- 1Department of Medical Education, the Anne Burnett Marion School of Medicine at Texas Christian University, Fort Worth, TX, United States
- 2Department of Pediatrics, the Anne Burnett Marion School of Medicine at Texas Christian University, Fort Worth, TX, United States
The increasing demand for natural products in the United States reflects a cultural shift towards health and sustainability. This trend infiltrates consumer sectors such as the sunscreen industry, amidst concerns about health and environmental impacts of chemical ingredients. The Hawaii Sunscreen Ban has intensified sunscreen formula safety discussions, particularly regarding butylparaben, oxybenzone, and octinoxate. Even at low concentrations, these compounds bleach hard corals eventually leading to their death. As well, these chemicals pose threats to marine ecosystems and raise concerns about human health, particularly systemic absorption and the possibility of causing endocrine disruption. While some argue for chemical-based sunscreens for skin cancer prevention, others advocate for mineral-based alternatives that avoid harmful ingredients. However, public opinion on sunscreen varies, influenced by adverse reactions, socioeconomic status, gender, and cultural perceptions. Future studies should explore diverse demographic perspectives and long-term health and environmental impacts of products containing potentially toxic ingredients. As well, effective communication strategies to promote sunscreen safety and encourage sustainable sun protection practices is needed.
Introduction
One sector that has suffered considerable debate is the sunscreen industry. Up to 6,000 tons of sunscreen – more than the weight of 50 blue whales – wash through U.S. reef areas every year, according to the National Park Service (Coral Disease & Health Consortium, 2023). Scientists have known for some time that oxybenzone, an organic compound found in many sunscreens, can damage corals. Independent testing of sun care products uncovered concerning levels of benzene contamination, raising serious questions about the safety of these products for consumers (Hudspeth et al., 2022). In response, the U.S. Food and Drug Administration (2021) has urged manufacturers to address the potential for benzene contamination and implement preventive measures. As a result, sunscreens with this compound have been banned in the U.S. Virgin Islands, Hawaii, the island nation of Palau, and Bonaire, an island municipality of the Netherlands, among other places. A study conducted by Downs et al., 2022 concluded that beach sands directly in the discharge of beach showers on three of the islands of Hawaii (Maui, Oahu, Hawai’i) were found to be contaminated with multiple petrochemical-based UV-filters that are found in sunscreens. Risk assessments for both sand and water samples at the sampling sites had a Risk Quotient > 1, indicating that these chemicals could pose a serious threat to coral reef habitats.
The chemicals in sunscreens can cause coral bleaching by inducing DNA damage, hormonal disruption, oxidative stress, inhibition of photosynthesis, increased disease susceptibility, and exacerbation of heat stress. These mechanisms collectively compromise coral health and lead to the expulsion of symbiotic algae, resulting in the characteristic whitening of bleached corals (Figure 1) (Danovaro et al., 2008). An example is seen with oxybenzone, a chemical designed to dissipate the light energy as heat, preventing sunburn. Within the coral and after exposure to sunlight, oxybenzone is metabolized to a reactive intermediate which produces damaging radicals. Symbiotic algae, a coral defense mechanism, appears to sequester the oxybenzone metabolites. As ocean water warms, stressed corals expel their algae symbiotes which then, leaves bone-white coral skeletons (Stanford University, 2022). Even at extremely low concentrations, organic ultraviolet filters in sunscreens are able to induce the lytic viral cycle in symbiotic zooxanthellae with latent infections, promoting viral infection (Danovaro et al., 2008).
