 μm mol/L, PT 14.10 s, and APTT 58.40 s. The patient was given aspirin to decrease platelets, atorvastatin calcium tablets to lower lipids, and methylcobalamin tablets to nourish nerves. At the same time, we gave him symptomatic treatments, including blood pressure control, blood sugar adjustment, and hemodialysis.
A CTA examination of lower extremity arteries was performed on 25 November 2020, and the inspection report showed arteriosclerosis obliterans in both lower extremities. The left common iliac artery, bilateral femoral artery, and popliteal artery had multiple localized stenoses. The upper segment of the left femoral artery and the left anterior tibial artery were segmentally occluded. Combined with the ABI and CTA examinations of the patient, we considered multiple localized stenoses of the left common iliac artery, bilateral femoral artery, and popliteal artery. Considering the patient’s medical history, the risk of cerebrovascular accidents during the intervention was relatively high. After sufficient communication with the patient and family members, we planned to perform angiography in both lower extremity arteries to clarify the scope of the disease. As the patient felt more severe symptoms on the right side and had symptoms of gangrene in the fourth toe on the right side, this angiographic examination and treatment mainly focused on the lesions of the right lower limb.
After completing the relevant assessment, the patient underwent the first interventional surgery on 30 November 2020. The patient was placed in a supine position, and his left groin area was routinely sterilized. We inserted a 5F short sheath and placed a 4F pigtail catheter in the lower part of the abdominal aorta for the angiography of the abdominal aorta and iliac artery. Then, we replaced the short sheath with a 6F long sheath (Terumo, Japan) and placed the tips of both the sheath and the pigtail catheter on the right iliac artery for further angiography. After clarifying the location and scope of the lesion, we introduced a 4F Hunter’s head catheter and microcatheter (Progreat, Terumo, Japan). The guidewire was used to pass through the right superficial femoral artery occlusion segment. After confirming that the microcatheter was in the true cavity, we replaced the V18 guidewire and placed the tip of the wire on the right popliteal artery. Meanwhile, a 2.5 mm × 150 mm, 4 mm × 150 mm balloon catheter (Savy Long, Cordis) was introduced through the guidewire to expand the occluded segment step by step, and the site was re-examined by sheath angiography. The guidewire was introduced into the 4F perfusion catheter. Finally, we kept the thrombolytic catheter and long sheath, bandaged the device, and returned the patient to the ward for further treatment. Papaverine was pumped to the patient through the thrombolytic catheter after the operation.
The patient underwent the second interventional operation on the morning of 1 December 2020. The patient was placed in a supine position, and the right lower limb artery angiography was performed through the reserved thrombolytic catheter. The tip of the guidewire fractured during the withdrawal of the occluded guidewire, and a fragment of the guidewire fell off and flowed to the P1 segment of the popliteal artery due to the blood flow (Figure 1). We tried to use the anterior loop of the exchange guidewire to intercept the broken tip of the occluded guidewire and pull it out of the arterial lumen to prevent it from drifting further, but we failed. At this time, the tip of the fractured occluding guidewire gradually shifted forward along the direction of blood flow and reached the posterior tibial a few minutes later. We repeated the attempt to use the conventional exchange guidewire but failed to grasp the broken tip of the occluding guidewire.
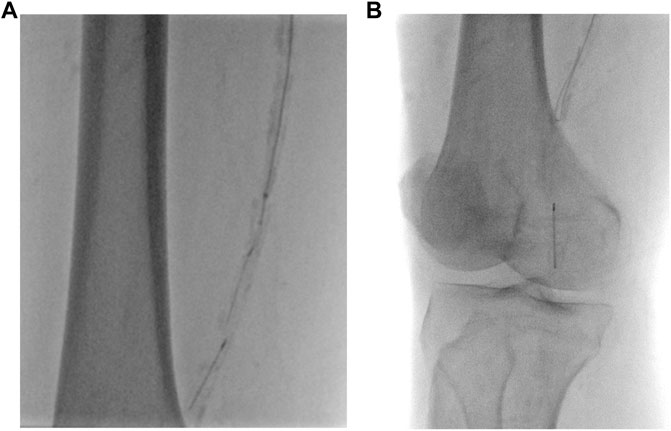
FIGURE 1. The tip of the guidewire was fractured during the withdrawal of the occluded guidewire. (A) The tip of the guidewire was fractured and dislodged. (B) Unsuccessfully attempting to use the exchange guidewire to intercept the fractured guidewire.
