- 1Department of Psychiatry, Faculty of Medicine, Geneva University (UNIGE), Geneva, Switzerland
- 2Department of Psychiatry, Faculty of Biomedical Sciences, University of Italian Switzerland (USI), Lugano, Switzerland
- 3Department of Psychiatry, Adult Psychiatry Service, Geneva University Hospital (HUG), Geneva, Switzerland
- 4Department of Neuroscience, Rehabilitation, Ophthalmology, Genetics, Maternal and Child Health, Section of Psychiatry, University of Genoa, Genoa, Italy
- 5IRCCS Polyclinic Hospital San Martino, Genoa, Italy
- 6Department of Psychiatry, San Maurizio Hospital of Bolzano, Bolzano, Italy
- 7Geriatric-Rehabilitation Department, University Hospital of Parma, Parma, Italy
- 8Chinese University of Hong Kong, Hong Kong, Hong Kong SAR, China
- 9Department of Microbiology and Immunology, Stanford University, Stanford, CA, United States
- 10Department of Neurosciences, Mental Health and Sensory Organs, Suicide Prevention Centre, Sant’Andrea Hospital, Faculty of Medicine and Psychology, Sapienza University, Rome, Italy
The association between inflammation with depression and suicide has prompted many investigations of the potential contributors to inflammatory pathology in these psychiatric illnesses. However, a distillation of diverse clinical findings into an integrated framework of the possible involvement of major physiological processes in the elicitation of pathological inflammation in depression and suicide has not yet been explored. Therefore, this review aims to provide a concise synthesis of notable clinical correlates of inflammatory pathology in subjects with various depressive and suicidal clinical subtypes into a mechanistic framework, which includes aberrant immune activation, deregulated neuroendocrine signaling, and impaired host-microbe interaction. These issues are of significant research interest as their possible interplays might be involved in the development of distinct subtypes of depression and suicide. We conclude the review with discussion of a pathway-focused therapeutic approach to address inflammatory pathology in these psychiatric illnesses within the realm of personalized care for affected patients.
1 Pathobiology of depression and suicide
Investigation of the complex pathobiology of depression and suicide, including both suicidal ideation (SI) and behavior (SB), is pivotal to achieve advances in diagnosis, prevention, and treatment of these psychiatric illnesses. There is a variety of neurobiological hypotheses of depression and SI/SB, often involving abnormalities from multiple areas of biology with ramified interactions (1–5). Currently, neurobiological hallmarks of depression and SI/SB are of immense research interest as no current markers of such origins are of sufficient clinical utility (6–12). Moreover, a thorough understanding of molecular and cellular pathways of these two conditions can be hindered by their complex behavioral manifestations, interaction with psychosocial, cultural, and environmental factors, diverse patient subpopulations, and the presence of somatic and psychiatric comorbidities (10, 13–17).
Recent evidence of associations between inflammatory mediators with various neurological and psychiatric illnesses, including depression and suicide, has highlighted the important role of pathological inflammation in the development of these conditions (18–26). Therefore, this review aims to categorically distill major clinical observations of the presence of inflammation in depression and SI/SB into a putative etiological framework, which involves crosstalks among immunological abnormalities, neurometabolic impairment, and dysregulated host-microbe interactions.
2 Inflammatory hallmarks of depression and suicide
The etiological connection between inflammation, depression, and suicide was first suggested by the increased risk of these neuropsychiatric conditions in patients with inflammatory somatic illnesses (27). Depressive symptoms and SI/SB were also observed in some patients receiving immunotherapy that elicits robust inflammatory responses, such as IFN-α (28). More importantly, the presence of focal inflammation in depression- and SI/SB-associated brain structures, such as the pre-frontal and anterior cingulate cortex (29, 30), further supported the involvement of pathological inflammation in these psychiatric illnesses. Here, we aim to synthesize notable clinical observations of diverse inflammatory manifestations in depressed and suicidal patients into specific inflammatory phenotypes of different clinical subtypes of these neuropsychiatric illnesses.
2.1 Depression
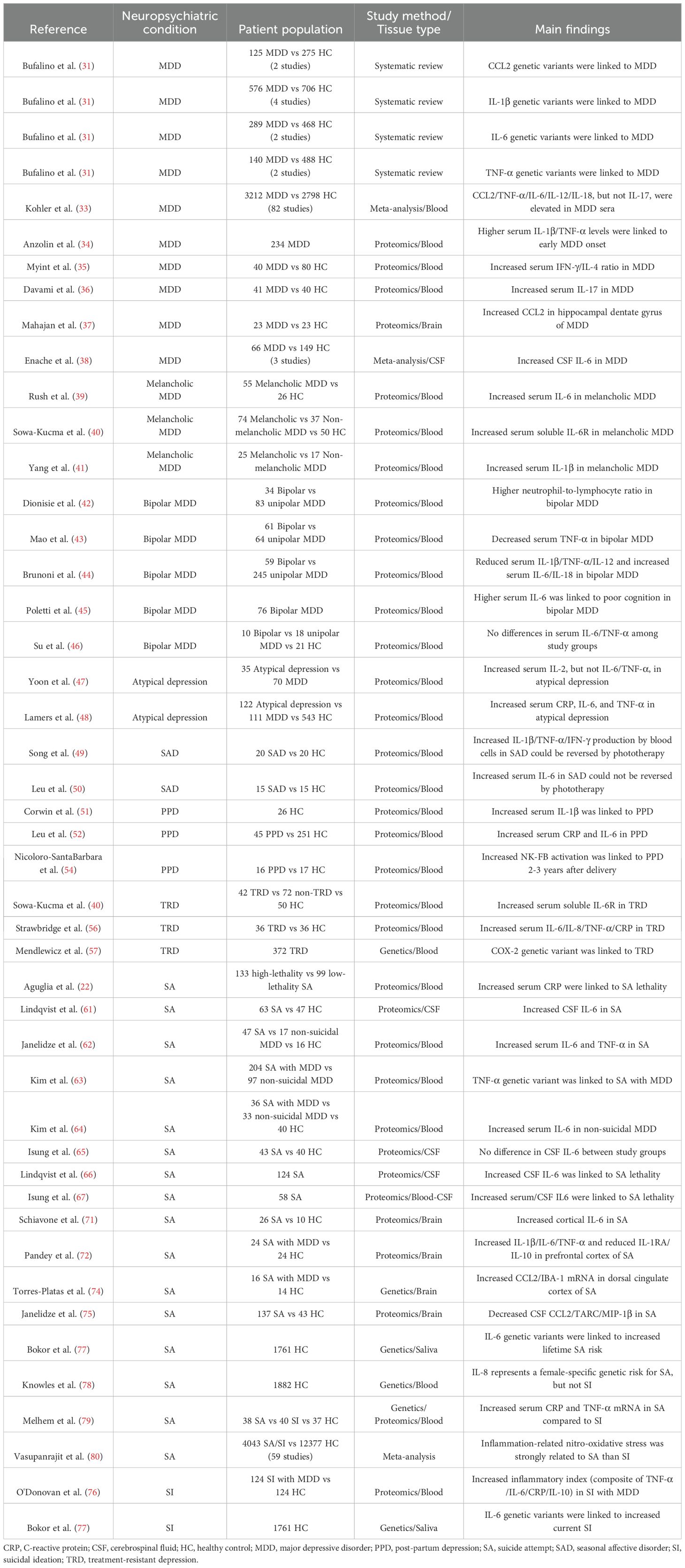
Major depressive disorder (MDD) is characterized by the persistent presence of depressed mood, reduced interest in pleasure-seeking activities, feelings of guilt/worthlessness, low energy, poor concentration, alterations in appetite/sleep/psychomotor functions, or suicidal thoughts. MDD has been the primary focus of studies of inflammation in patients with depressive symptoms. Notably, (epi)genetic as well as proteomic alterations of circulating and central nervous system (CNS)-specific inflammatory mediators were detected in MDD patients (Table 1). In this regard, polymorphisms in several innate immunity-associated inflammatory cytokines, such as CCL2, IL-1β, IL-6, and TNF-α, were correlated with more severe MDD symptoms (31). Conversely, a unique variant in IL-6R was also linked to reduced risk of depression and/or psychosis (32). In agreement with these genetic analyses, protein levels of selected innate immunity-associated inflammatory cytokines, including CCL2, TNF-α, IL-6, IL-12, and IL-18, were elevated in sera of MDD patients compared to healthy individuals (33). Importantly, early MDD-onset age was linked to a systemic pro-inflammatory state (34), driven by IL-1β and TNF-α.
Besides alterations that are closely related to innate-immune mediated inflammation, the adaptive immunity-associated inflammatory cytokine, IFN-γ, has also been implicated in the pathogenesis of depression, with increased expression of serum IFN-γ/IL-4 ratio in MDD patients (35). Another T lymphocyte-associated inflammatory cytokine, IL-17, was reportedly elevated in MDD blood samples, with some discrepancies between reports (33, 36). While the majority of MDD studies focused on peripheral inflammatory markers, neuroinflammation in MDD has also been documented. In this regard, CCL2 expression in brain parenchyma was elevated in post-mortem brain tissues of MDD patients (37). Additionally, IL-6 level in cerebrospinal fluid (CSF) were increased in MDD subjects (38).
While the aforementioned clinical findings suggest that prototypical inflammation is prominently present in MDD, some variants of this neuropsychiatric condition might exhibit distinct inflammatory profiles (Table 1). In this regard, melancholic MDD was associated with elevated serum IL-1β, IL-6, and soluble IL-6R levels (39–41). Furthermore, selected inflammatory alterations were uniquely linked to bipolar MDD compared to unipolar MDD. For example, increased neutrophil-to-lymphocyte ratio (NLR), an inflammatory index, has been proposed as a diagnostic parameter to distinguish bipolar from unipolar MDD (42). Other indicators to distinguish bipolar from unipolar MDD are reduced serum levels of IL-1β, TNF-α, and IL-12, and increased serum levels of IL-6 and IL-18 (43, 44). Of mechanistic importance, increased serum IL-6 was linked to poorer cognition in bipolar MDD (45). It’s worth noting that some unique inflammatory features of bipolar MDD have been disputed. For example, no significant differences in serum TNF-α and IL-6 levels were observed between bipolar and unipolar MDD (46). These differences might be related to disease activity at the time of inflammatory marker measurements. Hence, further longitudinal analyses of fluctuations in inflammatory markers of MDD patients might provide important insights on the role of specific inflammatory pathways in the onset of manic episodes.
Similar to MDD, inflammatory pathology has been observed in other depression subtypes (Table 1). In atypical depression, circulating inflammatory mediators, such as IL-2, C-reactive protein (CRP), IL-6, and TNF-α, were significantly elevated, although differences in IL-6 and TNF-α were not consistently observed (47, 48). In seasonal affective disorder (SAD), production of IL-1β, TNF-α, and IFN-γ in cultures of circulating immune cells was elevated, which could be reversed by phototherapy (49). Interestingly, serum IL-6 was also elevated in SAD patients but could not be normalized by this therapeutic approach (50), suggesting distinct effects of this treatment on different inflammatory mediators. In post-partum depression (PPD), depressive symptoms were associated with increased expression of serum CRP, IL-1β, and IL-6 (51, 52). Notably, elevated inflammation was detected as early as 1-3 days after childbirth (53) and their persistence for several years after delivery was linked to PPD (54), highlighting the possible initiating role of inflammation in this type of depression as well as its long-lasting epigenetic impact.
Treatment responsiveness represents a therapeutic challenge for patients with depression (55), partly owing to the delayed impact of anti-depressants that occur only after an extended treatment period (of at least one month). Consequentially, pre-treatment biomarkers that could predict therapeutic efficacy of anti-depressants are of immense clinical interest. In this regard, several predictors of treatment-resistant depression (TRD) have been proposed, including elevated serum levels of IL-6, IL-8, TNF-α, soluble IL-6R, and CRP (40, 56) or polymorphisms in COX-2 (57). However, some conflicting findings regarding correlations between changes in inflammatory markers and antidepressant response to ketamine in TRD exist (58), which might be explained by the heterogeneity of this patient population. In fact, anti-inflammatory therapy was only effective in a subset of TRD patients with elevated expression of inflammatory mediators (59).
