- 1Institute of Complementary and Integrative Medicine, Faculty of Medicine, University of Bern, Bern, Switzerland
- 2Eurythmy4you, Nidau, Switzerland
Introduction: Cancer is a debilitating disease with an often chronic course. One of the most taxing and prevalent sequelae in this context is cancer-related fatigue (CRF) resulting from the disease and/or associated treatments. Over the last years mindfulness-based interventions such as eurythmy therapy (ERYT), a mindful-movement therapy from anthroposophic medicine, have emerged as promising adjunct therapies in oncology. This prospective study investigated an online implementation of ERYT for CRF using a single arm repeated-measures design based on two consecutive studies.
Method: Study 1 consisted of an initial assessment before, during, after, and at follow up of a 6-week online ERYT-based program in a mixed sample of N = 165 adults with or without cancer diagnosis. Study 2 involved a similar design with an adapted 8-week online ERYT-based program in a sample of N = 125 adults who had been diagnosed with cancer. Outcomes were assessed using the Functional Assessment of Chronic Illness Therapy–Fatigue, Perceived Stress Scale, Mindful Attention Awareness Scale, and Insomnia Severity Index (for Study 1 all, for Study 2 only the former three). We additionally performed an exploratory analysis regarding practice frequency and duration. Data were analyzed using Linear Mixed-Effect Models per outcome; ANOVA was used for practice times.
Results: For Study 1, mixed-effects model estimates showed no significant effect on fatigue, but pointed to significantly improved emotional and physical well-being, reduced stress, as well as increased mindfulness (mixed subjects). Functional and social well-being or sleep quality did not change significantly. Study 2 model estimates on the other hand showed significantly improved CRF in conjunction with the ERYT-based online intervention, as well as improved stress and mindfulness scores (cancer-diagnosed subjects).
Conclusion: Taken together, while our results should be interpreted with caution given the single-arm design and relatively high dropout, they suggest online ERYT may be associated with a reduction in fatigue for individuals diagnosed with cancer, an increase in mindfulness, and benefits for stress and certain well-being indicators. The online group format is advantageous in view of affordability and accessibility, the latter being particularly relevant for individuals who due to high symptom severity cannot leave their homes. Randomized-controlled studies will be needed to confirm these findings.
1 Introduction
Cancer is a complex and debilitating disease with an often chronic course, affecting millions of individuals worldwide (Tran et al., 2022; Sung et al., 2021). One of the most prevalent and taxing sequelae in this context is cancer-related fatigue (CRF), a general and persistent lack of energy not relieved by rest, which results from both the disease and associated treatments (Bower, 2014; Cleeland et al., 2013). Reported prevalence rates of CRF depend on type of treatment, population, and assessment methodology, but may range between 25 and 99% (Bower, 2014) or 14–100% (Ma et al., 2020), with the latter meta-analysis reporting a pooled prevalence of 52% based on 84 studies.
Mind–body therapies and particularly mindfulness-based movement practices such as Yoga, Tai Chi, Qi Gong, or Feldenkrais, which combine bodily movements (and often also breath) with focused attention, have emerged as promising adjunct therapies in oncology to improve common sequelae like CRF, sleep disturbances, reduced quality of life, or stress (Chen et al., 2024; Firkins et al., 2020; Mayden, 2012; Zhang et al., 2019; Wu et al., 2022; Desveaux et al., 2015; Raman et al., 2013; Gouw et al., 2019; Wang et al., 2013; Hillier and Worley, 2015; Cramer et al., 2012b; Vergeer et al., 2021; Miller et al., 2020; Stephens and Hillier, 2020; Wang and Szabo, 2020; Cocchiara et al., 2020). Eurythmy therapy (ERYT) is an integrative movement-based therapy in this context rooted in anthroposophic medicine, which involves integrated sequences of movements, performed with arms, hand, legs, or the whole body, in a state of focused concentration and intentionality (Kirchner-Bockholt, 1977; Kienle et al., 2013). Guided by a trained therapist, the technique is said to develop mindfulness to outer movement, inner sensation, and the connection between the two (Berger et al., 2015), a process engaging both proprioceptive and interoceptive awareness. Generally speaking, ERYT protocols can be practiced individually or in groups, and consist of movement sequences based on a core set of principles which are then tailored to a given disease or patient at hand (Hamre H. J. et al., 2007). Emerging scientific evidence points to benefits for a range of conditions (Lötzke et al., 2015) such as stress (Berger et al., 2015; Kanitz et al., 2011), depression (Hamre et al., 2006; Hamre et al., 2013), anxiety (Schwab et al., 2011; Hamre et al., 2009), or chronic pain (Hamre H. et al., 2007; Michalsen et al., 2021). Indeed, ERYT has also been applied in complementary cancer care, with promising first results (Kanitz et al., 2013). A challenge in this context however remains that disease- and treatment-related symptoms, including CRF, often restrict patients’ ability to travel to practice sessions (Kim et al., 2020). Online delivery of ERYT could hence be a promising avenue in oncology, as it allows patients to engage in the therapeutic activity without requiring them to leave their homes. Indeed, online applications of other mindful movement practices, such as Tai Chi or Qi Gong, have been shown to present useful alternatives in similar and other relevant contexts (Oh et al., 2021; Gao et al., 2022; Sohl et al., 2024; Brosnan et al., 2021; Gravesande et al., 2023; Teo et al., 2024). Nonetheless, research assessing the online delivery of ERYT in particular to our knowledge has not yet been conducted.
The current study thus assessed an online intervention based on ERYT to improve CRF and associated symptoms. More specifically, using an exploratory approach with repeated-measures design based on two consecutive observational studies, we aimed to assess changes in CRF (main outcome), sleep quality, stress, quality of life indicators, and mindfulness (secondary outcomes) during and after an online ERYT-based intervention for adults diagnosed with cancer. The study was conducted by the University of Bern (Institute of Complementary and Integrative Medicine) in collaboration with a healthcare provider specializing in ERYT.1
2 Study 1: exploratory assessment (mixed subjects)
2.1 Study 1 methods
2.1.1 Study design and setting
The first study (11/2022–2/2023) involved an observational assessment with repeated-measures design on a mixed subjects sample, focusing on fatigue, sleep quality, mindfulness, quality of life indicators, and perceived stress as outcomes. The study included five measurement points, namely t1 at baseline, t2–t3 during the intervention, t4 just after completion of the intervention, and t5 at follow up. All surveys were conducted online and in full anonymity of participants. Anonymous self-generated codes were used to link an individuals’ repeated measures between assessment times. Given the design was observational and no potentially identifying data were collected (no names, email or IP addresses, birthdates, etc.), ethics approval was not required for this study according to the responsible Ethics Committee guidelines and the Federal Act on Research involving Human Beings (Human Research Act, 2011).
2.1.2 Participants and procedure
Information about the intervention as well as the study were announced on the health provider’s website, newsletters, in psychology networks, adverts in clinics also practicing anthroposophic medicine, physicians’ practices, and social media. All individuals who registered for the two cycles of the intervention (one held in German and one in English) between November and December 2022 were invited to participate in the study. They were thoroughly informed about the study, specifying that participation was voluntary and that opting not to take part in the study would not impact their enrollment and participation in the intervention itself. In view of the exploratory aim of Study 1, we included all individuals who registered for the program and agreed to participate in the study. This meant that also individuals who did not have a cancer diagnosis but enrolled in the program for other reasons (e.g., relatives of cancer patients) and agreed to participate were included. Except for the intervention itself (free of charge), no compensation was offered to participants. All participants were asked to fill in the baseline survey at the outset of the intervention (t1), 2 weeks later (t2), 4 weeks later (t3), 6 weeks later (t4, which marked the completion of the intervention), as well as at follow-up (t5) after 14 weeks (i.e., 8 weeks after completion).
2.1.3 Measures
The online survey was made of a set of validated psychological questionnaires programmed by means of SoSci Survey (Leiner, 2023) for anonymous computer-assisted implementation, and was available in German and English. For the validated scales the recall period was set to the last 7 days. The survey further included single items to indicate age, gender, cancer status, motive for enrolment, and practice times. For self-reported practice times we used the following quantitative items (t2–t5 assessment: how many days in the last 2 weeks/at follow-up: per week on average; were you able to do the exercises? answer options: 0–2 days, 3–5 days, 6–8 days, 9–11 days, 12–14 days; and, respectively, 0–1 days, 2–3 days, 4–5 days, and 6–7 days). They were also asked how much time they have spent on the exercises per practice day (1–10 min, 11–20 min, 21–30 min, more than 30 min, or not done). Functional Assessment of Chronic Illness Therapy - Fatigue: To assess CRF and associated quality of life/well-being indicators we used the Functional Assessment of Chronic Illness Therapy–Fatigue (FACIT-F; Cella, 1997, validated German version: Montan et al., 2018; facit.org, 2022). The 40 items of this instrument were rated on a five-point Likert scale ranging from 0 (not at all) to 4 (very much). The overall FACIT-F score was calculated by summing the item scores (range 0–160), with higher scores indicating less fatigue/higher quality of life. The instrument includes five subscales, namely Fatigue (FA; 13 items), Physical Well-Being (PWB; 7 items), Social/Family Well-Being (SWB; 7 items), Emotional Well-Being (EWB; 6 items), and Functional Well-Being (FWB; 7 items). Most pertinently here, the FA subscale can range from 0 to 52, with lower scores implying more fatigue (clinical cut-off at 36; Alexander et al., 2009). Mindful Attention Awareness Scale: The Mindful Attention Awareness Scale (MAAS; Brown and Ryan, 2003; Carlson and Brown, 2005, validated German version: Michalak et al., 2008) is a widely used brief mindfulness questionnaire that showed good psychometric properties in cancer patient samples (Tseng, 2024). It is made of 15 items, each presenting a statement related to mindful awareness rated on a scale from 1 (almost always) to 6 (almost never). The MAAS score is the mean of all items and ranges from 1 to 6, with higher scores indicating higher mindfulness. Perceived Stress Scale: The Perceived Stress Scale (PSS-10; Cohen et al., 1983, validated German version: Klein et al., 2016; Copyright © 2022 Mapi Research Trust) is a well-established validated questionnaire for assessing perceived stress, which has also been extensively used in the context of cancer patients (Yılmaz Koğar and Koğar, 2024; Tseng, 2024; Chui, 2021; Chrobak et al., 2023; Trojnar et al., 2024; Soria-Reyes et al., 2023). Each of the 10 items is rated on a five-point Likert scale from 0 (never) to 4 (very often), with higher scores indicating greater perceived stress (total score calculated by summing the items, range: 0–40). PSS-10 total scores can be interpreted as low (0–13), moderate (14–26), or high (27–40) stress (Adamson et al., 2020). Insomnia Severity Index. The Insomnia Severity Index (ISI; Morin et al., 2011; Morin, 1993, German version: Dieck et al., 2018; Copyright © 2022 Mapi Research Trust) is a 7 item instrument assessing the perceived severity of insomnia. It has been frequently used in research on cancer populations with good validity and reliability (Yusufov et al., 2019; Lin et al., 2020; Michaud et al., 2021; Savard et al., 2005). Each item is rated on a five-point Likert scale from 0 to 4. The total score (calculated by summing the items) ranges from 0 to 28, with higher scores indicating greater severity (i.e., worse sleep quality).