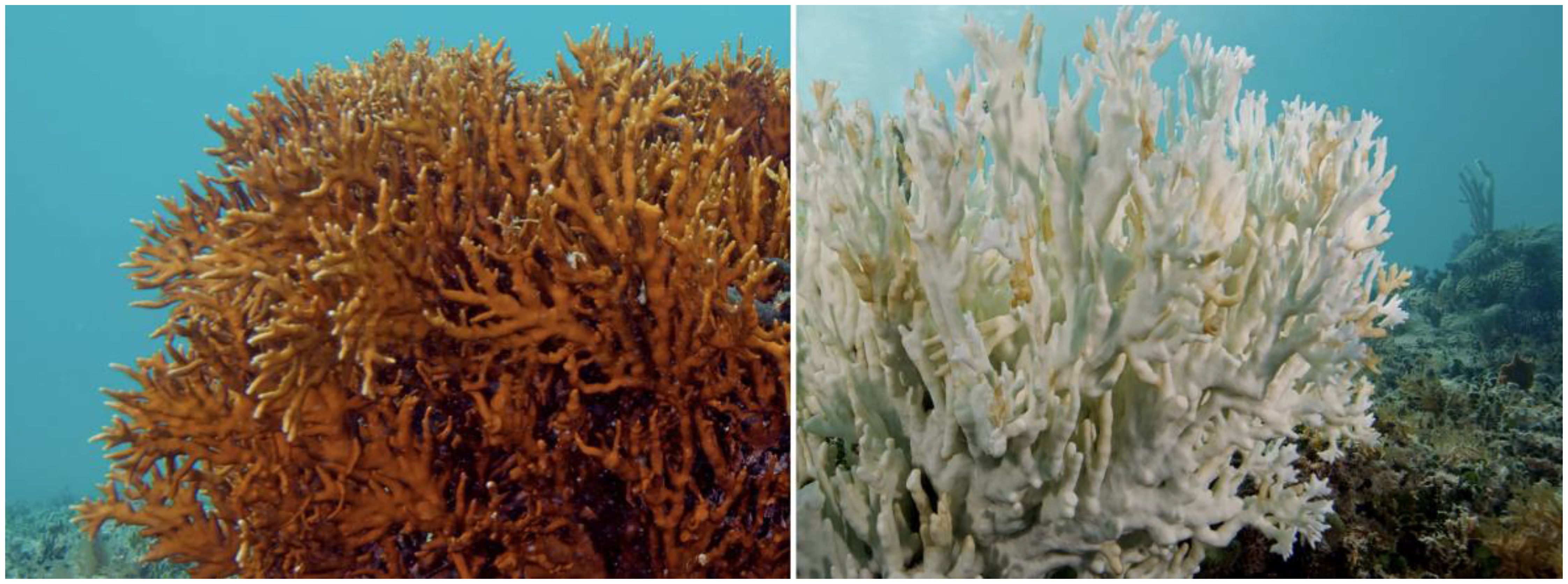
Figure 1. (Dasgupta, 2015). Photo by the XL Catlin Seaview Survey.
If the coral reefs are threatened by these UV filters, it is reasonable to question whether the same toxic effects may be applicable to the humans who apply them directly to their skin. In a study conducted by Matta et. al., (2020) 48 randomized participants were exposed to 1 of 4 sunscreen products. Via blood testing, they found that the mean maximum plasma concentrations of all 6 active ingredients (avobenzone, oxybenzone, octocrylene, homosalate, octisalate, and octinoxate) were greater than 0.5 ng/mL, and this threshold was surpassed on day 1 after a single application. This demonstrates that after percutaneous administration, that these xenobiotics are reaching the systemic circulation. Some sources have deemed these UV filters to be endocrine disruptors (EDs) based on in vitro and animal models (Lorigo et al., 2018). Attempts have been made to identify criteria by which a substance shall be considered as having ED properties (Onyango et al., 2023). In summary, such as a substance must meet all the following criteria: (1) show an adverse biologic effect (e.g., a change in morphology, physiology, organ function; (2) have an endocrine mode of action, and (3) the adverse effect is a direct consequence of the mode of action.
While these xenobiotics are believed to have the potential to cause significant harm to human health, the available data appear to be somewhat equivocal. For example, data from previous in vitro and cell-based bioassays have demonstrated the potential of oxybenzone to mimic estrogen, interfere with testosterone production, and disrupt adrenal hormones (Wang et al., 2016). However, a more recent systematic review published by Suh et al. (2020) of 29 published human studies revealed that current evidence is not sufficient to support the causal relationship between the elevated levels of oxybenzone in the body and impact on thyroid hormone function as well as male and female reproductive function. While the potential for oxybenzone and other UV filters contained in some sunscreen products have the potential to adversely affect human health, controlled clinical trials will be required to prove their causative association.
