
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
MINI REVIEW article
Front. Integr. Neurosci. , 09 May 2011
Volume 5 - 2011 | https://doi.org/10.3389/fnint.2011.00017
This article is part of the Research Topic The development of deep brain stimulation for neurological and psychiatric disorders: clinical, societal and ethical issues. View all 18 articles
Deep brain stimulation (DBS) is currently used to treat neurological disorders like Parkinson’s disease, essential tremor, and dystonia, and is explored as an experimental treatment for psychiatric disorders like major depression and obsessive compulsive disorder. This mini review discusses ethical issues in DBS treatment and research, as they have been discussed in the medical and ethical literature. With regard to DBS treatment, the most important issues are balancing risks and benefits and ensuring respect for the autonomous wish of the patient. This implies special attention to patient selection, psycho-social impact of treatment, effects on personal identity, and treatment of children. Moreover, it implies a careful informed consent process in which unrealistic expectations of patients and their families are addressed and in which special attention is given to competence. In the context of research, the fundamental ethical challenge is to promote high-quality scientific research in the interest of future patients, while at the same time safeguarding the rights and interests of vulnerable research subjects. Several guidelines have been proposed to ensure this. One of the preconditions to further development of responsible and transparent research practices is the establishment of a comprehensive registry.
Deep brain stimulation (DBS) is currently used to treat neurological disorders like Parkinson’s disease (PD), essential tremor and dystonia, and is explored as an experimental treatment for psychiatric disorders like major depression (MD) and obsessive compulsive disorder (OCD).
Since DBS involves brain surgery and modulation of brain-states, it may invoke reminiscences of unethical neurosurgical practices from the past. For instance, it may remind one of the lobotomies performed by Moniz and Freeman or of the Tulane electrical stimulation program by Heath. Images from works of popular fiction, such as One Flew Over the Cuckoo’s Nest or The Manchurian Candidate, in which interventions in the brain are used to manipulate or otherwise abuse people, may also come to mind. Such images may influence the public perception of DBS and related ethical issues. There are, however, clear differences between past forms of neurosurgery and current DBS, which make the comparison go awry. Most importantly, operation techniques such as MRI-guided stereotactic surgery have improved and the intervention is therefore much safer. Moreover, the effects of DBS are mostly reversible – the stimulation can be turned off if it is not effective or causes too many adverse effects. Unlike some of the controversial neurosurgical interventions in the past, DBS is performed only in otherwise treatment-resistant patients, and only with informed consent from the patient (Synofzik and Schlaepfer, 2008).
Still, DBS raises some important ethical issues, both in the context of treatment and in that of research. These issues have been discussed in the medical as well as bioethical community, and researchers from both fields have often collaborated in identifying and discussing ethical issues. This contribution will give an overview of these discussions, based on a review of the relevant medical and ethical literature.
An ethical assessment of DBS treatment can depart from – and be structured by – the four basic principles of medical ethics: non-maleficence, beneficence, justice and respect for autonomy, and the additional principles of subsidiarity and proportionality (Table 1).
The first important ethical question is whether DBS is beneficial and does not harm the patient. In other words: are the expected risks and side-effects proportional to the expected benefits? This must be assessed both at a group-level and at the level of individual patients. At the group-level, this means that the available evidence regarding effectiveness, risks, and side effects of DBS for various conditions, in various target areas, and for various patient-populations must be assessed.
For disorders like PD, dystonia, and essential tremor DBS has been proven to be effective.
The risks and complications associated with DBS surgery include hemorrhage (1.3–4%), infection (2.8–6.1%), lead migration, misplacement or breakage (5.1%), and even death (0.4%; Clausen, 2010). Side effects depend partly on the stimulation target and include effects on cognition, behavior and psyche, including speech disturbances (10.8–33%), memory impairment (1.1–20%), aggression (2%), (hypo)mania (2–28%), hypersexuality (0.8%), depression (1.5–25%), and increased suicide risk (Clausen, 2010). The principle of subsidiarity implies that DBS should only be used when other less risky or burdensome treatment options have been exhausted.
