
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Integr. Neurosci. , 29 August 2024
Volume 18 - 2024 | https://doi.org/10.3389/fnint.2024.1432270
This article is part of the Research Topic Mind-body medicine and its impacts on psychological networks, quality of life, and health - Volume II View all 39 articles
Introduction: Pain is a complex phenomenon influenced by psychosocial variables, including the placebo effect. The effectiveness of mindfulness-based interventions (MBIs) for pain has been demonstrated in experimental studies and systematic reviews, but the mechanisms of action are only starting to be established. Whether the expectations of individuals experiencing pain can be manipulated during MBIs remains to be systematically evaluated, and what role placebo effects might play remains to be explored.
Methods: To evaluate the literature analyzing placebo effects in MBIs for pain, we performed a systematic review based on searches conducted in PubMed, Web of Science, and SCOPUS databases. Our search revealed a total of 272 studies, of which only 19 studies were included (10 acute pain and nine chronic pain), considering the inclusion and exclusion criteria related to expectations and placebo effects.
Results: From the 19 included studies, six measured placebo effects only in relation to the pharmacological intervention used in the study and not to an MBI.
Discussion: The results of the few studies that focused on the placebo effects of the MBIs indicate that placebo and expectations play a role in the MBIs' effects on pain. Although expectations and placebo effects are frequently discussed in the context of mindfulness and pain research, these results show that these factors are still not routinely considered in experimental designs. However, the results of the few studies included in this systematic review highlight a clear role for placebo and expectancy effects in the overall effects of MBIs for both acute and chronic pain, suggesting that routine measurement and further consideration in future studies are warranted. Additional research in this fascinating and challenging field is necessary to fully understand the connection between MBIs, placebo/expectations, and their effects on pain relief.
Pain is a multidimensional phenomenon with a significant biopsychosocial dimension. According to the International Association for the Study of Pain (IASP), pain is defined as “an unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential damage” (Raja et al., 2020). The biopsychosocial dimension of pain is fully recognized in the first note attached to the abovementioned pain definition. It determines the individuality of the pain experience: “Pain is always a personal experience that is influenced to varying degrees by biological, psychological, and social factors” (Raja et al., 2020). This subjective response to pain is dynamically modulated by complex interactions between sensory, cognitive, and affective factors (Price, 2000; Auvray et al., 2010). Pain is challenging to treat, and chronic pain is considered a medical issue (Turk, 2002; Cohen et al., 2021; Knopp-Sihota et al., 2022). Pain treatment is also an ethical issue since many patients fail to receive adequate pain relief (Hall and Boswell, 2009; Gatchel et al., 2014). Each pain patient is unique, and it is crucial to consider the individual behind the pain. The principles of autonomy, non-maleficence, beneficence, and justice are necessary to assist patients and their families in pain management (Swenson, 2002; Reeves and Jones, 2022). The use of cognitive-behavioral approaches in pain management is growing, as these methods help improve the patient's relationship with a painful experience (Moisset et al., 2020; Brandel et al., 2022; Yang et al., 2022).
Among cognitive-behavioral approaches, mindfulness-based interventions (MBIs) are increasingly used (Baminiwatta and Solangaarachchi, 2021). By defining mindfulness as the “awareness that arises through paying attention, on purpose, in the present moment, non-judgmentally,” Kabat-Zinn laid the foundation for using MBIs in pain management and other medical areas (Kabat-Zinn, 1982; Ludwig and Kabat-Zinn, 2008). Despite numerous studies on the efficacy of MBIs in pain management, the extent of their efficacy varies (Mcclintock et al., 2019; Shires et al., 2020; Schmidt and Pilat, 2023). Notably, the efficacy of MBIs is predominantly observed in reducing the aversive component of pain rather than its sensory component (Jinich-Diamant et al., 2020).
The variability in the efficacy of MBIs for pain can be attributed to some of the challenges in their design (Leca and Tavares, 2022; Cardle et al., 2023). The challenges include the lack of active controls in MBIs, the need for better reporting of important parameters such as the background of the meditation instructors, the wide diversity of evaluated outcome domains, and the lack of agreement on the operational definition of MBIs (session lengths, number of sessions, frequency of sessions, and duration of the intervention). One significant issue to consider in MBIs for pain management is the placebo effect. Several studies show that the efficacy of MBIs in pain management is lower when active controls (i.e., an experimental group that controls for the placebo effect) are used instead of passive controls (Goldberg et al., 2018; Shires et al., 2020; Hohenschurz-Schmidt et al., 2023a,b). Furthermore, the more specifically the active control is matched to the treatment (i.e., the better it controls for the placebo effect), the smaller the observed efficacy of MBIs is.
Placebo effects in pain responses are well-established (Coleshill et al., 2018; Bingel, 2020; Rossettini et al., 2020; Van Lennep et al., 2021). The term “placebo” originates from the Latin word “placere,” which means “to please” (Schedlowski et al., 2015; Meissner and Linde, 2018). The placebo effect involves the improvement of symptoms or physiological conditions following an inert treatment. It can be influenced by various factors, such as the natural progression of a disease, symptom fluctuations, response biases, the effects of co-interventions, and statistical phenomena. The placebo response, defined as the “outcome caused by a placebo manipulation,” depends on emotional and cognitive aspects.
Factors such as patient expectations, the quality of the doctor–patient relationship, and other variables were shown to significantly affect the placebo response (Schedlowski et al., 2015; Meissner and Linde, 2018).
The importance of the placebo effect is well-recognized, and its effects may be manipulated. It is well-established that the placebo effect may confound the specific actions of active compounds in pharmacologic studies (Scott et al., 2008). In clinical pharmacological trials, the placebo arm groups and the interference of non-specific effects are considered to fully evaluate the specific effect of a new treatment (Pollo and Benedetti, 2009; Enck et al., 2013). Recent research has advanced our understanding of the neural mechanisms underlying placebo effects. The potential to harness the placebo effect (Scott et al., 2008; Bingel et al., 2011) to influence therapy outcomes and benefit patients is currently being considered and discussed (Pollo and Benedetti, 2009; Enck et al., 2013).
Pain is modulated by a network of brain areas known as the supraspinal endogenous pain modulatory system. The understanding of this system has evolved considerably to include the dynamic interaction of pain with other interconnected dimensions, such as emotion and cognition (Tracey and Mantyh, 2007; Heinricher et al., 2009). Furthermore, the dynamic balance between inhibition and facilitation of top-down descending modulation is recognized, and an imbalance toward facilitation is considered to contribute to chronic pain (Tracey and Mantyh, 2007).
Among the brain areas of the endogenous pain modulatory system, the periaqueductal gray (PAG) plays a key role in top-down modulation by conveying most of the input from higher brain areas, such as the prefrontal cortex (PFC), which is involved in cognitive and executive control, and the amygdala, which is involved in emotional responses (Martins and Tavares, 2017; Ng et al., 2018). There are, however, direct effects on the spinal cord, such as direct cortico-spinal pathways from the anterior cingulate cortex (ACC), which facilitate the transmission of nociceptive information (Chen et al., 2018).
Regarding the neurobiological networks that may underlie the effects of MBIs on pain, a reduction in the activity of areas involved in emotional reactions to pain, such as the amygdala, may account for the reduction in aversion to the noxious event (Zeidan and Vago, 2016). Regarding the placebo effect, a neural network between the rostral ACC (rACC) and brain stem areas, including the PAG, has been proposed to account for placebo responses, showing similar activation patterns during opioid analgesia (Petrovic et al., 2002). In addition to the cingulofrontal brain regions, placebo analgesia is associated with activation in other areas, such as the PAG, hypothalamus, and amygdala.
The unique role of the ACC and its connections with the emotional components of the limbic system and the cognitive PFC is interesting due to the emotional and cognitive components of the placebo effect. The PFC also plays an important role in this network (Wager et al., 2004; Lui et al., 2010). Neuroimaging studies have also shown a negative correlation between the magnitude of placebo analgesia and the activation of the rACC, contralateral insula, primary somatosensory cortex (S1), and thalamus (Wager et al., 2004; Eippert et al., 2009).