2.2 Suicidal ideation and behavior
The interconnected pathobiology of depression and suicide suggests that overlapping inflammatory signatures might exist between these two conditions. However, few studies have examined potential differences in inflammatory features between suicidal depressed and suicidal non-depressed subjects (24). It has been hypothesized that subjects at risk for suicide might be biologically distinguishable from depressed individuals without such risk by a heightened pro-inflammatory state, characterized by elevated serum IL-6 (60). Nevertheless, a consensus on unique and/or shared inflammatory features between depression and SI/SB has not been reached, given the diverse approaches to patient stratification in studies of these two conditions. As such, mechanistic insights from clinical correlates must be carefully interpreted. The following section aims to highlight inflammatory changes in different suicidal subtypes, while acknowledging the possible coexistence of depressive symptoms in affected individuals.
In subjects who made an suicidal attempt (SA), increased serum levels of IL-6 and TNF-α, elevated CSF levels of IL-6, and TNF-α polymorphisms were observed (61–63). However, differences in IL-6 in CSF and sera could not be confirmed by other studies (64, 65), possibly due to confounding demographic factors, such as patient stratification and/or medication status. Interestingly, the lethality of SA was reportedly associated with specific inflammatory chemokines/cytokines in the CSF (66) as well as serum CRP and IL-6 (a stimulator of hepatic CRP synthesis) (22, 67). Mechanistically, increased expression of inflammatory markers might predispose subjects with specific behavioral traits, such as impulsivity, aggression, and hostility (15, 68–70), to violent SA.
Besides fluid-based biomarker studies, post-mortem brain tissue analysis has provided important insights on the possible association between neuroinflammation and SA. For example, cortical IL-6 was upregulated in asphytic suicidal subjects (71). Depressed suicidal patients also showed elevated expression of inflammatory cytokines (IL-1β, IL-6, and TNF-α) and reduced levels of anti-inflammatory mediators (IL-1RA and IL-10) in the prefrontal cortex (72). Interestingly, aberrant epigenetic regulation might account for the elevated expression of TNF-α in the brains of subjects with SA (73). Increased CCL2 mRNA expression were also noted in the dorsal anterior cingulate cortex of suicide victims, which was correlated with IBA-1-expressing brain macrophage accumulation (74). However, decreased macrophage-attracting chemokines, including CCL2, TARC, and MIP-1β, were observed in another study (75).
In MDD subjects with SI, a higher systemic inflammatory score was observed compared to healthy controls (76). Furthermore, IL-6 genetic variants appeared to interact with childhood adversities or recent life stress to influence lifetime risk of SA and current SI (77). However, different magnitudes of inflammatory changes might distinguish SA from SI. For example, the chemokine IL-8 represented a female-specific genetic risk factor for SA but not SI (78). Increased serum CRP and TNF-α mRNA from blood cells were also observed in SA compared to SI (79). Finally, inflammation-related nitro-oxidative stress was more strongly related to SA than SI (80).
While these observations need to be further validated with detailed consideration of patient characteristics and other confounders, they have prompted a provocative hypothesis that dynamic changes in inflammation might underlie the development of SI/SA and progression from the former to the latter. Furthermore, inflammatory pathology has also been documented in various psychiatric illnesses, suggesting the possible existence of a common inflammatory pathway among behavioral disorders.
3 Contributors to inflammation in depression and suicide
While the relative contribution of each inflammatory mediator to distinct pathological manifestations of depression and SI/SB needs to be further examined, abnormalities in major inflammation-associated physiological processes have been observed in these conditions. Notably, immunological and neuroendocrinological abnormalities have been linked to inflammatory pathology in depression and suicide. Furthermore, dysregulated host-microbe interaction has recently emerged as another major contributor to inflammation in these conditions. While we do not exclude the possible crosstalks between these signaling axes with other factors, such as those of (epi)genetic and environmental origins, the following sections will propose a mechanistic synthesis of clinical evidence focusing on abnormalities in these three major physiological processes (Figure 1).
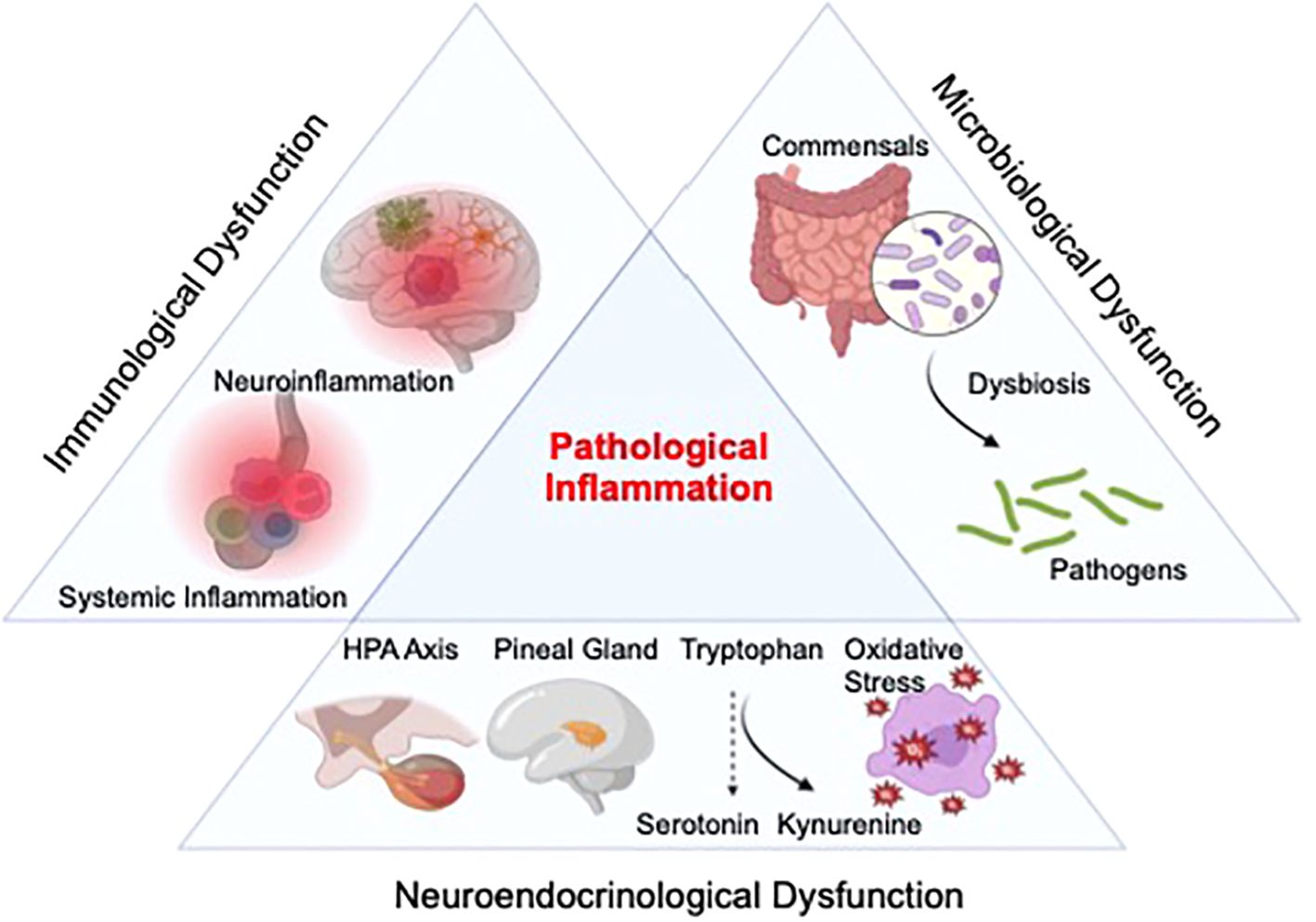
Figure 1. Proposed etiological framework of inflammation in depression and suicide. Inflammation in depression and suicide might result from overactivation of the neuroimmune system, with abnormalities in the function/distribution of various circulating adaptive and innate immune cell as well as possible alterations in activation profiles and concentration of cellular components of the central nervous system (CNS), including astrocytes, microglia, and infiltrated macrophages. Furthermore, alterations in several neurometabolic axes, such as the hypothalamic-pituitary-adrenal (HPA) pathway, melatonin signaling, kynurenine metabolism, and oxidative stress, might also contribute to this pathology. Lastly, dysregulated host-microbe interaction (dysbiosis) may heighten the production of inflammatory mediators in these neuropsychiatric conditions.
3.1 Aberrant activation of the immune system
As a major source of inflammatory mediators, the immune system has long been implicated in the development of inflammatory pathology in depression and suicide (23, 24, 81). Peripheral perturbations in various immune cell subsets have been observed in these conditions. For example, reduced function and numbers of T cells and natural killer cells were linked to MDD (82). However, expansions of various T-helper subtypes, including Th-17 cells, were also detected in depressed patients (83), suggesting that temporally distinct immune activation profiles might exist during the progression of this psychiatric illness. Regarding innate immunity-related changes, increased numbers of blood monocytes and frequencies of neutrophils were observed in depressed subjects (60, 84). Notably, a heightened systemic accumulation of these cells might distinguish subjects with increased suicide risk from non-suicidal depressed patients (60).
Besides alterations in peripheral immunity, abnormal activation of microglia and macrophages in the CNS has also been examined in the context of depression and suicide. However, observations of gliosis-related changes were inconsistent in depressed and suicidal patients (38), possibly due to the impact of death on glial cell reactivity as well as the different types of tissue-sampling methods (brain regions, cerebrospinal fluid vs. brain parenchyma). Alternatively, gliosis might have resulted from an influx of peripheral monocytes/macrophages. The latter viewpoint is supported by observations of higher concentrations of blood vessels surrounded by macrophages in the anterior cingulate cortex of depressed suicidal patients, evidenced by increased IBA-1 and CD45 mRNA expression (74). Increased activation markers of astrocytes have also been implicated in suicide and depression. For instance, increased circulating levels of S100B and CSF levels of glial fibrillary acidic protein (GFAP) were observed in depressed subjects (85, 86), while reactive astrocytosis with hypertrophic morphology was noted in the white matter of the anterior cingulate cortex of depressed suicide completers (87).
Altogether, the clinical findings above highlight hyper-activation of the peripheral and CNS immune repertoires as a root cause of pathological inflammation in depression and suicide. Mechanistically, exuberant inflammatory responses of peripheral and CNS immune cells in the context of these psychiatric conditions might be mediated by abnormally activated pro-inflammatory signaling cascades (Figure 2). In this regard, increased expression of various molecular regulators of the toll-like receptors (TLR)/nuclear factor-kappa B (NF-KB) pathway have been associated with depression and suicide. For example, increased TLR4 expression in peripheral immune cells was linked to MDD symptoms while elevated TLR3/TLR4 expression was observed in the dorsolateral prefrontal cortex of depressed suicidal patients (88, 89). NF-KB and the expression of its related genes were reportedly higher in depressed adolescents and adults (90, 91). Another master regulator of inflammation, the nod-like receptor pyrin-containing 3 (NLRP3) inflammasome, has also been implicated in these neuropsychiatric conditions (92). For example, mRNA expression of NLRP3 and its related genes (the adaptor apoptosis-associated speck-like protein ASC, caspase-1) in peripheral immune cells were increased in MDD patients compared to healthy controls (93, 94). Specific DNA methylation pattern of NLRP3 in depressed brains was also linked to depression-associated neuroanatomical changes (cortical thickness) and neuroinflammatory processes (95). In an analysis of post-mortem brain samples from depressed suicidal patients, evidence of hyperactive NLRP3 inflammasome (elevated protein and mRNA expression of NLRP3, Caspase-1, and the inflammasome adaptor protein ASC) was also observed (96). Importantly, two anti-depressants, amitriptyline (97) and ketamine (98), could respectively reduce NLRP3 and NK-FB expressive, and consequentially, inflammatory cytokine production in peripheral blood cells from MDD subjects. Collectively, these findings provide further mechanistic support for the involvement of pro-inflammatory signaling cascades in the orchestration of immunological inflammation in MDD.
