
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Immunol. , 12 November 2024
Sec. Viral Immunology
Volume 15 - 2024 | https://doi.org/10.3389/fimmu.2024.1472189
 Yaning Zhuo1†
Yaning Zhuo1† Zhaojun Lu2†
Zhaojun Lu2† Xuechao Zhang2
Xuechao Zhang2 Xiaoping Zhang2
Xiaoping Zhang2 Yingying Yang2
Yingying Yang2 Jiayin Han2
Jiayin Han2 Jian Du2
Jian Du2 Yuyang Xu2
Yuyang Xu2 Yan Liu2*
Yan Liu2* Chuanxi Fu3*
Chuanxi Fu3*Objectives: To gain a comprehensive understanding of rubella seroprevalence in the healthy population in China and to offer data-driven support for the goal of rubella elimination.
Methods: CNKI, Wanfang database, VIP database, CBM, PubMed, web of Science, and Embase databases were searched to collect studies reporting the positive rate of rubella antibody among the Chinese healthy populations between 2001 and 2022. We conducted a meta-analysis using R language, and data were combined using random effects model.
Results: A total of 97 studies were included, encompassing a sample size of 103,018. Meta-analysis showed that the overall prevalence of rubella antibody positivity in the Chinese healthy population was 77.29% (95% CI: 75.26-79.33). The prevalence of rubella antibody varied significantly based on age and vaccination status. Among the age groups studied, the <1-year-old group exhibited the lowest positivity rate for rubella antibody at 47.87% (95% CI: 41.53-54.21),while the ≥50 years old group showed the highest positivity rate at 85.43% (95% CI: 81.01-89.85); individuals with a history of vaccination demonstrated a higher antibody positivity rate compared to those without vaccination history.
Conclusions: The prevalence of rubella antibody in healthy Chinese population is relatively low. In order to establish a solid immunity threshold levels, it requires conducting timely immunization programs on key groups such as middle school students and the women of childbearing age on the basis of ensuring a high level of rubella-containing-vaccines (RCV) coverage, so as to achieve the goal of eliminating rubella.
Systematic review registration: https://www.crd.york.ac.uk/PROSPERO/, identifier CRD42024607949.
Rubella is an acute infectious disease caused by the rubella virus, primarily transmitted through respiratory droplets and direct contact. The main clinical manifestations of rubella include fever, a generalized erythematous maculopapular rash, and lymphadenopathy. Complications may include arthralgia, arthritis, thrombocytopenic purpura, and encephalitis (1). While the general clinical symptoms of rubella are usually mild, the infection with the rubella virus during early pregnancy can lead to adverse outcomes such as spontaneous abortion, stillbirth, or congenital rubella syndrome (CRS) in newborns. Currently, there is no specific clinical treatment for CRS. The World Health Organization (WHO) estimates that approximately 100,000 cases of CRS occur worldwide annually, posing significant challenges to the advancement of public health. However, these adverse consequences of rubella can be prevented and controlled through the administration of RCV, potentially leading to eventual elimination of rubella (2).
In 1993, China introduced the rubella vaccine (RV); however, its availability for vaccination is limited to certain regions (3). In 2008, China included measles-rubella vaccine (MR) and measles-mumps-rubella vaccine (MMR) into the national expanded program on immunization, implementing a two-dose immunization schedule for eligible children (4). The coverage of RCV immunization has steadily increased and has consistently remained above 95% since 2012. The incidence of rubella in China decreased from 9.11/100,000 in 2008 to 0.12/100,000 in 2017. Nevertheless, there was a notable increase in rubella incidence during the years 2018 to 2019 (5). In this study, we employed meta-analysis to investigate the nationwide rubella seroprevalence utilizing data from rubella antibody surveillance among healthy populations conducted in various regions of China over multiple years, aiming to enhance rubella immunization strategies.
Literature to be included in the meta-analysis was sought in the Chinese data base and English data base respectively. Chinese data bases included CNKI, Wanfang database, VIP database and CBM; English data bases included PubMed, Web of Science, Embase. The searching terms were (Rubella OR Rubellas OR Three Day Measles OR Three Day Measle OR German Measles) AND (Antibody positive rate OR seropositive OR seropositivity OR serosurvey OR serosurveillance OR seroprevalence) AND (Enzyme-linked immunosorbent assay OR ELISA) AND (China OR Chinese). The search period for this study spanned from the inception of the database up to December 31, 2023.
①The study population consisted of physically healthy individuals; ②Seroprevalence were examined using enzyme-linked immunosorbent assay (ELISA), values≥20 IU/ml were considered positive, values of 10-20 IU/ml were considered equivocal, and values<10 IU/ml were considered negative; ③The positive rates were either directly reported or had data available for calculating the positivity rates.
Two investigators independently evaluated the abstracts of the literature independently and screened them according to the literature selection and exclusion. Then read the full articles, which were scored based on the quality assessment criteria. When encountering differences, the investigators can consult with each other or seek resolution from a third investigator to reach a final decision regarding inclusion. After completing the literature screening process, data including the first author, publication year, age, gender, survey time, survey location, number of positive antibody individuals, sample size, antibody positive rate and immunization history were extracted from the articles.
The literature using the assessment criteria of the cross-sectional studies which recommended by Joanna Briggs institute (JBI) to assess their quality. The quality assessment tool includes 9 items. The specific content of each item is as follows: ①Does the sample represent the target population?②Is the sampling method appropriate for the study population? ③Is the sample size sufficient? (At least≥200 ) ④Are the study subjects and research settings described in detail? ⑤Do the subgroups in the sample have similar response rates to ensure sufficient coverage during data analysis? ⑥Is an effective method used to identify the health issue? ⑦Are standard and reliable methods used to assess the health issue in all study subjects? ⑧Is the data analysis method appropriate? ⑨Are the response rates sufficient? Are appropriate methods used to address low response rates?
The evaluation results are defined based on four dimensions: "yes," "no," "unclear," and "not applicable." A score of 1 is assigned for "yes," while all other responses receive a score of 0. The score below 5 is considered low-quality and excluded from the analysis (6, 7).
①The study population included patients with rubella, suspected rubella cases, or with additional symptoms or diseases; ②The timing and method of seroprevalence testing of the study population are unspecified; ③The types of literature are conference papers, clinical trial studies, animal experiments, discussions on the prevalence of the disease and so on; ④The objective of the literature is to explore the effectiveness of the vaccine itself, such as the antibody conversion rate; ⑤The literature has a low-quality assessment score.
The data analysis in this study utilized the "meta" package in R4.3.2 for conducting meta-analysis. The positive rate of the antibody served as the statistical analysis index, with the corresponding 95% confidence interval (CI) calculated according. We evaluate the heterogeneity among studies using the I2. If I2<50%, the heterogeneity among the studies was low, and a fixed-effects model was used for combining. Conversely, the random effects model was used. The Egger's test combined with a funnel plot was used to evaluate publication bias, and sensitivity analysis was conducted using a one-by-one exclusion approach. Two-sided tests will be performed with a significance level of α=0.05.