Regarding expectations and their relation to the placebo effect, the manipulation of expectations modulates pain through endogenous opioidergic release (Case et al., 2021). In contrast, conditioned placebo responses to pain do not appear to be mediated by opioids (Amanzio and Benedetti, 1999). Interestingly, reappraisal-based manipulations based on mindfulness are postulated to reduce pain through non-opioid mechanisms (Zeidan et al., 2016; May et al., 2018; Wells et al., 2020).
Based on the abovementioned literature, we hypothesize that the efficacy of MBIs in pain may be affected by placebo effects and that the expectations of the participants may affect the outcome of these interventions. Therefore, it is important to systematically evaluate the literature to understand the mechanisms specific to mindfulness that are not activated by a placebo intervention. To this end, we conducted a systematic review to assess the evidence for the evaluation of placebo effects in MBIs for pain and to analyze if the expectations of the participants were considered in the studies and if the involvement of opioid mechanisms was examined.
The present research was conducted in accordance with the Cochrane recommendations on systematic reviews and adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Moher et al., 2009; Higgins et al., 2011). The review protocol was not preregistered in the International Prospective Register of Systematic Reviews (PROSPERO).
For this project, three different databases, namely Pubmed, Web of Science, and SCOPUS, were searched until May 2024. The search was performed between 1 November and 30 November 2022 and updated on 30 May 2024. For the present systematic review, the population, intervention, comparison, outcomes (PICO) question was: “What is the evidence for the evaluation of placebo effects of participants in MBI studies for pain?” No a priori distinctions were made between the types of MBI interventions or the duration of pain (acute or chronic).
The following MeSH terms were used in all the databases: “placebo,” AND “pain,” AND “mindfulness,” with no restrictions applied to the results. Initially, we included all articles that met our search criteria. All the articles were organized in a table specifying the name, author, and study design. Two authors (AL and IT) examined the titles and abstracts of the selected studies. Review articles were excluded, and all the original articles were considered eligible for further analysis.
The full text of these original articles was extracted, and after analysis by both authors, it was consensually agreed that an additional six articles should be discarded for not meeting the inclusion criteria (studies using MBIs for pain). In the end, we were left with a total of 19 articles. For each of these articles, both authors analyzed the population (the inclusion and exclusion criteria), experimental design, the type of pain studied, the type and duration of the MBIs, the characteristics of the instructors providing the interventions, the communication between the research team and participants, participant expectations (if they were considered), and the study of placebo and outcomes. The selection process followed the recent PRISMA guidelines (Page et al., 2021; Figure 1).
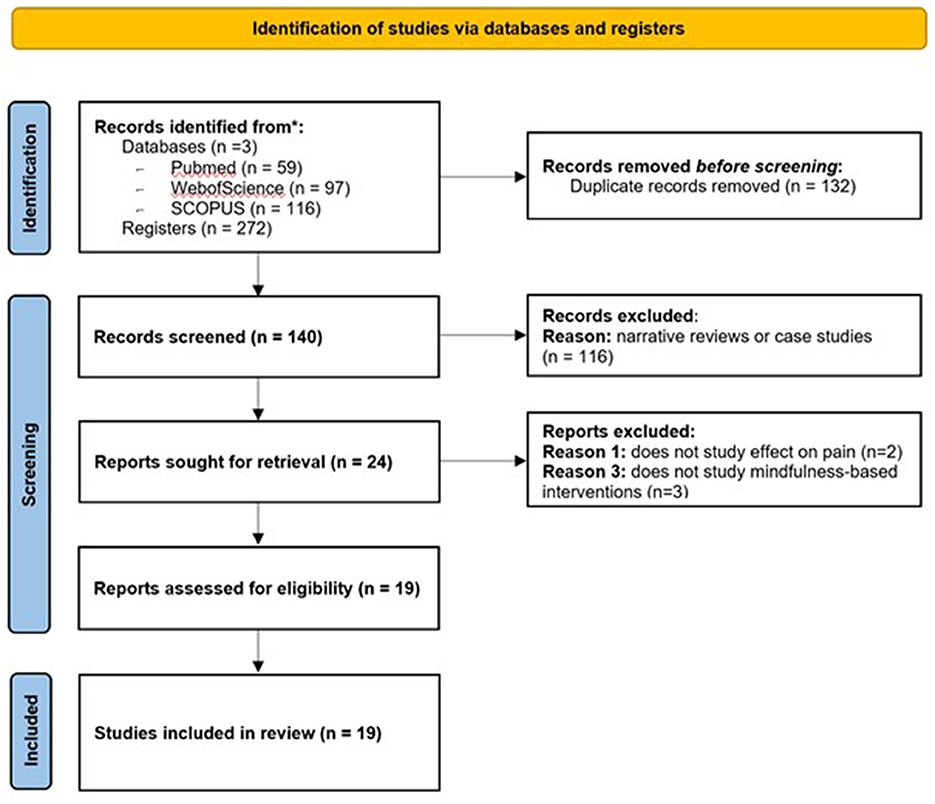
Figure 1. PRISMA 2020 flow diagram for new systematic reviews which included searches of databases and registers only. *Means registered databases.
To assess the risk of bias, both authors used the Cochrane Risk of Bias Tool for randomized controlled trials (Higgins et al., 2011) and the Newcastle-Ottawa Scale for non-randomized studies (Wells et al., 2021). The Cochrane Risk of Bias Tool for Randomized Controlled Trials evaluates six different criteria. An article was considered to have a low risk of bias if all criteria were met, a moderate risk of bias if one criterion was missing or two criteria were not followed, and a high risk of bias if two or more criteria were missing.
The Newcastle-Ottawa Scale evaluates eight different criteria, which are grouped into three categories: selection (a maximum of four stars), comparison (a maximum of two stars), and result/exposition (a maximum of three stars). For classifying the articles, an article was considered to have a low risk of bias if it had three or four stars in the selection category. It was considered to have a moderate risk of bias if it had two stars in the selection category, one or two stars in the comparison category, and two or three stars in the result/exposition category. An article was considered to have a high risk of bias if it had zero or one star in the selection category, zero stars in the comparison category, and zero or one star in the result/exposition category.
A total of 272 articles were collected from all databases, namely 59 from PubMed, 67 from Web of Science, and 116 from SCOPUS databases. After removing duplicates, we were left with 140 different results. After screening the titles and abstracts of these studies, only original articles were considered eligible, and all reviews were excluded, resulting in a total of 25 articles proceeding to the inclusion phase. Both authors analyzed the full text of these 25 studies and agreed to eliminate six additional articles for not meeting the inclusion criteria: two articles did not focus on the study of pain and three did not use an MBI. In the end, we were left with a total of 19 articles.
For each of these 19 articles, both authors analyzed the population of participants concerning the inclusion and exclusion criteria, specifically regarding their previous experience in meditation and mindfulness, as it could affect the answer to the main question of our study. We also extracted data regarding the experimental design, the type of pain studied, the type and duration of MBIs, the experience and possible conflicts of interest of the instructors guiding the MBIs, the communication between the research team and the participants, whether the expectations of the participants were considered, and the study of placebo effects. The main outcomes analyzed were the effects on pain, both in sensory intensity and unpleasantness (Table 1). Table 1 presents the results of the 19 analyzed studies concerning (1) the effects of MBIs on pain; (2) the involvement of endogenous opioids in the effects of MBIs on pain; and (3) participant expectations and analysis of placebo effects.