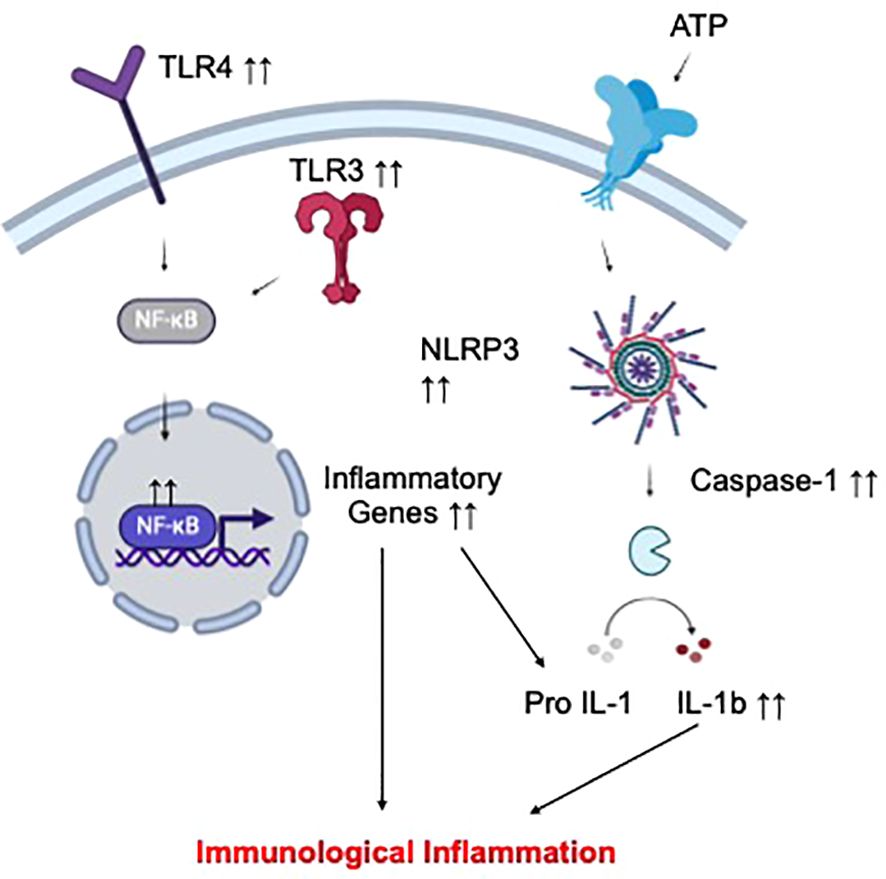
Figure 2. Proposed mechanism of immunological inflammation in depression and suicide. Increased activation status of different circulating and CNS immune cell subsets has been implicated in depression and suicide. Such hyperinflammatory phenotype of these cells might result from elevated signal transduction via selected pro-inflammatory pathways, including those of TLR-NFKB and the NLRP3 inflammasome, leading to overproduction of inflammatory cytokines, and ultimately, peripheral and CNS inflammation.
3.2 Impaired neurometabolic signaling
Quantitative analyses of clinical specimens from depressed and suicidal subjects revealed changes in the concentrations of various metabolites and hormones compared to healthy individuals. Importantly, these bioactive molecules point to the potential disruption of homeostatic signaling of several neuroendocrine systems as another important contributor to pathological inflammation in these neuropsychiatric illnesses (Figure 3). Their putative mechanistic contributions to pathological inflammation in depression and suicide will be detailed in this section.
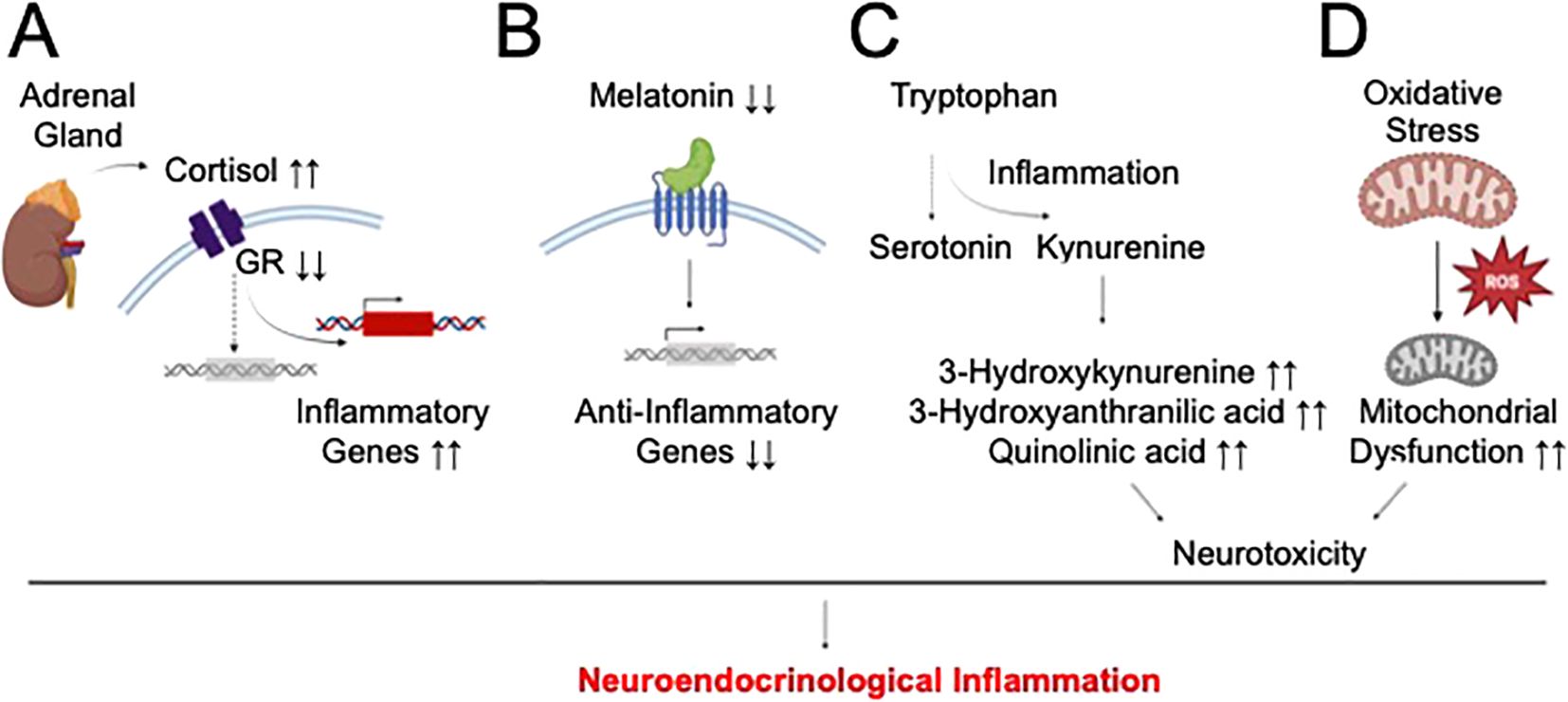
Figure 3. Proposed mechanism of neuroendocrinological inflammation in depression and suicide. Several neuroendocrine pathways might contribute to the inflammatory pathology of depression and suicide by distinct pathways. (A) HPA dysfunction-induced hypercortisolemia might result in glucocorticoid receptor (GR) downregulation/desensitization and activation of non-canonical inflammation signaling of cortisol. (B) Impaired melatonin production might dampen its downstream anti-inflammatory properties. (C) Primary inflammatory insult might induce the divergence of tryptophan’s catabolic fate away from serotonin synthesis and towards neurotoxic kynurenine metabolism, and ultimately, secondary inflammation. (D) Oxidative stress might result in mitochondrial dysfunction and impaired antioxidant defense, causing neurotoxicity and inflammation.
Abnormalities in the hypothalamic-pituitary-adrenal (HPA) axis, a major stress response system, have been noted in depression and suicide, regardless of the presence of any other psychiatric conditions (99). This signaling pathway consists of various neuroendocrine hormones, such as corticotropin-releasing hormone (CRH), adrenocorticotropic hormone (ACTH), and cortisol, which are released in response to stress. In this regard, more than 40% of depressed patients exhibited hypercortisolemia, increased CRH production or reduced ACTH release (100), with hypercortisolemia being associated with MDD severity and MDD-associated psychosis (101). Similarly, increased cortisol response has been observed in depressed suicidal subjects (102). Age-dependent hypercortisolemia were also linked to SA (103). Mechanistically, hypercortisolemia might represent a compensatory response to reduced glucocorticoid receptor (GR) expression. In fact, reduced hippocampal GR expression was observed in brain specimens of abused suicidal patients and linked to early-life trauma-induced epigenetic changes (methylation) in the NR3C1 gene (104). Alternatively, hypercortisolemia might desensitize GR signaling (105), thereby increasing the propensity for non-canonical inflammatory signaling of cortisol (Figure 3A). In fact, reduced GR-α expression in the prefrontal cortex and amygdala of suicide victims was linked to higher expression of CRP and TNF-α (106).
Beside HPA dysfunction, perturbations in the signaling pathway of melatonin, a pineal gland-derived hormone that regulates the sleep-wakefulness cycle, have been observed in depression and suicide. Specifically, single-nucleotide polymorphism of the melatonin receptor in the brain was associated with depression (107), while changes in melatonin levels and production patterns was documented in various depression subtypes (108). Decreased melatonin concentrations in the pineal gland was also observed in suicide victims (109). A connection between melatonin dysregulation and inflammatory pathology in depression and suicide might be related to the compromised anti-inflammatory properties of this hormone on innate immune cells (110) (Figure 3B).
Another prominent hypothesis of depression and suicide development focuses on dysregulated kynurenine metabolism. This metabolite of the tryptophan catabolic pathway represents a rate-limiting step in the diversion of tryptophan availability from the synthesis of serotonin, a neuroprotective neurotransmitter in depression. In fact, acute tryptophan deprivation might be able to trigger clinical symptoms of depression (111). Additionally, kynurenine pathway activation was observed in various forms of depression (112, 113) and correlated with depression severity (114). Increased toxic metabolites of the kynurenine pathway, such as 3-hydroxykynurenine, 3-hydroxyanthranilic acid, and quinolinic acid, have been associated with reduced cortical thickness in MDD (115) or linked to MDD development (116, 117). In suicidal patients, reduced serotonin metabolism was linked to possible dysregulation of kynurenine signaling (118). In fact, positive correlations between the cytokine activation marker neopterin with the kynurenine:tryptophan ratio and between abnormally elevated quinolinic acid concentration and increased inflammatory potential have been reported (119, 120). Elevated serum concentration of kynurenine was also observed in MDD patients with SA (121). Of mechanistic interest, a bidirectional interaction between kynurenine metabolism and inflammation might occur in depression and suicide. While kynurenine catabolic activation might be induced by inflammatory signals, toxic metabolites of this pathway might cause neuronal injuries and secondary inflammatory response, thereby propagating this vicious interactome (Figure 3C).
Finally, oxidative stress has been implicated in depression and suicide (23, 24, 122). Reduced antioxidant levels and/or increased oxidative stress markers were observed in brain specimens and blood samples of depressed subjects (122, 123). In suicide pathophysiology, increased NADPH oxidase was associated with SI, while increased nitro-oxidative stress markers and reduced antioxidant levels were linked to SA (80, 124). Mechanistically, oxidative stress can damage the mitochondria, triggering inflammatory reactions (Figure 3D). In fact, concomitant increases in inflammation and oxidative stress were observed in maltreated children, who developed higher risk of depression in adulthood (125). Reduced circulating antioxidants in depressed patients were also linked to elevated serum inflammatory cytokines (126). Furthermore, the high-oxygen demand of the CNS renders this tissue highly susceptible to oxidative stress-induced mitochondrial damage and reduced antioxidant defense, followed by the vicious cycle of elevated neuroinflammation and neurotoxicity in vulnerable brain regions, which underlies various behavioral pathologies of depression and suicide development.
3.3 Dysregulated host-microbe interaction
Alterations in the microbiome have recently emerged as a novel pathology of various neuropsychiatric illnesses, including depression and suicide (127, 128). In depressed subjects, the most commonly observed alterations in the microbiome are related to those of the gastrointestinal compartment. In this regard, most studies found changes in beta-diversity (dissimilarity between depressed and control subjects) as well as alterations in abundance (the concentrations of specific microbes) of selected microbial phyla (Proteobacteria and Fusobacteria), families (Rikenellaceaea, Enterobacteriaceae, and Ruminococcaeceae), and geniuses (Eggerthella, Alistipes, Parabacteroides, Enterococcus, Lactobacillus, Veillonella, Flavonifractor, Streptococcus and Faecalibacterium) in fecal samples of MDD patients compared to health controls (129). In other studies, alterations in abundance, but not diversity, of selected salivary microbial genera (Prevotella, Haemophilus, Rothia, Treponema, Schaalia, Neisseria, Solobacterium, Lepotrichia, Fusobacterium, and Veillonella) and species (Lachnoanaerobaculum orale, Fusobacterium periodonticum, and Mobiluncus Mulieris) were associated with depressive symptoms (130, 131). In suicidal MDD patients, six microbial taxa were linked to suicidal behaviors (positive associations: Hungatella and Fusicatenibacter, negative associations: Butyricicoccus, Clostridium, Parabacteroides merdae, and Desulfovibrio piger) (132). Furthermore, SI was reportedly associated with changes in salivary abundance of various microbial genera (Veillonella, Streptococcus, Prevotella, Rothia, Alloprevotella, Granulicatella, Porphyromonas, Peptostreptococcus, Stomatobaculum, Gemella, and Solobacterium) and species (Streptococcus oralis, Prevotella melaninogenica, Fusobacterium periodoncitum, Rothia mucilagniosa, Graulicatella adiacens, Streptococcus parasanguinis, Prevotella nanciensis, Solobacterium moorei, Dialister pneumosintes, Peptoanaerobacter stomatis, Actinomyces naeslundii, Bacteroides dorei, and Fusobacterium naviforme) (133). Last but not least, increased laxative misuse, which is associated with gastrointestinal microbial dysbiosis, were linked to a history of SA (134).