2.1.4 Intervention
The mindful movement-based intervention consisted of weekly online group sessions (90 min) and guided self-practice between sessions over six consecutive weeks. In the online sessions participants were familiarized with a specific sequence of ERYT exercises tailored to address cancer-related symptoms and CRF (for further information on ERYT in the context of cancer and CRF, see Kröz et al., 2013; Meier-Girard et al., 2020; Kröz et al., 2017), conveyed step by step over the course of the program. In a given session, the facilitator (an experienced and certified eurythmy therapist; TH) demonstrated each of the exercises at full length live on camera, while also verbally describing the specifics of the movements and pointing out relevant meaning content. After some initial rounds of demonstration, participants were encouraged to actively join the facilitator, gradually imitating the movements until they were able to perform the exercise independently. This practice time (30–40 min) was followed by a short resting period (5 min), during which the facilitator guided participants through a body scan, aimed to enable them to sense directly in their body the impact of the exercise. Participants then had the opportunity to ask questions. The facilitator finally provided instructions on how to perform the exercise on their own in their forthcoming self-practice during the time lapse between sessions, including what to pay specific attention to, context of practice, and duration, with a recommendation of 10–15 min of daily self-practice. In the subsequent session, the facilitator encouraged participants to discuss their experiences and ask questions if needed. Furthermore, participants had access to video recordings of the live sessions and of demonstrations of specific ERYT exercises, as well as to an online group forum for exchange.
2.1.5 Data analysis
All statistical analyses were performed using R version 4.4.0 (R Core Team, 2024). For all inferential statistics the significance level was set to α < 0.05. Surveys that had been filled in outside the defined time windows (for t1 more than 1 week after intervention onset, for t2–t4 less than one or more than 3 weeks apart, and for t5 outside the required period of 4–10 weeks post intervention end) where excluded from the analysis. To analyze time-dependent changes in the outcome variables and test for significance we performed Linear Mixed-Effects Models (LMM) (Brown, 2021) using the R packages lme4 (Bates et al., 2015) and nlme (Pinheiro et al., 2023). We opted for LMM among other reasons due to its capacity to calculate accurate models in spite of missing data, a common challenge in longitudinal studies (Gabrio et al., 2022). Models were calculated for each outcome separately, with all models adjusted for age, gender, and survey language. Finally, to test the effect of self-practice time on the outcomes we performed explorative one-way Analysis of Variance (ANOVA) with Tukey post-hoc tests for practice frequencies and duration for each measurement point, starting with t2.
2.2 Study 1 results
2.2.1 Subjects
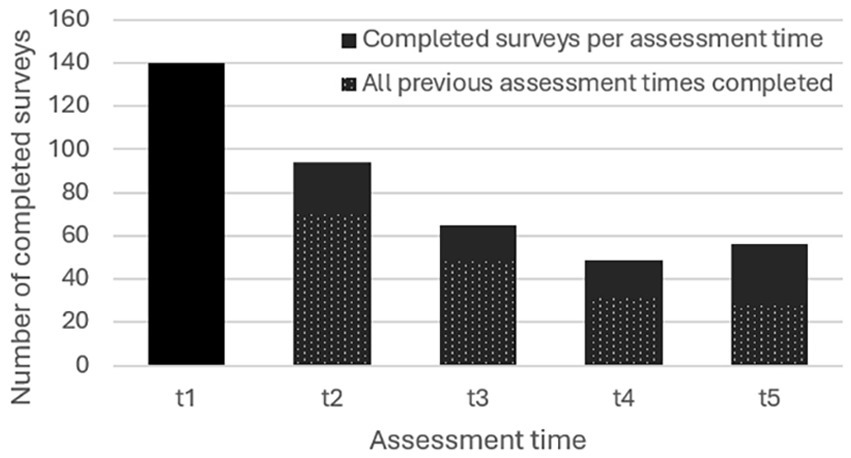
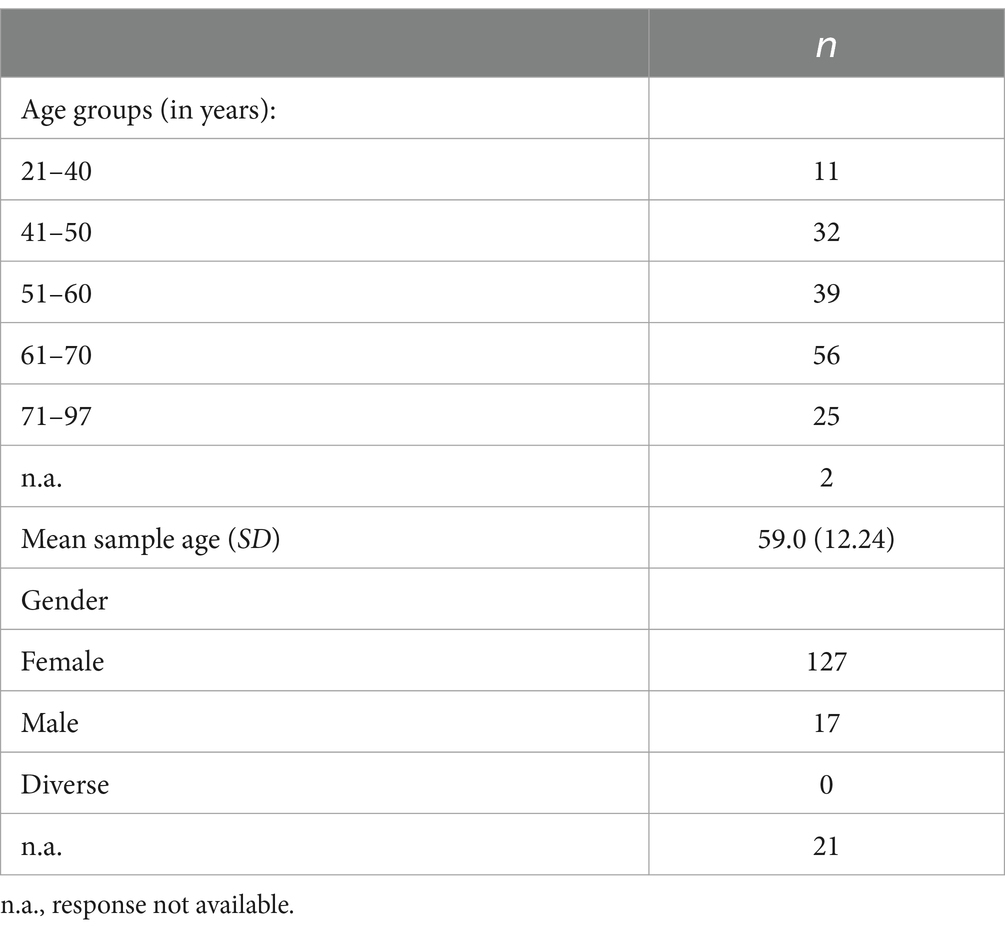