The fact that potentially harmful sunscreen constituents (e.g., oxybenzone, avobenzone) are absorbed systemically (Sander et al., 2020), the risk profile of systemic toxicity for these xenobiotics may be very different in adults vs. infants and children. As recently reviewed by Druml et al. (2023), both the American Academy of Pediatrics and the American Academy of Dermatology recommend the routine use of sunscreen products in children over the age of six months. Based on well described developmental differences in the structure of the dermis, young infants may, hypothetically, be at greater risk for developing adverse dermal and systemic adverse effects to the potentially injurious xenobiotics contained in some sunscreen products. It is well known that as compared to adults, neonates and young infants have a higher skin surface area to body ratio. As recently reviewed by Yun et al. (2022), differences in stratum corneum thickness (i.e., lower in infants) and skin hydration ratio in early life would be expected to increase both the rate and extent of percutaneous absorption of both hydrophilic and hydrophobic xenobiotics. Consequently, for a given application of sunscreen products to an infant, it is likely that systemic concentrations of agents capable of ED would be higher than those observed in adults, thus increasing the chance of adverse effects. Moreover, the gap between sunscreen application in theory and practice adds to the complexity, as incorrect, excessive usage can leave individuals exposed to harmful contaminants (Petersen and Wulf, 2014).
Public opinion regarding chemical sunscreen, particularly after the Hawaii sunscreen ban, has been mixed. The ban, which prohibits the sale of sunscreens containing oxybenzone and octinoxate due to their harmful effects on coral reefs, sparked research into the public’s concern for environmental issues, the extent to which these concerns may influence consumer behavior, and the willingness of consumers to pay for alternative products. One study showed that 96% of people would buy coral safe sunscreen with an accumulated average premium of $17. 9% and also, that they would support a ban of coral toxic sunscreens in their area (Woodruff, 2019). In short, the Hawaii sunscreen ban has increased awareness of the potential adverse effect of many products on the environment and human health. As well it has increased interest in alternative “reef-safe” sunscreen products and greater scrutiny of applicable regulations, policies and practices.
Toxicity analysis
There are varying opinions regarding the risk associated with use of chemical-based sunscreens including benzene derivatives. One viewpoint emanates from the knowledge that benzene is a known human carcinogen. The U.S. Food and Drug Administration (FDA) prohibits companies from intentionally adding benzene to regulated products, with one narrow exception. Specifically, when benzene use is unavoidable for manufacturing a product that represents a “significant therapeutic advance,” it may be present at concentrations up to 2ppm (Nicole, 2022). Given that sunscreen offers UVA/UVB protection which ultimately, reduces the chance for development of skin cancer, benzene is permitted within its formulation. However, it is misleading to conclude that benzene is “unavoidable for manufacturing”, as there are effective mineral based sunscreens that do not contain benzene or other chemical congeners and/or compounds associated with the production of endocrine disruption (Nicole, 2022).
Oxybenzone (Benzophenone-3) is a human and environmental contaminant used in many sunscreen formulations to protect against the damaging effects of ultraviolet radiation. It should be known that oxybenzone and avobenzone are not derivatives of or metabolized to benzene, rather, they are distinct xenobiotics (National Center for Biotechnology Information, 2024). Oxybenzone has been associated with a multitude of adverse effects in humans which include dermal allergic reactions, endocrine disruption and Hirschsprung’s disease. For those sunscreen products that still contain benzene as a constituent or contaminant (American Chemical Society, 2021), it is important to note that an additional strong association has been noted between benzene and susceptibility to blood disorders and cancers, as extensively reviewed by Smith (2010). These health risks are further supported by occupational and environmental exposure studies as denoted by Vlaanderen et al. (2011) who conducted a meta-analysis linking occupational benzene exposure to an increased risk of various lymphoma subtypes, thereby highlighting the severity of long-term exposure. Similarly, residential exposure to ambient benzene in the U.S. has been correlated with a higher risk of hematologic malignancies, according to Teras et al. (2019). This is consistent with findings by Switchenko et al. (2016), who examined the spatial relationships between passive benzene exposure and non-Hodgkin lymphoma risk. Additionally, proximity to benzene release sites has been associated with an increased incidence of non-Hodgkin lymphoma, as demonstrated by Bulka et al. (2013).
The Center for Disease Control fourth national report on human exposure to environmental chemicals reported that approximately 97% of the people tested have oxybenzone in their urine (DiNardo and Downs, 2018). Other studies point out the presence of various concentrations of oxybenzone in waterways and fish worldwide. Aside from applying this contaminant directly to the skin as a result of sunscreen use, adverse reactions may also occur through ingesting fish contaminated with oxybenzone. Yet another concern involves the act of washing the ingredient from the body, only for it contaminate drinking water as treatment plants do not effectively remove the chemical as part of their filtration protocols (DiNardo and Downs, 2018).