Mechanistically, microbial dysbiosis might contribute to inflammatory pathology by triggering the loss of intestinal barrier integrity, exposing intestinal immune cells to inflammatory environmental stimuli. In fact, higher depressive symptoms were reportedly associated with increased intestinal permeability in cancer patients (135). Reduced zonulin expression, a biomarker of increased intestinal permeability, was also observed in patients with MDD or those with SA (136). Furthermore, compositional changes in commensals, as a result of dysbiosis, might trigger excessive release of microbe-associated inflammatory stimuli (137) and reduce the availability of anti-inflammatory microbial products, such as short-chain fatty acids (138), leading to unrestrained intestinal immune activation. Of note, the gut-brain interactome might relay microbiome-associated inflammatory signals from peripheral tissues to the brain (137, 139), contributing to depression- and suicide-associated neuroinflammation (Figure 4).
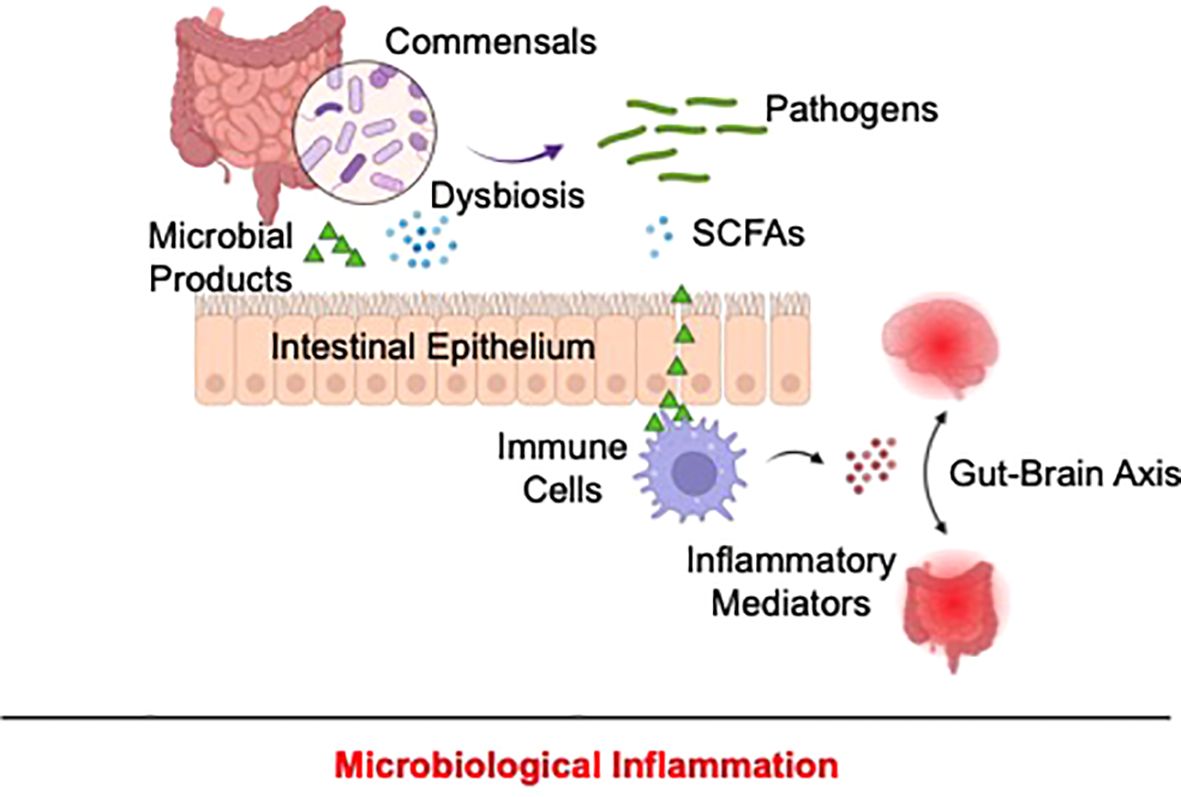
Figure 4. Proposed mechanism of microbiological inflammation in depression and suicide. In depression and suicide, alterations of the microbiome might disrupt intestinal barrier, allowing exposure of resident immune cells to pathogen-associated pro-inflammatory stimuli and concomitantly reducing the production of anti-inflammatory microbial products, including as short-chain fatty acids. As a result, unrestrained gastrointestinal immune activation occurs and might be relayed to the CNS via the gut-brain interactome, resulting in depression and suicide-associated inflammation.
4 Therapeutic insights
Current literature on the involvement of inflammation and various putative etiological pathways of this pathology in depression and suicide has prompted clinical examination of the efficacy of anti-inflammatory agents for the treatment of these psychiatric conditions. Early trials primarily focused on non-steroidal anti-inflammatory drugs (NSAIDs). NSAIDs’ primary mechanism of action is to inhibit the enzyme cyclooxygenase (COX), which is responsible for the production of inflammatory eicosanoids (thromboxanes, prostaglandins, and prostacyclins). As a standalone (140, 141) or adjunct therapy (142, 143), NSAIDs yielded promising outcomes as a treatment for depressive symptoms in MDD patients as well as those with other comorbid illnesses. NSAIDs were also suggested to be effective in mitigating SI risk (26), providing the impetus for further exploration of these agents in suicide prevention. Besides NSAIDs, glucocorticoids, whose binding on their cognate receptor, GR, turns on anti-inflammatory gene expression to curb immune cell activation, also exhibited short-term efficacy in alleviating depression (144, 145). Minocycline, an antibiotic with dual immunosuppressive function via its inhibition of the inflammasome (Caspase-1 and Caspase-3), pro-inflammatory enzymes (COX-2, inducible nitric oxide synthase [iNOS], matrix metalloproteinase [MMP], and phospholipase A2 [PLA2]), and immune cell proliferation/activation, also exerted anti-depressant effects in TRD patients and depressed HIV-infected subjects (146, 147). However, the efficacy of these agents requires further clinical validation (148). To date, the most compelling evidence for a pathway-focused treatment of depression, with mechanistic relevance to inflammatory pathology, emerged in clinical studies of inhibitors against different inflammatory cytokines (148). For example, IL-6 inhibitors (sirukumab and siltuximab) (149), IL-12/IL-23 inhibitor (ustekinumab) (150), IL-17 inhibitor (ixekizumab) (151), and TNF-α inhibitors (adalilumab and etanercept) (152–155) were effective in reducing depressive symptoms in patients with comorbid inflammatory diseases. Notably, infliximab, another TNF-α inhibitor, also showed some promising anti-depressant effect in TRD patients (60).
Besides these immune-related therapies, microbiome modifications have emerged as an attractive therapeutic promise in depression. Some proprietary probiotic formulations (live microorganisms with health-promoting benefits) were reportedly effective in reducing depressive symptoms (156–159). Additionally, prebiotics (nutrients that promote the growth of beneficial microorganisms) might possess some anti-depressant effects, with conflicting outcomes that require further confirmation (159, 160). Various molecular regulators of oxidative stress, HPA axis, and kynurenine pathway have also been proposed as promising therapeutic targets in depression treatment and suicide prevention (126, 161). Additionally, the impact of melatonin on depression-related inflammation warrants further examination, given its preliminary clinical effectiveness in depression (162). Other treatment approaches for depression focused on anti-infective agents (163) and their potential inhibitory effect on inflammation. Notably, melatonin and some anti-infective/anti-inflammatory therapies have been linked to the development of depressive symptoms and SB/SI, prompting additional caution when using these agents to treat psychiatric illnesses (164–166). Lastly, other treatment approaches with anti-inflammatory properties, such as psilocybin and cognitive behavioral therapies (167, 168), might provide additional mechanistic insights on the origin of inflammation in depression and suicide.
Given the diverse nature of inflammatory phenotypes of different subtype of depression and suicide, future treatment approaches might be more clinically impactful with detailed considerations of unique alterations in inflammatory biomarkers in prescribing anti-inflammatory treatments. Such biomarkers might also be of utility in monitoring treatment responsiveness, which are of urgent need in the case of TRD. Furthermore, the co-existence of dysfunctions in multiple inflammatory signaling pathways might require a combination treatment approach to achieve optimal therapeutic outcomes. Finally, integrated care that combines interventions addressing specific inflammatory pathology with current psychopharmacologic and psychotherapeutic treatments, is expected to improve therapeutic efficacy in depression and suicide.
5 Conclusions
The development of inflammatory pathology in depression and suicide may stem from dysregulation in immunological and neuroendocrinological signaling and improper microbial interactions with the host. Further investigations are required to elucidate the precise contributions of and/or interactions among these major physiological processes in distinct clinical subtypes of depression and suicide. These questions are of great clinical interest as they could help identify disease patterns, in the context of pathological inflammation, that may allow more targeted treatment approaches and personalized preventive strategies for depression and suicide.
Author contributions
AC: Conceptualization, Writing – original draft, Writing – review & editing. AAm: Writing – review & editing. AAg: Writing – review & editing. LM: Conceptualization, Writing – original draft. AP: Writing – review & editing. KN: Conceptualization, Writing – original draft. IB: Writing – review & editing. MP: Supervision, Validation, Writing – review & editing. MA: Supervision, Validation, Writing – review & editing. GS: Supervision, Validation, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. Open access funding by University of Geneva.
Conflict of interest
KN is the scientific founder of Tranquis Therapeutics, a biotechnology company that develops novel treatments for neuroinflammatory and neurodegenerative diseases. KN is also a scientific advisor for Tochikunda, a biotechnology company that develops SARS-CoV-2 diagnostic devices.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Hawton K, van Heeringen K. Suicide. Lancet. (2009) 373:1372–81. doi: 10.1016/s0140-6736(09)60372-x
2. Turecki G. The molecular bases of the suicidal brain. Nat Rev Neurosci. (2014) 15:802–16. doi: 10.1038/nrn3839
3. van Heeringen K, Mann JJ. The neurobiology of suicide. Lancet Psychiatry. (2014) 1:63–72. doi: 10.1016/s2215-0366(14)70220-2
4. Dean J, Keshavan M. The neurobiology of depression: An integrated view. Asian J Psychiatry. (2017) 27:101–11. doi: 10.1016/j.ajp.2017.01.025
5. Mann JJ, Rizk MM. A brain-centric model of suicidal behavior. Am J Psychiatry. (2020) 177:902–16. doi: 10.1176/appi.ajp.2020.20081224
6. Costanza A, D’Orta I, Perroud N, Burkhardt S, Malafosse A, Mangin P, et al. Neurobiology of suicide: do biomarkers exist? Int J Legal Med. (2013) 128:73–82. doi: 10.1007/s00414-013-0835-6
7. Oquendo MA, Sullivan GM, Sudol K, Baca-Garcia E, Stanley BH, Sublette ME, et al. Toward a biosignature for suicide. Am J Psychiatry. (2014) 171:1259–77. doi: 10.1176/appi.ajp.2014.14020194
8. Sudol K, Mann JJ. Biomarkers of suicide attempt behavior: towards a biological model of risk. Curr Psychiatry Rep. (2017) 19:31–1. doi: 10.1007/s11920-017-0781-y
9. Kouter K, Paska AV. Biomarkers for suicidal behavior: miRNAs and their potential for diagnostics through liquid biopsy - a systematic review. Epigenomics. (2020) 12:2219–35. doi: 10.2217/epi-2020-0196
10. Orsolini L, Latini R, Pompili M, Serafini G, Volpe U, Vellante F, et al. Understanding the complex of suicide in depression: from research to clinics. Psychiatry Invest. (2020) 17:207–21. doi: 10.30773/pi.2019.0171
11. Fusar-Poli L, Aguglia A, Amerio A, Orsolini L, Salvi V, Serafini G, et al. Peripheral BDNF levels in psychiatric patients with and without a history of suicide attempt: A systematic review and meta-analysis. Prog Neuropsychopharmacol Biol Psychiatry. (2021) 111:110342. doi: 10.1016/j.pnpbp.2021.110342
12. Ivanets NN, Svistunov AA, Chubarev VN, Kinkulkina MA, Tikhonova YG, Syzrantsev NS, et al. Can molecular biology propose reliable biomarkers for diagnosing major depression? Curr Pharm design. (2021) 27:305–18. doi: 10.2174/1381612826666201124110437
13. Turecki G, Ernst C, Jollant F, Labonté B, Mechawar N. The neurodevelopmental origins of suicidal behavior. Trends Neurosci. (2012) 35:14–23. doi: 10.1016/j.tins.2011.11.008
14. Hawton K, Casañas I Comabella C, Haw C, Saunders K. Risk factors for suicide in individuals with depression: a systematic review. J Affect Disord. (2013) 147:17–28. doi: 10.1016/j.jad.2013.01.004
15. Turecki G, Brent DA. Suicide and suicidal behaviour. Lancet. (2016) 387:1227–39. doi: 10.1016/S0140-6736(15)00234-2
16. Costanza A, Baertschi M, Weber K, Canuto A. Maladies neurologiques et suicide: de la neurobiology au manque d'éspoir [Neurological diseases and suicide: from neurobiology to hopelessness. Rev Med Suisse. (2015) 11:402–5.