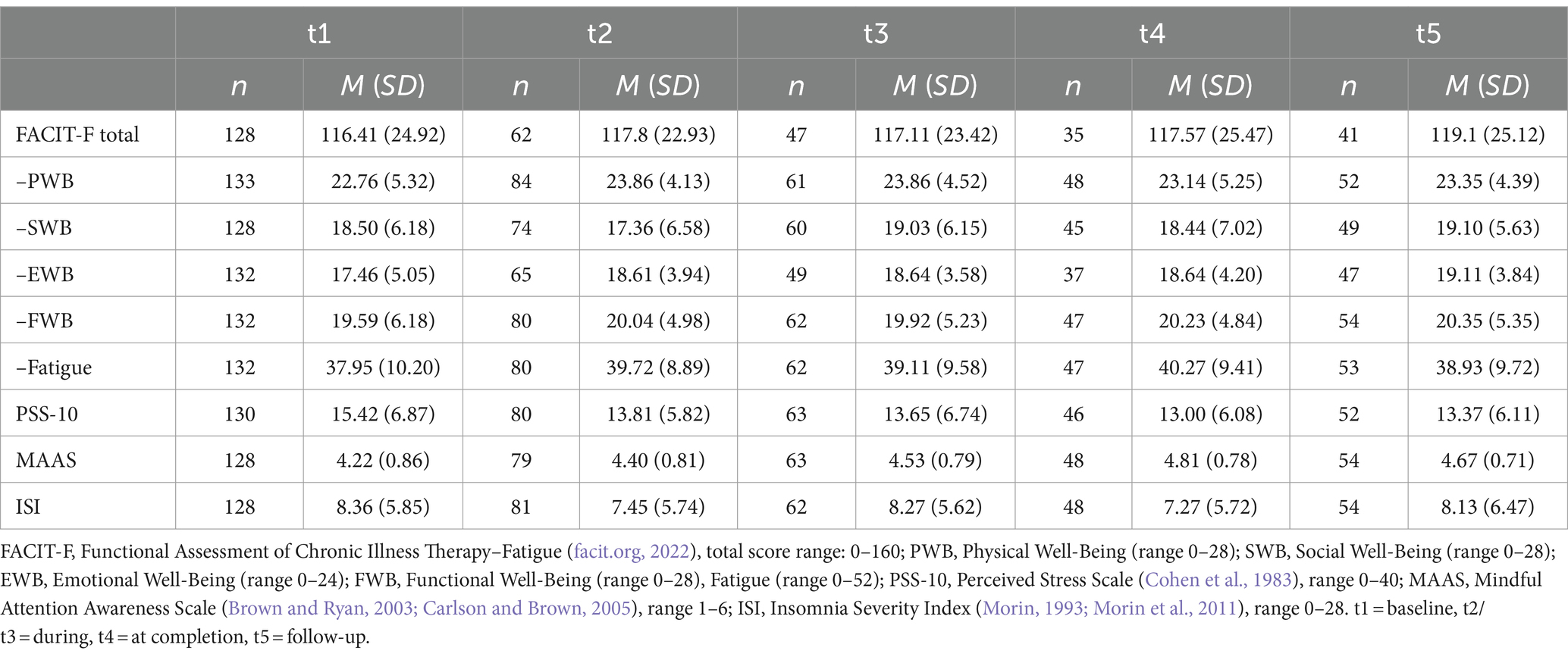
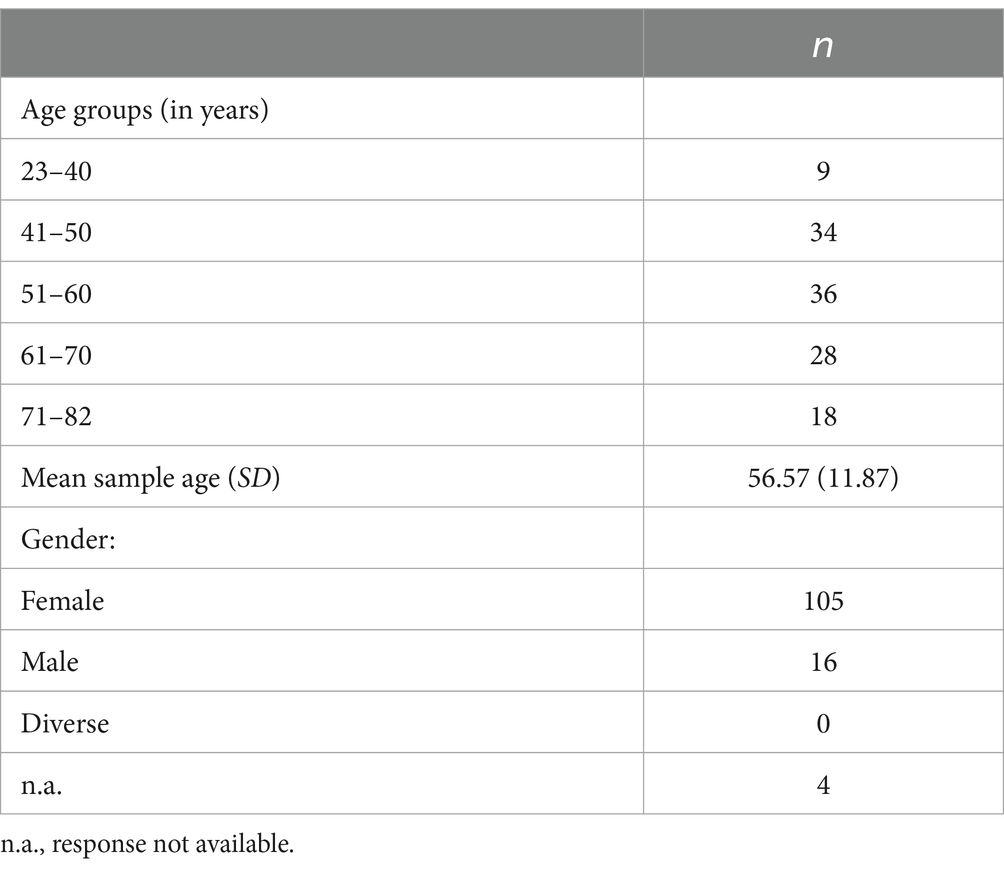
Of the 283 individuals who registered for the program in Study 1 (187 for the English and 96 for the German iteration), N = 165 agreed to participate in the study and filled in at least one questionnaire (57.6% filled in at least two questionnaires and 17% filled in all five questionnaires, see Figure 1). About two thirds of participants (n = 99) filled in the English version of the survey, the rest used the German version (n = 66). Sociodemographic characteristics of Study 1 participants are given in Table 1. The mean age was 59 years (SD = 12.2), a large majority being female. Nearly a third (n = 52) reported to have received a cancer diagnosis during their lifetime, of which 26 participants indicated to be currently in treatment. Means and standard deviations of Study 1 outcome variables at each of the five assessment times can be found in Table 2. The subjects’ baseline FACIT-F FA score was above 36 and can thus be considered non-clinical (Alexander et al., 2009). Baseline PSS-10 scores pointed to moderate stress levels (Adamson et al., 2020), and baseline MAAS scores can be considered within the normative range based on a large-scale norming study (Brown and Kasser, 2005; Carlson and Brown, 2005). Finally, the subjects’ baseline ISI scores suggest mild to moderate severity of insomnia as per clinical benchmarks (Morin et al., 2011).
2.2.2 Time-dependent changes in outcome variables
Figure 2 shows significant changes in the outcomes over time found in Study 1. CRF and quality of life indicators. There was a significant improvement in the FACIT-F physical well-being (F(4, 197) = 2.764, p = 0.029) and emotional well-being (F(4, 158) = 5.181, p < 0.001) scales (Figures 2A,B, respectively). The FACIT-F fatigue subscale score also improved, but not significantly (F(4, 198) = 1.948, p = 0.104). The same was the case for social (F(4, 180) = 1.831, p = 0.125) and functional (F(4, 199) = 1.227, p = 0.301) well-being and the overall FACIT-F score (F(4, 144) = 2.362, p = 0.056). For EWB all estimates were significant relative to t1 at p < 0.001, except for t2 (p < 0.01) and t3 (p < 0.05). For PWB only t2 (p < 0.05) and t3 (p < 0.01) estimates were significant relative to t1. Perceived stress. Figure 2C shows changes in the PSS-10 scores, pointing to a significant reduction in stress over the course of the intervention (F(4, 198) = 4.110, p = 0.003). Except for t2 (n.s), all estimates were significant relative to t1 at p < 0.01. Mindfulness. Time-dependent changes in mindfulness are visible in Figure 2D, with MAAS scores increasing significantly over the course of the intervention (F(4, 200) = 12.467, p < 0.001). The estimates were significant relative to t1 at p < 0.001, except for t3 (p < 0.01) and t2 (n.s.). Sleep. Sleep quality as per ISI did not significantly change in conjunction with the intervention (F(4, 201) = 1.724 p = 0.146).
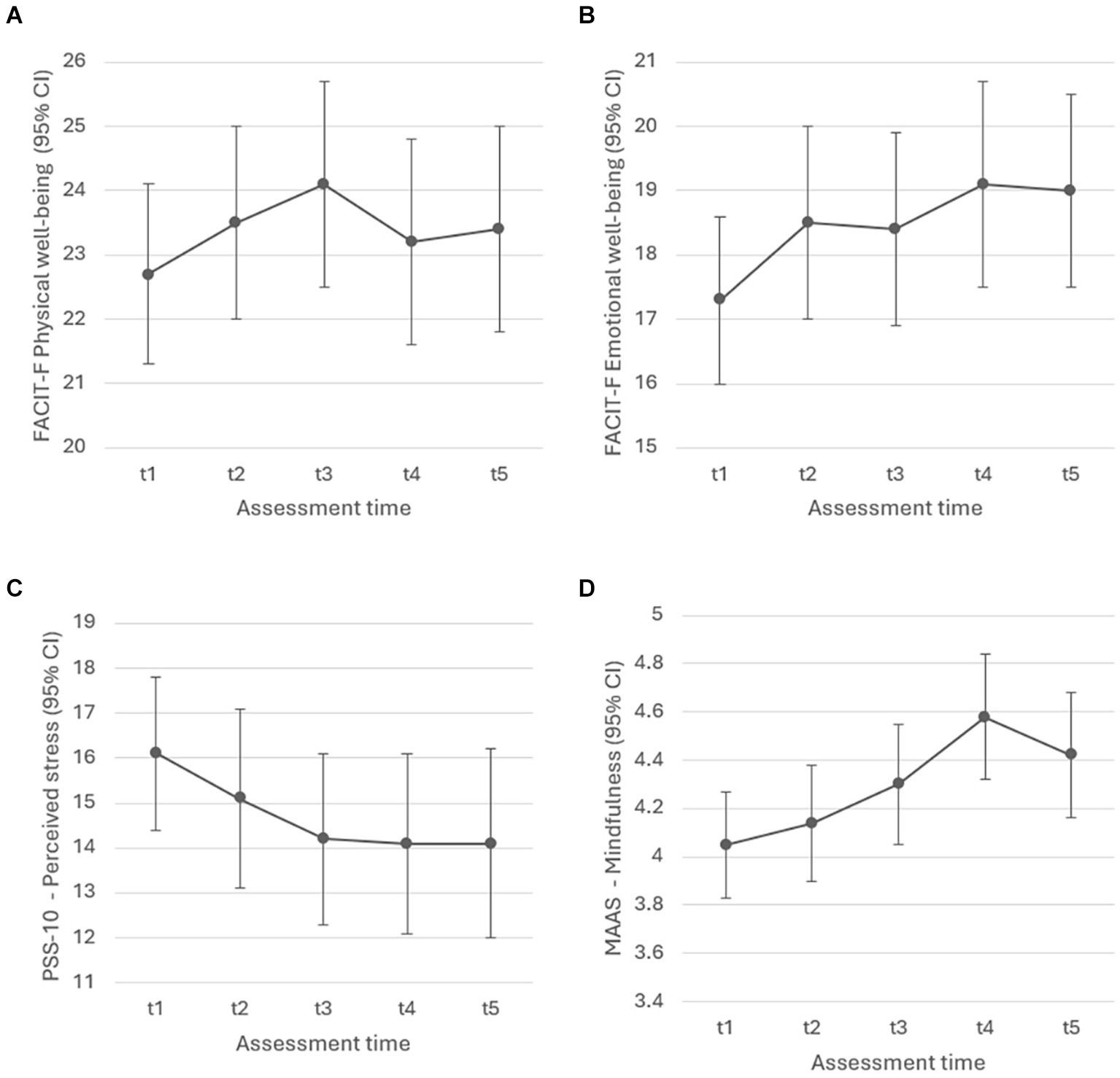
Figure 2. Study 1: Liner Mixed-Effect Model estimates with (A) physical well-being (p = 0.029), (B) emotional well-being (p < 0.001), (C) perceived stress (p = 0.003), and (D) mindfulness (p < 0.001) as outcomes.