After conducting an initial database search using the specified search terms, a total of 1902 articles identified. Around 566 articles were removed due to the duplication. Following the inclusion and exclusion criteria, 97 articles were ultimately selected (Figure 1). Among these, 94 were written in Chinese while 3 were in English.
The 97 included papers are all cross-sectional studies published between 2003 and 2023, encompassing seven geographical regions in China. The maximum sample size of the literature was 11013 and the minimum sample size was 197. The literature quality scores ranged from 5 to 8, with the highest score being 8 and the lowest score being 5 (Table 1).
A total of 97 papers reported the seroprevalence of rubella in the population. The study encompassing 103,018 individuals, among whom 79,091 tested positive for antibodies. The highest positive rate was 98.20% while the lowest was 45.90%. Based on the random-effects model, the estimated positive rate of rubella antibody in the healthy Chinese population was 77.36% (95%CI:75.30-79.42,I2 = 98.50%).
A total of 96 papers were included in the analysis, reporting rubella seroprevalence across different ages groups. After integration of the data by age group that was previously set, the stratified comparison revealed a significant difference in the positive rate of rubella antibodies among different age groups (χ2 = 121.76,P<0.001). The<1-year-old group exhibited the lowest positive rate at 47.71% (95%CI:41.25-54.16), while the ≥50-years-old group showed the highest positive rate at 85.43% (95%CI:81.01-89.85) (Table 2).
A total of 46 papers reported the seroprevalence of rubella across genders. The analysis revealed the positive rate of rubella antibody of 78.28% (95%CI:74.95-81.62) in males and 79.18% (95%CI:76.10-82.26) in females. There was no significant difference observed in the positive rate of rubella antibodies between the different gender groups (χ2 = 0.15,P=0.70) (Table 2).
A total of 15 papers reported the seroprevalence of rubella in different districts. The results showed that the positive rate of rubella antibody was 79.50% (95%CI:73.49-85.50) in the urban population and 78.12% (95%CI:71.75-84.49) in the rural population. There was no significant difference in the positive rate of rubella antibodies in different district groups (χ2 = 0.10, P=0.76) (Table 2).
A total of 13 papers reported the seroprevalence of rubella in different registrations. The results showed that the positive rate of rubella antibody was 79.45% (95%CI:73.25-85.64) in permanent population and 78.12% (95%CI:71.75-84.49) in migrant population. No significant difference was found in the positive rates of rubella antibodies between the different registration groups (χ2 = 0.24, P=0.63) (Table 2).
The Chinese provinces were categorized into seven regions according to their geographical location. The analysis revealed no significant difference in the positive rate of rubella antibody among different regions (χ2 = 6.99,P=0.32). The lowest positive rate of rubella antibody was 74.01%(95%CI:68.75-79.27) in the southwest region, while the highest positive rate was 82.52%(95%CI:77.55-87.48) in the northeast region (Table 2).
There was a significant difference observed among the different immunization history groups (χ2 = 8.2, P=0.02). The lowest positive rate of rubella antibody was 58.23% (95%CI:47.2-69.25) in the population with no RCV vaccination history, and the highest positive rate was 80.45% (95%CI:76.36-84.55) in the population with histories of receiving at least 2 doses of RCV (Table 2).
After integration of the data by the groups of study year that previously set, the results of integration showed that the lowest rubella antibody positive rate was 70.42% (95%CI:62.17-79.56) during 2001-2008, while the highest value was 78.17% (95%CI:74.28-82.05) during 2009-2013. There was no significant difference in the positive rate of rubella antibodies among different registration groups (χ2 = 3.26,P=0.35) (Table 2).
By conducting sensitivity analysis involving the stepwise exclusion of included studies, the results remained consistent with the original findings, indicating the stability of the meta-analysis results. The publication bias was not found in this Meta-analysis, which was confirmed by using Egger's test (P=0.08) and shown in Figure 2. (Each point represents the included article).
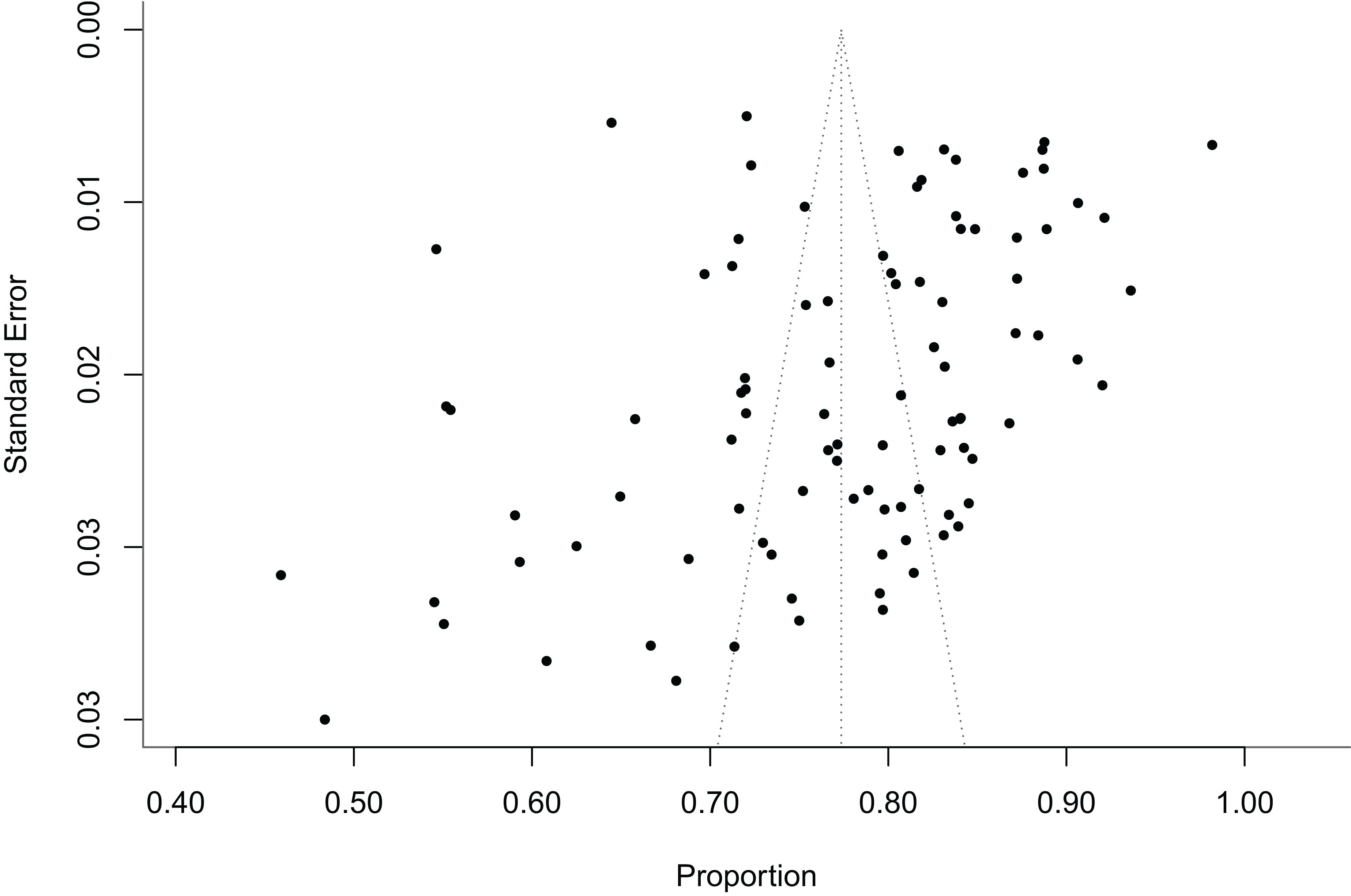
Figure 2. The funnel plots assessing the publication bias in the study of rubella antibody levels in the healthy Chinese population.