While it is warranted to investigate the potential harmful effects of chemical based sunscreens, some argue that immediate actions must be taken. As well, a rush to action brings with it a risk of compromising research quality and not considering other facts which may serve as contributors to widespread coral bleaching (Matts and Nash, 2023). Specifically, some studies have shown that rising ocean temperature is responsible for coral bleaching (Hughes et al., 2017; Wyatt et al., 2023). Although this is a well-established association, it is an inconvenient explanation given its solution is seemingly unachievable. Many individuals believe that since influencing policy on climate change appears to be too daunting of a task for an individual, sunscreens have become a convenient scapegoat as they present a seemingly straightforward short-term remedy through bans or restrictions on the use of products containing potentially harmful chemical constituents (Matts and Nash, 2023).
Current public opinion and market trends
Despite the growing knowledge of sunscreen toxicity from a scientific perspective, current public opinion regarding the use of these products reveals that the new findings might not easily make their way into the public sector. According to Sander et al. (2020), commonly reported adverse reactions to sunscreens are what deter most civilians from their routine use. Reactions such as stinging, burning, and irritant contact dermatitis commonly result from the use of octocrylene, oxybenzone, and octyl methoxycinnamate. Patients who experience these allergic reactions might be more inclined to skip their daily sunscreen application despite knowledge about the beneficial effects of sunscreen products because they want to avoid discomfort.
Many studies suggest there are discrepancies in public perception of sunscreen products based on varied demographics of a sampled population, including socioeconomic differences. According to Agarwal et al. (2018), patients in modernized first world countries such as the United States and Australia have a greater knowledge base about the use of sunscreen and its potential beneficial and adverse effects. In developing nations such as India, there is less scientific knowledge about sunscreen and more cultural focus on the benefits of the sun itself. For example, in India, having tan skin is considered to be a symbol of hard work and healthiness. The impact of this cultural bias is that routine sunscreen use is unlikely, thereby minimizing its beneficial effects to health.
Another discrepancy resides between males and females. In a study by Patel et al. (2019) that surveyed people of differing sexes and ages regarding their sun protection use, 12.2% of males reported never wearing sunscreen in contrast to only 5.7% of females. This disparity could be due to growing market trends in the skincare industry, which combine medical skin treatment recommendations with beauty standards that value healthy, youthful-looking skin, which mainly targets females. Age also played a factor in attitudes towards sun protection, with children and adolescents looking upon sunscreen use in a negative way (Patel et al., 2019). As well, the prevailing attitude regarding regular sunscreen use is more likely associated with a lack of knowledge and societal or cultural norms rather than scientific evidence regarding the risks associated with the ingredients of specific sunscreen products.
A growing theme amongst previous studies appears to be a lack of knowledge about sunscreen ingredients and new research regarding sunscreen effects. In a survey study about the Hawaiian Sunscreen Ban, only one third of people knew about the ban itself, and even less knew about the reasons why sunscreen use was banned (Glanz et al., 2022). This knowledge gap manifests as patients both failing to use sunscreen and blindly using sunscreen without knowing its proven risks (Geoffrey et al., 2019).
Discussion and conclusions
While there is research that examines people’s attitudes towards sunscreen use, more studies to determine public perception of sunscreen use are needed. Large discrepancies in opinion exist depending on surveyed patient demographics and varied results between surveys. The public needs to be made increasingly aware of the evolving knowledge base regarding sunscreen use and its attendant risks to both human health and the environment. This will only be possible if more research is completed on long-term effects of sunscreen usage. With increased knowledge within the scientific community and the public, the most appropriate use of sunscreen products will be driven by reason as opposed to public perception and opinion.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Author contributions
TT: Writing – review & editing, Writing – original draft. MF: Writing – review & editing, Writing – original draft. GK: Writing – review & editing, Writing – original draft, Validation, Supervision.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. The authors received financial support to enable publication of this work through a grant-in-aid provided by the Anne Burnett Marion School of Medicine at Texas Christian University Open Access Fund.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Agarwal S. B., Godse K., Patil S., Nadkarni N. (2018). Knowledge and attitude of general population toward effects of sun exposure and use of sunscreens. Indian J. Dermatol. 63, 285–291. doi: 10.4103/ijd.IJD_609_17
American Chemical Society (2021). Lab finds benzene in 78 sunscreens (Chemical & Engineering News). Available at: https://cen.acs.org/business/consumer-products/Lab-finds-benzene-78-sunscreens/99/i21.