In order to secure a favorable risk–benefit ratio for individual patients, careful patient selection is necessary. Patients need to stand a good chance to benefit from the procedure, have severe functional impairments and be refractory to other, less invasive or less burdensome, treatments. Also, candidates should be physically, cognitively, and emotionally capable of tolerating surgery and participating in postoperative care (Bell et al., 2009). This is best assessed in a multidisciplinary team (Kubu and Ford, 2007). Progress in DBS research may provide new insights that justify an expansion of indications for DBS. For example, it may prove to be beneficial for PD patients to start DBS treatment earlier in the disease process, because this may have a neuroprotective effect, or because it may prevent psycho-social problems related to advanced PD. In essential tremor, on the other hand, earlier intervention may not be beneficial because tolerance may develop.
With regard to the side effects of DBS it is increasingly recognized that these include not only physical or psychiatric symptoms. The psycho-social impact of the DBS treatment and the effects on overall quality of life should be included as well. Several studies have found that sometimes “the doctor is happy, the patient less so” (Agid et al., 2006), and DBS has been described as “a unique form of biographical disruption” (Gisquet, 2008). It was found that quality of life on aspects such as emotional well-being, social support, and interpersonal relationships may actually decrease after surgery, even when physical symptoms improve. These findings may be partly due to unrealistic expectations of patient. This emphasizes the need for good pre-operation counseling and the provision of clear and honest information in the informed consent process. Moreover, these findings point to the unsettling effects of successful treatment. Paradoxically, regained functioning may upset established social and relational patterns. Many patients have difficulties with psycho-social adjustment after surgery, especially with regard to their marital relationships, self-perception, and work. After surgery, a period of adaptation is necessary for both patients and their families. This requires professional psycho-social preparation and follow-up support (Schüpbach et al., 2006).
A special and frequently mentioned concern regarding the side effects of DBS is that changes in behavior, mood, or cognition caused by DBS might result in changes in “personal identity.” The ethical discussion on this point is complicated by the lack of clear and undisputed definitions of central concepts such as personality, self, identity, and authenticity (Merkel et al., 2007). A useful distinction can be made between numerical identity and narrative identity (Schermer, 2009a; Schechtman, 2010). The first refers to continuity of the same person over time, defined by bodily criteria (like DNA), or psychological criteria such as (autobiographical) memory or a set of core-characteristics. A change in numerical identity would mean that someone literally became someone else. If DBS would cause changes in mood, cognition, or behavior that would affect numerical identity (e.g., by completely wiping out or changing biographical memory), they would indeed be problematic since they would put people out of existence and create new people. This is not the case, however.
The relevant notion of personal identity is therefore narrative identity, which involves the person’s self-conception, his biography, values, and roles as well as his psychological characteristics and style. It is the answer to the question “who am I?” A person’s personality, defined by the DSM as “the enduring patterns of perceiving, relating to, and thinking about the environment and oneself that are exhibited in a wide range of social and personal contexts,” is thus part of his narrative identity. Mood, cognitions and behavior are also part of one’s personal narrative.
Changes in narrative personal identity are not necessarily ethically problematic in themselves – that is, apart from possible harmful consequences for others. People always change in many respects throughout their lives; personal identities are not static but develop over time. Disorders such as PD or dystonia can have a profound impact on the development of a person’s identity, as can their (successful) treatment. Some of the changes that DBS can bring about in personality, cognition, behavior, or mood may actually be sought by the patient and be the goal of treatment, for example mood improvement in depression, or tic-reduction in Tourette’s syndrome. Other changes may not be intended but can still be welcomed by the patient, for example an elevated mood or increased libido. The same changes can, however, be evaluated differently by different patients. The relevant ethical point is therefore whether or not the patient himself perceives the changes in his personality, mood, behavior, or cognition brought about by DBS as disruptive of his personal narrative identity (Schermer, 2009a; Synofzik and Schlaepfer, 2008). Moreover, the acute, rapid changes that DBS can bring about, can disrupt the normal, “narrative flow of life” and it may take time and effort of the patient to pick up and continue his life story (Schechtman, 2010). This may well account for the adjustment problems discussed above. Finally, if changes in personality and behavior negatively affect others, this may raise the problem of responsibility (see Schermer, 2009b).