2.2.3 Effects of self-practice frequency and duration
In Study 1, the frequency of practice (number of days practiced during the past 2 weeks/during 1 week on average in case of t5) had a significant effect on stress levels as per ANOVA at t4 (F(4, 41), p = 0.031), with post-hoc tests showing significantly lower stress if 12–14 rather than 6–8 days had been practiced (p = 0.021). The duration of self-practice (minutes per day) in the preceding weeks also had a significant effect on stress at t4 (F(4, 41) = 3.038, p = 0.028), but only a trend of higher stress if over 30 min per day were practiced compared to 11–20 min (p = 0.073). As with stress, practice frequency of preceding weeks also had a significant effect on SWB at t4 (F(4, 40) = 2.738, p = 0.042). Post-hoc tests showed significantly higher SWB if 9–11 rather than 6–8 days had been practiced (p = 0.041). Furthermore, the duration of self-practice had a significant effect on SWB at t2 (F(4, 65) = 3.316, p = 0.016), with significantly higher SWB if they had practiced 1–10 min per day (p = 0.009) or 11–20 min per day (p = 0.035) during preceding weeks rather than no practice at all. Similarly, practice duration had a significant effect on FWB at t4 (F(4, 42), p = 0.021), with significantly lower FWB if they had practiced more than 30 min compared to 11–20 min during preceding weeks (p = 0.022). Finally, self-practice duration had a significant effect on sleep quality at t2 (F(4, 71), p = 0.034), with significantly better sleep quality if they had practiced 11–20 min compared to no practice at all (p = 0.033), and a significant effect at t4 (F(4, 43), p = 0.010) in which sleep quality was worse if they had practiced more than 30 min compared to 11–20 min during preceding weeks (p = 0.009).
2.3 Study 1 discussion
Study 1 assessed outcomes of a 6-week online intervention employing ERYT for CRF. While we found significant improvements in emotional and physical well-being, perceived stress, as well as mindfulness, there were no significant changes in fatigue, sleep quality, or social and functional well-being. The lack of significant changes in fatigue could be related to the subjects’ non-clinical degree of baseline fatigue. The sample’s baseline scores pointed to slightly more fatigue compared to normative values from healthy adults (Webster et al., 2003) but slightly less fatigue (although only by one point) than cancer-specific reference scores from a large-scale population survey (Butt et al., 2010). Indeed, the rather small proportion of cancer patients/survivors in the sample does not allow conclusions regarding CRF per se, a limitation of Study 1 which we subsequently addressed in Study 2. A further limitation of the study was the relatively high dropout between assessment times, which is common in online survey-based research, but could potentially give rise to bias and hence advises caution for the interpretation of the data. As with fatigue, baseline PSS-10 scores were somewhat above general population norms (Cohen, 1988) but below reference scores based on a breast cancer sample (Soria-Reyes et al., 2023). ISI scores were in contrast largely in line with cancer-specific normative values (Savard et al., 2005). Finally, the frequency and duration of self-practice of ERYT exercises beyond the practice during the guided online sessions appeared to play a role in shaping the magnitude of beneficial effects. While in several cases more frequent or longer self-practice times seemed to exert a favorable impact on the outcomes, this did not hold for all intervals, assessment times, or outcomes. Moreover, practice durations larger than 30 min in some cases even had a detrimental impact on sleep quality and functional well-being in the assessment thereafter, bearing in mind however that the exploratory design and modest number of cancer-diagnosed participants do not allow definitive conclusions with reference to causality and in general. Further research will be needed to establish optimal practice frequencies and durations per intervention phase. Taken together, the results suggest the online ERYT-based CRF intervention to merit further investigation; the findings from the first study were taken into account in the design of Study 2.
3 Study 2: assessment of CRF intervention (cancer-diagnosed subjects)
3.1 Study 2 methods
3.1.1 Study design and setting
Study 2 (9/2023–2/2024) employed a similar design as the first study but focused on a sample diagnosed with cancer, with the assessment schedule and intervention adapted to the clinical requirements of the subjects at hand: In order to reduce participant burden we shortened the survey by limiting the FACIT-F to the fatigue subscale and dropping the ISI. Furthermore, by omitting one of the two assessment times during the intervention we reduced the number of surveys to be completed from 5 to 4. As in Study 1, all survey data was collected online and in full anonymity of participants (including anonymous self-generated codes to link the repeated measures) without collecting any potentially identifying information; the study hence did not require ethics approval. The main outcome of Study 2 was CRF, with stress and mindfulness as secondary outcomes.
3.1.2 Participants and procedure
The study was announced in the same fashion as in Study 1. All individuals who registered to one of two cycles of the intervention (one held in German, one in English, and the latter also being simultaneously translated to Chinese and Indonesian with the support of two professional interpreters) between September and November 2023 were invited to participate in the study. As in Study 1, no compensation was offered to participants except for the free of charge intervention. They were thoroughly informed about the study, specifying that participation was voluntary and that opting out would not impact their participation in the intervention itself. Only those who indicated that they had been diagnosed with cancer within the last 5 years were included in the study. The choice of a 5-year period was based on evidence that CRF may persist for up to 5 years after treatment, or longer (Bower, 2014). All participants were asked to fill in the baseline survey at the outset of the intervention (t1), 4 weeks later (t2), 8 weeks later (t3–completion of the intervention), and 16 weeks later (i.e., 8 weeks after the end of the intervention) as a follow-up assessment (t4).
3.1.3 Measures
We used the same measures as in Study 1 to assess CRF, stress, and mindfulness, using the original recall periods for all instruments. In addition to the English and German language versions, a Chinese version of the survey was prepared using validated translations of the FACIT-F fatigue subscale (facit.org, 2022; Cai et al., 2023), the PSS-10 (Jiang et al., 2023), and the MAAS (Chen et al., 2012). Finally, we again asked about frequency and duration of self-practice (e.g., On average, how many days per week were you able to do the exercises?).
3.1.4 Intervention
Like in Study 1, the intervention consisted of weekly online group sessions, but the overall duration was extended to 8 weeks. Furthermore, the specific ERYT exercises shown to the participants were adapted to target fatigue more specifically and match an 8-weeks program, and additional behavioral exercises designed to foster mindfulness and self-awareness based on anthroposophic medicine (Haas, 2017) were incorporated into the intervention. As in Study 1, participants were encouraged to practice the learned exercises by themselves during the subsequent week, with a recommendation to practice at least 15 min daily, and were invited to use the video-recorded demonstrations of the exercises and a group forum.
3.1.5 Data analysis
Except for the outcome variables that were dropped, the data analysis protocol was identical to the one described in Study 1. The defined time windows for filling in Study 2 surveys were adapted to match the number of measurement points; namely, surveys were excluded from the analysis if t1 survey was filled in more than 1 week after intervention start, t1–t3 surveys less than 3 or more than 6 weeks apart from each other, or t4 survey outside the required 4–10 weeks after t3 survey.
3.2 Study 2 results
3.2.1 Subjects
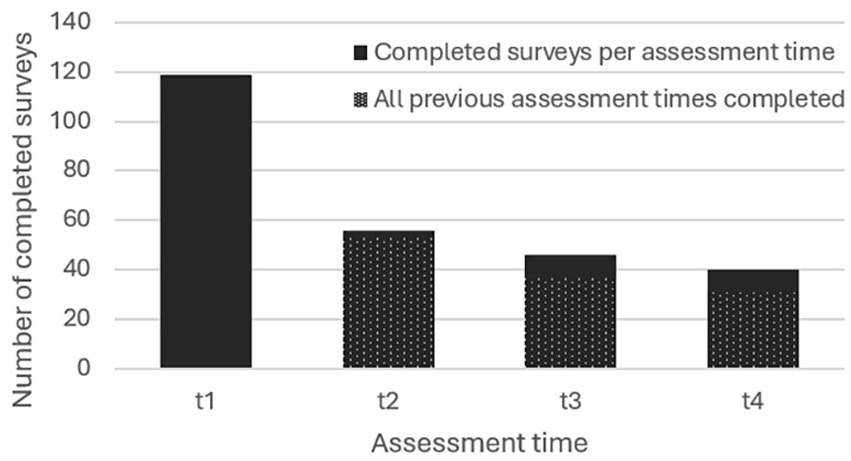
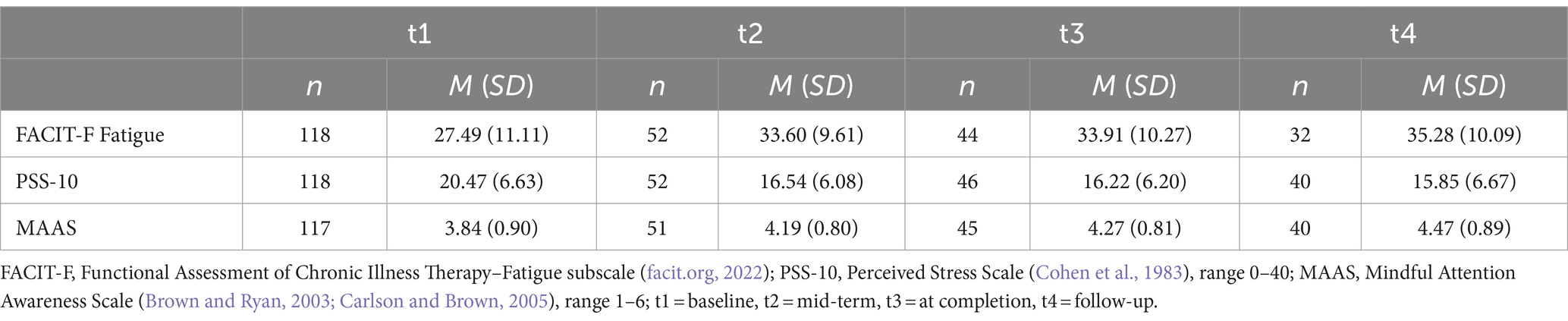
Of the 303 individuals who registered for the intervention in Study 2 (242 for the English, 61 for the German iteration), N = 125 agreed to participate in the study and filled in at least one survey. Of these subjects, 48% filled in at least two surveys and 24.8% filled in all four surveys (see Figure 3). About half of them used the English version of the survey (n = 64), slightly more than a third used the German (n = 46), and the remainder the Chinese version (n = 15). Table 3 shows sociodemographic characteristics of Study 2 participants. As in the former study, a large majority of participants were female, and the mean age was 56.57 years (SD = 11.87). Means and standard deviations of Study 2 outcome variables at all assessment times are found in Table 4. The subjects’ baseline FACIT-F fatigue subscale scores were below the cut-off of 36 (Alexander et al., 2009) which suggests a clinically significant degree of fatigue; they were also below reference values from a large cancer patients sample (Butt et al., 2010) and norms for healthy adults (Webster et al., 2003). Baseline PSS-10 scores were indicative of moderate stress levels (Adamson et al., 2020) comparable to reference scores of a large-scale cancer patients sample (Soria-Reyes et al., 2023) and above general population norms (Cohen, 1988). Finally, baseline MAAS scores of participants were somewhat below general population normative values (Brown and Kasser, 2005), as well as a large-scale sample of cancer patients (Carlson and Brown, 2005).