Regarding the effects of MBIs on pain, it should be noted that the studies evaluated mostly acute pain (i.e., experimentally induced pain), with 10 out of the 19 analyzed studies focusing on this type of pain. Among these studies, noxious heat was the predominant stimulus applied in seven studies, followed by cold (one study), ischemic stimulation (one study), and electric stimulation (one study). For chronic pain, several types of pain were analyzed, with a predominance of migraine/headache (three studies). Other types of chronic pain studied included musculoskeletal pain, such as arthritis (two studies), fibromyalgia (one study), low back pain (one study), diabetic neuropathy (one study), and diverse types of chronic pain (one study).
Information regarding the duration of chronic pain and the occurrence of pain co-morbidities, such as cognitive deficits and emotional imbalances, could not always be retrieved from the analyzed papers. A randomized controlled trial (Westenberg et al., 2018) studied the effect of a brief 60-s mindfulness video exercise on musculoskeletal pain in upper extremity patients and concluded that there were improvements in momentary pain, anxiety, depression, and anger. Three studies focused on the effect of mindfulness therapies on headaches. One of them was conducted in a population of adolescents using adaptations of MBSR and MBCT and revealed that the intervention resulted in reduced headache frequency and medication intake, disability, trait anxiety, symptoms of depression, and catastrophizing (Grazzi et al., 2021). The other two studies were conducted with adults and demonstrated that mindfulness reduced headache frequency, headache-related disability (Seminowicz et al., 2020), and decreased pain severity (Namjoo et al., 2019).
Mindfulness-based interventions have been proven to improve the quality of life in patients with painful diabetic neuropathy, with better results observed when combined with vitamin D supplementation (Davoudi et al., 2021). Additionally, they reduced pain in rheumatoid arthritis patients, with greater benefits observed in patients with recurrent depression (Zautra et al., 2008). However, when focusing on a population of fibromyalgia patients, the analyzed study (Schmidt et al., 2011) did not support the improvement of quality of life in patients receiving MBSR. Overall, regarding the net effects of MBIs, the results indicate the benefits of MBIs in acute and chronic pain.
Regarding the neurobiological mechanisms involved in MBIs' effects on pain, particularly concerning endogenous opioids, the majority of the results indicate that mindfulness meditation pain relief is not mediated by endogenous opioids (Zeidan et al., 2016; Esch et al., 2017; May et al., 2018; Wells et al., 2020). However, this finding was not supported by another study (Sharon et al., 2016), which concluded that the effects of mindfulness meditation on pain relief were mediated by endogenous opioids. Notably, the result of the latter study was based on a small population size (n = 14). The remaining studies did not analyze opioid involvement in MBIs for pain in detail. Collectively, the analyzed literature predominantly suggests that the effects of MBIs on pain are not mediated by endogenous opioids.
Finally, regarding participants' expectations and the analysis of the placebo effect, the analyzed literature presented a variety of results. Information about collecting participants' expectations concerning the pain relief they could receive from MBIs was sparse. Five studies clearly evaluated the expectations of the participants. The studies of the Davies group (Davies et al., 2021, 2022, 2023) analyzed in detail the initial expectations of the participants, including manipulating expectations to test the effects of the MBIs (Davies et al., 2022). One of the studies (Vencatachellum et al., 2021) hypothesized that mindfulness could reduce cue-induced hypoalgesia and hyperalgesia and found evidence supporting the role of mindfulness in the reduction of cue-induced hyperalgesia. Another study was a secondary analysis of a previous study (Zeidan et al., 2016; Case et al., 2021) and demonstrated that participant expectations about MBIs-induced effects on pain relief predicted pain reductions, with this correlation being higher during opioid antagonism (naloxone).
Some studies indicate that the placebo effect plays an important role in MBIs' pain relief and that expectancy is the strongest predictor of decreases in pain unpleasantness and intensity, as well as increases in pain tolerance (Davies et al., 2021, 2022). One study indicates that mindfulness meditation produces greater pain relief than a placebo intervention (Zeidan et al., 2015) while engaging different brain mechanisms. According to this study, mindfulness is associated with the activation of brain areas responsible for the cognitive modulation of pain, such as the ACC, bilateral anterior insula, and putamen nucleus, and the deactivation of nociceptive and sensory areas, including the thalamus and PAG. In contrast, the placebo effect is associated with greater activation in the bilateral dorsolateral PFC, PAG, thalamus, cerebellum, posterior cingulate cortex, and superior frontal gyrus. SHAM mindfulness activates brain areas that partially overlap with those activated and deactivated by mindfulness, producing greater activation in the thalamus, periaqueductal gray, bilateral dorsolateral prefrontal cortex, and cerebellum and a minor activation in the posterior cingulate cortex and right globus pallidus.
We also conducted a specific analysis of the control groups in the studies, considering acute (Table 2) and chronic (Table 3) pain separately, given the diversity of the analyzed outcomes. Two of the 19 studies were not included in the analysis because they did not have a control group (Grazzi et al., 2021; Vencatachellum et al., 2021) and were longitudinal evaluations of the interventions. As previously mentioned, the main aims of the studies varied, such as evaluating the opioid-mediated mechanisms of MBIs and/or the MBIs themselves. Therefore, the control groups were specifically designed, including saline infusion (e.g., Zeidan et al., 2016; Esch et al., 2017; May et al., 2018; Namjoo et al., 2019; Wells et al., 2020; Case et al., 2021; Khatib et al., 2024) or a specific placebo (Davoudi et al., 2021).
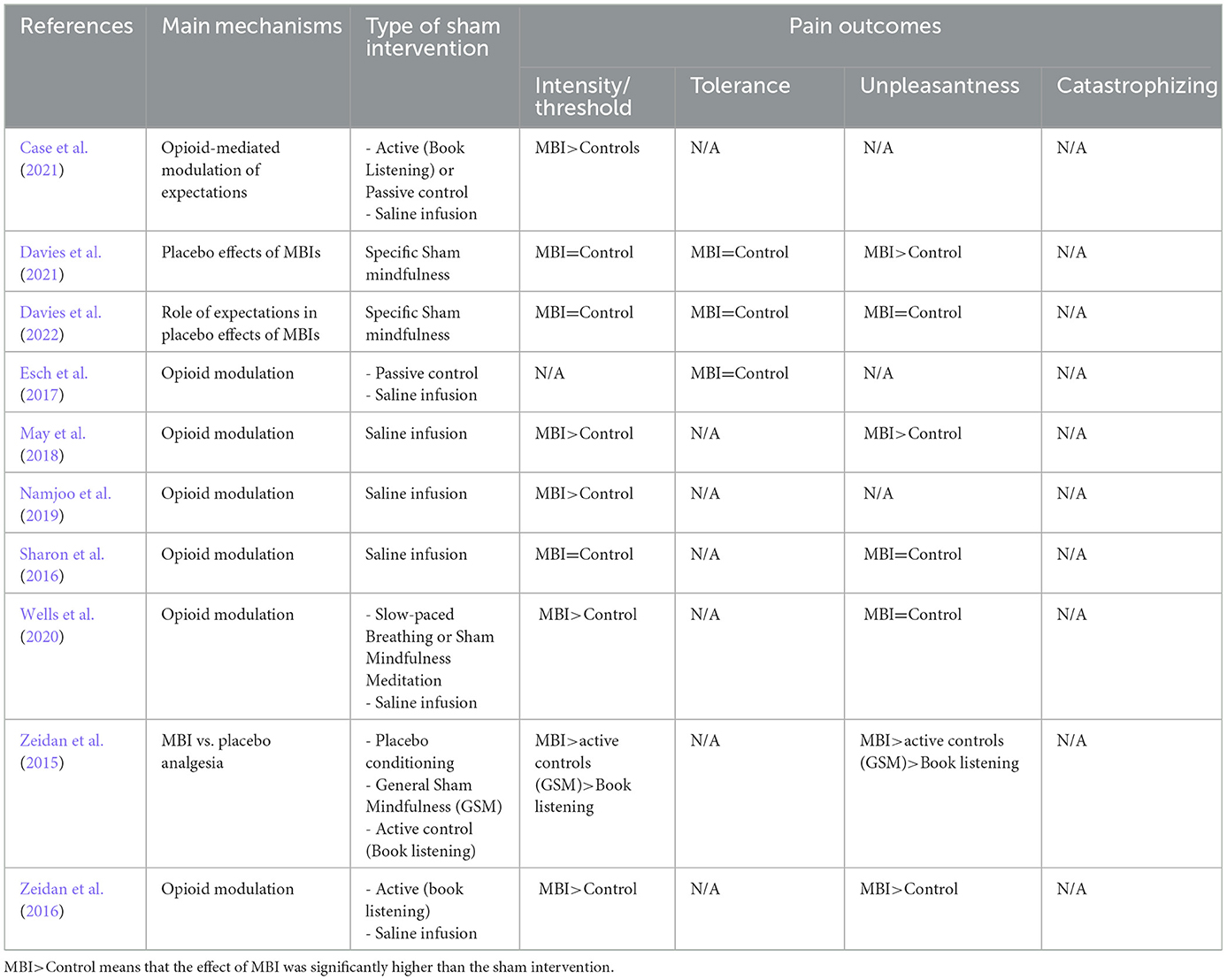
Table 2. Comparison of the effects of MBIs and sham (control) interventions in the acute pain studies, focusing on the main pain outcomes.