Bulka C., Nastoupil L. J., McClellan W., Ambinder A., Phillips A., Ward K., et al. (2013). Residence proximity to benzene release sites is associated with increased incidence of non-Hodgkin lymphoma. Cancer 119, 3309–3317. doi: 10.1002/cncr.28183
Coral Disease & Health Consortium (2023). Available online at: https://cdhc.noaa.gov/ (Accessed 11 July 2024).
Danovaro R., Bongiorni L., Corinaldesi C., Giovannelli D., Damiani E., Astolfi P., et al. (2008). Sunscreens cause coral bleaching by promoting viral infections. Environ. Health Perspect. 116, 441–447. doi: 10.1289/ehp.10966
Dasgupta S. (2015). Massive bleaching event puts world’s coral reefs at risk (Mongabay). Available online at: https://news.mongabay.com/2015/10/massive-bleaching-event-puts-worlds-coral-reefs-at-risk/ (Accessed 11 July 2024).
DiNardo J. C., Downs C. A. (2018). Dermatological and environmental toxicological impact of the sunscreen ingredient oxybenzone/benzophenone-3. J. Cosmetic Dermatol. 17, 15–19. doi: 10.1111/jocd.12449
Downs C. A., Diaz-Cruz M. S., White W. T., Rice M., Jim L., Punihaole C., et al. (2022). Beach showers as sources of contamination for sunscreen pollution in marine protected areas and areas of intensive beach tourism in Hawaii, USA. J. Hazardous Materials 438, 129546. doi: 10.1016/j.jhazmat.2022.129546
Druml L., Ilyas A. M., Ilyas E. (2023). Sunscreen label marketing towards pediatric populations: guidance for navigating sunscreen choice. Cureus 15, e46785. doi: 10.7759/cureus.46785
Geoffrey K., Mwangi A. N., Maru S. M. (2019). Sunscreen products: Rationale for use, formulation development and regulatory considerations. Saudi Pharm. J. 27, 1009–1018. doi: 10.1016/j.jsps.2019.08.003
Glanz K., Kwong P. L., Avelis J., Cassel K. (2022). Development of a survey of sunscreen use and attitudes among adults in two coastal states 2019. Int. J. Environ. Res. Public Health 19, 2677. doi: 10.3390/ijerph19052677
Hudspeth A., Zenzola N., Kucera K., Wu Q., Light D. (2022). Independent sun care product screening for benzene contamination. Environ. Health Perspect. 130, 37701. doi: 10.1289/EHP10386
Hughes T. P., Kerry J. T., Álvarez-Noriega M., Álvarez-Romero J. G., Anderson K. D., Baird A. H., et al. (2017). Global warming and recurrent mass bleaching of corals. Nature 543, 373–377. doi: 10.1038/nature21707
Lorigo M., Mariana M., Cairrao E. (2018). Photoprotection of ultraviolet-B filters: Updated review of endocrine disrupting properties. Steroids 131, 46–58. doi: 10.1016/j.steroids.2018.01.006
Matta M. K., Florian J., Zusterzeel R., Pilli N. R., Patel V., Volpe D. A., et al. (2020). Effect of sunscreen application on plasma concentration of sunscreen active ingredients: a randomized clinical trial. JAMA 323, 256–267. doi: 10.1001/jama.2019.20747
Matts P. J., Nash J. F. (2023). Sunscreens - another endangered species? Int. J. Cosmetic Sci. 45 Suppl 1, 20–32. doi: 10.1111/ics.12902
National Center for Biotechnology Information (2024). PubChem compound summary for CID 4632 (Oxybenzone). Available at: https://pubchem.ncbi.nlm.nih.gov/compound/Oxybenzone.