3.2.2 Time-dependent changes in outcome variables
Cancer-related fatigue. Fatigue as assessed by the FACIT-F fatigue subscale showed a significant decrease over the course of the intervention (F(3, 119) = 23.618, p < 0.001) in Study 2, as can be seen in Figure 4A. Perceived stress. Similarly, scores on the PSS-10 showed a significant reduction in stress over time (F(3, 129) = 22.414, p < 0.001), as depicted in Figure 4B. Mindfulness. Finally, Figure 4C shows MAAS scores per assessment time, pointing to a significant increase in mindfulness over the course of the intervention (F(3, 128) = 24.323, p < 0.001). For all three Study 2 outcomes, estimates (t2, t3, t4) were significant relative to t1 at p < 0.001.
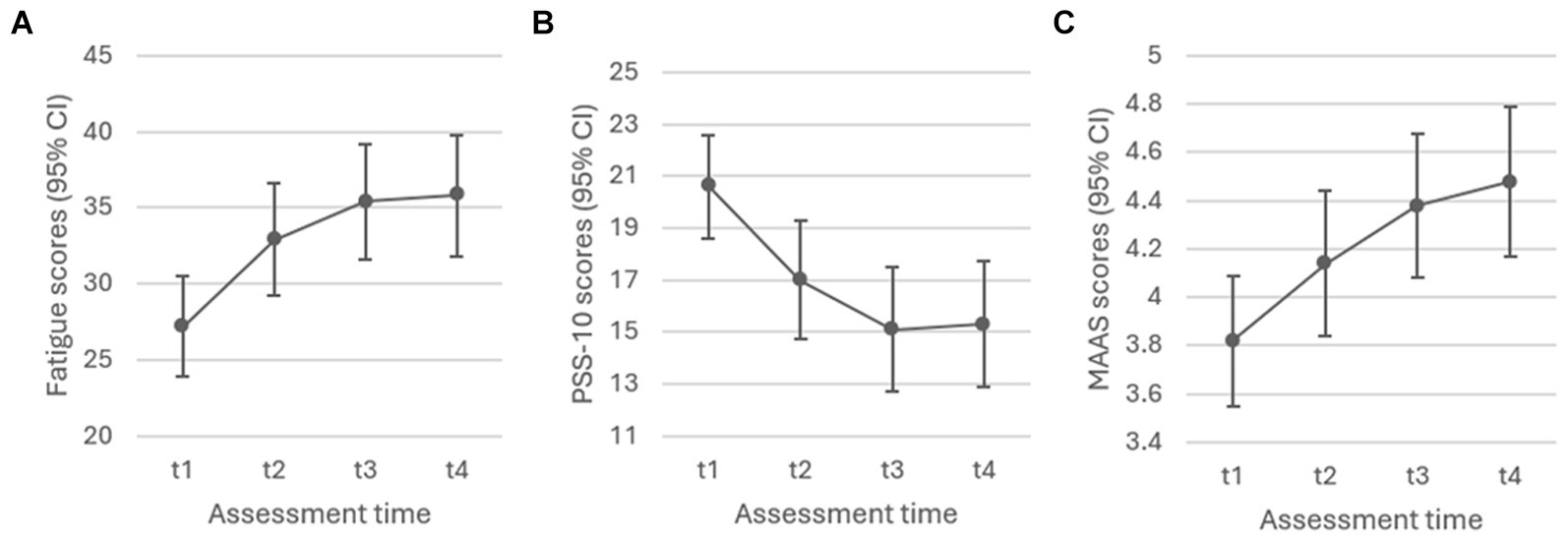
Figure 4. Study 2: Liner Mixed-Effect Model estimates with (A) fatigue (p < 0.001), (B) perceived stress (p < 0.001), and (C) mindfulness (p < 0.001) as outcomes.
3.2.3 Effects of self-practice frequency and duration
As per ANOVA, the mean number of days per week of self-practice over the past 4 weeks/8 weeks in case of t4 (frequency) had a significant effect on stress in Study 2 at t3 (F(3, 42) = 4.248, p = 0.010), with 4–5 days of practice in the preceding weeks associated with less stress compared to 0–1 days (p = 0.006). Conversely, at t4 (F(3, 36) = 2.925, p = 0.047) 4–5 days of self-practice during the preceding weeks was associated with higher stress compared to 2–3 days of self-practice (p = 0.037). Self-practice frequency had a significant effect on mindfulness at t3 (F(3, 41) = 3.951, p = 0.015), with 4–5 days of self-practice associated with higher mindfulness scores than precedent self-practice of only 2–3 days (p = 0.045). Finally, the mean duration of self-practice per day in the preceding weeks had a significant effect on fatigue at t2 (F(4, 45), p = 0.037), with significantly more fatigue in conjunction with a practice of longer than 30 min compared to no practice at all (p = 0.024).
3.3 Study 2 discussion
Using a repeated-measures design with four assessment times (follow-up at 8 weeks post intervention) in subjects diagnosed with cancer (past 5 years), Study 2 found significantly improved CRF, stress, and mindfulness scores in conjunction with the adapted ERYT-based online intervention. The exploratory analysis of practice frequency and duration yielded inconclusive results. As with the former study, the interpretability of our findings is challenged by relatively high dropout rates, a common problem of online survey-based research. A detailed discussion of findings follows in the subsequent section.
4 General discussion
Persistent fatigue is one of the most common and taxing sequelae of cancer (Bower, 2014) and presents a challenge in a series of other chronic illnesses (Whitehead, 2009). Using an exploratory single-arm repeated measures design based on two consecutive studies, the current work assessed an online application of ERYT to address CRF and associated symptoms. Study 1 consisted of a preliminary assessment in a mixed subjects sample of N = 165 adults with or without cancer diagnosis. Mixed-effects model estimates of the repeated measures before, during, after, and at follow up of the 6-week ERYT online program pointed to significantly improved emotional and physical well-being, reduced stress, and increased mindfulness, but had no effect on fatigue, functional and social well-being, or sleep quality. However, given the low proportion of cancer patients and survivors in this first sample, conclusions regarding CRF could not be drawn based on Study 1. Study 2 therefore involved a similar design with a sample of N = 125 adults who had been diagnosed with cancer within the past 5 years. Model estimates showed significant improvements of CRF, stress, and mindfulness scores in conjunction with the adapted 8-week long ERYT-based online intervention.
To our knowledge this is the first study examining an online application of ERYT. Taken together, our results suggest that online ERYT may reduce CRF in individuals diagnosed with cancer, may involve an increase in mindfulness, and could be associated with benefits for stress and well-being. However, controlled clinical trials will be needed to confirm and further elaborate these findings. Clinical research on ERYT in general is still scarce, but our results are in line with the few existent face-to-face ERYT studies that found reduced CRF in breast cancer patients and survivors (Oei et al., 2021; Kröz et al., 2023). Another study found reduced fatigue scores in moderately stressed adults after receiving ERYT (Kanitz et al., 2012), and a systematic review on the effectiveness of ERYT in various clinical populations (e.g., cancer, hypertension, chronic low back pain, anxiety, and other indications) concluded the implementation of ERYT as an adjunct therapy to be associated with improvements in health (Lötzke et al., 2015). Furthermore, our results are in line with findings on other mindful-movement based practices: Meta-analyses and reviews on Yoga, Tai Chi, and Qigong for instance concluded that these practices were able to relieve CRF in cancer patients/survivors (Dong et al., 2019; Sadja and Mills, 2013; Cramer et al., 2012a; Armer and Lutgendorf, 2019; Liu et al., 2020; Song et al., 2018; Yin et al., 2020; Zeng et al., 2019), but described magnitude of effects varied from study to study. Furthermore, our results converge with meta-analytic findings reporting significantly reduced CRF in RCTs of Mindfulness-Based Stress Reduction (MBSR, Kabat-Zinn, 2003) and similar interventions in oncology populations (Johns et al., 2021; Chayadi et al., 2022; Xie et al., 2020; Zhang et al., 2019; McCloy et al., 2022), although one meta-analysis found improved stress and sleep but no significant effects on fatigue or quality of life in conjunction with MBSR (Wu et al., 2022). In several of the former meta-analyses results regarding sleep quality were less consistent (Zhang et al., 2019; McCloy et al., 2022), which was perhaps mirrored in our Study 1, although, as mentioned before, the sample did not allow conclusions regarding oncology populations. Finally, we found a series of significant but inconclusive effects of differential practice times (frequencies and durations) of ERYT on CRF, stress, and mindfulness (Study 2), as well as sleep and well-being indicators (Study 1), but only for selected assessment times, and the optimal amount of self-practice appeared to differ in relation to the various assessment times and outcome variables. While further research with systematic comparisons of self-practice times will be needed to elucidate these findings, the current exploratory assessment suggests a tendency of more/longer self-practice associated with benefits, although in a few instances the opposite was the case. Given the latter occurred particularly in the context of extended self-practice times, it is not inconceivable that lengthening practice beyond a certain optimum could turn benefit into detriment. Several reviews of mindfulness-based interventions report positive associations between home practice and intervention outcomes in both general and cancer-affected populations (Parsons et al., 2017; Baydoun et al., 2021; Kang et al., 2021), but research in this context is scarce, and a consensus on optimal practice times in view of treatment effectiveness and adherence remains to be established.
Although single-arm evaluations are an important step in exploratory research, the lack of a control condition and randomization was a limitation of the current work and will be necessary to confirm beneficial effects of online ERYT. Furthermore, due to the voluntary nature of participation and hence self-selection of participants we cannot rule out sampling bias, which limits the generalizability of our findings. Finally, response and survey completion rates per assessment time (Figures 1, 3) were relatively low, which is however not unusual for online studies based on voluntary and non-compensated participation (Rostaminezhad et al., 2013; Bawa, 2016; Fish et al., 2016; Meyerowitz-Katz et al., 2020), but nonetheless speaks for cautious interpretation of results. Indeed, the possibility of dropout effects represents a notorious challenge for clinical research relying on longitudinal assessments; such effects may compromise interpretability of findings in particular, in cases in which the dropout-related missingness is non-random (Bell et al., 2013), which is generally difficult to rule out, but for which mixed-effect models are considered a method of choice, given their capacity to minimize dropout bias in longitudinal research with both random or non-random missingness (Mallinckrodt et al., 2001; Bell et al., 2013). Although our findings provide promising first indications, future studies should hence attempt to reduce dropout (Meyerowitz-Katz et al., 2020), include controlled designs, as well as systematic comparisons of varying practice times and subgroups (e.g., individuals currently in treatment vs. cancer survivors). In addition, assessing the duration of disease and/or remission period as well as therapeutic protocols per participant would be favourable for an enhanced contextualization of CRF levels and other outcomes at the various assessment times. Strengths of the current work include the novelty of the approach and its potential to expand the still limited toolkit for addressing CRF in oncology populations, as well as the limited research on ERYT in general. Furthermore, the group format and online delivery imply affordability and scalability, which along with the adaptability of ERYT exercises, renders the intervention more broadly accessible, also in locations in which ERYT therapists are not readily available, and, pertinently, for individuals who are unable to leave their home due to debilitating cancer treatment side-effects (e.g., dizziness, nausea, swollen joints; Kim et al., 2020) and not least CRF itself (Bower, 2014). A recent meta-analysis of online interventions involving mindfulness-based practices for cancer patients concluded online delivery to be both feasible and acceptable to manage cancer-related symptoms (Fan et al., 2023), with similar conclusions reiterated in studies examining online delivery of specific mindfulness-based movement practices, such as Tai Chi and Qigong (Oh et al., 2021; Gao et al., 2022; Sohl et al., 2024). Online ERYT may be an additional such option, with promising first results that should be further investigated.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
Ethical approval was not required for the studies involving humans given full anonymity of participants at all stages of the research (fully encrypted survey via anonymous self-generated codes, no collection of IP or E-Mail addresses, no collection of identifying participant data). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements because participants were thoroughly informed in written form about the study and the voluntary nature of participation; they provided implied informed consent by completing the online survey (opt-in).