17. Costanza A, Amerio A, Aguglia A, Escelsior A, Serafini G, Berardelli I, et al. When sick brain and hopelessness meet: some aspects of suicidality in the neurological patient. CNS Neurol Disord Drug Targets. (2020) 19:257–63. doi: 10.2174/1871527319666200611130804
18. Aguglia A, Amerio A, Asaro P, Caprino M, Conigliaro C, Giacomini G, et al. High-lethality of suicide attempts associated with platelet to lymphocyte ratio and mean platelet volume in psychiatric inpatient setting. World J Biol Psychiatry. (2021) 22:119–27. doi: 10.1080/15622975.2020.1761033
19. Costanza A, Xekardaki A, Kovari E, Gold G, Bouras C, Giannakopoulos P. Microvascular burden and Alzheimer-type lesions across the age spectrum. J Alzheimers Dis. (2012) 32:643–52. doi: 10.3233/JAD-2012-120835
20. Aguglia A, Serafini G, Solano P, Giacomini G, Conigliaro C, Salvi V, et al. The role of seasonality and photoperiod on the lethality of suicide attempts: A case-control study. J Affect Disord. (2019) 246:895–901. doi: 10.1016/j.jad.2018.12.094
21. Aguglia A, Giacomini G, Montagna E, Amerio A, Escelsior A, Capello M, et al. Meteorological variables and suicidal behavior: air pollution and apparent temperature are associated with high-lethality suicide attempts and male gender. Front Psychiatry. (2021) 12:653390–0. doi: 10.3389/fpsyt.2021.653390
22. Aguglia A, Natale A, Fusar-Poli L, Gnecco GB, Lechiara A, Marino M, et al. C-reactive protein as a potential peripheral biomarker for high-lethality suicide attempts. Life (Basel Switzerland). (2022) 12(10):1557. doi: 10.3390/life12101557
23. Serafini G, Costanza A, Aguglia A, Amerio A, Trabucco A, Escelsior A, et al. The role of inflammation in the pathophysiology of depression and suicidal behavior: implications for treatment. Med Clinics North America. (2023) 107:1–29. doi: 10.1016/j.mcna.2022.09.001
24. Serafini G, Parisi VM, Aguglia A, Amerio A, Sampogna G, Fiorillo A, et al. A specific inflammatory profile underlying suicide risk? Systematic review of the main literature findings. Int J Environ Res Public Health. (2020) 17(7):2393. doi: 10.3390/ijerph17072393
25. Amasi-Hartoonian N, Pariante CM, Cattaneo A, Sforzini L. Understanding treatment-resistant depression using "omics" techniques: A systematic review. J Affect Disord. (2022) 318:423–55. doi: 10.1016/j.jad.2022.09.011
26. Costanza A, Amerio A, Aguglia A, Serafini G, Amore M, Hasler R, et al. Hyper/neuroinflammation in COVID-19 and suicide etiopathogenesis: Hypothesis for a nefarious collision? Neurosci Biobehav Rev. (2022) 136:104606. doi: 10.1016/j.neubiorev.2022.104606
27. Miller V, Hopkins L, Whorwell PJ. Suicidal ideation in patients with irritable bowel syndrome. Clin Gastroenterol Hepatol. (2004) 2:1064–8. doi: 10.1016/S1542-3565(04)00545-2
28. Raison CL, Demetrashvili M, Capuron L, Miller AH. Neuropsychiatric adverse effects of interferon-alpha: recognition and management. CNS Drugs. (2005) 19:105–23. doi: 10.2165/00023210-200519020-00002
29. Thomas AJ, Ferrier IN, Kalaria RN, Davis S, O'Brien JT. Cell adhesion molecule expression in the dorsolateral prefrontal cortex and anterior cingulate cortex in major depression in the elderly. Br J Psychiatry. (2002) 181:129–34. doi: 10.1192/bjp.181.2.129
30. Pandey GN, Rizavi HS, Ren X, Fareed J, Hoppensteadt DA, Roberts RC, et al. Proinflammatory cytokines in the prefrontal cortex of teenage suicide victims. J Psychiatr Res. (2012) 46:57–63. doi: 10.1016/j.jpsychires.2011.08.006
31. Bufalino C, Hepgul N, Aguglia E, Pariante CM. The role of immune genes in the association between depression and inflammation: a review of recent clinical studies. Brain behavior Immun. (2013) 31:31–47. doi: 10.1016/j.bbi.2012.04.009
32. Khandaker GM, Zammit S, Burgess S, Lewis G, Jones PB. Association between a functional interleukin 6 receptor genetic variant and risk of depression and psychosis in a population-based birth cohort. Brain behavior Immun. (2018) 69:264–72. doi: 10.1016/j.bbi.2017.11.020
33. Köhler CA, Freitas TH, Maes M, de Andrade NQ, Liu CS, Fernandes BS, et al. Peripheral cytokine and chemokine alterations in depression: a meta-analysis of 82 studies. Acta psychiatrica Scandinavica. (2017) 135:373–87. doi: 10.1111/acps.12698
34. Anzolin AP, Feiten JG, Bristot G, Possebon GMP, Fleck M, Caldieraro MA, et al. Earlier age of onset is associated with a pro-inflammatory state in major depressive disorder. Psychiatry Res. (2022) 314:114601–1. doi: 10.1016/j.psychres.2022.114601
35. Myint A-M, Leonard BE, Steinbusch HWM, Kim Y-K. Th1, Th2, and Th3 cytokine alterations in major depression. J Affect Disord. (2005) 88:167–73. doi: 10.1016/j.jad.2005.07.008
36. Davami MH, Baharlou R, Ahmadi Vasmehjani A, Ghanizadeh A, Keshtkar M, Dezhkam I, et al. Elevated IL-17 and TGF-β Serum levels: A positive correlation between T-helper 17 cell-related pro-inflammatory responses with major depressive disorder. Basic Clin Neurosci. (2016) 7:137–42. doi: 10.15412/J.BCN.03070207
37. Mahajan GJ, Vallender EJ, Garrett MR, Challagundla L, Overholser JC, Jurjus G, et al. Altered neuro-inflammatory gene expression in hippocampus in major depressive disorder. Prog Neuropsychopharmacol Biol Psychiatry. (2018) 82:177–86. doi: 10.1016/j.pnpbp.2017.11.017
38. Enache D, Pariante CM, Mondelli V. Markers of central inflammation in major depressive disorder: A systematic review and meta-analysis of studies examining cerebrospinal fluid, positron emission tomography and post-mortem brain tissue. Brain behavior Immun. (2019) 81:24–40. doi: 10.1016/j.bbi.2019.06.015
39. Rush G, O'Donovan A, Nagle L, Conway C, McCrohan A, O'Farrelly C, et al. Alteration of immune markers in a group of melancholic depressed patients and their response to electroconvulsive therapy. J Affect Disord. (2016) 205:60–8. doi: 10.1016/j.jad.2016.06.035
40. Sowa-Kućma M, Styczeń K, Siwek M, Misztak P, Nowak RJ, Dudek D, et al. Lipid peroxidation and immune biomarkers are associated with major depression and its phenotypes, including treatment-resistant depression and melancholia. Neurotoxicity Res. (2018) 33:448–60. doi: 10.1007/s12640-017-9835-5
41. Yang C, Tiemessen KM, Bosker FJ, Wardenaar KJ, Lie J, Schoevers RA. Interleukin, tumor necrosis factor-α and C-reactive protein profiles in melancholic and non-melancholic depression: A systematic review. J psychosomatic Res. (2018) 111:58–68. doi: 10.1016/j.jpsychores.2018.05.008
42. Dionisie V, Filip GA, Manea MC, Movileanu RC, Moisa E, Manea M, et al. Neutrophil-to-lymphocyte ratio, a novel inflammatory marker, as a predictor of bipolar type in depressed patients: A quest for biological markers. J Clin Med. (2021) 10(9):1924. doi: 10.3390/jcm10091924
43. Mao R, Zhang C, Chen J, Zhao G, Zhou R, Wang F, et al. Different levels of pro- and anti-inflammatory cytokines in patients with unipolar and bipolar depression. J Affect Disord. (2018) 237:65–72. doi: 10.1016/j.jad.2018.04.115
44. Brunoni AR, Supasitthumrong T, Teixeira AL, Vieira EL, Gattaz WF, Benseñor IM, et al. Differences in the immune-inflammatory profiles of unipolar and bipolar depression. J Affect Disord. (2020) 262:8–15. doi: 10.1016/j.jad.2019.10.037
45. Poletti S, Mazza MG, Calesella F, Vai B, Lorenzi C, Manfredi E, et al. Circulating inflammatory markers impact cognitive functions in bipolar depression. J Psychiatr Res. (2021) 140:110–6. doi: 10.1016/j.jpsychires.2021.05.071
46. Su S-C, Sun M-T, Wen M-J, Lin C-J, Chen Y-C, Hung Y-J. Brain-derived neurotrophic factor, adiponectin, and proinflammatory markers in various subtypes of depression in young men. Int J Psychiatry Med. (2011) 42:211–26. doi: 10.2190/PM.42.3.a
47. Yoon H-K, Kim Y-K, Lee H-J, Kwon D-Y, Kim L. Role of cytokines in atypical depression. Nordic J Psychiatry. (2012) 66:183–8. doi: 10.3109/08039488.2011.611894
48. Lamers F, Vogelzangs N, Merikangas KR, de Jonge P, Beekman ATF, Penninx BWJH. Evidence for a differential role of HPA-axis function, inflammation and metabolic syndrome in melancholic versus atypical depression. Mol Psychiatry. (2013) 18:692–9. doi: 10.1038/mp.2012.144
49. Song C, Luchtman D, Kang Z, Tam EM, Yatham LN, Su K-P, et al. Enhanced inflammatory and T-helper-1 type responses but suppressed lymphocyte proliferation in patients with seasonal affective disorder and treated by light therapy. J Affect Disord. (2015) 185:90–6. doi: 10.1016/j.jad.2015.06.003
50. Leu SJ, Shiah IS, Yatham LN, Cheu YM, Lam RW. Immune-inflammatory markers in patients with seasonal affective disorder: effects of light therapy. J Affect Disord. (2001) 63:27–34. doi: 10.1016/S0165-0327(00)00165-8
51. Corwin EJ, Johnston N, Pugh L. Symptoms of postpartum depression associated with elevated levels of interleukin-1 beta during the first month postpartum. Biol Res Nurs. (2008) 10:128–33. doi: 10.1177/1099800408323220
52. Liu H, Zhang Y, Gao Y, Zhang Z. Elevated levels of Hs-CRP and IL-6 after delivery are associated with depression during the 6 months post partum. Psychiatry Res. (2016) 243:43–8. doi: 10.1016/j.psychres.2016.02.022
53. Maes M, Lin AH, Ombelet W, Stevens K, Kenis G, De Jongh R, et al. Immune activation in the early puerperium is related to postpartum anxiety and depressive symptoms. Psychoneuroendocrinology. (2000) 25:121–37. doi: 10.1016/S0306-4530(99)00043-8
54. Nicoloro-SantaBarbara JM, Carroll JE, Minissian M, Kilpatrick SJ, Cole S, Merz CNB, et al. Immune transcriptional profiles in mothers with clinically elevated depression and anxiety symptoms several years post-delivery. Am J Reprod Immunol (New York N.Y: 1989). (2022) 88:e13619. doi: 10.1111/aji.13619.