Nicole W. (2022). Skin protection dilemma: testing detects benzene in some sun care products. Environ. Health Perspect. 130, 54002. doi: 10.1289/EHP11423
Onyango D. O., Selman B. G., Rose J. L., Ellison C. A., Nash J. F. (2023). Comparison between endocrine activity assessed using ToxCast/Tox21 database and human plasma concentration of sunscreen active ingredients/UV filters. Toxicological Sci. 196, 25–37. doi: 10.1093/toxsci/kfad082
Patel A. R., Zaslow T. L., Wren T. A. L., Daoud A. K., Campbell K., Nagle K., et al. (2019). A characterization of sun protection attitudes and behaviors among children and adolescents in the United States. Prev. Med. Rep. 16, 100988. doi: 10.1016/j.pmedr.2019.100988
Petersen B., Wulf H. C. (2014). Application of sunscreen–theory and reality. Photodermatol. Photoimmunol. Photomed. 30, 96–101. doi: 10.1111/phpp.12099
Sander M., Sander M., Burbidge T., Beecker J. (2020). The efficacy and safety of sunscreen use for the prevention of skin cancer. Can. Med. Assoc. J. 192, E1802–E1808. doi: 10.1503/cmaj.201085
Smith M. T. (2010). Advances in understanding benzene health effects and susceptibility. Annu. Rev. Public Health 31, 133–148. doi: 10.1146/annurev.publhealth.012809.103646
Stanford University (2022). Understanding how sunscreens damage coral (ScienceDaily). Available online at: https://www.sciencedaily.com/releases/2022/05/220505143215.htm (Accessed 11 July 2024).
Suh S., Pham C., Smith J., Mesinkovska N. A. (2020). The banned sunscreen ingredients and their impact on human health: a systematic review. Int. J. Dermatol. 59, 1033–1042. doi: 10.1111/ijd.14824
Switchenko J. M., Bulka C., Ward K., Koff J. L., Bayakly A. R., Ryan P. B., et al. (2016). Resolving uncertainty in the spatial relationships between passive benzene exposure and risk of non-Hodgkin lymphoma. Cancer Epidemiol. 41, 139–151. doi: 10.1016/j.canep.2016.02.007
Teras L. R., Diver W. R., Deubler E. L., Krewski D., Flowers C. R., Switchenko J. M., et al. (2019). Residential ambient benzene exposure in the United States and subsequent risk of hematologic Malignancies. Int. J. Cancer 145, 2647–2660. doi: 10.1002/ijc.32202
U.S. Food and Drug Administration (2021). FDA alerts drug manufacturers to the risk of benzene contamination in certain drugs. Available online at: https://www.fda.gov/drugs/pharmaceutical-quality-resources/fda-alerts-drug-manufacturers-risk-benzene-contamination-certain-drugs (Accessed: June 24, 2024).
Vlaanderen J., Lan Q., Kromhout H., Rothman N., Vermeulen R. (2011). Occupational benzene exposure and the risk of lymphoma subtypes: A meta-analysis of cohort studies incorporating three study quality dimensions. Environ. Health Perspect. 119, 159–167. doi: 10.1289/ehp.1002318
Wang J., Pan L., Wu S., Lu Y., Zhu Y., Guo M., et al. (2016). Recent advances on endocrine disrupting effects of UV filters. Int. J. Environ. Res. Public Health 13, 782. doi: 10.3390/ijerph13080782
Woodruff C. (2019). Assessment of willingness to pay for coral-safe sunscreen. ProQuest Dissertations & Theses Global. (College of Charleston). Available at: http://library.tcu.edu/PURL/EZproxy_link.asp?/login?url=https://www.proquest.com/dissertations-theses/assessment-willingness-pay-coral-safe-sunscreen/docview/2303837546/se-2.
Wyatt A. S. J., Leichter J. J., Washburn L., Kui L., Edmunds P. J., Burgess S. C. (2023). Hidden heatwaves and severe coral bleaching linked to mesoscale eddies and thermocline dynamics. Nat. Commun. 14, 25. doi: 10.1038/s41467-022-35550-5
Keywords: sunscreen toxicity, environmental impact, endocrine disruption, benzene, chemical exposure, human health risk sunscreen toxicity and endocrine disruption
Citation: Thomas T, Fat M and Kearns G (2024) Sunscreens: potential hazards to environmental and human health. Front. Mar. Sci. 11:1471574. doi: 10.3389/fmars.2024.1471574
Received: 27 July 2024; Accepted: 13 September 2024;
Published: 01 October 2024.
Edited by:
André Rolim Baby, University of São Paulo, BrazilReviewed by:
Fabiana Pessoa, Federal University of Espirito Santo, BrazilCopyright © 2024 Thomas, Fat and Kearns. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Gregory Kearns, Zy5rZWFybnNAdGN1LmVkdQ==
†These authors have contributed equally to this work and share first authorship
 Talia Thomas
Talia Thomas Marisa Fat1†
Marisa Fat1†