In 2012, WHO established the goal of rubella elimination as part of the "Global Measles and Rubella Strategic Framework 2012-2020". In 2015, the WHO Region of the Americas verified that 35 countries and regions within that region were eliminated rubella. The World Health Organization's Western Pacific Region (WPRO), to which China belongs, set a goal for rubella elimination in 2014 (3). As of 2021, several WPRO member countries and regions, including Australia, Brunei, New Zealand, South Korea, Macau, and Hong Kong, have declared rubella elimination (105, 106). In the “Global Measles and rubella Strategic Framework 2021-2030” issued by WHO in 2021, it is pointed out that strengthening the control and elimination of rubella can be combined with measles. The framework aims to achieve and maintain regional elimination of measles and rubella by 2030 (107). While seroepidemiological survey data can reflect the epidemiological characteristics of rubella, routine monitoring of rubella seroprevalence has not been conducted in China. It is resulting in a lack of comprehensive and dynamic control and understanding. This paper conducted a meta-analysis to explore the level of rubella antibody in healthy people in China from the whole to the extraction of relevant influencing factors.
The WHO has indicated that achieving the rubella seroprevalence of over 83% to 85% is necessary to establish robust herd immunity (80). Our study showed that the rubella seroprevalence in healthy people in China was 77.36%, lower than the standard recommended by WHO. Weak immunity threshold levels can lead to an increased incidence of rubella in high-risk populations and an increased risk of CRS in children.
To enhance rubella prevention and control efforts, RCV was incorporated into the immunization program in China in 2008, and the positive rate of rubella antibody has increased significantly since 2009. From this study, it can be seen that when there was no large-scale introduction of RCV, the rubella seroprevalence can be as low as 45.9% (9). The introduction of the vaccine has significantly increased the rubella seroprevalence in the population. It was found that the rubella seroprevalence increased with the increase in vaccination dose, which was consistent with the results of Wang Jun et al. (73). Similarly, a study in Beijing on the detection of measles and rubella seroprevalence in children aged 18-24 months after multiple doses of the MMR vaccine found that the antibody positive rate and antibody Geometric mean concentration (GMC) increased significantly after multiple doses. The positive rate of rubella antibody increased from 97.22% to 100%, and the GMC reached (283.52 ± 90.83)IU/ml (108). Although a single dose of MMR can obtain more than 95% long-term immunity (109), the annual decline rate of seroprevalence of a single dose vaccine is 0.014 (0.012-0.017), showing an exponential attenuation. After receiving two doses of MMR, the decline rate of seroprevalence decreased to 0.012 (0.010-0.014) (110). Multiple doses of vaccine, such as two or more, can enhance the seroprevalence and promote immune persistence in healthy individuals.
Several factors influence the level of rubella antibody. Based on the findings of this study, age and vaccination history emerge as significant factors that impact the level of rubella antibody. The modified immunization schedule has significantly contributed to the variations in rubella seroprevalence across different age groups.
The rubella immunization schedule in China involves administering the RCV at 8 months and 18 months of ages, respectively (111). The majority of children aged 1-4 years have a history of RCV, leading to a higher positive rate of antibodies. Conversely, children below 8 months of age have not yet reached the age for RCV and depend on maternally-derived antibodies. Additionally, Zhu Q et al. showed that newborn measles and rubella antibody levels increased with the increase of maternal antibody levels (118). However, since the mothers of infants included in this analysis were born in the period when rubella vaccine was not widely administered, fewer were vaccinated, most of which were immune after tacit infection with rubella virus (119). Consequently, the level of maternal antibodies has decreased, which is associated with the low antibody positivity rate observed in children under 1-year-old. Since the current RCV program primarily focuses on children, the positive rate of rubella antibody starts to decrease after the age of 5. Studies have shown that individual antibody levels decrease over time in the absence of widespread virus transmission (121). This finding may be one of the reasons why antibody levels drop after age of 5. The relevant studies have demonstrated that the risk of rubella will increase with time (112), and the use of rubella vaccine in children cannot reduce the incidence of rubella in adolescents and adults (113). Currently, the main affected population for rubella in China is concentrated among middle school students (3), and in the outbreak of rubella in 2018-2019, the age of onset was concentrated in the 10-29 age group (105). In response to this phenomenon, Zhejiang Province implemented intensified RCV immunization for the third-year middle school students. After enhanced immunization of 15-19 age group, the positive rate of rubella antibody and GMC were significantly higher than those of 10-14 age group (114). Therefore, administering RCV to rubella-susceptible populations, such as adolescents and adults who failed to respond to the primary vaccination, can compensate for the immunological gap created by basic childhood immunity (3, 117). This could prevent and control adult rubella epidemics (114). Individuals aged 35 and above, who were born before the inclusion of RCV in the national expanded immunization program have had more opportunities for exposure to infectious sources, which has led to higher levels of naturally acquired antibodies. According to the data of a study on the introduction of RCV in the immunization program, the annual incidence of rubella decreased from 91.09 cases per million to 3.31 cases per million after the vaccine was widely used. This means that most people at that time had a higher risk of exposure to rubella, which may be one of the reasons for the high positive rate of rubella in older age groups (120). It may be one of the reasons for the high positive rate of rubella in older age groups.
There was no statistically significant difference in rubella seroprevalence between genders, which is consistent with the majority of findings in the Chinese literature (29, 71, 94). Our study with age-specific subgroup analysis revealed a relatively low prevalence of rubella seropositivity among women of reproductive age. It may lead to an increased risk of CRS infection, and there is a need to strengthen the immunity threshold levels in this age group (115). The reduction of CRS occurrence in the United States was achieved by recommending one dose of MMR for adults, based on the implementation of two doses of MMR for children (115). Similarly, a 75% reduction in the number of cases of CRS in schoolgirls vaccinated with the RCV was achieved in the United Kingdom (116). These findings suggest that women of childbearing age who are either unvaccinated or do not have sufficient evidence of rubella-specific immunity may benefit from receiving the RCV to boost their seropositive level.
Our study has several limitations. First the included studies were predominantly cross-sectional, which are susceptible to measurement bias and non-response bias. Second, some primary studies lacked adequate analysis of study factors, had small sample sizes, or focused on narrow age groups, contributing to increased heterogeneity in the literature. Third, our study adopts the commonly used definition in the literature of antibody positive rate, which is more than 20 IU/ml. However, there are variations in definitions across studies, with some using a threshold of more than 10 IU/ml or lacking a clear definition altogether, potentially leading to non-unique meta-analysis results. In view of these issues, we adopted a strategy of expanding the number of papers and broadening the coverage of time and geographical dimensions to minimize the impact on the results and uphold scientific rigor to a certain extent.