55. Gaynes BN, Lux L, Gartlehner G, Asher G, Forman-Hoffman V, Green J, et al. Defining treatment-resistant depression. Depression Anxiety. (2020) 37:134–45. doi: 10.1002/da.22968
56. Strawbridge R, Hodsoll J, Powell TR, Hotopf M, Hatch SL, Breen G, et al. Inflammatory profiles of severe treatment-resistant depression. J Affect Disord. (2019) 246:42–51. doi: 10.1016/j.jad.2018.12.037
57. Mendlewicz J, Crisafulli C, Calati R, Kocabas NA, Massat I, Linotte S, et al. Influence of COX-2 and OXTR polymorphisms on treatment outcome in treatment resistant depression. Neurosci Lett. (2012) 516:85–8. doi: 10.1016/j.neulet.2012.03.063
58. Park M, Newman LE, Gold PW, Luckenbaugh DA, Yuan P, MaChado-Vieira R, et al. Change in cytokine levels is not associated with rapid antidepressant response to ketamine in treatment-resistant depression. J Psychiatr Res. (2017) 84:113–8. doi: 10.1016/j.jpsychires.2016.09.025
59. Raison CL, Rutherford RE, Woolwine BJ, Shuo C, Schettler P, Drake DF, et al. A randomized controlled trial of the tumor necrosis factor antagonist infliximab for treatment-resistant depression: the role of baseline inflammatory biomarkers. JAMA Psychiatry. (2013) 70:31–41. doi: 10.1001/2013.jamapsychiatry.4
60. Keaton SA, Madaj ZB, Heilman P, Smart L, Grit J, Gibbons R, et al. An inflammatory profile linked to increased suicide risk. J Affect Disord. (2019) 247:57–65. doi: 10.1016/j.jad.2018.12.100
61. Lindqvist D, Janelidze S, Hagell P, Erhardt S, Samuelsson M, Minthon L, et al. Interleukin-6 is elevated in the cerebrospinal fluid of suicide attempters and related to symptom severity. Biol Psychiatry. (2009) 66:287–92. doi: 10.1016/j.biopsych.2009.01.030
62. Janelidze S, Mattei D, Westrin Å, Träskman-Bendz L, Brundin L. Cytokine levels in the blood may distinguish suicide attempters from depressed patients. Brain behavior Immun. (2011) 25:335–9. doi: 10.1016/j.bbi.2010.10.010
63. Kim Y-K, Hong J-P, Hwang J-A, Lee H-J, Yoon H-K, Lee B-H, et al. TNF-alpha –308G>A polymorphism is associated with suicide attempts in major depressive disorder. J Affect Disord. (2013) 150:668–72. doi: 10.1016/j.jad.2013.03.019
64. Kim Y-K, Lee S-W, Kim S-H, Shim S-H, Han S-W, Choi S-H, et al. Differences in cytokines between non-suicidal patients and suicidal patients in major depression. Prog Neuropsychopharmacol Biol Psychiatry. (2008) 32:356–61. doi: 10.1016/j.pnpbp.2007.08.041
65. Isung J, Aeinehband S, Mobarrez F, Mårtensson B, Nordström P, Asberg M, et al. Low vascular endothelial growth factor and interleukin-8 in cerebrospinal fluid of suicide attempters. Trans Psychiatry. (2012) 2:e196. doi: 10.1038/tp.2012.123
66. Lindqvist D, Janelidze S, Erhardt S, Träskman-Bendz L, Engström G, Brundin L. CSF biomarkers in suicide attempters–a principal component analysis. Acta psychiatrica Scandinavica. (2011) 124:52–61. doi: 10.1111/j.1600-0447.2010.01655.x
67. Isung J, Aeinehband S, Mobarrez F, Nordström P, Runeson B, Asberg M, et al. High interleukin-6 and impulsivity: determining the role of endophenotypes in attempted suicide. Trans Psychiatry. (2014) 4:e470–0. doi: 10.1038/tp.2014.113
68. Brent DA, Johnson BA, Perper J, Connolly J, Bridge J, Bartle S, et al. Personality disorder, personality traits, impulsive violence, and completed suicide in adolescents. J Am Acad Child Adolesc Psychiatry. (1994) 33:1080–6. doi: 10.1097/00004583-199410000-00003
69. Coccaro EF, Lee R, Coussons-Read M. Elevated plasma inflammatory markers in individuals with intermittent explosive disorder and correlation with aggression in humans. JAMA Psychiatry. (2014) 71:158–65. doi: 10.1001/jamapsychiatry.2013.3297
70. Costanza A, Rothen S, Achab S, Thorens G, Baertschi M, Weber K, et al. Impulsivity and impulsivity-related endophenotypes in suicidal patients with substance use disorders: an exploratory study. Int J Ment Health Addict. (2021) 19:1729–44. doi: 10.1007/s11469-020-00259-3
71. Schiavone S, Neri M, Mhillaj E, Morgese MG, Cantatore S, Bove M, et al. The NADPH oxidase NOX2 as a novel biomarker for suicidality: evidence from human post mortem brain samples. Trans Psychiatry. (2016) 6:e813. doi: 10.1038/tp.2016.76
72. Pandey GN, Rizavi HS, Zhang H, Bhaumik R, Ren X. Abnormal protein and mRNA expression of inflammatory cytokines in the prefrontal cortex of depressed individuals who died by suicide. J Psychiatry neuroscience: JPN. (2018) 43:376–85. doi: 10.1503/jpn.170192
73. Wang Q, Roy B, Turecki G, Shelton RC, Dwivedi Y. Role of complex epigenetic switching in tumor necrosis factor-α Upregulation in the prefrontal cortex of suicide subjects. Am J Psychiatr. (2018) 175:262–74. doi: 10.1176/appi.ajp.2017.16070759
74. Torres-Platas SG, Cruceanu C, Chen GG, Turecki G, Mechawar N. Evidence for increased microglial priming and macrophage recruitment in the dorsal anterior cingulate white matter of depressed suicides. Brain Behavior Immun. (2014) 42:50–9. doi: 10.1016/j.bbi.2014.05.007
75. Janelidze S, Ventorp F, Erhardt S, Hansson O, Minthon L, Flax J, et al. Altered chemokine levels in the cerebrospinal fluid and plasma of suicide attempters. Psychoneuroendocrinology. (2013) 38:853–62. doi: 10.1016/j.psyneuen.2012.09.010
76. O'Donovan A, Rush G, Hoatam G, Hughes BM, McCrohan A, Kelleher C, et al. Suicidal ideation is associated with elevated inflammation in patients with major depressive disorder. Depress Anxiety. (2013) 30:307–14. doi: 10.1002/da.22087
77. Bokor J, Sutori S, Torok D, Gal Z, Eszlari N, Gyorik D, et al. Inflamed mind: multiple genetic variants of IL6 influence suicide risk phenotypes in interaction with early and recent adversities in a linkage disequilibrium-based clumping analysis. Front Psychiatry. (2021) 12:746206. doi: 10.3389/fpsyt.2021.746206
78. Knowles EEM, Curran JE, Göring HHH, Mathias SR, Mollon J, Rodrigue A, et al. Family-based analyses reveal novel genetic overlap between cytokine interleukin-8 and risk for suicide attempt. Brain Behav Immun. (2019) 80:292–9. doi: 10.1016/j.bbi.2019.04.004
79. Melhem NM, Munroe S, Marsland A, Gray K, Brent D, Porta G, et al. Blunted HPA axis activity prior to suicide attempt and increased inflammation in attempters. Psychoneuroendocrinology. (2017) 77:284–94. doi: 10.1016/j.psyneuen.2017.01.001
80. Vasupanrajit A, Jirakran K, Tunvirachaisakul C, Solmi M, Maes M. Inflammation and nitro-oxidative stress in current suicidal attempts and current suicidal ideation: a systematic review and meta-analysis. Mol Psychiatry (2022) 27(3):1350–61. doi: 10.1038/s41380-021-01407-4
81. Dantzer R. Cytokine, sickness behavior, and depression. Immunol Allergy Clinics North America. (2009) 29:247–64. doi: 10.1016/j.iac.2009.02.002
82. Grosse L, Carvalho LA, Birkenhager TK, Hoogendijk WJ, Kushner SA, Drexhage HA, et al. Circulating cytotoxic T cells and natural killer cells as potential predictors for antidepressant response in melancholic depression. Restor T Regul Cell populations after antidepressant Ther Psychopharmacol. (2016) 233:1679–88. doi: 10.1007/s00213-015-3943-9
83. Schiweck C, Valles-Colomer M, Arolt V, Müller N, Raes J, Wijkhuijs A, et al. Depression and suicidality: A link to premature T helper cell aging and increased Th17 cells. Brain behavior Immun. (2020) 87:603–9. doi: 10.1016/j.bbi.2020.02.005
84. Valesco Á, Rodríguez-Revuelta J, Olié E, Abad I, Fernández-Peláez A, Cazals A, et al. Neutrophil-to-lymphocyte ratio: A potential new peripheral biomarker of suicidal behavior. Eur psychiatry: J Assoc Eur Psychiatrists. (2020) 63:e14. doi: 10.1192/j.eurpsy.2019.20
85. Tural U, Irvin MK, Iosifescu DV. Correlation between S100B and severity of depression in MDD: A meta-analysis. World J Biol Psychiatry. (2022) 23:456–63. doi: 10.1080/15622975.2021.2013042
86. Michel M, Fiebich BL, Kuzior H, Meixensberger S, Berger B, Maier S, et al. Increased GFAP concentrations in the cerebrospinal fluid of patients with unipolar depression. Trans Psychiatry. (2021) 11:308. doi: 10.1038/s41398-021-01423-6
87. Torres-Platas SG, Hercher C, Davoli MA, Maussion G, Labonté B, Turecki G, et al. Astrocytic hypertrophy in anterior cingulate white matter of depressed suicides. Neuropsychopharmacology. (2011) 36:2650–8. doi: 10.1038/npp.2011.154
88. Wu MK, Huang TL, Huang KW, Huang YL, Hung YY. Association between toll-like receptor 4 expression and symptoms of major depressive disorder. Neuropsychiatr Dis Treat. (2015) 11:1853–7. doi: 10.2147/NDT.S88430
89. Pandey GN, Rizavi HS, Ren X, Bhaumik R, Dwivedi Y. Toll-like receptors in the depressed and suicide brain. J Psychiatr Res. (2014) 53:62–8. doi: 10.1016/j.jpsychires.2014.01.021
90. Pace TW, Wingenfeld K, Schmidt I, Meinlschmidt G, Hellhammer DH, Heim CM. Increased peripheral NF-kappaB pathway activity in women with childhood abuse-related posttraumatic stress disorder. Brain behavior Immun. (2012) 26:13–7. doi: 10.1016/j.bbi.2011.07.232
91. Miklowitz DJ, Portnoff LC, Armstrong CC, Keenan-Miller D, Breen EC, Muscatell KA, et al. Inflammatory cytokines and nuclear factor-kappa B activation in adolescents with bipolar and major depressive disorders. Psychiatry Res. (2016) 241:315–22. doi: 10.1016/j.psychres.2016.04.120
92. Kaufmann FN, Costa AP, Ghisleni G, Diaz AP, Rodrigues ALS, Peluffo H, et al. NLRP3 inflammasome-driven pathways in depression: Clinical and preclinical findings. Brain behavior Immun. (2017) 64:367–83. doi: 10.1016/j.bbi.2017.03.002
93. Taene A, Khalili-Tanha G, Esmaeili A, Mobasheri L, Kooshkaki O, Jafari S, et al. The association of major depressive disorder with activation of NLRP3 inflammasome, lipid peroxidation, and total antioxidant capacity. J Mol Neurosci. (2020) 70:65–70. doi: 10.1007/s12031-019-01401-0
94. Momeni M, Ghorban K, Dadmanesh M, Khodadadi H, Bidaki R, Kazemi Arababadi M, et al. ASC provides a potential link between depression and inflammatory disorders: A clinical study of depressed Iranian medical students. Nordic J Psychiatry. (2016) 70:280–4. doi: 10.3109/08039488.2015.1100328
95. Han KM, Choi KW, Kim A, Kang W, Kang Y, Tae WS, et al. Association of DNA methylation of the NLRP3 gene with changes in cortical thickness in major depressive disorder. Int J Mol Sci. (2022) 23:5768. doi: 10.3390/ijms23105768