Author contributions
ET: Data curation, Formal analysis, Investigation, Project administration, Writing – original draft, Writing – review & editing. YK: Data curation, Writing – review & editing. TH: Conceptualization, Funding acquisition, Writing – review & editing. IB: Writing – original draft, Writing – review & editing. UW: Conceptualization, Funding acquisition, Project administration, Supervision, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. Namely, the expenses related to conducting the interventions were covered by Eurythmy4you. Förderverein Anthroposophische Medizin covered the PSS-10 license fee.
Acknowledgments
We extend our thanks to Monika Birkhofer, Joachim Luger, Tobias Friedly, Esther Gwee, Mikan Xuan, and Adele Waldmann for kindly offering administrative, technical, and linguistic support in this study. For consultation on data analysis we are indebted to the statistician Dr. André Moser (Clinical Trials Unit, University of Bern).
Conflict of interest
TH works as a therapist at the health provider Eurythmy4you but was not involved in the collection, handling, or analysis of data in this study, which was done independently by the scientific authors.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Footnotes
1. ^Eurythmy4you.
References
Adamson, M. M., Phillips, A., Seenivasan, S., Martinez, J., Grewal, H., Kang, X., et al. (2020). International prevalence and correlates of psychological stress during the global COVID-19 pandemic. Int. J. Environ. Res. Public Health 17:9248. doi: 10.3390/ijerph17249248
Alexander, S., Minton, O., and Stone, P. C. (2009). Evaluation of screening instruments for cancer-related fatigue syndrome in breast cancer survivors. J. Clin. Oncol. 27, 1197–1201. doi: 10.1200/JCO.2008.19.1668
Armer, J. S., and Lutgendorf, S. K. (2019). The impact of yoga on fatigue in cancer survivorship: a meta-analysis. JNCI Cancer Spectr. 4:pkz098. doi: 10.1093/jncics/pkz098
Bates, D., Mächler, M., Bolker, B., and Walker, S. (2015). Fitting linear mixed-effects models using lme4. J. Stat. Softw. 67, 1–48. doi: 10.18637/jss.v067.i01
Bawa, P. (2016). Retention in online courses: exploring issues and solutions—a literature review. SAGE Open 6:2158244015621777. doi: 10.1177/2158244015621777
Baydoun, M., Moran, C., Mclennan, A., Piedalue, K.-A. L., Oberoi, D., and Carlson, L. E. (2021). Mindfulness-based interventions in cancer survivors: a systematic review of participants’ adherence to home practice. Patient Prefer. Adherence 15, 1225–1242. doi: 10.2147/PPA.S267064
Bell, M. L., Kenward, M. G., Fairclough, D. L., and Horton, N. J. (2013). Differential dropout and bias in randomised controlled trials: when it matters and when it may not. BMJ 346:e8668. doi: 10.1136/bmj.e8668
Berger, B., Bertram, M., Kanitz, J., Pretzer, K., and Seifert, G. (2015). “Like walking into an empty room”: effects of eurythmy therapy on stress perception in comparison with a sports intervention from the subjects’ perspective—a qualitative study. Evid. Based Complement. Alternat. Med. 2015:856107. doi: 10.1155/2015/856107
Bower, J. E. (2014). Cancer-related fatigue—mechanisms, risk factors, and treatments. Nat. Rev. Clin. Oncol. 11, 597–609. doi: 10.1038/nrclinonc.2014.127
Brosnan, P., Nauphal, M., and Tompson, M. C. (2021). Acceptability and feasibility of the online delivery of hatha yoga: a systematic review of the literature. Complement. Ther. Med. 60:102742. doi: 10.1016/j.ctim.2021.102742
Brown, K. W., and Kasser, T. (2005). Are psychological and ecological well-being compatible? The role of values, mindfulness, and lifestyle. Soc. Indic. Res. 74, 349–368. doi: 10.1007/s11205-004-8207-8
Brown, K. W., and Ryan, R. M. (2003). The benefits of being present: mindfulness and its role in psychological well-being. J. Pers. Soc. Psychol. 84, 822–848. doi: 10.1037/0022-3514.84.4.822
Brown, V. A. (2021). An introduction to linear mixed-effects modeling in R. Adv. Methods Pract. Psychol. Sci. 4:2515245920960351. doi: 10.1177/2515245920960351
Butt, Z., Rao, A. V., Lai, J.-S., Abernethy, A. P., Rosenbloom, S. K., and Cella, D. (2010). Age-associated differences in fatigue among patients with cancer. J. Pain Symptom Manag. 40, 217–223. doi: 10.1016/j.jpainsymman.2009.12.016
Cai, T., Chen, J., Ni, F., Zhu, R., Wu, F., Huang, Q., et al. (2023). Psychometric properties of the Chinese version of the functional assessment of chronic illness therapy–fatigue (FACIT–F) among patients with breast cancer. Health Qual. Life Outcomes 21:91. doi: 10.1186/s12955-023-02164-4
Carlson, L. E., and Brown, K. W. (2005). Validation of the mindful attention awareness scale in a cancer population. J. Psychosom. Res. 58, 29–33. doi: 10.1016/j.jpsychores.2004.04.366
Cella, D. (1997). FACIT manual: manual of the functional assessment of chronic illness therapy (FACIT) measurement system: Center on Outcomes, Research and Education. Evanston IL: Evanston Northwestern Healthcare and Northwestern University.
Chayadi, E., Baes, N., and Kiropoulos, L. (2022). The effects of mindfulness-based interventions on symptoms of depression, anxiety, and cancer-related fatigue in oncology patients: a systematic review and meta-analysis. PLoS One 17:e0269519. doi: 10.1371/journal.pone.0269519
Chen, M.-Y., Zheng, W.-Y., Liu, Y.-F., Li, X.-H., Lam, M. I., Su, Z., et al. (2024). Global prevalence of poor sleep quality in cancer patients: a systematic review and meta-analysis. Gen. Hosp. Psychiatry 87, 92–102. doi: 10.1016/j.genhosppsych.2023.12.004
Chen, S.-Y., Cui, H., Zhou, R.-L., and Jia, Y.-Y. (2012). Revision of mindful attention awareness scale (MAAS). Chin. J. Clin. Psych. 20, 148–151. doi: 10.16128/j.cnki.1005-3611.2012.02.024
Chrobak, A. A., Przydacz, M., Chłosta, M., Machalska, K., Turek, A., Popiół, M., et al. (2023). Bipolar spectrum in prostate cancer patients and its role in stress related symptoms. Psycho-Oncology 32, 438–445. doi: 10.1002/pon.6096
Chui, P. L. (2021). Mindful breathing: effects of a five-minute practice on perceived stress and mindfulness among patients with cancer. Clin. J. Oncol. Nurs. 25, 174–180. doi: 10.1188/21.CJON.174-180
Cleeland, C. S., Zhao, F., Chang, V. T., Sloan, J. A., Omara, A. M., Gilman, P. B., et al. (2013). The symptom burden of cancer: evidence for a core set of cancer‐related and treatment‐related symptoms from the eastern cooperative oncology group symptom outcomes and practice patterns study. Cancer 119, 4333–4340. doi: 10.1002/cncr.28376
Cocchiara, R. A., Dorelli, B., Gholamalishahi, S., Longo, W., Musumeci, E., Mannocci, A., et al. (2020). Tai Chi and workplace wellness for health care workers: a systematic review. Int. J. Environ. Res. Public Health 17:343. doi: 10.3390/ijerph17010343
Cohen, S. (1988). Perceived stress in a probability sample of the United States. in The Social Psychology of Health. Eds. S. Spacapan and S. Oskamp. Thousand Oaks, California, USA: Sage Publications, Inc. 31–67.
Cohen, S., Kamarck, T., and Mermelstein, R. (1983). A global measure of perceived stress. J. Health Soc. Behav. 24, 385–396. doi: 10.2307/2136404
Cramer, H., Lange, S., Klose, P., Paul, A., and Dobos, G. (2012a). Can yoga improve fatigue in breast cancer patients? A systematic review. Acta Oncol. 51, 559–560. doi: 10.3109/0284186X.2011.637960
Cramer, H., Lange, S., Klose, P., Paul, A., and Dobos, G. (2012b). Yoga for breast cancer patients and survivors: a systematic review and meta-analysis. BMC Cancer 12:412. doi: 10.1186/1471-2407-12-412
Desveaux, L., Lee, A., Goldstein, R., and Brooks, D. (2015). Yoga in the management of chronic disease: a systematic review and meta-analysis. Med. Care 53, 653–661. doi: 10.1097/MLR.0000000000000372
Dieck, A., Morin, C. M., and Backhaus, J. (2018). A German version of the insomnia severity index. Somnologie 22, 27–35. doi: 10.1007/s11818-017-0147-z
Dong, B., Xie, C., Jing, X., Lin, L., and Tian, L. (2019). Yoga has a solid effect on cancer-related fatigue in patients with breast cancer: a meta-analysis. Breast Cancer Res. Treat. 177, 5–16. doi: 10.1007/s10549-019-05278-w
facit.org. (2022). Available at: https://www.facit.org/ (Accessed 2023).