Little has been written on the issue of justice with regard to DBS treatment. DBS is an expensive form of treatment, although it has been argued that DBS may turn out to be cost effective in the longer run as compared to alternative treatment options (Bell et al., 2009). In the face of scarcity of resources, it may be necessary to prioritize between (groups of) patients. From a perspective of justice, ideally, priority should be given to those who are most seriously impaired and who will benefit the most from the intervention. Priority setting becomes more difficult when “chance to benefit” and “seriousness of impairment” do not go together. Anyway, one should be careful not to exclude patients who might benefit from the procedure on grounds not related to expected benefit, for example because of their age.
Patients undergoing DBS must give their voluntary and fully informed consent to this procedure, just like for any other medical intervention. In practice this may be problematic for a number of reasons. First, some patients may be desperate because of their hopeless situation, suffering as they are from a serious, progressive, and treatment-refractory disease. They may feel they have no other option but to consent to the proposed treatment. However, this is not a unique situation for DBS and the fact that there are no other treatment options left does not imply that consent is not voluntary. Second, patients’ hopes and expectations of DBS may have been raised to unrealistic levels by enthusiastic media reports (Bell et al., 2010). Balanced and realistic information is therefore needed, not only regarding risks and side effects of the procedure but also regarding the expected benefits and the limitations of this treatment. It must be clear to patients, for example, that DBS will not cure their PD and will not stop its progression.
Another important consideration is the patient’s competence to consent to treatment. Competence can be challenged by the primary neurological disorder, or by co-morbidity like cognitive impairments or depression. It can however also be affected by DBS itself (Glannon, 2009).
Deep brain stimulation can, for example, induce a (hypo)manic state in patients and there are case reports of such patients who subsequently refuse adaptation of the stimulator settings because they are not aware of their disturbed mental state. These patients may harm themselves or others, for example by excessive gambling or reckless driving. Here, assessment of competence to decide is crucial to determine whether or not the treatment team may change the settings or discontinue treatment without the patient’s consent. If an incompetent patient inflicts severe harm on himself or others, it is ethically justified to intervene, under conditions of proportionality and subsidiarity. Because the effects of DBS are reversible, adjustment of settings or discontinuation of stimulation can restore the patient’s competence. In this way, the patient can be enabled to make his own autonomous decisions considering the further course of action. Fortunately, dramatic dilemma-situation as in the case report by Leentjens et al. (2004) – where a PD patient had to choose between being either completely bed-ridden but competent, or physically improved but manic – seem to be rare.
Deep brain stimulation treatment in children or adolescents, e.g., for dystonias or tic disorders, warrants extra ethical attention. First, because children are incompetent to decide for themselves about risks and benefits and are therefore more vulnerable to abuse. While this is no reason to exclude them from beneficial treatment – parents can act as representatives and make decisions in the best interest of their child – it necessitates an extra careful assessment of the risk–benefit ratio. Second, research on DBS in children is scarce. Only 35 children have been treated for dystonia and so there is little evidence regarding benefits and risks in children especially regarding long term effects on the developing brain (Lipsman et al., 2010). DBS treatment for neurological disorders in children should therefore be regarded as experimental and should only be performed by highly specialized teams and within well-designed and independently reviewed research protocols.
A special case that generates significant controversy concerns DBS treatment for treatment-refractory Tourette’s syndrome. Because the majority of Tourette’s patients have meaningful clinical improvement in adolescence or early adulthood, it is very questionable whether the immediate benefits that DBS may give these children in the short term, will eventually outweigh the risks in the longer run. Moreover, evidence of effectiveness of DBS is very limited, even in adult Tourette’s patients (Sassi et al., 2010). A consensus seems to be developing that only in extreme cases where tics cause spinal cord injury or myelopathy DBS may be considered as last-resort treatment in children (Lipsman et al., 2010).
Many new indications for DBS are currently investigated, among which many psychiatric disorders such as MD, OCD, and addiction. For clinical research involving human subjects the fundamental ethical challenge is to promote high-quality scientific research in the interest of (future) patients, while at the same time safeguarding the rights and interests of vulnerable research subjects. In the United States and Europe, national and international regulations apply to scientific research with human subjects and Institutional Review Boards (IRBs) or local ethics committees oversee their observance. With regard to DBS research in psychiatric disorders a number of ethical requirements have been specified and guidelines have been proposed by experts from the field (Nuttin et al., 2002; Kuhn et al., 2009; Rabins et al., 2009). The ethical principles underlying these guidelines are respect for autonomy and protection of research subjects, benefit for future patients, quality of research, and transparency (Table 2).