96. Pandey GN, Zhang H, Sharma A, Ren X. Innate immunity receptors in depression and suicide: upregulated NOD-like receptors containing pyrin (NLRPs) and hyperactive inflammasomes in the postmortem brains of people who were depressed and died by suicide. J Psychiatry Neurosci. (2021) 46:E538–47. doi: 10.1503/jpn.210016
97. Sokołowska P, Seweryn Karbownik M, Jóźwiak-Bębenista M, Dobielska M, Kowalczyk E, Wiktorowska-Owczarek A. Antidepressant mechanisms of ketamine's action: NF-κB in the spotlight. Biochem Pharmacol. (2023) 218:115918. doi: 10.1016/j.bcp.2023.115918
98. Alcocer-Gómez E, de Miguel M, Casas-Barquero N, Núñez-Vasco J, Sánchez-Alcazar JA, Fernández-Rodríguez A, et al. NLRP3 inflammasome is activated in mononuclear blood cells from patients with major depressive disorder. Brain behavior immunity. (2014) 36:111–7. doi: 10.1016/j.bbi.2013.10.017
99. Berardelli I, Serafini G, Cortese N, Fiaschè F, O'Connor RC, Pompili M. The involvement of hypothalamus-pituitary-adrenal (HPA) axis in suicide risk. Brain Sci. (2020) 10(9):653. doi: 10.3390/brainsci10090653
100. Du X, Pang TY. Is dysregulation of the HPA-axis a core pathophysiology mediating co-morbid depression in neurodegenerative diseases? Front Psychiatry. (2015) 6:32–2. doi: 10.3389/fpsyt.2015.00032
101. Schatzberg AF, Rothschild AJ, Langlais PJ, Bird ED, Cole JO. A corticosteroid/dopamine hypothesis for psychotic depression and related states. J Psychiatr Res. (1985) 19:57–64. doi: 10.1016/0022-3956(85)90068-8
102. Hennings JM, Ising M, Uhr M, Holsboer F, Lucae S. Effects of weariness of life, suicide ideations and suicide attempt on HPA axis regulation in depression. Psychoneuroendocrinology. (2021) 131:105286–6. doi: 10.1016/j.psyneuen.2021.105286
103. O'Connor DB, Ferguson E, Green JA, O'Carroll RE, O'Connor RC. Cortisol levels and suicidal behavior: A meta-analysis. Psychoneuroendocrinology. (2016) 63:370–9. doi: 10.1016/j.psyneuen.2015.10.011
104. McGowan PO, Sasaki A, D'Alessio AC, Dymov S, Labonté B, Szyf M, et al. Epigenetic regulation of the glucocorticoid receptor in human brain associates with childhood abuse. Nat Neurosci. (2009) 12(3):342–8. doi: 10.1038/nn.2270
105. Raison CL, Miller AH. When not enough is too much: the role of insufficient glucocorticoid signaling in the pathophysiology of stress-related disorders. Am J Psychiatry. (2003) 160:1554–65. doi: 10.1176/appi.ajp.160.9.1554
106. Pandey GN, Rizavi HS, Ren X, Dwivedi Y, Palkovits M. Region-specific alterations in glucocorticoid receptor expression in the postmortem brain of teenage suicide victims. Psychoneuroendocrinology. (2013) 38:2628–39. doi: 10.1016/j.psyneuen.2013.06.020
107. Demirkan A, Lahti J, Direk N, Viktorin A, Lunetta KL, Terracciano A, et al. Somatic, positive and negative domains of the Center for Epidemiological Studies Depression (CES-D) scale: a meta-analysis of genome-wide association studies. psychol Med. (2016) 46:1613–23. doi: 10.1017/S0033291715002081
108. Srinivasan V, Smits M, Spence W, Lowe AD, Kayumov L, Pandi-Perumal SR, et al. Melatonin in mood disorders. World J Biol Psychiatry. (2006) 7:138–51. doi: 10.1080/15622970600571822
109. Sandyk R, Awerbuch GI. Nocturnal melatonin secretion in suicidal patients with multiple sclerosis. Int J Neurosci. (1993) 71:173–82. doi: 10.3109/00207459309000602
110. Won E, Na K-S, Kim Y-K. Associations between melatonin, neuroinflammation, and brain alterations in depression. Int J Mol Sci. (2021) 23(1):305. doi: 10.3390/ijms23010305
111. Moreno FA, Parkinson D, Palmer C, Castro WL, Misiaszek J, El Khoury A, et al. CSF neurochemicals during tryptophan depletion in individuals with remitted depression and healthy controls. Eur neuropsychopharmacology: J Eur Coll Neuropsychopharmacol. (2010) 20:18–24. doi: 10.1016/j.euroneuro.2009.10.003
112. Capuron L, Gumnick JF, Musselman DL, Lawson DH, Reemsnyder A, Nemeroff CB, et al. Neurobehavioral effects of interferon-alpha in cancer patients: phenomenology and paroxetine responsiveness of symptom dimensions. Neuropsychopharmacology: Off Publ Am Coll Neuropsychopharmacol. (2002) 26:643–52. doi: 10.1016/S0893-133X(01)00407-9
113. Kohl C, Walch T, Huber R, Kemmler G, Neurauter G, Fuchs D, et al. Measurement of tryptophan, kynurenine and neopterin in women with and without postpartum blues. J Affect Disord. (2005) 86:135–42. doi: 10.1016/j.jad.2004.12.013
114. Raison CL, Dantzer R, Kelley KW, Lawson MA, Woolwine BJ, Vogt G, et al. CSF concentrations of brain tryptophan and kynurenines during immune stimulation with IFN-alpha: relationship to CNS immune responses and depression. Mol Psychiatry. (2010) 15:393–403. doi: 10.1038/mp.2009.116
115. Meier TB, Drevets WC, Wurfel BE, Ford BN, Morris HM, Victor TA, et al. Relationship between neurotoxic kynurenine metabolites and reductions in right medial prefrontal cortical thickness in major depressive disorder. Brain behavior Immun. (2016) 53:39–48. doi: 10.1016/j.bbi.2015.11.003
116. Lugo-Huitrón R, Blanco-Ayala T, Ugalde-Muñiz P, Carrillo-Mora P, Pedraza-Chaverrí J, Silva-Adaya D, et al. On the antioxidant properties of kynurenic acid: free radical scavenging activity and inhibition of oxidative stress. Neurotoxicology teratology. (2011) 33:538–47. doi: 10.1016/j.ntt.2011.07.002
117. Steiner J, Walter M, Gos T, Guillemin GJ, Bernstein H-G, Sarnyai Z, et al. Severe depression is associated with increased microglial quinolinic acid in subregions of the anterior cingulate gyrus: evidence for an immune-modulated glutamatergic neurotransmission? J Neuroinflamm. (2011) 8:94–4. doi: 10.1186/1742-2094-8-94
118. Asberg M. Neurotransmitters and suicidal behavior. evidence cerebrospinal fluid Stud Ann New York Acad Sci. (1997) 836:158–81. doi: 10.1111/j.1749-6632.1997.tb52359.x
119. Bay-Richter C, Linderholm KR, Lim CK, Samuelsson M, Träskman-Bendz L, Guillemin GJ, et al. A role for inflammatory metabolites as modulators of the glutamate N-methyl-d-aspartate receptor in depression and suicidality. Brain Behav Immun. (2015) 43:110–7. doi: 10.1016/j.bbi.2014.07.012
120. Brundin L, Sellgren CM, Lim CK, Grit J, Pålsson E, Landén M, et al. An enzyme in the kynurenine pathway that governs vulnerability to suicidal behavior by regulating excitotoxicity and neuroinflammation. Trans Psychiatry. (2016) 6:e865. doi: 10.1038/tp.2016.133
121. Sublette ME, Galfalvy HC, Fuchs D, Lapidus M, Grunebaum MF, Oquendo MA, et al. Plasma kynurenine levels are elevated in suicide attempters with major depressive disorder. Brain behavior Immun. (2011) 25:1272–8. doi: 10.1016/j.bbi.2011.05.002
122. Szebeni A, Szebeni K, DiPeri TP, Johnson LA, Stockmeier CA, Crawford JD, et al. Elevated DNA oxidation and DNA repair enzyme expression in brain white matter in major depressive disorder. Int J Neuropsychopharmacol. (2017) 20:363–73. doi: 10.1093/ijnp/pyw114
123. Jiménez-Fernández S, Gurpegui M, Garrote-Rojas D, Gutiérrez-Rojas L, Carretero MD, Correll CU. Oxidative stress parameters and antioxidants in adults with unipolar or bipolar depression versus healthy controls: Systematic review and meta-analysis. J Affect Disord. (2022) 314:211–21. doi: 10.1016/j.jad.2022.07.015
124. Vargas HO, Nunes SOV, Pizzo de Castro M, Bortolasci CC, Sabbatini Barbosa D, Kaminami Morimoto H, et al. Oxidative stress and lowered total antioxidant status are associated with a history of suicide attempts. J Affect Disord. (2013) 150:923–30. doi: 10.1016/j.jad.2013.05.016
125. Danese A, Pariante CM, Caspi A, Taylor A, Poulton R. Childhood maltreatment predicts adult inflammation in a life-course study. Proc Natl Acad Sci United States America. (2007) 104:1319–24. doi: 10.1073/pnas.0610362104
126. Rybka J, Kędziora-Kornatowska K, Banaś-Leżańska P, Majsterek I, Carvalho LA, Cattaneo A, et al. Interplay between the pro-oxidant and antioxidant systems and proinflammatory cytokine levels, in relation to iron metabolism and the erythron in depression. Free Radical Biol Med. (2013) 63:187–94. doi: 10.1016/j.freeradbiomed.2013.05.019
127. Jiang H, Ling Z, Zhang Y, Mao H, Ma Z, Yin Y, et al. Altered fecal microbiota composition in patients with major depressive disorder. Brain behavior Immun. (2015) 48:186–94. doi: 10.1016/j.bbi.2015.03.016
128. Miranda O, Fan P, Qi X, Yu Z, Ying J, Wang H, et al. DeepBiomarker: identifying important lab tests from electronic medical records for the prediction of suicide-related events among PTSD patients. J personalized Med. (2022) 12(4):524. doi: 10.3390/jpm12040524
129. McGuinness AJ, Davis JA, Dawson SL, Loughman A, Collier F, O'Hely M, et al. A systematic review of gut microbiota composition in observational studies of major depressive disorder, bipolar disorder and schizophrenia. Molelcular Psychiatry. (2022) 27:1920–35. doi: 10.1038/s41380-022-01456-3
130. Simpson CA, Adler C, du Plessis MR, Landau ER, Dashper SG, Reynolds EC, et al. Oral microbiome composition, but not diversity, is associated with adolescent anxiety and depression symptoms. Physiol Behav. (2020) 226:113126. doi: 10.1016/j.physbeh.2020.113126
131. Wingfield B, Lapsley C, McDowell A, Miliotis G, McLafferty M, O'Neill SM, et al. Variations in the oral microbiome are associated with depression in young adults. Sci Rep. (2021) 11:15009. doi: 10.1038/s41598-021-94498-6
132. Maes M, Vasupanrajit A, Jirakran K, Klomkliew P, Chanchaem P, Tunvirachaisakul C, et al. Adverse childhood experiences and reoccurrence of illness impact the gut microbiome, which affects suicidal behaviours and the phenome of major depression: towards enterotypic phenotypes. Acta neuropsychiatrica. (2023) 13:1–18. doi: 10.1017/neu.2023.21
133. Ahrens AP, Sanchez-Padilla DE, Drew JC, Oli MW, Roesch LFW, Triplett EW. Saliva microbiome, dietary, and genetic markers are associated with suicidal ideation in university students. Sci Rep. (2022) 12:14306. doi: 10.1038/s41598-022-18020-2
134. Lengvenyte A, Strumila R, Maimoun L, Seneque M, Olié E, Lefebvre P, et al. A specific association between laxative misuse and suicidal behaviours in patients with anorexia nervosa and bulimia nervosa. Eating weight Disord. (2022) 27:307–15. doi: 10.1007/s40519-021-01180-x
135. Ohlsson L, Gustafsson A, Lavant E, Suneson K, Brundin L, Westrin Å, et al. Leaky gut biomarkers in depression and suicidal behavior. Acta psychiatrica scandinavia. (2019) 139:185–93. doi: 10.1111/acps.2019.139.issue-2