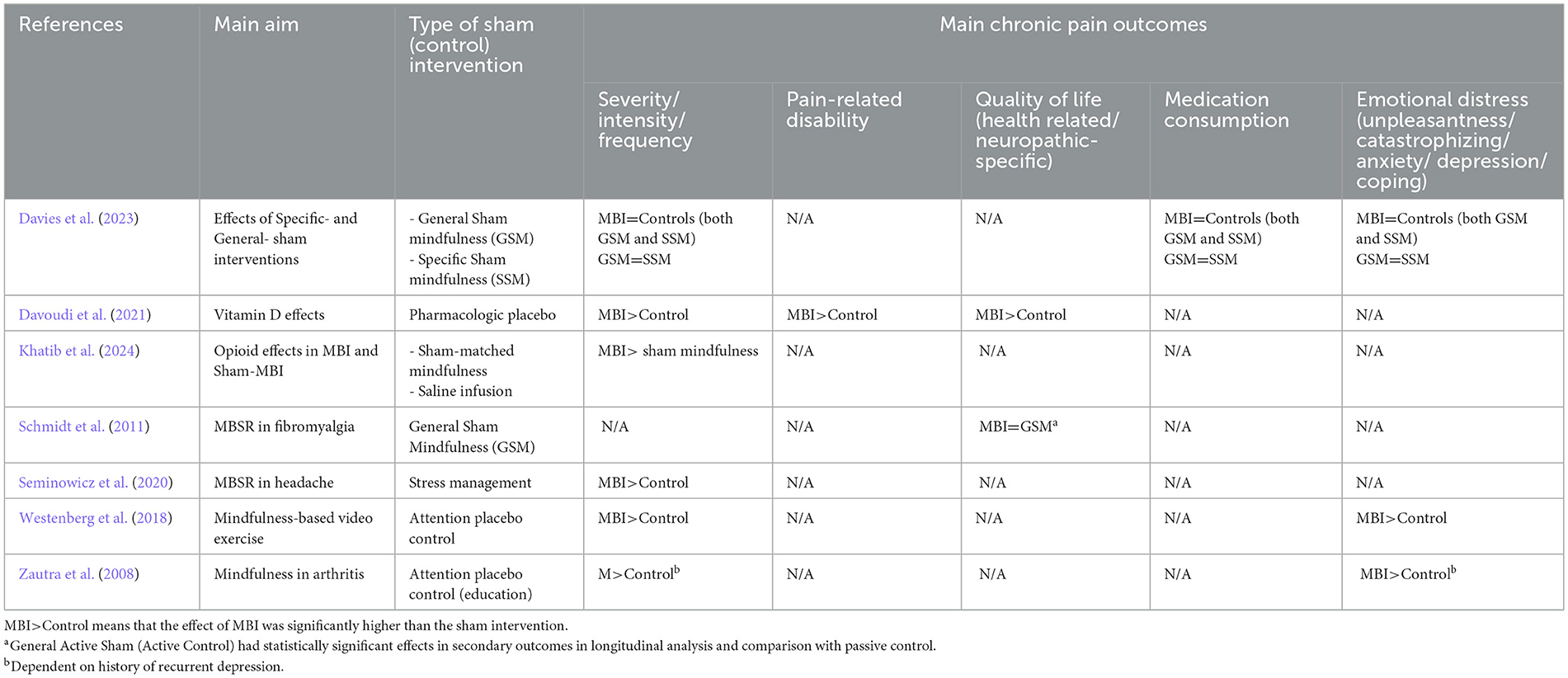
Table 3. Comparison of the effects of MBIs and sham (control) interventions in the chronic pain studies, focusing on the main pain outcomes.
Interestingly, the analysis of the control groups when the interventions were MBIs frequently included interventions such as passive controls, book listening, or educational programs (Zautra et al., 2008; Zeidan et al., 2016; Esch et al., 2017; Case et al., 2021). Controls more closely related to MBIs were also designed to equate the non-specific features of the MBI (general Sham mindfulness), stress management, or slow breathing techniques (Zeidan et al., 2015; Seminowicz et al., 2020; Wells et al., 2020; Davies et al., 2021, 2022, 2023; Khatib et al., 2024). A recent study included an experimental group specific to the MBI, in which all conditions matched the structural features of the MBI (e.g., attention to the intervention and instructions designed to give the meditator the sense that they were practicing a guided meditation) but lacked the instructions to provide attentional stability and meta-awareness (Davies et al., 2023).
The studies varied widely in terms of outcomes, covering sensory (intensity and threshold) and cognitive-emotional (e.g., catastrophizing, anxiety, and depression) aspects. Among the 11 studies that specifically controlled for the MBI (and not the pharmacologic intervention), MBIs had a similar effect to the control intervention in at least one of the analyzed parameters. These parameters included sensory aspects (Sharon et al., 2016; Davies et al., 2021, 2022, 2023; pain intensity), emotional components (pain unpleasantness; Davies et al., 2023), medical consumption (Davies et al., 2023), and multifactorial parameters (quality of life; Schmidt et al., 2011).
MBIs had a higher effect than the sham intervention in sensory parameters (Zautra et al., 2008; Zeidan et al., 2015; Westenberg et al., 2018; Seminowicz et al., 2020; Wells et al., 2020; Case et al., 2021; Khatib et al., 2024; pain intensity) and several cognitive/emotional aspects of pain (Zautra et al., 2008; Zeidan et al., 2015; Westenberg et al., 2018; Davies et al., 2021). In none of the analyzed studies did sham interventions have a higher effect than MBIs.
To assess the quality of the studies included in this review, the Cochrane Risk of Bias Tool for Randomized Controlled Trials was used (Higgins et al., 2011), as well as the Newcastle-Ottawa Scale for non-randomized studies (Tables 4, 5). Most of the studies reviewed have a moderate risk of bias, and therefore, the sample of articles analyzed may be considered of good quality.
To the best of our knowledge, this is the first systematic review evaluating the possible effects of expectations and the placebo effect on the outcomes of MBIs for pain management. Systematic reviews support the efficacy of MBIs in pain management, suggesting that these cognitive-behavioral therapies could be useful (Hilton et al., 2017; Mcclintock et al., 2019; Pardos-Gascon et al., 2021). However, these studies highlight the need for further research due to the variability in the effects observed. This need is also supported by the present systematic review since all analyzed studies showed an effect of MBIs on pain management. Notably, the studies often evaluated the effects of MBIs on both the sensory and emotional dimensions of pain by measuring pain intensity and pain unpleasantness, which is commendable given the multidimensional nature of pain (Price, 2000; Raja et al., 2020).