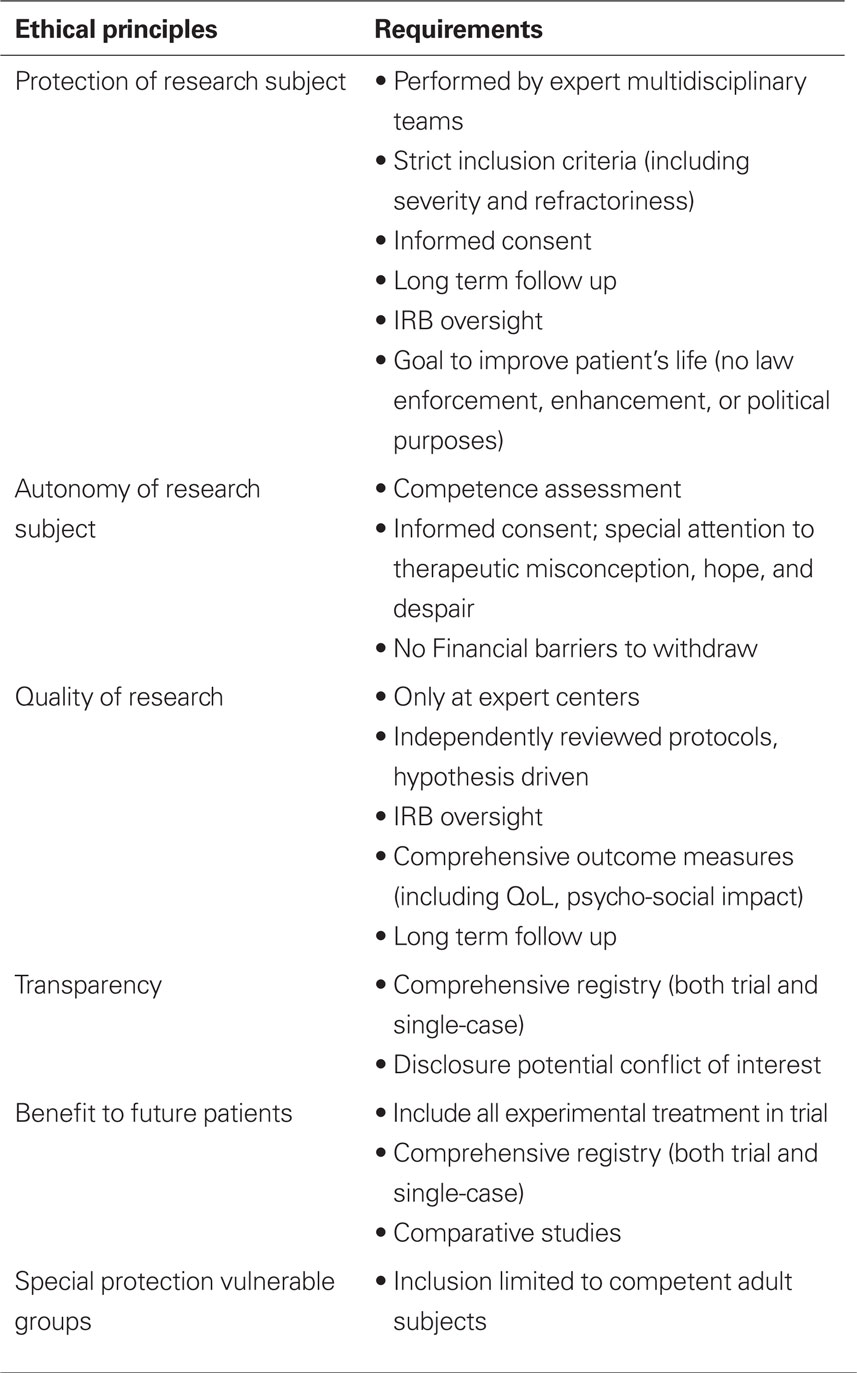
Table 2. Ethical guidelines for DBS research (based on: Nuttin et al., 2002; Kuhn et al., 2009; Rabins et al., 2009; Clausen, 2010; Schlaepfer and Fins, 2010).