In conclusion, to achieve the goal of rubella elimination, China needs to implement a comprehensive strategy that integrates rubella disease surveillance and serological testing. This approach should be built upon a high vaccination coverage rate for RCV within the immunization program. Furthermore, it is crucial to timely targeted immunization efforts for high-risk groups, such as middle school students and women of childbearing age, to enhance their immunity against rubella. By establishing a robust rubella immunity threshold levels, significant reductions can be achieved in the harm caused by rubella and its associated complications.
The datasets presented in this article are not readily available because you need to send an email request before using this data. Requests to access the datasets should be directed to c21pbGVmb3JldmVyODFAMTI2LmNvbQ==.
YZ: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Resources, Software, Validation, Visualization, Writing – original draft, Writing – review & editing. ZL: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Resources, Software, Validation, Writing – original draft, Writing – review & editing. XCZ: Investigation, Methodology, Writing – review & editing. XPZ: Investigation, Methodology, Writing – review & editing. YY: Writing – review & editing, Data curation, Formal analysis, Software. JH: Data curation, Formal analysis, Software, Writing – review & editing. JD: Formal analysis, Software, Validation, Writing – review & editing. YX: Project administration, Software, Validation, Writing – review & editing. YL: Conceptualization, Supervision, Writing – review & editing. CF: Conceptualization, Supervision, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was supported by Zhejiang Provincial Basic Public Welfare Research Projects (grant number: LGF22H260013).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Winter AK, Moss WJ. Rubella. Lancet (London England). (2022) 399:1336–46. doi: 10.1016/S0140-6736(21)02691-X
2. Lambert N, Strebel P, Orenstein W, Icenogle J, Poland GA. Rubella. Lancet (London England). (2015) 385:2297–307. doi: 10.1016/S0140-6736(14)60539-0
3. Su QR. Study on the supplementary immunization strategy to eliminate measles and rubella in China. China: Chinese Center for Disease Control and Prevention (2018).
4. The National Health Commission of the People's Republic of China. The National Health Commission of the People's Republic of China on the issuance of the implementation plan of the Expanded Programme on lmmunization Vol. 03). China: Gazette of the National Health Commission of the People's Republic of China (2008) p. 17–21.
5. Li YQ, Ma C, Hao LX, Wang FZ, Wen N, Yang H, et al. Epidemiology of rubella in China, 2018-2019. Chin J Vaccines Immunization. (2021) 27:62–6. doi: 10.19914/j.CJVI.2021003
6. Hu YH, Luo XF, Lyu M, Yin DP. A Meta-analysis on varicella-zoster virus seroprevalence in healthy population in China. Chin J Epidemiol. (2021) 09):1650–61. doi: 10.3760/cma.j.cn112338-20210308-00185
7. Li MM, Yuan DF, Liu YX, Liu YB, Wang B. Meta analysis on mumps virus seroprevalence and evaluation of immunization effect in Chinese healthy population. Chin J Epidemiol. (2022) 07):994–1003. doi: 10.3760/cma.j.cn112150-20220402-00313
8. Kezhong A, YJ Z, SC Z, LX F, WP Z, Qi GH. Analysis on measles and rubella seroprevalence among Healthy population in Huangyuan County and Guide County in 2014. J Med Pest Control. (2016) 32:832–4+7. doi: 10.7629/yxdwfz201608003
9. Cai ZK, Pan WY, Yang XH, Zhou Y, Zhang HR. Surveillance of rubella immunity in urban and rural population aged 1-19 years in Fujian Province. Strait J Prev Med. (2003) 9:58. doi: 10.3969/j.issn.1007-2705.2003.04.031
10. Chen JH, Zhang H, Cai XQ. Results Analysis on Monitoring seroprevalence of Rubella among Health Population in Fuzhou City in 2007. Occupation Health. (2009) 25:2201–3. doi: 10.13329/j.cnki.zyyjk.2009.20.031
11. Cao H. Survey on Epidemiological Characteristics and the seroprevalence of Measles, Rubella and Mumps among the Healthy Population. China: Tianjing Medical University (2015).
12. Cao Y, Tian YQ, Yang DM, Kang XL, Zhang RP, Yang F, et al. Surveillance on measles, rubella and mumps seroprevalence and measures for disease prevention of children in Fuling district, Chongqing. Modern Prev Med. (2017) 44:1232–5,47. doi: CNKI:SUN:XDYF.0.2017-07-020
13. Feng YF, Zeng XY. Surveillance and analysis of measles, rubella and varicella lgG seroprevalence in healthy people in Liwan District, Guangzhou City in 2020. Prog Microbiol Immunol. (2021) 49(05):67–70. doi: 10.13309/j.cnki.pmi.2021.05.011
14. Wang HL, Zhang H, Gong HX, Huang LJ, Cheng JB. Monitoring measles, rubella, mumps and varicella seroprevalence in healthy people in Zhoushan. Int J Epidemiol Infect Disease. (2016) 43(1):39–42. doi: 10.3760/cma.j.issn.1673-4149.2016.01.010
15. Zhang H, Huang XX, Cheng JH. Analysis on measles and rubella seroprevalence in migrant population in Fuzhou City, 2007. Chin J Viral Diseases. (2009) 11(5):347–9. doi: 10.16505/j.2095-0136.2009.05.022
16. Gong H, Zhang B, Chen X C. Measles antibody and rubella seroprevalence among healthy population in 2016 in chenghua district in chengdu city. J Prev Med Inf. (2018) 34(05):660–3. doi: CNKI:SUN:YFYX.0.2018-05-029
17. Chen SJ. Analysis of the monitoring results of measles, rubella and mumps seroprevalence in healthy people in a certain area. Health Guide. (2018) 2018:368. doi: 10.3969/j.issn.1006-6845.2018.47.361
18. Chen YW, Jia HM, Miu L. Results Analysis on Monitoring seroprevalence of measles and rubella among Health Population in Fuzhou City in 2019. J Appl Prev Med. (2022) 28:533–5. doi: 10.3969/j.issn.1673-758X.2022.06.009
19. Li S, Tan CS, Chen JH. Analysis of the seroprevalence of the vaccine against the disease in pingxiang children under the age of 10. Drug Evaluation. (2016) 13(21):41–4. doi: 10.3969/j.issn.1672-2809.2016.21.010
20. Cheng J, Huo XX, Zhang C, Zhan FX, Yang BF, Zhan JB. Analysis of immune levels against measles, rubella and mumps in healthy population in Hubei province. Chin J Health Lab Technology. (2011) 21:2737–8,41. doi: CNKI:SUN:ZWJZ.0.2011-11-057l
21. Deng YB, Sheng RL, Tang SP. Results Analysis on Monitoring seroprevalence of Measles and Rubella among Health Population in Jinghe County. Endemic Dis Bulletin(China). (2016) 31:40–1,72. doi: 10.13215/j.cnki.jbyfkztb.1512022
22. Wang XL, Ding YX. The antibodies levels of measles, mumps and rubella in residents, Tianjin. Chin Prev Med. (2010) 11(5):491–4. doi: 10.16506/j.1009-6639.2010.05.014
23. Fan Y, He WQ, Liu YQ, Wen XY. Monitoring result of measles and rubella igG seroprevalence in healthy population in mianyang city in 2018. Occup Health Damage. (2020) 35:168–72.