Further research is needed to understand the mechanisms of MBIs in pain, considering the established effects of expectations and placebo on pain and their neurobiological mechanisms (Zunhammer et al., 2021; Benedetti et al., 2022). In this study, we attempted to systematically evaluate whether participant expectations of MBIs for pain were evaluated and whether the potential for MBI-derived placebo effects was considered. Previous systematic reviews and meta-analyses have suggested that the mechanisms of action should be studied (Hilton et al., 2017; Mcclintock et al., 2019; Pardos-Gascon et al., 2021). Given the knowledge of placebo-induced analgesia, we hypothesized that MBI-induced placebo effects could have an effect.
Despite the growing body of research on MBIs, the “next generation of mindfulness-based intervention research” (Rosenkranz et al., 2019) emphasizes the need for better experimental designs to investigate the underlying mechanisms of MBIs' beneficial effects. In general, studies on MBIs, not only for pain, should prioritize longitudinal evaluations and active controls, as well as account for the instructors' experience and the participants' expectations (Caspi and Burleson, 2007; Davidson and Kaszniak, 2015; Van Dam et al., 2018). Additional research using matched sham interventions is necessary in this field.
In a recent review of MBIs' effects on fibromyalgia, we identified several study limitations (Leca and Tavares, 2022), confirming that experimental design concerns also apply to pain studies. Further studies with adequate experimental designs are needed to better evaluate the effects of MBIs, particularly regarding the instructors' experience. In the present study, we found similar constraints in the 19 analyzed studies, particularly regarding the instructors' experience. A total of eight of the 15 analyzed studies did not report the experience of the instructors. It was shown that the experience of the instructors and their time of practice may influence the outcomes of some MBIs (Davidson and Kaszniak, 2015; Van Dam et al., 2018).
Attempts to contact authors for missing information were unsuccessful. Two studies (Zeidan et al., 2015; Sharon et al., 2016) did not have instructors, as their aims differed from the others, reducing the number of relevant studies to 15 instead of 17 studies.
Other studies only mentioned that the instructors were psychologists with expertise in mindfulness practices (Wells et al., 2020; Davoudi et al., 2021), which is also vague information.
Some studies referred to both the extent of the instructors' experience and the type of practice (Schmidt et al., 2011; Namjoo et al., 2019). One additional constraint in the analyzed studies is the lack of reporting and/or evaluation of participants' previous experience with mindfulness or meditation in six of the analyzed studies (Zautra et al., 2008; Schmidt et al., 2011; Namjoo et al., 2019; Case et al., 2021; Davoudi et al., 2021; Vencatachellum et al., 2021). This is a challenging issue since participants' prior experience with mindfulness or meditation may prompt them to recognize if they are receiving a sham intervention. Consequently, these participants may not experience the same placebo effect as those who believe they are receiving active treatment. This bias could be mitigated by selecting participants who are completely naive to mindfulness. Addressing these issues in future research would be an important step in better understanding the factors that influence MBIs' effects on pain. Among the 19 analyzed studies, 10 used acute stimuli, while the remaining studies evaluated various chronic pain conditions such as recurrent headaches/migraines, diabetic neuropathy, and musculoskeletal/articular pain. However, acute and chronic pain may differ in terms of the mechanisms of mindfulness. Due to neuroplastic changes in the nervous system from acute to chronic pain and the specificities of chronic pain types, caution is needed when translating MBIs for pain management in both acute and chronic pain.
There are still very few articles focusing on the role of expectations in MBIs' pain relief. There is a considerable gap in the field of pain research, given that the role of expectations in MBIs for other conditions has been demonstrated. The label “mindfulness” in a study has been shown to drive expectancy (Ghanbari Noshari et al., 2023), potentially leading to the placebo effect. Since pain has a cognitive dimension and lacks objective biomarkers, MBIs primarily rely on self-reported experiences. Therefore, understanding patients' expectations and the information they received about the intervention is crucial. However, our analysis revealed that most studies did not clearly specify the type of information provided to participants.
The information in the three studies that analyzed the effects of MBIs on pain responses was clear. Two of these studies concluded that the placebo effect plays a role in pain responses during MBIs, with expectancy being the strongest predictor of decreases in pain unpleasantness and intensity and increases in pain tolerance (Davies et al., 2021, 2022). In one study, investigators created a cover story, informing the participants that they would be allocated to one of two groups (mindfulness or no treatment), while they were allocated to one of three groups (mindfulness, sham mindfulness, or placebo; Davies et al., 2021).
In another study, participants were informed that the aim of the study was to test a newly developed MBI that integrated highly effective elements of existing MBIs for pain and was expected to greatly reduce pain. A similar cover story was used, but participants were allocated to one of three groups (mindfulness, sham mindfulness, or no treatment), while they were, in fact, allocated to one of five groups (MM+: told they were receiving mindfulness and actually received mindfulness; MM-: told they were receiving sham but actually received mindfulness; SHAM+: told they were receiving mindfulness but actually received sham; SHAM-: told they were receiving sham and actually received sham; and no treatment control). This design demonstrated the effects of patients' expectation on MBI results for pain and the occurrence of a placebo effect (Davies et al., 2022).
For a placebo effect to be accurately measured and controlled for, the sham intervention must fulfill two roles. First, it must match in credibility (i.e., from a participant's or patient's perspective, it must be indistinguishable from actual mindfulness), as evidenced by equivalent scores on credibility or manipulation checks. Second, the sham intervention must elicit expectations of benefit equal to those receiving mindfulness, as evidenced by equivalent expectancy ratings post-exposure or by pre-exposure and post-exposure changes in expectancy ratings across both groups. In this regard, defining sham-mindfulness interventions or even sham-mindfulness interventions with specific MBI features is crucial (Davies et al., 2023) and may provide new insights into the specific mechanisms of MBIs.
Two studies focused on the effect of expectation on MBIs' pain relief. One of them hypothesized that mindfulness could reduce cue-induced hypoalgesia and hyperalgesia and found evidence to support the role of mindfulness in reducing cue-induced hyperalgesia (Vencatachellum et al., 2021). The other study was a secondary analysis of a previous study (Zeidan et al., 2016) and demonstrated that the expectations of the participants about MBI-induced pain relief predicted pain reductions, with the correlation being higher during opioid antagonism (naloxone). Collectively, the results of studies that properly control MBIs for factors such as expectations show that these expectations should be considered. The studies by the Davies group (Davies et al., 2022, 2023) provide a solid ground for collecting and numerically measuring participant expectations to manipulate them and evaluate the placebo effect.
It should be noted that only a few studies have properly measured and manipulated pain expectancies. Therefore, the intentions of the participants in MBIs and their expectations regarding pain improvement should be evaluated using appropriate questionnaires before and after the interventions.
One study investigated the neurobiological mechanisms underlying MBIs' pain relief and whether they were similar to those mediating the placebo effect (Zeidan et al., 2015). This study concluded that MBIs produce greater pain relief than a placebo intervention while engaging different brain mechanisms. The differences in the magnitude of the effects and the underlying brain structures indicate that the MBIs' effects on pain relief are not entirely mediated by placebo, although placebo plays a role. However, the limited number of studies, along with some of the abovementioned pitfalls in the experimental design, prevents solid conclusions to be drawn about the influence of expectations on “MBIs-induced” pain relief. Further studies are necessary to allow additional systematic reviews and meta-analyses on this fascinating issue in neuroscience, psychology, and medicine.
Overall, this systematic review indicates that certain aspects of MBIs for pain management need to be considered before this type of cognitive-behavioral intervention is widely adopted for pain management. For example, it is important to determine the expectations of the participants in the interventions, as these may be manipulated to maximize placebo effects and better establish the mechanisms behind the beneficial effects of MBIs. The importance of including adequate sham controls should be highlighted in the experimental design of MBIs for pain management. Regarding the neurobiological mechanisms underlying the effects of MBIs on pain management, such as opioid involvement, future neuroimaging studies may be important. Due to the neuroplastic changes induced by chronic pain and its impact on human suffering, it is crucial to continue studying chronic pain rather than focusing predominantly on acute pain. Evaluating the long-term impact of MBIs and assessing the durability of treatment effects is also essential, particularly for chronic pain conditions.