We placed the 6F vascular long sheath (Terumo, Japan) above the fractured guidewire (approximately the level of the P2 section of the popliteal artery) and placed a single-curved catheter near the broken guidewire. We fed the micro-guidewire and micro-catheter (Progreat, Terumo, Japan) to the bottom of the fractured guidewire through the single-curved catheter, withdrew the micro-guidewire, and delivered the Solitaire AB Neurovascular Remodeling Device (Solitaire AB 4.0 mm × 20 mm, eV3, United States) through the micro-catheter to the right side of the tibia and fibula to trap the tip of the broken guidewire. Due to the large angle (approximately 120°) at the tip end of the broken guidewire, the resistance against retrieving the guidewire into the 6F long sheath was relatively large, and it could not be retracted into the sheath together with the Solitaire stent. Therefore, we used a guidewire to bypass the catheter to the P1 segment of the popliteal artery while retaining the guidewire, slowly withdrawing the 6F long sheath, microcatheter, and Solitaire AB system (Figure 2). The withdrawal process was carried out under radiography to ensure the entire system did not damage the endothelium. After removing the fractured guidewire, the 6F long sheath (Terumo, Japan) and the 4F MPA catheter were introduced through the retained exchange guidewire. The tip of the catheter was placed in the right popliteal artery segment, and the protective umbrella (Spider 6mm, ev3, United States) was introduced through the catheter to the right popliteal artery. It was realized that balloon dilation was safe. A 4.0 mm × 20 mm balloon dilatation catheter (Viatrac 14 Plus, Abbott) and a 5.0 mm × 150 mm balloon dilatation catheter (Cordis, SAVY LONG, United States) were introduced through the umbrella guidewire for further expansion. We also exchanged the stent delivery system again. A 6 mm × 150-mm stent (SMART, Cordis, United States) was implanted at the anchoring site under radiography, and a 5.0 mm × 150 mm balloon dilatation catheter (Cordis, SAVY LONG, United States) was introduced again to the stenosis area (Figure 3). After the expansion, angiography of the right lower extremity artery was performed, indicating that the right superficial femoral artery was well developed. There was no sign of contrast agent overflow, the stent was patent, the residual stenosis was less than 10%, and the right dorsal vascular network was more clear than pre-operation. Finally, the puncture point was sealed with a vessel closure device (Angioseal, Terumo, Japan). The patient returned to the ward without discomfort.
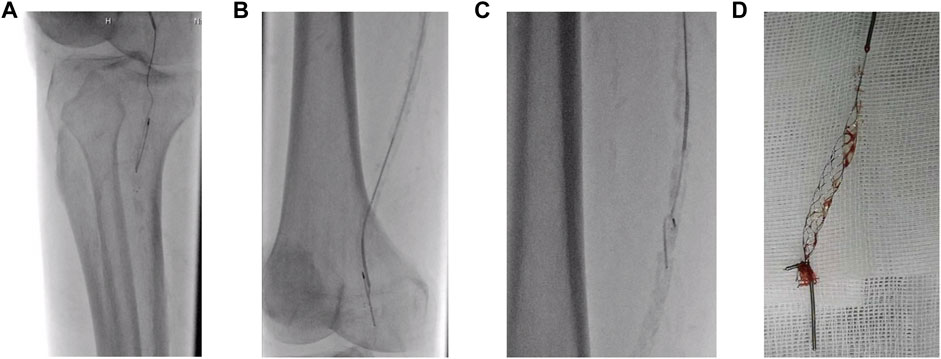
FIGURE 2. Process of successfully removing a fractured guidewire using Solitaire AB. (A) Using Solitaire AB to capture the guidewire successfully. (B,C) The Solitaire AB stent was used to pull the fractured guidewire out of the body under radiography. (D) The fractured guidewire has been removed, and the Solitaire AB stent remains.
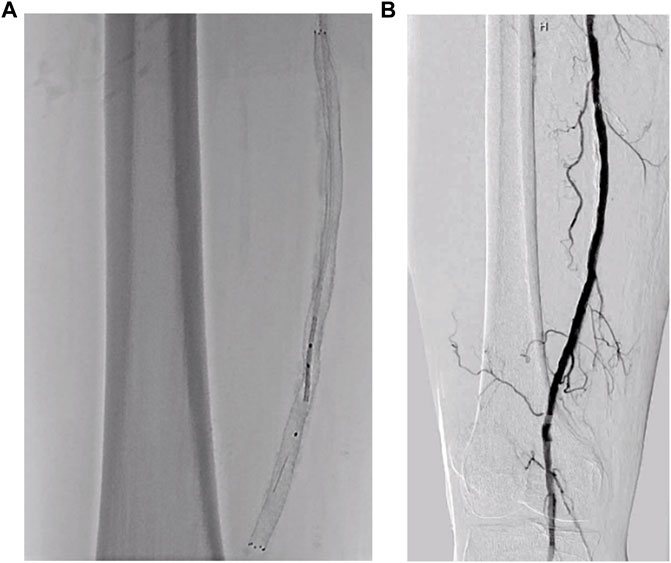
FIGURE 3. Balloon dilatation and stent implantation. (A) The stent was released under the protective umbrella. (B) The angiographic review after the stent implantation shows that the blood flow of the right femoral artery has significantly improved.