136. Madison AA, Andridge R, Kantaras AH, Renna ME, Bennett JM, Alfano CM, et al. Depression, inflammation, and intestinal permeability: associations with subjective and objective cognitive functioning throughout breast cancer survivorship. Cancers (Basel). (2023) 15:4414. doi: 10.3390/cancers15174414
137. Rudzki L, Maes M. The microbiota-gut-immune-glia (MGIG) axis in major depression. Mol Neurobiol. (2020) 57:4269–95. doi: 10.1007/s12035-020-01961-y
138. Skonieczna-Żydecka K, Grochans E, Maciejewska D, Szkup M, Schneider-Matyka D, Jurczak A, et al. Faecal short chain fatty acids profile is changed in polish depressive women. Nutrients. (2018) 10(12):1939. doi: 10.3390/nu10121939
139. Kim IB, Park SC, Kim YK. Microbiota-gut-brain axis in major depression: A new therapeutic approach. Adv Exp Med Biol. (2023) 1411:209–24. doi: 10.1007/978-981-19-7376-5
140. Schwarz MJ, Dehning S, Douhe A, Cerovecki A, Goldstein-Müller B, Spellmann I, et al. The cyclooxygenase-2 inhibitor celecoxib has therapeutic effects in major depression: results of a double-blind, randomized, placebo controlled, add-on pilot study to reboxetine. Mol Psychiatry. (2006) 11:680–4. doi: 10.1038/sj.mp.4001805
141. Akhondzadeh S, Jafari S, Raisi F, Nasehi AA, Ghoreishi A, Salehi B, et al. Clinical trial of adjunctive celecoxib treatment in patients with major depression: a double blind and placebo controlled trial. Depression Anxiety. (2009) 26:607–11. doi: 10.1002/da.20589
142. Jafari S, Ashrafizadeh SG, Zeinoddini A, Rasoulinejad M, Entezari P, Seddighi S, et al. Celecoxib for the treatment of mild-to-moderate depression due to acute brucellosis: a double-blind, placebo-controlled, randomized trial. J Clin Pharm Ther. (2015) 40:441–6. doi: 10.1111/jcpt.12287
143. Alamdarsaravi M, Ghajar A, Noorbala AA, Arbabi M, Emami A, Shahei F, et al. Efficacy and safety of celecoxib monotherapy for mild to moderate depression in patients with colorectal cancer: A randomized double-blind, placebo controlled trial. Psychiatry Res. (2017) 255:59–65. doi: 10.1016/j.psychres.2017.05.029
144. DeBattista C, Posener JA, Kalehzan BM, Schatzberg AF. Acute antidepressant effects of intravenous hydrocortisone and CRH in depressed patients: a double-blind, placebo-controlled study. Am J Psychiatry. (2000) 157:1334–7. doi: 10.1176/appi.ajp.157.8.1334
145. Arana GW, Santos AB, Laraia MT, McLeod-Bryant S, Beale MD, Rames LJ, et al. Dexamethasone for the treatment of depression: a randomized, placebo-controlled, double-blind trial. Am J Psychiatry. (1995) 152:265–7. doi: 10.1176/ajp.152.2.265
146. Emadi-Kouchak H, Mohammadinejad P, Asadollahi-Amin A, Rasoulinejad M, Zeinoddini A, Yalda A, et al. Therapeutic effects of minocycline on mild-to-moderate depression in HIV patients: a double-blind, placebo-controlled, randomized trial. Int Clin Psychopharmacol. (2016) 31:20–6. doi: 10.1097/YIC.0000000000000098
147. Husain MI, Chaudhry IB, Husain N, Khoso AB, Rahman RR, Hamirani MM, et al. Minocycline as an adjunct for treatment-resistant depressive symptoms: A pilot randomised placebo-controlled trial. J Psychopharmacol. (2017) 31:1166–75. doi: 10.1177/0269881117724352
148. Köhler-Forsberg O, Lydholm C N, Hjorthøj C, Nordentoft M, Mors O, Benros ME. Efficacy of anti-inflammatory treatment on major depressive disorder or depressive symptoms: meta-analysis of clinical trials. Acta psychiatrica scandinavica. (2019) 139:404–19. doi: 10.1111/acps.13016
149. Sun Y, Wang D, Salvadore G, Hsu B, Curran M, Casper C, et al. The effects of interleukin-6 neutralizing antibodies on symptoms of depressed mood and anhedonia in patients with rheumatoid arthritis and multicentric Castleman's disease. Brain behaviors immunity. (2017) 66:156–64. doi: 10.1016/j.bbi.2017.06.014
150. Langley RG, Feldman SR, Han C, Schenkel B, Szapary P, Hsu M-C, et al. Ustekinumab significantly improves symptoms of anxiety, depression, and skin-related quality of life in patients with moderate-to-severe psoriasis: Results from a randomized, double-blind, placebo-controlled phase III trial. J Am Acad Dermatol. (2010) 63:457–65. doi: 10.1016/j.jaad.2009.09.014
151. Griffiths CEM, Fava M, Miller AH, Russell J, Ball SG, Xu W, et al. Impact of ixekizumab treatment on depressive symptoms and systemic inflammation in patients with moderate-to-severe psoriasis: an integrated analysis of three phase 3 clinical studies. Psychotheraryand psychosomatics. (2017) 86:260–7. doi: 10.1159/000479163
152. Loftus EV, Feagan BG, Colombel JF, Rubin DT, Wu EQ, Yu AP, et al. Effects of adalimumab maintenance therapy on health-related quality of life of patients with Crohn's disease: patient-reported outcomes of the CHARM trial. Am J gastroenterology. (2008) 103:3132–41. doi: 10.1111/j.1572-0241.2008.02175.x
153. Kekow J, Moots R, Khandker R, Melin J, Freundlich B, Singh A. Improvements in patient-reported outcomes, symptoms of depression and anxiety, and their association with clinical remission among patients with moderate-to-severe active early rheumatoid arthritis. Rheumatol (Oxford). (2011) 50:401–9. doi: 10.1093/rheumatology/keq327
154. Menter A, Augustin M, Signorovitch J, Yu AP, Wu EQ, Gupta SR, et al. The effect of adalimumab on reducing depression symptoms in patients with moderate to severe psoriasis: a randomized clinical trial. J Am Acad Dermatol. (2010) 62:812–8. doi: 10.1016/j.jaad.2009.07.022
155. Tyring S, Bagel J, Lynde C, Klekotka P, Thompson EH, Gandra SR, et al. Patient-reported outcomes in moderate-to-severe plaque psoriasis with scalp involvement: results from a randomized, double-blind, placebo-controlled study of etanercept. J Eur Acad Dermatol Venereol. (2013) 27:125–8. doi: 10.1111/j.1468-3083.2011.04394.x
156. Tian P, Chen Y, Zhu H, Wang L, Qian X, Zou R, et al. Bifidobacterium breve CCFM1025 attenuates major depression disorder via regulating gut microbiome and tryptophan metabolism: A randomized clinical trial. Brain behaviors Immun. (2022) 100:233–41. doi: 10.1016/j.bbi.2021.11.023
157. Akkasheh G, Kashani-Poor Z, Tajabadi-Ebrahimi M, Jafari P, Akbari H, Taghizadeh M, et al. Clinical and metabolic response to probiotic administration in patients with major depressive disorder: A randomized, double-blind, placebo-controlled trial. Nutr (Burbank Los Angeles County Calif.). (2016) 32:315–20. doi: 10.1016/j.nut.2015.09.003
158. Ullah H, Di Minno A, Esposito C, El-Seedi HR, Khalifa SAM, Baldi A, et al. Efficacy of a food supplement based on S-adenosyl methionine and probiotic strains in subjects with subthreshold depression and mild-to-moderate depression: A monocentric, randomized, cross-over, double-blind, placebo-controlled clinical trial. Biomed pharmacotherapy. (2022) 156:113930. doi: 10.1016/j.biopha.2022.113930
159. Kazemi A, Noorbala AA, Azam K, Eskandari MH, Djafarian K. Effect of probiotic and prebiotic vs placebo on psychological outcomes in patients with major depressive disorder: A randomized clinical trial. Clin Nutr. (2019) 38:522–8. doi: 10.1016/j.clnu.2018.04.010
160. Ben Othman R, Ben Amor N, Mahjoub F, Berriche O, El Ghali C, Gamoudi A, et al. A clinical trial about effects of prebiotic and probiotic supplementation on weight loss, psychological profile and metabolic parameters in obese subjects. Endocrinology diabetes Metab. (2023) 6:e402. doi: 10.1002/edm2.402
161. Pompili M, Serafini G, Innamorati M, Möller-Leimkühler AM, Giupponi G, Girardi P, et al. The hypothalamic-pituitary-adrenal axis and serotonin abnormalities: a selective overview for the implications of suicide prevention. Eur Arch Psychiatry Clin Neurosci. (2010) 260:583–600. doi: 10.1007/s00406-010-0108-z
162. Garzón C, Guerrero JM, Aramburu O, Guzmán T. Effect of melatonin administration on sleep, behavioral disorders and hypnotic drug discontinuation in the elderly: a randomized, double-blind, placebo-controlled study. Aging Clin Exp Res. (2009) 21:38–42. doi: 10.1007/BF03324897
163. Dinan K, Dinan T. Antibiotics and mental health: The good, the bad and the ugly. J Internal Med. (2022) 292:858–69. doi: 10.1111/joim.v292.6
164. Lebwohl MG, Papp KA, Marangell LB, Koo J, Blauvelt A, Gooderham M, et al. Psychiatric adverse events during treatment with brodalumab: Analysis of psoriasis clinical trials. J Am Acad Dermatol. (2018) 78:81–89.e5. doi: 10.1016/j.jaad.2017.08.024
165. Høier NK, Madsen T, Spira AP, Hawton K, Jennum P, Nordentoft M, et al. Associations between treatment with melatonin and suicidal behavior: a nationwide cohort study. J Clin sleep medicine: JCSM: Off Publ Am Acad Sleep Med. (2022) 18:2451–8. doi: 10.5664/jcsm.10118
166. Costanza A, Placenti V, Amerio A, Aguglia A, Serafini G, Amore M, et al. Chloroquine/hydroxychloroquine use and suicide risk: hypotheses for confluent etiopathogenetic mechanisms? Behav Sci (Basel). (2021) 11(11):154. doi: 10.3390/bs11110154
167. Goldberg SB, Pace BT, Nicholas CR, Raison CL, Hutson PR. The experimental effects of psilocybin on symptoms of anxiety and depression: A meta-analysis. Psychiatry Res. (2020) 284:112749–9. doi: 10.1016/j.psychres.2020.112749
Keywords: suicide, suicidal ideation, suicidal behavior, inflammation, immune system, neuroendocrine, host-microbe deregulation, clinical subtypes
Citation: Costanza A, Amerio A, Aguglia A, Magnani L, Parise A, Nguyen KD, Berardelli I, Pompili M, Amore M and Serafini G (2024) Inflammatory pathology in depression and suicide: a mechanistic distillation of clinical correlates. Front. Immunol. 15:1479471. doi: 10.3389/fimmu.2024.1479471
Received: 12 August 2024; Accepted: 12 December 2024;
Published: 23 December 2024.
Edited by:
Jason C. O’Connor, The University of Texas Health Science Center at San Antonio, United StatesReviewed by:
Ivana Kawikova, National Institute of Mental Health (Czechia), CzechiaJimin Guo, Beijing University of Chemical Technology, China
Copyright © 2024 Costanza, Amerio, Aguglia, Magnani, Parise, Nguyen, Berardelli, Pompili, Amore and Serafini. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Alessandra Costanza, YWxlc3NhbmRyYS5jb3N0YW56YUB1bmlnZS5jaA==
 Alessandra Costanza
Alessandra Costanza Andrea Amerio
Andrea Amerio Andrea Aguglia
Andrea Aguglia Luca Magnani
Luca Magnani Alberto Parise
Alberto Parise Khoa D. Nguyen
Khoa D. Nguyen Isabella Berardelli
Isabella Berardelli Maurizio Pompili
Maurizio Pompili Mario Amore
Mario Amore Gianluca Serafini
Gianluca Serafini