This study presents some limitations. The small number of studies that actually evaluated the effects of expectations was much smaller than the 19 analyzed studies, which impairs the ability to conduct a meta-analysis. Nevertheless, the large majority of the studies were of good quality, as demonstrated by the risk of bias assessment. Another limitation was the inability to consistently retrieve data regarding the population, such as age and gender, which considerably affect pain responses and responses to psychological interventions such as MBIs.
It is important for researchers in MBIs for pain to openly discuss the limitations and constraints of the current available interventions to evaluate the mechanisms of the placebo effect in MBIs for pain. Replicating studies that show that the placebo effect plays a role in MBIs for pain (e.g., Zeidan et al., 2016; Davies et al., 2022) would be important. There is a clear need for better development, validation, and reporting of the sham interventions used in MBIs. Longitudinal studies of novice and expert meditators are necessary to evaluate how specific (mindfulness) and non-specific (placebo) effects change over time with more training and expertise.
Currently, there is a significant scope in MBIs for pain to develop useful and specific placebo interventions, as the concept of a “universal placebo” does not exist in MBIs. The present systematic review also highlights the need to continue analyzing the neurobiological basis of MBI to gain a better understanding of the pain modulatory mechanisms, other than opioids, that may support controlled therapeutic interventions of MBIs in pain management.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
AL: Conceptualization, Investigation, Validation, Visualization, Writing – original draft, Writing – review & editing, Data curation, Formal analysis, Methodology, Software. RS: Supervision, Validation, Writing – review & editing. IT: Conceptualization, Investigation, Validation, Visualization, Writing – original draft, Writing – review & editing, Funding acquisition, Resources, Supervision.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was performed within the aims of Cátedra de Medicina da Dor (Fundação Grunenthal, Portugal).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Amanzio, M., and Benedetti, F. (1999). Neuropharmacological dissection of placebo analgesia: expectation-activated opioid systems versus conditioning-activated specific subsystems. J. Neurosci. 19, 484–494. doi: 10.1523/JNEUROSCI.19-01-00484.1999
Auvray, M., Myin, E., and Spence, C. (2010). The sensory-discriminative and affective-motivational aspects of pain. Neurosci. Biobehav. Rev. 34, 214–223. doi: 10.1016/j.neubiorev.2008.07.008
Baminiwatta, A., and Solangaarachchi, I. (2021). Trends and developments in mindfulness research over 55 years: a bibliometric analysis of publications indexed in web of science. Mindfulness 12, 2099–2116. doi: 10.1007/s12671-021-01681-x
Benedetti, F., Shaibani, A., Arduino, C., and Thoen, W. (2022). Open-label nondeceptive placebo analgesia is blocked by the opioid antagonist naloxone. Pain 2022:2791. doi: 10.1097/j.pain.0000000000002791
Bingel, U. (2020). Placebo 2.0: the impact of expectations on analgesic treatment outcome. Pain 161, S48–S56. doi: 10.1097/j.pain.0000000000001981
Bingel, U., Wanigasekera, V., Wiech, K., Ni Mhuircheartaigh, R., Lee, M. C., Ploner, M., et al. (2011). The effect of treatment expectation on drug efficacy: imaging the analgesic benefit of the opioid remifentanil. Sci. Transl. Med. 3:70ra14. doi: 10.1126/scitranslmed.3001244
Brandel, M. G., Lin, C., Hennel, D., Khazen, O., Pilitsis, J. G., and Ben-Haim, S. (2022). Mindfulness meditation in the treatment of chronic pain. Neurosurg. Clin. N. Am. 33, 275–279. doi: 10.1016/j.nec.2022.02.005
Cardle, P., Kumar, S., Leach, M., Mcevoy, M., and Veziari, Y. (2023). Mindfulness and chronic musculoskeletal pain: an umbrella review. J. Multidiscip. Healthc. 16, 515–533. doi: 10.2147/JMDH.S392375
Case, L., Adler-Neal, A. L., Wells, R. E., and Zeidan, F. (2021). The role of expectations and endogenous opioids in mindfulness-based relief of experimentally induced acute pain. Psychosom. Med. 83, 549–556. doi: 10.1097/PSY.0000000000000908
Caspi, O., and Burleson, K. O. (2007). Methodological challenges in meditation research. Adv. Mind Body Med. 22, 36–43.
Chen, T., Taniguchi, W., Chen, Q. Y., Tozaki-Saitoh, H., Song, Q., Liu, R. H., et al. (2018). Top-down descending facilitation of spinal sensory excitatory transmission from the anterior cingulate cortex. Nat. Commun. 9:1886. doi: 10.1038/s41467-018-04309-2
Cohen, S. P., Vase, L., and Hooten, W. M. (2021). Chronic pain: an update on burden, best practices, and new advances. Lancet 397, 2082–2097. doi: 10.1016/S0140-6736(21)00393-7
Coleshill, M. J., Sharpe, L., Colloca, L., Zachariae, R., and Colagiuri, B. (2018). Placebo and active treatment additivity in placebo analgesia: research to date and future directions. Int. Rev. Neurobiol. 139, 407–441. doi: 10.1016/bs.irn.2018.07.021
Davidson, R. J., and Kaszniak, A. W. (2015). Conceptual and methodological issues in research on mindfulness and meditation. Am. Psychol. 70, 581–592. doi: 10.1037/a0039512
Davies, J. N., Colagiuri, B., Sharpe, L., and Day, M. A. (2023). Placebo effects contribute to brief online mindfulness interventions for chronic pain: results from an online randomized sham-controlled trial. Pain. 164, 2273–2284. doi: 10.1097/j.pain.0000000000002928
Davies, J. N., Sharpe, L., Day, M. A., and Colagiuri, B. (2021). Mindfulness-based analgesia or placebo effect? The development and evaluation of a sham mindfulness intervention for acute experimental pain. Psychosom. Med. 83, 557–565. doi: 10.1097/PSY.0000000000000886
Davies, J. N., Sharpe, L., Day, M. A., and Colagiuri, B. (2022). How do placebo effects contribute to mindfulness-based analgesia? Probing acute pain effects and interactions using a randomized balanced placebo design. Pain 163, 1967–1977. doi: 10.1097/j.pain.0000000000002593
Davoudi, M., Allame, Z., Niya, R. T., Taheri, A. A., and Ahmadi, S. M. (2021). The synergistic effect of vitamin D supplement and mindfulness training on pain severity, pain-related disability and neuropathy-specific quality of life dimensions in painful diabetic neuropathy: a randomized clinical trial with placebo-controlled. J. Diabet. Metab. Disord. 20, 49–58. doi: 10.1007/s40200-020-00700-3
Eippert, F., Bingel, U., Schoell, E. D., Yacubian, J., Klinger, R., Lorenz, J., et al. (2009). Activation of the opioidergic descending pain control system underlies placebo analgesia. Neuron 63, 533–543. doi: 10.1016/j.neuron.2009.07.014
Enck, P., Bingel, U., Schedlowski, M., and Rief, W. (2013). The placebo response in medicine: minimize, maximize or personalize? Nat. Rev. Drug Discov. 12, 191–204. doi: 10.1038/nrd3923