After the operation, the patient’s condition was stable. We measured the ABI on the right as 0.62. The skin temperature of the right limb was improved and higher than the left side. The patient was discharged from the hospital 10 days after the operation and was followed in the outpatient clinic after discharge. The patient is still being followed.
Since the successful implementation of STILE and TOPAS trials in the 1990s, catheter-directed thrombolysis (CDT) has become an important treatment method for acute arterial ischemic diseases (McNamara and Fischer, 1985; Weaver et al., 1996). For patients with atherosclerotic occlusion, the use of catheterization can perfuse the drug to the target site more specifically. At the same time, angiography assessment can also be performed during local medication to expose specific vascular lesions. With the wide application of CDT technology, the reporting of related complications has also increased. At present, there is no report about the fracture or dislodgment of the occluding guidewire. However, according to the clinical study of Khonsari et al., the probability of guidewire fracture during the percutaneous coronary intervention is about 0.1–0.2% (Khonsari et al., 1986). Once the occlusion guidewire is fractured, it can cause serious and even fatal complications such as embolism, thrombosis, vascular injury, perforation, and bleeding.
The fracture of the guidewire in this case report may be due to the following reasons. The tip of the guidewire is made of spring coils that are entangled with the atherosclerotic plaque during the withdrawal process, or the tip of the guidewire may become incarcerated with the thrombolytic catheter, and the spring coil at the head end is stretched until it peels off during the pulling process. The fractured guidewire should be taken out of the body as quickly as possible; however, traditional surgical treatment is more complicated and has a higher incidence of complications. At present, the common interventional methods to remove intravascular foreign matters include the following: 1. Gooseneck or other catchers. The gooseneck is used to grasp the foreign body. The diameter of the snare part at the head is 15 mm. A coronary artery snare with a head end diameter of 5 mm is used for capture. However, if the guidewire enters a smaller branch, the gooseneck often cannot be deployed. Forcing the snare tip to enter the secondary branches has the risk of damaging vessels. 2. Biopsy forceps. This involves clamping the broken guidewire head end with biopsy forceps and then removing it. However, this method has the risk of vascular injury, and it is also difficult to be widely used in small vascular branches. This method highly relies on the experience of the surgeon. 3. Multi-guidewire winding technology. Trehan et al. reported wrapping a guidewire around the ruptured balloon to make it whole and then pulling it out of the body (Trehan et al., 2003). This method has a better effect on the ruptured balloon. Because the fractured guidewire has no supporting point and is easy to slide, this method is often difficult to connect the guidewire with it as a whole, and it is easy to cause the guidewire to flow with the blood into more branches. We can use a gooseneck trap to catch the displaced broken guidewire. This method is more effective for thick blood vessels, but foreign objects often reach the distal branch of the blood vessel with the blood flow. At this time, due to the diameter of the gooseneck snare often being 10–12 mm, the distal branch of the blood vessel is often too small to use the snare to remove the foreign object. The gooseneck trap is composed of a single or three-ring platinum and nickel–titanium alloy interwoven twisted cable, which can effectively capture, has strong capture power, and is often used for filter recycling. However, due to the lack of a good force point for the broken guidewire and the short length in this case, the gooseneck trap at the far end of the branch often cannot be used.
The Solitaire AB stent is a laser-engraved self-expandable stent that can be delivered and released through a microcatheter with satisfactory control performance (Roth et al., 2010). A Solitaire stent can straddle both ends of a fractured guidewire to remove it. At the same time, the Solitaire AB stent has a closed mesh roll-on design that can be completely released and recovered before being released. Furthermore, three of the four developed marks can be seen on the distal end of the stent, which allows more precise positioning. In terms of mechanism of action, ordinary stents utilize the radial support force of the stent itself to achieve vascular patency after implantation into blocked blood vessels, and the stent cannot be retrieved after placement. Embolization uses a retrievable stent that can be inserted into the mesh structure of the stent after being placed in the displaced blood vessel of the foreign object while also retracting as a whole. Therefore, it is minimally invasive and efficient.