24. li Li, Wang Y, QR Y, Liu Y, Fang QY. Investigation of seroprevalence of measles, rubella and mumps in Huizhou, Guangdong province. Modern Dis Control Prev. (2022) 33(12):939–42. doi: 10.13515/j.cnki.hnjpm.1006-8414.2022.12.014
25. Geng LN, Suan GW, Wu SN. Evaluation of rubella seroprevalence in health people in Xinyi City. Chin J School Doctor. (2017) 31:751–3. doi: CNKI:SUN:XIYI.0.2017-10-015
26. Gu F, Wang X, Wei WQ, Zhao XL, Lei CL. Surveillance on immunity levels of hepatitis B, measles, rubella, Japanese encephalitis, epidemic cerebrospinal meningitis among healthy populations in wolong district, nanyang city, 2010. Prev Med Tribune. (2012) 18:676–8. doi: 10.16406/j.pmt.issn.1672-9153.2012.09.019
27. Guan TJ, Huang H, Zheng YK, Zhu HX. Surveillance on immunity levels of rubella among populations in zhuhai city. Med Information. (2013) 7):254. 10.3969/j.issn.1006-1959.2013.07.250
28. Guo W, Wang Y, Yu H, Yu XQ, Wang J, Wang ZY, et al. Survey on levels of measles, rubella and mumps antibodies among normal population, dezhou city. Prev Med Tribune. (2013) 19:106–7+11. doi: 10.16406/j.pmt.issn.1672-9153.2013.02.012
29. Hao BY, Lu HZ, Shao HM, Zhang JL, Ren L, Wang LJ, et al. Monitoring and analysis of measles, mumps and rubella seroprevalence among healthy people in binhai new area of tianjin in 2020. Med Information. (2023) 36:60–3. doi: 10.3969/j.issn.1006-1959.2023.17.011
30. He PQ, Wang YM. Investigation on measles, rubella seroprevalence in Anding district of Dingxi city, 2015. Chin J Public Health Management. (2016) 32:504–6. doi: 10.19568/j.cnki.23-1318.2016.04.027
31. He Q, Xu Y, Li YL, Luo L, Zhu PT. seroprevalence against measles, rubella, and mumps among healthy people in Guangzhou: a cross-sectional survey in 2020. Chin J Vaccines Immunization. (2023) 29:392–6. doi: 10.19914/j.CJVI.2023067
32. Hu JY, Sheng J, Tang SW, Wang JG. Analysis on immunity to rubella among healthy people in Shanghai. Int J Biologicals. (2008) 31:200–2. doi: 10.3760/cma.j.issn.1673-4211.2008.05.003
33. Hu LY, Cheng GJ, Li FK, Xing ZH. Investigation of seroprevalence of measles and rubella in the urban of Nanyang City. Modern Dis Control Prev. (2017) 28:516–7. doi: 10.13515/j.cnki.hnjpm.1006-8414.2017.07.013
34. Hu YG, Wang AB, Guo J, Gao Y, luan RS. Surveillance of the antibodies against five vaccine-preventabl diseases among healthy population in Deyang City. Int J Virology. (2018) 25:349–53. doi: 10.3760/cma.j.issn.1673-4092.2018.05.017
35. Xing WY, Gao L, Zhu LS, Zhao PB, Xu WB, Hu RP. A retrospective survey of rubella seroprevalence among 0-15 year old healthy children and new mothers in two regions of China. Chin J Vaccines Immunization. (2018) 24(4):412–6. doi: 10.19914/j.cjvi.2018.04.009
36. Huang C, Tang JF, Liang LZ, Gan WY, Nong CS. Investigation of seroprevalence to measles, rubella and mumps in healthy populations of Nanning City in 2017-2019. J Community Med. (2023) 21:599–605. doi: 10.19790/j.cnki.JCM.2023.12.01
37. Yang C, Pei JX, Liang BY, Qing JQ, Nong CS, Huang C. Surveillance and control strategies of measles and rubella mumps’ seroprevalence in healthy population in Nanning in 2017. Chin J Health Lab Technology. (2019) 29(23):2825–27,2832. doi: CNKI:SUN:ZWJZ.0.2019-23-003
38. Huang N. Results Analysis on Monitoring seroprevalence of Rubella among Health Population in Changshun County in 2016. Diet Health. (2018) 5:281–2. doi: 10.3969/j.issn.2095-8439.2018.19.348
39. Ye N, Zhou YS, Huang QJ. seroprevalence of measles, rubella and mumps in healthy population in renshou county in 2018. Occup Health Damage. (2021) 36(5):286–90.
40. Lan X, Wei XP, Zhou XL, Huang XM. Rubella seroprevalence in healthy people in panzhihua city in 2015. J Prev Med Inf. (2018) 34(2):169–72. doi: CNKI:SUN:YFYX.0.2018-02-012
41. Shen WH, Lv YL, Liao MT, Lun XE, Jian MT. Survey on seroprevalence of rubella and pertussis in whole population of zhaoqing city in 2020. Chin Community Doctors. (2022) 38(19):151–3. doi: 10.3969/j.issn.1007-614x.2022.19.051
42. Yang AX, Li F. Analysis of immune level of EPI targeted diseases in Kuitun, Xinjiang. Bull Dis Control Prevention(China). (2016) 31(2):22–4,43. doi: 10.13215/j.cnki.jbyfkztb.1510030
43. Li JM, Li X, Huang YL. Monitoring and analyzing the levels of measles and rubella antibodies among healthy people in Karamay in 2014. Modern Prev Med. (2016) 43(18):3409–12. doi: CNKI:SUN:XDYF.0.2016-18-037
44. Li LJ, Qiu DS, Guan EF. Survey on levels of measles, rubella and mumps antibody among healthy population, weifang city,2011. Prev Med Tribune. (2013) 19:28–9. doi: 10.3969/j.issn.1005-5673.2013.01.012
45. Li P, Si Y, Guang RH. Levels of antibodies of measles,mumps and rubella in children of Shaanxi. Chin J Public Health. (2009) 25:1229–30. doi: 10.11847/zgggws2009-25-10-40
46. Li WX, Wang CY, Song LZ, Fang XQ, Xu Q. Survey on levels of measles, mumps and rubella antibodies among normal children in the west of shandong province,2010. Prev Med Tribune. (2012) 18:184–6. doi: 10.16406/j.pmt.issn.1672-9153.2012.03.013
47. Liu XL, Hu GX, Liang LL. Epidemiological characteristics of rubella and seroprevalence in healthy population in Tongchuan City, Shaanxi Province, China. Chin J Biologicals. (2020) 33(11):1276–9,1291. doi: 10.13200/j.cnki.cjb.003198
48. Lin Q, Zhang M, Zhang Y. Survey on establishment of rubella immune barrier in natural population in Dalian City. Occupation Health. (2020) 36:371–4. 10.13329/j.cnki.zyyjk.2020.0098
49. Liu DS, Song XZ, Liu XY. Survey on seroprevalence of measles, rubella and mumps in healthy population in suining county in 2016. Chin J School Doctor. (2018) 32:112+4. doi: CNKI:SUN:XIYI.0.2018-02-014
50. Xu CH, He JL, Tong WB, Liu L. Levels of antibody to measles, rubella and mumps viruses in a healthy population in Sichuan province in 2018. Chin J Exp Clin Virology. (2020) 34(01):29–32. doi: 10.3760/cma.j.issn.1003-9279.2020.01.006
51. Liu Y, Xu YY, Zhang XC, Yuan HY, Suan XJ, Chen J, et al. IgG seroprevalence against rubella among a healthy population in Hangzhou city, 2016-2018. Chin J Vaccines Immunization. (2020) 26:517–20. doi: 10.19914/j.cjvi.2020.05.007
52. Liu Y, Li WW, Zhang YY. Surveillance on measles and rubella seroprevalence among couples in a preconception care program in Hechuan District of Chongqing Municipality. Pract Prev Med. (2022) 29:112–4. doi: 10.26914/c.cnkihy.2023.035263