Esch, T., Winkler, J., Auwarter, V., Gnann, H., Huber, R., and Schmidt, S. (2017). Neurobiological aspects of mindfulness in pain autoregulation: unexpected results from a randomized-controlled trial and possible implications for meditation research. Front. Hum. Neurosci. 10:674. doi: 10.3389/fnhum.2016.00674
Gatchel, R. J., Mcgeary, D. D., Mcgeary, C. A., and Lippe, B. (2014). Interdisciplinary chronic pain management: past, present, and future. Am. Psychol. 69, 119–130. doi: 10.1037/a0035514
Ghanbari Noshari, M., Kempton, H. M., and Kreplin, A. (2023). Mindfulness or expectancy? The label of mindfulness leads to expectancy effects. Counsel. Psychother. Res. 23, 49–63. doi: 10.1002/capr.12589
Goldberg, S. B., Tucker, R. P., Greene, P. A., Davidson, R. J., Wampold, B. E., Kearney, D. J., et al. (2018). Mindfulness-based interventions for psychiatric disorders: a systematic review and meta-analysis. Clin. Psychol. Rev. 59, 52–60. doi: 10.1016/j.cpr.2017.10.011
Grazzi, L., Grignani, E., Raggi, A., Rizzoli, P., and Guastafierro, E. (2021). Effect of a mindfulness-based intervention for chronic migraine and high frequency episodic migraine in adolescents: a pilot single-arm open-label study. Int. J. Environ. Res. Publ. Health 18:2211739. doi: 10.3390/ijerph182211739
Hall, J. K., and Boswell, M. V. (2009). Ethics, law, and pain management as a patient right. Pain Physician 12, 499–506. doi: 10.36076/ppj.2009/12/499
Heinricher, M. M., Tavares, I., Leith, J. L., and Lumb, B. M. (2009). Descending control of nociception: specificity, recruitment and plasticity. Brain Res. Rev. 60, 214–225. doi: 10.1016/j.brainresrev.2008.12.009
Higgins, J. P., Altman, D. G., Gotzsche, P. C., Juni, P., Moher, D., Oxman, A. D., et al. (2011). The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. Br Med J. 343:d5928. doi: 10.1136/bmj.d5928
Hilton, L., Hempel, S., Ewing, B. A., Apaydin, E., Xenakis, L., Newberry, S., et al. (2017). Mindfulness meditation for chronic pain: systematic review and meta-analysis. Ann. Behav. Med. 51, 199–213. doi: 10.1007/s12160-016-9844-2
Hohenschurz-Schmidt, D., Draper-Rodi, J., Vase, L., Scott, W., Mcgregor, A., Soliman, N., et al. (2023a). Blinding and sham control methods in trials of physical, psychological, and self-management interventions for pain (article I): a systematic review and description of methods. Pain 164, 469–484. doi: 10.1097/j.pain.0000000000002723
Hohenschurz-Schmidt, D., Draper-Rodi, J., Vase, L., Scott, W., Mcgregor, A., Soliman, N., et al. (2023b). Blinding and sham control methods in trials of physical, psychological, and self-management interventions for pain (article II): a meta-analysis relating methods to trial results. Pain 164, 509–533. doi: 10.1097/j.pain.0000000000002730
Jinich-Diamant, A., Garland, E., Baumgartner, J., Gonzalez, N., Riegner, G., Birenbaum, J., et al. (2020). Neurophysiological mechanisms supporting mindfulness meditation-based pain relief: an updated review. Curr. Pain Headache Rep. 24:56. doi: 10.1007/s11916-020-00890-8
Kabat-Zinn, J. (1982). An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: theoretical considerations and preliminary results. Gen. Hosp. Psychiatry 4, 33–47. doi: 10.1016/0163-8343(82)90026-3
Khatib, L., Dean, J. G., Oliva, V., Riegner, G., Gonzalez, N. E., Birenbaum, J., et al. (2024). The role of endogenous opioids in mindfulness and sham mindfulness-meditation for the direct alleviation of evoked chronic low back pain: a randomized clinical trial. Neuropsychopharmacol. 49, 1069–1077. doi: 10.1038/s41386-023-01766-2
Knopp-Sihota, J. A., Macgregor, T., Reeves, J. T. H., Kennedy, M., and Saleem, A. (2022). Management of chronic pain in long-term care: a systematic review and meta-analysis. J. Am. Med. Dir. Assoc. 23, 1507–1516.e0. doi: 10.1016/j.jamda.2022.04.008
Leca, S., and Tavares, I. (2022). Research in mindfulness interventions for patients with fibromyalgia: a critical review. Front. Integr. Neurosci. 16:920271. doi: 10.3389/fnint.2022.920271
Ludwig, D. S., and Kabat-Zinn, J. (2008). Mindfulness in medicine. J. Am. Med. Assoc. 300, 1350–1352. doi: 10.1001/jama.300.11.1350
Lui, F., Colloca, L., Duzzi, D., Anchisi, D., Benedetti, F., and Porro, C. A. (2010). Neural bases of conditioned placebo analgesia. Pain 151, 816–824. doi: 10.1016/j.pain.2010.09.021
Martins, I., and Tavares, I. (2017). Reticular formation and pain: the past and the future. Front. Neuroanat. 11:51. doi: 10.3389/fnana.2017.00051
May, L. M., Kosek, P., Zeidan, F., and Berkman, E. T. (2018). Enhancement of meditation analgesia by opioid antagonist in experienced meditators. Psychosom. Med. 80, 807–813. doi: 10.1097/PSY.0000000000000580
Mcclintock, A. S., Mccarrick, S. M., Garland, E. L., Zeidan, F., and Zgierska, A. E. (2019). Brief mindfulness-based interventions for acute and chronic pain: a systematic review. J. Altern. Complement. Med. 25, 265–278. doi: 10.1089/acm.2018.0351
Meissner, K., and Linde, K. (2018). Are blue pills better than green? How treatment features modulate placebo effects. Int. Rev. Neurobiol. 139, 357–378. doi: 10.1016/bs.irn.2018.07.014
Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G., and Group, P. (2009). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 6:e1000097. doi: 10.1371/journal.pmed.1000097
Moisset, X., Bouhassira, D., Avez Couturier, J., Alchaar, H., Conradi, S., Delmotte, M. H., et al. (2020). Pharmacological and non-pharmacological treatments for neuropathic pain: systematic review and French recommendations. Rev. Neurol. 176, 325–352. doi: 10.1016/j.neurol.2020.01.361
Namjoo, S., Borjali, A., Seirafi, M., and Assarzadegan, F. (2019). Use of mindfulness-based cognitive therapy to change pain-related cognitive processing in patients with primary headache: a randomized trial with attention placebo control group. Anesth. Pain Med. 9:e91927. doi: 10.5812/aapm.91927
Ng, S. K., Urquhart, D. M., Fitzgerald, P. B., Cicuttini, F. M., Hussain, S. M., and Fitzgibbon, B. M. (2018). the relationship between structural and functional brain changes and altered emotion and cognition in chronic low back pain brain changes: a systematic review of MRI and fMRI studies. Clin. J. Pain 34, 237–261. doi: 10.1097/AJP.0000000000000534
Page, M. J., Mckenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., et al. (2021). The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Br Med. J. 372:n71. doi: 10.1136/bmj.n71
Pardos-Gascon, E. M., Narambuena, L., Leal-Costa, C., and Van-Der Hofstadt-Roman, C. J. (2021). Differential efficacy between cognitive-behavioral therapy and mindfulness-based therapies for chronic pain: systematic review. Int. J. Clin. Health Psychol. 21:100197. doi: 10.1016/j.ijchp.2020.08.001
Petrovic, P., Kalso, E., Petersson, K. M., and Ingvar, M. (2002). Placebo and opioid analgesia– imaging a shared neuronal network. Science 295, 1737–1740. doi: 10.1126/science.1067176
Pollo, A., and Benedetti, F. (2009). The placebo response: neurobiological and clinical issues of neurological relevance. Prog. Brain Res. 175, 283–294. doi: 10.1016/S0079-6123(09)17520-9
Price, D. D. (2000). Psychological and neural mechanisms of the affective dimension of pain. Science 288, 1769–1772. doi: 10.1126/science.288.5472.1769