In this article, we introduce a minimally invasive intracavitary treatment method to reduce the occurrence of serious complications. After analyzing the reason for and removal of the broken guidewire in this case, the following measures are suggested to reduce the possibility of a guidewire fracture: 1. Avoid forcibly pulling the guidewire during the removal of the guidewire, especially if resistance is felt at the same time. Remove guidewire under angiography. 2. Avoid excessive clamping or twisting of the guidewire that might change its physical properties. In clinical practice, wire breakage in the vascular lumen is a complication that can have serious consequences.
The original contributions presented in the study are included in the article/Supplementary Material; further inquiries can be directed to the corresponding author.
The studies involving human participants were reviewed and approved by the Ethics Committee of the Nanjing First Hospital, Nanjing Medical University. The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
ZL, BZ, and XH completed the surgical procedures, with ZL, MG, and JG participating in the writing of the article. JK made revisions to the article and put forward suggestions. All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
This work was supported by a grant from the Science and Technology Development Foundation Project of Nanjing Medical University (No. NMUB20210212).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors, and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Khonsari, S., Livermore, J., Mahrer, P., and Magnusson, P. (1986). Fracture and dislodgment of floppy guidewire during percutaneous transluminal coronary angioplasty. Am. J. Cardiol. 58, 855–856. doi:10.1016/0002-9149(86)90370-x
McNamara, T. O., and Fischer, J. R. (1985). Thrombolysis of peripheral arterial and graft occlusions: Improved results using high-dose urokinase. AJR Am. J. Roentgenol. 144, 769–775. doi:10.2214/ajr.144.4.769
Orief, T., Bin-Nafisah, S., Almusrea, K., and Alfawareh, M. (2011). Guidewire breakage: An unusual complication of anterior odontoid cannulated screw fixation. Asian Spine J. 5 (4), 258–261. doi:10.4184/asj.2011.5.4.258
Roth, C., Papanagiotou, P., Behnke, S., Walter, S., Haass, A., Becker, C., et al. (2010). Stent-assisted mechanical recanalization for treatment of acute intracerebral artery occlusions. Stroke 41, 2559–2567. doi:10.1161/strokeaha.110.592071
Shammas, N. W., Dippel, E. J., Shammas, G., Gayton, L., Coiner, D., and Jerin, M. (2008). Dethrombosis of the lower extremity arteries using the power-pulse spray technique in patients with recent onset thrombotic occlusions: Results of the DETHROMBOSIS registry. J. Endovasc. Ther. 15, 570–579. doi:10.1583/08-2453.1
Trehan, V., Mukhopadhyay, S., Yusuf, J., C. Ramgasetty, U., Mukherjee, S., and Arora, R. (2003). Intracoronary fracture and embolization of a coronary angioplasty balloon catheter: Retrieval by a simple technique. Catheter Cardiovasc Interv. 58, 473–477. doi:10.1002/ccd.10477
Weaver, F. A., Comerota, A. J., Youngblood, M., Froehlich, J., Hosking, J. D., Papanicolaou, G., et al. (1996). Surgical revascularization versus thrombolysis for nonembolic lower extremity native artery occlusions: Results of a prospective randomized trial. J. Vasc. Surg. 24, 513–523. doi:10.1016/s0741-5214(96)70067-8
Keywords: solitaire AB neurovascular remodeling device, fracture, embolism, guidewire, retrieval
Citation: Liu Z, Zhao B, He X, Gu J, Gong M and Kong J (2023) Fracture and dislodgment of a guidewire retrieved by a Solitaire AB neurovascular remodeling device. Front. Mater. 10:1177468. doi: 10.3389/fmats.2023.1177468
Received: 02 March 2023; Accepted: 25 May 2023;
Published: 09 June 2023.
Edited by:
Luiz Fernando Romanholo Ferreira, Tiradentes University, BrazilReviewed by:
Abbas Rahdar, Zabol University, IranCopyright © 2023 Liu, Zhao, He, Gu, Gong and Kong. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jie Kong, a2lsb2dyYW1AMTYzLmNvbQ==
†ORCID: Zhengli Liu, orcid.org/0000-0002-5157-2768; Xu He, orcid.org/0000-0003-0241-6694; Maofeng Gong, orcid.org/0000-0003-0781-0682; Jianping Gu, orcid.org/0000-0001-9683-6053; Jie Kong, orcid.org/0000-0003-0241-6694
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.