Important and generally agreed upon recommendations are that research with DBS for psychiatric disorders should only be performed in expert centers, with experienced multidisciplinary teams. An IRB should review the research protocol and monitor the research-process. The research goals should include finding the appropriate anatomic sites and stimulation parameter, and comparing safety and efficacy of DBS with established treatments. Patient selection should be conducted carefully, and only severely afflicted and otherwise treatment-refractory patient should be included. Informed consent should be obtained, making sure the patient is competent and has realistic expectations and is not drive by sheer desperation and unrealistic hopes. According to Rabins et al. (2009) only adults and no children should be included. In general, experimental treatment should only be performed within the context of an established, duly constituted and independently reviewed research protocol. This will protect research subjects, as well as ensure that the experimental treatment will add to our scientific understanding of DBS and thus be potentially beneficial to future patients. Because of the importance of creating a sound evidence base and in order to prevent publication bias the creation of an independent registry has been proposed, both for trials and single-case studies (Rabins et al., 2009; Schlaepfer and Fins, 2010).
Long term follow up by a multidisciplinary team is ethically required both to ensure the well-being of the research subjects as for the benefit of future patients. This follow up should include safety and efficacy but also quality of life and psycho-social effects; follow up should also take into account information provided by a person close to the patient (Kuhn et al., 2009).
One ethical issue that has great salience in DBS research concerns the role of the industry. As Fins and Schiff(2010: 125) state: “clinical research in DBS presents a unique nexus of science and commerce in which market forces influence the contours of discovery, a small cadre of investigators is dependent upon an even smaller number of manufacturers for its tools of inquiry, and conflicts of interest complicate research.” Although companies may sincerely take the interests of patients at heart they also have a – legitimate – interest in making a profit. These two interests do not always coincide and the commercial motive may hamper free and innovative research, especially when researchers also have conflicting roles (e.g., both company-advisor and principal investigator). Disclosure of potential conflict of interest is important, but insufficient, since it does not resolve the underlying conflict of interest itself. This issue has been underexposed in the ethical discussion up till now but warrants serious attention from researchers, companies, and regulators.
Deep brain stimulation is an established treatment in neurology and is emerging as experimental treatment in the field of psychiatry. Over the past years, bioethicists and philosophers have been working in close cooperation with clinicians and researchers to identify and discuss the most important ethical issues in both clinical practice and research. There is a growing corpus of literature available that addresses these issues. The most pressing issues to be explored in further bioethical research are the psycho-social and identity-effects of DBS, its use in children, and the further development of responsible and transparent research practices.
The research for this mini review was conducted in the absence of any commercial or financial relationships that could be construed as potential conflict of interest.
Agid, Y., Schüpbach, M., Gargiulo, M., Mallet, L., Houeto, J. L., Behar, C., Maltête, D., Mesnage, V., and Welter, M. L. (2006). Neurosurgery in Parkinson’s patients: the doctor is happy, the patient less so? J. Neural Transm. 70, 409–414.
Bell, E., Mathieu, G., and Racine, E. (2009). Preparing the ethical future of deep brain stimulation. Surg. Neurol. 72, 577–586.
Bell, E., Maxwell, B., McAndrews, M. P., Sadikot, A., and Racine, E. (2010). Hope and patients’ expectations in deep brain stimulation: healthcare providers’ perspectives and approaches. J. Clin. Ethics 21, 112–124.
Clausen, J. (2010). Ethical brain stimulation – neuroethics of deep brain stimulation in research and clinical practice. Eur. J. Neurosci. 32, 1152–1162.
Fins, J. J., and Schiff, N. D. (2010). Conflicts of interest in deep brain stimulation research and the ethics of transparency. J. Clin. Ethics 21, 125–132.
Gisquet, E. (2008). Cerebral implants and Parkinson’s disease: a unique form of biographical disruption? Soc. Sci. Med. 67, 1847–1851.