53. Liu Y, Wu YY, Wang Q. seroprevalence of measles and rubella among healthy population aged 1-30 years in Chongqing municipality. Pract Prev Med. (2020) 27:1220–2. doi: 10.3969/j.issn.1006-3110.2020.10.016
54. Liu Y, Liu Y, Li YQ, Liu JJ, Liu LJ, Yang Q, et al. Measles, rubella, and mumps seroprevalence among 0-6-year-old children in Sichuan province in 2022. Chin J Vaccines Immunization. (2023) 29:508–11. doi: 10.19914/j.CJVI.2023088
55. Lu HM, Sheng JH, Cheng WH, Zhu Q, Gu SK. Surveillance of measles, rubella and mumps seroprevalence in healthy population in Songjiang District, Shanghai. Chin J Biologicals. (2016) 29:51–6. doi: 10.13200/j.cnki.cjb.001201
56. Lv WY, Shi LB, Wang Y, Feng DX, Li GW, Yang JH, et al. seroprevalence of measles, rubella and mumps in a healthy population in Henan province,2016. Chin J Vaccines Immunization. (2017) 23:393–6,418. doi: 10.19914/j.cjvi.2017.04.009
57. Lv WY, Wang Y, Shi LB, Feng DX, Li GW, Yang JH, et al. Antibody levels of measles, rubella and mumps in a healthy population in Henan Province in 2015. Chin J Vaccines Immunization. (2016) 22:530–2,14. doi: 10.19914/j.cjvi.2016.05.011
58. Yang Y, Cheng ZJ, Hou TJ, Wu R, Liu JF, Ma CF. Seroprevalence of Antibody against Measles and Rubella among Children Aged 2-5 Years in Xi'an City of Shaanxi Province. Chin J Vaccines Immunization. (2016) 22(04):395–8+394. doi: 10.19914/j.cjvi.2016.04.008
59. Wu MX, Li JY, Ma SS. Analysis of Immune level of Measles and Rubella in Huli district in 2016. Strait J Prev Med. (2017) 23(6):3. doi: CNKI:SUN:HXYF.0.2017-06-020
60. Ma Y, Hu WJ, Lv T, Zhang XY, Liu CS, Zhang XH, et al. Measles, rubella and mumps seroprevalence in healthy people in Shaanxi province, 2017. Chin J Vaccines Immunization. (2019) 25:405–8+35. doi: 10.19914/j.cjvi.2019.04.010
61. Zhang FX, Li HC, Si Y, Ma Y. Survey on seroprevalence of measles, rubella and mumps in healthy population in zhidan county. Chin J Dis Control Prev. (2013) 17(11):2. doi: CNKI:SUN:JBKZ.0.2013-11-026
62. Pang H, Zhang ZS, Liu HL, Xu YS. Investigation of measles, rubella and varicella igG seroprevalence among migrant and native pupils in changning district of shanghai. Chin J Vaccines Immunization. (2009) 15:223–5. doi: 10.19914/j.cjvi.2009.03.014
63. Qi QR, Yang ZJ, Sun LN. Surveillance and analysis of rubella seroprevalence in school-age children in Hualong district, Puyang City. Appl Prev Med. (2019) 25(1):2. doi: CNKI:SUN:GXYX.0.2019-01-020
64. Wang AQ, Cheng GZ, Qiu DS. Survey on the seroprevalence of measles, rubella and mumps among the normal healthy population in Weifang. Prog Microbiol Immunol. (2013) 41(01):52–4. doi: 10.3969/j.issn.1005-5673.2013.01.012
65. Qiu XB, He G. Analysis of measles, rubella and mumps seroprevalence in healthy people in Suining City. J Prev Med Information. (2014) 30:682–3. doi: CNKI:SUN:YFYX.0.2014-08-029
66. Ruan JW, Hong LC, Hu PW, Yu JT, Yu MH, Cheng H, et al. Investigation on seroprevalence of measles, rubella, and mumps among freshmen in Shenzhen in 202. Modern Prev Med. (2023) 50:3999–4003. doi: 10.20043/j.cnki.MPM.202305505
67. Sheng WH, Kong DL, Li BH, Zhu BL, Liao TM, Li YH, et al. Investigation of seroprevalence of Measles, Rubella and Mumps among Whole Population in Zhaoqing, Guangdong Province, 2012. Chin J Vaccines Immunization. (2015) 21:519–23,42. doi: 10.19914/j.cjvi.2015.05.010
68. Shi ZH, Niu HM, Li Q, Huo T. Monitoring and analysis of measles and rubella IgG seroprevalence in healthy people in Gaobeidian city in 2014. Electronic J Clin Med Literature. (2016) 3:7273–4. doi: 10.16281/j.cnki.jocml.2016.36.122
69. Shu XD, Zhao H, Ping JM, Xu LR. Analysis of the serum seroprevalence of measles and rubella in healthy population of Yinzhou District, Ningbo. Chin J Health Lab Technology. (2016) 26:3306–9,22. doi: CNKI:SUN:ZWJZ.0.2016-22-037
70. Tang XM, Zhu Q, Ye XF, Ren G, Xu F. Investigation of rubella seroprevalence in healthy population in rural area of Guizhou Province. Guizhou Med J. (2013) 37:348–50. doi: 10.3969/j.ISSN.1000-744X.2013.04.024
71. Turhong MUSA, Ayiguzaili SIMAYI, Liu SD, Wu M. Surveillance of seroprevalence of measles and rubella among healthy children aged from 9 months to 6 years. Bull Dis Control Prevention(China). (2021) 36:50–3. doi: 10.13215/j.cnki.jbyfkztb.2010001
72. Wang CY, Xu Q, Song LZ, Fang XQ, Li WX, Xu AQ. Analysis on serum levels of rubella antibodies among healthy people in shandong province. Chin J Vaccines Immunization. (2013) 19(4):4. doi: CNKI:SUN:ZGJM.0.2013-04-014
73. Wang J, Yuan YL. Surveillance of seroprevalence of measles, rubella and mumps in healthy people in Jiaozuo city of Henen province, 2019-2021. Modern Dis Control Prev. (2023) 34:452–6. doi: 10.13515/j.cnki.hnjpm.1006-8414.2023.06.012
74. Wang MC, Bu JQ, Miao W, Hu SF, Song YJ, Li R, et al. Investigation on seroprevalence of measles, rubella and epidemic mumps in rizhao healthyPopulation. Occupation Health. (2010) 26:1980–1. doi: 10.13329/j.cnki.zyyjk.2010.17.016
75. Wang T. Monitoring of rubella and mumps seroprevalence among healthy population in changping district beijing. Pract Prev Med. (2012) 19:45–7. doi: 10.3969/j.issn.1006-3110.2012.01.015
76. Wang WS, An XH, Zhu LJ, Zhao L, Han LX, Fang X, et al. Serological analysis on antibody levels to measles, rubella and mumps in healthy people in different age groups in Liaoning, 2020. Dis Surveillance. (2022) 37:1290–3. doi: 10.3784/jbjc.202203210110
77. Wang YL, Ling GW. Surveillance results of measles and rubella immunity in Xianju County. Zhejiang Prev Med. (2012) 24:30–1. doi: 10.19485/j.cnki.issn1007-0931.2012.07.009
78. Wu R, Xue SF, Zhang YT, Kang JJ, Zhang WQ. seroprevalence of measles and rubella in a healthy population in Bole city of Xinjiang Uygur Autonomous Region, 2016. Chinese. J Vaccines Immunization. (2018) 24:422–+8. doi: 10.19914/j.cjvi.2018.04.011
79. Hu Y, Lu PS, Deng XY, Liu YB, Leng HY, Wu Y. Analysis of measles, rubella and mumps seroprevalence in healthy people in Jiangsu province in 2012. Chin J Health Laboratory. (2013) 23(12):2650–4. doi: CNKI:SUN:ZWJZ.0.2013-12-032
80. Wu FY, He RW, Wu ZL, Xu F, Zheng M, Zhao HP, et al. Measles and rubella seroprevalence in healthy population of JiangXi, 2015-2020. Modern Prev Med. (2021) 48:1160–4.