Fan, M., Wang, Y., Zheng, L., Cui, M., Zhou, X., and Liu, Z. (2023). Effectiveness of online mindfulness-based interventions for cancer patients: a systematic review and meta-analysis. Jpn. J. Clin. Oncol. 53, 1068–1076. doi: 10.1093/jjco/hyad101
Firkins, J., Hansen, L., Driessnack, M., and Dieckmann, N. (2020). Quality of life in “chronic” cancer survivors: a meta-analysis. J. Cancer Surviv. 14, 504–517. doi: 10.1007/s11764-020-00869-9
Fish, J., Brimson, J., and Lynch, S. (2016). Mindfulness interventions delivered by technology without facilitator involvement: what research exists and what are the clinical outcomes? Mindfulness 7, 1011–1023. doi: 10.1007/s12671-016-0548-2
Gabrio, A., Plumpton, C., Banerjee, S., and Leurent, B. (2022). Linear mixed models to handle missing at random data in trial-based economic evaluations. Health Econ. 31, 1276–1287. doi: 10.1002/hec.4510
Gao, Z., Ryu, S., and Chen, Y. (2022). Effects of Tai Chi app and Facebook health education programs on breast cancer survivors’ stress and quality of life in the era of pandemic. Complement. Ther. Clin. Pract. 48:101621. doi: 10.1016/j.ctcp.2022.101621
Gouw, V. X. H., Jiang, Y., Seah, B., He, H., Hong, J., and Wang, W. (2019). Effectiveness of internal qigong on quality of life, depressive symptoms and self-efficacy among community-dwelling older adults with chronic disease: a systematic review and meta-analysis. Int. J. Nurs. Stud. 99:103378. doi: 10.1016/j.ijnurstu.2019.06.009
Gravesande, J., Almeida De Oliveira, L., Malik, N., Vrkljan, B., Zheng, R., Gardner, P. M., et al. (2023). Feasibility, usability, and acceptability of online mind–body exercise programs for older adults: a scoping review. J. Integr. Compl. Med. 29, 538–549. doi: 10.1089/jicm.2022.0822
Haas, H. (2017). Salutogenese und achtsamkeitsorientierte anthroposophische Psychotherapie am Beispiel ambulanter Gruppentherapien bei «Nervosität». Swiss J. Integr. Med. 29, 330–335. doi: 10.1159/000484462
Hamre, H., Witt, C., Glockmann, A., Wegscheider, K., Ziegler, R., Willich, S., et al. (2007). Anthroposophic vs. conventional therapy for chronic low back pain: a prospective comparative study. Eur. J. Med. Res. 12:302.
Hamre, H. J., Kiene, H., Glockmann, A., Ziegler, R., and Kienle, G. S. (2013). Long-term outcomes of anthroposophic treatment for chronic disease: a four-year follow-up analysis of 1510 patients from a prospective observational study in routine outpatient settings. BMC. Res. Notes 6, 1–13. doi: 10.1186/1756-0500-6-269
Hamre, H. J., Witt, C. M., Glockmann, A., Ziegler, R., Willich, S. N., and Kiene, H. (2006). Anthroposophic therapy for chronic depression: a four-year prospective cohort study. BMC Psychiatry 6, 1–13. doi: 10.1186/1471-244X-6-57
Hamre, H. J., Witt, C. M., Glockmann, A., Ziegler, R., Willich, S. N., and Kiene, H. (2007). Eurythmy therapy in chronic disease: a four-year prospective cohort study. BMC Public Health 7:61. doi: 10.1186/1471-2458-7-61
Hamre, H. J., Witt, C. M., Kienle, G. S., Glockmann, A., Ziegler, R., Willich, S. N., et al. (2009). Anthroposophic therapy for anxiety disorders: a two-year prospective cohort study in routine outpatient settings. Clin. Med. Insights Psychiatry 2:S2791. doi: 10.4137/CMPsy.S2791
Hillier, S., and Worley, A. (2015). The effectiveness of the Feldenkrais method: a systematic review of the evidence 2015:752160.
Human Research Act, H. (2011). “810.30 Federal Act of 30 September 2011 on Research involving Human beings (Human Research Act, HRA)” in. ed. T. F. C. O. T. S. Confederation. Available at: https://www.fedlex.admin.ch/eli/cc/2013/617/en Federal Council of Switzerland
Jiang, C., Ma, H., Luo, Y., Fong, D. Y. T., Umucu, E., Zheng, H., et al. (2023). Validation of the Chinese version of the perceived stress scale-10 integrating exploratory graph analysis and confirmatory factor analysis. Gen. Hosp. Psychiatry 84, 194–202. doi: 10.1016/j.genhosppsych.2023.07.008
Johns, S. A., Tarver, W. L., Secinti, E., Mosher, C. E., Stutz, P. V., Carnahan, J. L., et al. (2021). Effects of mindfulness-based interventions on fatigue in cancer survivors: a systematic review and meta-analysis of randomized controlled trials. Crit. Rev. Oncol. Hematol. 160:103290. doi: 10.1016/j.critrevonc.2021.103290
Kang, C., Sun, S., Yang, Z., Fan, X., Yuan, J., Xu, L., et al. (2021). The psychological effect of internet-based mindfulness-based stress reduction on the survivors of breast cancer during the COVID-19. Front. Psych. 12:738579. doi: 10.3389/fpsyt.2021.738579
Kanitz, J. L., Pretzer, K., Calaminus, G., Wiener, A., Längler, A., Henze, G., et al. (2013). Eurythmy therapy in the aftercare of pediatric posterior fossa tumour survivors—a pilot study. Complement. Ther. Med. 21, S3–S9. doi: 10.1016/j.ctim.2012.02.007
Kanitz, J. L., Pretzer, K., Reif, M., Voss, A., Brand, R., Warschburger, P., et al. (2011). The impact of eurythmy therapy on stress coping strategies and health-related quality of life in healthy, moderately stressed adults. Complement. Ther. Med. 19, 247–255. doi: 10.1016/j.ctim.2011.06.008
Kanitz, J. L., Pretzer, K., Reif, M., Witt, K., Reulecke, S., Voss, A., et al. (2012). The impact of eurythmy therapy on fatigue in healthy adults—a controlled trial. Eur. J. Integr. Med. 4, e289–e297. doi: 10.1016/j.eujim.2012.02.006
Kienle, G. S., Albonico, H. U., Baars, E., Hamre, H. J., Zimmermann, P., and Kiene, H. (2013). Anthroposophic medicine: an integrative medical system originating in europe. Glob. Adv. Health Med. 2, 20–31. doi: 10.7453/gahmj.2012.087
Kim, S., Han, J., Lee, M. Y., and Jang, M. K. (2020). The experience of cancer-related fatigue, exercise and exercise adherence among women breast cancer survivors: insights from focus group interviews. J. Clin. Nurs. 29, 758–769. doi: 10.1111/jocn.15114
Kirchner-Bockholt, M. (1977). Fundamental principles of curative eurythmy. London: Temple Lodge publishing Rudolf Steiner Press.
Klein, E. M., Brähler, E., Dreier, M., Reinecke, L., Müller, K. W., Schmutzer, G., et al. (2016). The German version of the perceived stress scale – psychometric characteristics in a representative German community sample. BMC Psychiatry 16:159. doi: 10.1186/s12888-016-0875-9
Kröz, M., Fink, M., Reif, M., Grobbecker, S., Zerm, R., Quetz, M., et al. (2013). Multimodal therapy concept and aerobic training in breast cancer patients with chronic cancer-related fatigue 12, 301–311.
Kröz, M., Quittel, F., Reif, M., Zerm, R., Pranga, D., Bartsch, C., et al. (2023). Four-year follow-up on fatigue and sleep quality of a three-armed partly randomized controlled study in breast cancer survivors with cancer-related fatigue. Sci. Rep. 13:2705. doi: 10.1038/s41598-022-25322-y
Kröz, M., Reif, M., Glinz, A., Berger, B., Nikolaou, A., Zerm, R., et al. (2017). Impact of a combined multimodal-aerobic and multimodal intervention compared to standard aerobic treatment in breast cancer survivors with chronic cancer-related fatigue – results of a three-armed pragmatic trial in a comprehensive cohort design. BMC Cancer 17:166. doi: 10.1186/s12885-017-3142-7
Lin, C. Y., Cheng, A. S., Nejati, B., Imani, V., Ulander, M., Browall, M., et al. (2020). A thorough psychometric comparison between Athens insomnia scale and insomnia severity index among patients with advanced cancer. J. Sleep Res. 29:e12891. doi: 10.1111/jsr.12891
Liu, L., Tan, H., Yu, S., Yin, H., and Baxter, G. D. (2020). The effectiveness of Tai Chi in breast cancer patients: a systematic review and meta-analysis. Complement. Ther. Clin. Pract. 38:101078. doi: 10.1016/j.ctcp.2019.101078
Lötzke, D., Heusser, P., and Büssing, A. (2015). A systematic literature review on the effectiveness of eurythmy therapy. J. Integr. Med. 13, 217–230. doi: 10.1016/S2095-4964(15)60163-7
Ma, Y., He, B., Jiang, M., Yang, Y., Wang, C., Huang, C., et al. (2020). Prevalence and risk factors of cancer-related fatigue: a systematic review and meta-analysis. Int. J. Nurs. Stud. 111:103707. doi: 10.1016/j.ijnurstu.2020.103707
Mallinckrodt, C. H., Clark, W. S., and David, S. R. (2001). Accounting for dropout bias using mixed-effects models. J. Biopharm. Stat. 11, 9–21. doi: 10.1081/BIP-100104194
Mayden, K. D. (2012). Mind-body therapies: evidence and implications in advanced oncology practice. J. Adv. Pract. Oncol. 3, 357–373
Mccloy, K., Hughes, C., Dunwoody, L., Marley, J., and Gracey, J. (2022). Effects of mindfulness-based interventions on fatigue and psychological wellbeing in women with cancer: a systematic review and meta-analysis of randomised control trials. Psycho-Oncology 31, 1821–1834. doi: 10.1002/pon.6046
Meier-Girard, D., Ribi, K., Gerstenberg, G., Ruhstaller, T., and Wolf, U. (2020). Eurythmy therapy versus slow movement fitness in the treatment of fatigue in metastatic breast cancer patients: study protocol for a randomized controlled trial. Trials 21:612. doi: 10.1186/s13063-020-04542-5
Meyerowitz-Katz, G., Ravi, S., Arnolda, L., Feng, X., Maberly, G., and Astell-Burt, T. (2020). Rates of attrition and dropout in app-based interventions for chronic disease: systematic review and Meta-analysis. J. Med. Internet Res. 22:e20283. doi: 10.2196/20283
Michalak, J., Heidenreich, T., Ströhle, G., and Nachtigall, C. (2008). Die deutsche version der mindful attention and awareness scale (maas) psychometrische befunde zu einem achtsamkeitsfragebogen. Z. Klin. Psychol. Psychother. 37, 200–208. doi: 10.1026/1616-3443.37.3.200
Michalsen, A., Jeitler, M., Kessler, C. S., Steckhan, N., Robens, S., Ostermann, T., et al. (2021). Yoga, eurythmy therapy and standard physiotherapy (YES-trial) for patients with chronic non-specific low back pain: a three-armed randomized controlled trial. J. Pain 22, 1233–1245. doi: 10.1016/j.jpain.2021.03.154
Michaud, A. L., Zhou, E. S., Chang, G., and Recklitis, C. J. (2021). Validation of the insomnia severity index (ISI) for identifying insomnia in young adult cancer survivors: comparison with a structured clinical diagnostic interview of the DSM-5 (SCID-5). Sleep Med. 81, 80–85. doi: 10.1016/j.sleep.2021.01.045
Miller, S. M., Hui-Lio, C., and Taylor-Piliae, R. E. (2020). Health benefits of Tai Chi exercise: a guide for nurses. Nurs. Clin. 55, 581–600. doi: 10.1016/j.cnur.2020.07.002
Montan, I., Löwe, B., Cella, D., Mehnert, A., and Hinz, A. (2018). General population norms for the functional assessment of chronic illness therapy (FACIT)-fatigue scale. Value Health 21, 1313–1321. doi: 10.1016/j.jval.2018.03.013
Morin, C. M., Belleville, G., Bélanger, L., and Ivers, H. (2011). The insomnia severity index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep 34, 601–608. doi: 10.1093/sleep/34.5.601
Oei, S. L., Thronicke, A., Matthes, H., and Schad, F. (2021). Assessment of integrative non-pharmacological interventions and quality of life in breast cancer patients using real-world data. Breast Cancer 28, 608–617. doi: 10.1007/s12282-020-01193-x
Oh, B., Van Der Saag, D., Morgia, M., Carroll, S., Boyle, F., Back, M., et al. (2021). An innovative Tai Chi and Qigong telehealth service in supportive cancer care during the COVID-19 pandemic and beyond. Am. J. Lifestyle Med. 15, 475–477. doi: 10.1177/1559827620983762
Parsons, C. E., Crane, C., Parsons, L. J., Fjorback, L. O., and Kuyken, W. (2017). Home practice in mindfulness-based cognitive therapy and mindfulness-based stress reduction: a systematic review and meta-analysis of participants' mindfulness practice and its association with outcomes. Behav. Res. Ther. 95, 29–41. doi: 10.1016/j.brat.2017.05.004
Pinheiro, J., and Bates, D.R Core Team (2023). _nlme: linear and nonlinear mixed effects models_. R Package Version. The R Foundation: Vienna, Austria. 3, 1–164.