Kubu, C. S., and Ford, P. J. (2007). Ethics in the clinical application of neural implants. Camb. Q. Healthc. Ethics 16, 317–321.
Kuhn, J., Gaebel, W., Klosterkoetter, J., and Woopen, C. (2009). Deep brain stimulation as a new therapeutic approach in therapy-resistant mental disorders: ethical aspects of investigational treatment. Eur. Arch. Psychiatry Clin. Neurosci. 259, S135–S141.
Leentjens, A. F., Visser-Vandewalle, V., Temel, Y., and Verhey, F. R. (2004). Manipulation of mental competence: an ethical problem in a case of electric stimulation of the subthalamic nucleus for severe Parkinson’s disease. Ned. Tijdschr. Geneeskd. 148, 1394–1398.
Lipsman, N., Ellis, M., and Lozano, A. M. (2010). Current and future indications for deep brain stimulation in pediatric populations. Neurosurg. Focus 29, E2.
Nuttin, B., Gründler, T. O., Lenartz, D., Sturm, V., Klosterkötter, J., and Huff, W. (2002). Deep brain stimulation for psychiatric disorders. Neurosurgery 51, 519.
Rabins, P., Appleby, B. S., Brandt, J., DeLong, M. R., Dunn, L. B., Gabriëls, L., Greenberg, B. D., Haber, S. N., Holtzheimer, P. E. III, Mari, Z., Mayberg, H. S., McCann, E., Mink, S. P., Rasmussen, S., Schlaepfer, T. E., Vawter, D. E., Vitek, J. L., Walkup, J., and Mathews, D. J. (2009). Scientific and ethical issues related to deep brain stimulation for disorders of mood, behavior and thought. Arch. Gen. Psychiatry 66, 931–937.
Merkel, R., Boer, G., Fegert, J., Galert, T., Hartmann, D., Nuttin, B., and Rosahl, S. (2007). Intervening in the Brain. Changing Psyche and Society. Berlin: Springer.
Sassi, M., Porta, M., and Servello, D. (2010). Deep brain stimulation therapy for treatment refractory Tourette’s syndrome. Acta Neurochir. (Wein) 153, 639–645.
Schechtman, M. (2010). Philosophical reflections on narrative and deep brain stimulation. J. Clin. Ethics 21, 133–139.
Schermer, M. (2009a). Changes in the self: the need for conceptual next to empirical research. Am. J. Bioeth. 9, 45–47.
Schermer, M. (2009b). The mind and the machine. On the conceptual and moral implications of brain-machine interaction. Nanoethics 3, 217–230.
Schlaepfer, T. E., and Fins, J. J. (2010). Deep brain stimulation and the ethics of responsible publishing. JAMA 303, 775–776.
Schüpbach, M., Gargiulo, M., Welter, M. L., Mallet, L., Béhar, C., Houeto, J. L., Maltête, D., Mesnage, V., and Agid, Y. (2006). Neurosurgery in Parkinson’s disease. A distressed mind in a repaired body? Neurology 66, 1811–1816.
Keywords: medical ethics, bioethics, neuroethics, deep brain stimulation, neuromodulation, research ethics, psychosurgery, neuro-psychiatric disorders
Citation: Schermer M (2011) Ethical issues in deep brain stimulation. Front. Integr. Neurosci. 5:17. doi: 10.3389/fnint.2011.00017
Received: 14 December 2010; Accepted: 26 April 2011;
Published online: 09 May 2011.
Edited by:
Chiara Saviane, Scuola Internazionale Superiore di Studi Avanzati, ItalyReviewed by:
Eric Racine, Institut de recherches cliniques de Montréal, CanadaCopyright: © 2011 Schermer. This is an open-access article subject to a non-exclusive license between the authors and Frontiers Media SA, which permits use, distribution and reproduction in other forums, provided the original authors and source are credited and other Frontiers conditions are complied with.
*Correspondence: Maartje Schermer, Department of Medical Ethics and Philosophy, Erasmus University Medical Center, AE 340, PO Box 2040, 3000 CA Rotterdam, Netherlands. e-mail:bS5zY2hlcm1lckBlcmFzbXVzbWMubmw=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.