81. Xing QM, Su N, Wu DP. Surveillance on immunity levels of measles, rubella, tetanus, varicella among healthy populations in Panyu district, GuangZhou. J Med Pest Control. (2016) 32:723–5+8. doi: 10.7629/yxdwfz201607005
82. Xu Q, Wang CY, Fang XQ, Song LZ, Li WX, Liu XD, et al. Analysis on serum level of antibodies of measles and rubella among college students in shandong. Chin J Vaccines Immunization. (2015) 21(5):515–8. doi: CNKI:SUN:ZGJM.0.2015-05-011
83. Xuehelaiti· B, Yeerjiang· B. Comparative Analysis of seroprevalence of Measles, Rubella and Mumps among Different Healthy People in Qapqal County. World Latest Med Information. (2018) 18:7–8+43. doi: 10.19613/j.cnki.1671-3141.2018.69.004
84. Zhu HM, Pan YZ, Xue M. Investigation on the seroprevalence of measles rubella and mumps in Wujin district of ChangZhou City. Zhejiang Prev Med. (2015) 27(01):55–56+59. doi: 10.19485/j.cnki.issn1007-0931.2015.01.015
85. Yan R, Li JR, Zhou Y, He HQ, Deng X, Tang XW, et al. Rubella seroprevalence among 0-59-year-old healthy people of Zhejiang province in 2020. Chin J Vaccines Immunization. (2023) 29:300–4. doi: 10.19914/j.CJVI.2023051
86. Zhang RP, Yang DM, Tian YQ, Cao Y, Kang XL, Wang XM, et al. Surveillance on measles, rubella and mumps seroprevalence of primary and secondary school students in Fuling district of Chongqing. Chin J School Health. (2016) 37(5):721–3. doi: 10.16835/j.cnki.1000-9817.2016.05.025
87. Yang JP, Li XJ, Xu HQ, Wang Y, Wang Y, Yang XT. Surveillance of measles, rubella and mumps seroprevalence in healthy population in Baoshan District, Shanghai. Chin J Biologicals. (2018) 31:276–9+86. doi: 10.13200/j.cnki.cjb.002120
88. Yang YN, Tong ZQ, Yang S. Monitoring of measles and rubella seroprevalence among people aged 1-79 years in a district of Luoyang city, Henan province in 2021. Modern Dis Control Prev. (2023) 34(4):280–2,302. doi: 10.13515/j.cnki.hnjpm.1006-8414.2023.04.010
89. Wang J, Gan L, He AX, Yang YF. Analysis of seroprevalence of measles, rubella, mumps of healthy population in Yingshan in 2014. J North Sichuan Med College. (2016) 31:126–9. doi: 10.3969/j.issn.1005-3697.2016.01.36
90. Yang YY, Tang SW, Tang W, Fan JL, Li Z, Yang JW, et al. seroprevalence of measles, rubella and mumps viruses in healthy population in Shanghai from 2010 to 2020. Chin J Prev Med. (2022) 56:1095–100. doi: 10.3760/cma.j.cn112150-20211116-01057
91. Ye ZD, Zhang X, Chen X, Zhang J, Yuan P. Measles, rubella and mumps seroprevalence in healthy population under 15 years in zigong city in 2018. J Prev Med Information. (2021) 37:472–7.
92. Zhang AN. Investigation on the seroprevalence of measles and rubella in college students in jilin province. China: Jilin University (2019).