Raja, S. N., Carr, D. B., Cohen, M., Finnerup, N. B., Flor, H., Gibson, S., et al. (2020). The revised International Association for the Study of Pain definition of pain: concepts, challenges, and compromises. Pain 161, 1976–1982. doi: 10.1097/j.pain.0000000000001939
Reeves, K., and Jones, N. (2022). Ethical challenges in chronic pain. Prim. Care 49, 497–506. doi: 10.1016/j.pop.2022.01.002
Rosenkranz, M. A., Dunne, J. D., and Davidson, R. J. (2019). The next generation of mindfulness-based intervention research: what have we learned and where are we headed? Curr. Opin. Psychol. 28, 179–183. doi: 10.1016/j.copsyc.2018.12.022
Rossettini, G., Camerone, E. M., Carlino, E., Benedetti, F., and Testa, M. (2020). Context matters: the psychoneurobiological determinants of placebo, nocebo and context-related effects in physiotherapy. Arch. Physiother. 10:11. doi: 10.1186/s40945-020-00082-y
Schedlowski, M., Enck, P., Rief, W., and Bingel, U. (2015). Neuro-bio-behavioral mechanisms of placebo and nocebo responses: implications for clinical trials and clinical practice. Pharmacol. Rev. 67, 697–730. doi: 10.1124/pr.114.009423
Schmidt, H., and Pilat, C. (2023). Effects of meditation on pain intensity, physical function, quality of life and depression in adults with low back pain—a systematic review with meta-analysis. Complement. Ther. Med. 72:102924. doi: 10.1016/j.ctim.2023.102924
Schmidt, S., Grossman, P., Schwarzer, B., Jena, S., Naumann, J., and Walach, H. (2011). Treating fibromyalgia with mindfulness-based stress reduction: results from a 3-armed randomized controlled trial. Pain 152, 361–369. doi: 10.1016/j.pain.2010.10.043
Scott, D. J., Stohler, C. S., Egnatuk, C. M., Wang, H., Koeppe, R. A., and Zubieta, J. K. (2008). Placebo and nocebo effects are defined by opposite opioid and dopaminergic responses. Arch. Gen. Psychiat. 65, 220–231. doi: 10.1001/archgenpsychiatry.2007.34
Seminowicz, D. A., Burrowes, S. A. B., Kearson, A., Zhang, J., Krimmel, S. R., Samawi, L., et al. (2020). Enhanced mindfulness-based stress reduction in episodic migraine: a randomized clinical trial with magnetic resonance imaging outcomes. Pain 161, 1837–1846. doi: 10.1097/j.pain.0000000000001860
Sharon, H., Maron-Katz, A., Ben Simon, E., Flusser, Y., Hendler, T., Tarrasch, R., et al. (2016). Mindfulness meditation modulates pain through endogenous opioids. Am. J. Med. 129, 755–758. doi: 10.1016/j.amjmed.2016.03.002
Shires, A., Sharpe, L., Davies, J. N., and Newton-John, T. R. O. (2020). The efficacy of mindfulness-based interventions in acute pain: a systematic review and meta-analysis. Pain 161, 1698–1707. doi: 10.1097/j.pain.0000000000001877
Swenson, C. J. (2002). Ethical issues in pain management. Semin. Oncol. Nurs. 18, 135–142. doi: 10.1053/sonu.2002.32511
Tracey, I., and Mantyh, P. W. (2007). The cerebral signature for pain perception and its modulation. Neuron 55, 377–391. doi: 10.1016/j.neuron.2007.07.012
Turk, D. C. (2002). Clinical effectiveness and cost-effectiveness of treatments for patients with chronic pain. Clin. J. Pain 18, 355–365. doi: 10.1097/00002508-200211000-00003
Van Dam, N. T., Van Vugt, M. K., Vago, D. R., Schmalzl, L., Saron, C. D., Olendzki, A., et al. (2018). Mind the hype: a critical evaluation and prescriptive agenda for research on mindfulness and meditation. Perspect. Psychol. Sci. 13, 36–61. doi: 10.1177/1745691617709589
Van Lennep, J., Trossel, F., Perez, R., Otten, R. H. J., Van Middendorp, H., Evers, A. W. M., et al. (2021). Placebo effects in low back pain: a systematic review and meta-analysis of the literature. Eur. J. Pain 25, 1876–1897. doi: 10.1002/ejp.1811
Vencatachellum, S., Van Der Meulen, M., Van Ryckeghem, D. M. L., Van Damme, S., and Vogele, C. (2021). Brief mindfulness training can mitigate the influence of prior expectations on pain perception. Eur. J. Pain 25, 2007–2019. doi: 10.1002/ejp.1817
Wager, T. D., Rilling, J. K., Smith, E. E., Sokolik, A., Casey, K. L., Davidson, R. J., et al. (2004). Placebo-induced changes in FMRI in the anticipation and experience of pain. Science 303, 1162–1167. doi: 10.1126/science.1093065
Wells, G. A., Shea, B., O'Connell, D., Peterson, J., Welch, V., Losos, M., et al. (2021). The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-analyses. Available at: https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed January 23, 2023).
Wells, R. E., Collier, J., Posey, G., Morgan, A., Auman, T., Strittmatter, B., et al. (2020). Attention to breath sensations does not engage endogenous opioids to reduce pain. Pain 161, 1884–1893. doi: 10.1097/j.pain.0000000000001865
Westenberg, R. F., Zale, E. L., Heinhuis, T. J., Ozkan, S., Nazzal, A., Lee, S. G., et al. (2018). Does a brief mindfulness exercise improve outcomes in upper extremity patients? A randomized controlled trial. Clin. Orthop. Relat. Res. 476, 790–798. doi: 10.1007/s11999.0000000000000086
Yang, J., Lo, W. L. A., Zheng, F., Cheng, X., Yu, Q., and Wang, C. (2022). Evaluation of cognitive behavioral therapy on improving pain, fear avoidance, and self-efficacy in patients with chronic low back pain: a systematic review and meta-analysis. Pain Res. Manag. 2022:4276175. doi: 10.1155/2022/4276175
Zautra, A. J., Davis, M. C., Reich, J. W., Nicassario, P., Tennen, H., Finan, P., et al. (2008). Comparison of cognitive behavioral and mindfulness meditation interventions on adaptation to rheumatoid arthritis for patients with and without history of recurrent depression. J. Consult. Clin. Psychol. 76, 408–421. doi: 10.1037/0022-006X.76.3.408
Zeidan, F., Adler-Neal, A. L., Wells, R. E., Stagnaro, E., May, L. M., Eisenach, J. C., et al. (2016). Mindfulness-meditation-based pain relief is not mediated by endogenous opioids. J. Neurosci. 36, 3391–3397. doi: 10.1523/JNEUROSCI.4328-15.2016
Zeidan, F., Emerson, N. M., Farris, S. R., Ray, J. N., Jung, Y., Mchaffie, J. G., et al. (2015). Mindfulness meditation-based pain relief employs different neural mechanisms than placebo and sham mindfulness meditation-induced analgesia. J. Neurosci. 35, 15307–15325. doi: 10.1523/JNEUROSCI.2542-15.2015
Zeidan, F., and Vago, D. R. (2016). Mindfulness meditation-based pain relief: a mechanistic account. Ann. N. Y. Acad. Sci. 1373, 114–127. doi: 10.1111/nyas.13153
Keywords: expectations, cognitive-behavioral therapy, pain measurements, placebo effects, mindfulness-based stress reduction (MBSR), mindfulness-based cognitive therapy (MBCT), meditation therapy
Citation: Lopes A, Sampaio R and Tavares I (2024) Pain, mindfulness, and placebo: a systematic review. Front. Integr. Neurosci. 18:1432270. doi: 10.3389/fnint.2024.1432270
Received: 13 May 2024; Accepted: 11 July 2024;
Published: 29 August 2024.
Edited by:
Steffen Schulz, Charité University Medicine Berlin, GermanyReviewed by:
Jonathan Davies, The University of Melbourne, AustraliaCopyright © 2024 Lopes, Sampaio and Tavares. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Isaura Tavares, aXNhdGF2QG1lZC51cC5wdA==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.