R Core Team (2024). R: a language and environment for statistical computing. Vienna, Austria: R Core Team.
Raman, G., Zhang, Y., Minichiello, V. J., D'ambrosio, C. M., and Wang, C. (2013). Tai Chi improves sleep quality in healthy adults and patients with chronic conditions: a systematic review and meta-analysis. J. Sleep Disord. Ther. 2:2–6. doi: 10.4172/2167-0277.1000141
Rostaminezhad, M., Mozayani, N., Norozi, D., and Iziy, M. (2013). Factors related to e-learner dropout: case study of IUST elearning center. Procedia Soc. Behav. Sci. 83, 522–527. doi: 10.1016/j.sbspro.2013.06.100
Sadja, J., and Mills, P. J. (2013). Effects of yoga interventions on fatigue in cancer patients and survivors: a systematic review of randomized controlled trials. Explore 9, 232–243. doi: 10.1016/j.explore.2013.04.005
Savard, M. H., Savard, J., Simard, S., and Ivers, H. (2005). Empirical validation of the insomnia severity index in cancer patients. Psycho-Oncology 14, 429–441. doi: 10.1002/pon.860
Schwab, J. H., Murphy, J. B., Anderson, P., Lunde, G., Kiene, H., Hamre, H. J., et al. (2011). Eurythmy therapy in anxiety. Altern. Ther. Health Med. 17:56.
Sohl, S. J., Strahley, A. E., Tooze, J. A., Levine, B. J., Kelly, M. G., Wheeler, A., et al. (2024). Qualitative results from a randomized pilot study of eHealth mindful movement and breathing to improve gynecologic cancer surgery outcomes. J. Psychosoc. Oncol. 42, 223–241. doi: 10.1080/07347332.2023.2236083
Song, S., Yu, J., Ruan, Y., Liu, X., Xiu, L., and Yue, X. (2018). Ameliorative effects of Tai Chi on cancer-related fatigue: a meta-analysis of randomized controlled trials. Support. Care Cancer 26, 2091–2102. doi: 10.1007/s00520-018-4136-y
Soria-Reyes, L. M., Cerezo, M. V., Alarcón, R., and Blanca, M. J. (2023). Psychometric properties of the perceived stress scale (pss-10) with breast cancer patients. Stress. Health 39, 115–124. doi: 10.1002/smi.3170
Stephens, J., and Hillier, S. (2020). Evidence for the effectiveness of the Feldenkrais method. Kinesiol. Rev. 9, 228–235. doi: 10.1123/kr.2020-0022
Sung, H., Ferlay, J., Siegel, R. L., Laversanne, M., Soerjomataram, I., Jemal, A., et al. (2021). Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 71, 209–249. doi: 10.3322/caac.21660
Teo, J. L., Bird, S. R., Wang, X., and Zheng, Z. (2024). Using telehealth to deliver Qi Gong and Tai Chi programs: a mixed-methods systematic review on feasibility, acceptability and participant engagement factors. Arch. Gerontol. Geriatr. 117:105203. doi: 10.1016/j.archger.2023.105203
Tran, K. B., Lang, J. J., Compton, K., Xu, R., Acheson, A. R., Henrikson, H. J., et al. (2022). The global burden of cancer attributable to risk factors, 2010–19: a systematic analysis for the global burden of disease study 2019. Lancet 400, 563–591. doi: 10.1016/S0140-6736(22)01438-6
Trojnar, A., Knetki-Wróblewska, M., Sobieraj, P., and Domagała-Kulawik, J. (2024). Lung cancer in women—sociodemographic, clinical and psychological characteristics with comparison to men. J. Clin. Med. 13:1450. doi: 10.3390/jcm13051450
Tseng, A. (2024). Effectiveness of mindfulness-based stress reduction (MBSR) interventions on mindfulness and stress symptoms for cancer patients: a quantitative assessment. OBM Integr. Compl. Med. 9, 1–30. doi: 10.21926/obm.icm.2401019
Vergeer, I., Johansson, M., and Cagas, J. Y. (2021). Holistic movement practices – an emerging category of physical activity for exercise psychology. Psychol. Sport Exerc. 53:101870. doi: 10.1016/j.psychsport.2020.101870
Wang, F., Man, J. K. M., Lee, E.-K. O., Wu, T., Benson, H., Fricchione, G. L., et al. (2013). The effects of qigong on anxiety, depression, and psychological well-being: a systematic review and meta-analysis. Evid. Based Complement. Alternat Med. 2013:152738. doi: 10.1155/2013/149363
Wang, F., and Szabo, A. (2020). Effects of yoga on stress among healthy adults: a systematic review. Altern. Ther. Health Med. 26:AT6214.
Webster, K., Cella, D., and Yost, K. (2003). The Functional assessment of Chronic Illness Therapy (FACIT) measurement system: properties, applications, and interpretation. Health Qual. Life Outcomes 1:79. doi: 10.1186/1477-7525-1-79
Whitehead, L. (2009). The measurement of fatigue in chronic illness: a systematic review of unidimensional and multidimensional fatigue measures. J. Pain Symptom Manag. 37, 107–128. doi: 10.1016/j.jpainsymman.2007.08.019
Wu, H., Li, F., and Zhang, F. (2022). The efficacy of mindfulness-based stress reduction vs. standard or usual care in patients with breast cancer: a systematic review and meta-analysis of randomized controlled trials. Transl. Cancer Res. 11, 4148–4158. doi: 10.21037/tcr-22-2530
Xie, C., Dong, B., Wang, L., Jing, X., Wu, Y., Lin, L., et al. (2020). Mindfulness-based stress reduction can alleviate cancer- related fatigue: a meta-analysis. J. Psychosom. Res. 130:109916. doi: 10.1016/j.jpsychores.2019.109916
Yılmaz Koğar, E., and Koğar, H. (2024). A systematic review and meta-analytic confirmatory factor analysis of the perceived stress scale (PSS-10 and PSS-14). Stress. Health 40:e3285. doi: 10.1002/smi.3285
Yin, J., Tang, L., and Dishman, R. K. (2020). The efficacy of qigong practice for cancer-related fatigue: a systematic review and meta-analysis of randomized controlled trials. Ment. Health Phys. Act. 19:100347. doi: 10.1016/j.mhpa.2020.100347
Yusufov, M., Zhou, E. S., and Recklitis, C. J. (2019). Psychometric properties of the insomnia severity index in cancer survivors. Psycho-Oncology 28, 540–546. doi: 10.1002/pon.4973
Zeng, Y., Xie, X., and Cheng, A. S. K. (2019). Qigong or Tai Chi in cancer care: an updated systematic review and meta-analysis. Curr. Oncol. Rep. 21:48. doi: 10.1007/s11912-019-0786-2
Keywords: fatigue, cancer, cancer-related fatigue, mindful movement, mindfulness-based, eurythmy therapy, integrative medicine, online intervention
Citation: Timm E, Ko YM, Hundhammer T, Berlowitz I and Wolf U (2024) Online eurythmy therapy for cancer-related fatigue: a prospective repeated-measures observational study exploring fatigue, stress, and mindfulness. Front. Integr. Neurosci. 18:1472562. doi: 10.3389/fnint.2024.1472562
Edited by:
Georg Seifert, Charité University Medicine Berlin, GermanyReviewed by:
Heidemarie Haller, University of Duisburg-Essen, GermanyHenrik Szőke, University of Pécs, Hungary
Copyright © 2024 Timm, Ko, Hundhammer, Berlowitz and Wolf. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ilana Berlowitz, aWxhbmEuYmVybG93aXR6QHVuaWJlLmNo
†These authors share last authorship
 Eliane Timm
Eliane Timm Yobina Melanie Ko1
Yobina Melanie Ko1 Ilana Berlowitz
Ilana Berlowitz Ursula Wolf
Ursula Wolf