93. Zhang FX, He L, Wu RQ, Wu JN, Yang WL, Yang XD, et al. Monitoring Result of rubella seroprevalence in healthy population in Yanan city. Chin Prev Med. (2011) 12:454. doi: CNKI:SUN:ZGYC.0.2011-06-002
94. Zhang LW. Surveillance on rubella seroprevalence in healthy population in Changping district in Beijng, 2007. Dis Surveillance. (2009) 24:181–2. doi: 10.3784/j.issn.1003-9961.2009.03.09
95. Cheng XZ, Li SG, Ma HW, Shan FX, Mo J, Lin LQ, et al. Rubella seroprevalence among immigrant workers in Shenzhen. Chin J Public Health. (2010) 26(10):1330–1. doi: 10.11847/zgggws2010-26-10-66
96. Sun TT, Zhang YJ. Investigation on seroprevalence of 6 vaccines preventabl diseases among healthy people in a county of Zhumadian city, 2021. Bull Dis Control Prevention(China). (2023) 38(3):17–20. doi: 10.13215/j.cnki.jbyfkztb.2303024
97. Zhu HL, Ji JM, He B. Epidemiological characteristics and control effect of rubella in jiaxing city, Zhejiang province, 2004-2013. Chin Rural Health Service Administration. (2016) 36:749–51. doi: CNKI:SUN:ZNWS.0.2016-06-025
98. Cheng H, Guo MY, Wang Y, Jiang QL. Analysis of four kinds of seroprevalence in healthy people in Qiqihaer City. Sci Technological Innovation. (2016) 35):78. doi: 10.3969/j.issn.1673-1328.2016.35.066
99. Luo J, Wu GX, Tang XM. Monitoring Result of rubella seroprevalence in healthy population in Changshun County in 2011. World Latest Med Information. (2013) 29):215–,7. doi: 10.3969/j.issn.1671-3141.2013.29.184
100. Luo FJ, Liu F, Zhang XX, Zhang J, Wang C, Wang HW, et al. Investigation on the seroprevalence of rubella and mumps among the floating population in Chaoyang District, Beijing. Chin J Epidemiol. (2008) 07):741–2. doi: 10.3321/j.issn:0254-6450.2008.07.031
101. Lai WZ, Zhang SJ, Fang ML, Li FC, Nie Y, Li H, et al. Rubella seroprevalence in a healthy population 0-19 years of age in three counties of Hunan province, 2020-2022. Chin J Vaccines Immunization. (2023) 29:655–60. doi: 10.19914/j.CJVI.2023114
102. Lin W, Wang D, Xiong Y, Tang H, Liao Z, Ni J. Rubella seroprevalence among the general population in dongguan, China. Japanese J Infect diseases. (2015) 68:192–5. doi: 10.7883/yoken.JJID.2014.255
103. Wang J, Xu Y, Wang X, Liu Y, Zhang X, Du J, et al. Epidemiological characteristic of rubella by age group during 12 years after the national introduction of rubella vaccine in Hangzhou, China. Hum Vaccines immunotherapeutics. (2022) 18:2054208. doi: 10.1080/21645515.2022.2054208
104. Wang X, Xu Y, Zhang X, Zhang X, Du J, Che X, et al. Do adolescents need a rubella vaccination campaign Rubella serosurvey among healthy children in Hangzhou, China. Hum Vaccines immunotherapeutics. (2023) 19:2254536. doi: 10.1080/21645515.2023.2254536
105. Liu Y, Xu WB, Zhu Z. Progress in control and elimination of rubella in China. Natl Med J China. (2021) 48):3981–6. doi: 10.3760/cma.j.cn112137-20211009-02229
106. Plotkin SA. Rubella eradication: not yet accomplished, but entirely feasible. J Infect Dis. (2021) 224:S360–s6. doi: 10.1093/infdis/jiaa530
107. World Health Organization. Measles and rubella strategic framework 2021-2030. Geneva: World Health Organization (2020). Available at: https://www.who.int/publications/i/item/measles-and-rubella-strategic-framework-2021-2030.
108. Wang FS, Peng XR, Xiao L, Liu Y, Wang HJ, Li B, et al. Monitoring and analysis of successful rate of basic mumps immunization as well as multiplecropping effects of measles and rubella induced by measles-mumps-rubella vaccine in Shunyi District, Beijing, China in 2015. Chin J Biologicals. (2016) 29:844–6. doi: 10.13200/j.cnki.cjb.001429
109. Zhan HC, Chen YH, Huang CH, Chen WT. The analysis of epidemiology of rubella in Quanzhou province China, 2008-2015. J Dis Monitor Control. (2016) 10:903–5.
110. Schenk J, Abrams S, Theeten H, Van Damme P, Beutels P, Hens N. Immunogenicity and persistence of trivalent measles, mumps, and rubella vaccines: a systematic review and meta-analysis. Lancet Infect diseases. (2021) 21:286–95. doi: 10.1016/S1473-3099(20)30442-4
111. National Health Commission of the People's Republic of China. Circular of the National Health Commission on lssuing the lmmunization Procedures and Instructions for Children Under the National lmmunization Program(2021 edition) Vol. 02). China: Gazette of the National Health Commission of the People's Republic of China (2021) p. 13–22.
112. Xu Q, Xu AQ, Song LZ, Zhang L, Xiao ZK, Wang CY, et al. Analysis on the changing of age patterns among rubella patients after rubella vaccine immunization for children in Shandong province, China. Chin J Epidemiol. (2005) 11):33–5. doi: 10.3760/j.issn:0254-6450.2005.11.007
113. A.Orenstein W, A.Offit P, M.Edwards K, Stanley A. Plotkin. In: Plotkin's vaccines, 8th Edition. Elsevier, UK (2023).
114. He HQ, Xie SY, Li Q, Yan R, Zhou Y, Deng X, et al. Serologic and Epidemiological Effect of Rubella-containing Vaccine lmmunization Activities among Third-year Students of Middle School in Some Areas of Zhejiang Province. Chin J Vaccines Immunization. (2016) 22:20–3. doi: 10.19914/j.cjvi.2016.01.004
115. World Health Organization. Rubella vaccines:WHO position paper-July 2020 (2020). Available online at: https://www.who.int/publications/i/item/WHO-WER9527. (Accessed July 3, 2020)
116. Ding YX, Liu Y, Xu EY, Chang LM, Su QR, Gou HC, et al. lmmunogenicity and safety of measles, mumps and rubella combined attenuated live vaccine in revaccination of children and in vaccination of childbearing-age women. Chin J Vaccines Immunization. (2017) 23:365–8. doi: 10.19914/j.cjvi.2017.04.002
117. Chen ZF, Zhou Y, Yang XH, Chen JL, Li D, Zhang SH, et al. Epidemiological characteristics of rubella before and after introduction of rubella vaccine into the immunization program in Fujian province. Chin J Vaccines Immunization. (2019) 25(01):37–40+53. doi: 10.19914/j.cjvi.2019.01.009
118. Zhu Q, Hu TJ, Shen JW, Shen JH, Chen WH, Gu SK, et al. A study on measles and rubella antibody level in 319 pairs of mothers and infants in Songjiang District of Shanghai. Chin Med J. (2019) 53:388–93. doi: 10.3760/cma.j.issn.0253-9624.2019.04.011
119. Ma R, Xu GZ, Ma C, An ZJ, Xu HJ, Ma YH, et al. Change of rubella antibody transferred by mother in infants. Chin J Vaccines Immunization. (2009) 15:429–31. doi: 10.19914/j.cjvi.2009.05.016
120. Su Q, Ma C, Wen N, Fan C, Yang H, Wang H, et al. Epidemiological profile and progress toward rubella elimination in China. 10 years after nationwide introduction of rubella vaccine. Vaccine. (2018) 36:2079–85. doi: 10.1016/j.vaccine.2018.03.013
Keywords: rubella, IgG antibody, vaccination, Chinese population, meta-analysis
Citation: Zhuo Y, Lu Z, Zhang X, Zhang X, Yang Y, Han J, Du J, Xu Y, Liu Y and Fu C (2024) Rubella antibody levels in the healthy Chinese population: a meta-analysis. Front. Immunol. 15:1472189. doi: 10.3389/fimmu.2024.1472189
Received: 29 July 2024; Accepted: 21 October 2024;
Published: 12 November 2024.
Edited by:
Pei-Hui Wang, Shandong University, ChinaReviewed by:
Stephen Crooke, Centers for Disease Control and Prevention (CDC), United StatesCopyright © 2024 Zhuo, Lu, Zhang, Zhang, Yang, Han, Du, Xu, Liu and Fu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yan Liu, c21pbGVmb3JldmVyODFAMTI2LmNvbQ==; Chuanxi Fu, ZnVjaHVhbnhpQHpjbXUuZWR1LmNu
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.